Introduction
Metabolic syndrome mainly refers to a group of
pathophysiological changes based on insulin resistance (1), the major clinical manifestations are
central obesity, increase in blood glucose, increase in blood lipid
and increase in blood pressure, seriously affecting the physical
health of patients. The above clinical manifestations of metabolic
syndrome, as a metabolic dysfunction-related disease (2), have certain common risk factors, which
are in line with the ‘concept of holism, homotherapy for
heteropathy’ in the traditional Chinese medicine. It is of
important significance to effectively intervene in patients with
cardiovascular diseases, such as hypertension, and endocrine
diseases (like type 2 diabetes mellitus) (3), alleviate or avoid the occurrence of
insulin resistance and make full use of the concept of ‘preventive
treatment of disease’, namely ‘prevention before disease onset,
prevention of disease from exacerbating’, in the traditional
Chinese medicine, thereby increasing the therapeutic effect on
metabolic syndrome and improving the prognosis of patients
(4).
Berberine, also known as Berberine hydrochloride in
clinic, is the isoquinoline alkaloid, an active ingredient
extracted from Chinese herbal medicines, such as Coptis
chinensis and Phellodendron amurense, which has dominant
advantages such as reducing blood glucose, and regulating blood
lipid and vascular endothelial cells (5). In recent years, berberine has been
widely used in the treatment of type 2 diabetes mellitus,
hypertension and hyperlipidemia (6).
With the deepening of fundamental research on berberine, it has
been confirmed that the main mechanisms of berberine in reducing
blood glucose and blood pressure and regulating blood lipid are
promotion of insulin secretion and improvement of the body's
insulin resistance (7). To better
investigate the clinical value of berberine in the treatment of
metabolic syndrome, this study was performed from the perspectives
of blood glucose, blood lipid, insulin resistance and inflammatory
factor levels.
Patients and methods
Patient data
A total of 80 patients with metabolic syndrome
treated in Linyi Central Hospital (Linyi, China) from January 2017
to December 2017 were selected. All patients met the diagnostic
criteria of the Chinese Medical Association (8) for type 2 diabetes mellitus,
hyperlipidemia and hypertension. Before enrollment, patients signed
an informed consent, and this study was approved by the Ethics
Committee of Linyi Central Hospital. Patients enrolled were aged
60–80 years, and they were physically healthy in the past.
Exclusion criteria: i) Patients complicated with other endocrine
system diseases, mental diseases, malignant tumor or chronic
obstructive pulmonary disease, ii) patients who were illiterate,
allergic to drugs applied or could not pay the medical expenses.
Patients were divided into two groups with 40 cases in each group
using the random number method. There were no statistically
significant differences in comparisons of general data and related
indexes between the two groups (P>0.05) (Table I).
 | Table I.Comparison of general data and related
indexes between the two groups (mean ± SD). |
Table I.
Comparison of general data and related
indexes between the two groups (mean ± SD).
| Group | Sex
(male/female) | Age (years) | Fasting blood glucose
(mmol/l) | 2 h postprandial
blood glucose (mmol/l) | Insulin
resistance |
|---|
| Observation
group | 20/20 | 65.6±1.8 | 10.5±0.6 | 13.5±1.3 | 1.5±0.1 |
| Control group | 20/20 | 65.5±1.8 | 10.6±0.6 | 13.6±1.3 | 1.5±0.1 |
| χ2 or t
value | <0.001 | 0.248 | 0.745 | 0.344 | <0.001 |
| P-value | >0.05 | 0.804 | 0.458 | 0.732 | >0.05 |
|
| Continued |
|
| Group | Triglyceride
(mmol/l) | Total cholesterol
(mmol/l) | Interleukin-6
(IL-6) (ng/l) | Tumor necrosis
factor-α (TNF-α) (ng/l) | High-sensitivity
C-reactive protein (hs-CRP) (ml/l) |
|
| Observation
group | 2.53±0.13 | 6.11±0.09 | 0.69±0.05 | 253.1±2.1 | 25.6±1.3 |
| Control group | 2.55±0.13 | 6.12±0.10 | 0.70±0.05 | 253.6±2.0 | 25.7±1.4 |
| χ2 or t
value | 0.688 | 0.470 | 0.894 | 1.090 | 0.331 |
| P-value | 0.493 | 0.640 | 0.374 | 0.279 | 0.742 |
Methods
Patients in control group were treated with regular
therapy using the Western medicine and drugs strictly in accordance
with the treatment guidelines of metabolic syndrome of the Chinese
Medical Association. First of all, the weight of patients was
reduced, the diet adjustment was strengthened, and the body mass
index ≤28. Patients exercised properly according to the body's
tolerance, and it was recommended that they take part in
light-moderate physical activity every day for half an hour. In
addition, the insulin resistance was reduced, in other words, the
blood glucose-regulating drugs, such as metformin and insulin
sensitizing drug thiazolidinedione, were applied while diet and
exercise interventions were performed. At the same time, the
intervention in hyperlipidemia was also performed, and it was
advised that fibrates and statins be applied. Finally, the
patient's blood pressure was adjusted and controlled within 130/80
mmHg. In terms of antihypertensive drugs, angiotensin-converting
enzyme inhibitor (ACEI) and/or angiotensin II receptor antagonist
(ARB) were preferred choices. Patients in observation group, based
on the treatment in control group, were treated with berberine
(Jiangxi Sinopharm Co., Ltd., Jiangxi, China, NMPN Z36020766) 3
times a day (4 tablets/time).
Observation indexes
All patients were followed up for 1 month. Changes
in relevant indexes to blood glucose and lipid metabolisms and
inflammatory factors were compared between the two groups at 1 week
and 1 month after treatment. The correlations of inflammatory
factor hs-CRP with fasting blood glucose, insulin resistance,
triglyceride and total cholesterol were analyzed.
Evaluation criteria
Related detection indexes to blood glucose included
fasting blood glucose (3.9–6.1 mmol/l), 2 h postprandial blood
glucose (≤7.8 mmol/l) and homeostasis model assessment - insulin
resistance (HOMA-IR) [reference value: 1, calculation formula:
fasting blood glucose (mmol/l) × fasting insulin (mU/l)]. Related
indexes to blood lipid included triglyceride (0.56–1.71 mmol/l) and
total cholesterol (2.83–5.17 mmol/l). Inflammation-related factors
included hs-CRP (<10 ml/l), IL-6 (0.37–0.46 ng/l) and TNF-α
(5–100 ng/l).
Statistical analysis
SPSS 13.0 software (SPSS Inc., Chicago, IL, USA) was
used for statistical analysis. Measurement data are presented as
mean ± standard deviation (mean ±SD). Student's t-test was used for
the comparison of related indexes to blood glucose and lipid
metabolisms between the two groups at different observation points,
the Chi-square test (χ2) was used for the comparison of
adverse reactions between the two groups, and correlations of
hs-CRP with fasting blood glucose, insulin resistance, total
cholesterol and triglyceride were analyzed using the Pearson's
correlation coefficient method. The procedure was repeated 3 times.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Changes in related indexes to blood
glucose and lipid metabolisms in both groups at 1 week and 1 month
after treatment
At 1 month after treatment, levels of fasting blood
glucose, 2 h postprandial blood glucose and insulin resistance
index in both groups were lower than those at 1 week after
treatment (P<0.05), and levels of blood lipid indexes
(triglyceride and total cholesterol) were also lower than those at
1 week after treatment (P<0.05). At 1 month after treatment,
levels of fasting blood glucose, 2 h postprandial blood glucose and
insulin resistance index in observation group were significantly
decreased compared with those in control group during the same
period (P<0.05), and levels of blood lipid indexes (triglyceride
and total cholesterol) were also lowered compared with those in
control group during the same period (P<0.05) (Table II).
 | Table II.Changes in related indexes to blood
glucose and lipid metabolisms in both groups at 1 week and 1 month
after treatment (mean ± SD). |
Table II.
Changes in related indexes to blood
glucose and lipid metabolisms in both groups at 1 week and 1 month
after treatment (mean ± SD).
| Group | Treatment | Fasting blood glucose
(mmol/l) | 2 h postprandial
blood glucose (mmol/l) | Insulin
resistance | Triglyceride
(mmol/l) | Total cholesterol
(mmol/l) |
|---|
| Observation
group | 1 week after
treatment | 7.9±0.3 | 9.9±0.5 | 1.3±0.1 | 2.12±0.08 | 5.39±0.15 |
|
| 1 month after
treatment | 5.6±0.2a,b | 7.5±0.3a,b | 1.1±0.11a,b |
1.56±0.07a,b |
3.69±0.08a,b |
| Control group | 1 week after
treatment | 8.0±0.4 | 10.0±0.5 | 1.4±0.1 | 2.13±0.09 | 5.40±0.16 |
|
| 1 month after
treatment | 6.5±0.3a | 8.5±0.61a | 1.3±0.11a |
1.96±0.061a |
5.23±0.101a |
|
|
t1 | 40.345 | 26.032 | 8.944 | 33.318 | 62.129 |
|
|
p1 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
|
|
t2 | 18.974 | 12.147 | 4.472 | 9.940 | 5.698 |
|
|
p2 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
|
|
t3 | 15.787 | 9.428 | 8.944 | 27.440 | 76.055 |
|
|
p3 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
Changes in inflammatory factors in
both groups at 1 week and 1 month after treatment
Levels of hs-CRP, IL-6 and TNF-α in both groups at 1
month after treatment were lower than those at 1 week after
treatment (P<0.05), and they were lower in observation group at
1 month after treatment than those in control group during the same
period (P<0.05) (Table
III).
 | Table III.Changes in inflammatory factors in
both groups at 1 week and 1 month after treatment (mean ± SD). |
Table III.
Changes in inflammatory factors in
both groups at 1 week and 1 month after treatment (mean ± SD).
| Group | Treatment | hs-CRP (ml/l) | IL-6 (ng/l) | TNF-α (ng/l) |
|---|
| Observation
group | 1 week after
treatment | 12.3±0.5 | 0.59±0.06 | 136.8±11.1 |
|
| 1 month after
treatment |
8.5±0.3a,b |
0.43±0.04a,b |
83.2±7.6a,b |
| Control group | 1 week after
treatment | 14.6±0.6 | 0.68±0.06 | 146.5±11.3 |
|
| 1 month after
treatment |
11.6±0.4a |
0.51±0.05a |
108.9±8.3a |
|
|
t1 | 41.217 | 14.033 | 25.199 |
|
|
p1 | <0.001 | <0.001 | <0.001 |
|
|
t2 | 26.312 | 13.766 | 16.961 |
|
|
p2 | <0.001 | <0.001 | <0.001 |
|
|
t3 | 39.212 | 7.902 | 14.443 |
|
|
p3 | <0.001 | <0.001 | <0.001 |
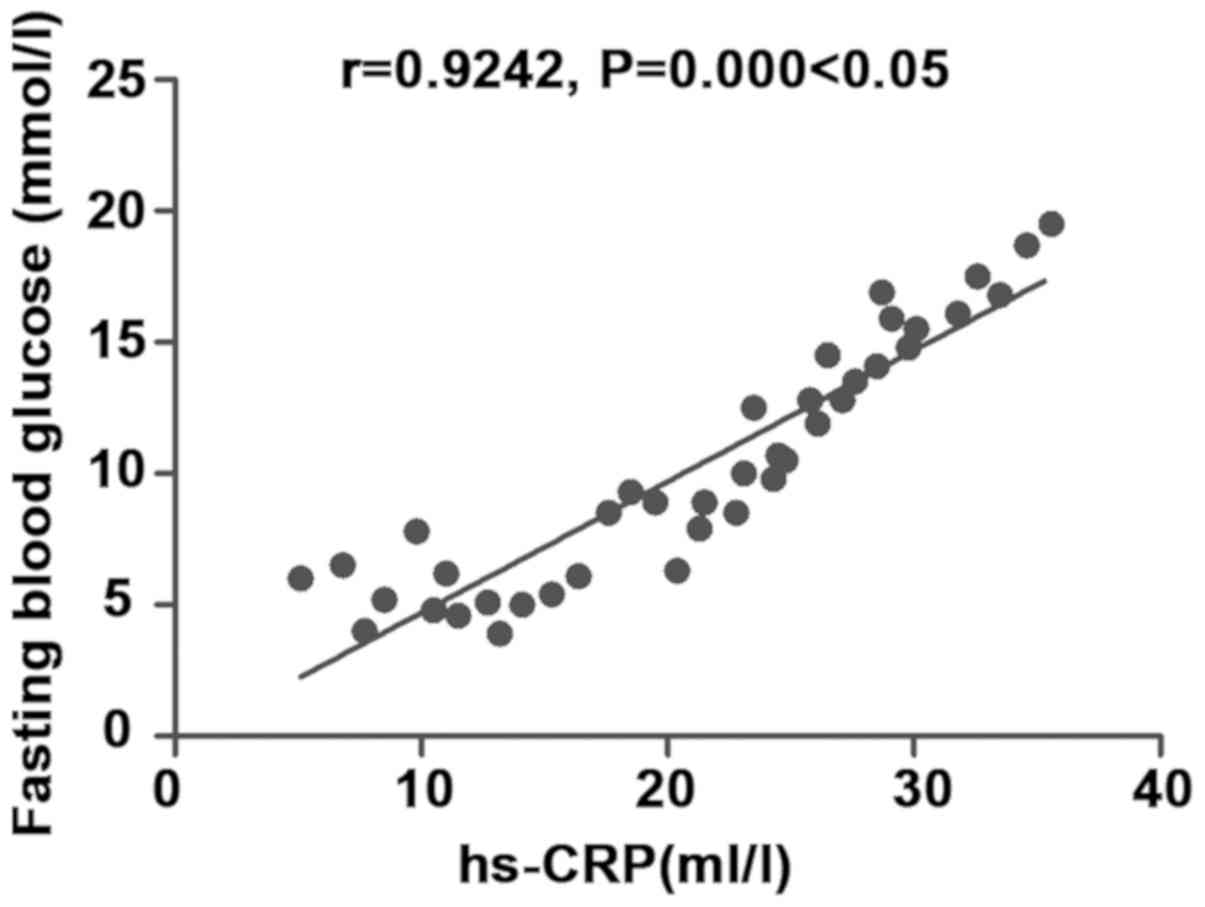
Correlation analysis of inflammatory
factor hs-CRP with fasting blood glucose
There was a positive correlation between
inflammatory factor hs-CRP and fasting blood glucose (r=0.9242,
P<0.05) (Fig. 1).
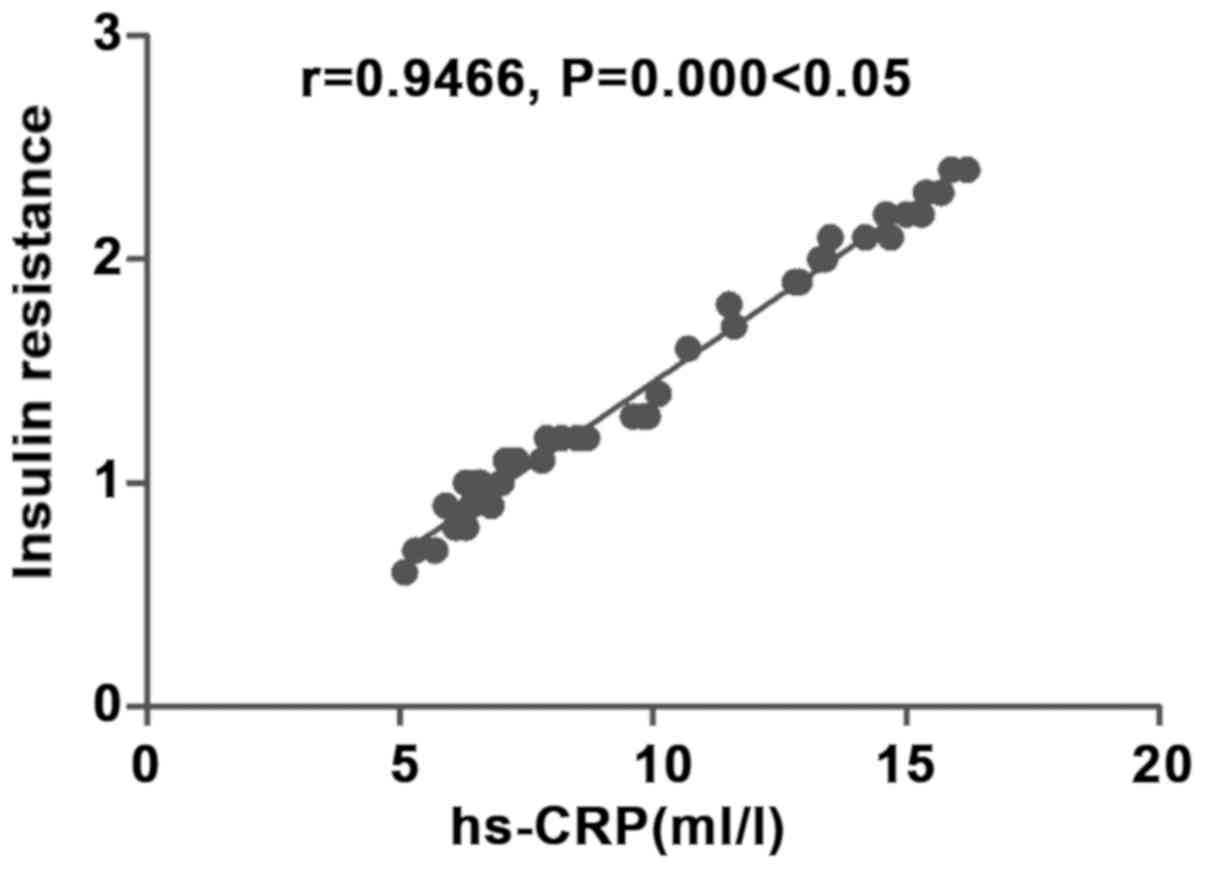
Correlation analysis of inflammatory
factor hs-CRP with insulin resistance
There was a positive correlation between
inflammatory factor hs-CRP and insulin resistance (r=0.9929,
P<0.05) (Fig. 2).
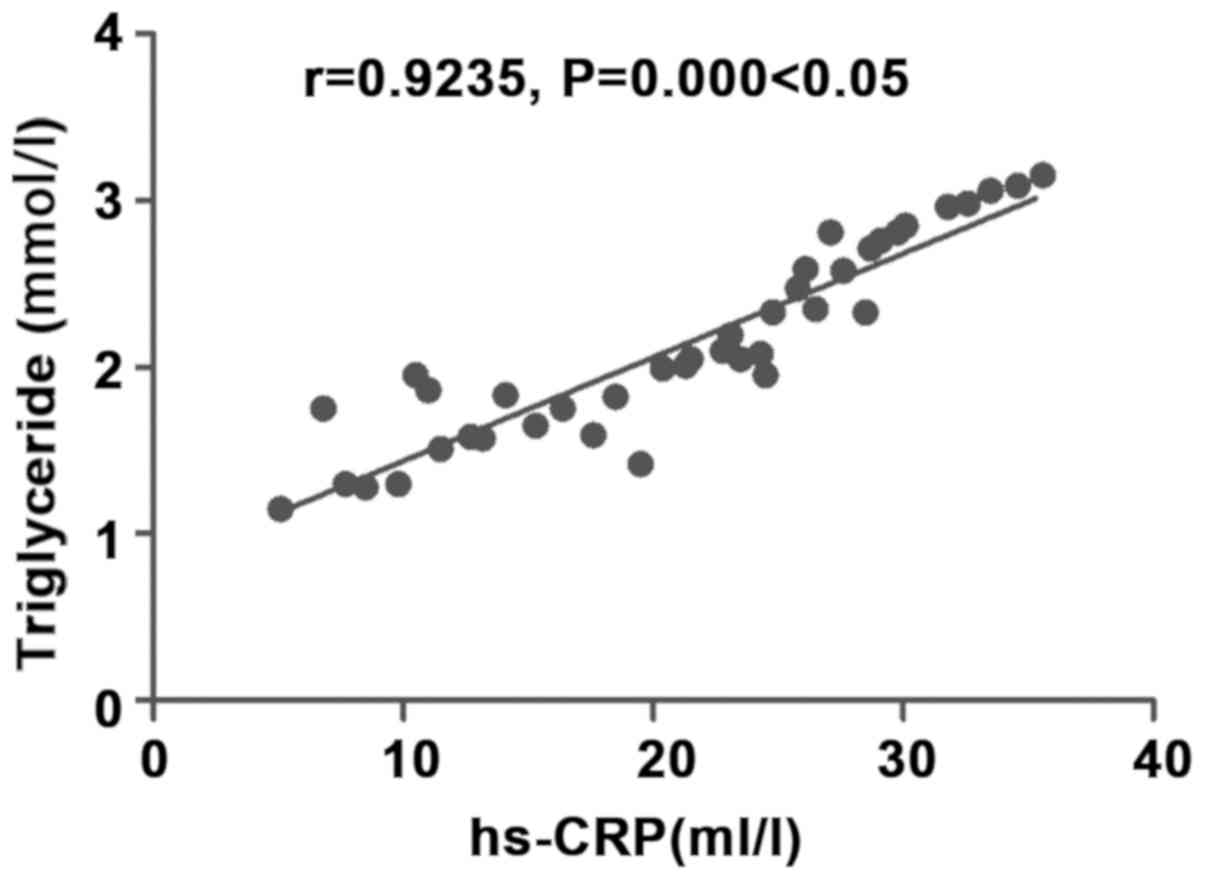
Correlation analysis of inflammatory
factor hs-CRP with triglyceride
There was a positive correlation between
inflammatory factor hs-CRP and triglyceride (r=0.9235, P<0.05)
(Fig. 3).
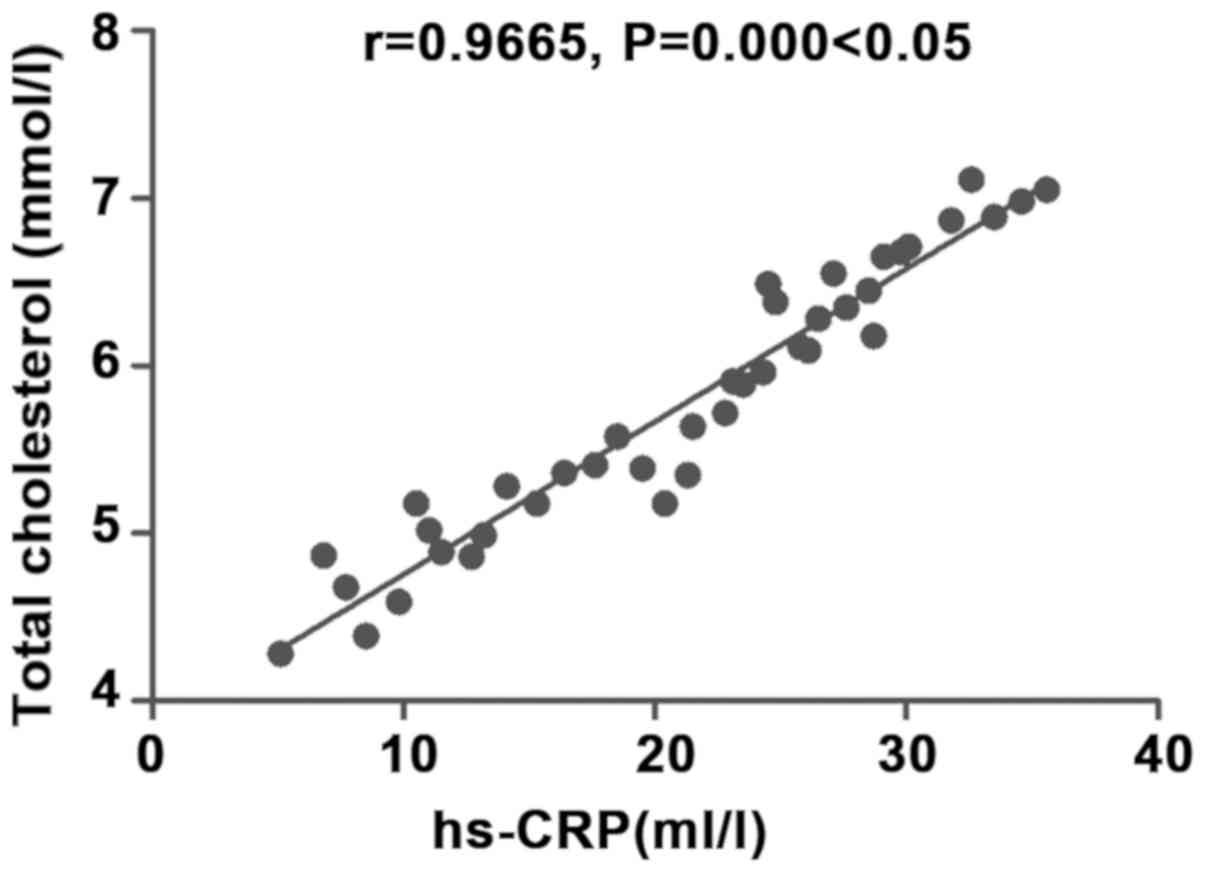
Correlation analysis of inflammatory
factor hs-CRP with total cholesterol
There was a positive correlation between
inflammatory factor hs-CRP and total cholesterol (r=0.9665,
P<0.05) (Fig. 4).
Comparison of adverse reactions
between the two groups
There was no statistically significant difference in
the overall incidence rate of adverse reactions, such as
ketoacidosis, hyperglycemic coma, hypoglycemia and nausea and
vomiting, between the two groups (P>0.05) (Table IV).
 | Table IV.Comparison of adverse reactions
between the two groups. |
Table IV.
Comparison of adverse reactions
between the two groups.
| Group | Ketoacidosis | Hyperglycemic
coma | Hypoglycemia | Nausea and
vomiting | Overall incidence
rate |
|---|
| Observation
group | 1 | 1 | 1 | 1 | 4 (10.0%) |
| Control group | 1 | 2 | 1 | 0 | 4 (10.0%) |
| χ2
value |
|
|
|
| <0.001 |
| P-value |
|
|
|
| <0.05 |
Discussion
Metabolic syndrome is a group of clinical syndromes
determined by heredity, environment, living habits and other
factors, whose main mechanism is insulin resistance (9). Patients have symptoms including central
obesity, atherosclerosis, rise of blood lipid, pathoglycemia and
elevation of blood pressure, which may be accompanied by
microalbuminuria, hyperuricemia and long-term rise of chronic
inflammatory cytokines (10).
Currently, most scholars consider that insulin resistance is the
most crucial independent risk factor and central link that lead to
metabolic syndrome (11). Treatment
for metabolic syndrome is based on improvement of patients' way of
life, regulation of eating habits, exercise training and loss of
weight, combined with drug therapy of reducing blood lipid and
regulating blood pressure and blood glucose (12). Berberine can regulate various
metabolic disorders of metabolic syndrome, which has advantages of
wide medicinal herbs resources, low price, smaller adverse
reactions, and is also safe and convenient (13).
In this study, patients with metabolic syndrome in
control group were given regular Western medicine treatment
strictly following guideline requirements, while those in
observation group received berberine treatment on the basis of that
in control group. By analyzing changes of related indexes to blood
glucose and lipid metabolisms in the groups at 1 week and 1 month
after treatment, it was found that related indexes to blood glucose
and lipid in both groups were improved at 1 month after treatment,
but levels of fasting blood glucose, 2 h postprandial blood glucose
and insulin resistance index in observation group were
significantly lower than those in control group at 1 month after
treatment, and levels of blood lipid indexes (triglyceride and
total cholesterol) in observation group were lower than those in
control group at 1 month after treatment, indicating that combined
use of berberine can regulate blood glucose and blood lipid levels
more effectively and lighten insulin resistance. By exploring
changes in relevant indexes of inflammatory factors in both groups
at 1 week and 1 month after treatment, it was found that hs-CRP,
IL-6 and TNF-α levels in both groups were also lower than those at
1 week after treatment, but hs-CRP, IL-6 and TNF-α levels in
observation group were all lower than those in control group at 1
month after treatment, indicating that combined use of berberine
tablets is of important significance for reducing inflammatory
reaction in patients with metabolic syndrome. From the correlation
research on inflammatory response factor hs-CRP with fasting blood
glucose, insulin resistance, total cholesterol and triglyceride, it
was revealed that hs-CRP was positively related to fasting blood
glucose, insulin resistance, total cholesterol and triglyceride,
which further indicates that there is chronic inflammatory response
in the body of patients with metabolic syndrome and the severity
degree of inflammatory response is related to blood glucose and
blood lipid metabolism. Chronic inflammatory response may also lead
to increase of insulin resistance in the body and further worsen
the disease condition. Besides, combined use of berberine tablets
did not increase the incidence of adverse reactions of treatment,
so combined use of berberine tablets is of high safety.
In this study, combined use of berberine could
effectively improve activity of adenosine monophosphate-activated
protein kinase (AMPK) of islet cells, thus promoting activation of
cyclic adenosine monophosphate (CAMP) signal pathway (14) and active secretion of insulin in the
body. Moreover, berberine can also stimulate free fatty acid to
induce secretion of insulin (15).
Berberine improves physiological stimulation of glucose via cascade
reaction of insulin-like growth factor-1 (IGF-1), thus inducing
secretion of insulin in the body, reducing insulin resistance, and
improving sensitivity of liver, muscle tissues and fat to insulin
(16). Berberine can improve the
activity and promote the proliferation of insulin β cells (17). Therefore, the combined use of
berberine in observation group could better control fasting blood
glucose and 2 h postprandial plasma glucose and reduce insulin
resistance in the body. Berberine inhibits synthesis and secretion
of proteolipid protein and activity of peroxisome by enhancing low
density lipoprotein receptor level and promoting
adenylate-phosphoric acid-activated protein kinase activity, thus
regulating blood lipid and inhibiting proliferation and
differentiation of adipocytes, so as to achieve the objective of
reducing free fatty acid in serum (18,19).
Consequently, triglyceride and total cholesterol decreased
significantly after combined use of berberine in observation group.
In addition, berberine can also evidently decrease levels of
hs-CRP, IL-6, TNF-α and other inflammatory cytokines in the body
(20), improve calcium overload and
ischemia reperfusion injury and provide anti-oxidative capacity
(21).
In conclusion, combined use of berberine for
patients with metabolic syndrome can effectively regulate blood
glucose and lipid, lighten insulin resistance in the body and
reduce inflammatory response level.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
CC wrote the manuscript and collected the general
data. CC and MS analyzed the relevant indexes to blood glucose and
lipid metabolisms and inflammatory factors. Both authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Linyi Central Hospital (Linyi, China) and informed consents were
signed by the patients or the guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Saleem F and Rizvi SW: New therapeutic
approaches in obesity and metabolic syndrome associated with
polycystic ovary syndrome. Cureus. 9:e18442017.PubMed/NCBI
|
|
2
|
Marchitto N, Sindona F, Fabrizio A, Mauti
M, Andreozzi S, Dalmaso S and Raimondi G: Effect of new
nutraceutical formulation with policosanol, berberine, red yeast
rice, cassia nomame, astaxantine and Q10 coenzyme in patients with
low-moderate dyslipidemia associated with intolerance to statins
and metabolic syndrome. Minerva Cardioangiol. 66:124–125.
2018.PubMed/NCBI
|
|
3
|
Liu Q, Zhu L, Cheng C, Hu YY and Feng Q:
Natural active compounds from plant food and chinese herbal
medicine for nonalcoholic fatty liver disease. Curr Pharm Des.
23:5136–5162. 2017.PubMed/NCBI
|
|
4
|
Dahlberg CJ, Ou JJ, Babish JG, Lamb JJ,
Eliason S, Brabazon H, Gao W, Kaadige MR and Tripp ML: A 13-week
low glycemic load diet and lifestyle modification program combining
low glycemic load protein shakes and targeted nutraceuticals
improved weight loss and cardio-metabolic risk factors. Can J
Physiol Pharmacol. 95:1414–1425. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sirtori CR, Pavanello C, Calabresi L and
Ruscica M: Nutraceutical approaches to metabolic syndrome. Ann Med.
49:678–697. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Guarino G, Strollo F, Carbone L, Della
Corte T, Letizia M, Marino G and Gentile S: Bioimpedance analysis,
metabolic effects and safety of the association Berberis
aristata/Bilybum marianum: A 52-week double-blind,
placebo-controlled study in obese patients with type 2 diabetes. J
Biol Regul Homeost Agents. 31:495–502. 2017.PubMed/NCBI
|
|
7
|
Tabeshpour J, Imenshahidi M and
Hosseinzadeh H: A review of the effects of Berberis vulgaris and
its major component, berberine, in metabolic syndrome. Iran J Basic
Med Sci. 20:557–568. 2017.PubMed/NCBI
|
|
8
|
Ong M, Peng J, Jin X and Qu X: Chinese
herbal medicine for the optimal management of polycystic ovary
syndrome. Am J Chin Med. 45:405–422. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lu YH, Lu JM, Wang SY, Li CL, Liu LS,
Zheng RP, Tian H, Wang XL, Yang LJ, Zhang YQ and Pan CY: Comparison
of the diagnostic criteria of metabolic syndrome by International
Diabetes Federation and that by Chinese Medical Association
Diabetes Branch. Zhonghua Yi Xue Za Zhi. 86:386–389. 2006.(In
Chinese). PubMed/NCBI
|
|
10
|
Zhao L, Cang Z, Sun H, Nie X, Wang N and
Lu Y: Berberine improves glucogenesis and lipid metabolism in
nonalcoholic fatty liver disease. BMC Endocr Disord. 17:132017.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Choi YJ, Lee KY, Jung SH, Kim HS, Shim G,
Kim MG, Oh YK, Oh SH, Jun DW and Lee BH: Activation of AMPK by
berberine induces hepatic lipid accumulation by upregulation of
fatty acid translocase CD36 in mice. Toxicol Appl Pharmacol.
316:74–82. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chow YL, Sogame M and Sato F:
13-Methylberberine, a berberine analogue with stronger
anti-adipogenic effects on mouse 3T3-L1 cells. Sci Rep.
6:381292016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
He Q, Mei D, Sha S, Fan S, Wang L and Dong
M: ERK-dependent mTOR pathway is involved in berberine-induced
autophagy in hepatic steatosis. J Mol Endocrinol. 57:251–260. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Li M, Shu X, Xu H, Zhang C, Yang L, Zhang
L and Ji G: Integrative analysis of metabolome and gut microbiota
in diet-induced hyperlipidemic rats treated with berberine
compounds. J Transl Med. 14:2372016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Millán J, Cicero AF, Torres F and Anguera
A: Effects of a nutraceutical combination containing berberine
(BRB), policosanol, and red yeast rice (RYR), on lipid profile in
hypercholesterolemic patients: A meta-analysis of randomised
controlled trials. Clin Investig Arterioscler. 28:178–187.
2016.PubMed/NCBI
|
|
16
|
Martínez-Abundis E, Méndez-Del Villar M,
Pérez-Rubio KG, Zuñiga LY, Cortez-Navarrete M, Ramírez-Rodriguez A
and González-Ortiz M: Novel nutraceutic therapies for the treatment
of metabolic syndrome. World J Diabetes. 7:142–152. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Caliceti C, Franco P, Spinozzi S, Roda A
and Cicero AF: Berberine: New insights from pharmacological aspects
to clinical evidences in the management of metabolic disorders.
Curr Med Chem. 23:1460–1476. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Patel S: Functional food red yeast rice
(RYR) for metabolic syndrome amelioration: A review on pros and
cons. World J Microbiol Biotechnol. 32:872016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Geng FH, Li GH, Zhang X, Zhang P, Dong MQ,
Zhao ZJ, Zhang Y, Dong L and Gao F: Berberine improves mesenteric
artery insulin sensitivity through up-regulating insulin
receptor-mediated signalling in diabetic rats. Br J Pharmacol.
173:1569–1579. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Oikawa N, Nobushi Y, Wada T, Sonoda K,
Okazaki Y, Tsutsumi S, Park YK, Kurokawa M, Shimba S and Yasukawa
K: Inhibitory effects of compounds isolated from the dried branches
and leaves of murta (Myrceugenia euosma) on lipid
accumulation in 3T3-L1 cells. J Nat Med. 70:502–509. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Cicero AF and Colletti A: Role of
phytochemicals in the management of metabolic syndrome.
Phytomedicine. 23:1134–1144. 2016. View Article : Google Scholar : PubMed/NCBI
|