Introduction
Congenital heart disease (CHD) is a common
congenital developmental malformation in pediatrics.
Cardiopulmonary bypass (CPB) is a representative technique of
cardiac surgery, and it has been increasingly improved and widely
popularized in recent years. However, CPB is an invasive treatment,
whose postoperative complications, such as postoperative infection,
low cardiac output syndrome, heart failure, arrhythmia and
bleeding, should be paid enough attention to. The surgical trauma,
low temperature, ischemia reperfusion and the contact with the
surface of artificial materials, such as the artificial tube during
CPB, can activate the immune system in the body, lead to activation
of inflammatory cells, coagulation system, complement system, white
blood cells (WBCs) and platelets, and release inflammatory factors
(1–3). Lipoxin A4 (LXA4),
as an important endogenous anti-inflammatory mediator, can reduce
the production of inflammatory factors and inhibit the activation
and chemotaxis of neutrophils (4).
This study compared the LXA4 levels between child
patients with CHD and non-CHD children, observed the dynamic
changes of LXA4 in the perioperative period of CPB, and
analyzed its correlation with blood routine indexes,
high-sensitivity C-reactive protein (hs-CRP) and other clinical
indexes, so as to find the correlation between LXA4 and
the inflammatory response of CHD.
Patients and methods
Clinical specimens
The clinical specimens used in this study were
obtained from child patients with CHD receiving CPB in the
Department of Cardiovascular Surgery of the Children's Hospital of
Soochow University (Suzhou, China), from February 2017 to December
2017. The children were aged from 10 days to 3 years without
genetic diseases and signs of acute infection. The study was
approved by the Ethics Committee of Children's Hospital of Soochow
University. Patients who participated in this research had complete
clinical data. Signed written informed consents were obtained from
the patients and/or their guardians.
All child patients received intravenous-inhalational
anesthesia and tracheal intubation, and extracorporeal circulation
was constructed via intubation in the aorta and superior and
inferior vena cava. Cold crystalloid cardioplegia (15–20 ml/kg), at
4°C, was injected into the aortic root of most patients for
myocardial protection, while HTK solution (50 ml/kg) was injected
into 1 case with complete transposition of the great artery and
into 1 case with left coronary anomaly. Conventional
ultrafiltration and modified ultrafiltration were combined (CUF +
MUF), and colloidal fluid was used as the priming fluid. There were
12 cases of low temperature (30-33°C) extracorporeal circulation, 3
cases of low to medium temperature (25-28°C) extracorporeal
circulation and 1 case of deep hypothermic circulatory arrest
(DHCA). All child patients had sinus cardiac re-beat, and
extracorporeal circulation was withdrawn successfully after
complete rewarming. Patients were routinely admitted into the
Pediatric Intensive Care Unit (PICU) and returned to the
Cardiothoracic Surgical Ward, after their condition became stable,
where they received treatments, such as routine infection
prevention, myocardial nutrition, diuretic therapy, and maintenance
of water-electrolyte and acid-base balance. After operation,
tracheal intubation was performed, and ventilator was connected for
assisted ventilation which was withdrawn as soon as possible after
hemodynamic stability. The ventilator was withdrawn in 9 patients
on the day of operation, and it was used for 115 h in maximum.
Specific clinical data are shown in Table I.
 | Table I.Clinical information and data of child
patients receiving CPB. |
Table I.
Clinical information and data of child
patients receiving CPB.
| Information/data | CPB group (n=16) |
|---|
| Age (months) | 3.5 (2, 11) |
| Sex
(male/female) | 10/6 |
| Weight (kg) | 7.063±3.228 |
| Atrial septal defect
(n) | 5 |
| Ventricular septal
defect (n) | 11 |
| Complete
transposition of great artery (n) | 1 |
| Left coronary anomaly
(n) | 1 |
| CPB time (min) | 92.938±45.261 |
| Aortic clamping time
(min) | 54.062±24.960 |
| Time in the PICU
(days) | 4.188±2.834 |
| Duration of
postoperative fever (days) | 2.875±1.857 |
| Application time of
ventilator (h) | 5 (3.25, 52.5) |
Experimental instruments and
materials
LXA4 enzyme-linked immunosorbent assay
(ELISA) kit (USCN Life Sciences, Inc., Wuhan, China); microplate
reader (Thermo Fisher Scientific, Inc., Waltham, MA, USA); Terumo
Advanced Perfusion System 1 artificial heart-lung machine, Terumo
membrane oxygenator (both from Terumo, Tokyo, Japan); Sorin
ultrafilter (Sorin Biomedica Spa, Saluggia, Italy); and Sysmex
XN-9000 blood analyzer (Sysmex Corp., Kobe, Japan).
Experimental methods
Peripheral blood (0.5 ml) was collected from child
patients in CPB group before operation (Tc), after operation (T0),
at 1 day after operation (T1), at 3 days after operation (T3), and
at 7 days after operation (T7); and 0.5 ml peripheral blood was
also collected from 17 child patients without a history of CHD
(control group), who were scheduled to undergo hernia and urinary
malformation repair. The peripheral blood was placed in an
ethylenediaminetetraacetic acid (EDTA) anticoagulant tube,
centrifuged at 1,000 × g, at room temperature, for 5 min to collect
the plasma and cryopreserved at −80°C. Every specimen was thawed to
be detected. The optical density (OD) value of the standard and
clinical specimens was determined using the microplate reader
(wavelength, 450 nm), according to the instructions of the ELISA
kit, and the standard curve was drawn, followed by LXA4
quantification using the ELISA Calc software. At the same time,
blood routine indexes and hs-CRP levels were detected, at each
time-point.
Statistical analysis
GraphPad 6.0 software (GraphPad Software, Inc., La
Jolla, CA, USA) and Statistical Product and Service Solutions
(SPSS) 18.0 software (IBM Corp., Armonk, NY, USA) were used for
statistical analysis and plotting. Normally distributed data were
expressed as mean ± standard deviation (mean ± SD), and non-normal
distribution data were expressed as median (M) and interquartile
spacing (Q). For normal distribution data, t-test was used for the
comparison between two groups. One-way ANOVA was used for the
comparison among three or more groups. LSD test was used for equal
variances, and Dunnett's test for unequal variances. Non-parametric
tests were used for non-normal distribution data. Pearson's linear
correlation analysis was adopted for the correlation analysis
between two indexes. P<0.05 was considered to indicate a
statistically significant difference.
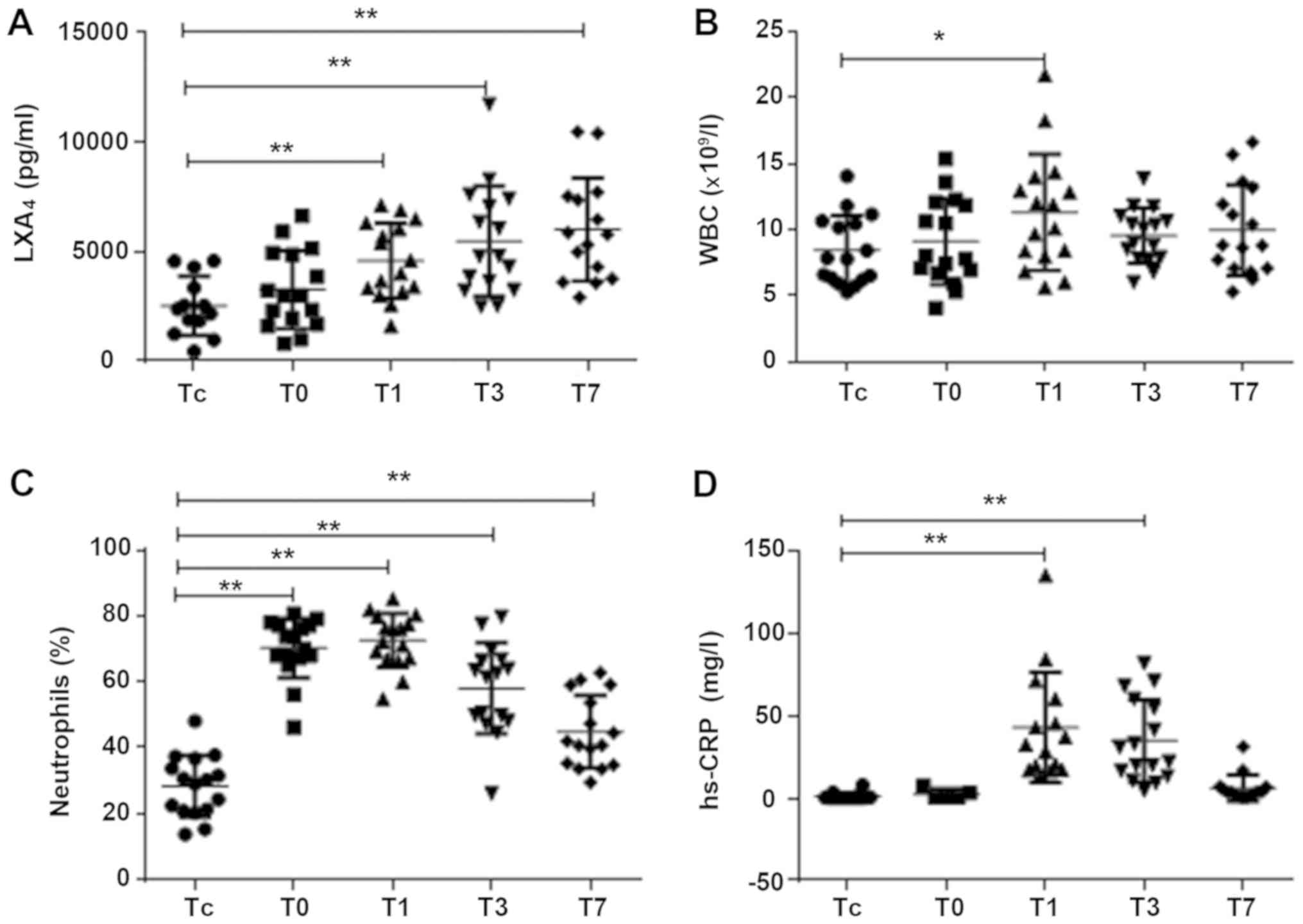
Results
There were no significant differences in age and sex
between CPB and control group, and the plasma LXA4 level
in CPB group was significantly lower at Tc compared to that in the
control group (P<0.01) (Table
II). LXA4 showed an increasing trend after
operation, which was significantly increased at T1 compared to that
at Tc (P<0.01), continued to show an upward trend, and was still
significantly increased at T3 and T7 compared to that at Tc
(P<0.01) (Fig. 1A). WBC was
increased significantly at T1 and T3 (P<0.05) for a short time,
and dropped at T7 near the level at Tc (Fig. 1B). The proportion of neutrophils (N%)
was obviously and rapidly increased at T0 compared to that at Tc
(P<0.01), for a long time, and was still remarkably increased at
T7 compared to that at Tc (P<0.01) (Fig. 1C). The dynamic changes in hs-CRP were
similar to those of WBC. hs-CRP level was significantly increased
at T1 and T3 compared to that at Tc (P<0.01) and dropped at T7
near the level at Tc (Fig. 1D).
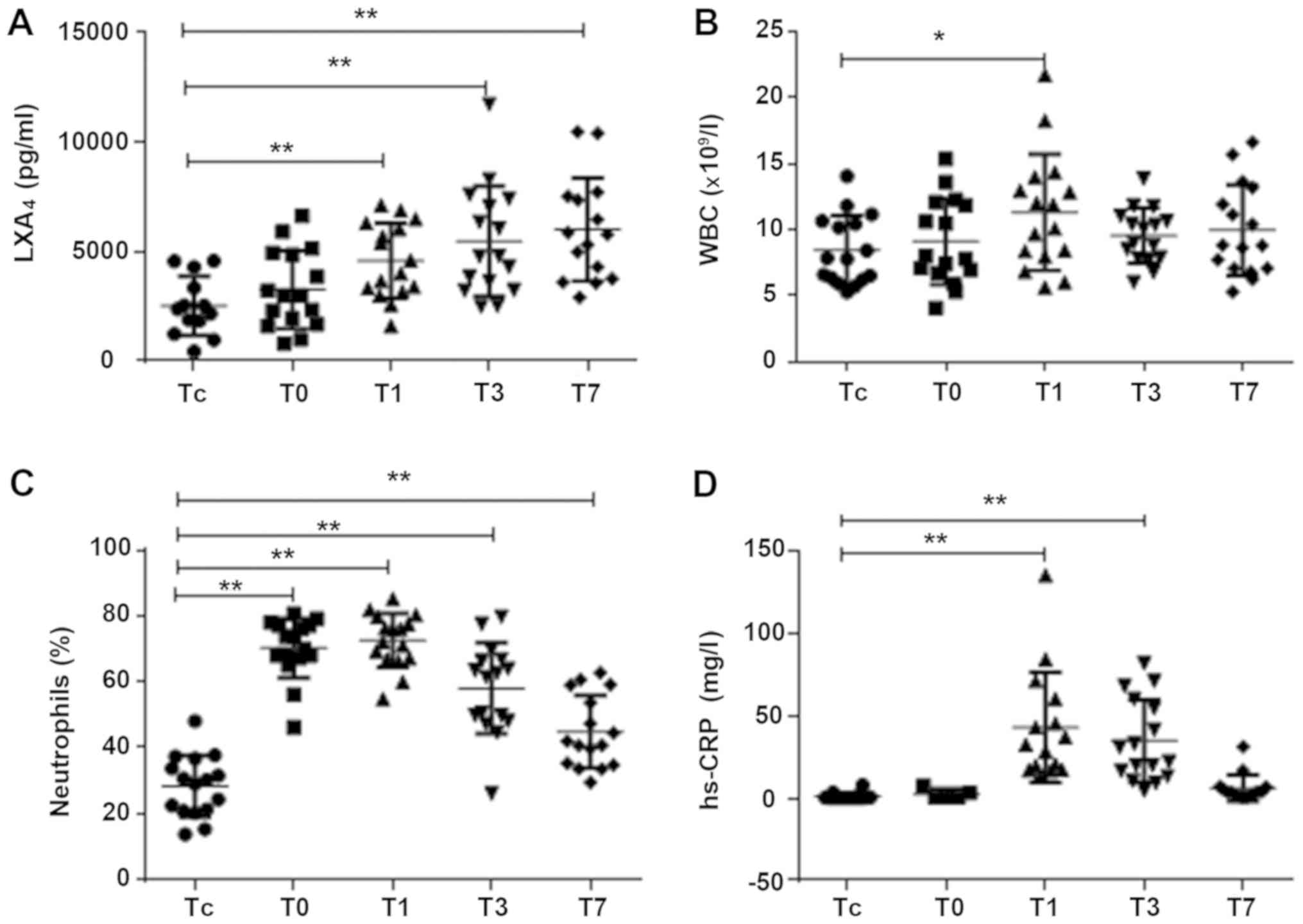 | Figure 1.The dynamic variations of
LXA4, WBC, N%, and hs-CRP in patients of the CPB group,
at 5 different time-points. Peripheral blood was collected from
children with CPB at 5 time-points: before operation (Tc), after
operation (T0), 1 day after operation (T1), 3 days after operation
(T3), and 7 days after operation (T7). (A) LXA4 was
detected by ELISA, and an upward trend was observed after
operation, compared to the LXA4 levels before operation
(**P<0.01). (B and D) WBC and hs-CRP increased significantly at
1 day after operation (*P<0.05, **P<0.01). (C) N%
significantly and rapidly increased at 1 day after operation, and
the high increase lasted longer (**P<0.01). LXA4,
lipoxin A4; WBC, white blood cell; N%, proportion of
neutrophils; hs-CRP, high-sensitivity C-reactive protein; ELISA,
enzyme-linked immunosorbent assay. |
 | Table II.Comparison of clinical data and
LXA4 expression levels between CPB and control group at
Tc. |
Table II.
Comparison of clinical data and
LXA4 expression levels between CPB and control group at
Tc.
| Category | CPB group (n=16) | Control group
(n=17) | P-value |
|---|
| Age (months) | 3.5 (2, 11) | 15 (1, 22.5) | >0.05 |
| Sex
(male/female) | 10/6 | 13/4 | >0.05 |
| LXA4
(pg/ml) | 2,552 (1,879,
4,586) | 17,129 (8,297,
33,267) | <0.01 |
According to Pearson's linear correlation analysis,
the CPB time and aortic clamping time were positively correlated
with the time in the PICU, application time of ventilator and
hs-CRP level at T0 (Table III).
LXA4 had no correlations with age, weight, CPB time and
aortic clamping time. No correlation was found between
LXA4 and WBC, N% and hs-CRP at the corresponding
time-points.
 | Table III.Correlation analysis between indexes
in child patients receiving CPB. |
Table III.
Correlation analysis between indexes
in child patients receiving CPB.
| Categories | Correlation
coefficient | P-value |
|---|
| CPB time - time in
the PICU | 0.7195 | 0.002b |
| Aortic clamping time
- time in the PICU | 0.7181 | 0.002b |
| CPB time -
application time of ventilator | 0.6570 | 0.006b |
| Aortic clamping time
- application time of ventilator | 0.6152 | 0.011a |
| CPB time - hs-CRP
(T0) | 0.8922 | 0.042a |
| Aortic clamping time
- hs-CRP (T0) | 0.9084 | 0.033a |
Discussion
LXA4, as the metabolite of arachidonic
acid, is the first endogenous lipid mediator found with extensive
functions of anti-inflammation and promotion of inflammatory
resolution, and is hailed as the ‘braking signal’ of inflammatory
response (5). LXA4 is the
metabolite produced by arachidonic acid through the lipoxygenase
(LOX) pathway in the inflammatory process, as well as an endogenous
antagonist of leukotrienes, and its major function is to inhibit
the chemotaxis of neutrophils and adhere to endothelial cells,
which is related to the inflammatory resolution (6). LX can also stimulate endothelial cells
to produce prostacyclin and nitric oxide, help dilate blood vessels
and improve blood flow (7). Under
the influence of inflammation or disease and the stimulus of
inflammatory factors, different LOXs will sequentially catalyze
arachidonic acid to promote LX synthesis, in which interactions
between cells, such as that between leukocytes, between leukocytes
and platelets and between leukocytes and epithelial cells, are
needed. If something is wrong in these interactions, the LX
synthesis will be affected (8,9). There
have been no studies on the correlations of LXA4 with
CHD and CPB. Reina-Couto et al have found that the severity
of chronic heart failure (CHF) is negatively related to the plasma
LXA4 level, and LXA4 can be considered as a
valuable marker for the risk stratification of CHF, which may be
related to the defects in pro-inflammatory and anti-inflammatory
mechanisms of CHF (10). Child
patients with CHD are often accompanied with cardiac insufficiency
in different degrees, and it has been found that the
LXA4 level declines in child patients with CHD compared
to that in normal children, in consistency with the research
results of Reina-Couto et al. Moreover, child patients with
CHD are prone to concurrent infection, and some studies have found
that they often suffer from immunodeficiency in different degrees,
such as the lower chemotaxis and phagocytosis of neutrophils,
complement function and secretion of IgA than normal subjects
(11). The immunodeficiency in child
patients with CHD may be related to the low content of
LXA4, which needs to be confirmed via further
experiments.
In the present study, it was found that
LXA4 showed a gradually increasing trend after CPB, and
its average level at T7 was still significantly different from that
in control group. The contact with a large number of artificial
materials, surgical trauma and pulmonary ischemia-reperfusion
injury during CPB can lead to activation of the monocyte/macrophage
and the release of a large number of inflammatory factors in the
body in order to resist stress and promote repair (1). Serhan et al (12) were the first to find that
inflammation resolution is a highly-ordered active process closely
regulated by a large number of lipid mediators produced by
unsaturated fatty acid via enzymatic catalysis. LXA4 can
bind to its coupled receptor to downregulate the expression of
inflammatory factors in tissues through a variety of signaling
pathways. Moreover, LXA4 can inhibit the chemotaxis of
leukocytes towards the inflammatory site and promote macrophages to
phagocytose apoptotic granulocytes and other damaged cells, thereby
inhibiting the inflammatory process, promoting the inflammation
resolution, and exerting specific anti-infection and
anti-inflammatory effects in inflammatory infection-related
diseases (13). Therefore, it is
speculated that the inflammatory response after CPB increases the
synthesis of LXA4 with a strong anti-inflammatory
effect.
In this study, it was also found that WBC, N% and
hs-CRP were transiently increased at T0 and were most significantly
increased at T1, which is consistent with the results of a number
of experiments (14,15). CRP is an acute-phase reactive protein
and an important inflammatory marker, which will obviously increase
in the case of acute inflammation and trauma in the body (16). With the application of
anti-inflammatory and anti-infective drugs after operation and
inflammation control, CRP gradually declines, and the body
temperature also gradually drops to normal. We also found that the
CPB time and aortic clamping time were positively correlated with
the time in the PICU, application time of ventilator and hs-CRP
level at T0. CPB time and aortic clamping time are often related to
the complexity of operation and general condition of patients. The
longer the surgical exposure is, the higher the probability of
infection will be. Therefore, from the perspective of postoperative
complications and recovery, the CPB time and aortic clamping time
should be reduced as soon as possible during operation, so as to
promote postoperative recovery.
In conclusion, the LXA4 level in child
patients with CHD is lower than that in normal children, but it has
dynamic changes and gradually increases during CPB under the
influence of inflammatory response. However, changes in
LXA4 have no correlation with inflammation and infection
indexes, such as WBC, N% and hs-CRP, so it cannot be used as a
sensitive index for monitoring inflammation, but can be used to
evaluate the recovery of the disease.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
MW, HZ and JW designed the study. MW, ZF and JL
collected the samples and performed the experiments. MW, ZF and HZ
were mainly devoted to the data analysis. MW, HZ and JW prepared
the manuscript. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
Children's Hospital of Soochow University (Suzhou, China). Patients
who participated in this research had complete clinical data.
Signed written informed consents were obtained from the patients
and/or their guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Cremer J, Martin M, Redl H, Bahrami S,
Abraham C, Graeter T, Haverich A, Schlag G and Borst HG: Systemic
inflammatory response syndrome after cardiac operations. Ann Thorac
Surg. 61:1714–1720. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Weerasinghe A, Athanasiou T, Philippidis
P, Day J, Mandal K, Warren O, Anderson J and Taylor K:
Platelet-monocyte pro-coagulant interactions in on-pump coronary
surgery. Eur J Cardiothorac Surg. 29:312–318. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Paśnik J, Siniewicz K, Moll JA, Moll J,
Baj Z, Sysa A and Zeman K: Effect of cardiopulmonary bypass on
neutrophil activity in pediatric open-heart surgery. Arch Immunol
Ther Exp (Warsz). 53:272–277. 2005.PubMed/NCBI
|
|
4
|
Hu F, Feng AP, Liu XX, Zhang S, Xu JT,
Wang X, Zhong XL, He MW and Chen HX: Lipoxin A4 inhibits
lipopolysaccharide-induced production of inflammatory cytokines in
keratinocytes by up-regulating SOCS2 and down-regulating TRAF6. J
Huazhong Univ Sci Technolog Med Sci. 35:426–431. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Börgeson E, McGillicuddy FC, Harford KA,
Corrigan N, Higgins DF, Maderna P, Roche HM and Godson C: Lipoxin
A4 attenuates adipose inflammation. FASEB J. 26:4287–4294. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lv W, Lv C, Yu S, Yang Y, Kong H, Xie J,
Sun H, Andersson R, Xu D, Chen B, et al: Lipoxin A4 attenuation of
endothelial inflammation response mimicking pancreatitis-induced
lung injury. Exp Biol Med (Maywood). 238:1388–1395. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ryan A and Godson C: Lipoxins: Regulators
of resolution. Curr Opin Pharmacol. 10:166–172. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Wu B, Walker J, Spur B, Rodriguez A and
Yin K: Effects of Lipoxin A4 on antimicrobial actions of
neutrophils in sepsis. Prostaglandins Leukot Essent Fatty Acids.
94:55–64. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wu B, Walker JA, Temmermand D, Mian K,
Spur B, Rodriguez A, Stein TP, Banerjee P and Yin K: Lipoxin A(4)
promotes more complete inflammation resolution in sepsis compared
to stable lipoxin A(4) analog. Prostaglandins Leukot Essent Fatty
Acids. 89:47–53. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Reina-Couto M, Carvalho J, Valente MJ,
Vale L, Afonso J, Carvalho F, Bettencourt P, Sousa T and
Albino-Teixeira A: Impaired resolution of inflammation in human
chronic heart failure. Eur J Clin Invest. 44:527–538. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dmitrieva VA, Samuilova DSh, Putiato NA
and Khurges IS: The role of immunological studies in the diagnosis
of bacterial endocarditis in patients with congenital heart
defects. Vestn Khir Im I I Grek. 149:147–151. 1992.(In Russian).
PubMed/NCBI
|
|
12
|
Serhan CN, Hamberg M and Samuelsson B:
Lipoxins: Novel series of biologically active compounds formed from
arachidonic acid in human leukocytes. Proc Natl Acad Sci USA.
81:5335–5339. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Cattaneo F, Parisi M and Ammendola R:
Distinct signaling cascades elicited by different formyl peptide
receptor 2 (FPR2) agonists. Int J Mol Sci. 14:7193–7230. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Saito J, Hashiba E, Mikami A, Kudo T, Niwa
H and Hirota K: Pilot study of changes in presepsin concentrations
compared with changes in procalcitonin and c-reactive protein
concentrations after cardiovascular surgery. J Cardiothorac Vasc
Anesth. 31:1262–1267. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Svensson AS, Kvitting JP, Kovesdy CP,
Cederholm I and Szabó Z: Changes in serum cystatin C, creatinine,
and C-reactive protein after cardiopulmonary bypass in patients
with normal preoperative kidney function. Nephrology. 21:519–525.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Dillenseger L, Langlet C, Iacobelli S,
Lavaux T, Ratomponirina C, Labenne M, Astruc D, Severac F, Gouyon
JB and Kuhn P: Early inflammatory markers for the diagnosis of
late-onset sepsis in neonates: The Nosodiag Study. Front Pediatr.
6:3462018. View Article : Google Scholar : PubMed/NCBI
|