Introduction
As the most important public health problem in the
world, cardiovascular and cerebrovascular diseases were reported to
have a death toll of 8.76 million in 2015, ranking first among the
10 leading causes of death according to the World Health
Organization (WHO) (1). The number
of death in China is second only to malignant tumors (2). Atherosclerosis usually refers to the
stenosis or obstruction of the lumen due to coronary
atherosclerosis, resulting in local ischemia and hypoxia (3). Subclinical atherosclerosis (SA), a type
of atherosclerosis, refers to the presence of atherosclerotic
plaque in patients, without any clinical symptom (4). A study (5) showed that in recent years, the
incidence of SA has decreased in developed countries, but increased
in developing countries, which may be caused by the changes in
dietary patterns as a result of economic development. Moreover,
high fat diet and low cholesterol consumption play an important
role in the pathogenesis of SA.
In the study of Weber et al (6), more than 50% of the patients with first
cardiovascular and cerebrovascular disease did not have definite
clinical symptoms. Therefore, early detection of cardiovascular
function and intervention through clinical protocols in patients
with SA can reduce the risk of cardiovascular diseases (7). With the continuous improvement of
medical equipment, the diagnostic methods for atherosclerosis have
been increasing, and the importance of ultrasonography in the
diagnosis of atherosclerosis has been widely recognized in clinical
practice (8). As a safe, rapid and
noninvasive imaging tool, ultrasonography can directly reflect the
structure and function of the heart and blood vessels in patients
(9).
Therefore, the carotid arteries and left ventricular
function of patients with SA were detected by ultrasonography in
this study to provide references for diagnosis in clinic.
Patients and methods
Clinical data
Retrospective analysis was carried out of 152
patients with no obvious clinical symptoms of atherosclerosis as
confirmed by carotid ultrasonography in Tengzhou Central People's
Hospital (Tengzhou, China) from September 2015 to March 2016. These
patients were enrolled as the experimental group, and 45 patients
with normal liver, kidney, heart function, no stroke, myocardial
infarction history examined in the above hospital at the same time
were collected as the control group. Inclusion criteria were:
patients with complete clinical data, no malignant tumor, in
accordance with SA diagnostic criteria. Exclusion criteria were:
patients with coronary atherosclerotic heart disease, heart valve
disease, renal failure, immune deficiency disease, stroke and
transient cerebral ischemia history. In total 139 cases were
enrolled in this study according to the above criteria. This study
was approved by the Medical Ethics Committee of Tengzhou Central
People's Hospital. Patients who participated in this research had
complete clinical data. Signed informed consents were obtained from
the patients or the guardians.
Detection methods and data
collection
MyLab90 color Doppler ultrasound (Yum Company,
Italy) with Echo-tracking technology, digital image management
system and LA523 probe was used at a frequency of 4–13 MHz. Philips
iE33 color Doppler ultrasound with TomTec workstation (3D speckle
tracing imaging technology) and S/X5-1 probe was used at a
frequency of 2–5 MHz. Carotid arteries and left ventricular
function in the two groups were measured. The parameters of common
carotid artery function and left ventricular function in the two
groups were collected. The serum was collected and the blood lipid
of patients was detected by Hitachi 7600 automatic biochemical
analyzer. Fasting plasma glucose (FPG), BMI index, blood pressure
and plaque detection rate were analyzed.
Subgroups in the experimental
group
According to the Framingham risk assessment, the
incidence probability of coronary disease in the next 10 years of
the 139 patients in the experimental group was analyzed (indicators
included age, total cholesterol, high density lipoprotein, systolic
pressure and smoking). In total, 46 patients, including 26 males
and 20 females, were included in the low risk group (incidence
<10%); 47 patients, including 25 males and 22 females, were
included in the medium risk group (>10% - <20% incidence); 46
patients, including 29 males and 17 females, were included in the
high risk group (incidence >20%).
Statistical analysis
SPSS 20.0 software package was used for statistical
analysis of the collected data. GraphPad Prism 7 software was used
to draw figures. Countable data were expressed as rate (%),
analyzed by Chi-square test (χ2). The measurement data
are expressed as means ± SD. Comparison between the two groups was
conducted by independent sample t-test and expressed by t-test.
Rank data were analyzed by rank-sum test and expressed by Z.
Multigroup comparison was conducted by single factor ANOVA, and
post pairwise comparison was analyzed by LSD-t test and expressed
by F. P<0.05 was considered to indicate a statistically
significant difference.
Results
Analysis of clinical data of patients
in the control group and the experimental group
The clinical data in the two groups showed that, in
the control group, there were 27 males and 18 females, 29 patients
were aged >60 years, and 15 patients smoked. BMI
(kg/m2): 23.54±3.25, FPG (mmol/l): 5.36±0.68, systolic
pressure (mmHg): 129.50±15.84, diastolic pressure (mmHg):
76.84±7.54, TG (mmol/l): 1.18±0.52, TC (mmol/l): 3.25±1.05, HDL
(mmol/l): 1.33±0.60, LDL (mmol/l): 2.69±1.01. In the experimental
group, there were 80 males and 59 females, 82 patients were aged
>60 years, and 40 patients smoked. BMI (kg/m2):
23.84±4.25, FPG (mmol/l): 5.29±0.70, systolic pressure (mmHg):
146.35±25.24, diastolic pressure (mmHg): 79.54±9.44, TG (mmol/l):
4.59±1.84, TC (mmol/l): 4.82±1.63, HDL (mmol/l): 1.35±0.62, LDL
(mmol/l): 2.48±0.84. There was no significant difference in gender,
age, smoking history, BMI, FPG, diastolic pressure, HDL and LDL
between the two groups (P>0.05), while there were differences in
the systolic pressure, TG and TC (P<0.05) (Table I).
 | Table I.Comparison of clinical data between
the two groups [n (%)]. |
Table I.
Comparison of clinical data between
the two groups [n (%)].
| Factor | Control group
(n=45) | Experimental group
(n=139) | t/χ2
value | P-value |
|---|
| Sex |
|
|
0.083 | 0.773 |
| Male | 27 (60.00) | 80 (57.55) |
|
|
|
Female | 18 (40.00) | 59 (42.25) |
|
|
| Age (years) |
|
|
0.422 | 0.516 |
| ≥60 | 29 (64.44) | 82 (58.99) |
|
|
|
<60 | 16 (35.56) | 57 (41.01) |
|
|
| Smoking history |
|
|
0.337 | 0.562 |
| Yes | 15 (33.33) | 40 (28.78) |
|
|
| No | 30 (66.67) | 99 (71.22) |
|
|
| BMI
(kg/m2) | 23.54±3.25 | 23.84±4.25 |
0.434 | 0.665 |
| FPG (mmol/l) | 5.36±0.68 | 5.29±0.70 |
0.587 | 0.558 |
| Systolic pressure
(mmHg) | 129.50±15.84 | 146.35±25.24 |
4.213 | <0.001 |
| Diastolic pressure
(mmHg) | 76.84±7.54 | 79.54±9.44 |
1.746 | 0.083 |
| TG (mmol/l) | 1.18±0.52 | 4.59±1.84 | 12.254 | <0.001 |
| TC (mmol/l) | 3.25±1.05 | 4.82±1.63 |
6.061 | <0.001 |
| HDL (mmol/l) | 1.33±0.60 | 1.35±0.62 |
0.189 | 0.850 |
| LDL (mmol/l) | 2.69±1.01 | 2.48±0.84 |
1.385 | 0.168 |
Comparison of carotid artery
parameters of patients
By comparing the carotid artery parameters of the
two groups, it was found that the expression levels of β, cIMT, Ep,
AI, AC and PWVβ in the experimental group were significantly
increased compared with those in the control group (P<0.05)
(Table II). Comparison of arterial
parameters in the low, middle and high risk groups according to the
Framingham risk assessment found that there was no statistical
difference in AC and AI among the three groups (P>0.05), but
there was a statistical difference in other indexes (P<0.05).
The expression levels of β, cIMT, Ep, PWVβ increased with the risk
degree in the low, medium and high risk groups, and there were
differences among the groups (P<0.05) (Table III).
 | Table II.Comparison of carotid artery
parameters between patients in the experimental and control
groups. |
Table II.
Comparison of carotid artery
parameters between patients in the experimental and control
groups.
| Index | Control group
(n=45) | Experimental group
(n=139) | t value | P-value |
|---|
| β value | 6.24±1.05 | 10.90±4.56 |
6.786 | <0.001 |
| cIMT (mm) | 0.69±0.13 | 0.96±0.19 |
8.876 | <0.001 |
| Ep (kPa) | 78.64±20.18 | 140.45±61.93 |
6.573 | <0.001 |
| AI (%) | 19.88±8.45 | 42.17±9.47 | 14.075 | <0.001 |
| AC
(mm2/kPa) | 0.84±0.22 | 2.63±0.79 | 14.987 | <0.001 |
| PWVβ (min/sec) | 4.78±1.20 | 7.45±1.50 | 10.862 | <0.001 |
 | Table III.Comparison of carotid artery
parameters in the low, medium and high risk groups. |
Table III.
Comparison of carotid artery
parameters in the low, medium and high risk groups.
| Index | Low risk group
(n=46) | Medium risk group
(n=47) | High risk group
(n=46) | F value | P-value |
|---|
| β value | 8.84±2.54 |
10.94±3.54a |
13.22±4.81a,b | 15.735 | <0.001 |
| cIMT (mm) | 0.84±0.18 |
0.99±0.17a |
1.08±0.14a,b | 25.070 | <0.001 |
| Ep (kPa) | 120.84±41.55 |
149.35±45.37a |
186.47±79.51a,b | 14.800 | <0.001 |
| AI (%) | 42.44±15.28 | 49.28±15.66 | 46.10±15.75 |
2.247 | 0.110 |
| AC
(mm2/kPa) | 0.79±0.29 | 0.77±0.22 | 0.75±0.32 |
0.236 | 0.790 |
| PWVβ (min/sec) | 6.88±1.62 |
7.35±1.25a |
8.29±1.71a,b | 10.033 | <0.001 |
Left ventricular function parameters
of patients
Comparison of left ventricular function parameters
between the two groups found that the expression levels of LVEDV,
LVESV, and LVEF in the experimental group were significantly
decreased compared with those in the control group (P<0.05),
while the expression levels of LAV, E/e, GLS and GCS were
significantly increased compared with those in the control group
(P<0.05) (Table IV). Comparison
of left ventricular function parameters in the low, medium and high
risk groups according to Framingham risk assessment found that
there were significant differences among the three groups
(P<0.05). The expression levels of LVEDV, LVESV, LAV and E/e
increased with the risk degree in the three groups (P<0.05).
There was no significant difference in GLS expression between low
and middle risk groups (P>0.05), while the expression was
significantly increased compared with that in the high risk group
(P<0.05), and there was no significant difference in LVEF and
GCS among the three groups (P>0.05) (Table V).
 | Table IV.Comparison of left ventricular
function parameters of patients in the experimental and control
groups. |
Table IV.
Comparison of left ventricular
function parameters of patients in the experimental and control
groups.
| Index | Control group
(n=45) | Experimental group
(n=139) | t value | P-value |
|---|
| LVEDV (ml) | 83.41±18.24 | 63.10±15.61 |
7.272 | <0.001 |
| LVESV (ml) | 35.84±9.24 | 22.25±7.56 |
9.906 | <0.001 |
| LVEF (%) | 70.54±16.38 | 63.84±5.81 |
4.107 | <0.001 |
| LAV (ml) | 30.84±8.84 | 43.69±14.06 |
5.768 | <0.001 |
| E/e | 6.84±3.27 | 11.68±3.35 |
8.472 | <0.001 |
| GLS (%) | 10.12±4.25 | 20.57±3.59 | 16.204 | <0.001 |
| GCS (%) | 9.15±2.22 | 31.92±5.67 | 26.255 | <0.001 |
 | Table V.Comparison of left ventricular
function parameters in the low, middle and high risk groups. |
Table V.
Comparison of left ventricular
function parameters in the low, middle and high risk groups.
| Index | Low risk group
(n=46) | Medium risk group
(n=47) | High risk group
(n=46) | F value | P-value |
|---|
| LVEDV (ml) |
56.47±10.84 |
63.84±11.36a |
71.35±16.88a,b | 14.402 | <0.001 |
| LVESV (ml) | 19.35±5.11 |
22.39±6.88a |
26.94±6.58a,b | 17.225 | <0.001 |
| LVEF (%) | 63.87±5.89 | 64.27±5.34 | 62.25±4.39 |
1.926 | 0.150 |
| LAV (ml) | 35.04±8.05 |
47.33±10.58a |
55.37±15.82a,b | 33.940 | <0.001 |
| E/e | 10.52±2.67 |
12.84±3.89a |
14.68±4.42a,b | 14.339 | <0.001 |
| GLS (%) | 20.95±3.81 | 20.17±3.80 |
18.66±3.17a,b |
4.794 | 0.010 |
| GCS (%) | 34.25±5.29 | 33.02±5.10 | 31.95±6.17 |
1.988 | 0.141 |
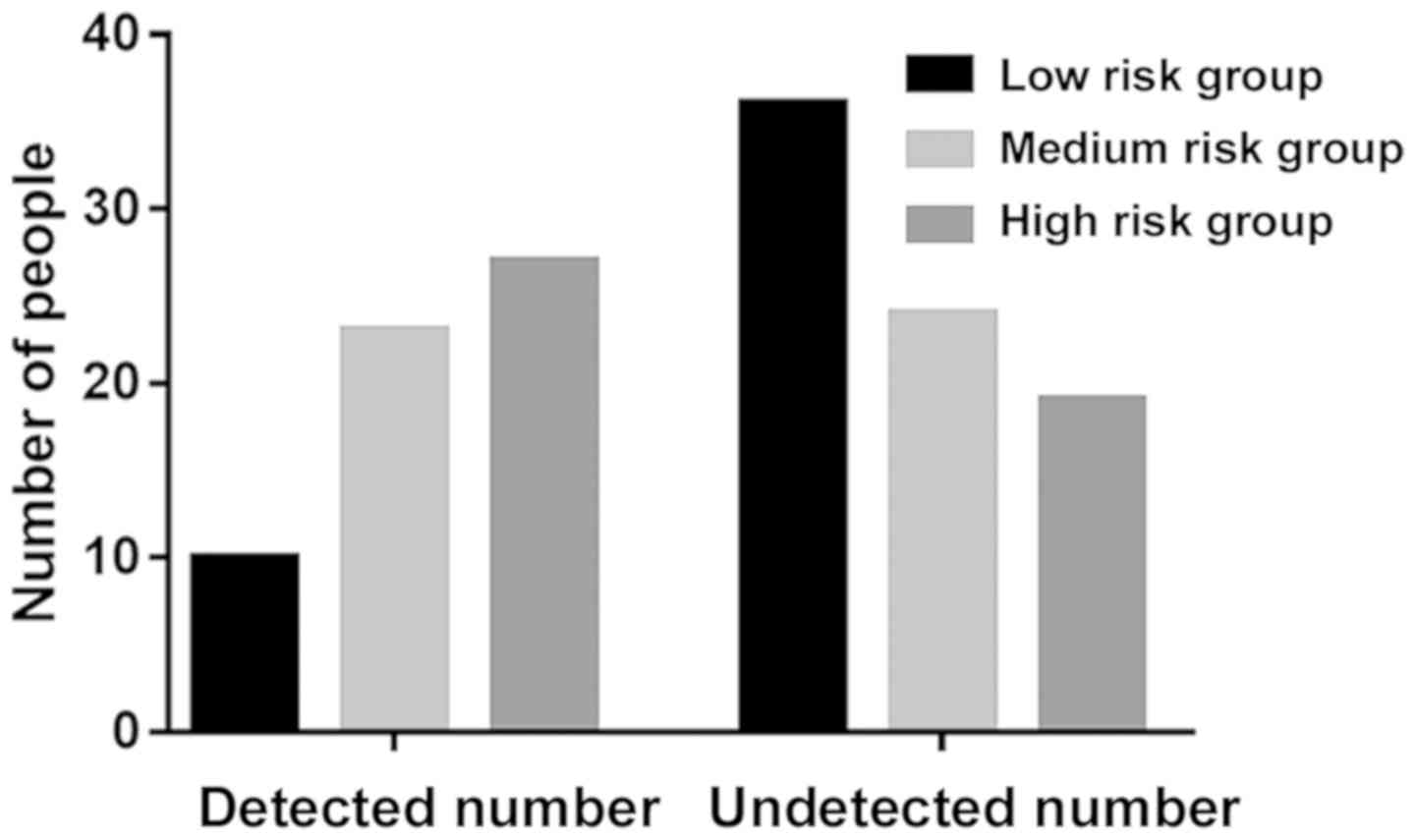
Plaque detection in the experimental
group
Analysis of plaque detection rate in the
experimental group found that the detection rate of plaque was
21.74% (n=10) in the low-risk group, 48.94% (n=23) in the medium
risk group and 58.70% (n=27) in the high-risk group. There were
significant differences in plaque detection rate among the three
groups (P<0.05) (Table VI and
Fig. 1).
 | Table VI.Plaque detection in the experimental
group [n (%)]. |
Table VI.
Plaque detection in the experimental
group [n (%)].
| Group | Patients with
plaques | Patients without
plaques | Z value | P-value |
|---|
| Low risk group
(n=46) | 10 (21.74) | 36 (78.26) | −3.565 | <0.001 |
| Medium risk group
(n=47) | 23 (48.94) | 24 (51.06) |
|
|
| High risk group
(n=46) | 27 (58.70) | 19 (41.30) |
|
|
Discussion
Cardiovascular and cerebrovascular diseases are the
most prevalent clinical diseases in the world, and coronary heart
disease is the most common disease (10). Atherosclerosis usually refers to the
stenosis or obstruction of the lumen due to coronary
atherosclerosis, resulting in local ischemia and hypoxia. A survey
shows (11) that patients with
coronary heart disease are getting younger as a result of improved
living standards and changes in dietary habits. With the increasing
incidence of coronary heart disease, it is receiving more
attention. As a chronic disease process, atherosclerosis can be
divided into pre-clinical stage and end-stage. End-stage patients
mainly have coronary heart disease, myocardial infarction or
ischemic stroke. Once patients enter the end-stage, they are prone
to death. Patients who are rescued in time have a high disability
rate, which seriously affects the life quality of patients.
Patients in the pre-clinical stage, also known as SA, can have the
presence of atherosclerosis through the corresponding examination
without any corresponding clinical symptoms (12–14). A
study has shown (15) that early
intervention in patients at SA stage can delay the course of
disease and reduce the occurrence of adverse reactions.
At present, Framingham risk assessment is commonly
used to evaluate the incidence of coronary heart disease in
patients, which calculates the incidence rate of coronary heart
disease in the next 10 years according to the cholesterol level and
non-cholesterol factors of the patients (16). Although the assessment evaluates
patients through a variety of factors, it can not effectively
diagnose and assess SA patients. Ultrasonography has been widely
used in clinical imaging for many years and has been widely
recognized by clinicians. It is non-invasive, safe, rapid and
accurate, and has a high accuracy in the diagnosis of
cardiovascular disease (17).
Carotid arteries and left ventricular function between healthy
subjects and patients with SA were compared and the carotid
arteries and left ventricular function in patients with SA with
different risk degrees were further analyzed in this study to
provide a reference for clinical diagnosis.
Patients in the experimental group and the control
group were examined by ultrasonography. The indexes of β, cIMT, Ep,
AI, AC, PWVβ have been reported (18,19) to
be important for the early lesion of arterial wall, and were
detected by Echo-tracking technique in this study. After analysis,
it was found that the above indexes in the experimental group were
significantly higher than those in the control group, and the
stratification analysis of the experimental group showed that the
expression of β, cIMT, Ep and PWVβ increased with the risk degree
in the low, middle and high risk groups, indicating that with the
increase of risk degree, the blood vessel wall gradually hardened,
carotid intima thickness increased, vascular elasticity gradually
weakened, pulse wave velocity increased, which increased the risk
of adverse cardiovascular events. It was assumed that this was
mainly due to the stimulation of the vascular intima under the
influence of various risk factors, thereby destroying the vascular
elastic fibers, causing smooth muscle proliferation, vascular
remodeling and inflammation, ultimately, leading to the above
symptoms (20–22). Then the left ventricular function of
the patients in the experimental group and the control group was
measured by 3D speckle tracing imaging technology that is a 3D
spatial quantitative measurement of myocardial strain and strain
rate, and can reflect the early contraction of myocardial fiber in
patients (23,24). The results showed that the LVEDV,
LVESV and LVEF in the experimental group were significantly lower
than those in the control group, while the LAV, E/e, GLS and GCS in
the experimental group were significantly higher than those in the
control group. Moreover, further analysis found that LVEDV, LVESV
and E/e increased with the risk of the disease, while LVEF was the
opposite. This was because the increase of β reduced the reserve of
vascular elasticity in the patient, and further caused the increase
of systolic pressure and the decrease of diastolic pressure,
therefore, causing myocardial ischemia in patients. A study by
Agoşton-Coldea et al (25)
showed that atherosclerosis occlusion in lower extremities is
closely related to carotid stiffness and left ventricular diastolic
function. The results of our study showed that there was no
difference in the incidence of LVEF and GCS between the groups, but
the incidence of GLS in the low and medium risk groups was
significantly higher than that in the high risk group, and there
was no significant difference between low and medium risk groups.
This suggests that the decrease of vascular elasticity does not
affect LVEF and GCS, and it is only when the patient reaches high
risk that the left ventricular GLS endocardial blood perfusion is
decreased. At the end of the study, the carotid plaque in the
experimental group was examined, and it was found that there were
significant differences between the three groups, and with the
increase of the degree of the disease, the number of detected
carotid plaques increased significantly.
This study preliminarily proved the difference
between the carotid artery parameters and left ventricular function
in healthy subjects and SA patients, and further analyzed their
relationship in patients with different risk degrees. However,
there are still some limitations in this study. There may be some
bias in the data in this study as a retrospective analysis.
Follow-up analysis was not conducted, the specific adverse
reactions are not clear. Therefore, clinical randomized controlled
trials and follow-up studies are needed.
In conclusion, by observing the parameters of
carotid arteries and left ventricular function, it was found that
ultrasonography has important clinical value in the early diagnosis
of SA, and can be widely promoted in clinic.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
TZ wrote the manuscript and analyzed the clinical
data of patients. HY compared carotid artery parameters and left
ventricular function parameters. HX was responsible for plaque
detection. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
Tengzhou Central People's Hospital (Tengzhou, China). Patients who
participated in this research had complete clinical data. Signed
informed consents were obtained from the patients or the
guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Dal-Ré R: Early phase drugs and
biologicals clinical trials on worldwide leading causes of death: A
descriptive analysis. Eur J Clin Pharmacol. 67:563–571. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Du H, Li L, Bennett D, Guo Y, Key TJ, Bian
Z, Sherliker P, Gao H, Chen Y, Yang L, et al China Kadoorie Biobank
Study, : Fresh fruit consumption and major cardiovascular disease
in China. N Engl J Med. 374:1332–1343. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Al-Sharea A, Murphy AJ, Huggins LA, Hu Y,
Goldberg IJ and Nagareddy PR: SGLT2 inhibition reduces
atherosclerosis by enhancing lipoprotein clearance in
Ldlr−/− type 1 diabetic mice. Atherosclerosis.
271:166–176. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ambrosino P, Lupoli R, Di Minno A, Tasso
M, Peluso R and Di Minno MN: Subclinical atherosclerosis in
patients with rheumatoid arthritis. A meta-analysis of literature
studies. Thromb Haemost. 113:916–930. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Benjamin EJ, Blaha MJ, Chiuve SE, Cushman
M, Das SR, Deo R, de Ferranti SD, Floyd J, Fornage M, Gillespie C,
et al American Heart Association Statistics Committee and Stroke
Statistics Subcommittee, : Heart Disease and Stroke Statistics-2017
Update: A report from the American Heart Association. Circulation.
135:e146–e603. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Weber LA, Cheezum MK, Reese JM, Lane AB,
Haley RD, Lutz MW and Villines TC: Cardiovascular imaging for the
primary prevention of atherosclerotic cardiovascular disease
events. Curr Cardiovasc Imaging Rep. 8:362015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
de Almeida-Pititto B, Ribeiro-Filho FF,
Bittencourt MS, Lotufo PA, Bensenor I and Ferreira SR: Usefulness
of circulating E-selectin to early detection of the atherosclerotic
process in the Brazilian Longitudinal Study of Adult Health
(ELSA-Brasil). Diabetol Metab Syndr. 8:192016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Huang R, Abdelmoneim SS, Ball CA, Nhola
LF, Farrell AM, Feinstein S and Mulvagh SL: Detection of carotid
atherosclerotic plaque neovascularization using contrast enhanced
ultrasound: A systematic review and meta-analysis of diagnostic
accuracy studies. J Am Soc Echocardiogr. 29:491–502. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
ten Kate GL, van Dijk AC, van den Oord SC,
Hussain B, Verhagen HJ, Sijbrands EJ, van der Steen AF, van der
Lugt A and Schinkel AF: Usefulness of contrast-enhanced ultrasound
for detection of carotid plaque ulceration in patients with
symptomatic carotid atherosclerosis. Am J Cardiol. 112:292–298.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Saleheen D, Scott R, Javad S, Zhao W,
Rodrigues A, Picataggi A, Lukmanova D, Mucksavage ML, Luben R,
Billheimer J, et al: Association of HDL cholesterol efflux capacity
with incident coronary heart disease events: A prospective
case-control study. Lancet Diabetes Endocrinol. 3:507–513. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wilmot KA, O'Flaherty M, Capewell S, Ford
ES and Vaccarino V: Coronary heart disease mortality declines in
the United States from 1979 through 2011: Evidence for stagnation
in young adults, especially women. Circulation. 132:997–1002. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Poredoš P and Ježovnik MK: Markers of
preclinical atherosclerosis and their clinical relevance. Vasa.
44:247–256. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
McClelland RL, Jorgensen NW, Budoff M,
Blaha MJ, Post WS, Kronmal RA, Bild DE, Shea S, Liu K, Watson KE,
et al: 10-Year coronary heart disease risk prediction using
coronary artery calcium and traditional risk factors: Derivation in
the MESA (Multi-Ethnic Study of Atherosclerosis) with validation in
the HNR (Heinz Nixdorf Recall) Study and the DHS (Dallas Heart
Study). J Am Coll Cardiol. 66:1643–1653. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Matsushita K, Sang Y, Ballew SH, Shlipak
M, Katz R, Rosas SE, Peralta CA, Woodward M, Kramer HJ, Jacobs DR,
et al: Subclinical atherosclerosis measures for cardiovascular
prediction in CKD. J Am Soc Nephrol. 26:439–447. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gourgari E, Dabelea D and Rother K:
Modifiable risk factors for cardiovascular disease in children with
type 1 diabetes: can early intervention prevent future
cardiovascular events? Curr Diab Rep. 17:1342017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Sansone R, Rodriguez-Mateos A, Heuel J,
Falk D, Schuler D, Wagstaff R, Kuhnle GG, Spencer JP, Schroeter H,
Merx MW, et al Flaviola Consortium, European Union 7th Framework
Program, : Cocoa flavanol intake improves endothelial function and
Framingham Risk Score in healthy men and women: A randomised,
controlled, double-masked trial: the Flaviola Health Study. Br J
Nutr. 114:1246–1255. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Rosengarten B and Kaps M: A simultaneous
EEG and transcranial Doppler technique to investigate the
neurovascular coupling in the human visual cortex. Cerebrovasc Dis.
29:211–216. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yang S, Wang DZ, Zhang HX, He W and Chen
BX: Echo-tracking technology assessment of carotid artery stiffness
in patients with coronary slow flow. Ultrasound Med Biol. 41:72–76.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhang P, Guo R, Li Z, Xiao D, Ma L, Huang
P and Wang C: Effect of smoking on common carotid artery wall
elasticity evaluated by echo tracking technique. Ultrasound Med
Biol. 40:643–649. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lee SJ and Park SH: Arterial ageing.
Korean Circ J. 43:73–79. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zhang P, Guo R, Xiao D, Chu S, Gong L,
Zhang C, Jing B and Li M: Influence of smoking cessation on carotid
artery wall elasticity evaluated by echo-tracking. J Clin
Ultrasound. 40:352–356. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Nahrendorf M, Jaffer FA, Kelly KA,
Sosnovik DE, Aikawa E, Libby P and Weissleder R: Noninvasive
vascular cell adhesion molecule-1 imaging identifies inflammatory
activation of cells in atherosclerosis. Circulation. 114:1504–1511.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ling Y, Wan Q, Chen Q and Zhu W:
Assessment of subtle cardiac dysfunction in patients with frequent
premature ventricular complexes by real-time three-dimensional
speckle tracking echocardiography. Clin Cardiol. 40:554–558. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Huang X, Kang X, Xue J, Kang C, Lv H and
Li Z: Evaluation of carotid artery elasticity changes in patients
with cerebral small vessel disease. Int J Clin Exp Med.
8:18825–18830. 2015.PubMed/NCBI
|
|
25
|
Agoşton-Coldea L, Mocan T and Bobar C:
Arterial stiffness and left ventricular diastolic function in the
patients with hypertension. Rom J Intern Med. 46:313–321.
2008.PubMed/NCBI
|