Introduction
The most common type of congenital absence of a
vagina is Mayer-Rokitansky-Kuster-Hauser (MRKH) syndrome. At
present, vaginoplasty is the best method for the treatment of MRKH
syndrome (1). Since the first
development of vaginoplasty, >100 other surgical methods have
been developed. The major difference between the various methods is
the tissue material used to create the artificial vagina. The
purpose of all operations is to make the anatomy and function of
the artificial vagina as close as possible to those of a normal
vagina (2,3). The replacement of traditional open
surgery with a simple operation (i.e., laparoscopy) and the use of
an autograft substitute as an allograft are currently major
development trends in vaginoplasty (4).
Intestinal vaginoplasty is widely performed in the
clinic, as the resulting artificial vagina has a function closer to
that of a normal vagina, natural lubrication and early intercourse
function (5,6). Compared with the small intestine, the
sigmoid colon has the advantages of tolerance to trauma due to its
thickness, no requirement of wearing a mold to maintain the
operation effect for a long time, moderate secretion and capacious
internal cavity (7,8). With the introduction of fine
laparoscopic instruments, sigmoid colon vaginoplasty has gradually
become a completely ‘minimally invasive’ laparoscopic procedure. In
recent years, patients' demand for improved post-operative
physiological and psychological quality has increased. As a result,
surgeons must now consider how best to optimize laparoscopic
surgical procedures to respond to this demand while reducing
post-operative complications. Improvements in the operative
procedure may enhance the quality of laparoscopic surgery.
Between March 2013 and March 2016, total
laparoscopic sigmoid vaginoplasty (LSV) was performed on 11
patients at our institution. All of the surgeries were performed
with sigmoid mesocolon rotation and reverse puncture under
laparoscopy. In the present study, the clinical data of these
patients were retrospectively analyzed to explore the clinical
effect of total LSV, and data regarding the procedures and outcomes
were reported. The clinical effect of LSV was compared to
laparoscopic sigmoid colovaginoplasty, reported in a previous study
(9), by comparing the female sexual
function indexes.
Patients and methods
Patients
The study comprised 11 patients (married, n=7;
unmarried, n=4) diagnosed with MRKH syndrome and had primary
amenorrhea prior to the operation. The average age of the patients
was 22.8±2.7 years (ranged from 18 to 27 years) and the body mass
index was 24.9±1.9 kg/m2. None of the patients had a
history of diseases associated with MRKH syndrome or a familial
history of MRKH syndrome. One of the patients had previously
undergone laparoscopic appendectomy and two patients had undergone
laparoscopic cholecystectomy. None of these patients experienced
any complications after the operation. Urinary system B-ultrasound
indicated no obvious abnormalities in the bilateral kidneys,
bilateral ureter and bladder. Uterine imaging and sex hormone
levels were normal in all patients. All of the patients had normal
external female genitalia and normal ovarian function. The
chromosomal pattern was 46, XX. In line with standard procedures,
enteroscopy was performed prior to the operation, revealing no
obvious abnormalities. All of the patients had requested total LSV
after being informed of various vaginal shaping methods.
Bowel preparation
All of the patients consumed a semiliquid diet for 3
days prior to the operation. Metronidazole was also prescribed. At
12 h prior to the operation, the patients received a cleansing
enema and received intravenous nutrition. Prophylactic
cephalosporin antibiotics were administered 30 min prior to the
operation. Traditional skin preservation of the perineal region was
performed prior to the operation.
Pre-operative preparation
After receiving a general anesthetic, the patients
were placed in the lithotomy position (left high right low,
Trendelenburg position). In the middle of the umbilicus, a veress
needle was inserted to establish a pneumoperitoneum and maintain a
pressure of 14 mmHg. A trocar was then placed in site, which is the
same procedure as during colorectal surgery. The ureters and
ovaries in the abdominal cavity were then examined and the depth of
the pelvic cavity was measured. The length of the sigmoid colon and
mesocolon were assessed. The distribution and shape of the arterial
branches were observed by using transillumination of the mesocolon
to determine the length of the sigmoid colon and artery
revascularization.
Operative method
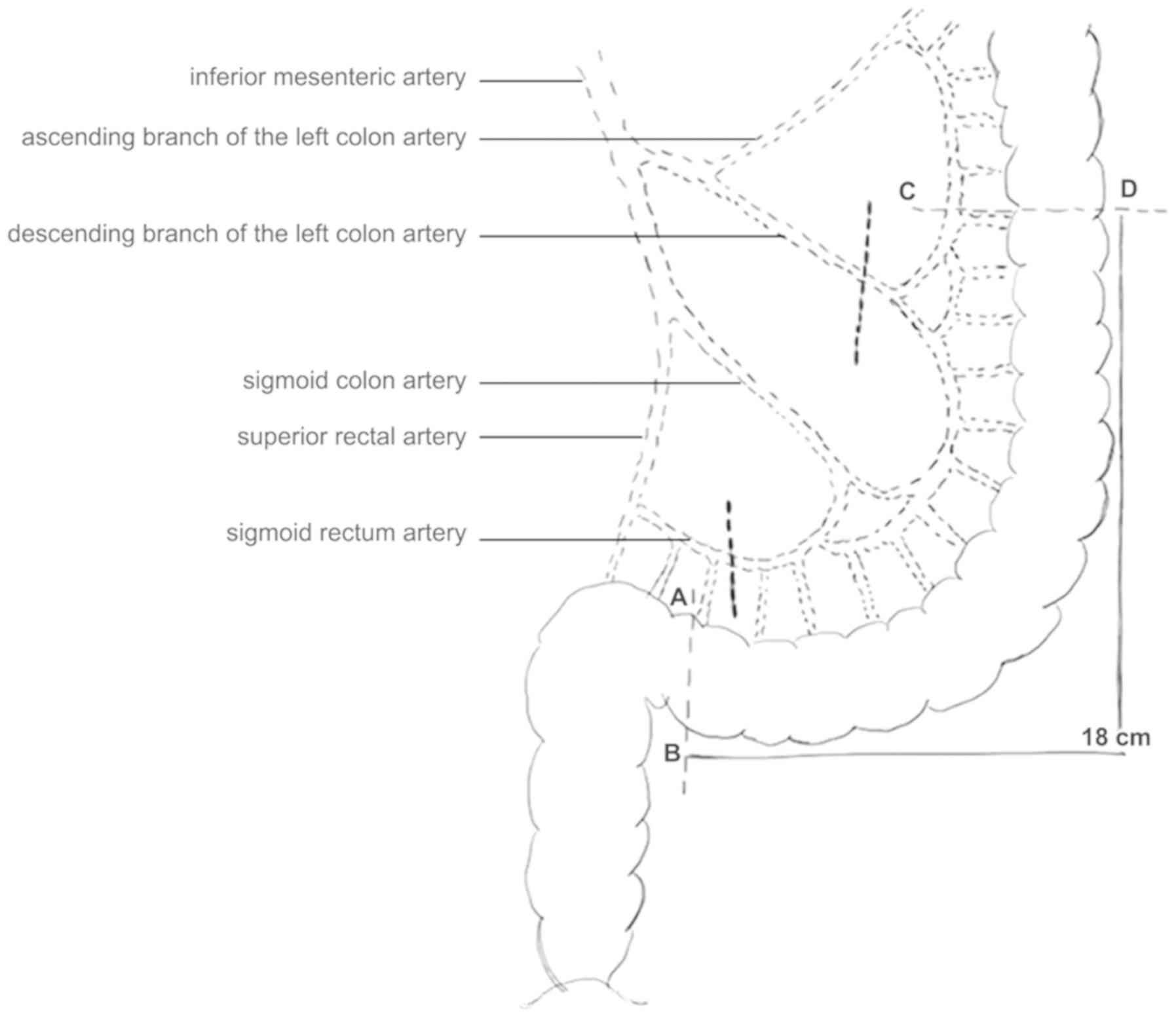
The operation was divided into 7 steps. The first
step was to probe the pelvic cavity and construct a tunnel. Under
the laparoscopy, the pelvic floor peritoneum was cut open and the
rectovesical pouch peritoneum was dissected. The pre-rectum space
was then separated by using sharp and blunt dissection, and the
width was 5–6 cm. The vagina and abdomen were then examined and a
tunnel linking the external vaginal stump was constructed. The
second step was to separate the sigmoid colon side peritoneum. The
third step was to locate the distal end of the transplanted
intestinal segment. The height of the sacral promontory was
considered the distal end of the transplanted intestinal segment
(AB terminus; Fig. 1), and was
divided under laparoscopy. The fourth step was to locate the
proximal end of the transplanted intestinal segment and to free it
completely. According to the depth of the pelvic cavity + 1/2
length of the mesocolon or a normal vaginal length + 5 cm, the
length of the transplanted intestinal segment was 16–18 cm due to
keeping the blood supply and meeting the length requirement for
transplantation. The length of a normal vagina is 13–14 cm, with an
average length of 12.8 cm. The measurement was performed from the
distal end of the transplanted intestinal segment (AB terminus)
using a scale line prepared prior to the operation. The proximal
segment of the sigmoid colon at a distance of 18 cm from the AB end
served as the proximal end of the transplanted intestinal segment
(CD terminus). The branches and shape of the sigmoid colon were
then observed, and the anterior and posterior peritoneum of the
mesocolon were freed along the AB and CD dotted line (Fig. 1). Subsequently, the lower artery of
the sigmoid colon and the descending branch of the left colon were
occluded and the main sigmoid colon artery was retained. The fifth
step was to cut the transplanted intestinal segment under the
laparoscopy and complete the anastomosis between the rectum and
sigmoid colon. The nail seat anastomat (PROXIMATE LLS Curved and
Straight Intraluminal Staplers; Johnson & Johnson) was
introduced into the pelvic cavity from the tunnel. The sigmoid
colon tube was longitudinally split 2 cm at 1.5 cm on the CD
terminus of the transplanted intestinal segment, and the anastomat
was placed in the intestinal tube through this incision and moved
to the upper section of the CD terminus. The puncture outfit of the
nail seat went out of the intestines from 1.0 cm above the CD
terminus. The proximal end of the sigmoid colon was then removed
using a closed cutter and the intestinal segment to be transplanted
was completely dissociated. Next, a stapler was inserted into the
rectum through the anus to the broken end, and the proximal end of
the sigmoid colon was anastomosed to the end of the rectum. The
sixth step was to rotate the intestinal segment mesocolon to be
transplanted 180 degrees clockwise horizontally to the pelvic
cavity. The seventh step was vaginoplasty (8).
Postoperative treatment
After the operation, the artificial vagina did not
require a vaginal mold and was washed once with clear water every
other day. Routine post-operative care included flushing around the
anus twice a day. Prior to the recovery of intestinal function, the
patients received intravenous nutrition support. After anal
exhaust, the diet of the patients gradually transitioned from a
liquid to a semi-liquid diet. All of the patients were given
prophylactic antibiotics and any changes in abdominal signs were
closely observed.
Follow-up
For the first month after the operation, the
patients were followed up once per week by using questionnaire as
previous (10) and telephone
interview. Two months after the operation, the period of follow-up
was once every 2 weeks. Three years after the operation, the period
of follow-up was once every 3 months. The follow-up included
assessments of vaginal size, volume, length and color, as well as
vaginal discharge and secretions. The married patients were also
questioned about aspects of their sex lives.
Control group of laparoscopic sigmoid
colovaginoplasty
After selecting a sigmoid segment based on vascular
anatomy and mesenteric length, the segment was mobilized using a
Harmonic scalpel. Through a 3-cm Pfannenstiel incision, the
dissociated sigmoid colon was pulled out to exteriorize and create
a purse. Continuity of the intestinal tract was restored using a
circular mechanical suture through the rectum. At the tip of the
newly created perineal space, an incision was made using a Harmonic
knife; the size of the incision was sufficient to allow free
passage of the isolated sigmoid colon segment. Subsequently, the
sigmoid autograft was sutured to achieve construction of a
normal-appearing vulva.
Statistical analysis
SPSS 22.0 software (IBM Corp.) was used to perform
the statistical analysis. Values are expressed as the mean ±
standard deviation or n (%). Statistical analyses were performed
using a Student's t-test for measurement data and a χ2
test for count data. P<0.05 was considered to indicate
statistical significance.
Results
Perioperative data
As presented in Table
I, the average operation time was 187±19 min, the average
intra-operative blood loss was 132±24 ml, the time of the first
meal after surgery was 4.3±1.1 days and the average post-operative
hospital stay was 7.5±1.2 days. The post-operative short-term
complication rate was 36.3% and the time of the first sexual
intercourse was 3.0±0.3 months. The operation time, intraoperative
blood loss, time of first meal after surgery, vaginal depth and
first sexual intercourse time of those who received total LSV were
significantly better compared with the control group of
laparoscopic sigmoid colovaginoplasty, whilst LSV also had higher
complication rate than laparoscopic sigmoid colovaginoplasty
(Table I). At two weeks after the
surgery, the abdominal laparoscopic incision had healed well. Four
cases developed surgical complications, such as excessive vaginal
secretion, vaginal opening stenosis and intermittent dull pain and
discomfort. The vaginal mucosa was pink with a small amount of
mucus.
 | Table I.Comparison of the relevant data
between total LSV and laparoscopic sigmoid colovaginoplasty. |
Table I.
Comparison of the relevant data
between total LSV and laparoscopic sigmoid colovaginoplasty.
| Group | Operation time
(min) | Intraoperative blood
loss (ml) | Time of first meal
after surgery (days) | Hospital stay
(days) | Complications | Vaginal depth
(cm) | First sexual
intercourse time (month) |
|---|
| Total LSV (n=11) | 187±19 | 132 (70–190) | 4.3
(3.0–6.0) | 7.5
(7.0–10.0) | 4 (36.3) | 16.4±0.6 | 3.0
(2.5–4.0) |
| Laparoscopic sigmoid
colovaginoplasty (n=14)a |
217±40.7 | 200
(100–300) | 5.5 (4.75–6) | 10.5 (6.7–12.5) | 3 (21.4) |
12.6±0.42 | 3 (2–6) |
| P-value | <0.05 | <0.05 | <0.05 | <0.05 | <0.05 | <0.05 | <0.05 |
Postoperative vaginal recovery during
3 year follow up
Anatomical success was defined as the ability to
insert two fingers with ease into the vagina and a vaginal length
of >6 cm (11). The follow-up
results at 3 years after the operation indicated that the depth and
width of the newly created vagina in all of the 11 patients reached
the anatomical standard, including vaginal secretions and the
possibility of sexual intercourse (12,13). The
average artificial vagina depth was 16.4±0.6 cm (Table I).
Female sexual function index
(FSFI)
Among the 7 married patients, 5 patients were
satisfied with their sex lives after the operation. In one patient,
vaginal secretion was excessive for the first 6 months. One married
patient felt no sexual arousal. The other married patients had
active sexual relations, function and satisfaction. The FSFIs of
the 7 married patients who received total LSV were not
significantly different from those in the control group of
laparoscopic sigmoid colovaginoplasty (Table II) (9). All subjects, including the control
group, were assessed in an identical/comparable way.
 | Table II.Comparison of the female sexual
function indexes of the married patients between total LSV and
laparoscopic sigmoid colovaginoplasty. |
Table II.
Comparison of the female sexual
function indexes of the married patients between total LSV and
laparoscopic sigmoid colovaginoplasty.
| Index | Total LSV (married
patients, n=7) | Laparoscopic sigmoid
colovaginoplasty (n=14)a | P-value |
|---|
| Sexual desire | 3.2±0.5 | 4.19±0.24 | 0.241 |
| Sexual arousal | 3.6±1.2 | 4.19±0.07 | 0.672 |
| Lubrication | 2.4±1.1 | 4.19±0.07 | 0.216 |
| Orgasm | 4.6±1.5 | 4.07±0.32 | 0.304 |
| Satisfaction | 3.3±1.5 | 4.41±0.25 | 0.215 |
| Pain | 3.1±2.1 | 4.22±0.33 | 0.402 |
| Total points | 20.2±7.9 | 24.79±1.17 | 0.202 |
Discussion
With the development of minimally invasive surgery,
the goal of surgeons is to improve the post-operative psychological
and physiological integrity of patients with congenital absence of
a vagina (14). This goal may be
achieved by non-invasive laparoscopy using fine laparoscopic
instruments. However, performing total LSV is relatively complex,
as the procedure involves resection of the transplanted intestinal
segment, the placement and fixation of a nail seat anastomat and
anastomosis of the broken ends of the intestine under laparoscopy.
Additional issues for surgeons are to ensure a sufficient length of
the sigmoid colonic flap and vascular bundles, and adequate blood
supply has always been a challenge for surgeons (15,16).
Therefore, in addition to improving operative details, it is
necessary to fully understand the mesenteric vascular anatomy,
which is important for increasing the quality of laparoscopic
surgery.
A key issue in LSV is dealing with the problem of
the large tension in down-placing the transplanted intestinal
segment. The two major factors that affect the success of
down-placement of the transplanted intestinal segment are the
mesocolon and the vascular distribution of the mesocolon. The
sigmoid colon arteriovenous vein is an important branch of the
inferior mesenteric artery and vein. Its position is closer to the
pelvic cavity as compared with the ascending branch and descending
branches of the left colon artery (17), which is the most important branch of
the transplanted intestinal segment. In the cases described in the
present study, the sigmoid colon was rotated 180 degrees clockwise
to the pelvic cavity, and vaginoplasty was then performed. This
procedure is relatively simple, and it does not necessitate
excessive dissociation of the sigmoid mesocolon and blood vessels.
It also minimizes the destruction of the vascular arch and ensures
the blood supply of the transplanted intestinal segments. Mesocolon
rotation has two major advantages: First, the arteriovenous
location of the sigmoid colon is close to the pelvic cavity, which
is near the surgical site; second, the activity of the sigmoid
mesocolon is high. Thus, the transplanted intestinal segment may be
freed relatively easily, followed by down-placement in the pelvic
cavity and pulling it to the vaginal entrance. The influence of the
mesocolon and vascular distribution on mesocolon rotation is
relatively small. Thus, mesocolon rotation has a wide range of
applications. As compared with the traditional longitudinal
down-placement of the transplanted intestinal segment, mesocolon
rotation is superior in terms of solving the problem of large
tension in down-placing the transplanted intestinal segment. A
problem with longitudinal down-placement of the transplanted
intestinal segment is that if the sigmoid mesocolon is too short or
there is adhesion in the intestinal tube and pelvic cavity during
the operation, excessive traction of the transplanted intestinal
segment may cause ischemic tissue necrosis. To solve the problem of
large tension when down-placing the transplanted intestinal
segment, Karateke et al (18)
suggested the following: First, in cases where the vascular
distribution is narrow but the mesocolon is long, all of the
sigmoid colon artery branches may be retained to create a vagina
directly or after rotating by 180 degrees. Second, in cases where
the mesocolon is relatively short but the sigmoid colon artery has
wide branches and a large area, it may cut off the proximal end and
middle part of the mesocolon may be cut off, followed by rotation
of the intestinal segment by 180 degrees clockwise without
affecting the blood supply. In addition, the length of the
mesocolon may be extended by transversely cutting the anterior and
posterior peritoneum in the root or middle part of the mesocolon,
thereby reducing the tension (19).
Due to the unique anatomical structure of the sigmoid colon,
mesocolon rotation may be employed safely and effectively to solve
the problem of tension while down-placing the transplanted
intestinal segment.
In the present study, the post-operative follow-up
indicated that all of the 11 patients achieved normal anatomical
function. Among the 7 married patients, 5 patients were satisfied
with their sex lives after the operation, and 1 patient had vaginal
pain or discomfort during sex. One married patient felt no sexual
arousal during intercourse. The other married patients had active
functioning sexual relations. The FSFIs of the 7 married patients
who received total LSV were not significantly different from those
in the control group of laparoscopic sigmoid colovaginoplasty.
Overall, the FSFI indicated a high degree of sexual satisfaction
after total LSV. Although post-operative intestinal complications,
including vaginal contracture, excessive vaginal secretion and
vaginal stenosis may occur (20),
these implications may still be effectively controlled and
treated.
The limitations of the present study are the short
follow-up times for the patients (<3 years). Further long-term
follow-up studies are therefore required. In addition, it may be
recommended to perform left colon angiography prior to the surgery,
but this was not performed in the present study.
In summary, the application of mesocolon rotation
and reverse puncture in total LSV is safe and feasible. As compared
with traditional surgery, the operation time was short, the wound
was small and the operative procedures affected by the mesocolon
and vascular distribution was less. To improve long-term outcomes
and ensure the best surgical results, multidisciplinary teams and
comprehensive psychological and medical support are required. The
sample size in the present study was small and the results require
to be confirmed in a large randomized multicenter study.
Acknowledgements
Not applicable.
Funding
This study was supported by Natural Science
Foundation of Xinjiang Uygur Autonomous Region (grant no.
2017D01C305).
Availability of data and materials
The datasets generated and/or analyzed during the
current study are available from the corresponding author on
reasonable request.
Authors' contributions
WZ and CL analyzed and interpreted the patient data.
WC, TL and HG collected the patients' information. XX designed the
study, interpreted the data and was a major contributer in writing
the manuscript. HZ interpreted the patient data, contributed
significantly to drafting the study, made revisions for important
intellectual content and gave final approval of the version to be
published. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The protocol of the present study was approved by
the Ethics Committee of the First Affiliated Hospital of Xinjiang
Medical University (Urumqi, China; no. K201301-01) and informed
consent was obtained from all participants.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Creatsas G and Deligeoroglou E: Creatsas
modification of Williams vaginoplasty for reconstruction of the
vaginal aplasia in Mayer-Rokitansky-Kuster-Hauser syndrome cases.
Womens Health (Lond). 6:367–375. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kuessel L, Wenzl R, Marschalek ML, Slavka
G, Doerfler D and Husslein H: Using the Wharton-Sheares-George
method to create a neovagina in patients with
Mayer-Rokitansky-Küster-Hauser syndrome: A step-by-step video
tutorial. Fertil Steril. 106:e20–e21. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Krege S, Walz KH, Hauffa BP, Körner I and
Rübben H: Long-term follow-up of female patients with congenital
adrenal hyperplasia from 21-hydroxylase deficiency, with special
emphasis on the results of vaginoplasty. BJU Int. 86:253–259. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zhao YZ, Jiang H, Liu AT, Jiang DZ, Zhu
XH, Qiu M, Zheng XM, Lin ZH, Yuan XB and Zhang JL:
Laparoscope-assisted creation of a neovagina using pedicled ileum
segment transfer. World J Surg. 35:2315–2322. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zhong CX, Wu JX, Liang JX and Wu QH:
Laparoscopic and gasless laparoscopic sigmoid colon vaginoplasty in
women with vaginal agenesis. Chin Med J (Engl). 125:203–208.
2012.PubMed/NCBI
|
|
6
|
Atallah D, Salameh C, Sarkis R, Ghossain
M, Safi J, Moubarak M, Ghanameh W, Moukarzel M and El Kassis N:
Laparoscopic treatment of vaginal agenesis: Three cases. J Med
Liban. 62:227–231. 2014.(In French). PubMed/NCBI
|
|
7
|
Ichihara K and Masumori N: Sex
reassignment surgery with laparoscopic sigmoid colon vaginoplasty
in a male to female transsexual: A case report. Nihon Hinyokika
Gakkai Zasshi. 107:126–128. 2016.(In Japanese). PubMed/NCBI
|
|
8
|
Bouman MB, Buncamper ME, van der Sluis WB
and Meijerink WJ: Total laparoscopic sigmoid vaginoplasty. Fertil
Steril. 106:e22–e23. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Cao L, Wang Y, Li Y and Xu H: Prospective
randomized comparison of laparoscopic peritoneal vaginoplasty with
laparoscopic sigmoid vaginoplasty for treating congenital vaginal
agenesis. Int Urogynecol J. 24:1173–1179. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Meston CM: Validation of the female sexual
function index (FSFI) in women with female orgasmic disorder and in
women with hypoactive sexual desire disorder. J Sex Marital Ther.
29:39–46. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Fedele L, Bianchi S, Zanconato G and
Raffaelli R: Laparoscopic creation of a neovagina in patients with
Rokitansky syndrome: Analysis of 52 cases. Fertil Steril.
74:384–389. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zhou JH, Sun J, Yang CB, Xie ZW, Shao WQ
and Jin HM: Long-term outcomes of transvestibular vaginoplasty with
pelvic peritoneum in 182 patients with Rokitansky's syndrome.
Fertil Steril. 94:2281–2285. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Allen LM, Lucco KL, Brown CM, Spitzer RF
and Kives S: Psychosexual and functional outcomes after creation of
a neovagina with laparoscopic Davydov in patients with vaginal
agenesis. Fertil Steril. 94:2272–2276. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Karateke A, Haliloglu B, Parlak O, Cam C
and Coksuer H: Intestinal vaginoplasty: Seven years' experience of
a tertiary center. Fertil Steril. 94:2312–2315. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zhang M, Li S, Huang X, Du H, Wang C,
Zhang L, Li Y, Zhang J and Wang Z: Transumbilical single-incision
laparoscopic vaginoplasty hybrid transperineal approach using a
sigmoid colon segment: Initial twenty-five cases. Int Urol Nephrol.
48:1401–1416. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Cai B, Zhang JR, Xi XW, Yan Q and Wan XP:
Laparoscopically assisted sigmoid colon vaginoplasty in women with
Mayer-Rokitansky-Kuster-Hauser syndrome: Feasibility and short-term
results. BJOG. 114:1486–1492. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Grimsby GM and Baker LA: The use of
autologous buccal mucosa grafts in vaginal reconstruction. Curr
Urol Rep. 15:4282014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Karateke A, Gurbuz A, Haliloglu B, Kabaca
C and Koksal N: Intestinal vaginoplasty: Is it optimal treatment of
vaginal agenesis? A pilot study. Surgical method of sigmoid colon
vaginoplasty in vaginal agenesis. Int Urogynecol J Pelvic Floor
Dysfunct. 17:40–45. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Pan P: Surgical and functional outcome of
sigmoid colon-vaginoplasty in Mayer-Rokitansky-Kuster-Hauser
syndrome. IJROG. 6:44412017.
|
|
20
|
Kapoor R, Sharma DK, Singh KJ, Suri A,
Singh P, Chaudhary H, Dubey D and Mandhani A: Sigmoid vaginoplasty:
Long-term results. Urology. 67:1212–1215. 2006. View Article : Google Scholar : PubMed/NCBI
|