Introduction
In the reconstruction of large full-thickness eyelid
defects, it is difficult to find a suitable tissue for functional
repair. Scuderi et al first reported the use of an axial
nasal chondromucosal flap for reconstruction of the
tarsoconjunctival plane in full-thickness eyelid defects (1–4). The
technique is associated with the use of a local skin flap or with a
skin graft for skin repair. The axial chondromucosal flap receives
its blood supply from the dorsal nasal artery. The question of
whether the angular artery may be used as a pedicle of the island
nasal chondromucosal flap remains to be clarified.
Currently, there is a lack of detailed description
on the angular artery, even where the retroangular artery flap has
been widely used. Therefore, in the present study, a detailed
analysis was performed on the angular artery. The different
origins, course, distributions and surrounding relationships of the
angular arteries were investigated. Utilizing the findings of this
anatomical study, an island nasal chondromucosal flap based on the
angular artery was used for clinical cases of full-thickness lower
eyelid defects, in association with an orbicularis oculi
myocutaneous flap for skin repair.
Materials and methods
Cadavers
Once institutional approval from the Chinese Peking
Union Medical College was obtained to perform the present study
using cadavers, 11 Chinese adult cadavers, including 7 males and 4
females (22 hemi-faces), were dissected to investigate the
relationship between the angular artery and other anatomic
structures of the nose.
Anatomical study in cadavers
The present study was conducted in accordance with
the declaration of Helsinki. Written informed consent had been
previously obtained from all participants. Prior to dissection, the
cadavers were injected with a red latex solution into the bilateral
common carotid arteries and two of the cadavers were injected
bilaterally with a blue latex solution into the facial veins. The
dissections were carried out from superficial to deep levels, and
the vessels and nerves were preserved as they were revealed. The
vascular and nervous anatomy of the nasal dorsum and paranasal
region was revealed under ×3.5 loupe magnification.
Clinical application
The anatomical results identifed in the present
study were then applied to clinical research.
Surgical technique
Flap elevation involves simple surgical steps and
can be performed under local anesthesia. In this study, the
surgical technique was applied to the clinical cases.
The flap based on the angular vessels, including the
cranial portion of the upper lateral cartilage and the
corresponding nasal mucosa, was harvested depending on the size of
the defect to be repaired. The cartilage harvest range utilized is
15–18×5–8 mm. The mucosal portion of the flap can be extended,
depending on the reconstructive need.
Following skin incision of ∼20–30 mm along the
nasojugal fold from the ala nasi up to the direction of inner
canthus, the subcutaneous dissection was extended superiorly to the
inner canthus and glabellum, and inferiorly to the lower margin of
the upper lateral cartilage. The angular artery was identified
using a preoperative Doppler probe and an intraoperative manual
palpation. During surgery, pressure was applied manually on the
artery at the lower border of the nasal alar groove to ensure blood
flow of the angular artery from the cephalic to the caudal region.
The angular artery and vein are close together, therefore, their
location in the pedicle of the flap was confirmed prior to
attempting dissection downwards. The pedicle includes the angular
vessels, a piece of muscle around them, and the infratrochlear
nerve. An incision was made through the upper lateral cartilage,
including the perichondrium and the nasal mucosa at the distal end
of the flap. From both ends of that incision, two vertical cuts
were made at a level where a part of the upper lateral cartilage
was to be included, based on the width of the defect to be
repaired. The flap was then raised (Fig. 8). Formation of the neurovascular
pedicle should be dissected in consideration of the rotation arc
from the donor to the defect site. Under certain conditions, this
pedicle may be extended to the medial canthus. A tunnel was
dissected in the subcutaneous plane of the infraorbital and medial
canthal region. The flap, elevated over the pedicle through careful
dissection, was passed through the tunnel and sutured in order to
reconstruct the tarsoconjunctival plate of the missing eyelid.
Meticulous attention was paid to the graft, and sutures and knots
on the conjunctival surface were avoided. The donor site was closed
immediately, and a nasal pack was applied for 48 h.
Reconstruction was then performed with a chondro
mucosal flap based on the angular vessels and the accompanying
nerve, associated with an orbicularis oculi myocutaneous flap for
skin repair.
Results
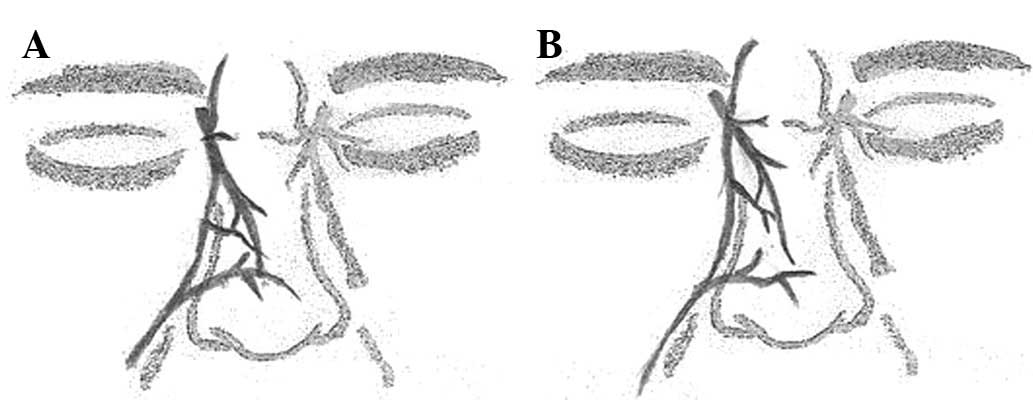
External nose vascular supply
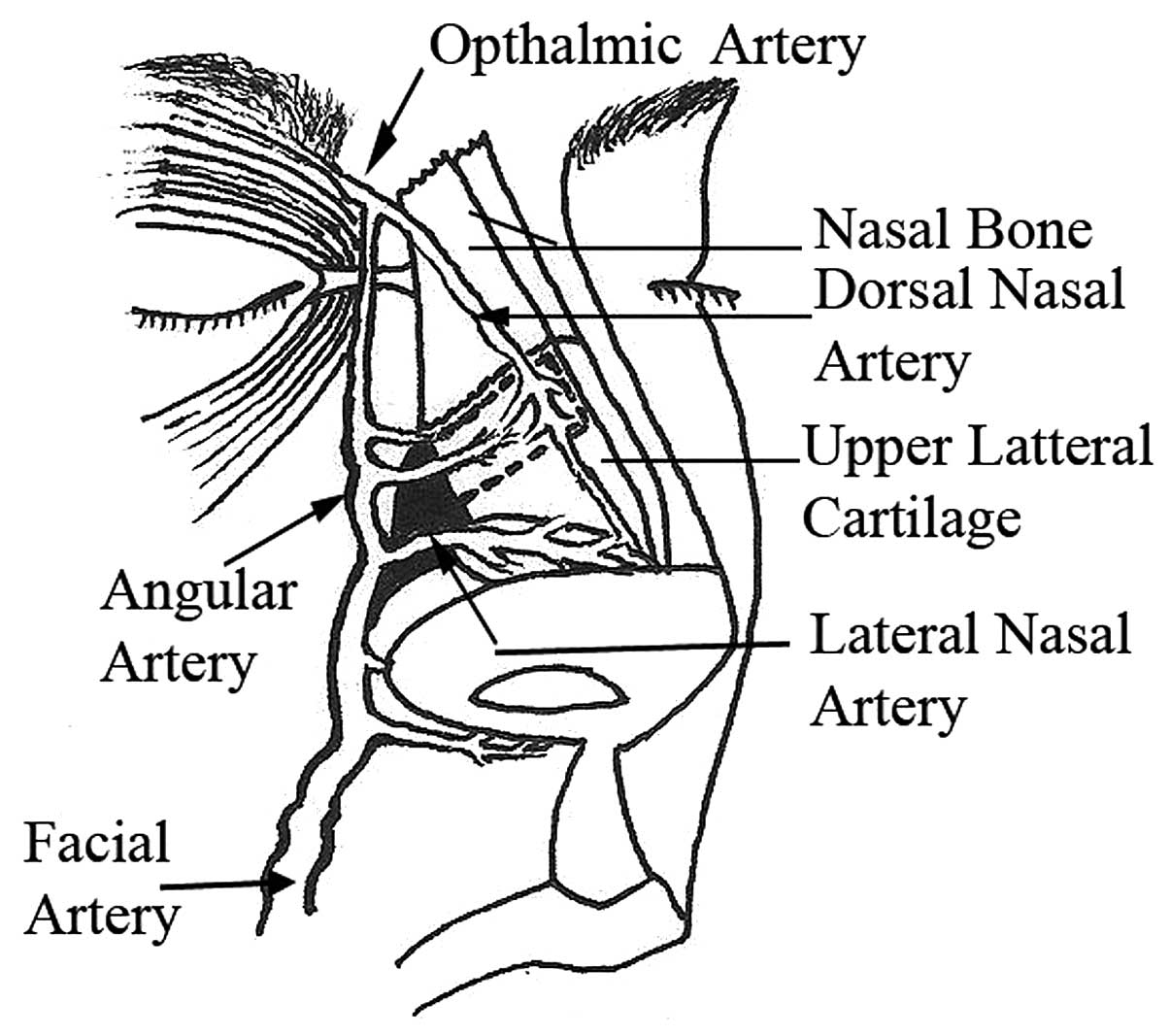
The external nose received its blood supply from the
lateral and dorsal nasal, angular and small columellar arteries.
These arteries were structured as branches and anastomoses, forming
a vascular network (Fig. 1).
Originating from the ophthalmic artery, the dorsal
nasal artery descended along the dorsum, terminated at the alar
groove and was anastomosed with the lateral nasal artery.
The lateral nasal artery originated mainly from the
facial artery. In certain samples, the facial artery did not
terminate at the nasal ala, thus the lateral nasal artery
originated from the infraorbital artery or the nasoseptal artery
from the superior labial artery.
The small columellar artery, a branch of the
superior labial artery of the facial artery, ran upward in the
columella and parallel to its contralateral partner.
The angular arteries (angled where the upper and
lower eyelids meet) traveling along the nasojugal fold (with one
end near the alar groove and the other end near the medial canthus)
were consistently observed in all specimens. The angular artery
branched out into the upper two-thirds of the lateral nasal region
and anastomosed with other vascular branches of the nasal dorsum.
The artery was involved in the composition of a reliable vascular
arcade in the external nasal region.
Angular artery origin
The angular artery was found to originate from
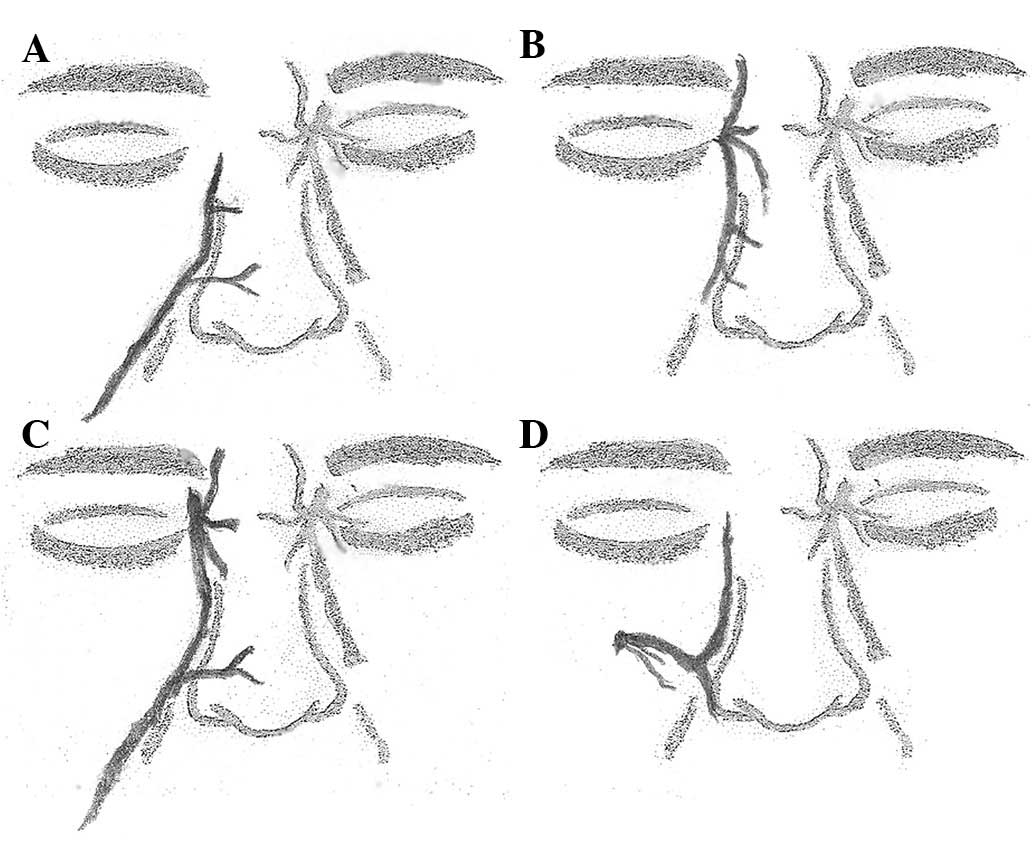
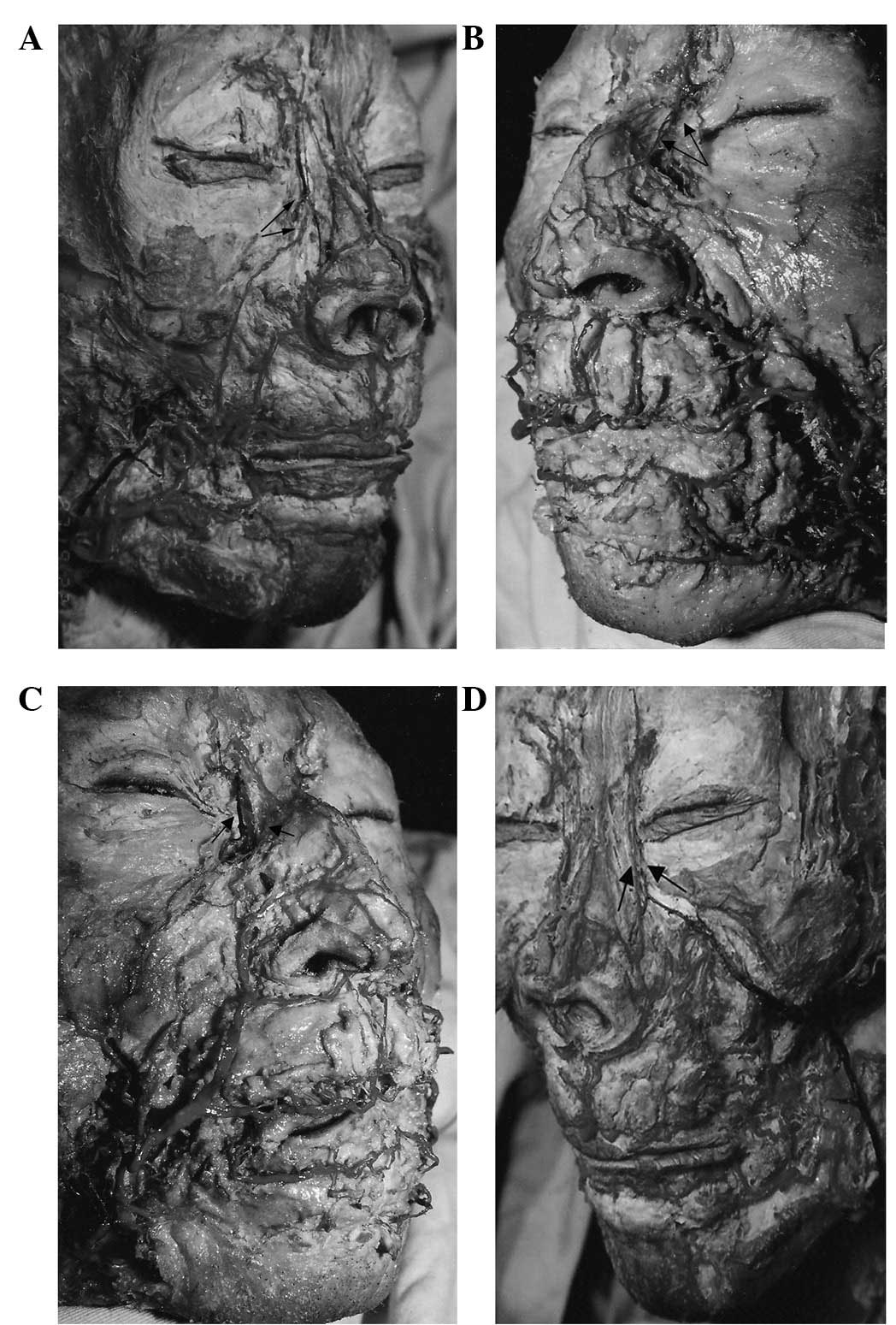
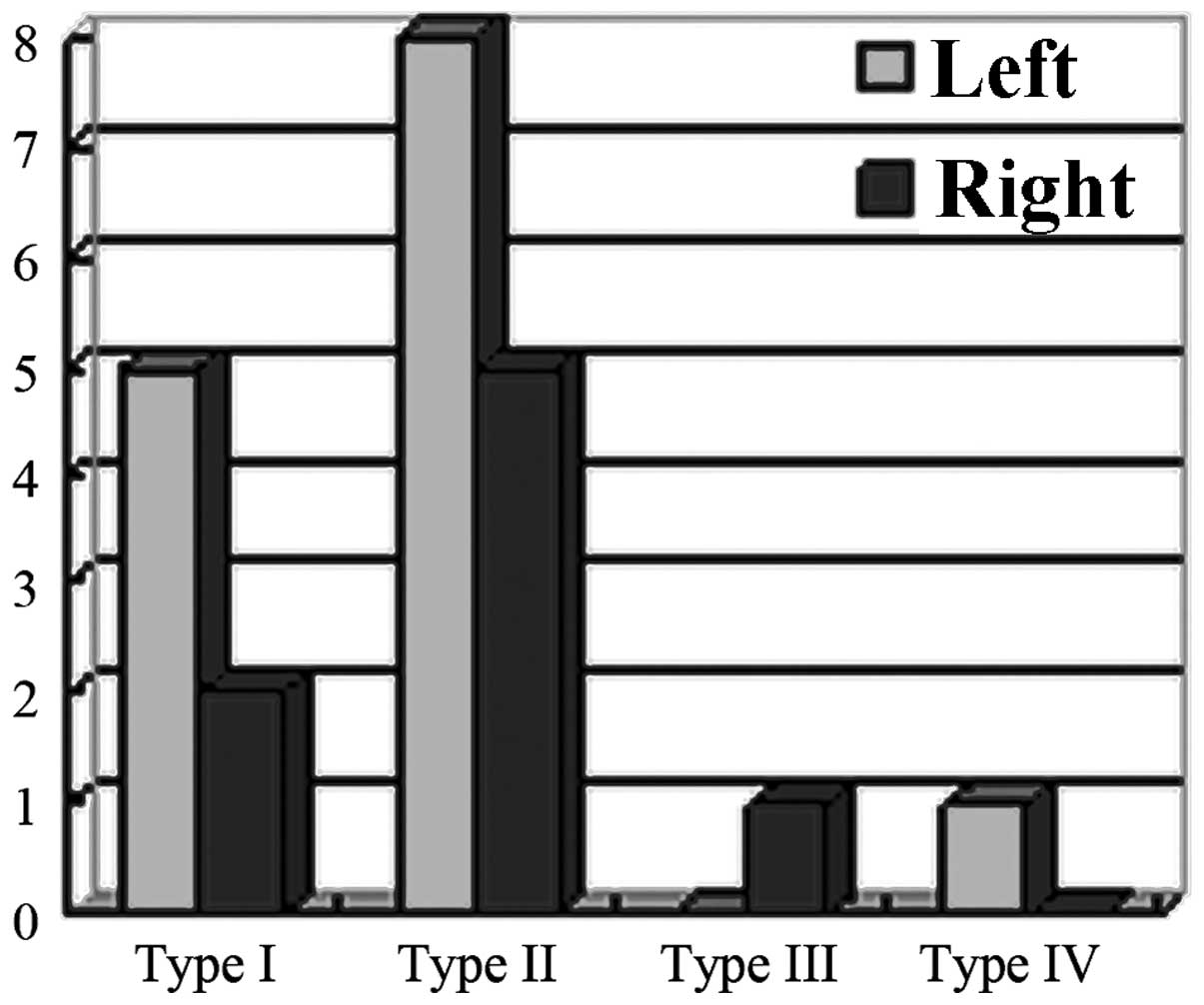
various other arteries. Four types of sources were observed in the
specimens (Figs. 2 and 3). In Type I examples, the angular
arteries originated at the terminal branch of the facial artery.
The facial artery branched out as the superior and inferior labial
arteries and the lateral nasal artery and then terminated as the
angular artery, which ran through the side of the nose and the
medial canthus. This type was observed in seven hemi-faces (31.8%,
5 in left hemi-faces, 2 in right; Fig.
3A). In Type II, the angular artery was revealed to originate
from the ophthalmic artery. The blood flow of the angular artery
was from top to bottom and its terminal branches were in the
paranasal region and the nasal dorsum. In this type, 13 hemi-faces
of specimens were observed (59.1%, 8 in left hemi-faces, 5 in
right; Fig. 3B). In Type III, the
angular artery was an anastomosis consisting of the terminal branch
of the facial artery and the branch of the dorsal nasal artery.
Anastomosis occurred on the surface of the upper lateral cartilage.
Type III was observed in 1 hemi-face (4.5%, 1 in right hemi-face;
Fig. 3C). In Type IV, the angular
artery originated from the infraorbital artery. The infraorbital
artery, the terminal branch of the maxillary artery, emerged at the
infraorbital foramen and terminated at the angular artery. Type IV
was also observed in only 1 hemi-face (4.5%, 1 in left hemi-face;
Fig. 3D). Asymmetry of the
vascular patterns between the two hemi-noses was encountered in the
same specimen in 6 cases (54.5%; Fig.
4).
Relationship between angular and dorsal
nasal arteries
In Types II and III, the angular artery originating
from the internal carotid arterial system was observed to have two
different special relationships with the dorsal nasal artery
(Fig. 5). In the one-branch type,
the angular artery shared the trunk of the dorsal nasal artery,
while in the multi-branch type, the angular artery originated
separately from the ophthalmic artery. Its terminal branches were
anastomosed with the branches of the dorsal or lateral nasal
artery.
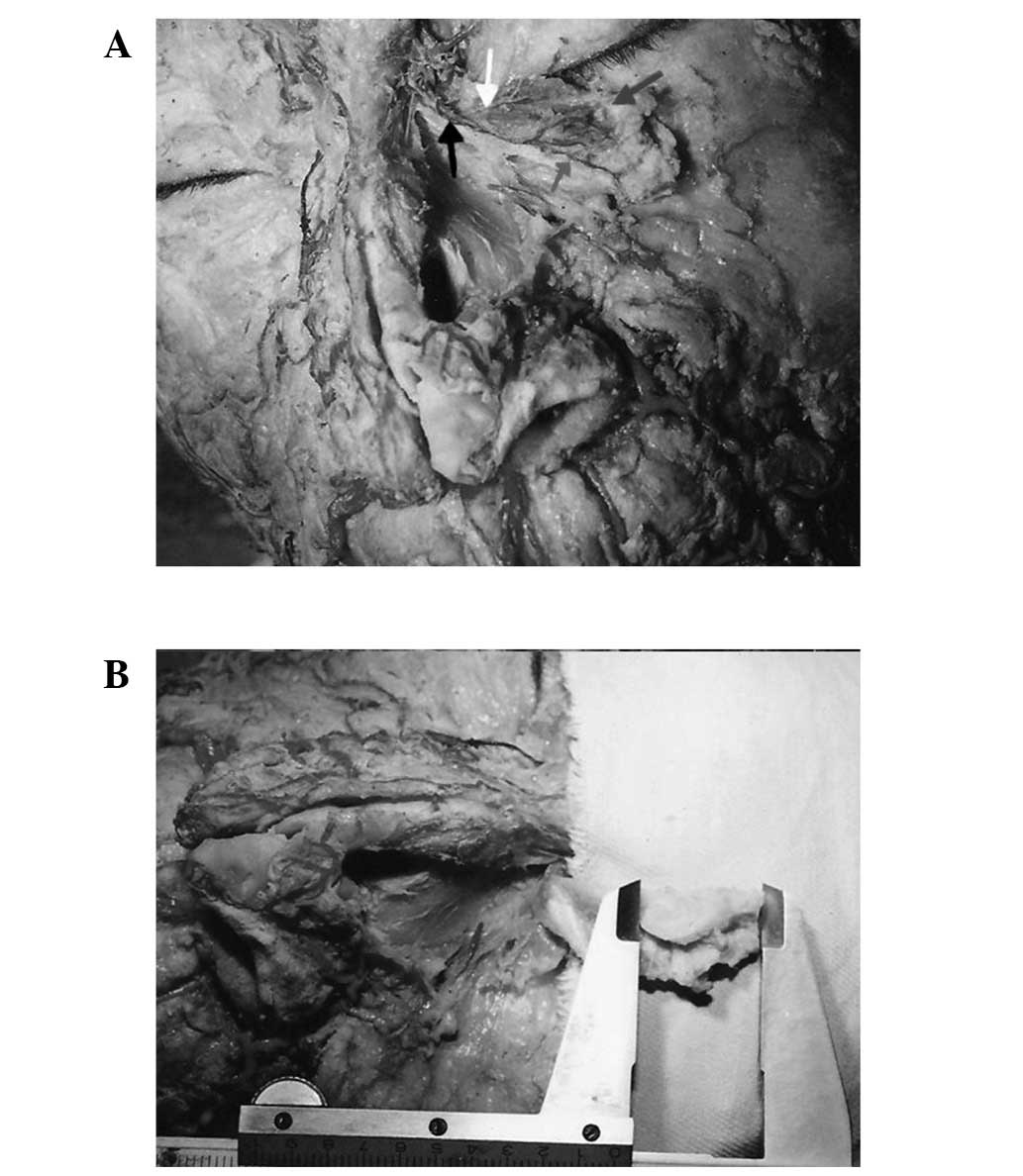
Course of the angular vessels and
surrounding structures
The venous drainage of the external nose had
similarly named veins that accompanied the arteries. The blood
drained via the facial veins or the pterygoid plexus, specifically
via the ophthalmic veins into the cavernous sinus.
The accompanying vein of the angular artery was also
observed in specimens of the present study. The angular artery and
its vein were located together. The artery was superficially
embedded in the fibres of the levator labii superioris alaeque nasi
and the vein was located at a deeper level with the angular artery
at the medial canthus. The angular vein was medial to the angular
artery above the medial canthus and lateral to the angular artery
below the medial canthus. At the inferior end of the nasal bone, a
vein originating from the surrounding tissues of the upper lateral
nasal cartilage was infused into the angular vein, which lay deep
in the layer of the levator labii superioris alaeque nasi (Fig. 3B and C and Fig. 6).
Another observation was that the infratrochlear
nerve consistently appeared to accompany the angular artery. The
nerve gave off branches that reached the nasal lateral region and
were distributed into the nasal lateral cartilage and the
corresponding mucosa.
Flap model in cadaver anatomy
In the present study, anatomical analysis showed
that the angular vessels were constant in course and distribution
and branched out into the surrounding tissues of the upper lateral
cartilage, even though the angular artery had diverse origins.
Therefore, the angular vessels were available for use as a vascular
pedicle of an island chondromucosal flap in the lateral side of the
nose, adjacent to the nasojugal fold. The blood supply to the flap
was derived from the branches of the angular artery, which
stretched onto the surface of the upper lateral cartilage. This
flap, based on the angular vessels and infratrochlear nerve, was
considered able to survive in an eyelid defect reconstruction and
provide sensation following a one-stage surgery (Fig. 7).
The anatomical results from the present study were
then applied to clinical research.
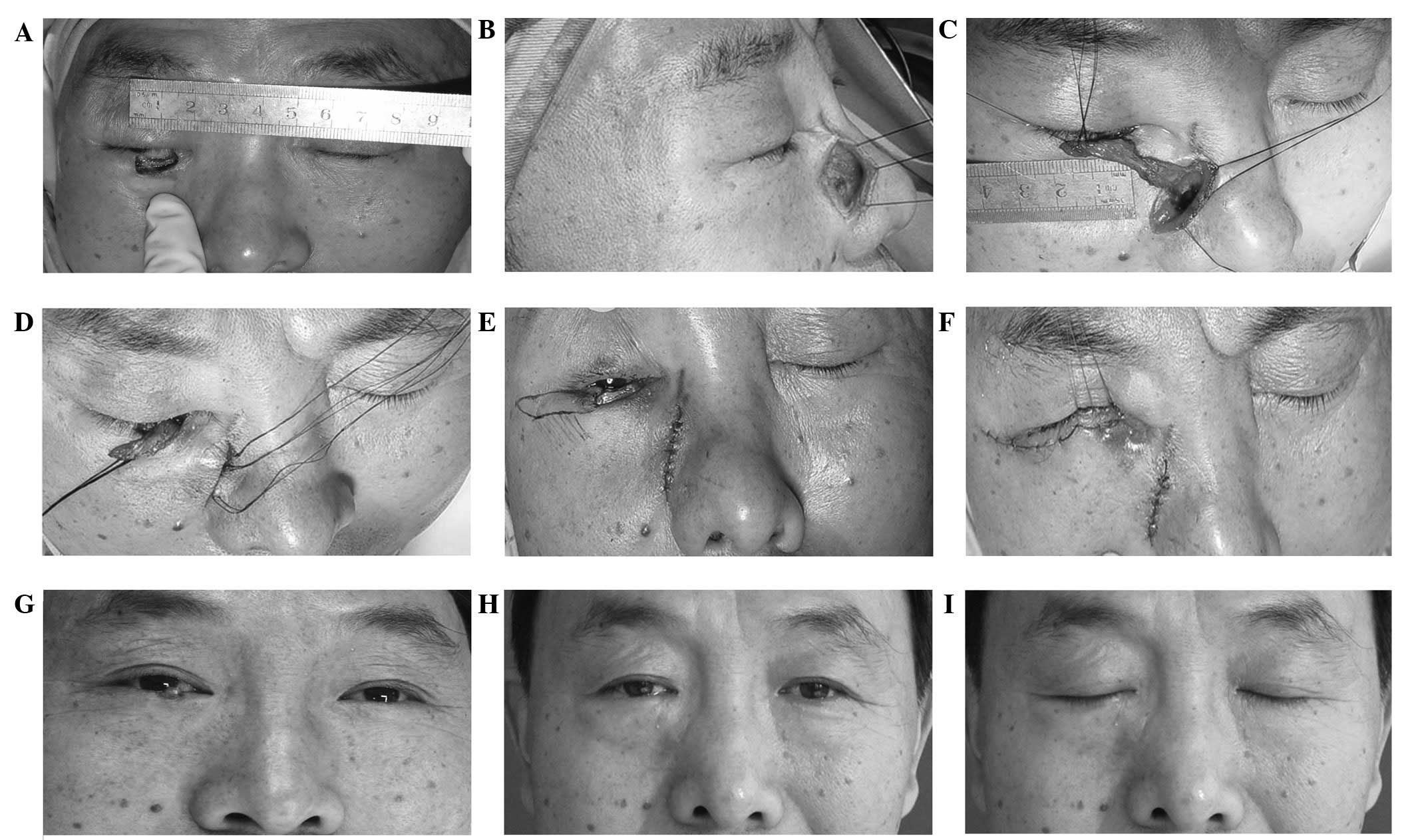
Clinical application - a representative
case
A 52-year-old male patient underwent ablation of a
malignant tumor on his right lower eyelid. Following a wide
excision of the tumor, there was a resulting 15×10 mm defect of the
eyelid. Pathological examination confirmed the absence of malignant
cells in the margins of the surgical specimen and therefore
reconstruction of the full-thickness eyelid defects was performed
during a one-stage surgery with the patient under local anesthesia.
An island chondromucosal nasal flap based on the angular artery was
used to reconstruct the posterior defects and an adjacent
orbicularis oculi myocutaneous flap was used to reconstruct the
anterior defects of the eyelid. The post-operative course of the
patient was uneventful and the donor site near the nose healed
completely. The reconstructed eyelid was not bulky and secondary
revisions were not required. A follow-up after two years showed
complete recovery of eyelid functions. The patient was extremely
satisfied with the esthetic results, which provided a close match
to the original quality of the skin and had minimal donor site
complications. There was no tumor recurrence, ectropion or
entropion, retraction, epiphora or minor conjunctival irritation of
the eyelid. No observations of airway obstructions due to a defect
in the donor site have been noted (Fig. 9).
Discussion
Numerous techniques have been utilized for eyelid
reconstruction (5–8). An axial chondromucosal flap from the
nose based on the dorsal nasal artery was first used for
reconstruction of the tarsoconjunctival plane of full-thickness
eyelid defects in 1992 (2). The
authors reviewed their experience of using the nasal chondromucosal
flap for an upper eyelid reconstruction and presented the merits of
the technique. Firstly, the chondromucosal flap was observed to be
safe, reliable and did not require long-term eye occlusion. The
procedure was a one-stage surgery and did not damage the remnant
lid (1). Secondly, the presence of
vascularized cartilage in the flap warranted the required support
of the reconstructed eyelid. Therefore, this reconstruction was
anatomically complete and esthetically well-accepted by patients
(3). Total reconstructions were
also achievable with this technique (9).
Through anatomical study of cadavers, the authors
identified that the nasal chondromucosal flap from the lateral side
of the nose received its vascular supply not only from the dorsal
nasal artery but also from the angular artery. This was involved in
the composition of a reliable vascular anastomosis network in the
external nasal region.
Although flaps based on the angular artery in an
antegrade or retrograde manner are widely used for reconstruction
of facial defects (10–14), detailed studies on the angular
artery are rare and generally inadequately described in anatomy
books and literature.
The angular artery had originally been thought of as
the terminal branch of the facial artery (15), however, various final branches of
the facial artery have been reported in previous literature. The
distribution patterns of the facial artery described in this
literature differ significantly from one another. Mitz et
al(16) stated that the facial
artery ended as the angular artery in only 4% of the 50 facial
arteries of adult French cadavers. Koh et al reported that
the facial artery ended as the angular artery in 36.3% of 91 Korean
specimens (17). According to
Niranjan, the final branch of the facial artery was the angular
artery in 68% of 25 British specimens (18). Loukas et al examined 284
hemi-faces and reported that the facial artery ended as the angular
artery in 51.4% of the cases, the others terminated as the lateral
nasal or superior labial artery or as a mere rudimentary branch
(19). Nakajima et al
observed the angular artery in 18 of 25 facial arteries (72%)
(20). In the present anatomical
study, the facial artery ended as the angular artery in 8 of 22
Asian hemi-faces (36.4%).
Previous studies reported that if the facial artery
was absent or poorly developed, the compensation of the blood
supply was usually provided by the ophthalmic artery, infraorbital
or transverse facial artery in the ipsilateral position or a more
developed contralateral facial artery (21,22).
In the present study, a detailed analysis on the
origins, courses, distributions and surrounding relationships of
the angular artery was performed. The origin of the angular artery
was classified into four types. The angular artery is usually an
arterial branch rather than a main continuation of the facial
artery. Even when the origin of the angular artery was the facial
or infraorbital artery, which were allocated as Types I and IV, a
reverse blood flow was observed following the blood flow of the
facial artery being stopped by the manual application of pressure
at the proximal end (23). This
procedure confirmed the possibility of safe elevation of an
antegrade or retrograde flow-arterialized flap based on the angular
artery. When the angular artery originated from the ophthalmic
artery (Types II and III), there were two patterns of relationships
with the dorsal nasal artery. The trunk of the dorsal nasal artery
was shared or the artery originated separately from the ophthalmic
artery. The angular artery reportedly anastomosed with the dorsal
nasal artery via a thin or thick branch in the region of the medial
canthus (24).
Although the angular artery had varying origins, its
course and distribution were constant. The angular artery branched
out onto the surface of the upper lateral cartilage. The vessel was
therefore available for use as a pedicle of the nasal
chondromucosal flap. Its accompanying vein was located at a deeper
level with the artery. A small vein draining the surrounding
tissues of the upper lateral cartilage coursed beneath the levator
labii superioris alaeque nasi and was infused into the angular vein
at the inferior end of the nasal bone. The infratrochlear nerve
consistently appeared to accompany the angular artery. Thus, the
pedicle of the island nasal chondromucosal flap includes the
angular artery, angular vein, and infratrochlear nerve. To preserve
the vein in the pedicle, a strip of muscle fiber from the levator
superioris alaeque nasi should be included in the pedicle.
Based on the anatomical findings, the present study
suggests the utilization of island nasal chondromucosal flap based
on the angular artery for repairing the posterior lamella of the
eyelids. In the present clinical case, an island nasal
chondromucosal flap based on the angular vessels and the
infratrochlear nerve, together with an orbicularis oculi
myocutaneous flap, were used successfully to reconstruct
full-thickness defects. Excellent results were achieved and nasal
distortion or abnormal scarring did not occur.
A flap based on the angular vessels has the same
merits as a flap based on the dorsal nasal artery. In addition, the
pedicle of the flap is closer to the incision, therefore the
pedicle elevation and rotation of the flap are easier. The design
of the pedicle does not damage the lateral nasal region, the nasal
dorsum or the thin soft tissues on the surface of the nasal bone,
allowing the figure of the nose to be maintained. Depending on the
reconstruction required, the island nasal chondromucosal flap and a
nasolabial groove skin flap based on the angular vessels may be
used together during a one-stage surgery.
In conclusion, angular artery is a good vascular
source for an island nasal chondromucosal flap. The flap is safe
and reliable. An island nasal chondromucosal flap and nasolabial
groove skin flap based on the angular vessels may be designed
simultaneously for use on full-thickness eyelid defects.
References
|
1.
|
Scuderi N, Ribuffo D and Chiummariello S:
Total and subtotal upper eyelid reconstruction with the nasal
chondromucosal flap: a 10-year experience. Plast Reconstr Surg.
115:1259–1265. 2005.PubMed/NCBI
|
|
2.
|
Scuderi N and Rubino C: The use of an
island chondromucosal flap in eyelid reconstruction: Preliminary
report. Plast Reconstr Surg. 92:1409–1410. 1993.PubMed/NCBI
|
|
3.
|
Scuderi N, Rubino C and Bertozzi E:
Clinical use of a new axial chondro-mucosal flap in wide
full-thickness eyelid reconstructions. Ophthalmic Surg Lasers.
30:91–97. 1999.PubMed/NCBI
|
|
4.
|
Scuderi N and Rubino C: Island
chondro-mucosal flap and skin graft: a new technique in eyelid
reconstruction. Br J Plast Surg. 47:57–59. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Mathijssen IM and van der Meulen JC:
Guidelines for reconstruction of the eyelids and canthal regions. J
Plast Reconstr Aesthet Surg. 63:1420–1433. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Pérez-Guisado J, de Haro-Padilla JM and
Rioja LF: Chondromucosal flap with the transposition flap of von
langenbeck as a good election for the total lower eyelid defect
reconstruction in an old patient with an elevated vision loss in
the contralateral eye. Eplasty. 11:e302011.
|
|
7.
|
Nigro MV, Friedhofer H, Natalino RJ and
Ferreira MC: Comparative analysis of the influence of perichondrium
on conjunctival epithelialization on conchal cartilage grafts in
eyelid reconstruction: experimental study in rabbits. Plast
Reconstr Surg. 123:55–63. 2009. View Article : Google Scholar
|
|
8.
|
Morley AM, deSousa JL, Selva D and
Malhotra R: Techniques of upper eyelid reconstruction. Surv
Ophthalmol. 55:256–271. 2010. View Article : Google Scholar
|
|
9.
|
Scuderi N, Ribuffo D, Onesti MG, et al:
Total and subtotal upper eyelid reconstruction with the nasal
chondromucosal flap. In: Abstracts of the 10th Congress of American
and Italian Plastic Surgeons, Ischia (NA). Rome. 1259–1265.
2002.
|
|
10.
|
Tellioglu AT, Tekdemir I, Saray A and Eker
E: Reconstruction of proximal nasal defects with island composite
nasal flaps. Plast Reconstr Surg. 115:416–422. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Fabrizio T, Savani A, Sanna M, Biazzi M
and Tunesi G: The retroangular flap for nasal reconstruction. Plast
Reconstr Surg. 97:431–435. 1996. View Article : Google Scholar
|
|
12.
|
Iida N, Ohsumi N and Tsutsumi Y: Use of
bilateral retroangular flaps for reconstruction of the glabella and
nose. Br J Plast Surg. 54:451–454. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Iida N, Ohsumi N, Tsutsumi Y and Tonegawa
M: The full-thickness retroangular flap. Ann Plast Surg.
45:544–549. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Seo YJ, Hwang C, Choi S and Oh SH: Midface
reconstruction with various flaps based on the angular artery. J
Oral Maxillofac Surg. 67:1226–1233. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Ascari-Raccagni A and Baldari U: The
retroangular flap used in the surgery of nasal tip defects.
Dermatol Surg. 30:1131–1137. 2004.PubMed/NCBI
|
|
16.
|
Mitz V, Ricbourg B and Lassau JP: The
branches of the facial artery in adults. Typology, variations and
respective cutaneous areas. Ann Chir Plast. 18:339–150. 1973.(in
French).
|
|
17.
|
Koh KS, Kim HJ, Oh CS and Chung IH:
Branching patterns and symmetry of the course of the facial artery
in Koreans. Int J Oral Maxillofac Surg. 32:414–418. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Niranjan NS: An anatomical study of the
facial artery. Ann Plast Surg. 21:14–22. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Loukas M, Hullett J, Louis RG Jr, Kapos T,
Knight J, Nagy R and Marycz D: A detailed observation of variations
of the facial artery, with emphasis on the superior labial artery.
Surg Radiol Anat. 28:316–324. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Nakajima H, Imanishi N and Aiso S: Facial
artery in the upper lip and nose: anatomy and a clinical
application. Plast Reconstr Surg. 109:855–861. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Pinar YA, Bilge O and Govsa F: Anatomic
study of the blood supply of perioral region. Clin Anat.
18:330–339. 2005. View
Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Standring S: Gray’s Anatomy: The
anatomical basis of clinical practice. 39th Edition. Churchill
Livingstone; Edinburgh: pp. 509pp. 567pp. 6962005
|
|
23.
|
Zhao Z, Li S, Xu J, et al: Color Doppler
flow imaging of the facial artery and vein. Plast Reconstr Surg.
106:1249–1253. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Erdogmus S and Govsa F: Arterial features
of inner canthus region: confirming the safety for the flap design.
J Craniofac Surg. 17:864–868. 2006. View Article : Google Scholar : PubMed/NCBI
|