Introduction
Chronic kidney disease is a worldwide public health
problem (1,2) and the number of patients with
end-stage renal disease is increasing steadily (3). Chronic kidney disease leads to huge
health and socio-economic problems. Primary (4,5) and
secondary glomerular diseases, including diabetic nephropathy
(6,7), are the major causes of end-stage
renal disease worldwide. Therefore, the early detection and
prevention of glomerular diseases may reduce their global burden.
Thus, it is imperative to investigate the pathogenesis of
glomerular diseases (8–11).
There are multiple autoimmune strains of mice with
glomerulonephritis and mice are also commonly used to create models
of diabetes, which develop renal injury similar to human diabetic
nephropathy (12). These models
are suitable for exploring the mechanisms that lead to kidney
disease. However, since the diameters of mouse glomeruli are
relatively similar to those of the tubules, it is difficult to
isolate pure glomeruli with sieving, as is possible for other
animals, including rats (13) and
rabbits (14).
Currently, the separation methods available for
isolating mouse glomeruli include laser capture microdissection,
differential sieving and Dynabead perfusion. Laser capture
microdissection has the advantage of high precision; however, the
amount of glomeruli obtained is relatively low. Furthermore, with
differential sieving it is difficult to isolate mouse glomeruli
with high purity. At present, Dynabead perfusion is the only method
for separating glomeruli in mice that yields high purity and large
amounts; however, the only drawback of this method is that it is
expensive (15).
In the present study, glomeruli were isolated from
mice via Dynabead perfusion of the kidney and they were of high
quality and were isolated at a lower cost. In this study, the
course and basic steps are explained, and a practical step-by-step
procedure is provided, for isolating mouse glomeruli with
Dynabeads. The aim is to aid researchers in the practical
application of this methodology in their studies.
Materials and methods
Animals
C57BL6 mice, aged 8 weeks, were purchased from the
Laboratory Animal Center, China Medical University (Shenyang,
China). Mice were housed in plastic cages with free access to food
and tap water throughout the experimental period. All mice were
maintained in a temperature- and humidity- controlled room (23±3°C;
humidity, 50±20%) in the China Medical University, Laboratory
Animal Center SPF rodent housing facility with a regular 12 h
light/dark cycle, according to the guidelines of the Chinese
National Standard (GB 14925-2001). All experiments were approved by
a local committee for ethics in animal research.
Reagents
Collagenase A (product no. 10103578001) was
purchased from Roche Diagnostics GmbH (Mannheim, Germany). The 2-D
Clean-Up kit and Ettan™ 2-D Quant kit were purchased from GE
Healthcare Life Sciences (Piscataway, NJ, USA). Dynabeads M-450
Tosylactivated (diameter 4.5 μm; product no. 140.13) and a
magnetic particle concentrator (product no. 123.21D) were purchased
from Dynal AS (Oslo, Norway). Cell strainers (100 μm;
product no. 352360) were purchased from BD Biosciences (Franklin
Lakes, NJ, USA).
Isolation of glomeruli
Mice were anesthetized with 10% chloral hydrate
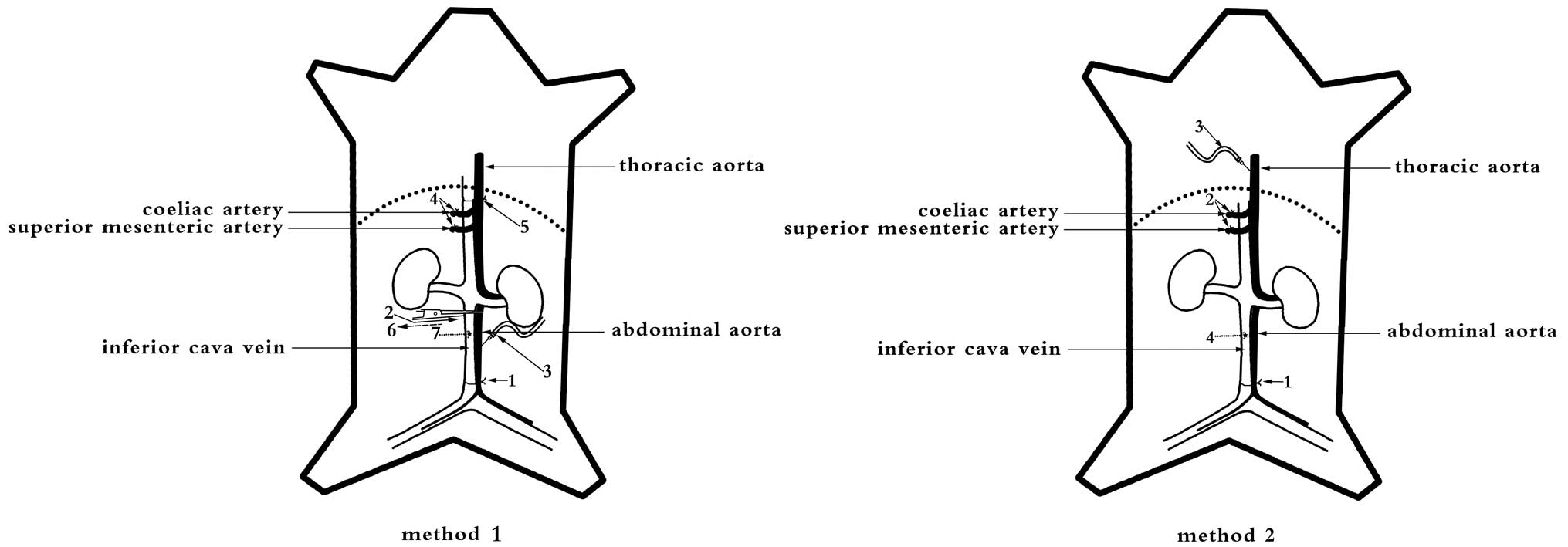
(0.03 ml/10 g). The kidneys were perfused via two methods (Fig. 1). Method 1 was performed as
follows: i) the distal abdominal aorta and distal inferior cava
vein were ligated; ii) the abdominal aorta and inferior cava vein
were clipped with vessel clamps below the renal artery and vein;
iii) polyethylene tubing (internal diameter, 0.3 mm) was inserted
into the middle of the abdominal aorta and fixed in place; iv) the
superior mesenteric and coeliac arteries were ligated; v) the
proximal abdominal aorta was ligated above the renal artery; vi)
the vessel clamp was removed; vii) a hole was cut in the inferior
cava vein to ensure venous drainage; and viii) the kidney was
perfused with ice-cold sterile phosphate-buffered saline (PBS)
through the polyethylene tubing at a constant flow rate of 8.2
ml/min/g kidney to clean the blood vessels of any remaining blood.
Method 2 was performed as follows: i) the distal abdominal aorta
and distal inferior cava vein were ligated; ii) the superior
mesenteric and coeliac arteries were ligated; iii) venous retention
needles (24 gauge; BD Biosciences) were inserted into the thoracic
aorta and fixed into place; iv) a hole was cut in the inferior cava
vein to ensure venous drainage; and v) the kidney was perfused with
ice-cold sterile PBS via the venous retention needles at a constant
flow rate of 8.2 ml/min/g kidney to clean the blood vessels of any
remaining blood.
Following the above mentioned surgical procedures,
the kidneys were perfused with Dynabeads. Briefly, Dynabeads were
washed prior to use, according to the manufacturer’s instructions.
Then, 20 ml Dynabeads at a concentration of 4×106
beads/ml PBS were injected into the kidneys at a constant flow rate
of 7.4 ml/min/g kidney. Following perfusion, kidneys were removed,
minced into small pieces and digested with collagenase A (1 mg/ml)
at 37°C for 30–40 min with gentle agitation. The digested tissue
was then gently pressed through a 100 μm cell strainer,
followed by intermittent ice-cold sterile PBS flushing. The cell
suspension was centrifuged at 200 × g at 4°C for 5 min. The
supernatant was discarded and the pellet was dissolved in 2 ml PBS,
which was transferred into a 2 ml tube. Glomeruli that contained
Dynabeads were isolated by a magnetic particle concentrator and
washed at least three times with ice-cold sterile PBS. The entire
procedure was performed on ice with the exception of the
collagenase digestion. Lastly, the extracted glomeruli were lysed
in 2-DE lysis buffer [7 M urea, 2 M thiourea, 4% CHAPS, 2% IPG
buffer and 40 mM dithiothreitol (DTT)] and sonicated (30 Hz, 4×5
sec pulses on ice). The lysates were then centrifuged at 12,500 × g
at 4°C for 10 min to remove the Dynabeads.
Measurement of the protein
concentration
Protein from glomeruli was purified using the 2-D
Clean-Up kit and the protein concentration was determined using the
Ettan™ 2-D Quant kit. All samples were stored at −70°C.
Assessing the isolation of glomeruli
Glomeruli containing Dynabeads were diluted with
ice-cold PBS to yield 1 ml and then mixed. Then, 10 μl
diluted glomeruli were transferred onto slides with a micropipette
and the number of glomeruli and renal tubules were determined by
two investigators on an inverted microscope (4× objective lens and
10× ocular lens; Nikon TS100, Tokyo, Japan). The investigators
repeated this procedure four separate times and obtained images
with a universal microscope (Nikon 80i). Following Dynabead
perfusion, the kidneys were fixed with 4% paraformaldehyde,
embedded in paraffin, sectioned into 2-μm thick slices,
stained with hematoxylin and eosin (H&E) and photographic
images were captured under a universal microscope. Renal cortices
were rapidly fixed in 2.5% glutaraldehyde, subjected to
ferrocyanide-reduced OsO4 treatment and dehydrated.
Then, plastic infiltration and ultrathin sectioning was performed
and the sections were observed and photographed under a
transmission electron microscope (EM; JEOL 1200EX). Separated
glomeruli containing Dynabeads were fixed in 2.5% glutaraldehyde,
osmicated according to the OTOTO protocol (16), dried with hexamethyldisilazane
evaporation and photographed under a scanning EM (JEOL T300).
Statistical analyses
Data are presented as the mean ± standard error of
the mean (SEM). P<0.05 was considered to indicate a
statistically significant difference. Data were analyzed with SPSS
software 15.0 (SPSS Inc., Chicago, IL, USA).
Results
Success rate of isolating glomeruli from
mice
Kidney perfusions and all steps involved in the
isolation of glomeruli in mice were completed with a success rate
of 100%.
Light microscopy
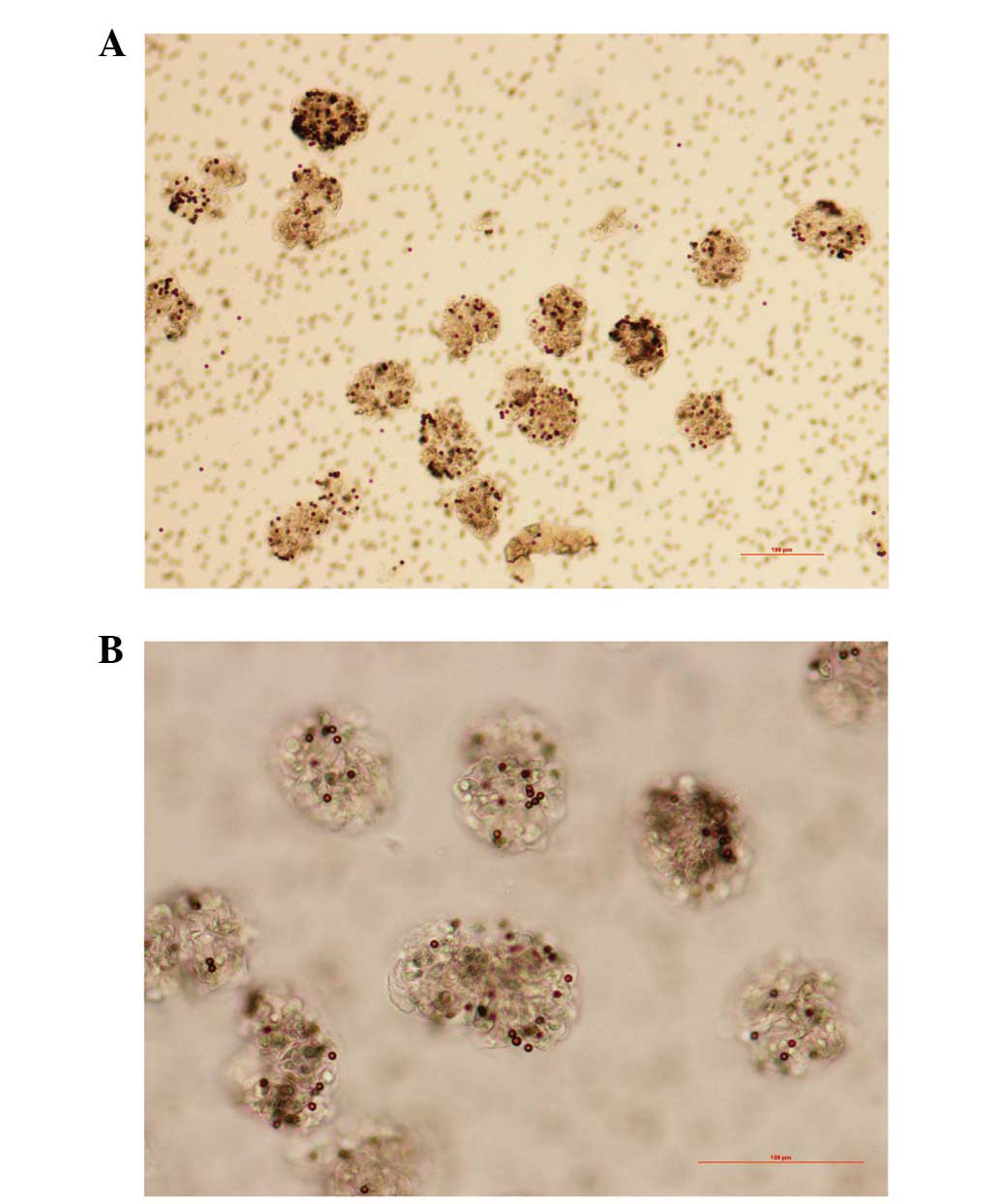
Under a light microscope, the isolated glomeruli
occupied the entire visual field (Fig.
2). A few glomeruli had part of the afferent and/or efferent
arterioles attached and only a few renal tubules were identified
with light microscopy. The number of glomeruli was estimated to be
9,960±1,575 at 8 weeks of age and 14,230±2,851 at 20 weeks of age
and the purity was estimated to be 96.67±1.16%.
H&E staining
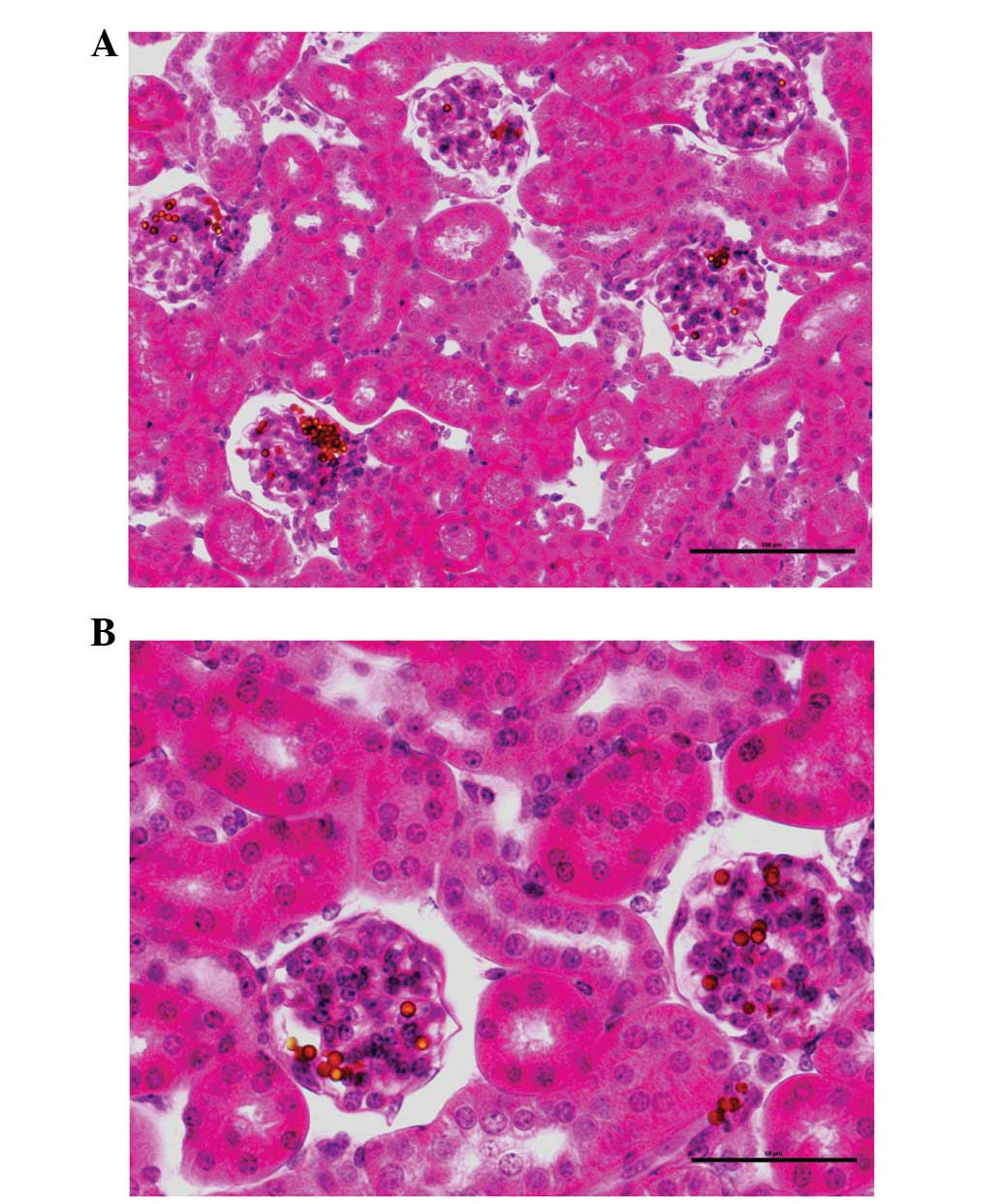
Dynabeads were identified in almost all the
glomeruli (Fig. 3) and only a few
beads were present in the surrounding renal tissues, which were
primarily the afferent and/or efferent arterioles.
Electron microscopy
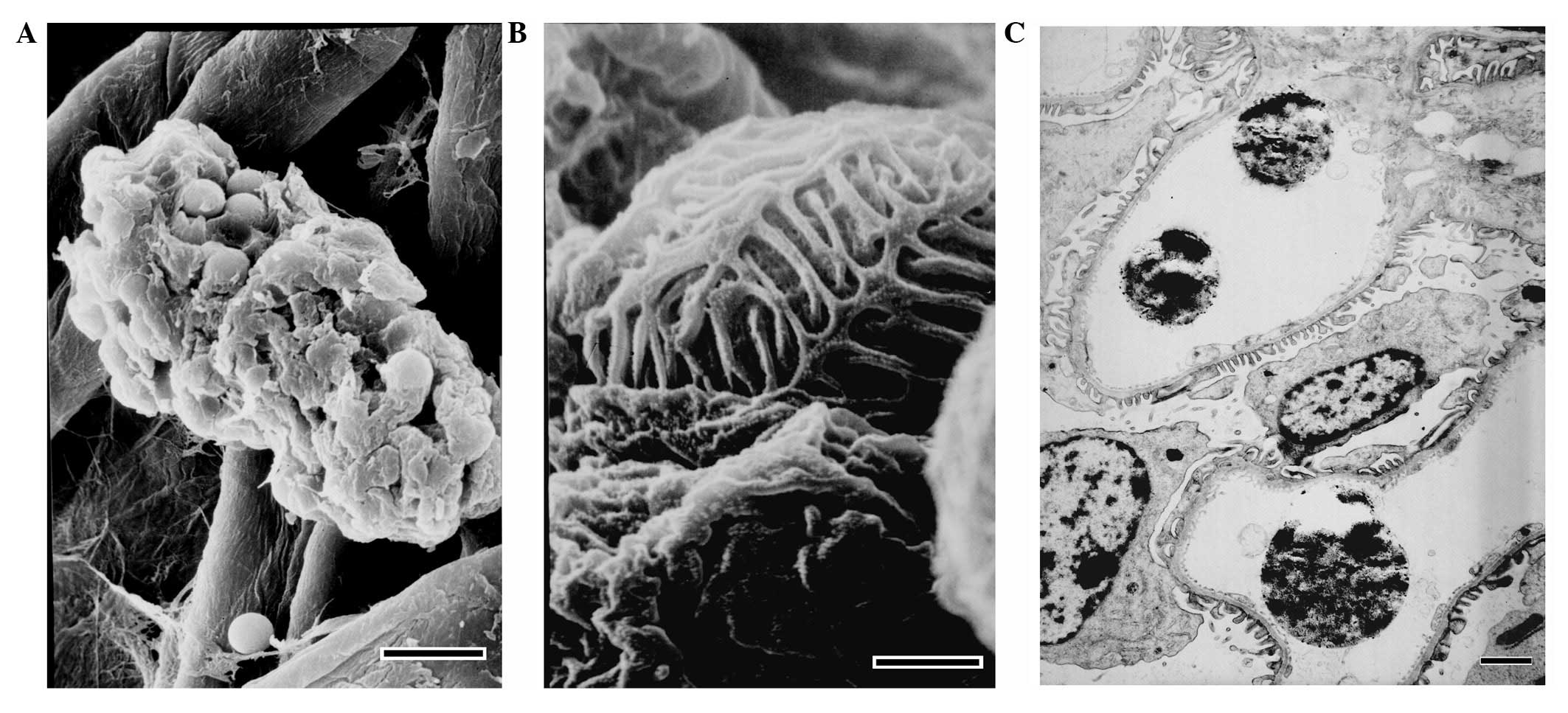
Under a scanning EM, closed glomeruli were observed
and the structural integrity of the isolated glomeruli was intact.
Under a transmission EM, it was identified that Dynabead particles
occupied the capillaries, the foot processes of podocytes were in
contact with the glomerular basement membrane and the glomeruli
structures were intact (Fig.
4).
Amount of glomerular protein
Twenty mice, 10 mice aged 8 weeks and 10 mice aged
20 weeks, were perfused with Dynabeads. The average amount of
protein obtained from the isolated glomeruli of one mouse (from the
two kidneys) was 45.6±13.4 μg at 8 weeks of age and
55.8±17.0 μg at 20 weeks of age.
Effects of different doses of
Dynabeads
Ten mice (20 weeks of age) were perfused with either
20 or 30 ml Dynabeads at a concentration of 4×106
beads/ml PBS. There were no significant differences in the average
amount of protein obtained from the isolated glomeruli of mice
perfused with either 20 or 30 ml Dynabeads (55.8±17.0 vs. 53.7±15.4
μg; P>0.05).
Ten mice (8 weeks of age) were perfused with either
10 or 20 ml Dynabeads at a concentration of 4×106
beads/ml PBS. The average amount of protein obtained from isolated
glomeruli from mice perfused with 20 ml Dynabeads was markedly
higher compared with that obtained from isolated glomeruli of mice
perfused with 10 ml Dynabeads (45.6±13.6 vs. 21.9±6.15 μg;
P<0.001).
Differences in the amount of Dynabeads
used following heart and kidney perfusion
The amount of Dynabeads used in the kidney
perfusions was one-fortieth of that used in heart perfusions
(Table I).
 | Table IAmount of Dynabeads used with either
heart or kidney perfusion. |
Table I
Amount of Dynabeads used with either
heart or kidney perfusion.
| Perfusion method | Operational
concentration (beads/ml) | Volume/mouse | Number of Dynabead
bottles usedb |
|---|
| Hearta | 8×107 | 40 ml | 1.6 |
| Kidney | 4×106 | 20 ml | 0.04 |
Discussion
Proteins are the ultimate indicators of biological
function. Proteomics has been extensively applied in various fields
of medicine, including nephrology (16–20).
The application of renal proteomics is likely to aid researchers in
gaining an improved understanding of renal pathophysiology and
discovering new therapeutic targets. However, the main limitation
of glomerular proteomics is obtaining an adequate amount of
glomeruli from mice that is also high in purity.
Due to this limitation, current proteomic studies
focus on investigating blood and urine proteomics, as well as
podocyte and mesangial cell proteomics, which are based on cell
culture (21,22). However, the glomerulus is a
functional unit with an interconnected organizational structure,
coordinated physiological functions and potential interacting
pathological changes. Tissues and cells growing in an artificial
culture differ greatly from those grown in their original
environment and as a result, glomerular proteomics are fundamental.
Thus, proteomics at all levels require comprehensive analysis in
order to determine the important factors involved and/or correlated
with various glomerular diseases. Consequently, it is necessary to
develop a practical method for preparing an adequate amount of pure
glomeruli, to allow researchers to engage in proteomic research
exploring the pathogenesis of glomerular diseases.
In the present study, mouse glomeruli were separated
via Dynabead perfusion with a success rate of 100%. The structures
of the isolated glomeruli remained intact and the purity was high,
while the cost was reduced. The cost of the procedure when the
kidneys are perfused, as described in the present study, is
one-fortieth of the cost when the heart is perfused, as described
by Takemoto et al(15). It
should be noted that the superior mesenteric and coeliac arteries,
which supply blood to the intestines and liver, were ligated to
ensure that all the Dynabeads directly entered the kidney. The
modification of this step significantly reduced the amount of
Dynabeads necessary and consequently reduced the cost. Moreover,
the superior mesenteric and coeliac arteries are simple to identify
and this modification was easily accomplished. Furthermore, it was
identified that even though the number of glomeruli was lower in
the 8-week-old mice than in 20-week-old mice, the same amount of
Dynabeads was required for perfusion to produce good results.
Kidney perfusion experiments are routinely conducted
by researchers studying kidney disease. Since the bore and
elasticity of arteries differ and depend on the strain, age or
state of the experimental animal, it is difficult for beginners to
conduct the surgical procedures involved in such kidney perfusion
experiments, particularly when laboratory mice are expensive and a
high success rate is required.
Perfusion through the abdominal aorta is common. In
the current study, the distal abdominal aorta and inferior cava
vein were ligated, and the abdominal aorta and inferior cava vein
were temporarily clipped below the renal artery and vein, in order
to prevent mice from hemorrhaging during the procedure.
In young mice, the abdominal aorta is thin and it is
difficult to insert catheters with a high success rate,
particularly for inexperienced researchers. In certain disease
models, including KK/Ta mice (23), which are a model of type 2 diabetic
nephropathy, the state of the abdominal aorta is poor and the
vessel is easily damaged when inserting a catheter. In the present
study, the catheter was inserted into the thoracic aorta, which is
thicker and easier to handle. Attempts to perfuse the kidneys via
the thoracic aorta in mice of different strains and ages were made
and a 100% success rate was achieved, even when the perfusion was
performed by beginners.
The purity of the isolated glomeruli obtained in the
present study was high and consistent with the results of other
studies (15,24). The step of isolating glomeruli
containing Dynabeads with a magnetic particle concentrator is
important for attaining a high purity. Thus, researchers need to
ensure that they wash glomeruli at least three times with ice-cold
sterile PBS. However, in the present study, the amounts of protein
and the numbers of isolated glomeruli were lower than those
reported previously (15,24). Subsequent experiments revealed that
collagenase A digestion is necessary to detach the glomeruli from
their surrounding tissues, otherwise a large amount of glomeruli in
undigested tissues would be removed by the cell strainer.
Furthermore, in another experiment, the time of collagenase A
digestion was prolonged, which increased the amount of protein and
the number of glomeruli isolated. Simultaneously, glomerular RNA
was also obtained (data not shown).
In conclusion, a useful method for isolating
glomeruli from mice in large amounts and with a high purity is
presented. The modified procedure is likely to reduce the
difficulty in performing the procedure, as well as the cost.
Consequently, the modified methodology provides researchers with an
opportunity to perform proteomic studies on glomerular
diseases.
Acknowledgements
This study was supported by the
National Natural Science Fund of China (30700369). The authors
thank Weifan Yao, Shuyan Du and Dongjuan Liu for their skillful
technical support.
References
|
1.
|
Garcia-Garcia G, Marquez-Magaña I,
Renoirte-Lopez K, et al: Screening for kidney disease on World
Kidney Day in Jalisco, Mexico. J Nephrol. 23:224–230.
2010.PubMed/NCBI
|
|
2.
|
Prodjosudjadi W, Suhardjono, Suwitra K, et
al: Detection and prevention of chronic kidney disease in
Indonesia: initial community screening. Nephrology (Carlton).
14:669–674. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
El Nahas M: The global challenge of
chronic kidney disease. Kidney Int. 68:2918–2929. 2005.
|
|
4.
|
Singh GR: Glomerulonephritis and managing
the risks of chronic renal disease. Pediatr Clin North Am.
56:1363–1382. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Glassock RJ: Glomerular disease in the
elderly. Clin Geriatr Med. 25:413–422. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Atkins RC and Zimmet P: Diabetic kidney
disease: act now or pay later. J Nephrol. 23:1–4. 2010.PubMed/NCBI
|
|
7.
|
Iseki K: Metabolic syndrome and chronic
kidney disease: a Japanese perspective on a worldwide problem. J
Nephrol. 21:305–312. 2008.PubMed/NCBI
|
|
8.
|
Remuzzi G, Benigni A and Remuzzi A:
Mechanisms of progression and regression of renal lesions of
chronic nephropathies and diabetes. J Clin Invest. 116:288–296.
2006. View
Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Martini S, Eichinger F, Nair V and
Kretzler M: Defining human diabetic nephropathy on the molecular
level: integration of transcriptomic profiles with biological
knowledge. Rev Endocr Metab Disord. 9:267–274. 2008. View Article : Google Scholar
|
|
10.
|
Piccoli GB, Bonino LD, Campisi P, et al:
Chronic kidney disease, severe arterial and arteriolar sclerosis
and kidney neoplasia: on the spectrum of kidney involvement in
MELAS syndrome. BMC Nephrol. 13:92012. View Article : Google Scholar
|
|
11.
|
Qu Z, Liu G, Li J, et al: Absence of
glomerular IgG4 deposition in patients with membranous nephropathy
may indicate malignancy. Nephrol Dial Transplant. 27:1931–1937.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Tesch GH and Allen TJ: Rodent models of
streptozotocin-induced diabetic nephropathy. Nephrology (Carlton).
12:261–266. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Kreisberg JI, Hoover RL and Karnovsky MJ:
Isolation and characterization of rat glomerular epithelial cells
in vitro. Kidney Int. 14:21–30. 1978. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Downer G, Phan SH and Wiggins RC: Analysis
of renal fibrosis in a rabbit model of crescentic nephritis. J Clin
Invest. 82:998–1006. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Takemoto M, Asker N, Gerhardt H, et al: A
new method for large scale isolation of kidney glomeruli from mice.
Am J Pathol. 161:799–805. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Friedman PL and Ellisman MH: Enhanced
visualization of peripheral nerve and sensory receptors in the
scanning electron microscope using cryofracture and
osmium-thiocarbohydrazide-osmium impregnation. J Neurocytol.
10:111–131. 1981. View Article : Google Scholar
|
|
17.
|
Rossing K, Mischak H, Dakna M, et al:
Urinary proteomics in diabetes and CKD. J Am Soc Nephrol.
19:1283–1290. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Hoorn EJ, Pisitkun T, Zietse R, et al:
Prospects for urinary proteomics: exosomes as a source of urinary
biomarkers. Nephrology (Carlton). 10:283–290. 2005.PubMed/NCBI
|
|
19.
|
Thongboonkerd V and Malasit P: Renal and
urinary proteomics: Current applications and challenges.
Proteomics. 5:1033–1042. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Niwa T: Biomarker discovery for kidney
diseases by mass spectrometry. J Chromatogr B Analyt Technol Biomed
Life Sci. 870:148–153. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Tilton RG, Haidacher SJ, Lejeune WS, et
al: Diabetes-induced changes in the renal cortical proteome
assessed with two-dimensional gel electrophoresis and mass
spectrometry. Proteomics. 7:1729–1742. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Schordan S, Schordan E, Endlich N, et al:
Alterations of the podocyte proteome in response to high glucose
concentrations. Proteomics. 9:4519–4528. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Li Z, Zhang H, Dong X, et al: Proteomic
profile of primary isolated rat mesangial cells in high-glucose
culture condition and decreased expression of PSMA6 in renal cortex
of diabetic rats. Biochem Cell Biol. 88:635–648. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Liao J, Kobayashi M, Kanamuru Y, et al:
Effects of candesartan, an angiotensin II type 1 receptor blocker,
on diabetic nephropathy in KK/Ta mice. J Nephrol. 16:841–849.
2003.PubMed/NCBI
|
|
25.
|
Bonvalet JP, Champion M, Courtalon A, et
al: Number of glomeruli in normal and hypertrophied kidneys of mice
and guinea-pigs. J Physiol. 269:627–641. 1977. View Article : Google Scholar : PubMed/NCBI
|