Introduction
Hydroxylapatite (HAP)/collagen (Col) composites have
often been utilized as bone substitute materials in dentistry and
orthopedic surgery for the regeneration of damaged hard tissue
(1). HAP has the capability of
excellent osteoconduction and slow biodegradation (2), while Col is the bio-absorbable
scaffold used to bind HAP (3).
Different sizes of HAP can be used in HAP/Col composites (4,5).
Nano-HAP (n-HAP) particles have attracted attention
in the field of biomaterials, as they are considered to have
unknown advantageous capabilities (4,6).
It is, however, necessary to mix n-HAP with Col to form a bone
substitute material (6).
Macro-pore sized HAP (m-HAP) is now solely employed as particulate
bone substitute material (5,7),
and can also be mixed with Col for new biomaterial. However, few
systematic studies have evaluated the osteoconductive capability of
n-HAP/Col and m-HAP/Col composites (4).
To achieve osteoregeneration following the
implantation of HAP/Col composites in the bone defect area, it is
required that osteoblasts adhere to and differentiate into a final
matured stage in contact with HAP/Col composites (8). It is known that osteoblasts
differentiate following a characteristic step-wise sequence, while
secreting respective phenotype marker enzymes/proteins in
multi-lineage differentiation [i.e., early-stage alkaline
phosphatase (ALP) and type 1 collagen (COL1); and
middle-to-late-stage bone sialoprotein (BSP) and the osteocalcin
precursor, bone gamma-carboxyglutamate (gla) protein (BGLAP)]
(9). Reverse transcription PCR
(RT-PCR) is a sophisticated technique which can be used to evaluate
the expression of genes (mRNAs) which produce marker
enzyme/proteins in osteoblasts cultured on implant materials
(10–12).
The aim of the current study was, therefore, to
evaluate the expression of four selected osteogenic
differentiation-related genes (i.e., ALP, COL1, BSP and BGLAP) in
osteoblast-like cells (SaOS-2) cultured on Col, n-HAP/Col and
m-HAP/Col composites, using a world class standard RT-PCR machine
in order to determine the effects of two HAP/Col composites
containing different HAP particle sizes (i.e., n-HAP/Col and
m-HAP/Col) on the osteogenic differentiation of osteoblasts.
Furthermore, SaOS-2 cells cultured on three test materials were
observed under a scanning electron microscope (SEM) in order to
osberved the cellular morphological changes that occurred during
the osteogenic differentiation of the SaOS-2 cells.
Materials and methods
HAP particles
The n-HAP particles used were mono-dispersed HAP
ceramics with an average diameter of 40 nm (MHS-00405 type
nano-SHAp; SofSera Corp., Tokyo, Japan), as previously described
(13). The m-HAP particles used
were novel interconnected porous HAP ceramics with a large
dimension of 0.5–1 mm (DK03-001, IP-CHA; Covalent Materials Co.,
Tokyo, Japan), as previously described (5). Both HAP particles were of high
purity, fired at >800°C and highly crystalline, as previously
described (5,13). The basic intrinsic difference
between the n-HAP and m-HAP particles lied in their size.
Preparation of HAP/Col composites
Collagen pellets produced from porcine skin (NMP
Collagen PS; Nippon Meat Packers Inc., Tokyo, Japan) (1 g) were
dissolved in distilled water (28 ml) in a 50 ml polystyrene conical
tube at 4°C. The formed acidic solution was neutralized by 0.1 N
NaOH solution (6.5 ml) in a disposable rectangular plastic plate
(100×70×12 mm) in order to obtain a collagen gel of pH 7.5. The
n-HAP or m-HAP powder (1.5 g) was then manually mixed with collagen
gel using a plastic spatula. The HAP/Col composite gel was then
frozen at −80°C for 3 h, and freeze-dried using a freeze-drier
(FD-5N; Eyela, Tokyo, Japan) for 12 h. The formed composite sponge
stored in a holed stainless steel case was subsequently
cross-linked by dehydrothermal treatment at 140°C for 24 h in a
vacuum drying oven (VO-300; Asone, Osaka, Japan). From the
composite sponge sheet, discs 6 mm in diameter and 1 mm thickness
were punched out with a hole puncher. Discs stored in exclusive
pouches were sterilized by ethylene oxide gas and kept in a
vacuumed desiccator before the cell culture experiments.
Culture of SaOS-2 cells on HAP/Col
composites
Human osteoblast-like cells (SaOS-2) (RCB0428; Riken
BioResource Center Cell Bank, Tsukuba, Japan) were regularly
cultured in Eagle’s α-modified minimum essential medium
(Invitrogen, Carlsbad, CA, USA) supplemented with 10% fetal bovine
serum (Cat. no. 10099-141; Invitrogen) and 2% antibiotics
(penicillin-streptomycin-amphotericin; Cat. no. 5240-096;
Invitrogen) in a 5% CO2 incubator at 37°C. After
subconfluence, the cells were collected by trypsinization with
phosphate-buffered saline [PBS(−)] containing 0.08% trypsin (Cat.
no. 15090-046; Invitrogen) and 0.14% EDTA (Cat. no. 15576-010;
Invitrogen) and subcultured at 1:3 ratios.
The culture of SaOS-2 cells on the Col, n-HAP/Col
and m-HAP/Col specimens was carried out as follows: The SaOS-2
cells (1×104) in 200 μl medium were inoculated on three
test materials held in wells of a 96-well polystyrene culture dish.
The SaOS-2 cells on the test materials were then continuously
cultured for 1, 2, 3 and 4 weeks in a 5% CO2 incubator
at 37°C, while the medium was changed twice each week.
Selection of osteogenic
differentiation-related genes
As osteogenic differentiation-related phenotype
markers, five genes were selected, including the β-actin gene,
which was used as the control. The ALP and COL1 genes, and the BSP
and BGLAP genes were used as early-stage and middle-to-late stage
osteogenic differentiation phenotype markers, respectively
(11). The formal nomenclatures
and GenBank accession numbers (in the genetic sequence database,
National Institutes of Health, Bethesda, MD, USA) (NM_) of the five
genes were as follows: β-actin, Homo sapiens actin, beta
(ACTB), mRNA, NM_001101.3; ALP, Homo sapiens alkaline
phosphatase, liver/bone/kidney, transcript variant 1, mRNA,
NM_000478.3; COL1, Homo sapiens collagen, type I, α1 mRNA,
NM_000088.3; BSP, Homo sapiens integrin-binding
sialoprotein, mRNA, NM_004967.3; and BGLAP, bone
gamma-carboxyglutamate (Gla) protein (osteocalcin precursor),
NM_199173.
RT-PCR
Total RNA was extracted from the cells using ISOGEN
reagent (Nippon Gene, Tokyo, Japan). Reverse transcription was
performed using the PrimeScript RT reagent kit (Takara Bio., Inc.,
Ohtsu, Japan). The mRNA expression levels of the five genes were
determined by RT-PCR using SYBR Premix Ex Taq II (Takara
Bio, Inc.) and the Thermal Cycler Dice Real Time System TP8000
(Takara Bio, Inc.) and five primers (Table I) designed by the Perfect Real
Time support system (Takara Bio, Inc.). The primer set for BGLAP
was specifically created upon our request, while those for the
other four genes were ready-made in the support system (Takara Bio,
Inc.). For each test run, cDNA derived from 50 ng total RNA was
used. After an initial denaturation at 95°C for 30 sec, a two-step
cycle procedure was used (denaturation at 95°C for 5 sec, annealing
and extension at 60°C for 30 sec) for 40 cycles. Gene expression
levels were normalized according to the expression level of the
β-actin gene. Relative amounts (RQ values) of each mRNA in each
sample were calculated using the ΔΔCt method. The gene expression
analyses were duplicated. To ensure reproducibility, each sample
was analyzed in triplicate. Data are presented as the means ±
standard deviation.
 | Table IPrimers of the five genes used for
RT-PCR. |
Table I
Primers of the five genes used for
RT-PCR.
| Genes | Sequences |
|---|
| β-actin | F:
TGGCACCCAGCACAATGAA
R: CTAAGTCATAGTCCGCCTAGAAGCA |
| ALP | F:
GGACCATTCCCACGTCTTCAC
R: CCTTGTAGCCAGGCCCATTG |
| COL1 | F:
TCTAGACATGTTCAGCTTTGTGGAC
R: TCTGTACGCAGGTGATTGGTG |
| BSP | F:
GGCCACGATTTATCTTTACAAGCA
R: TCACCCTCAGAGTCTTCATCTTCA |
| BGLAP | F:
AGGTGCAGCCTTTGTGTCCA
R: GGCTCCCAGCCATTGATACAG |
Statistical analysis
Statistical analysis was carried out using the
Student’s t-test and a value of α=0.05 was considered to indicate a
statistically significant difference.
Observations of SaOS-2 cells cultured on
HAP/Col composites with SEM
SaOS-2 cells cultured on Col, n-HAP/Col and
m-HAP/Col specimens for 1 and 4 weeks were freeze-dried at room
temperature for 1 h, following fixation in 2.5% glutaraldehyde
solution, fixation in 1% osmium solution, dehydration in graded
alcohols, infiltration by t-butyl alcohol and freezing at 0°C for
12 h. The cells cultured on the three test materials were then
observed under an SEM (S-2300; Hitachi, Ibaragi, Japan).
Results
RT-PCR
Early-stage osteogenic differentiation
marker genes (ALP and COL1)
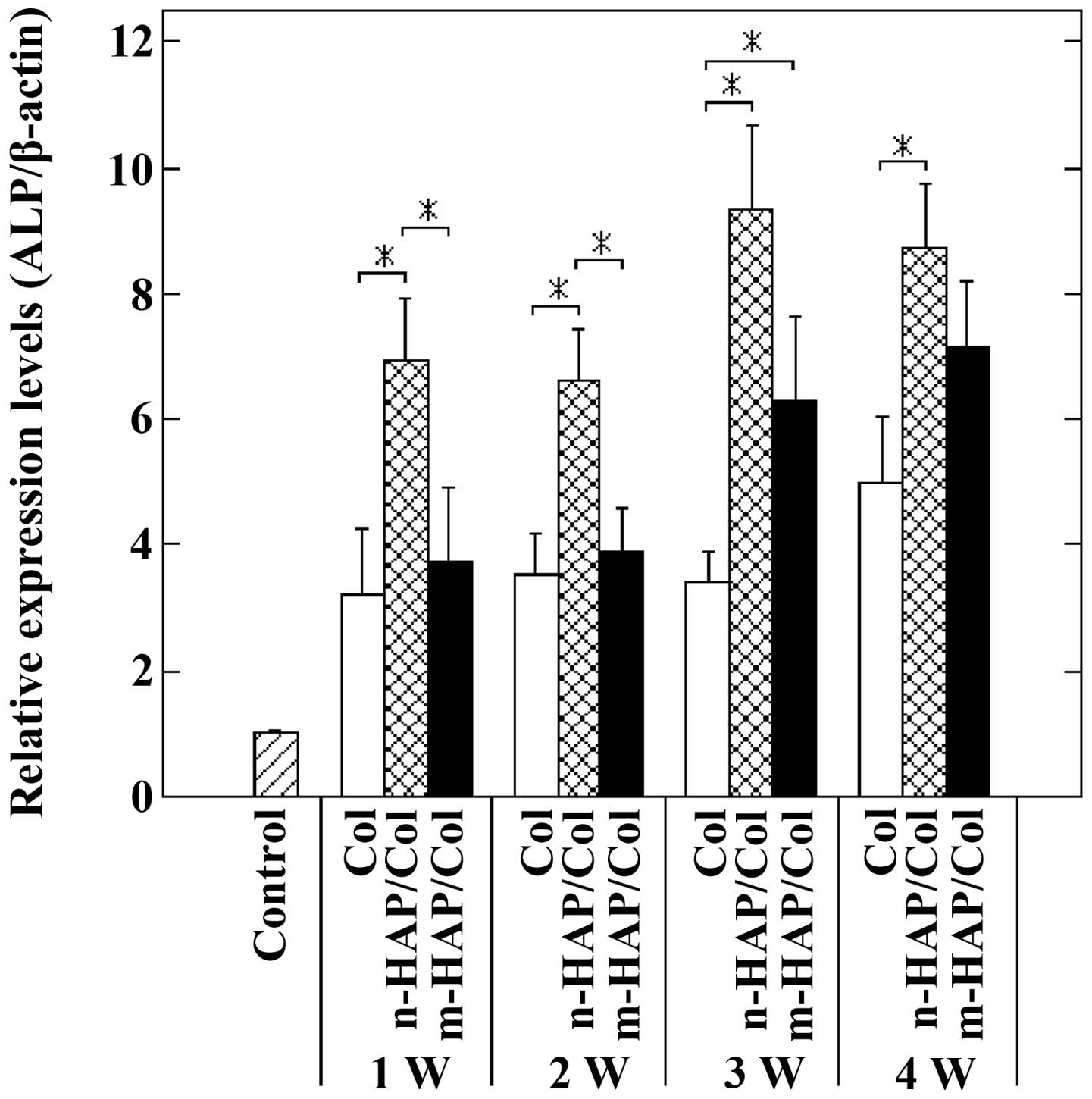
The expression of the ALP gene clearly distinguished
the early-stage osteogenic differentiation of the SaOS-2 cells
cultured on the three test materials. The n-HAP particles in the
n-HAP/Col composite rapidly (from 1 week) and continuously (over a
period of 4 weeks) accelerated early-stage osteogenic
differentiation characterized by the expression of the ALP gene,
compared with the m-HAP particles in the m-HAP/Col composite and
Col (Fig. 1).
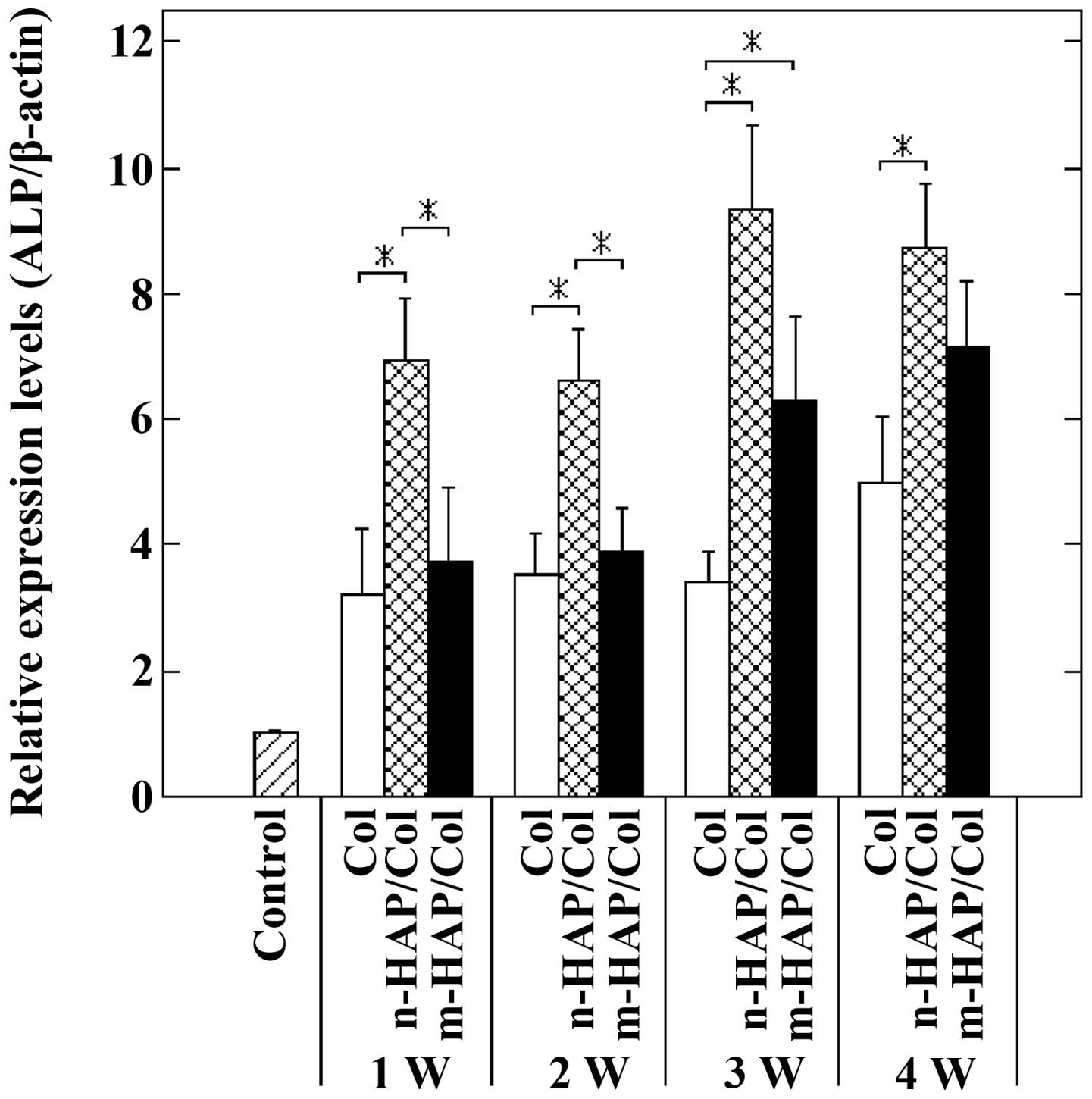 | Figure 1Expression of the alkaline phosphatase
(ALP) gene in osteoblast-like cells (SaOS-2) cells cultured on
collagen (Col), nano-sized hydroxylapatite (nHAP)/Col and
macro-pore sized hydroxylapatite (m-HAP)/Col composites for 1, 2, 3
and 4 weeks (*p<0.05). The expression levels of the
ALP gene in the SaOS-2 cells cultured on Col were greater than
those of the control, but remained quasi-constant for up to 4
weeks. At 1 and 2 weeks, culture on n-HAP/Col markedly upregulated
the expression of the ALP gene in the SaOS-2 cells compared with
culture on Col and m-HAP/Col (p<0.05), and the expression levels
of the ALP gene in the cells cultured on m-HAP/Col and Col were
similarly lower. Thus, n-HAP/Col solely had the ability to rapidly
induce early-stage osteogenic differentiation characterized by the
expression of the ALP gene. At 3 and 4 weeks, the expression of the
ALP gene in the cells cultured on n-HAP/Col tended to still be
higher, followed by m-HAP/Col, while cells cultured on Col tended
to have the weakest expression of ALP. These results demonstrate
that n-HAP/Col has the ability to induce the early-stage osteogenic
differentiation of SaOS-2 cells at 3 and 4 weeks, whilst the
osteogenic differentiation of cells cultured on m-HAP/Col virtually
only began at 3 weeks. W, week. |
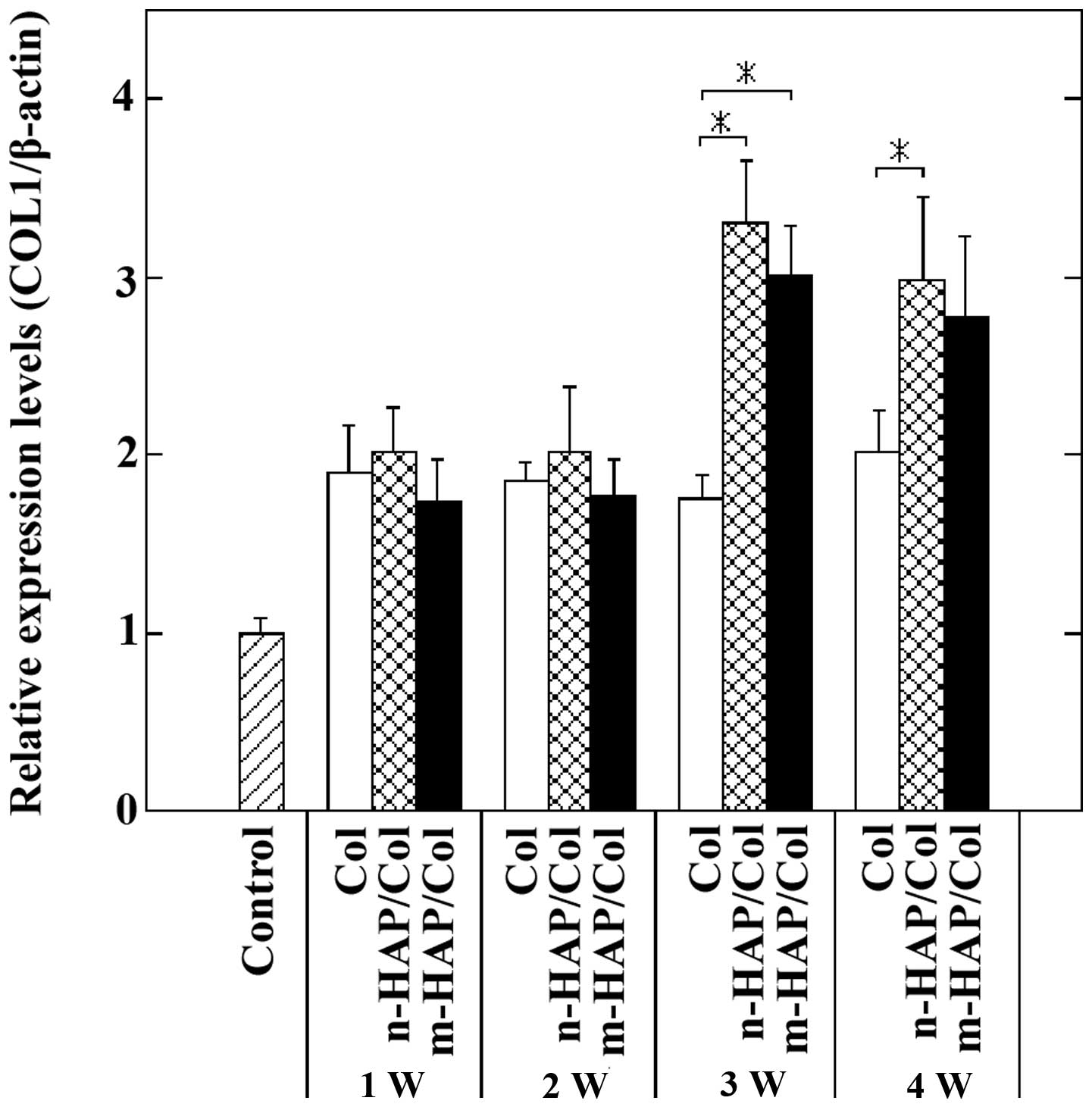
On the other hand, at 1 and 2 weeks, the expression
of the COL1 gene did not clearly display the difference in the
osteogenic differentiation of the cells cultured on the three test
materials. At 3 and 4 weeks, however, the SaOS-2 cells cultured on
the n-HAP/Col and m-HAP/Col specimens were larger than those
cultured on Col specimens with similar magnitude (Fig. 2).
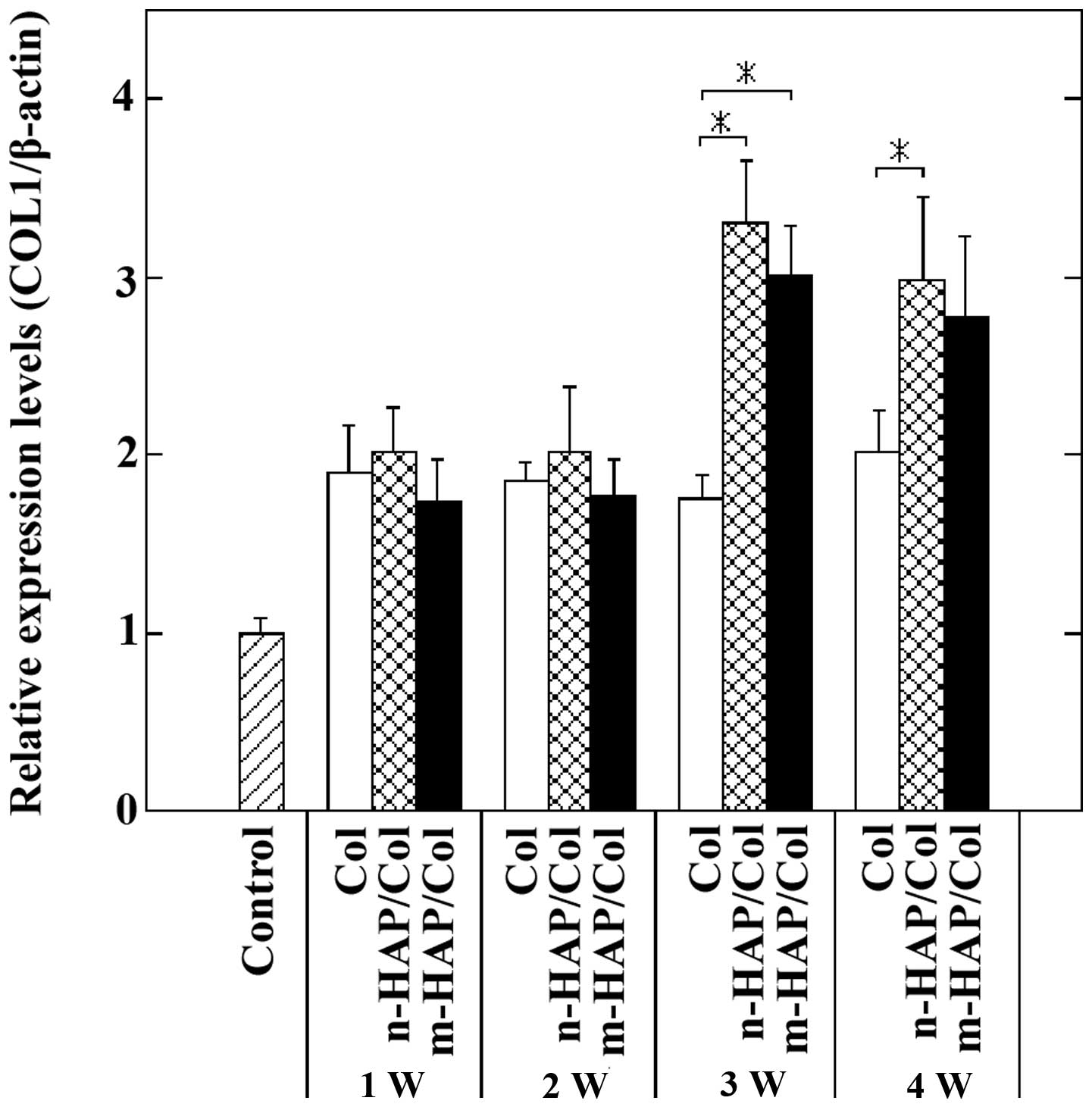 | Figure 2Expression of the type 1 collagen
(COL1) gene in osteoblast-like cells (SaOS-2) cells cultured on
collagen (Col), nano-sized hydroxylapatite (nHAP)/Col and
macro-pore sized hydroxylapatite (m-HAP)/Col composites for 1, 2, 3
and 4 weeks (*p<0.05). The expression levels of the
COL1 gene in cells cultured on Col were greater than those of the
control, but remained quasi-constant for up to 4 weeks. At 1 and 2
weeks, the relative expression levels of the COL1 gene in SaOS-2
cells cultured on Col, n-HAP/Col and m-HAP/Col composites were all
analogous to each other (approximately 1.9). It can be pointed out
that at 1 and 2 weeks, both n-HAP/Col and m-HAP/Col composites had
little effect on the upregulation of another early stage osteogenic
differentiation marker, the COL1 gene. However, at 3 and 4 weeks,
the expression levels of the COL1 gene in cells cultured on
n-HAP/Col were significantly higher than those of cells cultured on
Col (p<0.05), while those of cells cultured on m-HAP/Col tended
to exceed those of cells cultured on Col. These results indicated
that both n-HAP/Col and m-HAP/Col accelerated early-stage
osteogenic differentiation characterized by the expression of the
COL1 gene at 3 and 4 weeks. W, week. |
Middle-to-late stage osteogenic
differentiation marker (BSP and BGLAP) genes
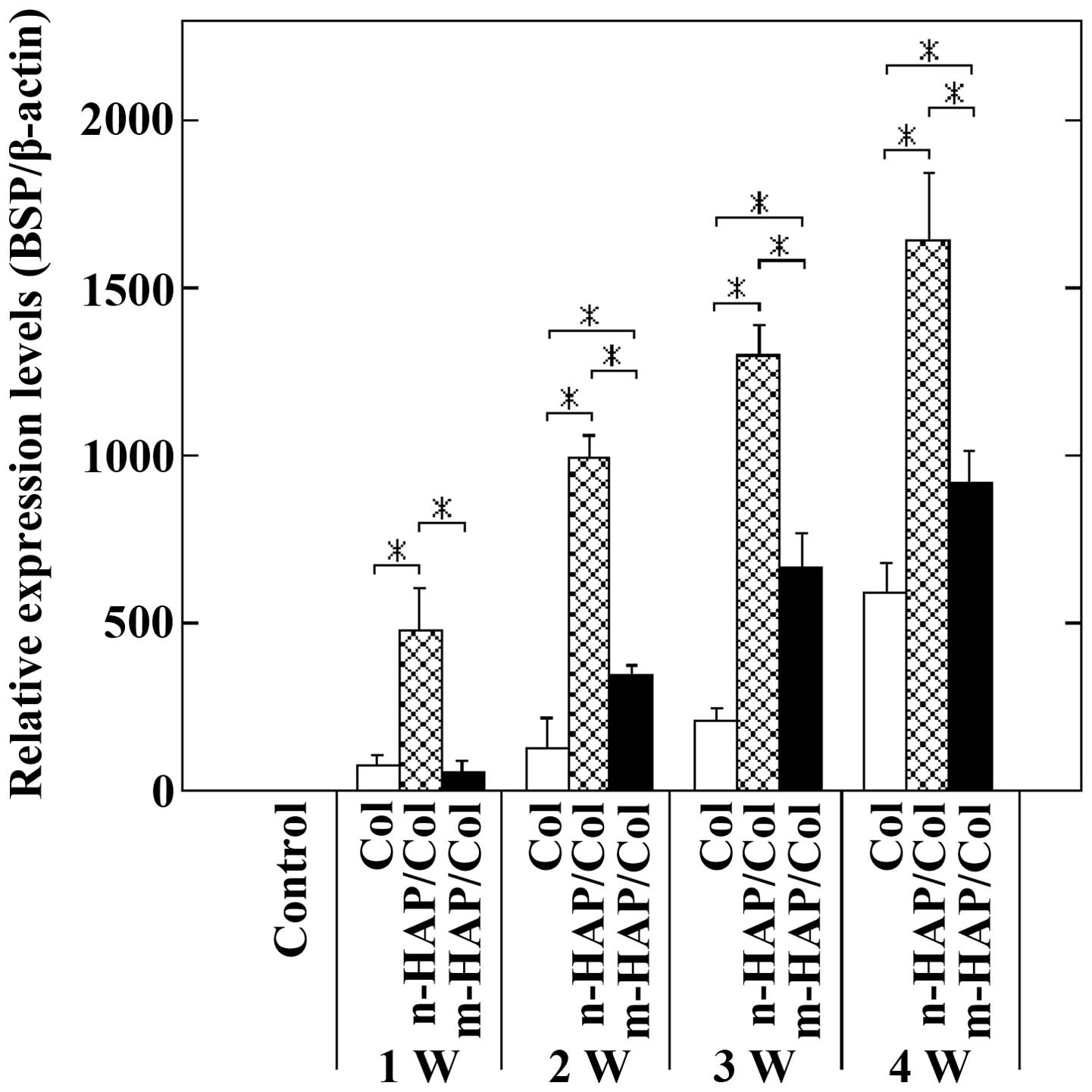
The expression of the BSP gene was the most
sensitive indicator of osteogenic differentiation of SaOS-2 cells
cultured on the three test samples. The n-HAP particles in the
n-HAP/Col composite significantly accelerated middle-to-late stage
osteogenic differentiation, characterized by the expression of the
BSP gene; this by far exceeded the osteogenic differentiation
induced by culture on m-HAP/Col and Col specimens (p<0.05)
(Fig. 3). It was observed that
the m-HAP particles in the m-HAP/Col composite also had the
capability to accelerate the said differentiation; however, the
levels were decreased by >2-fold compared with those induced by
n-HAP/Col.
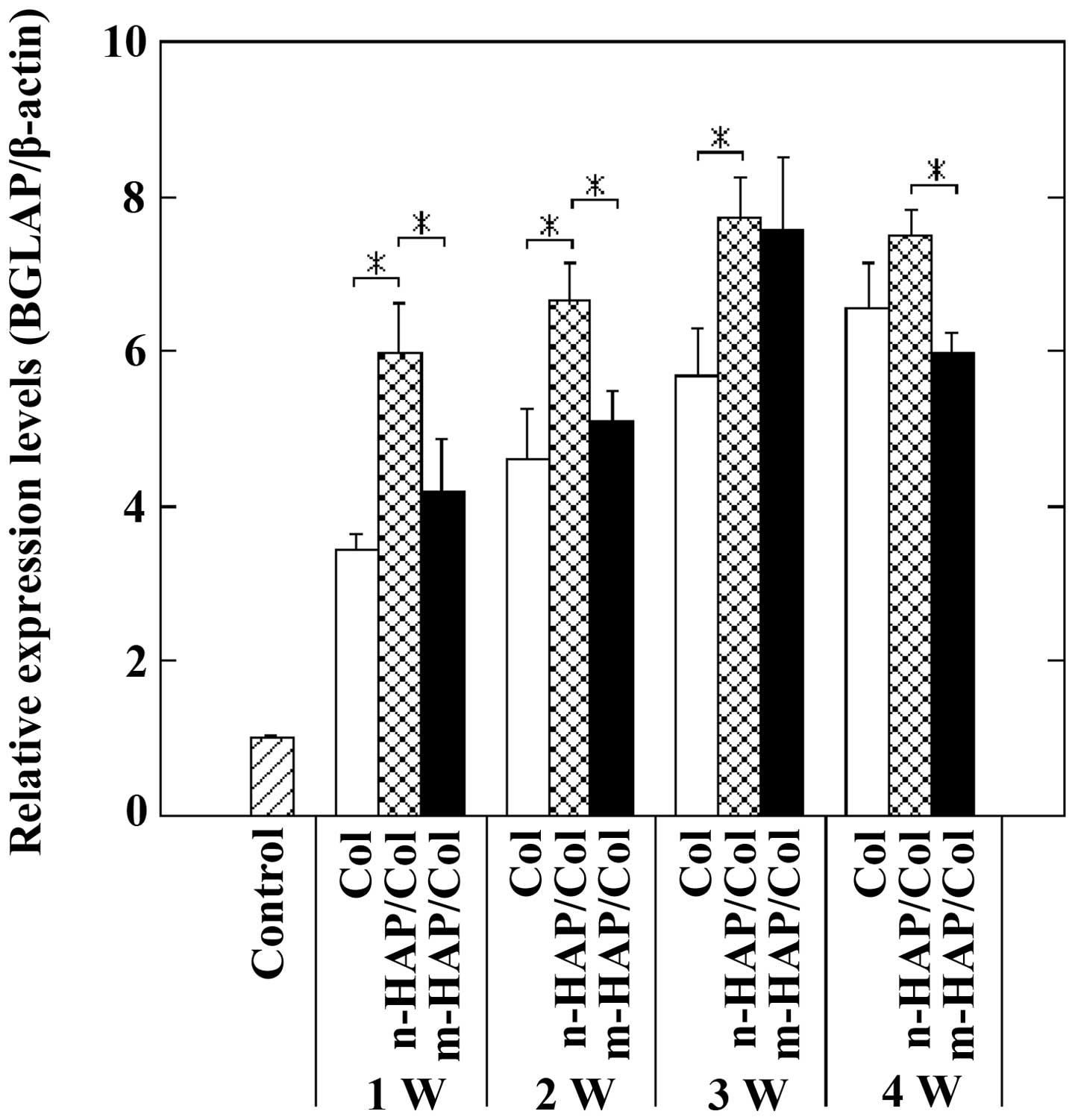
At 1 and 2 weeks, the expression levels of the BGLAP
gene in the SaOS-2 cells cultured on n-HAP/Col specimens were
higher than those of cells cultured on m-HAP/Col and Col specimens
(p<0.05), indicating that the n-HAP particles in the n-HAP/Col
composites had the ability to rapidly induce late-stage osteogenic
differentiation. At 3 and 4 weeks, however, the expression levels
of the BGLAP gene in the cells cultured on the three test materials
did not differ significantly, ranging between values of 6 to 7.5
(Fig. 4).
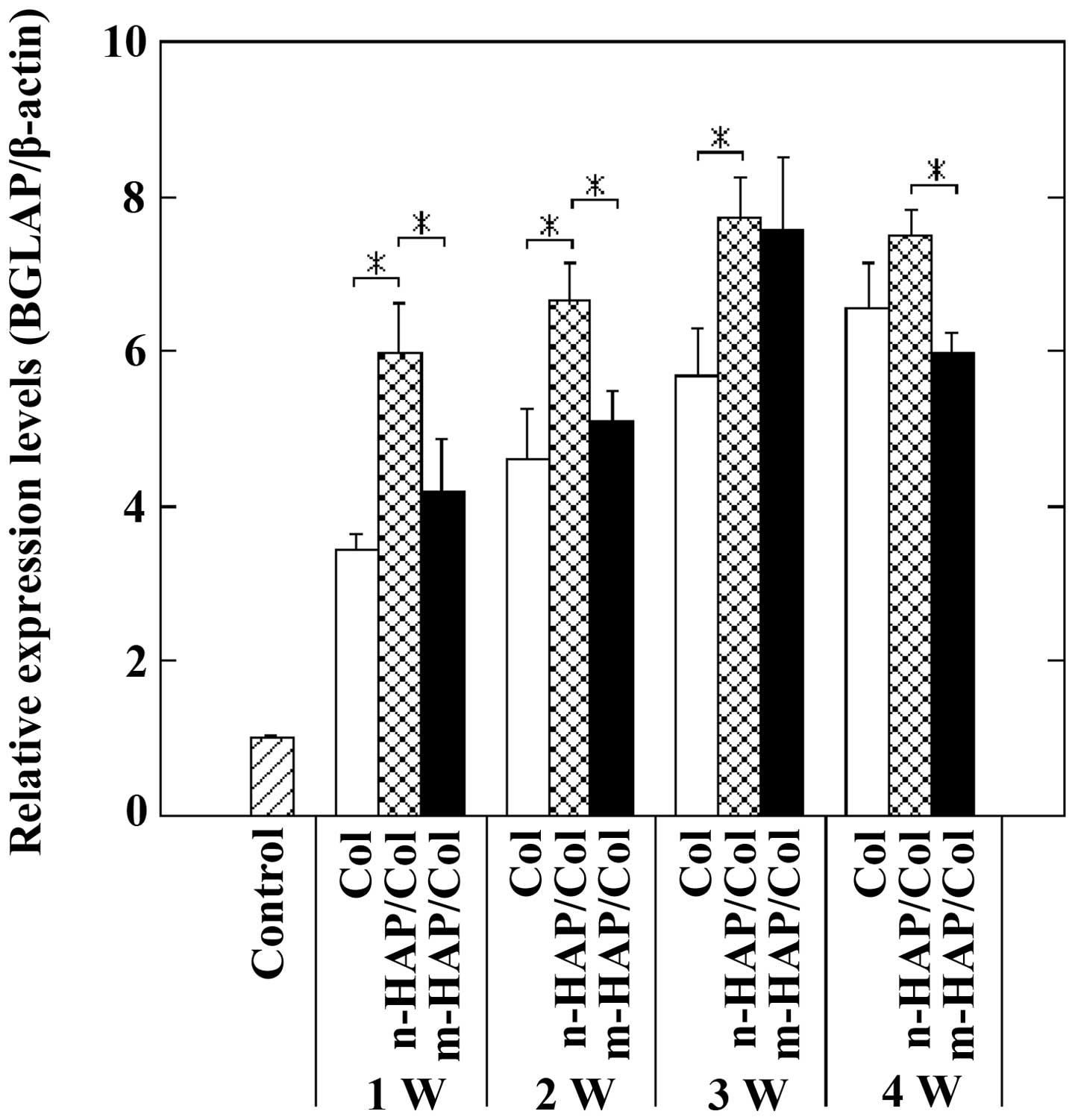 | Figure 4Expression of the bone
gamma-carboxyglutamate (gla) protein (BGLAP) gene (osteocalcin
precursor) in osteoblast-like cells (SaOS-2) cells cultured on
collagen (Col), nano-sized hydroxylapatite (nHAP)/Col and
macro-pore sized hydroxylapatite (m-HAP)/Col composites for 1, 2, 3
and 4 weeks (*p<0.05). The expression levels of the
BGLAP gene in SaOS-2 cells cultured on Col were greater than those
of the control, and gradually increased for up to 4 weeks. The
expression of the BGLAP gene in the cells cultured on n-HAP/Col and
m-HAP/Col slightly increased with time for up to 3 weeks, but
slightly decreased at week 3 to 4. At 1 and 2 weeks, culture on
n-HAP/Col markedly upregulated the expression of the BGLAP gene in
SaOS-2 cells, compared with culture on Col and m-HAP/Col
(p<0.05). It can be stated that n-HAP/Col solely had the ability
to accelerate late-stage osteogenic differentiation from the
beginning (at 1 week). At 3 and 4 weeks, the expression of the
BGLAP gene in cells cultured on Col, n-HAP/Col and m-HAP/Col
increased, but it became difficult to rank the ability to induce
late-stage osteogenic differentiation among the three test samples.
W, week. |
SEM observations
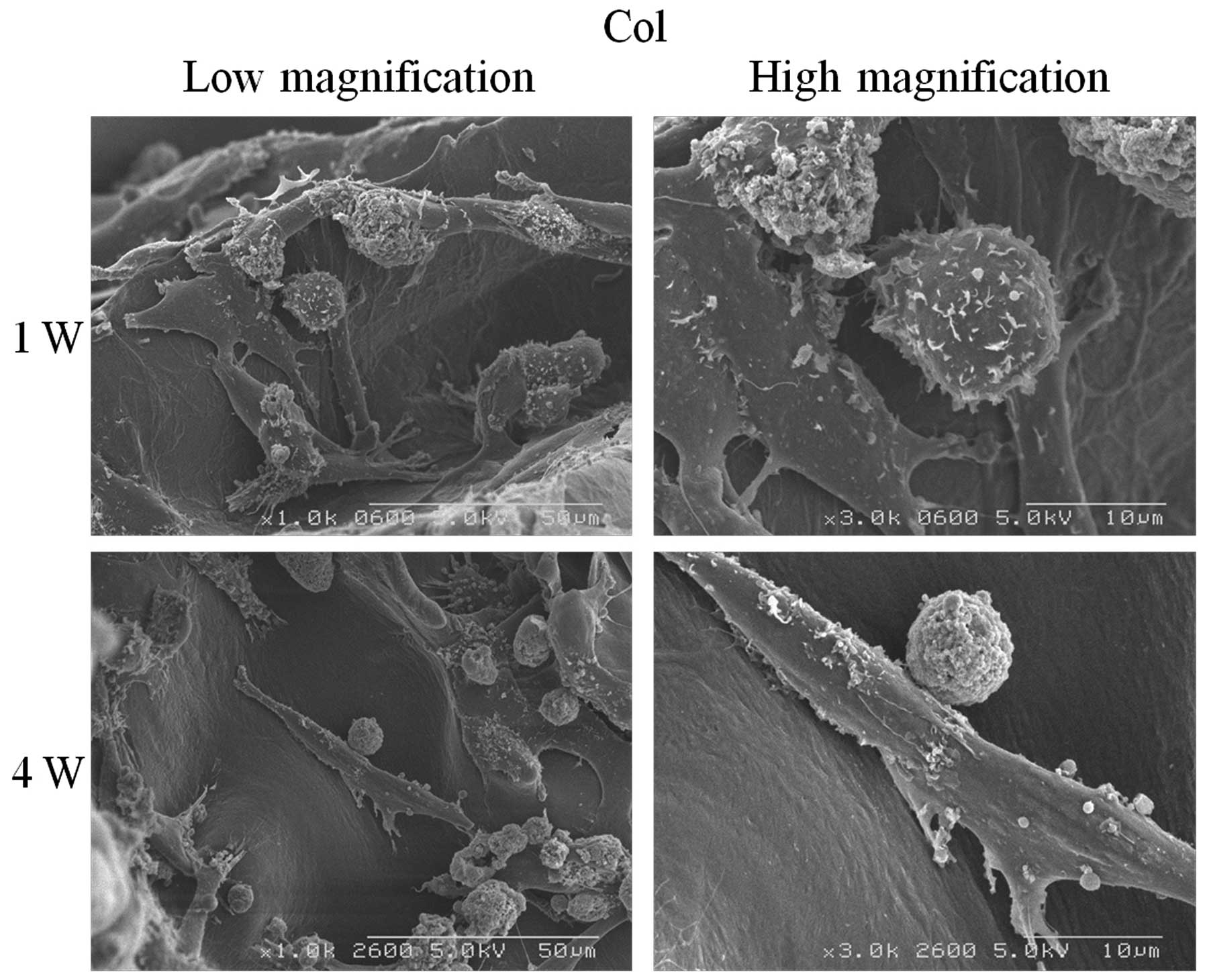
Col
Col was a scaffold, on which the osteoblasts adhered
and spread as fibroblasts. At 1 week, the SaOS-2 cells well covered
the Col surfaces. At 4 weeks, the cells remained as fibroblasts
with spherical particles (Fig.
5).
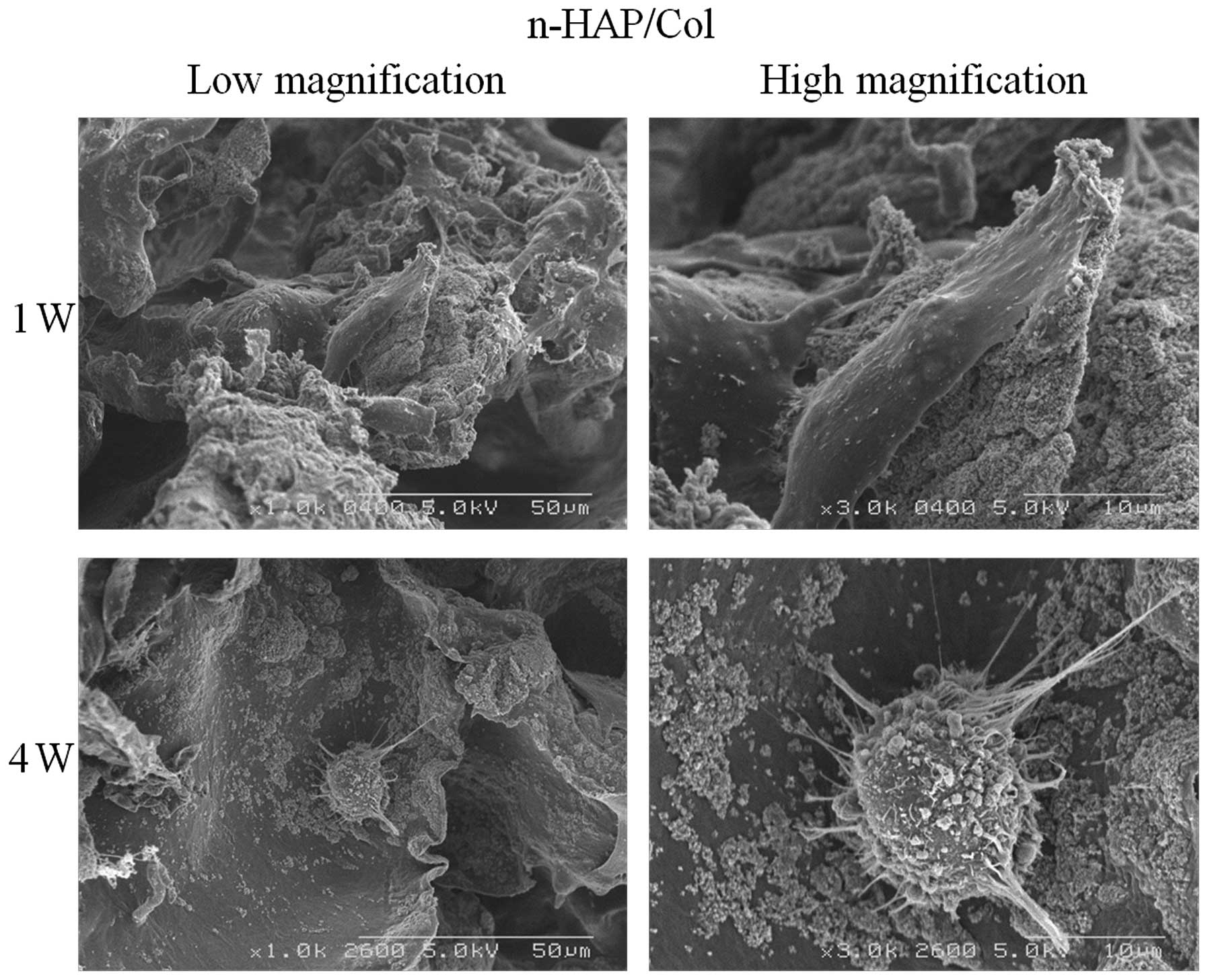
n-HAP/Col
n-HAP caused the SaOS-2 cells to significantly
change their shape as time progressed. At 1 week, the cells
preferentially covered and spread over the agglomerated n-HAP
particles in the n-HAP/Col composite as fibroblasts. At 4 weeks,
however, the cells seemed to move widely and appeared as spheroids
which actively phagocytized the n-HAP particles in the composite,
while extending many projections (Fig. 6). This positively affected the
osteogenic differentiation of the cells.
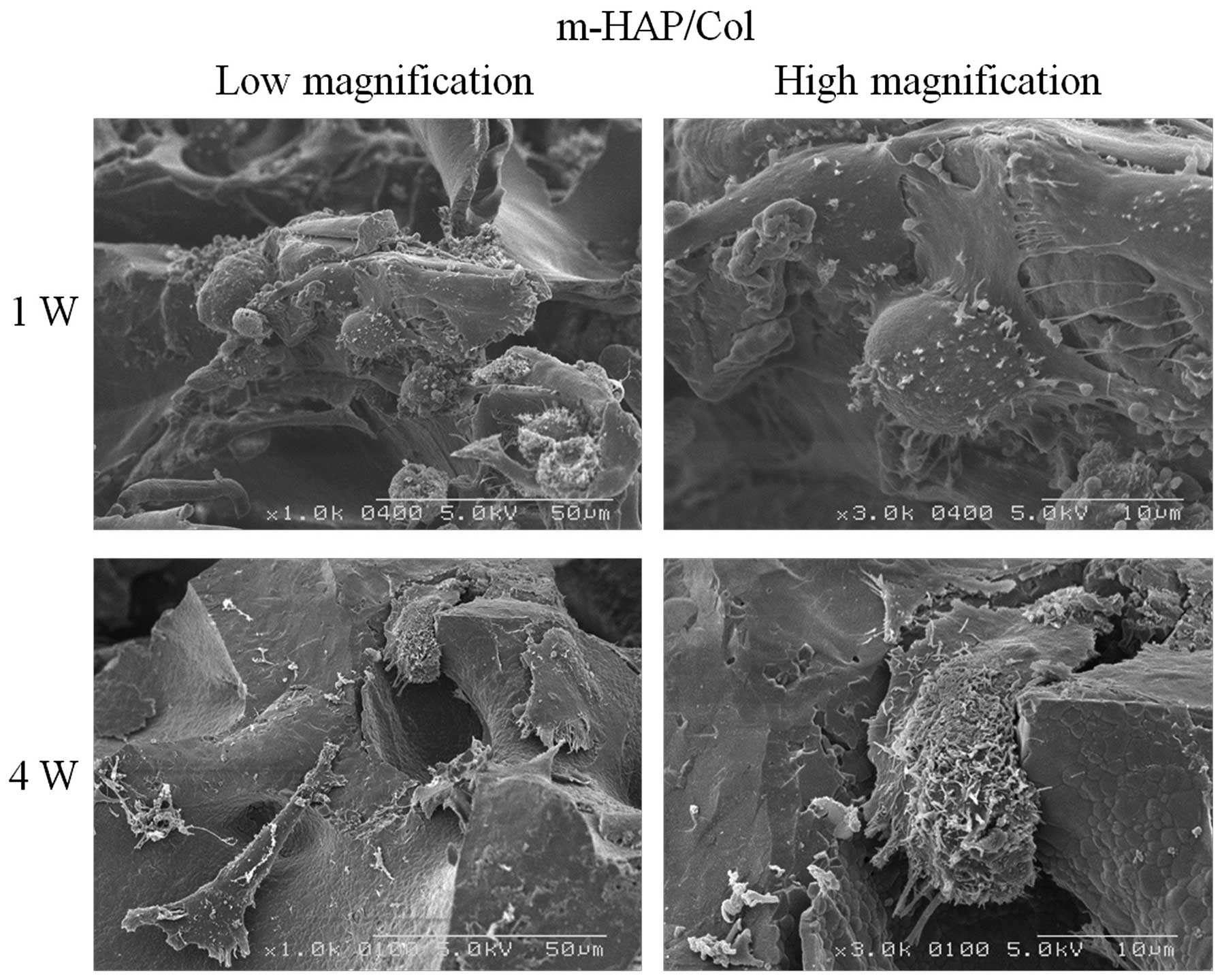
m-HAP/Col
Following culture for 1 week on the m-HAP/Col
composite containing the m-HAP particles, it was relatively
difficult for the fibroblastic SaOS-2 cells to adhere to the sponge
and spread over. At 4 weeks, the cells appeared as deformed
fibroblasts, detached from the m-HAP particles (Fig. 7).
Discussion
SaOS-2 cells are used as a standard cell model of
osteoblasts (14). We have
already reported that the osteogenic differentiation of SaOS-2
cells was more accelerated following culture on an apatite-coated
titanium plate surface than on a titanium plate, indicated by gene
expression analyses using SaOS-2 cells (15). As SaOS-2 cells are originally
found during early-stage osteogenic differentiation (i.e.,
ALP-positive cells), it was considered easy to evaluate the effects
of materials and chemicals on the osteogenic differentiation of
SaOS-2 cells at later stages.
It became clear from the results obtained that as
marker genes, the ALP (Fig. 1)
and BSP (Fig. 3) genes were
excellent indicators of osteogenic differentiation, while the COL1
(Fig. 2) and BGLAP (Fig. 4) genes were ambiguous. It was
emphasized that the BSP gene was the most outstanding indicator of
the (middle-to-late stage) osteogenic differentiation of SaOS-2
cells cultured on HAP/Col composites (Fig. 3). We also examined the expression
levels of a middle-stage marker, the opteopontin (SPP1) gene, in
the cells cultured on three test materials, but were unable to
determine the systematic effects of the materials on osteogenic
differentiation. The reason for these phenomena is unclear, and is
still under evaluation.
It should also be noted that higher levels of
differentiation of the SaOS-2 cells were observed when the cells
were cultured on three-dimensional Col compared with those cultured
(control) on a two-dimensional polystyrene culture dish (Figs. 1–4). It appeared that Col provided
three-dimensional space, allowing the SaOS-2 cells to have more
intercellular connections, and also benefitting the acceleration of
osteogenic differentiation (16).
The experimental results demonstrated that culture
on n-HAP/Col composites significantly accelerated the osteogenic
differentiation of SaOS-2 cells, followed by culture on m-HAP/Col
composites; the lowest acceleration rate was observed with culture
on Col composites. We considered that the reasons underlying these
phenomena are the following:
n-HAP particles in the n-HAP/Col composite existed
in an agglomerated state with a size of approximately 50 μm and
were loosely bound (Fig. 6). It
was observed that the SaOS-2 cells cultured for 1 week well adhered
to and spread over the agglomerated n-HAP particles as fibroblasts
(Fig. 6). It has been reported
that several proteins, including cellular adhesion proteins (e.g.,
fibronectin) are abundantly and preferentially absorbed on n-HAP
particles (17). These proteins
may facilitate good adhesion and the movement of SaOS-2 cells. It
was also observed that the SaOS-2 cells cultured for 4 weeks were
isolated and became spheroids. These cells may have moved and
actively phagocytized the n-HAP particles, while extending many
projections (Fig. 6). Similar
phagocytosis activity of osteoblasts has been reported by other
studies (18). It can be
hypothesized that the intracellular digestion of n-HAP particles
may accelerate the osteogenic differentiation of SaOS-2 cells
(4,18), partly due to the supply of calcium
and phosphate ions (19), and the
activation of cell signaling pathways (e.g., the MAPK pathway)
(20). However, it should be
noted that the digestion of n-HAP particles may cause the apoptosis
of cells and the secretion of inflammatory cytokines by cells due
to the production of reactive oxide species (ROS) (21,22). It may be necessary to balance the
positive and negative effects of n-HAP particles by adjusting the
quantities of n-HAP particles in n-HAP/Col composites. The use of
the most well-balanced n-HAP/Col composite may lead to the
development of a novel osteoconductive bone substitute material
with rapid effects, which may significantly contribute to the
treatment of patients with damaged or lost hard tissue in dental
and orthopedic surgeries. Future uses of n-HAP particles in
medicine may include the use of agents to release anti-microbial
chemicals (23), DNA-transfection
vectors (24) and biomaterial to
induce angiogenesis at sites of ischemia (25).
m-HAP particles have gained a good reputation as
particulate bone substitute materials in orthopedic surgery
(5). These much larger HAP
particles may play a different role in bone-rehabilitation in
bone-defect areas. It has been reported that m-HAP particles
effectively facilitate bone remodeling induced by osteoclasts and
osteoblasts (5). Osteoclasts may
be attracted to and mature on the surfaces of m-HAP particles in
vivo, leading to the partial dissolution of m-HAP particles.
Simultaneously, nearby osteoblasts are activated and new bone
formation follows (26). In the
cell culture condition using osteoblasts, bone-remodeling
conditions are lacking. Large m-HAP particles cannot be digested by
osteoblastic SaOS-2 cells. The more hydrophobic and less protein
absorbed surfaces of m-HAP particles in the m-HAP/Col composite
(27) may detach the SaOS-2 cells
with time, rendering strange morphological changes, as observed in
our study (Fig. 7). As a result,
the osteogenic differentiation of SaOS-2 cells cultured on
m-HAP/Col specimens may be sluggish, compared with those cultured
on n-HAP/Col.
Col itself does not have strong osteoconductive
properties (28). In brief, we
prepared Col, n-HAP/Col and m-HAP/Col specimens, and conducted an
expression analyses of four osteogenic differentiation marker genes
in SaOS-2 cells cultured for 1, 2, 3 and 4 weeks on three test
materials (Col, n-HAP/Col and m-HAP/Col) by RT-PCR. We then
observed morphological changes under an SEM. The following
experimental results were obtained: i) the osteogenic
differentiation of SaOS-2 osteoblastic cells cultured on
three-dimensional Col, n-HAP/Col and m-HAP/Col was considerably
superior to that of cells cultured on two-dimensional polystyrene
dishes (control); ii) the osteogenic differentiation of SaOS-2
cells cultured on n-HAP/Col was the most significant, followed by
m-HAP/Col, whilst the differentiation of cells cultured on Col was
the most insignificant; iii) the SaOS-2 cells phagocytized the
n-HAP particles in the n-HAP/Col composite, leading to the
acceleration of osteogenic differentiation; iv) the SaOS-2 cells
had limited contact with the m-HAP particles in the m-HAP/Col
composite, inducing inferior osteogenic differentiation.
Acknowledgements
This study was supported by the Grant-in-Aid Program
for the Strategic Research Foundation at Private Universities from
2010 to 2014 from the Ministry of Education, Culture, Sports,
Science and Technology (MEXT) of Japan, and by Grants-in-Aid from
the Japan Society for the Promotion of Science (JSPS) KAKENHI Grant
Numbers (C) 23592864, (C) 23592896, (C) 25463013 and (C)
25463053.
References
|
1
|
Nishikawa T, Masuno K, Tominaga K, Koyama
Y, Yamada T, Takakuda K, Kikuchi M, Tanaka J and Tanaka A: Bone
repair analysis in a novel biodegradable hydroxyapatite/collagen
composite implanted in bone. Implant Dent. 14:252–260. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Winter M, Griss P, de Groot K, Tagai H,
Heimke G, von Dijk HJ and Sawai K: Comparative histocompatibility
testing of seven calcium phosphate ceramics. Biomaterials.
2:159–160. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sionkowska A and Kozłowska J: Properties
and modification of porous 3-D collagen/hydroxyapatite composites.
Int J Biol Macromol. 52:250–259. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Huang Y, Zhou G, Zheng L, Liu H, Niu X and
Fan Y: Micro-/nano- sized hydroxyapatite directs differentiation of
rat bone marrow derived mesenchymal stem cells towards an
osteoblast lineage. Nanoscale. 4:2484–2490. 2012. View Article : Google Scholar
|
|
5
|
Tamai N, Myoui A, Kudawara I, Ueda T and
Yoshikawa H: Novel fully interconnected porous hydroxyapatite
ceramic in surgical treatment of benign bone tumor. J Orthop Sci.
15:560–568. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Liao S, Ngiam M, Watari F, Ramakrishna S
and Chan CK: Systematic fabrication of nano-carbonated
hydroxyapatite/collagen composites for biomimetic bone grafts.
Bioinspir Biomim. 2:37–41. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Shigeishi H, Takechi M, Nishimura M,
Takamoto M, Minami M, Ohta K and Kamata N: Clinical evaluation of
novel interconnected porous hydroxyapatite ceramics (IP-CHA) in a
maxillary sinus floor augmentation procedure. Dent Mater J.
31:54–60. 2012. View Article : Google Scholar
|
|
8
|
Bernhardt A, Lode A, Peters F and Gelinsky
M: Comparative evaluation of different calcium phosphate-based bone
graft granules - an in vitro study with osteoblast-like cells. Clin
Oral Implants Res. 24:441–449. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Id Boufker H, Lagneaux L, Fayyad-Kazan H,
Badran B, Najar M, Wiedig M, Ghanem G, Laurent G, Body JJ and
Journé F: Role of farnesoid X receptor (FXR) in the process of
differentiation of bone marrow stromal cells into osteoblasts.
Bone. 49:1219–1231. 2011.PubMed/NCBI
|
|
10
|
Tsigkou O, Hench LL, Boccaccini AR, Polak
JM and Stevens MM: Enhanced differentiation and mineralization of
human fetal osteoblasts on PDLLA containing Bioglass composite
films in the absence of osteogenic supplements. J Biomed Mater Res
A. 80:837–851. 2007. View Article : Google Scholar
|
|
11
|
Taira M, Hatekeyama W, Kihara H, Kondo H,
Ueda K and Narushima T: Quantitative analyses of
osteogenic-differentiation-related gene expressions in human
osteoblat-like cells (SaOS-2) cultured on hydroxyapatite and
titanium. J Oral Tissue Eng. 10:34–41. 2012.
|
|
12
|
Kohal RJ, Bächle M, Att W, Chaar S,
Altmann B, Renz A and Butz F: Osteoblast and bone tissue response
to surface modified zirconia and titanium implant materials. Dent
Mater. 29:763–776. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Okada M and Furuzono T: Calcination of
rod-like hydroxyapatite nanocrystals with an anti-sintering agent
surrounding the crystals. J Nanoparticle Res. 9:807–815. 2007.
View Article : Google Scholar
|
|
14
|
Czekanska EM, Stoddart MJ, Richards RG and
Hayes JS: In search of an osteoblast cell model for in vitro
research. Eur Cell Mater. 24:1–17. 2012.PubMed/NCBI
|
|
15
|
Chosa N, Taira M, Saitoh S, Sato N and
Araki Y: Characterization of apatite formed on
alkaline-heat-treated Ti. J Dent Res. 83:465–469. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Naito H, Yoshimura M, Mizuno T, Takasawa
S, Tojo T and Taniguchi S: The advantages of three-dimensional
culture in a collagen hydrogel for stem cell differentiation. J
Biomed Mater Res A. 101:2838–2845. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lock J, Nguyen TY and Liu H: Nanophase
hydroxyapatite and poly(lactide-co-glycolide) composites promote
human mesenchymal stem cell adhesion and osteogenic differentiation
in vitro. J Mater Sci Mater Med. 23:2543–2552. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Liu X, Zhao M, Lu J, Ma J, Wei J and Wei
S: Cell responses to two kinds of nanohydroxyapatite with different
sizes and crystallinities. Int J Nanomedicine. 7:1239–1250. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Matsumoto S, Hayashi M, Suzuki Y, Suzuki
N, Maeno M and Ogiso B: Calcium ions released from mineral trioxide
aggregate convert the differentiation pathway of C2C12 cells into
osteoblast lineage. J Endod. 39:68–75. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Chen G, Deng C and Li YP: TGF-β and BMP
signaling in osteoblast differentiation and bone formation. Int J
Biol Sci. 8:272–288. 2012.
|
|
21
|
Xu Z, Liu C, Wei J and Sun J: Effects of
four types of hydroxyapatite nanoparticles with different
nanocrystal morphologies and sizes on apoptosis in rat osteoblasts.
J Appl Toxicol. 32:429–435. 2012. View
Article : Google Scholar : PubMed/NCBI
|
|
22
|
Nadra I, Boccaccini AR, Philippidis P,
Whelan LC, McCarthy GM, Haskard DO and Landis RC: Effect of
particle size on hydroxyapatite crystal-induced tumor necrosis
factor alpha secretion by macrophages. Atherosclerosis. 196:98–105.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Rauschmann MA, Wichelhaus TA, Stirnal V,
Dingeldein E, Zichner L, Schnettler R and Alt V: Nanocrystalline
hydroxyapatite and calcium sulphate as biodegradable composite
carrier material for local delivery of antibiotics in bone
infections. Biomaterials. 26:2677–2684. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Chowdhury EH: pH-sensitive nano-crystals
of carbonate apatite for smart and cell-specific transgene
delivery. Expert Opin Drug Deliv. 4:193–196. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Mima Y, Fukumoto S, Koyama H, Okada M,
Tanaka S, Shoji T, Emoto M, Furuzono T, Nishizawa Y and Inaba M:
Enhancement of cell-based therapeutic angiogenesis using a novel
type of injectable scaffolds of hydroxyapatite-polymer
nanocomposite microspheres. PLoS One. 7:e351992012. View Article : Google Scholar
|
|
26
|
Bernhardt A, Thieme S, Domaschke H,
Springer A, Rösen-Wolff A and Gelinsky M: Crosstalk of osteoblast
and osteoclast precursors on mineralized collagen-towards an in
vitro model for bone remodeling. J Biomed Mater Res A. 95:848–856.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Svendsen IE, Santos O, Sotres J,
Wennerberg A, Breding K, Arnebrant T and Lindh L: Adsorption of
HSA, IgG and laminin-1 on model hydroxyapatite surfaces-effects of
surface characteristics. Biofouling. 28:87–97. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Taira M, Nezu T, Sasaki K, Saitoh S,
Kagiya T, Harada H, Takada Y and Araki Y: Preparation and in vivo
evaluation of apatite/collagen packed composite by alternate
immersion method and Newton press. J Biomed Mater Res B Appl
Biomater. 90:566–573. 2009. View Article : Google Scholar : PubMed/NCBI
|