Introduction
Hypertension is an important risk factor for the
development of cardiovascular disease. In addition to causing
damage to the heart, hypertension can also cause stress and damage
to several other organs and tissues, including the brain, liver,
kidneys and vascular tissue (1,2).
Previous studies have described the effects of high blood pressure
on heart and brain tissue damage, showing that such effects can
lead to myocardial hypertrophy and stroke (3). There are significant data showing
that treatment with anti-hypertensive drugs leads to changes in
gene expression in the kidneys and bladder tissue (4,5).
Additionally, a recent study demonstrated that treatment with such
drugs may also result in changes in gene expression directly in the
heart, brain and liver tissues (6). The authors reported on
differentially expressed genes following treatment with
anti-hypertensive drugs. While 33 of these genes were previously
linked to cardiovascular disease, this analysis also led to the
identification of 16 novel genes with no known link to
cardiovascular disease; some of the 16 newly identified genes
included interleukin (IL)-24, cathepsin Z (Ctsz), and secretory
carrier membrane protein (Scamp2). Genes that are differentially
expressed following treatment with anti-hypertensive drugs may be
potential biomarkers and novel targets for the prevention of
cardiovascular disease. Moreover, such genes may provide valuable
information for the development of new anti-hypertensive therapy
(6).
Initially identified in 1995 during a melanoma cell
treatment regimen, IL-24 [also known as melanoma differentiation
associated gene-7 (MDA-7)] possesses tumor suppressor
characteristics (7). IL-24 cDNA
encodes a protein of 206 amino acids with molecular weight of 23.8
kDa. N-terminal signal peptide sequences have indicated that IL-24
is a secreted protein (8). The
transfer of recombinant IL-24 into mononuclear cells in human
peripheral blood has been shown to lead to the release of IL-6,
interferon (IFN)-γ, tumor necrosis factor (TNF)-α, IL-12, and
granulocyte-macrophage colony-stimulating factor (GM-CSF), lending
to its characterization as a bona fide cytokine (8). Adenovirus-mediated IL-24 expression
has been shown to inhibit the growth of vascular endothelial cells
in tumor tissues, suggesting that IL-24 may inhibit angiogenesis
(9). In human melanoma, the loss
of IL-24 has been shown to be closely associated with tumor
invasion and metastasis, suggesting that IL-24 may be a tumor
suppressor in this setting as well (10).
Since IL-24 inhibits cancer cell proliferation
through multiple biological pathways, it may also exert
anti-proliferative effects in occlusive vascular disease. It has
been demonstrated that both atherosclerosis and cancer may
originate from local tissue injury, which can promote inflammation
and genomic instability (11).
Whereas some researchers have worked to elucidate the role of IL-24
in cancer (12–14,49), its role in cardiovascular disease
remains unclear.
A number of cardiovascular diseases, including
ischemia/reperfusion injury and myocardial infarction, have been
shown to be closely associated with cellular apoptosis (15). Reactive oxygen species (ROS), such
as hydrogen peroxide (H2O2), can lead to the
development of cardiovascular disease by promoting the apoptosis of
endothelial cells (16,17). Protecting endothelial cells from
apoptosis has a positive clinical significance in the prevention
and treatment of cardiovascular disease. Some have proposed
repairing endothelial cell injury as part of hypertension treatment
and have suggested that the degree of injury may be indicative of
disease severity (18,47). As such, the detection of
endothelial cell dysfunction is clinically important.
To date, to the best of our knowledge, there are no
studies available describing the protective effects of IL-24 on
vascular endothelial cells following injury. Previous studies have
suggested that the adenovirus-mediated introduction of tumor
suppressor genes, such as retinoblastoma (RB), p53, p21 and
phosphatase and tensin homolog (PTEN) inhibits vascular smooth
muscle cell (VSMC) proliferation and neointima formation following
vascular injury in vivo (19–22). However, the potential effects of
IL-24 on oxidative damage and the abnormal proliferation of
vascular endothelial cells have not yet been reported.
In the present study, we examined whether IL-24
exerts protective effects on vascular endothelial injury induced by
oxidative stress, and whether it is a therapeutic target of
anti-hypertensive drugs in the cardiovascular system. Performing
cellular experiments, we found that IL-24 protected against
H2O2-induced endothelial cell damage, and
that the expression of IL-24 could be altered by an increase in
blood pressure and anti-hypertensive drug therapy in a rat model of
hypertension. Our results revealed that the IL-24 gene is closely
related to cardiovascular disease and may thus provide a novel
therapeutic target for the treatment of cardiovascular disease.
Materials and methods
Materials and reagents
Human umbilical vein endothelial cells (HUVECs) were
obtained from the Shanghai Institute of Cell Biology, Chinese
Academy of Sciences, China. Normal male Sprague Dawley (SD) rats
(n=36, 6–7 weeks old; weight, 225±25 g) were purchased from the
Academy of Military Medical Sciences (Beijing, China). Dulbecco's
modified Eagle's medium (DMEM) and trypsin were from Gibco Life
Technologies (Grand Island, NY, USA); fetal bovine serum (FBS) was
obtained from (HyClone (Logan, UT, USA); the hypertension
construction pump (ALZET miniosmotic pump) was from Durect Corp.,
(Cupertino, CA, USA); angiotensin II was purchased from
Sigma-Aldrich (St. Louis, MO, USA); the IL-24 recombinant shuttle
plasmid, pDC316-h IL-24, and the empty plasmid, pDC316, were
obtained from Benyuan Zhengyang Gene Technology Co. Ltd. (Beijing
China); the plasmid extraction and purification kit was purchased
from Bioer Technology Co., Ltd. (Hangzhou, China); the liposome
transfection reagent, Lipofectamine® 2000, was from
Invitrogen (Carlsbad, CA, USA); the Cell Counting Kit-8 (CCK-8) was
obtained from the Beyotime Institute of Biotechnology (Shanghai
China); the ROS test kit was from Beijing Applygen Technology Ltd.
(Beijing, China); the Annexin V/PI staining kit was obtained from
Nanjing KGI Biotechnology Development Co., Ltd. (Nanjing, China).
The anti-cleaved caspase-3 antibody [(Asp175) Western Blot
Detection Kit] was from Cell Signaling Technology, Inc., (Danvers,
MA, USA); anti-IL-24 [EPR13281] antibody (ab182567) was from Abcam
(Cambridge, UK); anti-endothelin-1/ET-1 (N-8) (sc-21625),
anti-angiotensin II type 1 receptor-associated protein
(AGTRAP/ATRAP) (F-6) (sc-271367), anti-angiotensin (H-12)
(sc-374511) and anti-platelet-derived growth factor (PDGF-A) (H-77)
(sc-7958) antibodies were all from Santa Cruz Biotechnology, Inc.
(Heidelberg, Germany).
Cell culture
The HUVECs were grown in DMEM supplemented with 10%
(v/v) heat-inactivated FBS and 1% (v/v) penicillin-streptomycin at
37°C in a humidified atmosphere containing 5% CO2. All
experiments were performed using cells cultured for 3–4 days at
approximately 80–90% confluency.
Cell experimental groups
The cells were divided into the following groups: in
group A, control cells cultured in DMEM with 10% FBS. In group B,
cells were exposed to H2O2 (0.10 or 0.30
mmol/l). In group C, the cells were exposed to
H2O2 (same concentrations of
H2O2 described above) and also treated with
IL-24. The cells in this group were transfected with the
recombinant plasmid, pDC316-h IL-24 (100 ng/ml) using Lipofectamine
2000 to promote IL-24 expression. In group D, the cells were
treated with H2O2, but transfected with the
empty plasmid (served as a control). The other 2 control groups
were group E and F. In group E, the cells were transfected only
with the recombinant plasmid, pDC316-h IL-24. In group F, the cells
were transfected only with the empty plasmid. The cells were
examined by fluorescence microscopy for transfection efficiency at
24 h post-transfection. The cells incubated for 48 h to determine
the protective effects of IL-24 against
H2O2.
Animal grouping and intervention
The normal SD rats were divided into a control group
(n=12) and a hypertension group (n=24). An osmotic micropump was
used to generate the model of hypertension, as previously described
(23,24). The osmotic pump with the
pre-placement of angiotensin II was implanted subcutaneously. The
infusion of angiotensin II was carried out by subcutaneous
implantation [500 ng/(kg·min), 7 days]. Blood pressure was recorded
daily using a BP-6 animal non-invasive blood pressure measuring
instrument (Chengdu Taimeng Technology Co., Ltd., Chengdu, China).
The tail artery blood pressure of the rats was measured using the
tail-cuff method. The rats are arranged in the heating device,
which was heated to 37°C for 3 min, then the tail was connected
with the sensor, while the rats were in a quiescent state; food and
water was made availabe in the device, which helped to keep the
rats calm. Blood pressure was measured without anesthesia with the
rats in a quiescent state. The blood pressure of each rat was
continuously measured at least 10 times and the average values were
calculated.
After successfully establishing the model of
hypertension, 12 rats were sacrificed by cervical disclocation 2
weeks after they experienced a spike in blood pressure. The heart
and kidney tissues were harvested from these animals, and real-time
PCR was performed to detect the expression of IL-24. The remaining
12 hypertensive rats were administered enalapril (35 mg/kg/day;
Shanghai Modern Pharmaceutical Ltd., Shanghai, China) and
nifedipine (30 mg/kg/day; Beijing Bayer Healthcare Co., Ltd.,
Beijing, China) orally each day for 3 weeks. This leads to a steady
decline in blood pressure; 1 week after the blood pres-sure had
decreased and stabilized, the rats were sacrificed and IL-24 gene
expression was examined.
Ethics statement
All surgical and animal care procedures were
approved by the Institutional Ethics Committee. All research was
carried out in strict accordance with the provided guidelines. We
abided by all relevant provisions set forth by the Medical Ethics
Committee of Shanxi Medical University (Shanxi, China).
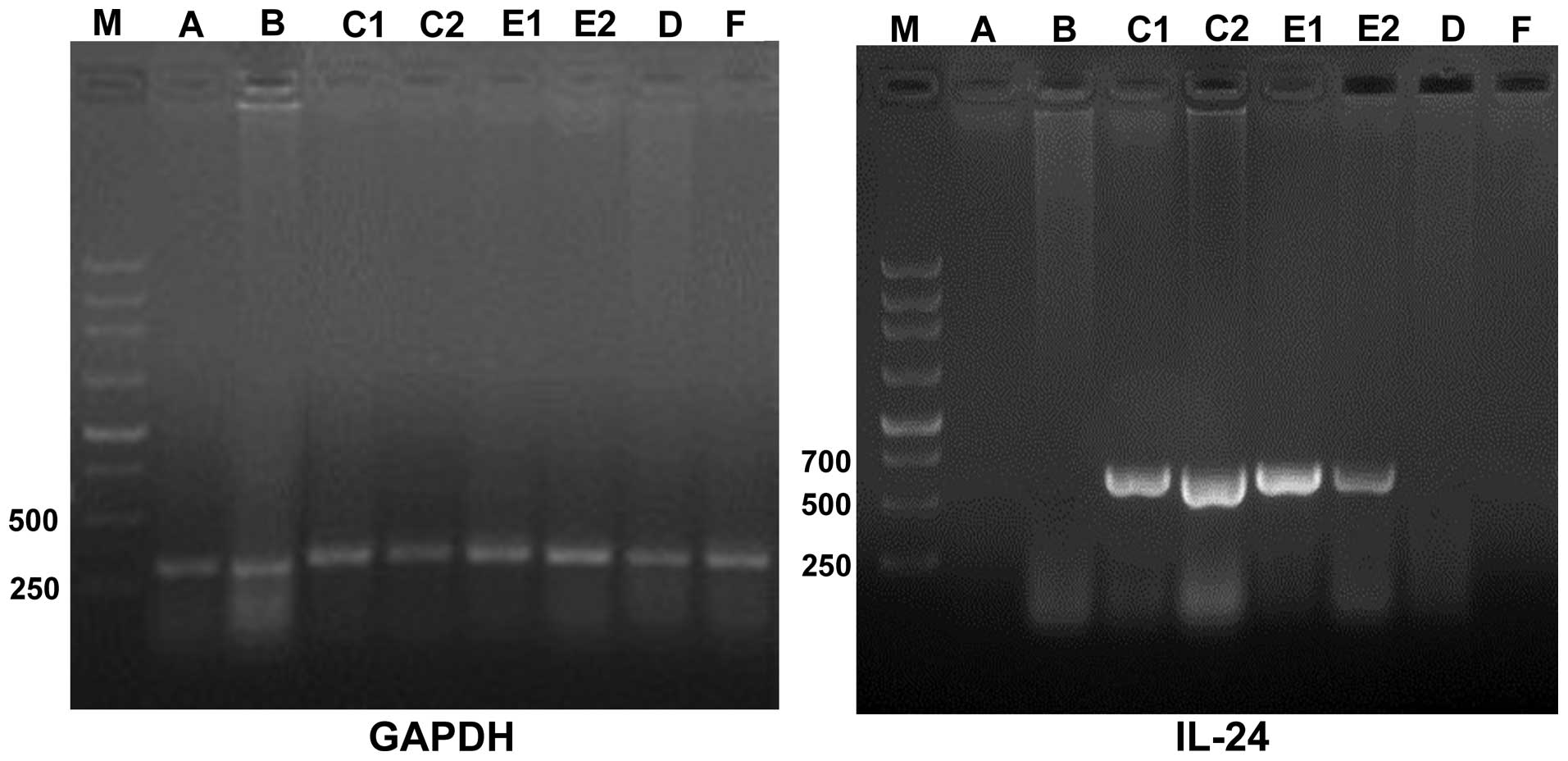
Determination of IL-24 transfection
efficiency by RT-PCR
Total RNA was extracted from the cells using TRIzol
reagent. RNA concentration and purity were determined by UV
spectrophotometry prior to reverse transcription and cDNA
synthesis. The reaction conditions were as follows: 95°C
denaturation for 5 min, followed by 95°C denaturation 30 sec, 58°C
annealing 30 sec, 72°C extension 60 sec, cycle 32 times, 72°C
terminal extension 7 min, 4°C hold. PCR products were analyzed by
1.0% agarose gel electrophoresis and sequenced by imaging analysis
using the IS-10,000 multifunction gel image analysis system
(Shanghai Tianneng Technology Co., Ltd., Shanghai, China). The
primers used for RT-PCR are listed in Table I. The amplified fragment length of
IL-24 was 624 bp and that of glyceraldehyde 3-phosphate
dehydrogenase (GAPDH) was 307 bp.
 | Table ISequences of primers used for
RT-PCR. |
Table I
Sequences of primers used for
RT-PCR.
| Gene | Primer sequences
(5′→3′) |
|---|
| IL-24 | F:
GCCAAGCTTATGAATTTTCAACAGAGG |
| R:
GCCGTCGACCTAGAGCTTGTAGAATTT |
| GAPDH | F:
TGAACGGGAAGCTCACTGG |
| R:
TCCACCACCCTGTTGCTGGA |
Cell migration assay
The study by Burdon and Gill indicated that
H2O2 is an 'information contact' between
cells, and that H2O2 is one of the essential
materials for cell maintenance (25). H2O2 at low
concentration may play the role of a mitogen and can stimulate cell
proliferation and migration. We wished to determine whether
H2O2 can stimulate cell proliferation and
migration. We performed a scratch test to determine the effects of
H2O2 (0.1 mmol/l) with or without the
presence of IL-24 on HUVEC migration. Briefly, a small scratch was
made using a 10-µl pipette tip in the culture dish at time
0, and the distance the cells had migrated was observed at 24
h.
Cytotoxicity assays
Cell viability was measured by CCK-8 assay,
according to the manufacturer's instructions (Beyotime Institute of
Biotechnology). The cells were seeded in a 96-well plate and
transfected with the empty plasmid or IL-24 plasmid the following
day using Lipofectamine 2000. At 24 h post-transfection, the cells
were switched to serum-free medium for 24 h. They were then exposed
to H2O2 (0.30 mmol/l) for 12 h. CCK-8
solution (10 µl) was then added to each well 1 h before the
absorbance was measured at 450 nm using a microplate reader
(Molecular Devices, LLC, Sunnyvale, CA, USA). Cell viability was
determined as follows: cell viability (%) = treatment group
OD/control group OD ×100.
Apoptosis assay
Annexin V/PI staining was performed to detect
apoptosis. The treated cells were collected, washed and then
stained with Annexin V/PI for 20 min in the dark at room
temperature. The percentage of apoptotic cells was analyzed by flow
cytometry (BD FACSCalibur flow cytometer, FACS101; BIO-RAD
Corporation, Hercules, CA, USA).
Determination of intracellular ROS
production
Intracellular ROS production was measured by flow
cytometry and fluorescence microscopy. Following treatment, the
cells were washed and incubated with
2′,7′-dichlorodihydrofluorescein diacetate (DCFH-DA; 10
µmol/l; Sigma-Aldrich) for 20 min at 37°C in the dark. The
fluorescence corresponding to the intra-cellular ROS levels was
monitored using a light microscope (Olympus BX51; Olympus, Tokyo,
Japan) and analyzed by flow cytometry (BD FACSCalibur flow
cytometer, FACS101; BIO-RAD Corporation).
Real-time PCR
We used real-time PCR to detect the expression of
the hypertension-related factors, angiotensinogen, endothelin-1,
ATRAP and PDGF in the HUVECs, as well as IL-24 gene expression in
the heart and kidney tissue of the rats in our model of
hypertension and following anti-hypertensive therapy. In the cell
experiments, total RNA was isolated from the treated HUVECs using
RNeasy spin columns obtained from Qiagen (Hilden, Germany).
Real-time PCR was performed in triplicate on a Stratagene Mx3005P
Multiplex Quantitative PCR system (Stratagene, La Jolla, CA, USA)
using 100 ng RNA, 12.5 µl 2X QuantiFast SYBR-Green PCR
Master Mix (Qiagen) and 1 µmol each of forward and reverse
primers (Table II) in a total
final volume of 25 µl. For the tissues, the tissue samples
were incubated at 94°C for 10 min. Subsequently, denaturation was
performed for 45 cycles at 94°C for 15 sec followed by annealing
and extension at 60°C for 60 sec. The amplification products were
normalized to β-actin. The expression of the target gene,
normalized to β-actin, was calculated using the 2−ΔΔCt
method, as previously described (26).
 | Table IISequences of primers used for
real-time PCR. |
Table II
Sequences of primers used for
real-time PCR.
| Gene | Primer sequences
(5′→3′) |
|---|
|
Angiotensinogen | F:
CTTCCAGCACTGGAGTGACA |
| R:
AGAGGCATAGTGAGGCTGGA |
| Endothelin-1 | F:
AATGCCATGCTTCCCATTAG |
| R:
CCCTGAGGACAACAGGGATA |
| ATRAP | F:
GGGTTTCCTTGGGTCTTCTC |
| R:
CAAGAGACGGAGGTCAGGAG |
| PDGF | F:
GGTGGTCACAGGTGCTTTTT |
| R:
TCCAAGACATTCCTGCTTCC |
| β-actin | F: GTCAGGTCATCACTA
TCGGCAAT |
| R:
AGAGGTCTTTACGGATGTCAACGT |
| IL-24 | F:
AATGCCATGCTTCCCATTAG |
| R:
CCCTGAGGACAACAGGGATA |
Western blot analysis
We used western blot analysis to detect the
expression of cleaved casepase-3, angiotensinogen, endothelin-1,
ATRAP and PDGF in the HUVECs, and that of IL-24 in the heart and
kidney tissue of the rats. In the cell experiments, protein was
extracted from the treated HUVECs and the concentration was
determined. Equal amounts of total protein were analyzed on
SDS-PAGE gels. The samples were transferred onto a membrane, which
was incubated with first primary and then secondary antibodies. The
protein bands were visualized by enhanced chemiluminescence (ECL)
and autoradiography. Protein bands were analyzed using Quantity One
image analysis software. In the animal experiments, specific
intervention and treatment times were the same as those described
for the determination IL-24 mRNA expression by RT-PCR. Protein was
harvested from the rat kidney and heart tissues and was analyzed as
described for the cell experiments.
Statistical analysis
We used SPSS 19 software for statistical analysis.
Data are presented as the means ± standard deviation. Data were
analyzed by one way analysis of variance (ANOVA) and Student's
t-test. A value of P<0.05 was considered to indicate a
statistically significant difference.
Results
Detection of IL-24 gene transcription in
endothelial cells
RT-PCR confirmed the successful transfection and
overexpression of IL-24 in endothelial cells in both the
H2O2 + IL-24 (group C) and IL-24 (group E)
groups (Fig. 1).
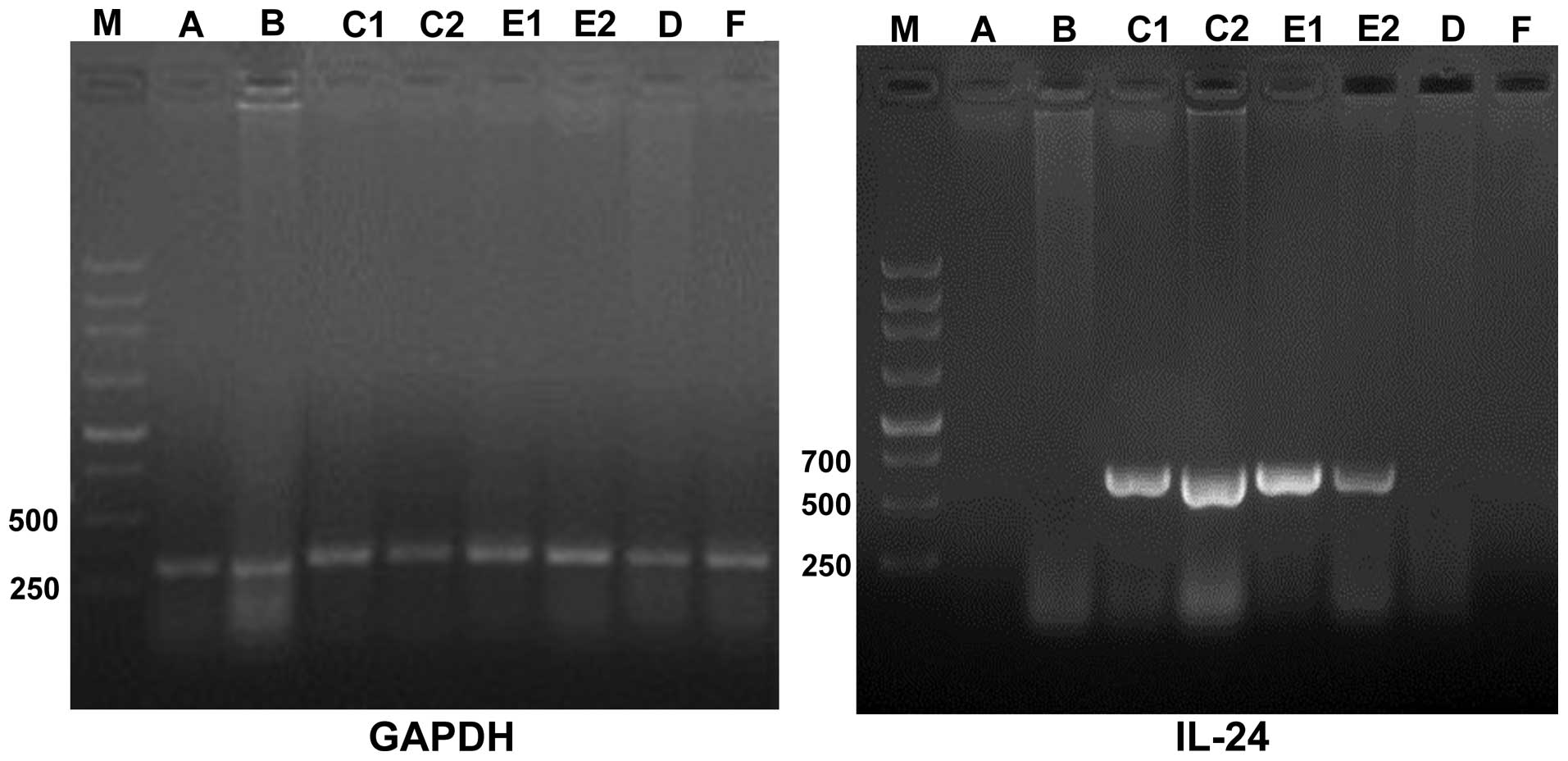 | Figure 1IL-24 gene transcription in
endothelial cells M, DNA marker; A, control group; B,
H2O2 group; C, H2O2 +
IL-24 group (C1 and C2 are double test groups); D,
H2O2 + empty plasmid group; E, IL-24 group
(E1 and E2 are double test groups); F, empty plasmid group. Each
sample shows the expression of the housekeeping gene, GAPDH, 307
bp, indicating that cDNA extraction was complete. Transfection of
IL-24, amplified 620 bp bands, indicating that IL-24 was
successfully transfected into the cells and was expressed in
vascular endothelial cells. IL-24, interleukin-24; GAPDH,
glyceraldehyde 3-phosphate dehydrogenase. |
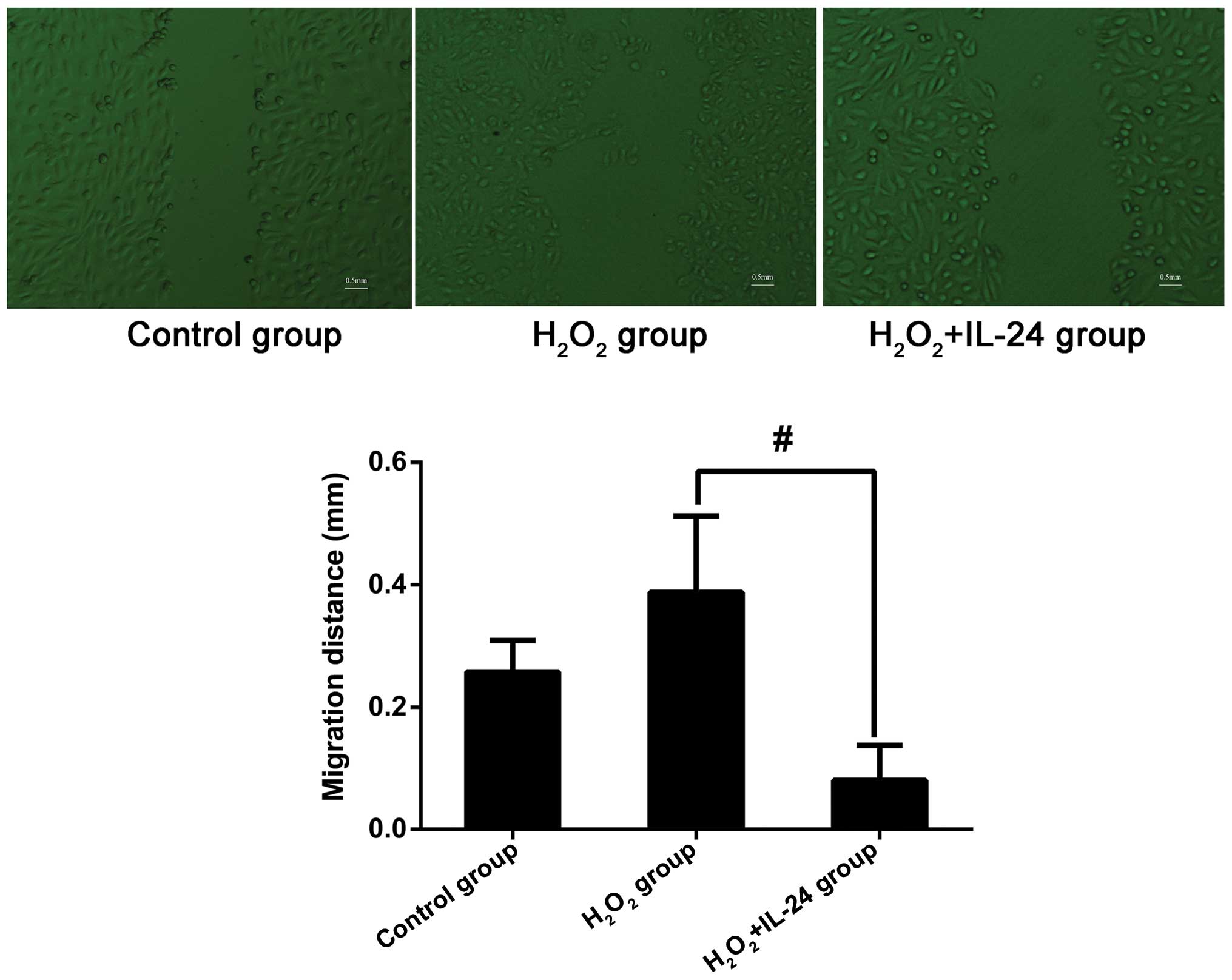
IL-24 attenuates the promoting effects of
H2O2 on endothelial cell proliferation
Low concentrations of H2O2
(0.1–0.15 mmol/l) can stimulate abnormal cell proliferation and
migration, which was determined in our pre-experiments. Compared
with the control group, following 24 h of exposure to
H2O2, cell proliferation and migration were
markedly increased in the H2O2 group compared
to the controls (controls, 0.2575±0.05123;
H2O2 group, 0.3875±0.01250 mm;
P=0.1026>0.05). We found that the overexpression of IL-24
significantly inhibited the H2O2-induced
proliferation of the HUVECs (0.0800±0.05715 mm;
H2O2 group compared with
H2O2 + IL-24 group; P=0.0042<0.05)
(Fig. 2).
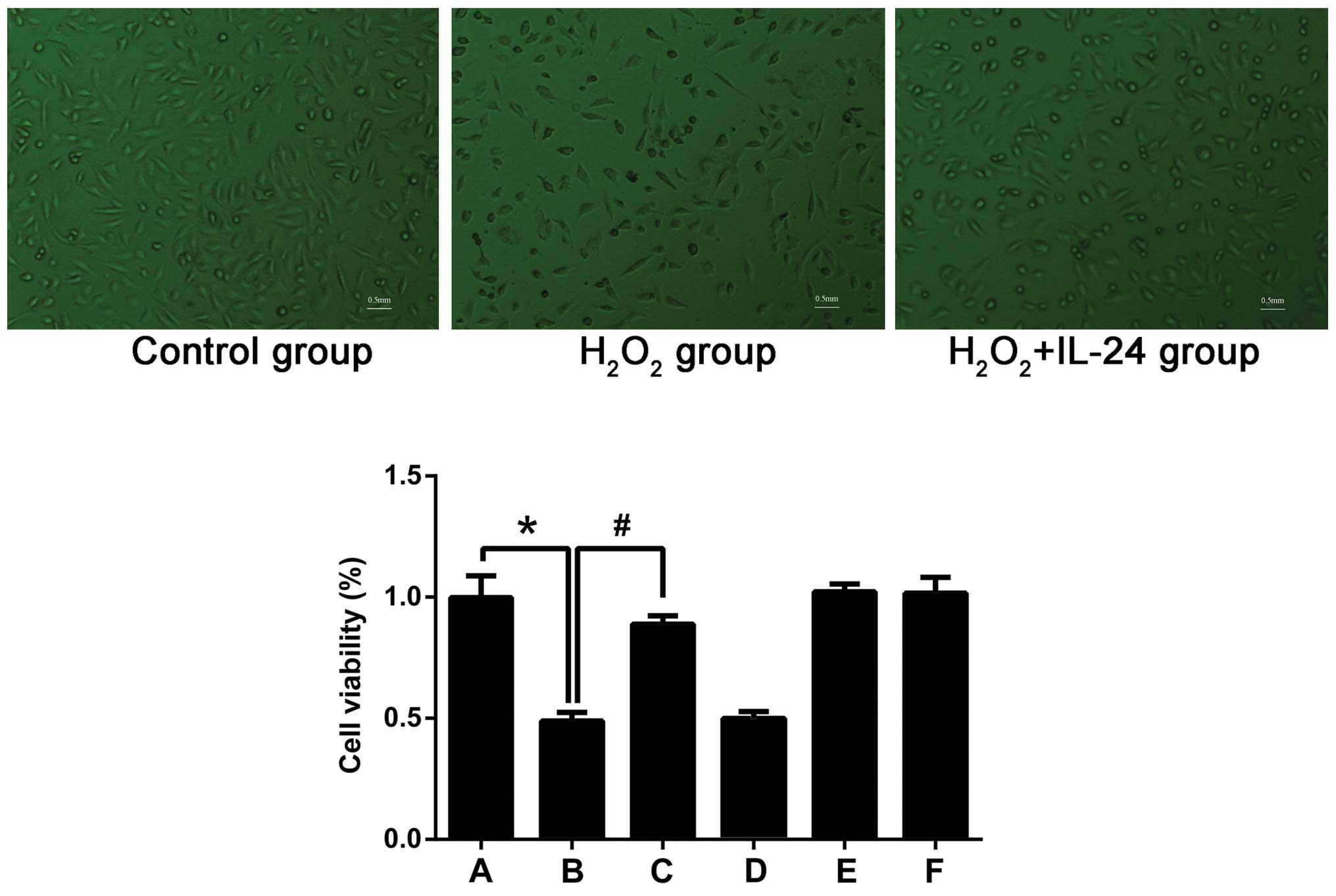
Cell viability determined by CCK-8
assay
IL-24 significantly decreased the apoptosis induced
by oxidative stress, thus improving the survival rate of the cells
(Fig. 3). Cell survival in the
H2O2 oxidative stress injury group was lowest
with a viability of 51±5.57% of the control group (P<0.001).
Cell injury due to oxidative stress was significantly attenuated by
IL-24, leading to an increase in cell viability to 81.66±4.81% of
the control group. The differences in cell viability between the
H2O2 and H2O2 + IL-24
groups were statistically significant (P=0.0019<0.05).
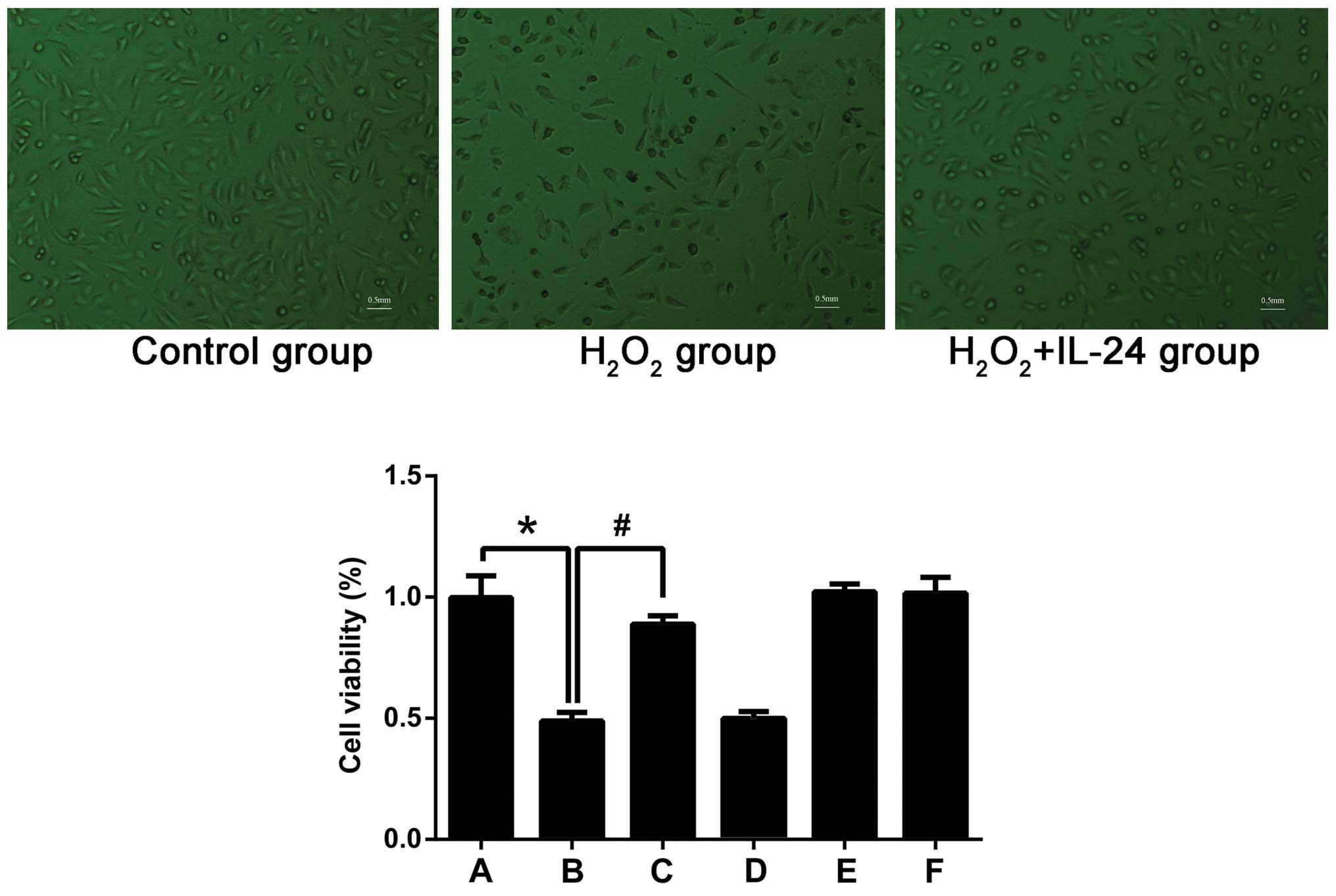 | Figure 3Cell viabitliy. A, control group; B,
H2O2 group; C, H2O2 +
IL-24 group; D, H2O2 + empty plasmid group;
E, IL-24 group; F, empty plasmid group. In the
H2O2 oxidative stress injury group
(H2O2, 0.3 mmol/l), the cell survival rate
was lowest; cell activity for this group was 51±5.57% of the
control group (*P<0.001). Cell injury due to oxidative stress
was significantly reduced by IL-24; the cell survival rate was
significantly increased to 81.66±4.81% of the control group. There
was a significant difference between the H2O2
injury group and the H2O2 + IL-24 group
(#P=0.0019<0.05). Magnification, ×40. Bar, 0.5 mm.
IL-24, interleukin-24. |
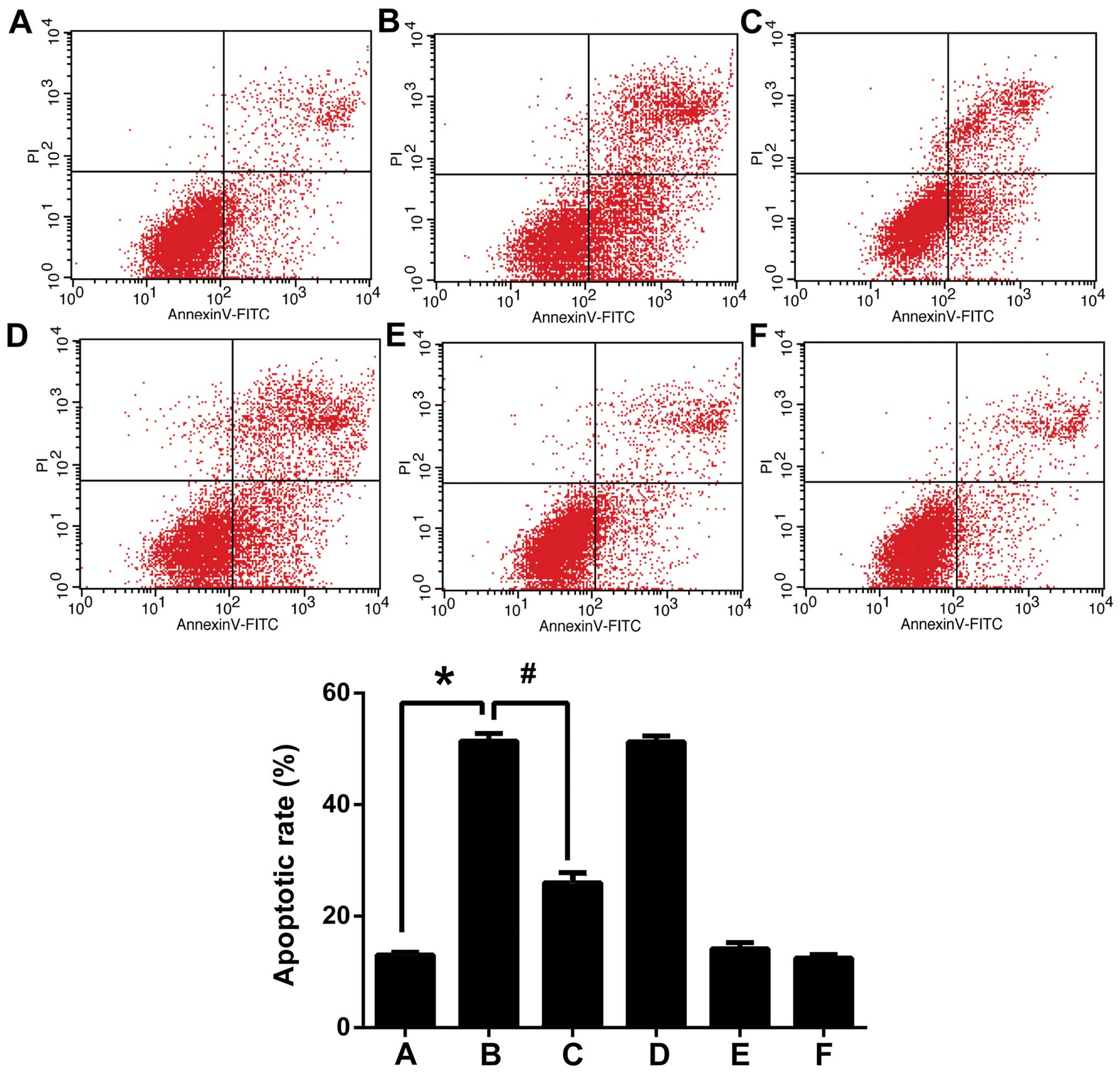
Cell apoptosis measured by flow
cytometry
The amount of apoptosis induced by
H2O2 was significantly higher than the basal
level of apoptosis observed in the control group (51.38±1. 39 vs.
13.01±0.50%; P<0.001; Fig. 4).
IL-24 was able to protect the cells against
H2O2-induced apoptosis (51.38±1.39% in the
H2O2 group compared to 25.93±1.902% in the
H2O2 + IL-24 group; P<0.001).
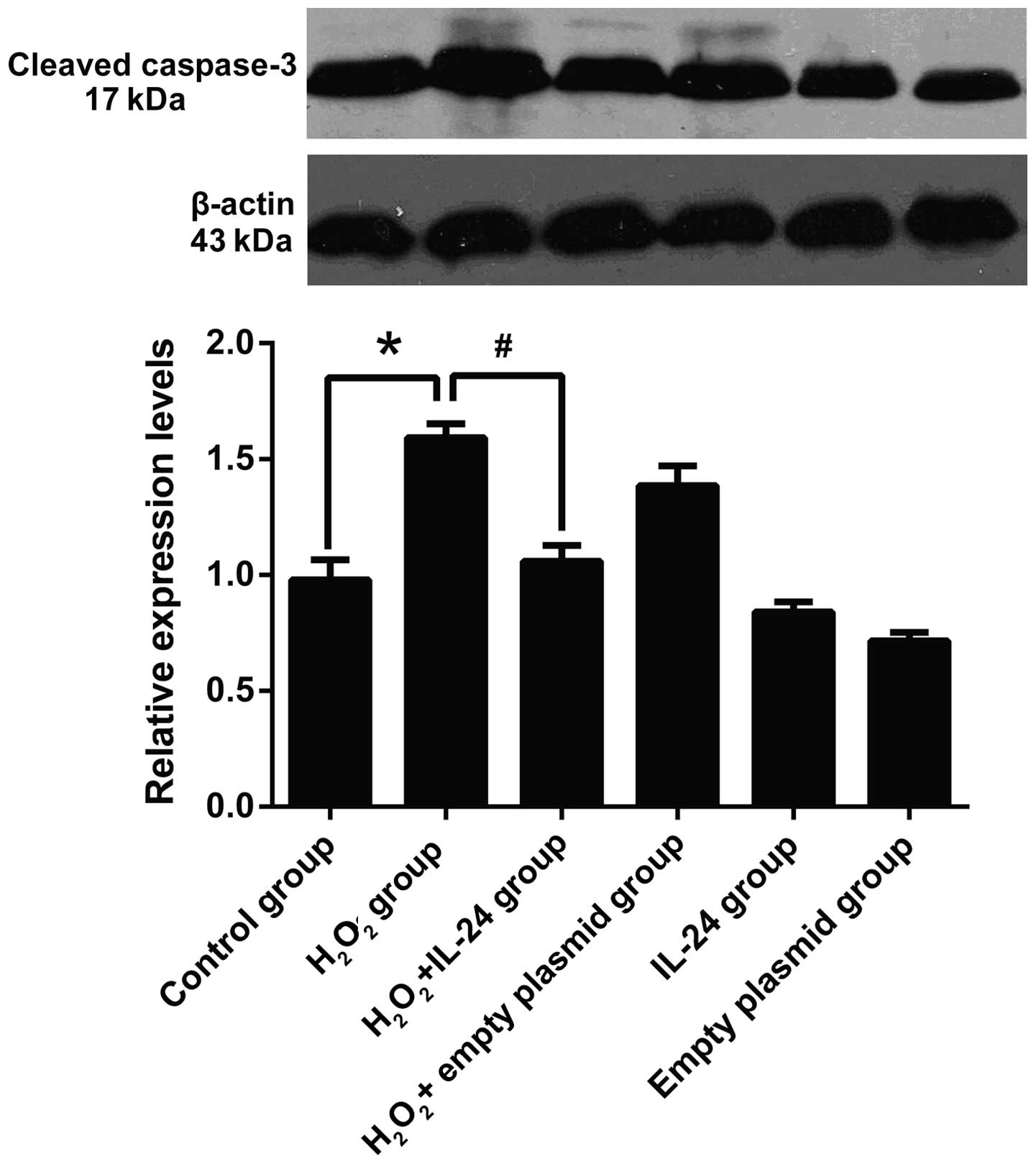
Cleaved caspase-3 expression determined
by western blot analysis
H2O2 can significantly induced
the activation and expression of caspase-3, while this effect was
attenuated in H2O2 + IL-24 group. There were
significant differences between the control group and the
H2O2 group (control group, 0.98±0.086;
H2O2 group, 1.59±0.061; P<0.001). The
difference between the H2O2 group and the
H2O2 + IL-24 group was statistically
significant. The mean values were 1.59±0.061, 1.06±0.067,
respectively (P<0.001; Fig.
5).
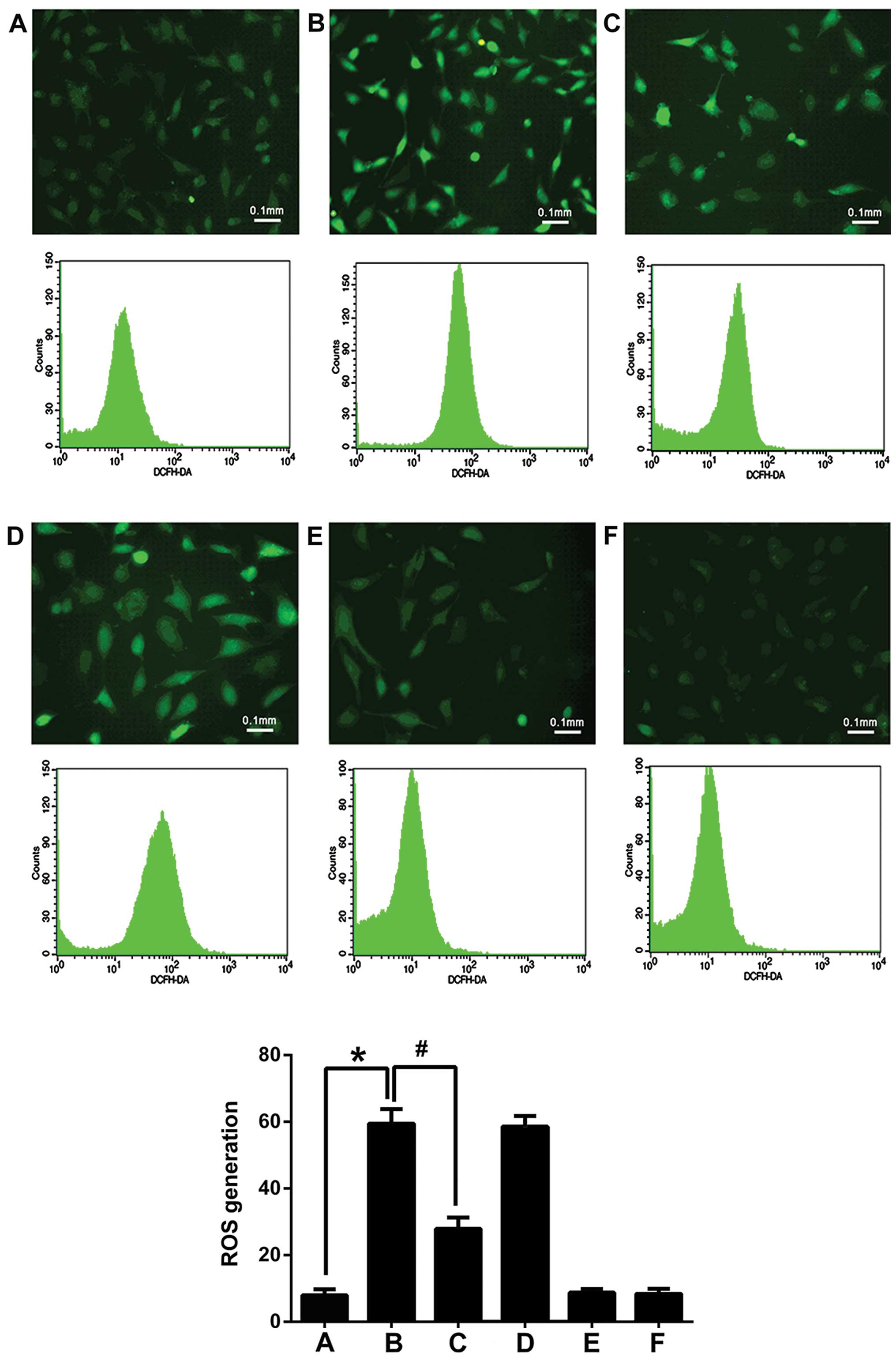
Flow cytometry to measure ROS production
in HUVECs
The quantitative detection of ROS production in each
treatment group was performed (Fig.
6). The ROS content in the the H2O2 group
was significantly higher than in any other group. The difference
between the control group and the H2O2 +
IL-24 group was statistically significant. The mean values of the
ROS content in the H2O2, control and
H2O2 + IL-24 groups were 59.43±4.39,
7.97±1.78 and 27.92±3.35, respectively (P<0.001). Taken
together, these results indicate that IL-24 decreases cellular ROS
levels induced by H2O2, thus reducing damage
induced by oxidative stress.
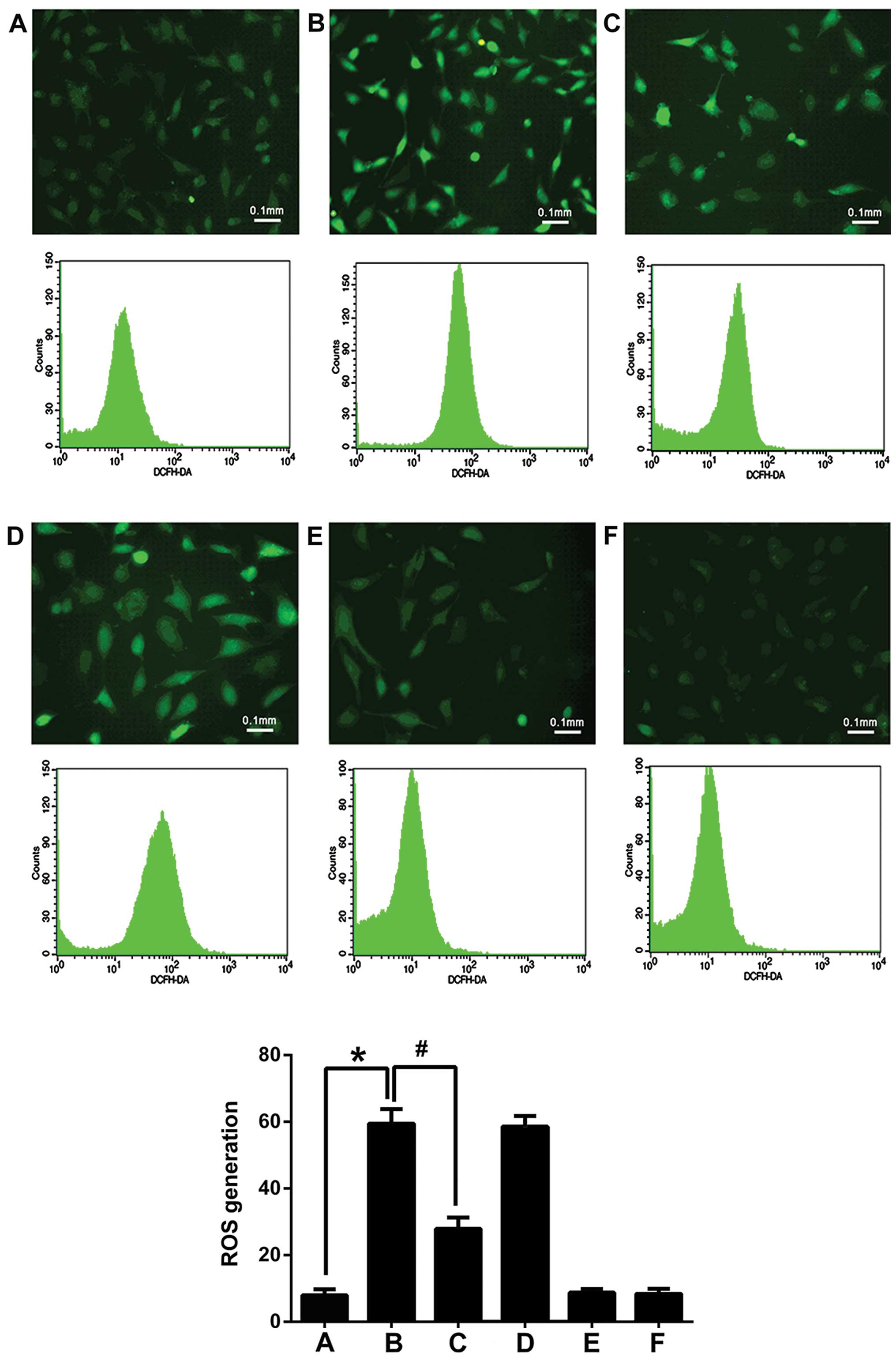 | Figure 6ROS generation. A, control group; B,
H2O2 group; C, H2O2 +
IL-24 group; D, H2O2 + empty plasmid group;
E, IL-24 group; F, empty plasmid group. The ROS content in the
H2O2 group was significantly higher than the
other groups; the difference between the control group and the
H2O2 + IL-24 group was statistically
significant. Mean values were 59.43±4.39, 7.97±1.78 and 27.92±3.35,
respectively (*,#P<0.001). Fluorescence images show
that H2O2 damage causes an increase in
intracellular ROS generation, while IL-24 attenuates this effect.
Magnification, ×100. Bar, 0.1 mm. IL-24, interleukin-24. |
ROS activity in HUVECs detected by
fluorescence microscopy
The overexpressio of IL-24 attenuated the
H2O2-inducd increase in the intracellular ROS
levels. The ROS levels were qualitatively observed by fluorescence
microscopy (Fig. 6).
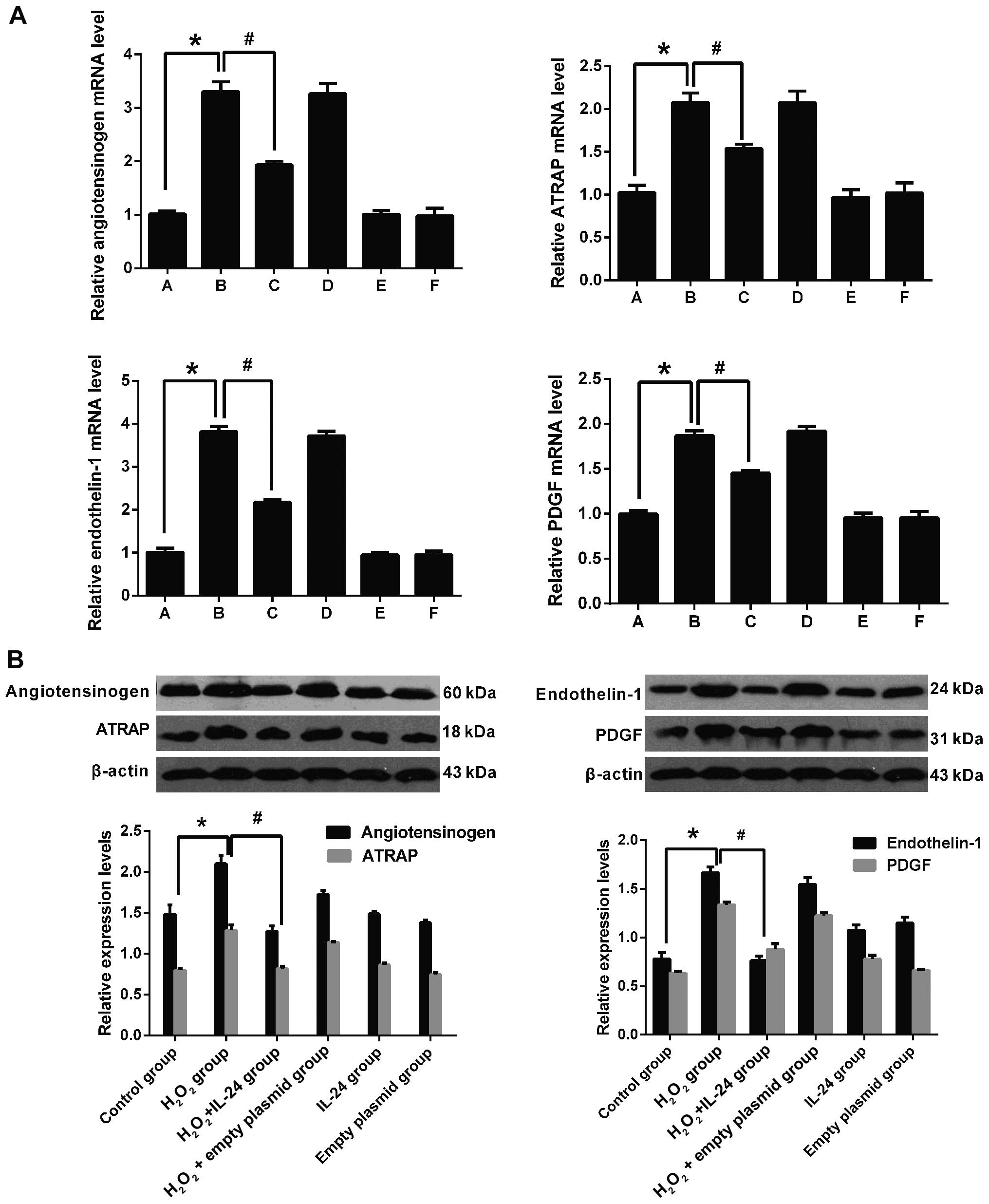
mRNA expression of cardiovascular
disease-related factors
Real-time PCR was performed to assess the levels of
angiotensinogen, endothelin-1, ATRAP and PDGF. The exposure of the
HUVECs to H2O2 significantly increased the
mRNA expression of each of these cardiovascular disease-related
factors (P<0.001). Importantly, IL-24 attenuated the increase in
the levels of these factors (P<0.001; Fig. 7A).
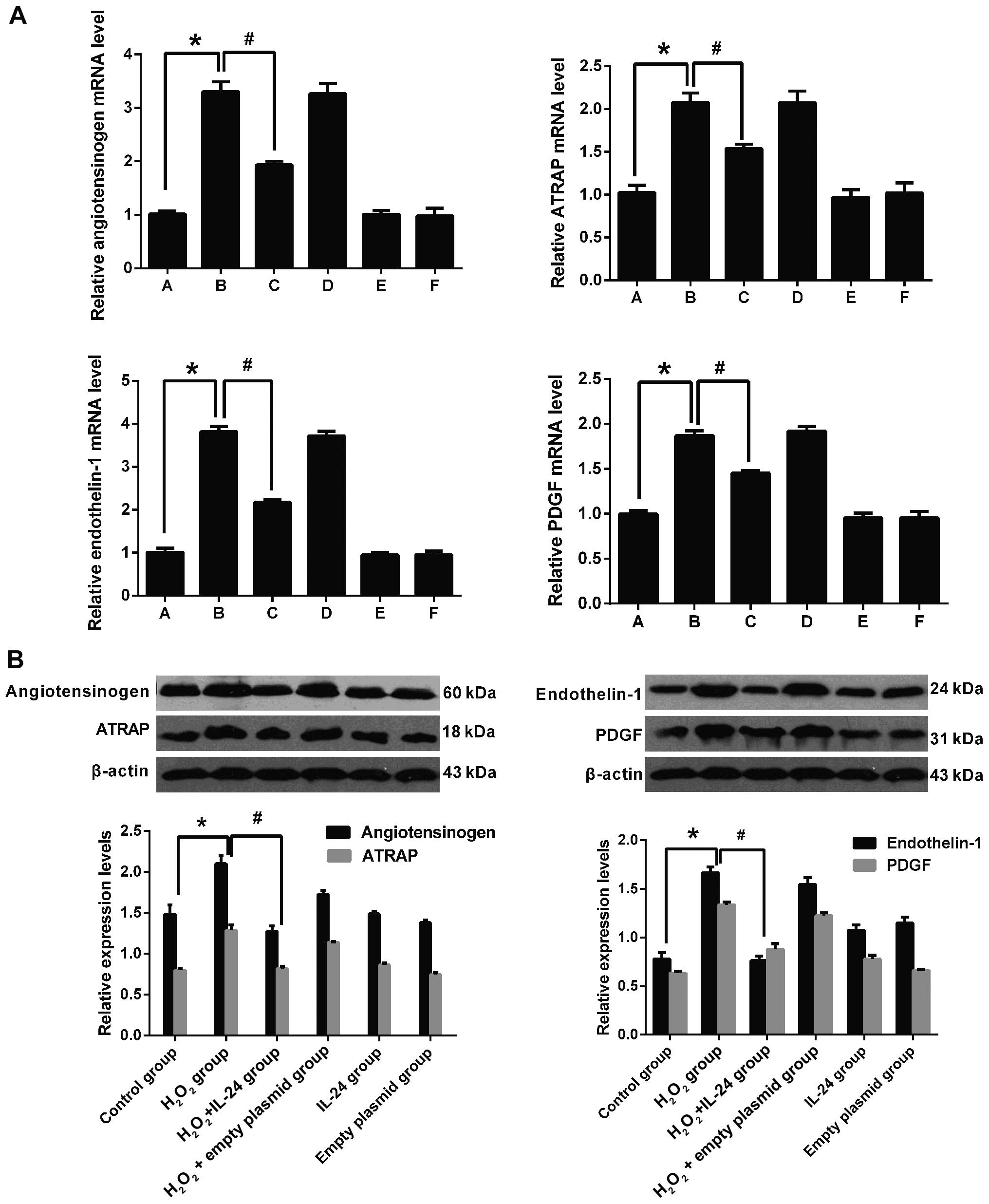 | Figure 7(A) H2O2
significantly stimulated the mRNA expression of cardiovascular
disease-related factors in HUVECs (*P<0.001). IL-24
attenuated this affect (#P<0.001). (B) Oxidative
stress induced by H2O2 damage induced the
upregulation of vascular disease-associated protein expression in
HUVECs compared with the control group. Compared with the control
group, the relative expression of angiotensinogen, endothelin-1,
ATRAP and PDGF in the H2O2 group was
2.10±0.097/1.48±0.112, 1.66±0.063/0.78±0.065, 1.28±0.068/0.80±0.023
and 1.33±0.031/0.63±0.020, respectively (*P<0.001).
Differences in protein expression in the H2O2
+ IL-24 group compared with the H2O2 group
were as follows: angiotensinogen (1.28±0.064/2.10±0.097),
endothelin-1 (0.76±0.046/1.66±0.063), ATRAP (0.82±0.027/1.28±0.068)
and PDGF (0.88±0.058/1.33±0.031) (#P<0.001); all
proteins normalized to β-actin. HUVECs, human umbilical vein
endothelial cells; ATRAP, angiotensin II type 1 receptor-associated
protein; PDGF, platelet-derived growth factor; IL-24,
interleukin-24. |
Protein expression of cardiovascular
disease-related factors
Western blot analysis was performed to measure the
protein expression of angiotensinogen, endothelin-1, ATRAP and
PDGF. Consistent with the results observed at the mRNA level,
oxidative stress induced by H2O2-induced
damage increased expression of these cardiovascular
disease-associated factors at the protein level as well. Compared
with the control group, each protein was normalized to the levels
of β-actin, and the relative expression of angiotensinogen,
endo-thelin-1, ATRAP and PDGF was 2.10±0.097/1.48±0.112,
1.66±0.063/0.78±0.065, 1.28±0.068/0.80±0.023 and
1.33±0.031/0.63±0.020, respectively (P<0.001). Compared with the
H2O2 group, the relative expression of
angiotensinogen, endothelin-1, ATRAP and PDGF in the
H2O2 + IL-24 group was 1.28±0.064/2.10±0.097,
0.76±0.046/1.66±0.063, 0.82±0.027/1.28±0.068 and
0.88±0.058/1.33±0.031, respectively (P<0.001). Taken together,
our results revealed that IL-24 significantly decreased the
expression of cardiovascular disease-related proteins (Fig. 7B).
Successful establishment of the rat model
of hypertension
The blood pressure of the normal rats was generally
90–115/67–90 mmHg. Blood pressure was measured at the second day
following the infusion of angiotensin II, and blood pressure began
to rise thereafter. As shown by continuous monitoring for 7 days,
blood pressure was significantly elevated (P<0.05), which shows
that the model of hypertension was successfully established. Blood
pressure in the control group was 91.72±4.89 mmHg, whereas blood
pressure in the hypertension group was 147.35±9.58 mmHg (Table III).
 | Table IIIComparison of systolic blood pressure
(SBP, mmHg). |
Table III
Comparison of systolic blood pressure
(SBP, mmHg).
| Group | N | Pre-angiotensin II
administration | Post-angiotensin II
administration |
|---|
| Control group | 12 | 90.87±4.76 | 91.23±4.85a |
| Hypertensive
group | 24 | 91.72±4.89b |
147.35±9.58a,b |
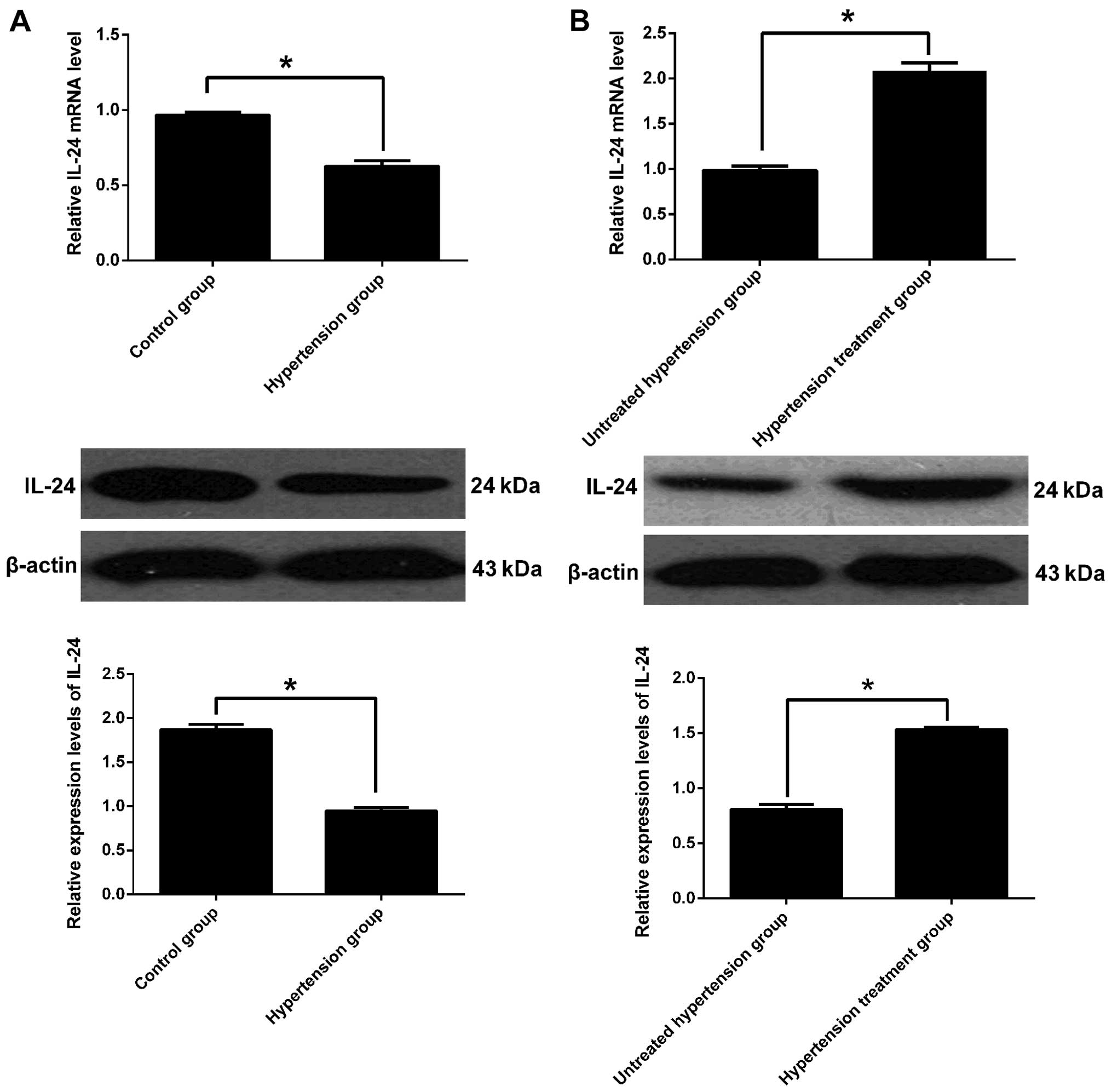
IL-24 mRNA levels in heart and kidney
tissue
The transcript levels of IL-24 in the heart and
kidney tissue from both the control and hypertensive rats were
measured by real-time PCR. The effects of anti-hypertensive therapy
were also examined. Compared to the rats in the control group, the
IL-24 transcript levels were significantly decreased in the heart
and kidney tissue from the hypertensive rats (Fig. 8A, top panel). Following
anti-hypertensive therapy, the expression of IL-24 was
significantly increased compared to the untreated group
(P<0.001; Fig. 8B, top
panel).
IL-24 protein levels in heart and kidney
tissue
IL-24 protein expression was significantly lower in
the hypertensive rats compared to the control rats. The relative
expression of IL-24 in the hypertension group, normalized to
β-actin, was 0.95±0.041/1.87±0.062 (P<0.001; Fig. 8A, bottom panel). Anti-hypertensive
therapy increased IL-24 protein expression; the relative expression
in this setting was 1.54±0.014/0.81±0.042 (P<0.001; Fig. 8B, bottom panel). Taken together,
our data indicate that IL-24 expression is closely associated with
hypertension.
Discussion
ROS play an important role in the pathophysiology of
cardiovascular diseases, such as hyperlipidemia, hypertension,
ischemic heart disease and chronic heart failure (27). Exogenous
H2O2 activates the NAD(P)H oxidase-induced
cell production of endogenous H2O2 (27). Intracellular ROS, such as
superoxide oxygen ion (O2−),
H2O2, and hydroxyl radical (OH−),
are associated with the pathogenesis of a number of diseases, such
as cardiovascular diseases, including hypertension, heart failure
and atherosclerosis, as well as diabetes (28). ROS can cause damage to blood
vessel walls; in turn, vascular wall damage can induce changes in
the expression of genes associated with cardiovascular diseases
(29,30). These genes can stimulate VSMC
migration and proliferation, and vascular intima hyperplasia, which
lead to the development of cardiovascular disease (31–34).
Methods to reduce and prevent these
pathophysiological processes include drug therapy and gene therapy.
Compared to drug treatment, gene therapy has the advantage of
promoting long-term efficacy with no systemic toxicity (19). Studies have demonstrated that
several growth regulatory genes, such as nitric oxide (NO)
synthase, Rb and p53 may play a role in preventing neointima
formation both in vitro and in vivo (35,36). However, the mechanisms through
which these pathophysiological processes can be prevented are still
unclear. Theoretically speaking, interfering with multiple
biological processes, such as migration, proliferation and
apoptosis, should provide the best efficacy. Along these lines,
IL-24 has emerged as a promising candidate.
Toxins, such as cigarette smoke or a high-fat diet,
can induce molecular pathways that are common to both
cardiovascular disease and cancer; such pathways result in
oxidative stress and cell damage. Atherosclerosis may arise from
the damage or infection of a single arterial smooth muscle cell; in
a similar manner, a tumor may arise from an acquired mutation
within a single cell. Regulators of cell proliferation, commonly
implicated in cancer, are also involved in the progression of
atherosclerosis, vascular stenosis, and vascular restenosis after
angioplasty. Likewise, cell adhesion molecules are closely related
to both the formation of plaques and thrombus and to tumor invasion
and metastasis (11,37,38).
Considering the common pathogenesis of cancer and
cardiovascular disease (38),
some researchers have suggested that IL-24 may play a potential
therapeutic role in the treatment of cardiovascular diseases, such
as atherosclerosis, arterial disease following organ transplants,
hypertension and post-operative valve restenosis (39,40). Chen et al found that IL-24
inhibited the growth of PAC1 cells, a rat pulmonary artery smooth
muscle cell line, through an intracellular pathway, while having no
effect on normal primary human coronary artery cells or rat aortic
smooth muscle cells (41). Ramesh
et al found that IL-24 inhibited the formation of two cell
capillary structure of cultured HUVECs and human vein endothelial
cells in a dose-dependent manner (42). Their study also demonstrated that
the anti-angiogenic effects of IL-24 were more prominent than the
effects of endostatin. Transwell migration assays revealed that
IL-24 significantly inhibited vascular endothelial growth factor
(VEGF)-induced HUVEC migration (42). Vascular calcification is an
important marker of cardiovascular disease. In a previous study,
the rat model of β-glycerophosphate (β-GP)-induced VSMC
calcification model was confirmed by Von Kossa staining and the
detection of the calcium content; the authors showed that IL-24
significantly inhibited the calcification of VSMCs in this model
(43). IL-24 inhibited
calcification, osteogenic cell marker expression and apoptosis
induced by β-GP. It also blocked the activation of the
Wnt/β-catenin signaling pathway, thereby inhibiting vascular
calcification. This research suggested that IL-24 may be a
potential therapeutic agent in the calcification of VSMCs. Beides
this, another study demonstrated that IL-24 suppressed the growth
of normal VSMCs by inhibiting H2O2-induced
ROS production through the regulation of mitochondrial ROS
production and the expression of antioxidant enzymes (44). In a recent study, the researchers
found that IL-24 polymorphisms were associated with cardiometabolic
parameters and cardiovascular risk factors (45). These results indicate that IL-24
plays an important role in cardiovascular disease.
In a previous study, IL-24 was demonstrated to
inhibit tumor cell growth and blood vessel formation; it also
induces tumor cell apoptosis and stimulates the expression of
several cytokine genes (46).
In recent years, much attentation has been paid to
obtaining a better understanding of the association between
endothelial cell dysfunction and hypertension. Some groups have
suggested that endothelial cell injury is a result of hypertension
(47). In contrast, others have
proposed that endothelial cell dysfunction is an important risk
factor for hypertension, and not merely the result of hypertension
(48).
Burdon and Gill demonstrated that
H2O2, along with a superoxide anion, play a
'contact information' role, so as to maintain a normal life state
of cells (25). ROS, such as
H2O2, promote the proliferation of both
cancer cells and normal cells in the body, including VSMCs and
vascular endothelial cells. IL-24 has been shown to significantly
inhibit cell proliferation in some studies (49–51). In this study, we demonstrated that
IL-24 inhibited the abnormal proliferation of vascular endothelial
cells induced by H2O2, a regulator of cell
proliferation involved in the progression of atherosclerotic
plaques, vascular stenosis, vascular restenosis following
angioplasty and cancer. As such, IL-24 may play a role in the
treatment of occlusive vascular disease through this mechanism.
H2O2 is the intermediate
product of oxidative metabolism in the body, and it can easily
permeate the cell membrane. If the intracellular levels of
H2O2 accumulate to toxic levels, it can have
dire consequences for vascular endothelial cells and myocardial
cells. H2O2 at 0.3 mmol/l can stimulate
intracellular ROS production, causing oxidative stress damage and
resulting in cellular injury, apoptosis and death (52–54). In this study, we demonstrated that
IL-24 significantly attenuated H2O2-induced
cell apoptosis. IL-24 intervention significantly reduced the
protein expression of cleaved caspase-3. Caspase-3 is one of the
most key executioners in the process of apoptosis, and the
activation of caspase-3 is often used as an important indicator of
apoptosis. Importantly, IL-24 may reduce apoptosis by reducing the
content of intracellular ROS. Taken together, our data indicate
that IL-24 is an effective protective agent and therapeutic target
for vascular endothelial cells and for the vascular system in
general.
Several genes, including angiotensinogen,
endothelin-1, ATRAP and PDGF are closely related to the
pathogenesis of cardiovascular disease (31–34). We found that exposure of the
HUVECs to H2O2 increased the expression of
these genes, and may thus contribute to the development of
hypertension. Importantly, we demonstrated that the ectopic
overexpression of IL-24 significantly reduced the expression levels
of these genes, indicating that IL-24 may reduce the incidence of
hypertension by affecting the expression of related genes.
In this study, we also examined the effects of
H2O2 and IL-24 in an in vivo rat model
of hypertension. We found that IL-24 expression was significantly
reduced in the tissues of hypertensive rats compared to the healthy
controls. Additionally, we found that treatment with
anti-hypertensive drugs increased the IL-24 levels. These data
suggest that IL-24 may be clinically useful.
In conclusion, our data demonstrate that IL-24
inhibits the the abnormal proliferation of vascular endothelial
cells induced by low concentrations of H2O2.
It also inhibits apoptosis via the inhibition of ROS production in
vascular endothelial cells. IL-24 can also downregulate the
expression of several cardiovascular disease-related genes.
Considering the common molecular mechanisms underlying the
pathogenesis of cancer and cardiovascular disease, and given that
IL-24 inhibits ROS production, IL-24 may provide a basic
therapeutic strategy for the treatment of vascular disease and
cancer caused by ROS overproduction.
References
|
1
|
Cohuet G and Struijker-Boudier H:
Mechanisms of target organ damage caused by hypertension:
Therapeutic potential. Pharmacol Ther. 111:81–98. 2006. View Article : Google Scholar
|
|
2
|
Lugo-Baruqui A, Munoz-Valle JF,
Arevalo-Gallegos S and Armendariz-Borunda J: Role of angiotensin II
in liver fibrosis-induced portal hypertension and therapeutic
implications. Hepatol Res. 40:95–104. 2010. View Article : Google Scholar
|
|
3
|
Mansia G, De Backer G, Dominiczak A,
Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE,
Laurent S, et al: European Society of Cardiology: 2007 ESH-ESC
Guidelines for the management of arterial hypertension: The task
force for the management of arterial hypertension of the European
Society of Hypertension (ESH) and of the European Society of
Cardiology (ESC). Blood Press. 16:135–232. 2007. View Article : Google Scholar
|
|
4
|
Okuda T, Sumiya T, Mizutani K, Tago N,
Miyata T, Tanabe T, Kato H, Katsuya T, Higaki J, Ogihara T, et al:
Analyses of differential gene expression in genetic hypertensive
rats by microarray. Hypertens Res. 25:249–255. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Yono M, Yoshida M, Yamamoto Y, Imanishi A,
Fukagawa A, Latifpour J and Eto M: Identification of potential
therapeutic targets in hypertension-associated bladder dysfunction.
BJU Int. 105:877–883. 2010. View Article : Google Scholar
|
|
6
|
Lee KM, Kang HA, Ko CB, Oh EH, Park M, Lee
HY, Choi HR, Yun CH, Jung WW, Oh JW and Kang HS: Differential gene
expression profiles in spontaneously hypertensive rats induced by
administration of enalapril and nifedipine. Int J Mol Med.
31:179–187. 2013.
|
|
7
|
Jiang H, Su ZZ, Lin JJ, Goldstein NI,
Young CS and Fisher PB: The melanoma differentiation associated
gene mda-7 suppresses cancer cell growth. Proc Natl Acad Sci USA.
93:9160–9165. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Caudell EG, Mumm JB, Poindexter N,
Ekmekcioglu S, Mhashilkar AM, Yang XH, Retter MW, Hill P, Chada S
and Grimm EA: The protein product of the tumor suppressor gene,
melanoma differentiation-associated gene 7, exhibits
immunostimulatory activity and is designated IL-24. J Immunol.
168:6041–6046. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Saeki T, Mhashilkar A, Swanson X, Zou-Yang
XH, Sieger K, Kawabe S, Branch CD, Zumstein L, Meyn RE, Roth JA, et
al: Inhibition of human lung cancer growth following
adenovirus-mediated mda-7 gene expression in vivo. Oncogene.
21:4558–4566. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ellerhorst JA, Prieto VG, Ekmekcioglu S,
Broemeling L, Yekell S, Chada S and Grimm EA: Loss of MDA-7
expression with progression of melanoma. J Clin Oncol.
20:1069–1074. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ross JS, Stagliano NE, Donovan MJ,
Breitbart RE and Ginsburg GS: Atherosclerosis: A cancer of the
blood vessels? Am J Clin Pathol. 116(Suppl): S97–S107. 2001.
|
|
12
|
Menezes ME, Shen XN, Das SK, Emdad L, Guo
C, Yuan F, Li YJ, Archer MC, Zacksenhaus E, Windle JJ, et al:
MDA-7/IL-24 functions as a tumor suppressor gene in vivo in
transgenic mouse models of breast cancer. Oncotarget.
6:36928–36942. 2015.PubMed/NCBI
|
|
13
|
Lin C, Liu H, Li L, Zhu Q, Liu H, Ji Z,
Liao J, Lang J, Wu J and Fan J: MDA-7/IL-24 inhibits cell survival
by inducing apoptosis in nasopharyngeal carcinoma. Int J Clin Exp
Med. 7:4082–4090. 2014.
|
|
14
|
Menezes ME, Bhatia S, Bhoopathi P, Das SK,
Emdad L, Dasgupta S, Dent P, Wang XY, Sarkar D and Fisher PB:
MDA-7/IL-24: multifunctional cancer killing cytokine. Adv Exp Med
Biol. 818:127–153. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Fliss H and Gattinger D: Apoptosis in
ischemic and reperfused rat myocardium. Circ Res. 79:949–956. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hampton MB and Orrenius S: Redox
regulation of apoptotic cell death. Biofactors. 8:1–5. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ying W: Deleterious network hypothesis of
apoptosis. Med Hypotheses. 50:393–398. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Puddu P, Puddu GM, Zaca F and Muscari A:
Endothelial dysfunction in hypertension. Acta Cardiol. 55:221–232.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Chang MW, Barr E, Seltzer J, Jiang YQ,
Nabel GJ, Nabel EG, Parmacek MS and Leiden JM: Cytostatic gene
therapy for vascular proliferative disorders with a constitutively
active form of the retinoblastoma gene product. Science.
267:518–522. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ascher E, Scheinman M, Hingorani A, Seth
P, Marella VK and Jacob T: Effect of p53 gene therapy combined with
CTLA4Ig selective immunosuppression on prolonged neointima
formation reduction in a rat model. Ann Vasc Surg. 14:385–392.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Chang MW, Barr E, Lu MM, Barton K and
Leiden JM: Adenovirus-mediated over-expression of the
cyclin/cyclin-dependent kinase inhibitor, p21 inhibits vascular
smooth muscle cell proliferation and neointima formation in the rat
carotid artery model of balloon angioplasty. J Clin Invest.
96:2260–2268. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Huang J and Kontos CD: Inhibition of
vascular smooth muscle cell proliferation, migration, and survival
by the tumor suppressor protein PTEN. Arterioscler Thromb Vasc
Biol. 22:745–751. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Xue B, Pamidimukkala J and Hay M: Sex
differences in the development of angiotensin II-induced
hypertension in conscious mice. Am J Physiol Heart Circ Physiol.
288:H2177–H2184. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Rugale C, Delbosc S, Cristol JP, Mimran A
and Jover B: Sodium restriction prevents cardiac hypertrophy and
oxidative stress in angiotensin II hypertension. Am J Physiol Heart
Circ Physiol. 284:H1744–H1750. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Burdon RH and Gill V: Cellularly generated
active oxygen species and HeLa cell proliferation. Free Radic Res
Commun. 19:203–213. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Pfaffl MW: A new mathematical model for
relative quantification in real-time RT-PCR. Nucleic Acids Res.
29:e452001. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Rao GN and Berk BC: Active oxygen species
stimulate vascular smooth muscle cell growth and proto-oncogene
expression. Circ Res. 70:593–599. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Touyz RM and Schiffrin EL: Reactive oxygen
species in vascular biology: Implications in hypertension.
Histochem Cell Biol. 122:339–352. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Ruef J, Hu ZY, Yin LY, Wu Y, Hanson SR,
Kelly AB, Harker LA, Rao GN, Runge MS and Patterson C: Induction of
vascular endothelial growth factor in balloon-injured baboon
arteries. A novel role for reactive oxygen species in
atherosclerosis. Circ Res. 81:24–33. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Chua CC, Hamdy RC and Chua BH:
Upregulation of vascular endothelial growth factor by
H2O2 in rat heart endothelial cells. Free
Radic Biol Med. 25:891–897. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Verdonk K, Saleh L, Lankhorst S, Smilde
JE, van Ingen MM, Garrelds IM, Friesema EC, Russcher H, van den
Meiracker AH, Visser W and Danser AH: Association studies suggest a
key role for endothelin-1 in the pathogenesis of preeclampsia and
the accompanying renin-angiotensin-aldosterone system suppression.
Hypertension. 65:1316–1323. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Puddu P, Puddu GM, Cravero E, Ferrari E
and Muscari A: The genetic basis of essential hypertension. Acta
Cardiol. 62:281–293. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Hollenberg NK: Genes, hypertension, and
intermediate phenotypes. Curr Opin Cardiol. 11:457–463. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Zou Y, Hu Y, Metzler B and Xu Q: Signal
transduction in arterio-sclerosis: mechanical stress-activated MAP
kinases in vascular smooth muscle cells (review). Int J Mol Med.
1:827–834. 1998.PubMed/NCBI
|
|
35
|
von der Leyen HE, Gibbons GH, Morishita R,
Lewis NP, Zhang L, Nakajima M, Kaneda Y, Cooke JP and Dzau VJ: Gene
therapy inhibiting neointimal vascular lesion: In vivo transfer of
endothelial cell nitric oxide synthase gene. Proc Natl Acad Sci
USA. 92:1137–1141. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Yonemitsu Y, Kaneda Y, Tanaka S, Nakashima
Y, Komori K, Sugimachi K and Sueishi K: Transfer of wild-type p53
gene effectively inhibits vascular smooth muscle cell proliferation
in vitro and in vivo. Circ Res. 82:147–156. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Markowitz SD: Atherosclerosis, just
another cancer? J Clin Invest. 100:2143–2145. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Ross JS, Stagliano NE, Donovan MJ,
Breitbart RE and Ginsburg GS: Atherosclerosis and cancer: common
molecular pathways of disease development and progression. Ann N Y
Acad Sci. 947:271–292; discussion 292–273. 2001. View Article : Google Scholar
|
|
39
|
Schwartz SM, deBlois D and O'Brien ER: The
intima. Soil for atherosclerosis and restenosis. Circ Res.
77:445–465. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Davies MG and Hagen PO: Pathobiology of
intimal hyperplasia. Br J Surg. 81:1254–1269. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Chen J, Chada S, Mhashilkar A and Miano
JM: Tumor suppressor MDA-7/IL-24 selectively inhibits vascular
smooth muscle cell growth and migration. Mol Ther. 8:220–229. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Ramesh R, Mhashilkar AM, Tanaka F, Saito
Y, Branch CD, Sieger K, Mumm JB, Stewart AL, Boquoi A, Dumoutier L,
et al: Melanoma differentiation-associated gene 7/interleukin
(IL)-24 is a novel ligand that regulates angiogenesis via the IL-22
receptor. Cancer Res. 63:5105–5113. 2003.PubMed/NCBI
|
|
43
|
Lee KM, Kang HA, Park M, Lee HY, Choi HR,
Yun CH, Oh JW and Kang HS: Interleukin-24 attenuates
β-glycerophosphate-induced calcification of vascular smooth muscle
cells by inhibiting apoptosis, the expression of calcification and
osteoblastic markers, and the Wnt/β-catenin pathway. Biochem
Biophys Res Commun. 428:50–55. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Lee KM, Kang HA, Park M, Lee HY, Song MJ,
Ko K, Oh JW and Kang HS: Interleukin-24 suppresses the growth of
vascular smooth muscle cells by inhibiting H(2)O(2)-induced
reactive oxygen species production. Pharmacology. 90:332–341. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Vargas-Alarcon G, Posadas-Romero C,
Villarreal-Molina T, Alvarez-León E, Angeles-Martinez J,
Posadas-Sanchez R, Monroy-Muñoz I, Luna-Fuentes S, González-Salazar
C, Ramirez-Bello J, et al: IL-24 gene polymorphisms are associated
with cardiometabolic parameters and cardiovascular risk factors but
not with premature coronary artery disease: the genetics of
atherosclerotic disease Mexican study. J Interferon Cytokine Res.
34:659–666. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Yacoub A, Mitchell C, Lister A, Lebedeva
IV, Sarkar D, Su ZZ, Sigmon C, McKinstry R, Ramakrishnan V, Qiao L,
et al: Melanoma differentiation-associated 7 (interleukin 24)
inhibits growth and enhances radiosensitivity of glioma cells in
vitro and in vivo. Clin Cancer Res. 9:3272–3281. 2003.PubMed/NCBI
|
|
47
|
Shimokawa H: Endothelial dysfunction in
hypertension. J Atheroscler Thromb. 4:118–127. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
McAllister AS, Atkinson AB, Johnston GD,
Hadden DR, Bell PM and McCance DR: Basal nitric oxide production is
impaired in offspring of patients with essential hypertension. Clin
Sci (Lond). 97:141–147. 1999. View Article : Google Scholar
|
|
49
|
Panneerselvam J, Jin J, Shanker M,
Lauderdale J, Bates J, Wang Q, Zhao YD, Archibald SJ, Hubin TJ and
Ramesh R: IL-24 inhibits lung cancer cell migration and invasion by
disrupting the SDF-1/CXCR4 signaling axis. PLoS One.
10:e01224392015. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Ma Q, Deng X, Jin B, Zhang Y, Luo D, Song
H, Wang P, Zhang C, Li X, Shi Y, et al: A novel human
interleukin-24 peptide created by computer-guided design
contributes to suppression of proliferation in esophageal squamous
cell carcinoma Eca-109 cells. Oncol Rep. 33:193–200. 2015.
|
|
51
|
Jiang G, Yang CS, Xu D, Sun C, Zheng JN,
Lei TC and Liu YQ: Potent anti-tumour activity of a novel
conditionally replicating adenovirus for melanoma via inhibition of
migration and invasion. Br J Cancer. 110:2496–2505. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Yang R, Hai C, Li R and Wu D:
Dose-response relationship between cell proliferation and hydrogen
peroxide. Carcinog Teratog Mutagen. 9:92–98. 1997.
|
|
53
|
Li L, Wei Y, Cai J, et al: Hydrogen
peroxide induced apoptosis in humanvascular endothelial cells in
vitro and expression of Caspase-3. Shaanxi Medical Journal.
37:960–961. 2008.
|
|
54
|
Chen QM, Tu VC, Wu Y and Bahl JJ: Hydrogen
peroxide dose dependent induction of cell death or hypertrophy in
cardio-myocytes. Arch Biochem Biophys. 373:242–248. 2000.
View Article : Google Scholar : PubMed/NCBI
|