Introduction
Bacterial pathogens can manipulate the cell survival
machinery of the host to establish infection by influencing the
host signaling pathways that converge on the mitochondria (1). Mitochondria have been identified as
the target of increasing numbers of bacterial products, which are
transferred to the cell during infection, a process that often
plays a crucial role in microbial pathogenesis (2). Bacterial small molecules have been
previously shown to alter mitochondrial function (3,4)
and induce apoptosis (5). In
addition, the bacterial cell-wall component lipopolysaccharide
(LPS) has been shown to promote apoptosis through oxidative stress
in host cells (6).
Oxidative stress can be induced by pathogens either
directly or indirectly through the induction of host inflammatory
mediators (7,8). A major cause of oxidative stress is
reactive oxygen species (ROS) generation in cells, which are a
by-product of energy production in the mitochondria (9,10).
The increased generation of ROS and changes in the redox
homeostasis have been described in the context of a number of
microbial infections (11–13),
and the failure to maintain an appropriate redox balance
contributes to microbial pathogenesis through alterations in
mitochondrial functions and the induction of apoptosis (14,15).
Apoptosis plays a critical role in tissue
homeostasis and regulates multiple physiological processes,
including immune responses, infection and reduces
inflammation-mediated tissue injury by removing damaged cells
(16). Apoptosis is initiated
through several processes: i) by the activation/stimulation of
death receptors, including Fas, tumor necrosis factor (TNF)-α
receptor I, and TNF-related apoptosis-inducing ligand receptors 1
and 2 (17); ii) by caspase
activation that is independent of death receptors (18); iii) or by mitochondrial factors,
such as apoptosis-inducing factor (AIF), which are independent of
caspase activation (18).
Increased apoptotic signals in the alveolar epithelium are related
to the presence of chronic infections in patients with cystic
fibrosis (CF) (19).
The opportunistic pathogen Pseudomonas
aeruginosa (PA) thrives in patients with CF, burns and/or
immunocompromised individuals (20,21) and utilizes cell-to-cell
communication systems, termed quorum sensing (QS) (22) to establish acute and chronic
infection (23–27). QS relies on the presence of
small-excreted molecules termed herein 'infochemicals', to
coordinate the concomitant expression of multiple virulence genes
(28). It has been reported that
PA QS-excreted infochemicals modulate the host innate immune
response (29,30). The PA-excreted info-chemical,
2-aminoacetophenone (2-AA), promotes phenotypic changes in the
pathogen that favor chronic infection (26,31) and dampens pathogen-induced
inflammation that in turn favors host tolerance to infection
(30). We have recently
demonstrated that 2-AA reduces energy metabolism, promotes
mitochondrial dysfunction and impairs muscle functions, which may
further favor chronic and persistent infections (32) and potentially induces oxidative
stress in skeletal muscle.
In this study, we used whole-genome expression and
ex vivo nuclear magnetic resonance (NMR) to examine the
effects of 2-AA on the oxidative response and apoptosis in skeletal
muscle. NMR spectroscopy can be used to determine mitochondrial
dysfunction and assess metabolic alterations in muscle (33,34). Furthermore, in vivo
microscopy can be used to determine the reduction in mitochondrial
membrane potential, which is a signature of mitochondrial
dysfunction and induces apoptosis. The results of the present study
demonstrated that the inhibition of genes involved in oxidative
homeostasis resulted in the accumulation of ROS and increased
apoptosis in skeletal muscle. Thus, 2-AA promotes mitochondrial
dysfunction and compromises normal skeletal muscle functions
(32) through the induction of
oxidative stress and apoptosis, thus promoting pathogenicity.
Materials and methods
Ethics statement
This study was carried out in strict accordance with
the recommendations of the Guide for the Care and Use of Laboratory
Animals of the National Institutes of Health. The study protocol
was approved by the Committee on the Ethics of Animal Experiments
at Massachusetts General Hospital (Boston, USA; permit nos.
2006N000093 and 2013N000034). All procedures were performed on mice
which had been anaesthetized with a combination of xylazine (12.5
mg/kg) and ketamine (125 mg/kg), and every effort was made to
minimize suffering.
Experimental animals
Six-week-old male CD1 mice weighing approximately
20–25 g were purchased from Charles River Laboratory (Boston, MA,
USA). Twenty-eight mice were used in this study. The animals were
kept in a controlled environment with a regular light-dark cycle
(lights on from 8:00 to 20:00) with an ambient temperature of
22±1°C, and were allowed free access to food and water. The mice
received an intraperitoneal (IP) injection of 2-AA (6.75 mg/kg),
and mouse skeletal muscle was analyzed 4 days post-AA treatment.
Ex vivo proton nuclear magnetic resonance (1H
NMR) spectroscopy was performed on intact gastrocnemius muscle
samples.
High-resolution magic-angle-spinning
(HRMAS) 1H NMR spectroscopy of intact skeletal muscle
tissue
At 4 days post-2-AA treatment, eight 2-AA-treated
and eight untreated animals (that served as a control) were
analyzed using HRMAS 1H NMR spectroscopy. The left
gastrocnemius muscle was harvested, immediately frozen in liquid
nitrogen, and stored at approximately −80°C. The same muscle from
untreated animals served as a control. HRMAS 1H NMR
spectroscopic analysis of muscle tissue was performed on a Bruker
Bio-Spin Avance NMR spectrometer (proton frequency at 600.13 MHz,
with an 89-mm vertical bore) using a 4-mm triple resonance
(1H, 13C, 2H) HRMAS probe (Bruker,
Billerica, MA, USA). The temperature was maintained at 4°C with a
BTO-2000 thermocouple unit in combination with a magic angle
spinning (MAS) pneumatic unit (Bruker). The MAS speed was
stabilized at 4.0±0.001 kHz using a MAS speed controller. The
1H NMR spectra were acquired for all samples using a
Carr-Purcell-Meiboom-Gill (CPMG) spin echo pulse sequence
[90°−(τ−180°−τ−)n-acquisition], with an inter-pulse
delay (τ−) of 250 µsec. Hard 90° (8 τ-s) and 180° (16 τ-s) were
employed. As previously described (32), the relaxation delay was set to 2
sec, and spectra were collected both with and without water
suppression. The transverse relaxation time (T2) was
measured using the same CPMG pulse sequence by varying n
from 0 to 520. Free induction decay (FID) signals were acquired
with 8k points, a 600 msec acquisition time, 8 dummy scans and 128
scans. HRMAS 1H NMR spectra were analyzed using the
MestRe-C NMR software package (Mestrelab Research, Santiago de
Compostela, Spain; www.mestrec.com). FIDs were zero-filled to 16k points
and apodized with exponential multiplication (1 Hz) prior to
Fourier transformation. The spectra were then manually phased and
corrected for baseline broad features (Whittaker smoother, smooth
factor 10,000). The Levenberg-Marquardt algorithm was used to
least-squares-fit a model of mixed Gaussian/Lorentzian functions to
the data. The (CH2)n−2 peak at 1.32 ppm was
selected for the quantification of intramyocellular lipids (IMCLs).
As the sample was spun at a magic angle, and the sample was much
smaller (25 μl) and more homogeneous (reduced bulk magnetic
susceptibility effects) than the typical voxel size (1 ml) of in
vivo 1H MRS, no chemical shift difference was
observed between IMCL and extramyocellular lipids (EMCL). The small
size of the muscle biopsies and the fact that the samples were
collected from the most myocellular part of the muscle suggest that
the main contribution to the (CH2)n−2 peak
was made by IMCL lipids.
Absolute quantification of metabolites
from 1-D CPMG spectra
Resonance intensities were measured for
−CH3 protons of the trimethylsilyl-propionic-2,2,3,3-d4
acid (TSP) and compared to the resonance intensities measured for
metabolites. The peak intensities of most of the metabolites, as
well as of TSP, were calculated from the intensity of the
respective resonance (X) measured from the T2-filtered
HRMAS 1H MR spectrum. The calculated peak intensities
were then corrected for T2 relaxation, using Ic(X) =
Ir(X) * exp(TCPMG/T2(X))/n, where
Ir(X) is the measured intensity, TCPMG is the CPMG echo
time, and n is the number of protons in the functional group
and corresponds to the resonance of the metabolite. In accordance
with the 'external standard' technique employed (35), metabolite concentrations were
quantified relative to the absolute concentration (μmol) of
the respective metabolite [M] = Ic(M)/(IcTSP(M)
* wt), where wt is the weight of the sample in
grams.
Statistical analysis of HRMAS
1H NMR spectroscopy data
Data are reported as the means ± standard errors of
the mean. Between-groups comparison was performed using analysis of
variance with Bonferroni correction for multiple comparisons. A
corrected p-value of <0.0125 was deemed to indicate a
statistically significant difference. A comparison between
measurements was performed in each group with a t-test (two-tailed,
p<0.0125). All analyses were performed using SPSS software (SPSS
version 12; SPSS Inc., Chicago, IL, USA).
Extraction of RNA samples
As previously described (32), the left gastrocnemius muscle was
harvested at 4 days post 2-AA treatment (n=3), to determine the
changes in gene expression in whole muscle. The muscle specimens of
the anesthetized animals were excised and immediately immersed in 1
ml TRIzol (Gibco-BRL, Invitrogen, Carlsbad, CA, USA) for RNA
extraction. Each muscle specimen was homogenized for 60 sec with a
Brinkmann Polytron 3000 homogenizer prior to total RNA extraction.
Chloroform (200 μl) was added to the homogenized muscle and
mixed by inverting the tube for 15 sec. Following centrifugation at
12,000 × g for 15 min, the upper aqueous phase was collected and
precipitated by the addition of 500 μl isopropanol. Further
centrifugation at 12,000 × g for 10 min separated the RNA pellet,
which was then washed with 500 μl of 70% ethanol and
centrifuged at 7,500 × g for 5 min prior to air drying. The pellet
was resuspended in 100 μl diethylpyrocarbonate (DEPC) water.
An RNeasy kit (Qiagen, Germantown, MA, USA) was used to purify the
RNA according to the manufacturer's instructions. The purified RNA
was quantified by UV absorbance at 260 and 280 nm, and stored at
−70°C for DNA microarray analysis.
Microarray hybridization
As previously described (32), biotinylated cRNA was generated
with 10 μg of total cellular RNA according to the protocol
outlined by Affymetrix Inc. (Santa Clara, CA, USA). cRNA was
hybridized onto MOE430A oligonucleotide arrays (Affymetrix),
stained, washed and scanned according to the Affymetrix
protocol.
Genomic data analysis
As previously described (32), data of the scanned image files
hybridized with probes from RNA extracted from the gastrocnemius
muscle isolated at the specified times from the 2-AA-treated and
untreated control mice (n=3) were converted to cell intensity files
(CEL files) with the Microarray suite 5.0 (MAS; Affymetrix). The
data were scaled to a target intensity of 500, and all possible
pairwise array comparisons of the replicates to normal control mice
were performed using a MAS 5.0 change call algorithm. Probe sets
that had a signal value difference >100 and for which one of the
two samples being compared was not termed 'absent', were scored as
differentially modulated when i) the number of change calls in the
same direction were at least 3, 4 and 6, when the number of
comparisons were 4, 6 and 9, respectively; and ii) the other
comparisons were unaltered. Based on the ratios of 100 genes
determined to be invariant in most conditions tested (Affymetrix),
an additional constraint of a minimum ratio of 1.65 was applied to
control the known false positives at 5%. The microarray data are
available at http://www.ncbi.nlm.nih.gov/geo/info/linking.html
and the accession number is GSE43779. Gene Ontology (GO) analysis
was performed using GeneSpring GX software (version 11) by Agilent
Technologies (Santa Clara, CA, USA).
In vivo microscopic measurement of
mitochondrial membrane potential
Following 4 days of treatment with 2-AA (6.75
mg/kg), the 2-AA treated mice and the untreated controls (n=3) were
anesthetized and underwent in vivo microscopic observation
as previously described (36,37) with modifications. Briefly,
sternocleidomastoid muscles were exposed and stained with 40 nM
3,3′-dihexyloxacarbocyanine iodide (DiOC6) and 1
μM CellTracker Orange (Invitrogen) for 30 min. After
washing, the fluorescence intensity of DiOC6, which
reflects mitochondrial membrane potential, was recorded. The
consistency of dye accessibility and image caption was confirmed by
internal control staining with CellTracker Orange. The captured
images were analyzed and their fluorescence intensity was analyzed
by densitometry with ImageJ software (http://imagej.nih.gov/ij/).
Results
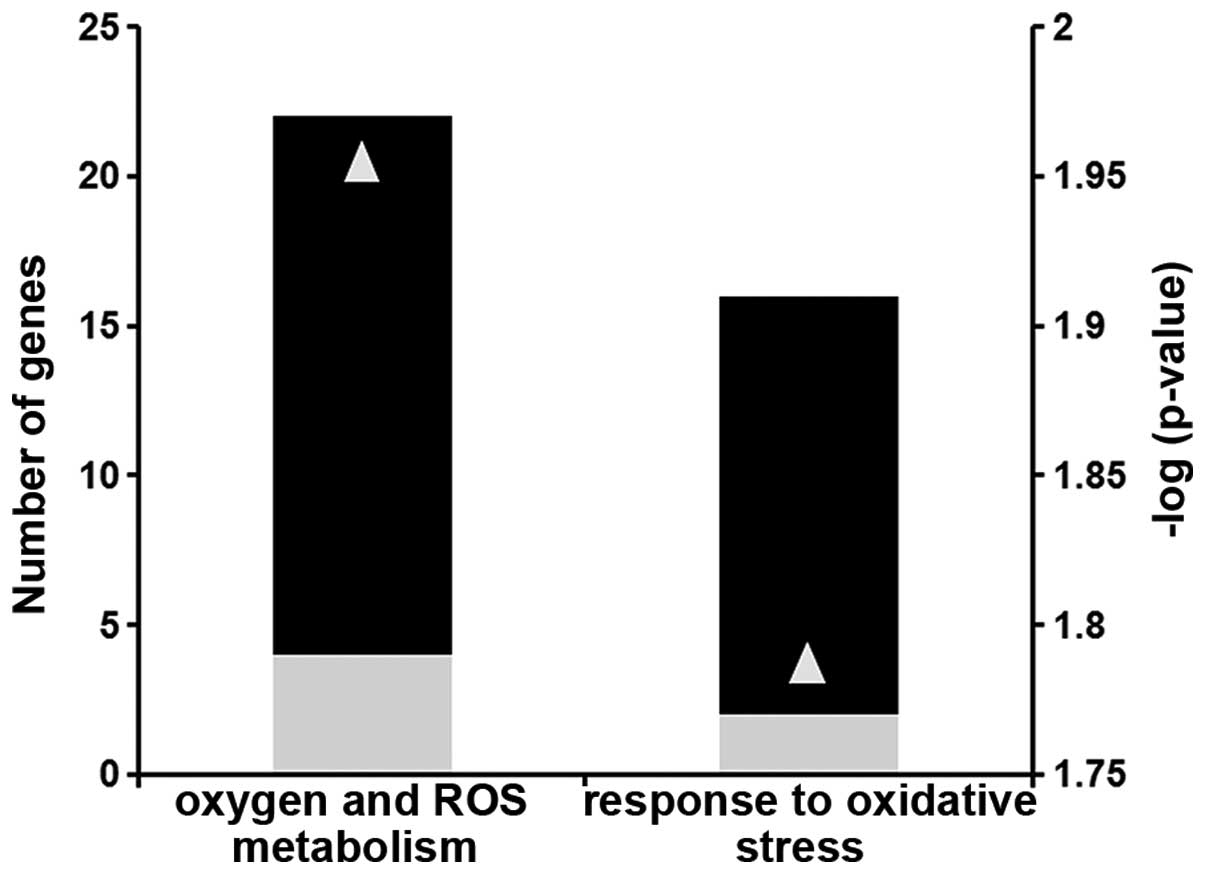
2-AA treatment affects ROS homeostasis
and production and the response to oxidative stress
Using microarray analysis, we identified a subset of
differentially expressed genes that have functional annotations of
oxidative stress and mitochondrial function. Several genes involved
in ROS homeostasis (group A) and in the response to oxidative
stress (group B) were down-regulated (Fig. 1 and Table I).
 | Table IDifferential expression of genes
involved in ROS homeostasis and oxidative stress in mouse skeletal
muscle 4 days following an injection of 2-AA. |
Table I
Differential expression of genes
involved in ROS homeostasis and oxidative stress in mouse skeletal
muscle 4 days following an injection of 2-AA.
| GenBank | Gene name | Fold change | p-value | GO Biological
process |
|---|
| Group A |
| NM_009127 | Stearoyl-coenzyme A
desaturase 1 | (−)4.3 | 0.024 | Oxygen and ROS
metabolism |
| AF173681 | Thioredoxin
interacting protein | (−)4.4 | 0.038 | Oxygen and ROS
metabolism |
| NM_009804 | Catalase | (−)8.6 | 0.013 | Oxygen and ROS
metabolism |
| NM_020569 | Parkinson disease
(autosomal recessive, early onset) 7 | (−)2.3 | 0.029 | Oxygen and ROS
metabolism |
| NM_011435 | Superoxide
dismutase 3, extracellular | (−)4.5 | 0.018 | Oxygen and ROS
metabolism |
| NM_021356 | Growth factor
receptor bound protein 2-associated protein 1 | (−)2.4 | 0.028 | Oxygen and ROS
metabolism |
| NM_011563 | Peroxiredoxin
2 | (−)2.1 | 0.016 | Oxygen and ROS
metabolism |
| NM_001111320 | Isocitrate
dehydrogenase 1 (NADP+), soluble | (−)4.2 | 0.041 | Oxygen and ROS
metabolism |
| NM_013603 | Metallothionein
3 | (+)2.8 | 0.023 | Oxygen and ROS
metabolism |
| NM_010497 | Isocitrate
dehydrogenase 1 (NADP+), soluble | (−)3.1 | 0.023 | Oxygen and ROS
metabolism |
| NM_018881 | Flavin containing
monooxygenase 2 | (−)4.6 | 0.022 | Oxygen and ROS
metabolism |
| NM_023505 | Glutaredoxin 2
(thioltransferase) | (−)2 | 0.027 | Oxygen and ROS
metabolism |
| BC019664 | Glutathione
peroxidase 8 (putative) | (−)4 | 0.005 | Oxygen and ROS
metabolism |
| NM_013711 | Thioredoxin
reductase 2 | (−)3.5 | 0.025 | Oxygen and ROS
metabolism |
| AF412308 | Thioredoxin
reductase 2 | (−)2.4 | 0.009 | Oxygen and ROS
metabolism |
| NM_027629 | Phosphoglucomutase
2-like 1 | (+)9.8 | 0.023 | Oxygen and ROS
metabolism |
| NM_013671 | Superoxide
dismutase 2, mitochondrial | (−)5.8 | 0.008 | Oxygen and ROS
metabolism |
| M14222 | Cathepsin B | (−)2.5 | 0.028 | Oxygen and ROS
metabolism |
| NM_008161 | Glutathione
peroxidase 3 | (−)3.7 | 0.005 | Oxygen and ROS
metabolism |
| AF274027 | Phospholipid
hydroperoxide glutathione peroxidase | (−)3 | 0.020 | Oxygen and ROS
metabolism |
| NM_018881 | Flavin containing
monooxygenase 2 | (−)5.3 | 0.007 | Oxygen and ROS
metabolism |
| XM_006508205 | Phosphoglucomutase
2-like 1 (predicted) | (+)5.1 | 0.013 | Oxygen and ROS
metabolism |
| Group B |
| AF173681 | Thioredoxin
interacting protein | (−)4.4 | 0.038 | Response to
oxidative stress |
| NM_009804 | Catalase | (−)8.6 | 0.013 | Response to
oxidative stress |
| NM_020569 | Parkinson disease
(autosomal recessive, early onset) 7 | (−)2.3 | 0.029 | Response to
oxidative stress |
| NM_021356 | Growth factor
receptor bound protein 2-associated protein 1 | (−)2.4 | 0.028 | Response to
oxidative stress |
| NM_011563 | Peroxiredoxin
2 | (−)2.1 | 0.016 | Response to
oxidative stress |
| NM_001111320 | Isocitrate
dehydrogenase 1 (NADP+), soluble | (−)4.2 | 0.041 | Response to
oxidative stress |
| NM_010497 | Isocitrate
dehydrogenase 1 (NADP+), soluble | (−)3.1 | 0.023 | Response to
oxidative stress |
| NM_023505 | Glutaredoxin 2
(thioltransferase) | (−)2 | 0.027 | Response to
oxidative stress |
| BC019664 | Glutathione
peroxidase 8 (putative) | (−)4 | 0.005 | Response to
oxidative stress |
| NM_013711 | Thioredoxin
reductase 2 | (−)3.5 | 0.025 | Response to
oxidative stress |
| AF412308 | Thioredoxin
reductase 2 | (−)2.4 | 0.009 | Response to
oxidative stress |
| NM_027629 | Phosphoglucomutase
2-like 1 | (+)9.8 | 0.023 | Response to
oxidative stress |
| NM_013671 | Superoxide
dismutase 2, mitochondrial | (−)5.8 | 0.008 | Response to
oxidative stress |
| M14222 | Cathepsin B | (−)2.5 | 0.028 | Response to
oxidative stress |
| NM_008161 | Glutathione
peroxidase 3 | (−)3.7 | 0.005 | Response to
oxidative stress |
| AF274027 | Glutathione
peroxidase 4 | (−)3 | 0.020 | Response to
oxidative stress |
| XM_006508205 | Phosphoglucomutase
2-like 1 (predicted) | (+)5.1 | 0.013 | Response to
oxidative stress |
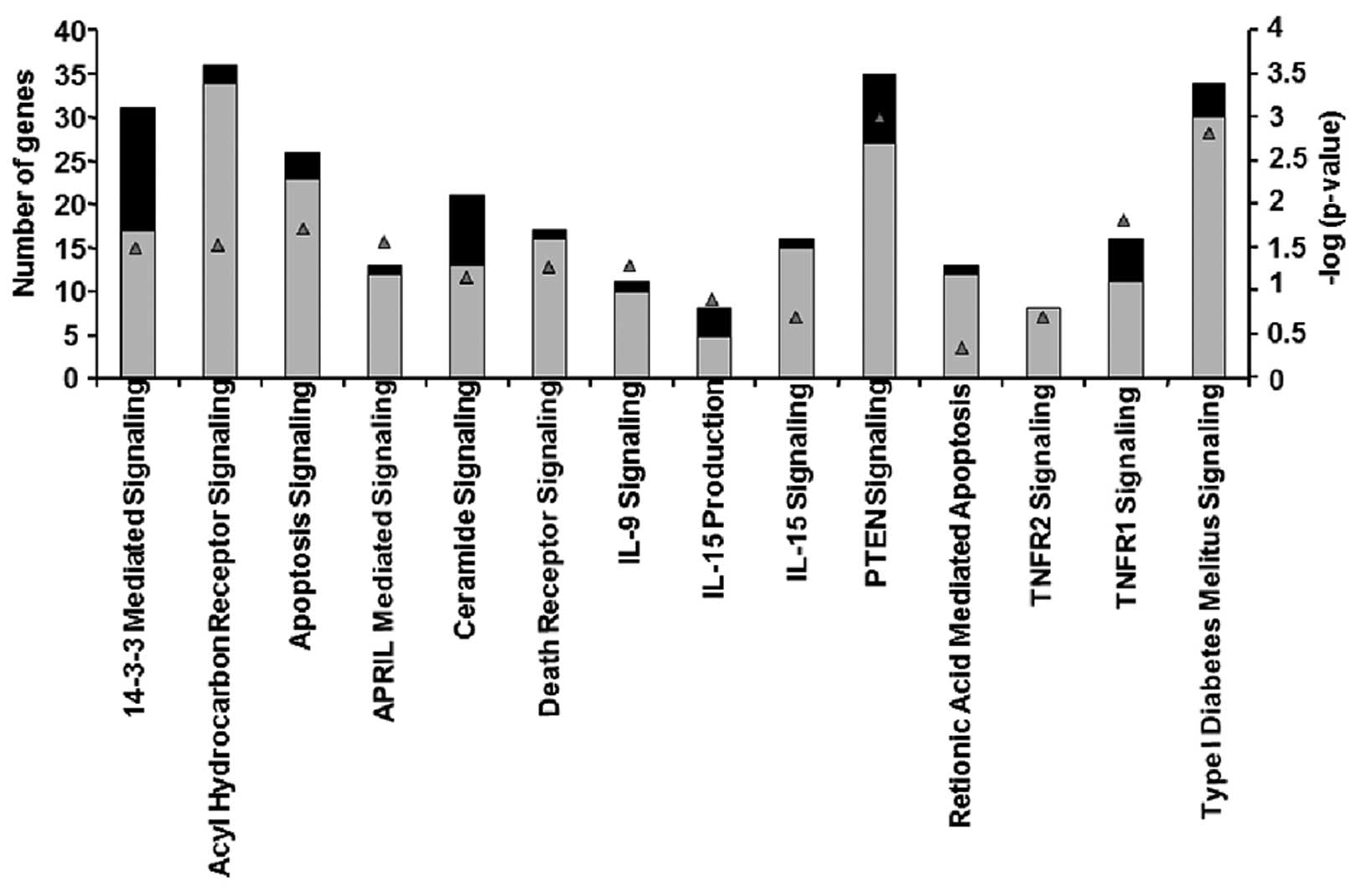
Differential expression of genes involved
in the apoptosis signaling pathway in skeletal muscle of
2-AA-treated mouse
The microarray data presented in Table II and Fig. 2 demonstrated that certain genes,
which had been identified as functioning in apoptosis via
annotation by Gene Ontology Consortium and Ingenuity, were
differentially expressed. Almost 97% of the genes involved in
apoptosis signaling were upregulated in mouse skeletal muscle after
4 days of treatment with 2-AA (Table
II and Fig. 2). For example,
the TNF receptor superfamily member 1α gene exhibited an increased
expression. This gene encodes a major TNF-α receptor that activates
nuclear factor-κB (NF-κB), mediates apoptosis and regulates
inflammation (17). In addition,
genes encoding B-cell lymphoma (Bcl)-2, which function downstream
of the TNF-α receptor in apoptosis signaling (38), exhibited an increased expression.
Specifically, the upregulation of Bcl-2-like 13 (apoptosis
facilitator), which is a member of Bcl-2 family of proteins,
promotes apoptosis by blocking caspase inhibitors (39). The upregulation of PERP (p53
apoptosis effector), a p53 transcriptional target, promotes
apoptosis (40). Fas apoptotic
inhibitory molecules which confer resistance to Fas-induced
apoptosis (41), were also
downregulated following 2-AA treatment. The increased expression of
growth arrest-specific 2 (Gas2) genes may activate apoptosis
(42) in murine muscle of
2-AA-treated mice.
 | Table IIDifferential expression of genes
involved in the apoptosis signaling pathway in mouse skeletal
muscle samples following 4 days of treatment with 2-AA. |
Table II
Differential expression of genes
involved in the apoptosis signaling pathway in mouse skeletal
muscle samples following 4 days of treatment with 2-AA.
| GenBank | Gene name | Fold change | p-value |
|---|
| NM_030711 | Endoplasmic
reticulum aminopeptidase 1 (Erap1) | 2.264 | 0.0158 |
| NM_134131 | Tumor necrosis
factor, α-induced protein 8 | 3.863 | 0.0183 |
| NM_023517 | Tumor necrosis
factor (ligand) superfamily, member 13 (Tnfsf13) | 3.293 | 0.0061 |
| NM_009396 | Tumor necrosis
factor-α-induced protein | 5.796 | 0.00082 |
| NM_009425 | Tumor necrosis
factor (ligand) superfamily, member 10 | 3.398 | 0.0226 |
| NM_011614 | Tumor necrosis
factor (ligand) superfamily, member 12 (Tnfsf12) | 2.735 | 0.03 |
| NM_022310 | Heat shock 70 kDa
protein 5 (glucose-regulated protein) | 4.146 | 0.0118 |
| AF250139 | Small stress
protein-like protein (HSP22) | 6.137 | 0.0106 |
| NM_010481 | Heat shock protein
9A | 3.462 | 0.0107 |
| NM_013560 | Heat shock protein
1 | 3.248 | 0.0146 |
| NM_013559 | Heat shock protein
110 | −3.95 | 0.0367 |
| U03561 | Heat shock protein
HSP27 internal deletion variant b | 4.008 | 0.025 |
| NM_010477 | Heat shock protein
1 (chaperonin) | 2.915 | 9.33E-05 |
| NM_010480 | Heat shock protein
90, α (cytosolic), class A member 1 (Hsp90aa1) | −2.63 | 0.0484 |
| NM_001163434 | Heat shock 70 kDa
protein 5 (glucose-regulated protein) | 3.076 | 0.00638 |
| NM_001164708 | Heat shock protein
2 | 5.374 | 0.0412 |
| NM_013868 | Heat shock protein
family, member 7 (cardiovascular) | 6.046 | 0.0427 |
| NM_011020 | Heat shock 70 kDa
protein 4 like | −2.43 | 0.0368 |
| NM_008303 | Heat shock protein
1 (chaperonin 10) | 3.313 | 0.034 |
| M12573 | Heat shock protein
1B | 3.49 | 3.49 |
| XM_006500766 | Heat shock 70 kDa
protein 4 like | −5.49 | 0.0266 |
| NM_028306 | Heat shock protein
12B | 8.802 | 0.0479 |
| NM_009883 | CCAAT/enhancer
binding protein (C/EBP)β | 4.288 | 0.0215 |
| NM_009884 | CCAAT/enhancer
binding protein (C/EBP)γ | 2.352 | 0.0479 |
| NM_010499 | Immediate early
response 2 | 2.68 | 0.0161 |
| NM_008495 | Lectin, galactose
binding, soluble 1 | 4.588 | 0.0481 |
| NM_001145953 | Lectin, galactose
binding, soluble 3 | 2.464 | 0.0162 |
| NM_001199043 | Lectin, galactose
binding, soluble 8 | 2.019 | 0.00659 |
| NM_010708 | Lectin, galactose
binding, soluble 9 | 4.736 | 0.0464 |
| NM_019738 | Nuclear protein
1 | 2.299 | 0.0239 |
| NM_134141 | Cytokine induced
apoptosis inhibitor 1 | 2.295 | 0.0222 |
| NM_022032 | PERP, TP53
apoptosis effector | 12.73 | 0.0252 |
| BC023121 | CASP8 and FADD-like
apoptosis regulator | 2.91 | 0.0075 |
| NM_001177552 | Bifunctional
apoptosis regulator | 2.006 | 0.0414 |
| NM_054056 | PRKC, apoptosis,
WT1, regulator | 3.307 | 0.03 |
| NM_001038658 | Fas apoptotic
inhibitory molecule 2 | −2.39 | 0.0493 |
| NM_153516 | BCL2-like 13
(apoptosis facilitator) | 2.796 | 0.0205 |
| NM_001039194 | Apoptosis-inducing
factor (AIF)-like mitochondrion-associated inducer of death | 2.033 | 0.0445 |
| NM_007609 | Caspase 4,
apoptosis-related cysteine peptidase (Casp4), mRNA | 3.446 | 0.00128 |
| NM_001042558 | Apoptotic peptidase
activating factor 1 | 2.701 | 0.016 |
| NM_001165935 | Apoptosis, caspase
activation inhibitor | 2.149 | 0.0206 |
| NM_001038658 | Fas apoptotic
inhibitory molecule 2 | −22.32 | 0.00627 |
| BC003292 | Programmed cell
death 8 | 3.129 | 0.0449 |
| BC026823 | Programmed cell
death 6 interacting protein | 2.436 | 0.00988 |
| NM_001164677 | Programmed cell
death 6 interacting protein | 4.606 | 0.000958 |
| NM_019746 | Programmed cell
death 5 | 2.834 | 0.0486 |
| BC024876 | Death-associated
protein | 3.706 | 0.0196 |
| NM_007566 | Baculoviral IAP
repeat-containing 6 | 2.586 | 0.00413 |
| NM_001301639 | X-linked inhibitor
of apoptosis (Xiap), transcript variant 1 | 2.44 | 0.0415 |
| NM_053207 | EGL nine homolog 1
(C. elegans) | 2.658 | 0.026 |
| AK017394 | Growth arrest
specific 7 | −34.15 | 0.000771 |
| NM_026832 | Cell growth
regulator with ring finger domain 1 | 3.016 | 0.0446 |
| NM_001109657 | Growth
arrest-specific 7-cb protein (Gas7-cb) | −32.15 | 0.0113 |
| NM_008655 | Growth arrest and
DNA-damage-inducible 45β | 3.297 | 0.0366 |
| NM_001033331 | Growth
arrest-specific 2 like 3 | 4.312 | 0.0324 |
| NM_001277080 | Growth
arrest-specific 7-cb protein (Gas7-cb) | −19.88 | 0.0303 |
| AF037370 | Cytochrome c
oxidase, subunit VIIa 1 | 10.56 | 0.0445 |
| NM_007808 | Cytochrome c,
somatic | 3.344 | 0.0391 |
| NM_007747 | Cytochrome c
oxidase, subunit Va | 3.291 | 0.035 |
| NM_009941 | Cytochrome c
oxidase subunit IV isoform 1 | 2.642 | 0.0202 |
| NM_007751 | Cytochrome c
oxidase, subunit VIIIb | 5.591 | 0.0399 |
| AA190297 | Cytochrome c
oxidase, subunit VIIc | 2.104 | 0.0296 |
| NM_025628 | Cytochrome c
oxidase, subunit VIb polypeptide 1 | 2.015 | 0.0144 |
| NM_024226 | Reticulon 4 | −7.51 | 0.0255 |
| BF455257 | Reticulon 1 | −29.85 | 0.00175 |
| BM246564 | Phosphodiesterase
4B, cAMP specific | 2.161 | 0.0488 |
| NM_009811 | Caspase 6 | 3.503 | 0.0107 |
| NM_007611 | Caspase 7 | 3.837 | 0.00433 |
| NM_001163138 | Caspase recruitment
domain family, member 6 | 3.344 | 0.00725 |
| NM_007611 | Caspase 7 | 4.957 | 0.0082 |
| BC008152 | Caspase 1 | 4.165 | 0.0361 |
| NM_001171007 | Nucleotide-binding
oligomerization domain containing 1 (Nod1)/Caspase recruitment
domain 4 | 2.35 | 0.0266 |
Several other genes were also upregulated, including
heat shock proteins, lectins and AIF, the death associated protein.
In addition, we noted that mitochondrial-dependent apoptosis genes
which encode cytochrome c and caspases exhibited an
increased expression.
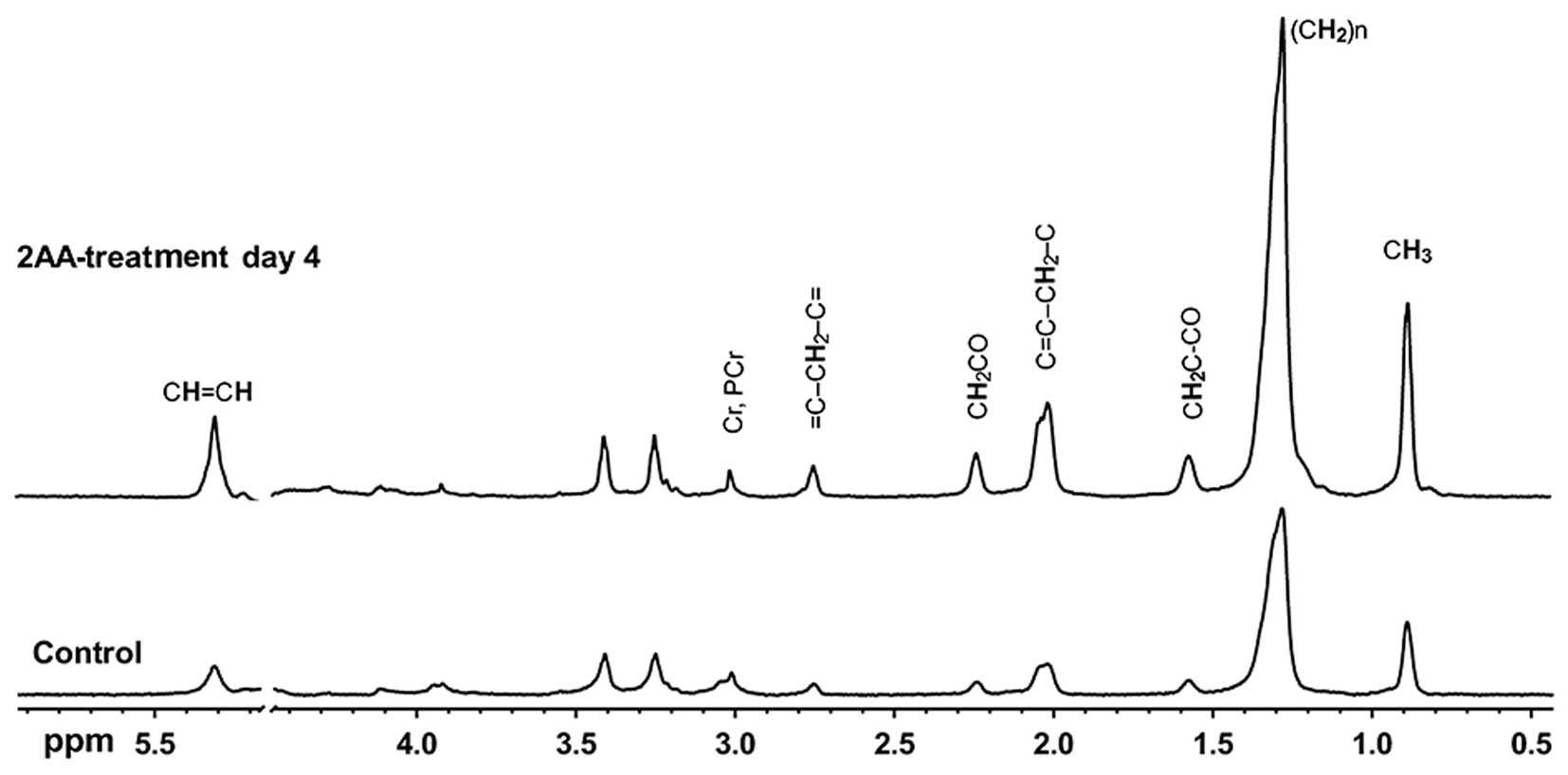
1H NMR detects muscle lipid
accumulation following 2-AA treatment
1H NMR spectroscopy has been used to
explore metabolic changes (33,34,43). The accumulation of mobile lipids
is associated with mitochondrial dysfunction, oxidative stress and
apoptosis (44,45). As shown in Fig. 3 and Table III, the results of NMR
spectroscopy demonstrated that most lipid peaks were consistently
increased in the skeletal muscle samples from the 2-AA-treated mice
compared to the control mice.
 | Table IIIResults of 1H NMR HRMAS
experiments performed on gastrocnemius muscle specimens from
2-AA-treated mice versus control mice. |
Table III
Results of 1H NMR HRMAS
experiments performed on gastrocnemius muscle specimens from
2-AA-treated mice versus control mice.
| Chemical shift
PPM | Chemical group | Control | 4 days
post-2-AA | Percent change | p-value |
|---|
| 2.8 | =CH-CH2-CH= | 0.012±0.004a | 0.040±0.007 | +233 | 0.0075b |
| 5.4 | CH=CH- | 0.041±0.015 | 0.226±0.058 | +451 | 0.0233 |
The stack plot presented in Fig. 3 shows typical examples of proton
HRMAS 1H MRS CPMG spectra from skeletal muscle samples.
This plot contains spectra of the control and 2-AA-treated animals
sacrificed 4 days post-2-AA-treatment, with the spectra scaled to
the phosphocreatine and creatine 3.02-ppm peak. Resonance signals
are due to residual water (4.7–4.8 ppm); terminal methyl (0.8–1.0
ppm); acyl chain methylene (1.1–1.5 ppm); α- and β-methylene
(2.0–2.5 ppm) and olefinic protons (5.4 ppm) of lipids; N-methyl
protons of phosphocreatine and creatine (3.0 ppm); and N-trimethyl
protons of betaines (3.2 ppm), which correspond to taurine and
choline-containing compounds. The phospholipids at 3.2 ppm appear
unaffected by 2-AA treatment and remain stable, along with other
peaks between 3 and 4 ppm. The results from quantitative analysis
of these high-resolution ex vivo HRMAS 1H MRS
measurements are shown in Table
III. Bisallylic methylene fatty acyl protons at 2.8 ppm
correspond to polyunsaturated fatty acids (PUFAs), which accumulate
due to apoptosis. Vinyl proton accumulation at 5.4 ppm, including
protons from ceramide and possibly other sphingolipids suggests
apoptosis.
Downregulation of mitochondrial membrane
potential in skeletal muscle from 2-AA-treated mice
Mitochondrial membrane potential is considered a
biomarker of oxidative stress and apoptosis (46,47). In vivo fluorescence
microscopy with DiOC6 indicated that 2-AA treatment
reduced skeletal muscle mitochondrial membrane potential by 41%
compared to the untreated control group (p<0.05; Fig. 4). The fact that internal control
staining with CellTracker Orange revealed equivalent staining
between the two groups confirmed that the difference observed in
membrane potential was not due to staining issues (i.e., dye
accessibility or fluctuation in image capturing).
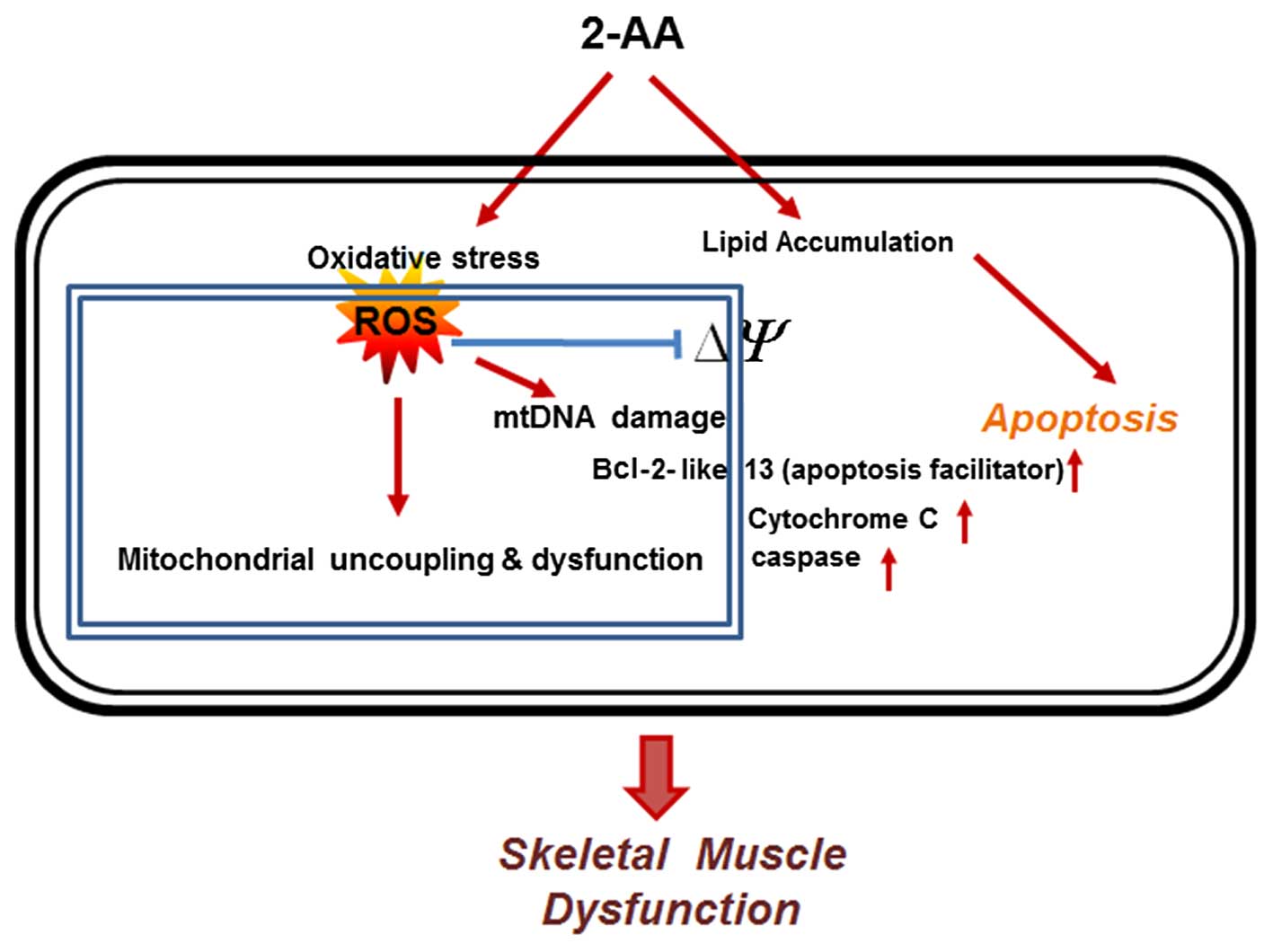
Discussion
In the present study, we demonstrate that 2-AA, a
QS-regulated requisite for PA pathogenesis and a diagnostically
important bacterial molecule, induces oxidative stress in skeletal
muscle, disrupts the defense against oxidative stress, reduces
mitochondrial membrane potential and enhances apoptotic signaling
(Fig. 5). The reduced expression
of genes involved in ROS metabolism and in the oxidative stress
response may be responsible for the accumulation of ROS in skeletal
muscle. ROS toxicity may lead to mitochondrial dysfunction,
possibly via damage to mitochondrial DNA (mtDNA) and reduced
mitochondrial potential. Our findings also suggest a reduction in
the oxidative stress response as a potential mechanism through
which 2-AA modulates the apoptotic pathway, and suggest candidate
targets through which to limit oxidative stress and apoptosis in
patients with infection.
The principal finding of the present study was the
effect of 2-AA on ROS production and the antioxidant status
homeostasis in skeletal muscle, which correlates with the induction
of apoptosis. Normally, increased ROS induce antioxidant defenses
and prevent damage to mitochondrial macromolecules; in the absence
of such defenses, oxidative damage ensues. In addition, the
oxidative stress caused by increased ROS production results in
apoptosis (8). Based on the
findings of this study, we suggest that 2-AA interferes with ROS
detoxification resulting in oxidative damage to mitochondrial
macromolecules, possibly including mtDNA. ROS initiate damage to
nucleic acids, proteins and lipids (10). Since mitochondrial DNA (mtDNA) is
located closer to the site of ROS generation, lacks protective
histones, and has more limited base excision repair mechanisms than
the nucleus, it is more vulnerable to oxidative damage than nuclear
DNA (nDNA) (48,49).
Another major finding of this study concurs with
oxidative stress and is accompanied by mitochondrial dysfunction.
In a recent study, we demonstrated that peroxisomal proliferator
activator receptor (PPAR)-γ and PPAR-γ co-activator (PGC)1
expression was downregulated by 2-AA (32). PGC1 is hypothesized to play a
central role in regulating energy homeostasis and metabolism
(50). Therefore, the observed
downregulation of genes involved in oxidative phosphorylation
(32) and also in ROS
detoxification by 2-AA may be explained by the effect of 2-AA on
PGC1 (32). As a result of this
dysregulation, the balance of detoxification and ROS generation may
be shifted towards ROS accumulation. To this end, this study
complies with the notion that certain components of the ROS
scavenging pathway are linked by PGC1 to mitochondrial oxidative
phosphorylation, apparently preventing cells from maintaining the
normal redox status in response to a change in ROS production
(51).
In this study, the expression of genes which encode
proteins with pro- or anti-apoptotic functions was altered in
response to 2-AA treatment (Fig.
2 and Table II); however,
their exact regulatory role remains unclear. These data may reflect
a heterogeneous mRNA population which is due to a direct effect of
2-AA on the underlying superficial layers of the hind limb muscle,
and the asynchronous state of apoptotic muscle cells. Nonetheless,
our data demonstrated that apoptotic pathways are activated in
muscle from 2-AA-treated mice, which further demonstrates a link
between the dysregulation of fatty acid oxidation (32), lipid accumulation (32) and apoptosis. Furthermore, the
mitochondrial release of pro-apoptotic proteins, such as cytochrome
c is promoted by the formation of specific channels in the
outer membrane of the mitochondria by pro-apoptotic Bcl-2 family
members (39). Once released,
cytochrome c triggers the activation of caspases, which in
turn regulates the apoptotic process (18) and has been suggested to induce
contractile dysfunction (52).
The orderly process of apoptosis is energy dependent and,
consequently, damage to the mitochondria to the point that they can
no longer produce ATP can easily shift to apoptosis (53). The core apoptotic pathway and
cellular energy metabolism maintain an important inter-relationship
between apoptosis and mitochondrial function (54), which is modulated by 2-AA.
In the present study, we noted that lipids
accumulated in muscle tissue following 2-AA treatment, as assessed
by 1H NMR. The lipid peak at 1.3 ppm in Fig. 3 has been attributed to methylene
protons of intramyocellular triglyceride acyl chains, primarily due
to IMCLs (55), which suggests
that the increase in NMR-visible lipids at 1.4 ppm after 2-AA
treatment is primarily due to increased quantifiable IMCL. This
conclusion is further supported by the results of previous studies
on humans (56,57). Conversely, EMCLs which may
contribute to the 1.4 ppm peak are relatively metabolically inert
and serve as a long-term energy storage depot with slow turnover.
EMCLs are therefore unlikely to correspond to the lipids observed
in this study, which rapidly accumulated post-2-AA treatment.
The accumulation of lipids is associated with
apoptosis (58,59); and the present study demonstrates
that 2-AA induced apoptosis-related gene expression (Table II) and increased the lipid
profile (Fig. 3) in skeletal
muscle, which could be linked. The increase in bisallylic methylene
fatty acyl protons at 2.8 ppm is in accordance with the data of
Hakumäki et al (60),
which suggested that these protons correspond to PUFAs, and PUFA
accumulation follows apoptosis. In addition, our data demonstrate
vinyl proton accumulation at 5.4 ppm, including protons from
ceramide and possibly other sphingolipids, such as sphingosine.
Indeed, ceramide and sphingolipids are known to be involved in
apoptosis (61). These increased
signals suggest that ceramide, a product of sphingolipid
metabolism, contributes to 2-AA-mediated apoptosis. Ceramide and
sphingolipids, in particular, have been implicated as second
messengers for apoptotic stimuli, including TNF-α (62), Fas ligand (63), ionizing radiation (64), heat shock (65) and oxidative stress (66).
The loss of mitochondrial membrane potential leads
to the activation of apoptotic signals in several tissues,
including skeletal muscle (67).
When apoptotic signals reach the mitochondria, membrane
permeability transition occurs, involving voltage-dependent anion
channels (VDAC), adenine nucleotide translocase (ANT) and
translocator protein (TSPO) (68). Damaged mitochondria are known to
release apoptosis-inducing molecules, including cytochrome
c, endonuclease G, AIF and Smac/Diablo and HtrA2/Omi
(36,67). Other research has also
demonstrated that uncoupled mitochondria become a major source for
cellular ROS production (69).
The data from our in vivo microscopic analysis support the
molecular biological observation that the increase in apoptosis and
ROS accumulation occurred in skeletal muscle of mice treated with
2-AA.
PA and 2-AA in the lungs of chronically infected
patients with CF are considered pathogenomic (70,71). Patients with CF often develop
skeletal muscle wasting due to inadequate antioxidant defenses
which cannot cope with the elevated oxidative stress (72,73), and increased apoptosis is observed
in airway cells of patients with CF (19,74). The characteristic loss of muscle
mass, coupled with a decrease in strength, force output and
alteration in oxidative stress, has previously been shown to be
associated with apoptotic pathways and is an underlying mechanism
of the pathogenesis of chronic disease (75,76). Oxidative stress and ROS
accumulation can alter muscle gene expression, causing protein loss
that consequently diminishes muscle mass or function (75). Nuclear receptor subfamily 2, group
F, member 2 (NR2F2), a member of the steroid thyroid hormone
superfamily of nuclear receptors, which is required for skeletal
muscle development (77) and
appears to be involved in the regulation of oxidative stress
(78), was also downregulated
(1.65-fold, p<0.0094) in the skeletal muscle of 2-AA-treated
mice (data not shown). This suggests that 2-AA-mediated muscle
dysfunction (32) may be the
result of increased oxidative stress and apoptosis.
Mitochondrial dysfunction may interact with
oxidative stress (14), lipid
accumulation (59), apoptosis
(79) and innate immune response
(80). 2-AA abridges energy
production and mitochondrial function in skeletal muscle, which may
favor chronic diseases (32,81) and chronic infection (30). Recently, we demonstrated that 2-AA
acts as an immunomodulatory signal (30) and likely affects insulin
resistance associated with a molecular signature of mitochondrial
dysfunction (32) that increases
the ability of the host to live with the pathogen, enabling
tolerance to infection and a long-term bacterial presence leading
to bacterial persistence (30).
Therefore, 2-AA-mediated oxidative stress and the activation of
apoptotic signals may serve to eliminate key immune cells or evade
host defenses (1) and further
contribute to a long-term bacterial presence (30). The results of the present study
are consistent with previous data of other chronic infections,
including Escherichia coli (82), tuberculosis (83), Helicobacter pylori
(84) and patients chronically
infected with CF (85).
In conclusion, our results from transcriptome
analysis and NMR spectroscopy provide strong evidence that the
altered NMR-visible lipid profile is related to apoptosis which is
induced by oxidative stress in response to the bacterial
infochemical, 2-AA. 2-AA-mediated oxidative stress leads to
mitochondrial dysfunction, which results in host metabolic
dysfunction and apoptosis, and such a dysregulation in host
metabolism can promote chronic/persistent disease state (30). Lipid accumulation may reflect
apoptosis, rather than providing a direct measure of mitochondrial
dysfunction. Since apoptosis and cellular energy metabolism are the
two major determinants of cell survival, NMR-visible lipids may
serve as biomarkers to monitor therapies for muscle wasting
following bacterial infection, as well as other disease states. To
this end, our results provide insight into the response of skeletal
muscle to the PA-excreted small molecule, 2-AA, and point to novel
therapeutic possibilities in targeting antioxidant pathways to
reduce oxidative stress and apoptosis in skeletal muscle.
Acknowledgments
This study was supported in part by Shriner's
Hospital for Children research grants (nos. 87100 and 85200), and
Basic Research Award, W81XWH-10-DMRDP-BRA from US Army Medical
Research Acquisition Act of US Department of Defense,
Congressionally Directed Medical Research Programs (CDMRP), Defense
Medical Research and Development Program (DMRDP) to Laurence G.
Rahme, and by a Center grant of the National Institutes of Health
(NIH) to the Stanford Genome Technology Cente, as well as by NIH
grant AI105902. We acknowledge Dr Damien Maura at the Massachusetts
General Hospital and Harvard Medical School for his insightful
comments on the manuscript.
References
|
1
|
Rudel T, Kepp O and Kozjak-Pavlovic V:
Interactions between bacterial pathogens and mitochondrial cell
death pathways. Nat Rev Microbiol. 8:693–705. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Jiang JH, Tong J and Gabriel K: Hijacking
mitochondria: bacterial toxins that modulate mitochondrial
function. IUBMB Life. 64:397–401. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Trumpower BL: Cytochrome bc1 complexes of
microorganisms. Microbiol Rev. 54:101–129. 1990.PubMed/NCBI
|
|
4
|
Van Ark G and Berden JA: Binding of HQNO
to beef-heart sub-mitochondrial particles. Biochim Biophys Acta.
459:119–127. 1977. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Schwarzer C, Fu Z, Shuai S, Babbar S, Zhao
G, Li C and Machen TE: Pseudomonas aeruginosa homoserine lactone
triggers apoptosis and Bak/Bax-independent release of mitochondrial
cytochrome C in fibroblasts. Cell Microbiol. 16:1094–1104. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Raza H, John A and Shafarin J: NAC
attenuates LPS-induced toxicity in aspirin-sensitized mouse
macrophages via suppression of oxidative stress and mitochondrial
dysfunction. PLoS One. 9:e1033792014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Valyi-Nagy T and Dermody TS: Role of
oxidative damage in the pathogenesis of viral infections of the
nervous system. Histol Histopathol. 20:957–967. 2005.PubMed/NCBI
|
|
8
|
Pohanka M: Role of oxidative stress in
infectious diseases. A review. Folia Microbiol (Praha). 58:503–513.
2013. View Article : Google Scholar
|
|
9
|
Murphy MP: How mitochondria produce
reactive oxygen species. Biochem J. 417:1–13. 2009. View Article : Google Scholar
|
|
10
|
Schieber M and Chandel NS: ROS function in
redox signaling and oxidative stress. Curr Biol. 24:R453–R462.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ding SZ, Minohara Y, Fan XJ, Wang J, Reyes
VE, Patel J, Dirden-Kramer B, Boldogh I, Ernst PB and Crowe SE:
Helicobacter pylori infection induces oxidative stress and
programmed cell death in human gastric epithelial cells. Infect
Immun. 75:4030–4039. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Strengert M, Jennings R, Davanture S,
Hayes P, Gabriel G and Knaus UG: Mucosal reactive oxygen species
are required for antiviral response: role of Duox in influenza a
virus infection. Antioxid Redox Signal. 20:2695–2709. 2014.
View Article : Google Scholar
|
|
13
|
Paracha UZ, Fatima K, Alqahtani M,
Chaudhary A, Abuzenadah A, Damanhouri G and Qadri I: Oxidative
stress and hepatitis C virus. Virol J. 10:2512013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Pieczenik SR and Neustadt J: Mitochondrial
dysfunction and molecular pathways of disease. Exp Mol Pathol.
83:84–92. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Garofalo RP, Kolli D and Casola A:
Respiratory syncytial virus infection: mechanisms of redox control
and novel therapeutic opportunities. Antioxid Redox Signal.
18:186–217. 2013. View Article : Google Scholar :
|
|
16
|
Ashida H, Mimuro H, Ogawa M, Kobayashi T,
Sanada T, Kim M and Sasakawa C: Cell death and infection: a
double-edged sword for host and pathogen survival. J Cell Biol.
195:931–942. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Guicciardi ME and Gores GJ: Life and death
by death receptors. FASEB J. 23:1625–1637. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Madeo F, Carmona-Gutierrez D, Ring J,
Büttner S, Eisenberg T and Kroemer G: Caspase-dependent and
caspase-independent cell death pathways in yeast. Biochem Biophys
Res Commun. 382:227–231. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Galli F, Battistoni A, Gambari R, Pompella
A, Bragonzi A, Pilolli F, Iuliano L, Piroddi M, Dechecchi MC and
Cabrini G: Working Group on Inflammation in Cystic Fibrosis:
oxidative stress and antioxidant therapy in cystic fibrosis.
Biochim Biophys Acta. 1822:690–713. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Navon-Venezia S, Ben-Ami R and Carmeli Y:
Update on Pseudomonas aeruginosa and Acinetobacter baumannii
infections in the healthcare setting. Curr Opin Infect Dis.
18:306–313. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kerr KG and Snelling AM: Pseudomonas
aeruginosa: a formidable and ever-present adversary. J Hosp Infect.
73:338–344. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Jimenez PN, Koch G, Thompson JA, Xavier
KB, Cool RH and Quax WJ: The multiple signaling systems regulating
virulence in Pseudomonas aeruginosa. Microbiol Mol Biol Rev.
76:46–65. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Déziel E, Gopalan S, Tampakaki AP, Lépine
F, Padfield KE, Saucier M, Xiao G and Rahme LG: The contribution of
MvfR to Pseudomonas aeruginosa pathogenesis and quorum sensing
circuitry regulation: multiple quorum sensing-regulated genes are
modulated without affecting lasRI, rhlRI or the production of
N-acyl-L-homoserine lactones. Mol Microbiol. 55:998–1014. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Xiao G, Déziel E, He J, Lépine F, Lesic B,
Castonguay MH, Milot S, Tampakaki AP, Stachel SE and Rahme LG:
MvfR, a key Pseudomonas aeruginosa pathogenicity LTTR-class
regulatory protein, has dual ligands. Mol Microbiol. 62:1689–1699.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Parker CT and Sperandio V: Cell-to-cell
signalling during pathogenesis. Cell Microbiol. 11:363–369. 2009.
View Article : Google Scholar :
|
|
26
|
Kesarwani M, Hazan R, He J, Que YA,
Apidianakis Y, Lesic B, Xiao G, Dekimpe V, Milot S, Deziel E, et
al: A quorum sensing regulated small volatile molecule reduces
acute virulence and promotes chronic infection phenotypes. PLoS
Pathog. 7:e10021922011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zhou L, Slamti L, Nielsen-LeRoux C,
Lereclus D and Raymond B: The social biology of quorum sensing in a
naturalistic host pathogen system. Curr Biol. 24:2417–2422. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Ng WL and Bassler BL: Bacterial
quorum-sensing network architectures. Annu Rev Genet. 43:197–222.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Rumbaugh KP and Kaufmann GF: Exploitation
of host signaling pathways by microbial quorum sensing signals.
Curr Opin Microbiol. 15:162–168. 2012. View Article : Google Scholar
|
|
30
|
Bandyopadhaya A, Kesarwani M, Que YA, He
J, Padfield K, Tompkins R and Rahme LG: The quorum sensing volatile
molecule 2-amino acetophenon modulates host immune responses in a
manner that promotes life with unwanted guests. PLoS Pathog.
8:e10030242012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Que YA, Hazan R, Strobel B, Maura D, He J,
Kesarwani M, Panopoulos P, Tsurumi A, Giddey M, Wilhelmy J, et al:
A quorum sensing small volatile molecule promotes antibiotic
tolerance in bacteria. PLoS One. 8:e801402013. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Tzika AA, Constantinou C, Bandyopadhaya A,
Psychogios N, Lee S, Mindrinos M, Martyn JA, Tompkins RG and Rahme
LG: A small volatile bacterial molecule triggers mitochondrial
dysfunction in murine skeletal muscle. PLoS One. 8:e745282013.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Astrakas LG, Goljer I, Yasuhara S,
Padfield KE, Zhang Q, Gopalan S, Mindrinos MN, Dai G, Yu YM, Martyn
JA, et al: Proton NMR spectroscopy shows lipids accumulate in
skeletal muscle in response to burn trauma-induced apoptosis. FASEB
J. 19:1431–1440. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Padfield KE, Astrakas LG, Zhang Q, Gopalan
S, Dai G, Mindrinos MN, Tompkins RG, Rahme LG and Tzika AA: Burn
injury causes mitochondrial dysfunction in skeletal muscle. Proc
Natl Acad Sci USA. 102:5368–5373. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Morvan D, Demidem A, Papon J and Madelmont
JC: Quantitative HRMAS proton total correlation spectroscopy
applied to cultured melanoma cells treated by chloroethyl
nitrosourea: demonstration of phospholipid metabolism alterations.
Magn Reson Med. 49:241–248. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Asai A, Sahani N, Kaneki M, Ouchi Y,
Martyn JA and Yasuhara SE: Primary role of functional ischemia,
quantitative evidence for the two-hit mechanism, and
phosphodiesterase-5 inhibitor therapy in mouse muscular dystrophy.
PLoS One. 2:e8062007. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Hosokawa S, Koseki H, Nagashima M, Maeyama
Y, Yomogida K, Mehr C, Rutledge M, Greenfeld H, Kaneki M, Tompkins
RG, et al: Title efficacy of phosphodiesterase 5 inhibitor on
distant burn-induced muscle autophagy, microcirculation, and
survival rate. Am J Physiol Endocrinol Metab. 304:E922–E933. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Burgmaier G, Schönrock LM, Kuhlmann T,
Richter-Landsberg C and Brück W: Association of increased bcl-2
expression with rescue from tumor necrosis factor-alpha-induced
cell death in the oligodendrocyte cell line OLN-93. J Neurochem.
75:2270–2276. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Tzifi F, Economopoulou C, Gourgiotis D,
Ardavanis A, Papageorgiou S and Scorilas A: The role of BCL2 family
of apoptosis regulator proteins in acute and chronic leukemias. Adv
Hematol. 2012:5243082012. View Article : Google Scholar
|
|
40
|
Davies L, Spiller D, White MR, Grierson I
and Paraoan L: PERP expression stabilizes active p53 via modulation
of p53-MDM2 interaction in uveal melanoma cells. Cell Death Dis.
2:e1362011. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Huo J, Xu S and Lam KP: Fas apoptosis
inhibitory molecule regulates T cell receptor-mediated apoptosis of
thymocytes by modulating Akt activation and Nur77 expression. J
Biol Chem. 285:11827–11835. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Zhou H, Ge Y, Sun L, Ma W, Wu J, Zhang X,
Hu X, Eaves CJ, Wu D and Zhao Y: Growth arrest specific 2 is
up-regulated in chronic myeloid leukemia cells and required for
their growth. PLoS One. 9:e861952014. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Tzika AA, Astrakas LG, Cao H, Mintzopoulos
D, Zhang Q, Padfield K, Yu H, Mindrinos MN, Rahme LG and Tompkins
RG: Murine intramyocellular lipids quantified by NMR act as
metabolic biomarkers in burn trauma. Int J Mol Med. 21:825–832.
2008.PubMed/NCBI
|
|
44
|
Yuzefovych LV, Musiyenko SI, Wilson GL and
Rachek LI: Mitochondrial DNA damage and dysfunction, and oxidative
stress are associated with endoplasmic reticulum stress, protein
degradation and apoptosis in high fat diet-induced insulin
resistance mice. PLoS One. 8:e540592013. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Blankenberg FG: In vivo detection of
apoptosis. J Nucl Med. 49(Suppl 2): 81S–95S. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Vayssier-Taussat M, Kreps SE, Adrie C,
Dall'Ava J, Christiani D and Polla BS: Mitochondrial membrane
potential: a novel biomarker of oxidative environmental stress.
Environ Health Perspect. 110:301–305. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Marchi S, Giorgi C, Suski JM, Agnoletto C,
Bononi A, Bonora M, De Marchi E, Missiroli S, Patergnani S, Poletti
F, et al: Mitochondria-ros crosstalk in the control of cell death
and aging. J Signal Transduct. 2012:3296352012. View Article : Google Scholar
|
|
48
|
Shokolenko I, Venediktova N, Bochkareva A,
Wilson GL and Alexeyev MF: Oxidative stress induces degradation of
mitochondrial DNA. Nucleic Acids Res. 37:2539–2548. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Blasiak J, Glowacki S, Kauppinen A and
Kaarniranta K: Mitochondrial and nuclear DNA damage and repair in
age-related macular degeneration. Int J Mol Sci. 14:2996–3010.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Handschin C and Spiegelman BM: Peroxisome
proliferator-activated receptor gamma coactivator 1 coactivators,
energy homeostasis, and metabolism. Endocr Rev. 27:728–735. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Lin J, Handschin C and Spiegelman BM:
Metabolic control through the PGC-1 family of transcription
coactivators. Cell Metab. 1:361–370. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Supinski GS and Callahan LA: Caspase
activation contributes to endotoxin-induced diaphragm weakness. J
Appl Physiol (1985). 100:1770–1777. 2006. View Article : Google Scholar
|
|
53
|
Tatsumi T, Shiraishi J, Keira N, Akashi K,
Mano A, Yamanaka S, Matoba S, Fushiki S, Fliss H and Nakagawa M:
Intracellular ATP is required for mitochondrial apoptotic pathways
in isolated hypoxic rat cardiac myocytes. Cardiovasc Res.
59:428–440. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Danial NN and Korsmeyer SJ: Cell death:
critical control points. Cell. 116:205–219. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Szczepaniak LS, Babcock EE, Schick F,
Dobbins RL, Garg A, Burns DK, McGarry JD and Stein DT: Measurement
of intracellular triglyceride stores by H spectroscopy: validation
in vivo. Am J Physiol. 276:E977–E989. 1999.PubMed/NCBI
|
|
56
|
Petersen KF, Befroy D, Dufour S, Dziura J,
Ariyan C, Rothman DL, DiPietro L, Cline GW and Shulman GI:
Mitochondrial dysfunction in the elderly: possible role in insulin
resistance. Science. 300:1140–1142. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Petersen KF, Dufour S, Befroy D, Garcia R
and Shulman GI: Impaired mitochondrial activity in the
insulin-resistant offspring of patients with type 2 diabetes. N
Engl J Med. 350:664–671. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Blankenberg FG, Katsikis PD, Storrs RW,
Beaulieu C, Spielman D, Chen JY, Naumovski L and Tait JF:
Quantitative analysis of apoptotic cell death using proton nuclear
magnetic resonance spectroscopy. Blood. 89:3778–3786.
1997.PubMed/NCBI
|
|
59
|
Boren J and Brindle KM: Apoptosis-induced
mitochondrial dysfunction causes cytoplasmic lipid droplet
formation. Cell Death Differ. 19:1561–1570. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Hakumäki JM, Poptani H, Sandmair AM,
Ylä-Herttuala S and Kauppinen RA: 1H MRS detects
polyunsaturated fatty acid accumulation during gene therapy of
glioma: implications for the in vivo detection of apoptosis. Nat
Med. 5:1323–1327. 1999. View
Article : Google Scholar
|
|
61
|
Mullen TD and Obeid LM: Ceramide and
apoptosis: Exploring the enigmatic connections between sphingolipid
metabolism and programmed cell death. Anticancer Agents Med Chem.
12:340–363. 2012. View Article : Google Scholar
|
|
62
|
Martinez TN, Chen X, Bandyopadhyay S,
Merrill AH and Tansey MG: Ceramide sphingolipid signaling mediates
Tumor Necrosis Factor (TNF)-dependent toxicity via caspase
signaling in dopaminergic neurons. Mol Neurodegener. 7:452012.
View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Giussani P, Tringali C, Riboni L, Viani P
and Venerando B: Sphingolipids: key regulators of apoptosis and
pivotal players in cancer drug resistance. Int J Mol Sci.
15:4356–4392. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Aureli M, Murdica V, Loberto N, Samarani
M, Prinetti A, Bassi R and Sonnino S: Exploring the link between
ceramide and ionizing radiation. Glycoconj J. 31:449–459. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Jenkins GM: The emerging role for
sphingolipids in the eukaryotic heat shock response. Cell Mol Life
Sci. 60:701–710. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Van Brocklyn JR and Williams JB: The
control of the balance between ceramide and sphingosine-1-phosphate
by sphingosine kinase: oxidative stress and the seesaw of cell
survival and death. Comp Biochem Physiol B Biochem Mol Biol.
163:26–36. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Yasuhara S, Asai A, Sahani ND and Martyn
JA: Mitochondria, endoplasmic reticulum, and alternative pathways
of cell death in critical illness. Crit Care Med. 35(Suppl):
S488–S495. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Bernardi P and Di Lisa F: The
mitochondrial permeability transition pore: molecular nature and
role as a target in cardioprotection. J Mol Cell Cardiol.
78:100–106. 2015. View Article : Google Scholar :
|
|
69
|
Nabben M, Shabalina IG, Moonen-Kornips E,
van Beurden D, Cannon B, Schrauwen P, Nedergaard J and Hoeks J:
Uncoupled respiration, ROS production, acute lipotoxicity and
oxidative damage in isolated skeletal muscle mitochondria from
UCP3-ablated mice. Biochim Biophys Acta. 1807:1095–1105. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Reynolds HY, Di Sant'Agnese PA and Zierdt
CH: Mucoid Pseudomonas aeruginosa. A sign of cystic fibrosis in
young adults with chronic pulmonary disease? JAMA. 236:2190–2192.
1976. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Scott-Thomas AJ, Syhre M, Pattemore PK,
Epton M, Laing R, Pearson J and Chambers ST: 2-Aminoacetophenone as
a potential breath biomarker for Pseudomonas aeruginosa in the
cystic fibrosis lung. BMC Pulm Med. 10:562010. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Velsor LW, Kariya C, Kachadourian R and
Day BJ: Mitochondrial oxidative stress in the lungs of cystic
fibrosis transmembrane conductance regulator protein mutant mice.
Am J Respir Cell Mol Biol. 35:579–586. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Divangahi M, Balghi H, Danialou G, Comtois
AS, Demoule A, Ernest S, Haston C, Robert R, Hanrahan JW, Radzioch
D and Petrof BJ: Lack of CFTR in skeletal muscle predisposes to
muscle wasting and diaphragm muscle pump failure in cystic fibrosis
mice. PLoS Genet. 5:e10005862009. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Rottner M, Tual-Chalot S, Mostefai HA,
Andriantsitohaina R, Freyssinet JM and Martínez MC: Increased
oxidative stress induces apoptosis in human cystic fibrosis cells.
PLoS One. 6:e248802011. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Moylan JS and Reid MB: Oxidative stress,
chronic disease, and muscle wasting. Muscle Nerve. 35:411–429.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Schwartz LM: Atrophy and programmed cell
death of skeletal muscle. Cell Death Differ. 15:1163–1169. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Aare S, Radell P, Eriksson LI, Akkad H,
Chen YW, Hoffman EP and Larsson L: Effects of corticosteroids in
the development of limb muscle weakness in a porcine intensive care
unit model. Physiol Genomics. 45:312–320. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Xu H, Lam SH, Shen Y and Gong Z:
Genome-wide identification of molecular pathways and biomarkers in
response to arsenic exposure in zebrafish liver. PLoS One.
8:e687372013. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Maestre I, Jordán J, Calvo S, Reig JA,
Ceña V, Soria B, Prentki M and Roche E: Mitochondrial dysfunction
is involved in apoptosis induced by serum withdrawal and fatty
acids in the beta-cell line INS-1. Endocrinology. 144:335–345.
2003. View Article : Google Scholar
|
|
80
|
Lartigue L and Faustin B: Mitochondria:
metabolic regulators of innate immune responses to pathogens and
cell stress. Int J Biochem Cell Biol. 45:2052–2056. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Nicolson GL: Mitochondrial dysfunction and
chronic disease: treatment with natural supplements. Altern Ther
Health Med. at50272013.PubMed/NCBI
|
|
82
|
Frick CG, Fink H, Gordan ML, Eckel B,
Martyn JA and Blobner M: Chronic Escherichia coli infection induces
muscle wasting without changing acetylcholine receptor numbers.
Intensive Care Med. 34:561–567. 2008. View Article : Google Scholar
|
|
83
|
Macallan DC, McNurlan MA, Kurpad AV, de
Souza G, Shetty PS, Calder AG and Griffin GE: Whole body protein
metabolism in human pulmonary tuberculosis and undernutrition:
evidence for anabolic block in tuberculosis. Clin Sci (Lond).
94:321–331. 1998. View Article : Google Scholar
|
|
84
|
Machado AM, Desler C, Bøggild S,
Strickertsson JA, Friis-Hansen L, Figueiredo C, Seruca R and
Rasmussen LJ: Helicobacter pylori infection affects mitochondrial
function and DNA repair, thus, mediating genetic instability in
gastric cells. Mech Ageing Dev. 134:460–466. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Morton RE, Hutchings J, Halliday D, Rennie
MJ and Wolman SL: Protein metabolism during treatment of chest
infection in patients with cystic fibrosis. Am J Clin Nutr.
47:214–219. 1988.PubMed/NCBI
|