Introduction
Aging is defined as the progressive accumulation of
damage over time, leading to the disruption of functions at the
cellular, tissue and organ levels. Eventually, disease and death
are induced by a complex, multifactorial process, involving
genetic, endogenous and environmental factors (1). The consequences of human aging are
mostly visible in the skin, manifesting as increased wrinkling,
sagging, uneven texture and decreased elasticity (2). It has been suggested that aged skin
has a disrupted barrier function and altered permeability,
resulting in a dry appearance and an enhanced risk of skin
disorders (3,4). A number of processes are also
impaired in aged skin, including angiogenesis, lipid and sweat
production, immune function and vitamin D synthesis. This often
results in impaired wound healing, atrophy, vulnerability to
external stimuli and in the development of several benign and
malignant diseases (3). Aging of
the skin is induced by both intrinsic and extrinsic factors
(5,6), all of which lead to a reduced
structural integrity and the loss of physiological function
(6). Critically, understanding
the mechanisms of skin aging is necessary for developing improved
skin care products that delay this process and reduce the hazardous
effects of aging-inducing factors (5,7).
Apigenin (4′,5,7-trihydroxyflavone), a member of the
flavone subclass of flavonoids, is widely found in herbs, fruits
and vegetables, and thus, is a substantial component of the human
diet. It has been shown to possess a variety of biological
characteristics, including antioxidant (8) and anti-inflammatory properties
(9). It has also been shown to
exert tumor-inhibitory effects (10) and to promote neurogenesis
(11). Apigenin has also been
shown to enhance wound healing and tissue repair in the skin of
diabetic rats (12). During the
process of wound healing, fibroblasts secrete collagen, and the
formation of collagen-rich granulation tissue is vital for the
pathophysiological mechanisms of wound closure (13).
Ultraviolet (UV) radiation that reaches the earth's
surface is comprised of wavelength ranges referred to as UVB
(280–315 nm) and UVA (315–400 nm); UV radiation
within the UVC wave band (100–280 nm) is absorbed entirely
within the atmosphere. UV irradiation is the main culprit
implicated in premature skin aging, which is referred to as
photoaging. A number of studies have explored the relative
contributions of UVA and UVB to the aging phenotype (14–16).
Notably, while UVA photons are, on average, 1,000 times less
energetic than UVB photons, they are capable of inducing
aging-related changes even in the dermis, partly due to their
greater average depth of skin penetration than UVB photons
(17).
Photoaging is characterized by the macro- and
micro-structural deterioration of the skin, which includes damage
to collagen fibers, the excessive deposition of abnormal elastic
fibers and increased levels of glycosaminoglycans (18–20).
Among these factors, matrix metalloproteinases (MMPs) are thought
to play a major role in mediating UV-induced skin aging (17). The MMPs are a family of
structurally related molecules, including collagenase-1 (MMP-1),
collage-nase-3 (MMP-13), gelatinases A and B (MMP-2 and MMP-9,
respectively), stromelysin-1 (MMP-3), membrane-type MMPs, and
others, all of which are capable of degrading components of the
extracellular matrix, such as collagen, elastin, fibronectin,
proteoglycans and laminin (21).
In particular, MMP-1 initiates the degradation of type I and III
fibrillary collagen, MMP-9 (gelatinase B) further degrades the
collagen fragments produced, and MMP-3 (stromelysin-1) degrades
type IV collagen and activates pro-MMP-1 (22–24).
In the present study, we examined the protective
effects of apigenin on skin aging and demonstrated that apigenin
induces anti-aging effects in skin by improving its barrier
function and reducing UVA-induced damage.
Materials and methods
Cell culture
Normal human dermal fibroblasts (nHDFs; Lonza,
Basel, Switzerland) were cultured in Dulbecco's modified Eagle's
medium (DMEM; Gibco Life Technologies, Carlsbad, CA, USA),
supplemented with 10% fetal bovine serum (FBS; Sigma-Aldrich, St.
Louis, MO, USA) and 1% penicillin/streptomycin (Gibco Life
Technologies) at 37°C in an atmosphere of 5% CO2.
Apigenin was purchased from Sigma-Aldrich and dissolved in dimethyl
sulfoxide (DMSO).
UVA irradiation
The nHDFs (1×106/well) were seeded into
6-well plates and cultured until 70–80% confluent. Prior to
irradiation, the cells were washed twice with phosphate-buffered
saline (PBS). Fresh PBS was then added, and the cells were
irradiated with UVA light (25 J/cm2 UVA; UVA lamp; UVP,
Inc., Upland, CA, USA). The radiation intensity was monitored by a
fiber optic spectrometer system USB2000 (Ocean Optics, Dunedin, FL,
USA). The control cells were treated identically, except for the
exposure to UV light. Following irradiation, various concentrations
(0–100 µM) of the treatment agent (apigenin) in fresh medium
were added to cells at 37°C for 24 h.
Cell viability assay
The nHDFs were seeded at a density of
3×103 cells/well in 96-well plates and incubated for 24
h. The cells were irradiated with UVA (0–50 J/cm2) and
incubated with various concentrations of apigenin (0–200 mM) for 24
h. nHDF cell toxicity due to apigenin was evaluated using the
EZ-Cytox Cell Viability Assay kit (Itsbio, Seoul, Korea), a
water-soluble tetrazolium salt (WST-1) assay. WST-1 solution was
added to the cultured cells at a volume equal to 10% that of the
culture medium, and the cells were then incubated at 37°C for 1 h.
Cell viability was evaluated by measuring the absorbance at 450 nm
using an iMark microplate reader (Bio-Rad, Hercules, CA, USA).
Isolation of total RNA and quantitative
PCR
Total RNA was isolated using TRIzol reagent
(Invitrogen Life Technologies, Carlsbad, CA, USA) according to the
manufacturer's instructions. The purity and concentration of the
RNA were evaluated using a MaestroNano®, a microvolume
spectrophotometer (Maestrogen, Las Vegas, NV, USA), and cDNAs were
synthesized using the miScript II RT kit (Qiagen, Hilden, Germany)
according to the manufacturer's instructions. In order to evaluate
the expression of MMP-1, quantitative PCR was performed using the
following primers: forward, 5′-TCT GACGTTGATCCCAGAGAGCAG-3′ and
reverse, 5′-CAGGG TGACACCAGTGACTGCAC-3′ using EvaGreen dye (Solis
BioDyne, Tartu, Estonia) with Line-Gene K software (Bioer
Technology Co., Ltd., Hangzhou, China). The Ct value for each gene
was normalized to β-actin using the following primers: forward,
5′-GGATTCCTATGTGGGCGACGA-3′ and reverse,
5′-CGCTCGGTGAGGATCTTCATG-3′. The relative expression levels of each
gene were calculated using the 2−ΔΔCt method, as
previously described (25).
Senescence-associated
(SA)-β-galactosidase assay
The expression of galactosidase as a marker for
senescent nHDFs was determined using the SA-β-galactosidase
staining kit (BioVision, Inc., Milpitas, CA, USA) following the
manufacturer's instructions. The nHDFs were seeded at a density of
2×105 cells/well in 60 mm cell culture plates and
incubated at 37°C until they were 90% confluent. The cells were
then pre-treated with apigenin, irradiated with UVA, and incubated
for 24 h. These cells were washed with PBS and fixed by treatment
with 0.5 ml fixing solution/well (4% formaldehyde, 0.5%
glutaraldehyde in PBS buffer, pH 7.2) for 1 h. The fixed cells were
stained in staining solution mix (staining solution, 470 µl;
staining supplement, 5 µl; 20 mg/ml X-Gal in
dimethyl-formamide, 25 µl) for 24 h, at 37°C. After 1 day,
70% glycerol (1 ml/well) was added, and images were captured using
an an Olympus IX51 microscope (Olympus, Tokyo, Japan).
Human subjects and clinical
evaluation
All clinical evaluations were approved by the Ethics
Committee of the Korea Institute for Skin and Clinical Sciences and
performed in accordance with the Declaration of Helsinki
Principles. We enrolled 40 women, aged over 30 years, in a
randomized and double-blinded clinical trial. The subjects were
selected based on age and were not pregnant or nursing. All
subjects were informed about the objective of the study, signed an
informed consent, and agreed to use only our products for skin care
during the study duration. Factors for dropping out of the trial
included itching, erythema, or hindrance to evaluation by excessive
drinking or smoking. Th subjects were divided into the control and
experimental groups, each containing 20 subjects (control group,
44.40±5.97 years; experimental group, 45.30±6.29 years). All
subjects were subjected to the same conditions, apart from the
experimental group which was administered the test treatment. The
study duration was 4 weeks, and no participants dropped out.
Biometric parameters were measured 3 times: before application, and
then at 2 and 4 weeks after application. An investigator also
questioned the subjects about their condition and performed visual
evaluations for skin disorders, such as erythema, itching, scaling,
edema, tingling and burning sensations, at each visitation.
Experimental procedures
To investigate the effects of apigenin on dermal
density, skin elasticity, skin texture, moisture, transepidermal
water loss (TEWL) and fine wrinkles around the eyes (also known as
crow's feet), the subjects were instructed to apply 2 g of the test
treatment to the face, including the eye rim, every morning and
night for 4 weeks. The subjects and investigators were blinded to
the test and control treatments. At each visit, all subjects washed
with the cleanser provided and lay quietly in a room with a
constant temperature (22±1°C) and humidity (45±5%), so that they
would all be evaluated under the same conditions. The cream
provided to the experimental group contained 1% (wt%) apigenin;
whereas, the cream provided to the control group was prepared using
the same volume of water in the place of apigenin.
Measurement of skin elasticity
To evaluate the improvement in skin elasticity, a
DermaLab USB elasticity probe (Cortex Technology Inc., Hadsund,
Denmark) was applied to the skin, and the results were analyzed
using the associated application software, version 1.09. The
measurement was performed by applying a single fixed elasticity
probe on the left cheek of a subject. To analyze the measured value
(in MPa), Young's modulus (E) was used, and the detected value is
dependent on skin elasticity. To evaluate improvement, measurements
were taken 3 times, before treatment and both at 2 and 4 weeks
after application.
Measurement of dermal density
To evaluate dermal density, a DUB®
SkinScanner (taberna pro medicum, Luneburg, Germany) was utilized.
Dermal density was measured (in µm) 3 cm beside the left
eye, applying a couplant for ultrasonic examination. The analysis
range was limited to the region between the dermis and the upper
panniculus. To evaluate improvement, measurements were performed
three times, before treatment and both 2 and 4 weeks after first
application.
Measurement of length of crow's feet
To evaluate the improvement of wrinkles,
particularly crow's feet, a Robo skin analyzer CS50 (Inforward
Inc., Tokyo, Japan) was used. All facial images were captured under
the same position and with equal lighting. The capturing was
performed 3 times at each evaluation, on the front, left and right
sides of the face. To evaluate improvement, measurements were
performed 3 times, before treatment and both at 2 and 4 weeks after
application. We analyzed the captured images matching the facial
feature points to reenact accurately, and the measurement unit was
in mm.
Evaluation of skin moisture
To evaluate improvement in skin moisture, a DermaLab
USB moisture probe (Cortex Technology Inc.) was applied to the
skin, and the data were analyzed using the associated application
software, version 1.09. All subjects were evaluated on the same
region of the right cheek, 5 times consecutively, and we calculated
the mean value, excluding the maximum and minimum values. To
evaluate improvement, measurements were performed 3 times, before
treatment and both at 2 and 4 weeks after application. The probe
measures skin conductance in micro Siemens (µS), and the
numerical value is dependent on skin moisture.
Measurements of TEWL
To evaluate improvements in TEWL, a DermaLab USB
TEWL probe (Cortex Technology, Inc.) was applied to the skin, and
the data were analyzed using the associated application software,
version 1.09. The measurement was performed 5 times consecutively,
on the right cheek of the subjects, and we calculated the mean
value, excluding the maximum and minimum values. To evaluate
improvement, measurements were performed 3 times, before treatment
and both at 2 and 4 weeks after application.
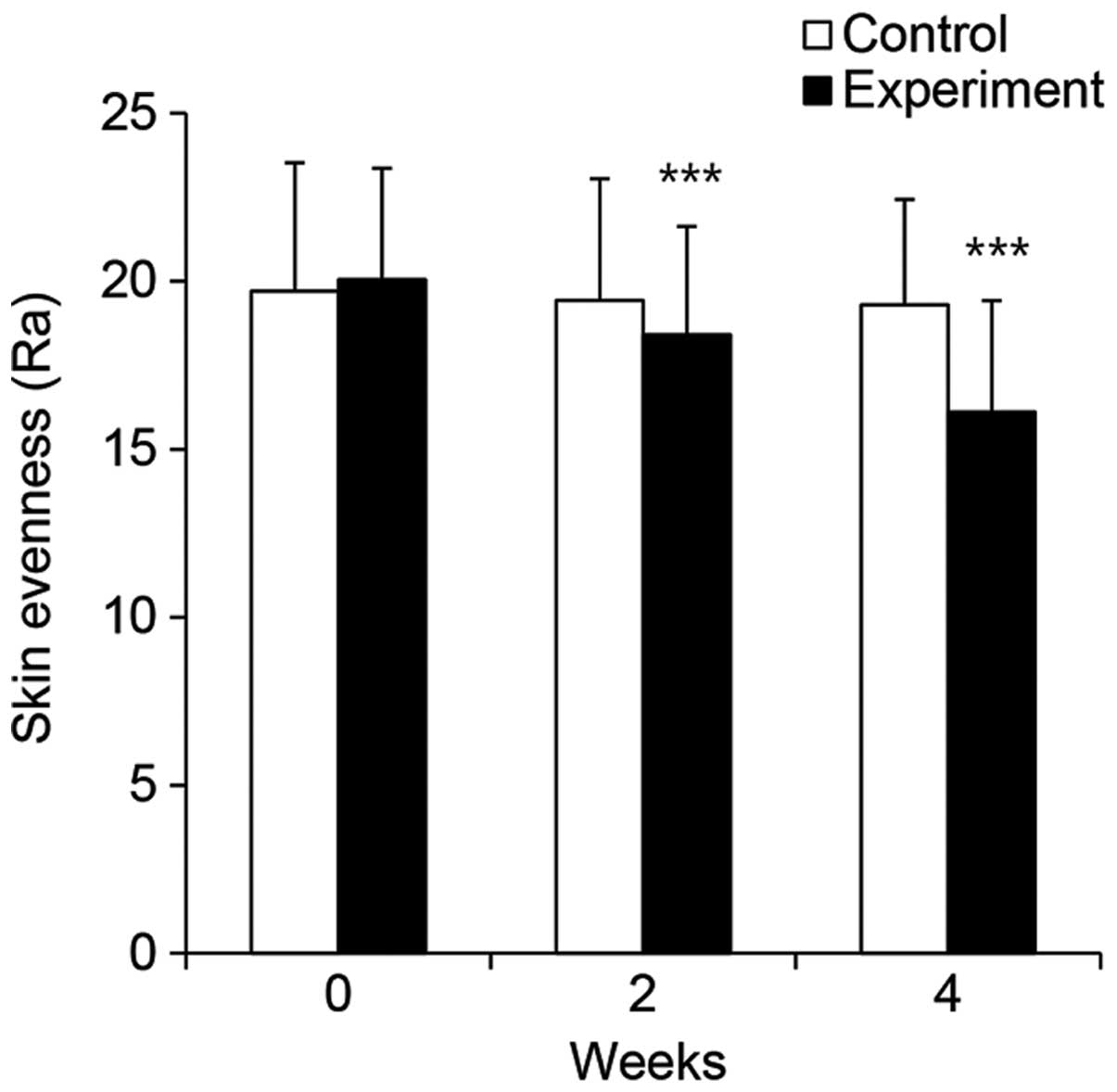
Measurements of facial evenness
To evaluate improvements in facial evenness, a
PRIMOS Lite system (field of view 45×30; GFMesstechnik GmbH,
Teltow, Germany) was used, and the captured clinical images were
analyzed using the associated imaging software, PRIMOS Lite version
5.6E. The images were captured 3 times consecutively, on the left
side of the forehead of the subjects. We analyzed facial evenness
by calculating surface roughness, Ra (average of all heights and
epths to the reference plane) value. The Ra value, which is the
most well used measurement for facial evenness, is the arithmetic
mean of the absolute values within the total measurement range. To
evaluate improvement, measurements were performed 3 times, before
treatment and both at 2 and 4 weeks after application.
Statistical analysis
For cellular efficacy tests, all results are
presented as the mean percentage ± standard deviation (SD) of 3
independent experiments. Differences with a P-value <0.05, as
determined by the Student's t-test, were considered statistically
significant. For clinical efficacy tests, statistical analyses were
conducted using SPSS software (SPSS, version 17.0 for Windows; IBM
SPSS, Armonk, NY, USA). Paired Student's t-tests were performed in
the cases of repeated measurements on the same subject. To analyze
subject questionnaires, the mean values, standard deviations and
percentages were calculated. The formula used to measure the
percentage change for each skin parameter was 'Percentage change =
[(A – B)/B] ×100', where A is defined as the individual value of
any parameter at the 2-and 4-week visits, and B represents the zero
hour of the assessed parameter.
Results
Cytotoxicity of apigenin and UVA in human
dermal fibroblasts
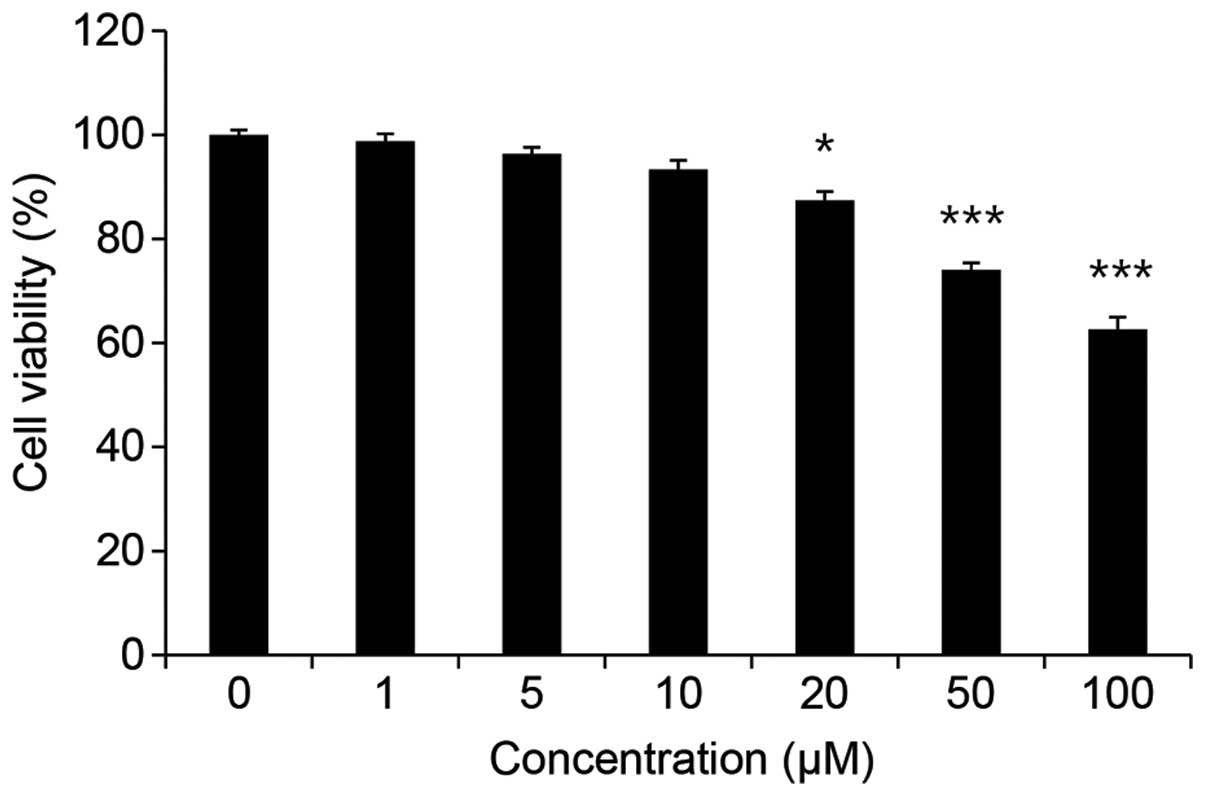
To determine whether apigenin affects nHDF
viability, the cells were exposed to apigenin at concentrations
ranging from 0–100 µM for 24 h. As shown in Fig. 1, apigenin reduced cell viability
by 1.23% at 1 µM, 3.63% at 5 µM, and 12.61% at 20
µM. The apigenin-induced cytotoxicity increased
significantly at concentrations >50 µM. Therefore, we
used the concentration of 20 µM as the maximum concentration
in all the subsequent experiments.
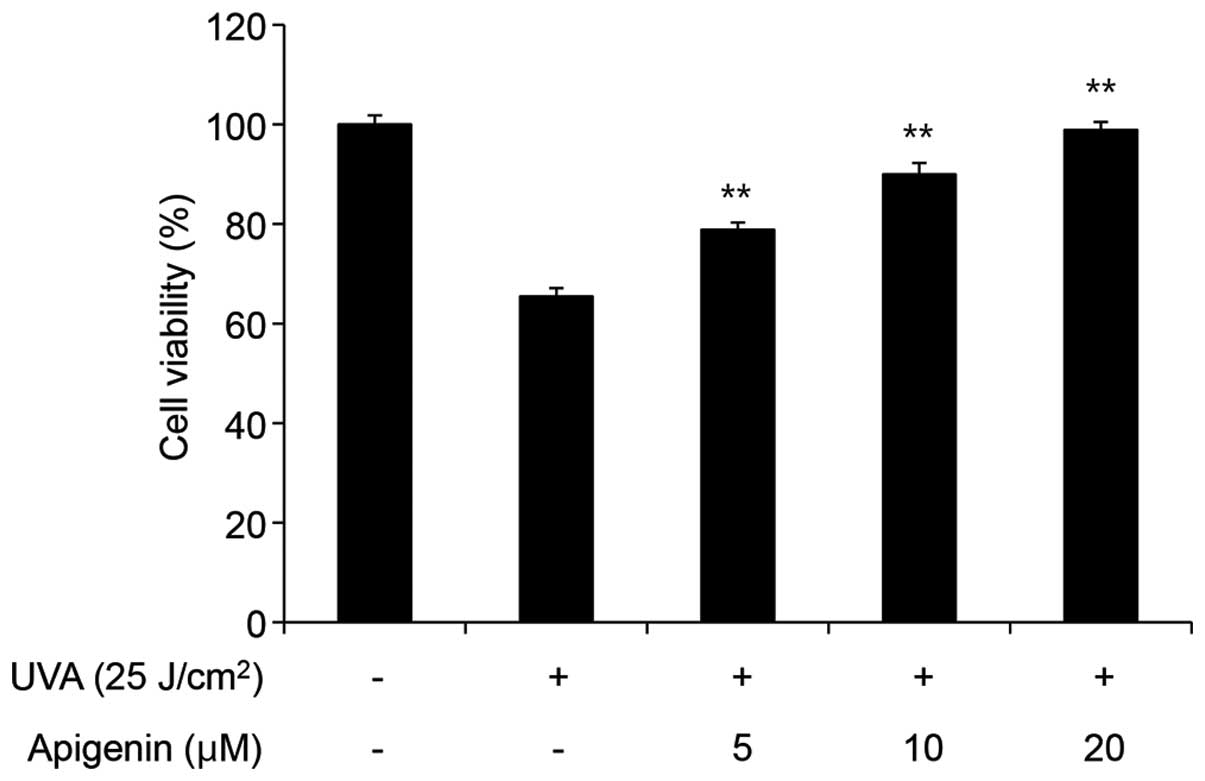
To evaluate the effects of apigenin on the viability
of damaged cells, the nHDFs were irradiated with 25
J/cm2 UVA, and these cells were then treated with
apigenin at various concentrations. As shown in Fig. 2, this dose of UVA reduced cell
viability by 34.60%; however, treatment with 10 and 20 µM
apigenin increased viability back to 90.00 and 98.92%,
respectively, suggesting that apigenin protects cells from
UVA-induced cytotoxicity.
Senescent cell detection assay
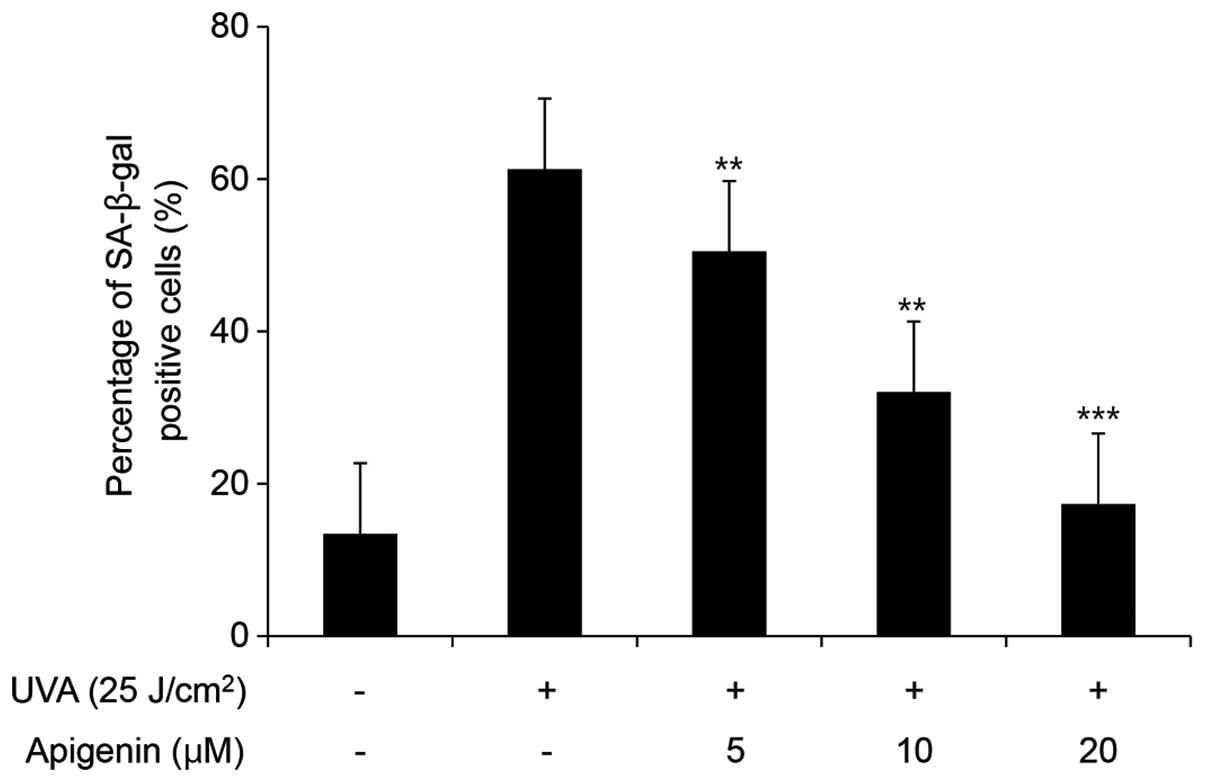
We then investigated the ability of apigenin to
inhibit senescence, using a SA-β-galactosidase assay. When the
cells were irradiated with 25 J/cm2 UVA, the percentage
of senescent cells was found to be as high as 61.29%. This number
decreased in a dose-dependent manner to 50.49, 32.03 and 17.34%
when cells were post-treated with 5, 10 and 20 µM apigenin,
respectively (Fig. 3). These
results indicate that UVA acts as a stimulator of senescence, and
that apigenin can inhibit UVA-induced cellular senescence.
Analysis of MMP-1 mRNA expression
UVA radiation corresponds to 90–95% of solar
UV radiation (26) and is mainly
responsible for the high production of reactive oxygen species
(ROS) in skin, leading to oxidative stress (27). ROS are able to induce several
disruptive cellular processes, such as senescence, DNA cleavage,
lipid peroxidation and cell death (28). In addition, UVA induces the
expression of MMP-1 in dermal fibroblasts in vivo and
stimulates the expression of MMP-1, MMP-2 and MMP-3 in cell
culture, all of which are induced during wrinkling and skin aging
(29,30). MMP-1, when generated from
fibroblasts, has been reported to ultimately promote a decrease in
collagen (23,31,32). Collagen is the most abundant
protein in the dermis, and type-1 collagen, in particular, provides
structure to skin and composes >90% of collagen in the body
(33). We found that the mRNA
expression of MMP-1 in the UVA-irradiated nHDFs increased up to
2.91-fold as compared with the non-irradiated cells. However,
treatment with 5, 10 and 20 µM apigenin reduced MMP-1
expression 2.43-, 1.85- and 1.31-fold, respectively (Fig. 4), indicating that apigenin
inhibits the UVA-induced induction of MMP-1 expression.
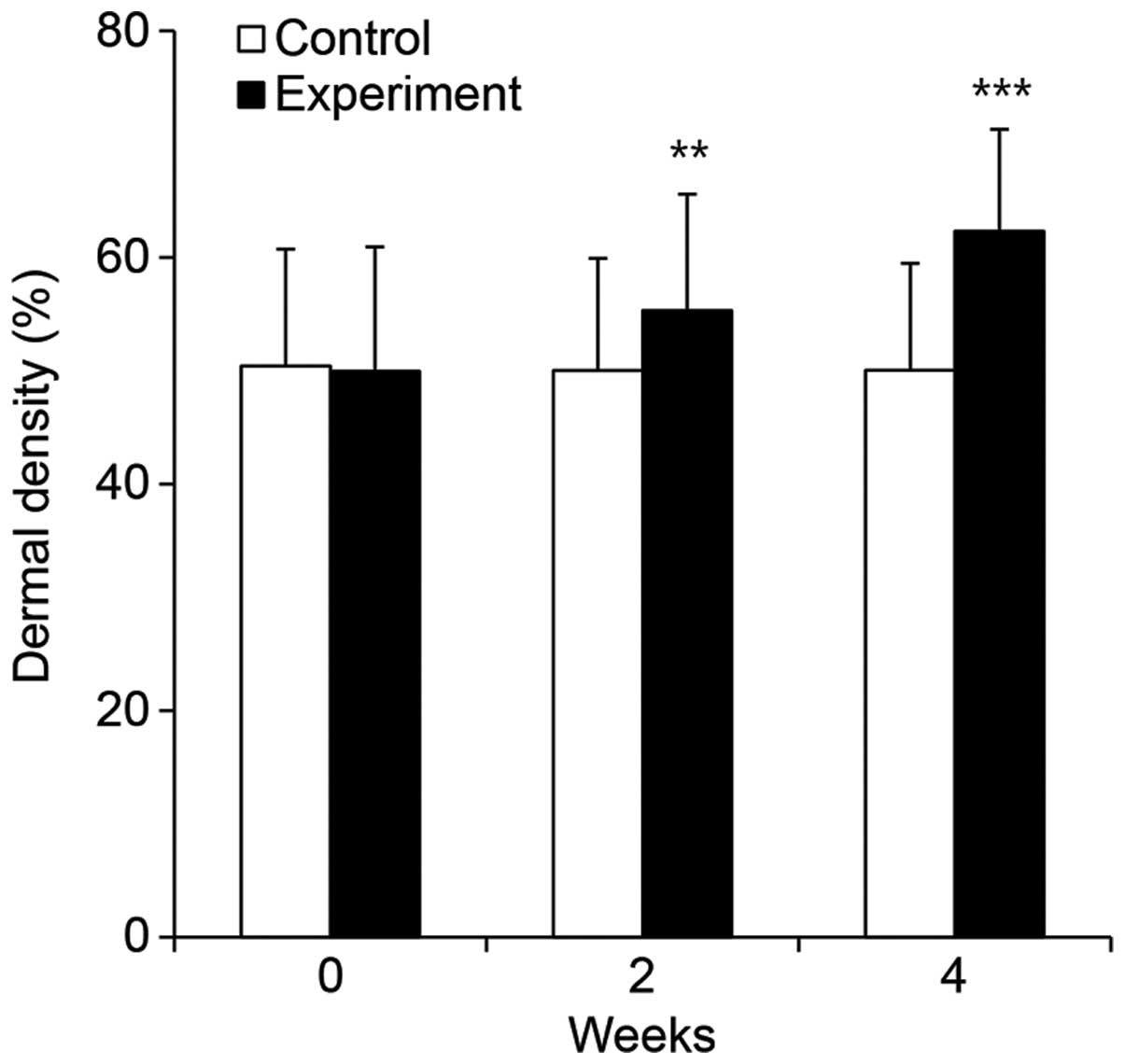
Evaluation of dermal density
To evaluate the effects of apigenin on skin aging
in vivo, we measured the density of the dermis in subjects
treated with a cream containing 1% apigenin. Using a DUB
SkinScanner, we found that the subjects using the
non-apigenin-containing control cream displayed a mean density of
50.41 µm before use, and densities of 50.02 and 50.05
µm after 2 and 4 weeks, respectively (Fig. 5). However, subjects using the
apigenin-containing cream displayed a mean density of 49.96
µm before use, and densities of 55.31 and 62.32 after 2 and
4 weeks of application, respectively (Fig. 5). Dermal density measurement,
represented as a mathematical value, is proportional to density,
and these experimental data were statistically significant
(P<0.001). To compare the results from the treatment and control
groups, we calculated the improvement as a percentage based on the
density values before and after application. Using this metric, the
dermal density improvement was found to be −0.77 and −0.72% after 2
and 4 weeks of application, respectively, in the control group.
Conversely, in the experimental group, the dermal density
improvement was calculated as 10.70 and 24.75% after 2 and 4 weeks
of application, respectively. These results suggest that the
topical application of apigenin enhances dermal thickness.
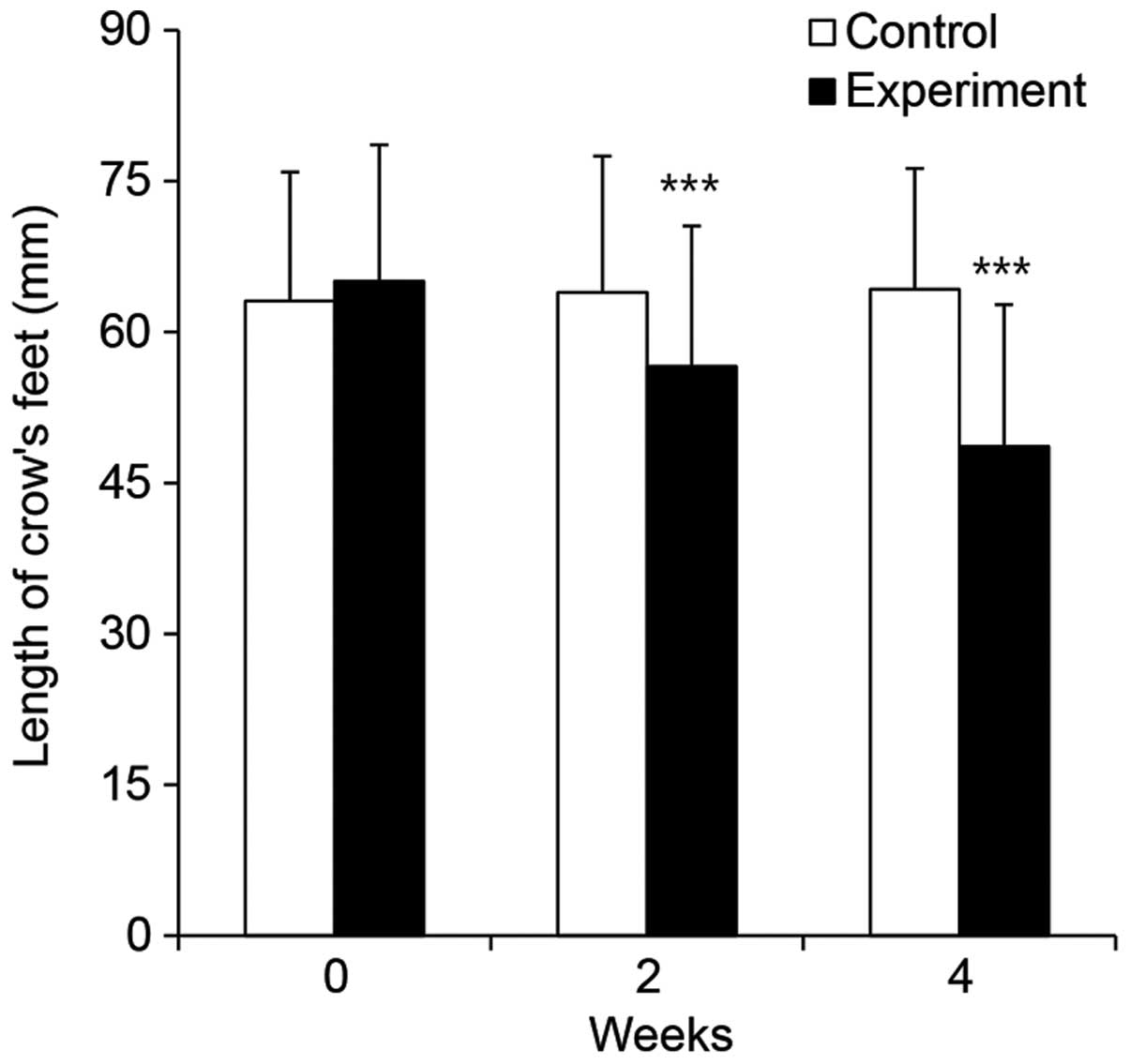
Evaluation of crow's feet length
We then measured the length of crow's feet in the
subjects treated with the apigenin-containing cream and the
controls. In the control group, the mean length was found to be
63.10 mm before application, and 63.95 and 64.25 mm after 2 and 4
weeks of application, respectively (Fig. 6). In the experimental group, the
mean length was 65.05 mm prior to application, and 56.60 and 48.65
mm after 2 and 4 weeks of application, respectively (Fig. 6). The measured values for the
experimental group were statistically significant (P<0.001). To
compare the results from the control and experimental groups, we
calculated the improvement as a percentage based on the values
before and after application. For the control group, the percentage
improvement was calculated as −1.35 and −1.82% after 2 and 4 weeks
of application, respectively. Whereas for the experimental group,
the percentage improvement was found to be 12.99 and 25.21% after 2
and 4 weeks of application, respectively. These data suggest that
the topical application of apigenin can lead to a reduction in
wrinkle length.
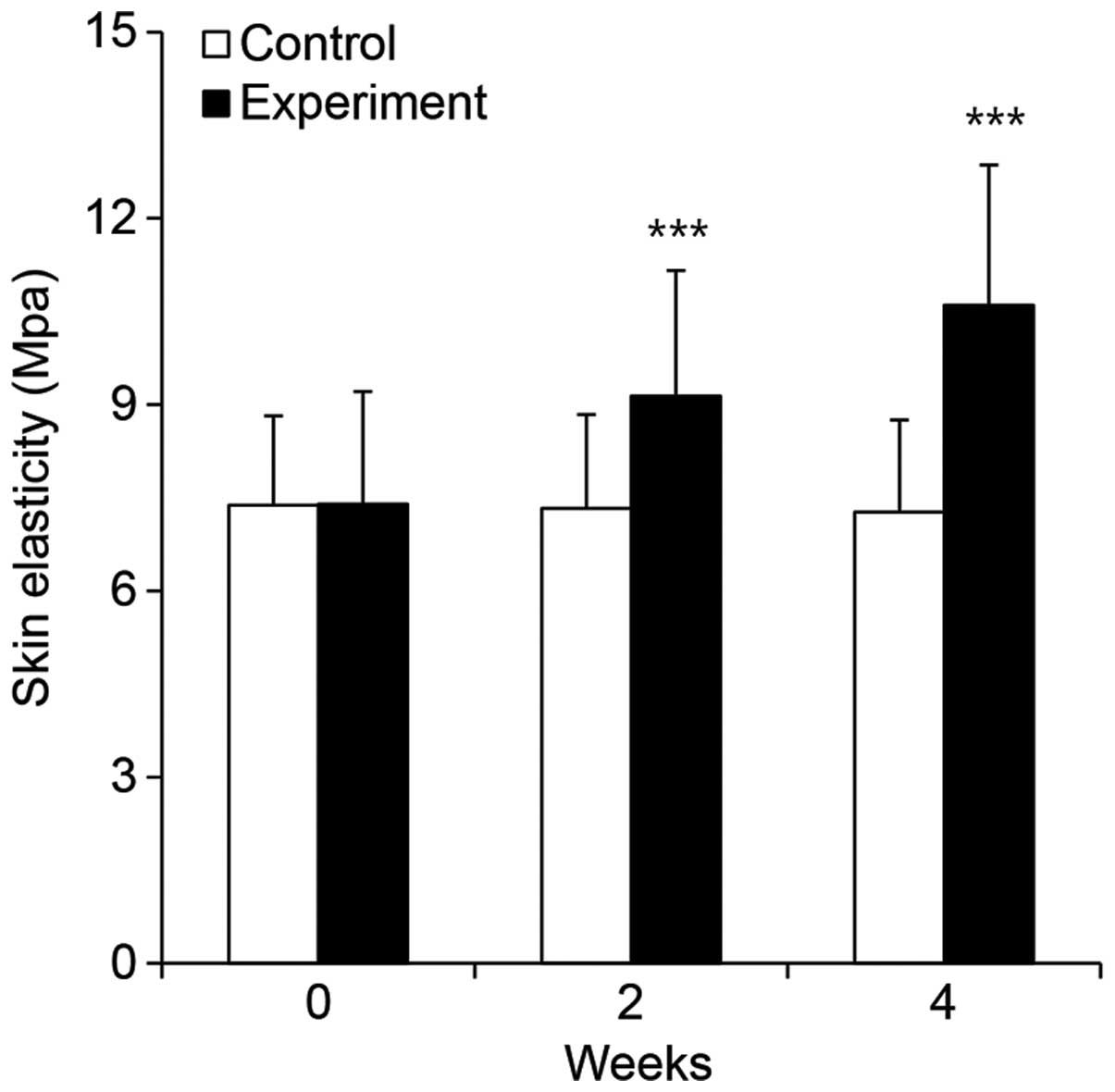
Evaluation of skin elasticity
The dermis is composed of an extracellular matrix
consisting of fibrous proteins, such as collagen and elastin, and
is involved in the regulation of skin elasticity. Factors such as
ROS, UV, or age can cause skin damage, wrinkle formation and a
reduction in elasticity through the estructural denaturation of
collagen and elastin (34). In
order to examine the effects of apigenin on skin elasticity, we
measured elasticity in subjects treated with apigenin-containing
cream or the control cream using a DermaLab USB probe. In the
control group, elasticity was found to be 7.38 MPa before
application, and 7.33 and 7.27 MPA after 2 and 4 weeks of
application, respectively. In the experimental group, elasticity
was 7.40 MPa before application, and 9.14 and 10.60 MPa after 2 and
4 weeks of application, respectively (Fig. 7). The experimental group values
were statistically significant (P<0.001). To compare the results
from the control and experimental groups, we calculated the
improvement as a percentage based on the values before and after
application. For the control group, the percentage improvement was
calculated to be −0.68 and −1.42% after 2 and 4 weeks of
application, respectively. However, the experimental group showed
an improvement of 23.60 and 43.34% after 2 and 4 weeks of
treatment, respectively. These results suggest that the topical
applicatino of apigenin increases skin elasticity.
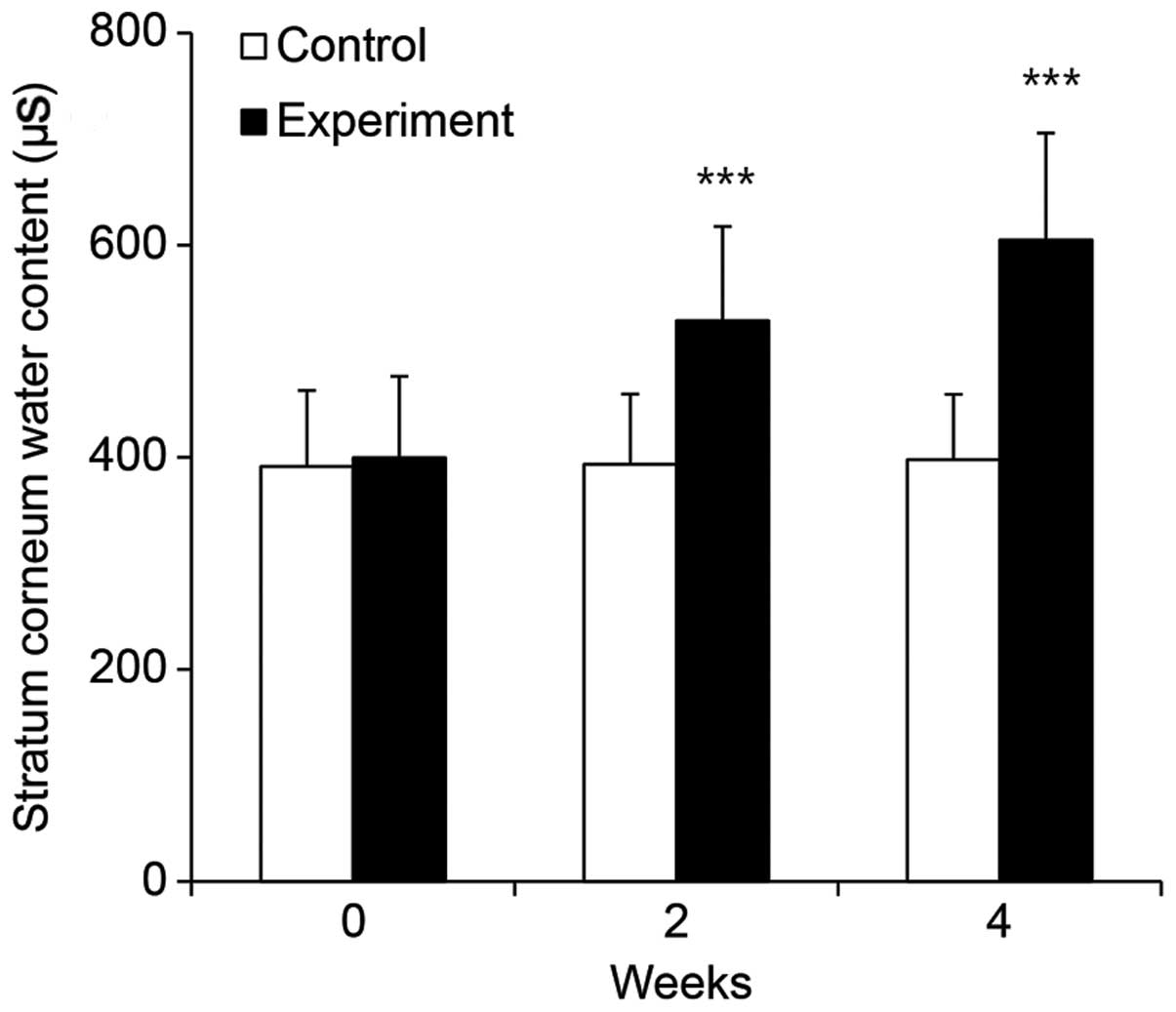
Apigenin-containing cream improves skin
hydration
Keratinocyte moisture content is pivotal for
maintaining moisture in the skin. Normal keratinocytes maintain
10–30% moisture; however, when the moisture content drops
below 10%, keratinocytes are unable to maintain the skin's barrier
function, and skin becomes dry, acquires an uneven texture and
produces wrinkles, accelerating senescence (4). To evaluate the effect of apigenin
treatment on skin moisture, we analyzed the skin moisture content
in our study subjects using the DermaLab USB moisture probe. We
found that the moisture content in the control group was 391.25
µS before use, and 393.30 and 397.87 µS after 2 and 4
weeks of application, respectively (Fig. 8). By contrast, the moisture
content in the experimental group, which used the
apigenin-containing cream, was 399.48 µS before use, and
528.75 and 604.74 µS after 2 and 4 weeks of application,
respectively (Fig. 8). To compare
the results from the control and experimental groups, we calculated
the degree of improvement as a percentage based on the values
before and after application. For the control group, moisture was
increased by 0.52 and 1.69% after 2 and 4 weeks, respectively.
These changes were not statistically significant (P>0.05),
indicating that the control cream had no measurable effect on
moisture content. Conversely, the use of the apigenin-containing
cream significantly improved skin moisture by 32.36 and 51.38%
after 2 and 4 weeks, respectively (P<0.001). These data
demonstrate that use of apigenin-containing cream results in an
improved skin moisture content.
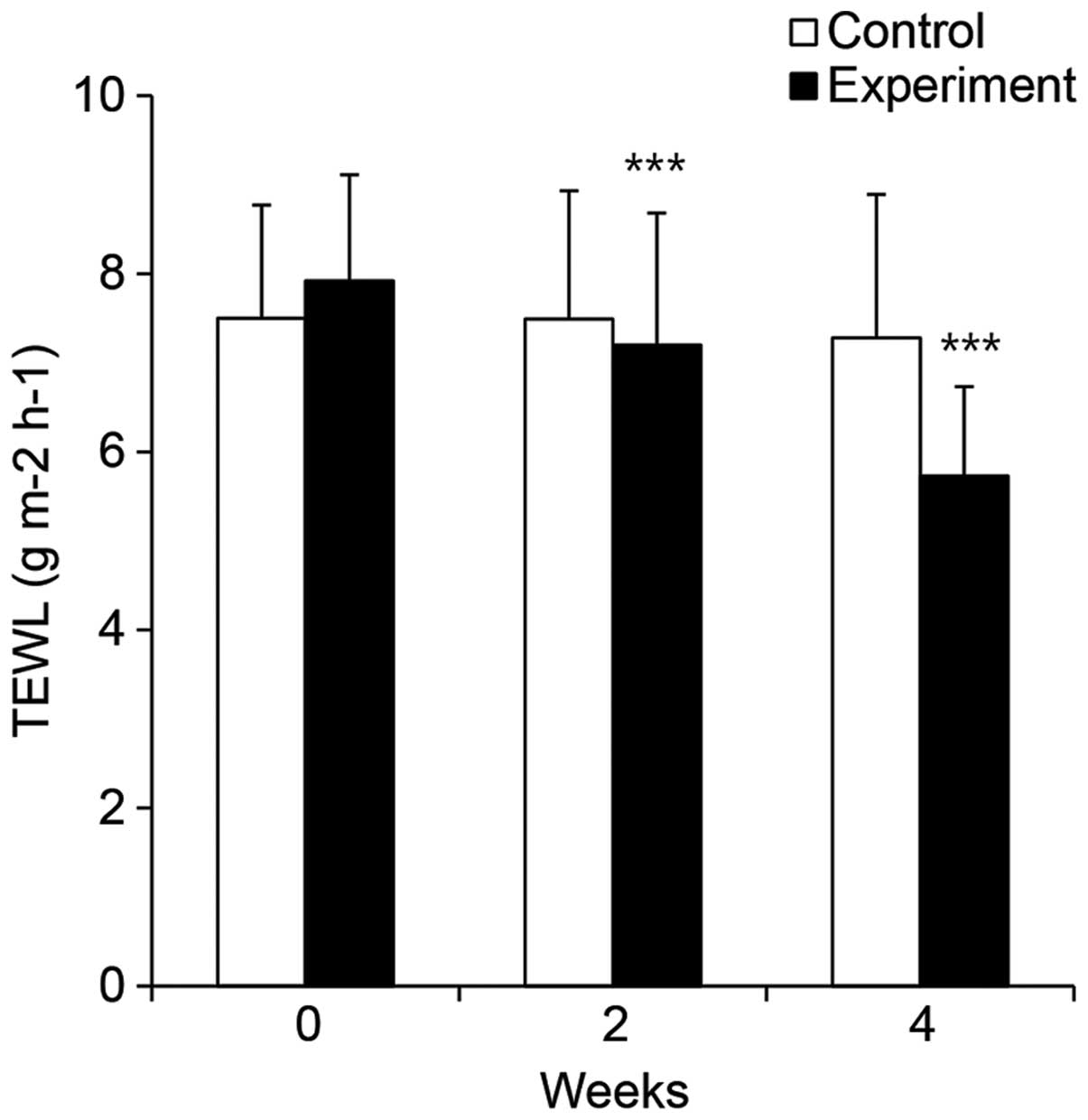
Apigenin-containing cream improves
TEWL
To determine the efficacy of apigenin as a skin
moisturizer, we used the DermaLab USB TEWL probe to measure TEWL in
the skin of subjects who used either the control or
apigenin-containing cream. In the control subjects, the TEWL was
found to be 7.50 g m−2 h−1 before use, and
7.49 and 7.28 g m−2 h−1 after 2 and 4 weeks
of application, respectively (Fig.
9). By contrast, in the experimental group, the TEWL was 7.92 g
m−2 h−1 before use, and 7.20 and 5.73 g
m−2 h−1 after 2 and 4 weeks of application,
respectively (Fig. 9). To compare
the results from the control and experimental groups, we calculated
the improvement in TEWL as a percentage based on the values before
application. In the control group, TEWL was increased by 0.20 and
2.93% after 2 and 4 weeks of use, respectively. These changes were
not statistically significant (P>0.05), indicating that the
control cream had no measurable effect on TEWL. Conversely, the use
of the apigenin-containing cream significantly improved the TEWL by
9.10 and 27.61% after 2 and 4 weeks, respectively (p<0.001).
Through these experiments, we identified an improvement in TEWL as
an outcome of using the apigenin-containing cream.
Use of apigenin-containing cream improves
the evenness of skin texture
The thickness of the stratum corneum changes
depending on its moisture content, and insufficient moisture in
this layer gradually roughens skin texture (35). To investigate the effects of the
apigenin-containing cream on skin texture, facial skin evenness was
measured using a PRIMOS Lite system. Evenness in the control group
was 19.71 Ra before use, and 19.43 and 19.30 Ra after 2 and 4 weeks
of application, respectively (Fig.
10). By contrast, skin evenness in the experimental group was
20.05 Ra before use, and 18.41 and 16.11 Ra after 2 and 4 weeks of
application, respectively (Fig.
10). To compare the results from the control and experimental
groups, we calculated the improvement as a percentage based on the
value before application. Consequently, we found that skin texture
in the control group improved by 1.42 and 2.06%, after 2 and 4
weeks of use, respectively. These data were not statistically
significant (P>0.05), indicating that the control cream had no
measurable effect on skin texture. However, the use of the
apigenin-containing cream significantly improved the evenness of
skin texture by 8.20 and 19.65% after 2 and 4 weeks of application
(P<0.001), respectively, suggesting that the use of the
apigenin-containing cream can improve skin texture.
Analysis of adverse effects of
apigenin-containing cream
In this study, investigators questioned the subjects
individually about the condition of their skin and performed a
visual evaluation of skin reactions, including erythema, itching,
scaling, tingling, tightness, prickling and burning sensations at
each visit. No extraordinary reactions were reported based on
either visual evaluation or the questionnaire (Table I).
 | Table IAdverse skin reactions reported by
the subjects. |
Table I
Adverse skin reactions reported by
the subjects.
| Abnormal
reaction | Severity | Abnormal
reaction | Severity |
|---|
| Erythema | 0a | Tingling | 0 |
| Swelling
(edema) | 0 | Burning | 0 |
| Scaling
(epidermis) | 0 | Tightness | 0 |
| Itching | 0 | Prickling | 0 |
Discussion
Apigenin has been reported to have various
biological activities in various cell types, such as antioxidant,
anti-inflammatory, anti-mutagenic and anti-tumorigenic properties
(36–39). However, it has not been determined
whether apigenin can affect the aging process. In this study, we
examined the effects of apigenin, particularly with regard to skin
aging and wrinkling, using cellular and clinical efficacy
experiments.
We first evaluated the viability of nHDFs that were
irradiated with 25 J/cm2 UVA and found that the
post-treatment of UVA-irradiated nHDFs with apigenin significantly
reduced cell cytotoxicity. This suggests that apigenin can reduce
and/or mitigate UVA-induced cellular damage. We then evaluated the
effects of apigenin on cellular senescence using a
SA-β-galactosidase assay and found that while the percentage of
senescent nHDFs increased in response to UVA irradiation, treatment
with apigenin reduced the percentage of senescent cells in a
dose-dependent manner. Furthermore, under the same conditions, the
mRNA expression of MMP-1 collage-nase-1, which is a reported
initiator for the degradation of type I and III fibrillary collagen
and is induced in response to UVA irradiation, was reduced by
apigenin in a dose-dependent manner (17). Thus, we demonstrated the cellular
efficacy of apigenin in inhibiting UVA-induced growth arrest,
cellular senescence and the expression of MMP-1 in nHDFs.
UVA, a component of the UV spectrum, has been
reported to have a greater average skin penetration than other UV
types. Based on previous studies (17,29), UV irradiation, including UVA, is
the main cause of skin aging, referred to as photoaging. It has
been reported that collagen fibers, which are dermal components
that maintain skin elasticity, are fragmented in photoaging skin
(40). Furthermore, UV
irradiation was found to decrease collagen synthesis and increase
collagenolytic MMP synthesis in dermal fibroblasts (22,23,41), which are believed to contribute to
the furrows observed in photoaging skin. MMPs are capable of
degrading all components of the extracellular matrix and are
upregulated by UV.
Based on the results of our cellular experiments
demonstrating an apigenin-mediated protection from UVA-induced
toxicity and an inhibition of MMP-1 upregulation in nHDFs, we
constructed an apigenin-containing cream and a
non-apigenin-containing control and enrolled 40 women (>30 years
old) in a randomized and double-blinded clinical trial to examine
the effects of apigenin on aging skin in vivo. We then
evaluated a number of features associated with aging in the skin of
subjects who used either the apigenin-containing cream or the
control. Of note, we detected a significant improvement in dermal
density and skin elasticity, and a reduction in the length of fine
wrinkles, particularly crow's feet, after 2 and 4 weeks of
application in the subjects using the apigenin-containing cream.
These results indicate that the topical application of apigenin
reduces aging phenomena and its aging-associated clinical
signs.
The skin is an important organ that separates the
human body from the external environment. It has been previously
reported that both the barrier function and the water-holding
capacity of human skin are decreased by solar UV exposure (42). Therefore, the dryness of
photoaging skin cannot be explained only under the direct influence
of UV irradiation to skin cells. Therefore, we also measured skin
moisture content, TEWL, and skin texture in subjects treated with
apigenin-containing cream or the control. We found that all these
parameters were significantly improved after 2 and 4 weeks of use
in those who applied the apigenin-containing cream. These results
strongly suggest that the topical application of the apigenin cream
can improve aging skin, by enhancing the skin's barrier
function.
Acknowledgments
This study was supported by the KU Research
Professor Program (H.-J. Cha) of Konkuk University. Support was
also provided by grants from the Ministry of Science, ICT and
Future Planning (grant no. 20110028646), the Korean Health
Technology R&D Project, the Ministry of Health & Welfare
(grant no. HN13C0075), and the Ministry of Oceans and Fisheries,
Republic of Korea (grant no. OF123321).
References
|
1
|
Viña J, Borrás C and Miquel J: Theories of
ageing. IUBMB Life. 59:249–254. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Jenkins G: Molecular mechanisms of skin
ageing. Mech Ageing Dev. 123:801–810. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zouboulis CC and Makrantonaki E: Clinical
aspects and molecular diagnostics of skin aging. Clin Dermatol.
29:3–14. 2011. View Article : Google Scholar
|
|
4
|
Hashizume H: Skin aging and dry skin. J
Dermatol. 31:603–609. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Farage MA, Miller KW, Elsner P and Maibach
HI: Intrinsic and extrinsic factors in skin ageing: a review. Int J
Cosmet Sci. 30:87–95. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Landau M: Exogenous factors in skin aging.
Curr Probl Dermatol. 35:1–13. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Elsner P, Fluhr JW, Gehring W, Kerscher
MJ, Krutmann J, Lademann J, Makrantonaki E, Wilhelm KP and
Zouboulis CC: Anti-aging data and support claims - consensus
statement. J Dtsch Dermatol Ges. 9(Suppl 3): S1–32. 2011.
View Article : Google Scholar
|
|
8
|
Sharma H, Kanwal R, Bhaskaran N and Gupta
S: Plant flavone apigenin binds to nucleic acid bases and reduces
oxidative DNA damage in prostate epithelial cells. PLoS One.
9:e915882014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wang J, Liu YT, Xiao L, Zhu L, Wang Q and
Yan T: Anti-inflammatory effects of apigenin in
lipopolysac-charide-induced inflammatory in acute lung injury by
suppressing COX-2 and NF-kB pathway. Inflammation. 37:2085–2090.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Polier G, Giaisi M, Köhler R, Müller WW,
Lutz C, Buss EC, Krammer PH and Li-Weber M: Targeting CDK9 by
wogonin and related natural flavones potentiates the anti-cancer
efficacy of the Bcl-2 family inhibitor ABT-263. Int J Cancer.
136:688–698. 2015.
|
|
11
|
Taupin P: Apigenin and related compounds
stimulate adult neurogenesis. Mars, Inc., the Salk Institute for
Biological Studies: WO2008147483. Expert Opin Ther Pat. 19:523–527.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lodhi S and Singhai AK: Wound healing
effect of flavonoid rich fraction and luteolin isolated from
Martynia annua Linn. on streptozotocin induced diabetic rats. Asian
Pac J Trop Med. 6:253–259. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Singer AJ and Clark RA: Cutaneous wound
healing. N Engl J Med. 341:738–746. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gonzaga ER: Role of UV light in
photodamage, skin aging, and skin cancer: importance of
photoprotection. Am J Clin Dermatol. 10(Suppl 1): 19–24. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ham SA, Kang ES, Lee H, Hwang JS, Yoo T,
Paek KS, Park C, Kim JH, Lim DS and Seo HG: PPARδ inhibits
UVB-induced secretion of MMP-1 through MKP-7-mediated suppression
of JNK signaling. J Invest Dermatol. 133:2593–2600. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lee YK, Cha HJ, Hong M, Yoon Y, Lee H and
An S: Role of NF-κB-p53 crosstalk in ultraviolet A-induced cell
death and G1 arrest in human dermal fibroblasts. Arch Dermatol Res.
304:73–79. 2012. View Article : Google Scholar
|
|
17
|
Mac-Mary S, Sainthillier JM, Jeudy A,
Sladen C, Williams C, Bell M and Humbert P: Assessment of
cumulative exposure to UVA through the study of asymmetrical facial
skin aging. Clin Interv Aging. 5:277–284. 2010.PubMed/NCBI
|
|
18
|
Smith JG Jr, Davidson EA, Sams WM Jr and
Clark RD: Alterations in human dermal connective tissue with age
and chronic sun damage. J Invest Dermatol. 39:347–350. 1962.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Grewe M, Trefzer U, Ballhorn A, Gyufko K,
Henninger H and Krutmann J: Analysis of the mechanism of
ultraviolet (UV) B radiation-induced prostaglandin E2 synthesis by
human epidermoid carcinoma cells. J Invest Dermatol. 101:528–531.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Chung JH, Seo JY, Choi HR, Lee MK, Youn
CS, Rhie G, Cho KH, Kim KH, Park KC and Eun HC: Modulation of skin
collagen metabolism in aged and photoaged human skin in vivo. J
Invest Dermatol. 117:1218–1224. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Inomata S, Matsunaga Y, Amano S, Takada K,
Kobayashi K, Tsunenaga M, Nishiyama T, Kohno Y and Fukuda M:
Possible involvement of gelatinases in basement membrane damage and
wrinkle formation in chronically ultraviolet B-exposed hairless
mouse. J Invest Dermatol. 120:128–134. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Fisher GJ, Datta SC, Talwar HS, Wang ZQ,
Varani J, Kang S and Voorhees JJ: Molecular basis of sun-induced
premature skin ageing and retinoid antagonism. Nature. 379:335–339.
1996. View
Article : Google Scholar : PubMed/NCBI
|
|
23
|
Fisher GJ, Wang ZQ, Datta SC, Varani J,
Kang S and Voorhees JJ: Pathophysiology of premature skin aging
induced by ultraviolet light. N Engl J Med. 337:1419–1428. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Fisher GJ, Talwar HS, Lin J, Lin P,
McPhillips F, Wang Z, Li X, Wan Y, Kang S and Voorhees JJ: Retinoic
acid inhibits induction of c-Jun protein by ultraviolet radiation
that occurs subsequent to activation of mitogen-activated protein
kinase pathways in human skin in vivo. J Clin Invest.
101:1432–1440. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) Method. Methods. 25:402–408. 2001.
View Article : Google Scholar
|
|
26
|
Nichols JA and Katiyar SK: Skin
photoprotection by natural polyphenols: Anti-inflammatory,
antioxidant and DNA repair mechanisms. Arch Dermatol Res.
302:71–83. 2010. View Article : Google Scholar
|
|
27
|
Pandel R, Poljšak B, Godic A and Dahmane
R: Skin photoaging and the role of antioxidants in its prevention.
ISRN Dermatol. 930164:20132013.
|
|
28
|
Tedesco AC, Martínez L and González S:
Photochemistry and photobiology of actinic erythema: Defensive and
reparative cutaneous mechanisms. Braz J Med Biol Res. 30:561–575.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Scharffetter K, Wlaschek M, Hogg A, Bolsen
K, Schothorst A, Goerz G, Krieg T and Plewig G: UVA irradiation
induces collagenase in human dermal fibroblasts in vitro and in
vivo. Arch Dermatol Res. 283:506–511. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Chung JH, Seo JY, Lee MK, Eun HC, Lee JH,
Kang S, Fisher GJ and Voorhees JJ: Ultraviolet modulation of human
macrophage metalloelastase in human skin in vivo. J Invest
Dermatol. 119:507–512. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Burke EM, Horton WE, Pearson JD, Crow MT
and Martin GR: Altered transcriptional regulation of human
interstitial collagenase in cultured skin fibroblasts from older
donors. Exp Gerontol. 29:37–53. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Vincenti MP, White LA, Schroen DJ, Benbow
U and Brinckerhoff CE: Regulating expression of the gene for matrix
metalloproteinase-1 (collagenase): mechanisms that control enzyme
activity, transcription, and mRNA stability. Crit Rev Eukaryot Gene
Expr. 6:391–411. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Lim JY, Kim OK, Lee J, Lee MJ, Kang N and
Hwang JK: Protective effect of the standardized green tea seed
extract on UVB-induced skin photoaging in hairless mice. Nutr Res
Pract. 8:398–403. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Kimura Y and Sumiyoshi M: Olive leaf
extract and its main component oleuropein prevent chronic
ultraviolet B radiation-induced skin damage and carcinogenesis in
hairless mice. J Nutr. 139:2079–2086. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Tagami H, Ohi M, Iwatsuki K, Kanamaru Y,
Yamada M and Ichijo B: Evaluation of the skin surface hydration in
vivo by electrical measurement. J Invest Dermatol. 75:500–507.
1980. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Singh JP, Selvendiran K, Banu SM,
Padmavathi R and Sakthisekaran D: Protective role of Apigenin on
the status of lipid peroxidation and antioxidant defense against
hepatocarcinogenesis in Wistar albino rats. Phytomedicine.
11:309–314. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Ha SK, Lee P, Park JA, Oh HR, Lee SY, Park
JH, Lee EH, Ryu JH, Lee KR and Kim SY: Apigenin inhibits the
production of NO and PGE2 in microglia and inhibits neuronal cell
death in a middle cerebral artery occlusion-induced focal ischemia
mice model. Neurochem Int. 52:878–886. 2008. View Article : Google Scholar
|
|
38
|
Myhrstad MC, Carlsen H, Nordström O,
Blomhoff R and Moskaug JØ: Flavonoids increase the intracellular
glutathione level by transactivation of the gamma-glutamylcysteine
synthetase catalytical subunit promoter. Free Radic Biol Med.
32:386–393. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Wei H, Tye L, Bresnick E and Birt DF:
Inhibitory effect of apigenin, a plant flavonoid, on epidermal
ornithine decarboxylase and skin tumor promotion in mice. Cancer
Res. 50:499–502. 1990.PubMed/NCBI
|
|
40
|
Fligiel SE, Varani J, Datta SC, Kang S,
Fisher GJ and Voorhees JJ: Collagen degradation in
aged/photodamaged skin in vivo and after exposure to matrix
metalloproteinase-1 in vitro. J Invest Dermatol. 120:842–848. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Chu ML and Prockop D: Collagen: gene
structure. Connective Tissue and Its Heritable Disorders. 2nd
edition. Wiley-Liss, Inc; New York, NY: pp. 149–165. 1993
|
|
42
|
Lim SH, Kim SM, Lee YW, Ahn KJ and Choe
YB: Change of biophysical properties of the skin caused by
ultraviolet radiation-induced photodamage in Koreans. Skin Res
Technol. 14:93–102. 2008.PubMed/NCBI
|