|
1
|
Strober W, Fuss I and Mannon P: The
fundamental basis of inflammatory bowel disease. J Clin Invest.
117:514–521. 2007. View
Article : Google Scholar : PubMed/NCBI
|
|
2
|
Pineton de Chambrun G, Peyrin-Biroulet L,
Lémann M and Colombel JF: Clinical implications of mucosal healing
for the management of IBD. Nat Rev Gastroenterol Hepatol. 7:15–29.
2010. View Article : Google Scholar
|
|
3
|
Baert F, Moortgat L, Van Assche G,
Caenepeel P, Vergauwe P, De Vos M, Stokkers P, Hommes D, Rutgeerts
P, Vermeire S, et al: Mucosal healing predicts sustained clinical
remission in patients with early-stage Crohn's disease.
Gastroenterology. 138:463–468. PubMed/NCBI
|
|
4
|
Frøslie KF, Jahnsen J, Moum BA, Vatn MH,
Group I and IBSEN Group: Mucosal healing in inflammatory bowel
disease: Results from a Norwegian population-based cohort.
Gastroenterology. 133:412–422. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sands BE: Biomarkers of inflammation in
inflammatory bowel disease. Gastroenterology. 149:1275–1285.e1272.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Foell D, Wittkowski H and Roth J:
Monitoring disease activity by stool analyses: From occult blood to
molecular markers of intestinal inflammation and damage. Gut.
58:859–868. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kopylov U, Rosenfeld G, Bressler B and
Seidman E: Clinical utility of fecal biomarkers for the diagnosis
and management of inflammatory bowel disease. Inflamm Bowel Dis.
20:742–756. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lehmann FS, Burri E and Beglinger C: The
role and utility of faecal markers in inflammatory bowel disease.
Therap Adv Gastroenterol. 8:23–36. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Schoepfer AM, Beglinger C, Straumann A,
Safroneeva E, Romero Y, Armstrong D, Schmidt C, Trummler M, Pittet
V and Vavricka SR: Fecal calprotectin more accurately reflects
endoscopic activity of ulcerative colitis than the Lichtiger Index,
C-reactive protein, platelets, hemoglobin, and blood leukocytes.
Inflamm Bowel Dis. 19:332–341. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Johne B, Fagerhol MK, Lyberg T, Prydz H,
Brandtzaeg P, Naess-Andresen CF and Dale I: Functional and clinical
aspects of the myelomonocyte protein calprotectin. Mol Pathol.
50:113–123. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Steinbakk M, Naess-Andresen CF, Lingaas E,
Dale I, Brandtzaeg P and Fagerhol MK: Antimicrobial actions of
calcium binding leucocyte L1 protein, calprotectin. Lancet.
336:763–765. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
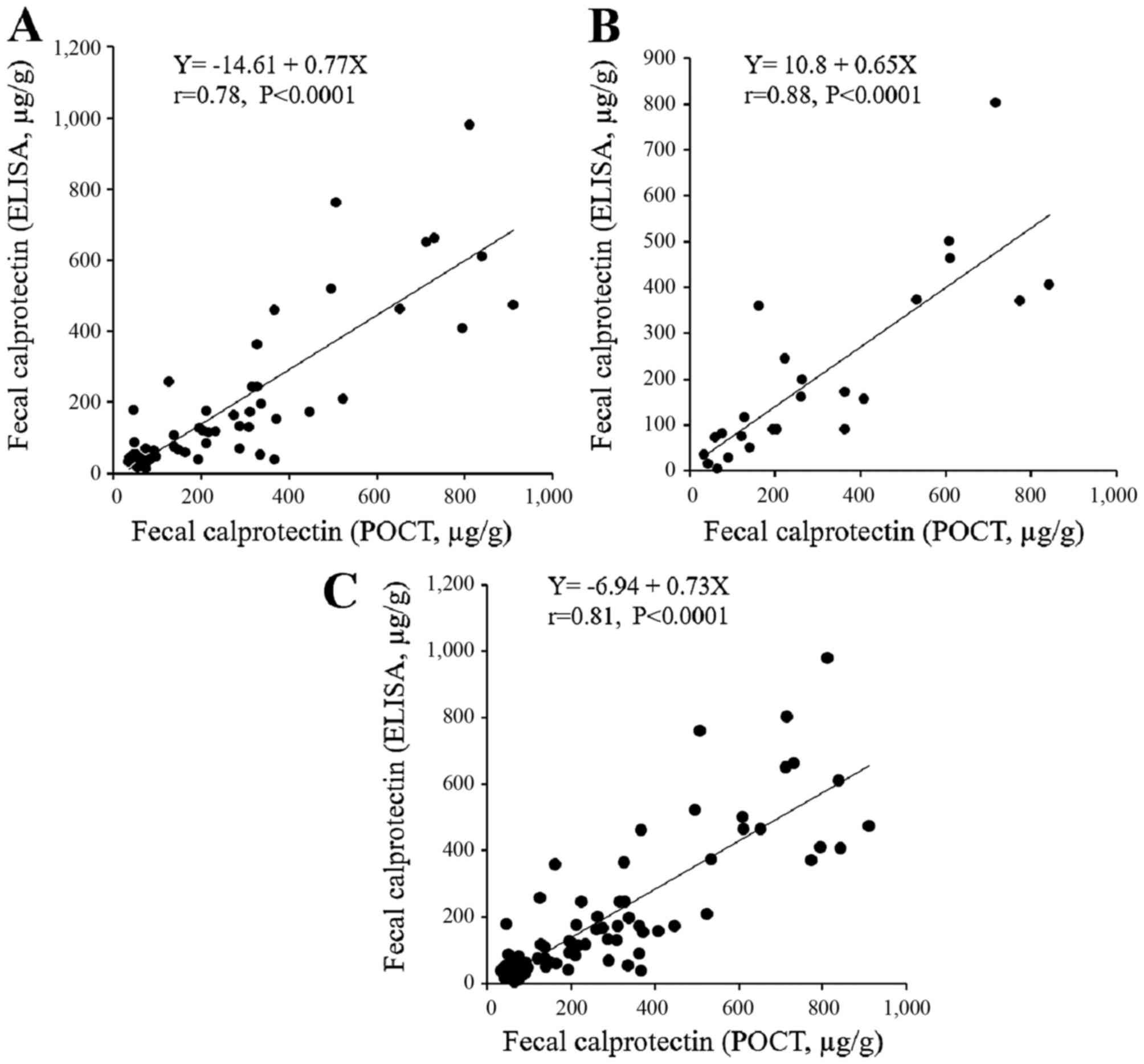
Coorevits L, Baert FJ and Vanpoucke HJ:
Faecal calprotectin: Comparative study of the Quantum Blue rapid
test and an established ELISA method. Clin Chem Lab Med.
51:825–831. 2013. View Article : Google Scholar
|
|
13
|
Rogler G, Aldeguer X, Kruis W, Lasson A,
Mittmann U, Nally K, Peyrin-Biroulet L, Schoepfer A, Vatn M,
Vavricka S, et al: Concept for a rapid point-of-care calprotectin
diagnostic test for diagnosis and disease activity monitoring in
patients with inflammatory bowel disease: Expert clinical opinion.
J Crohn's Colitis. 7:670–677. 2013. View Article : Google Scholar
|
|
14
|
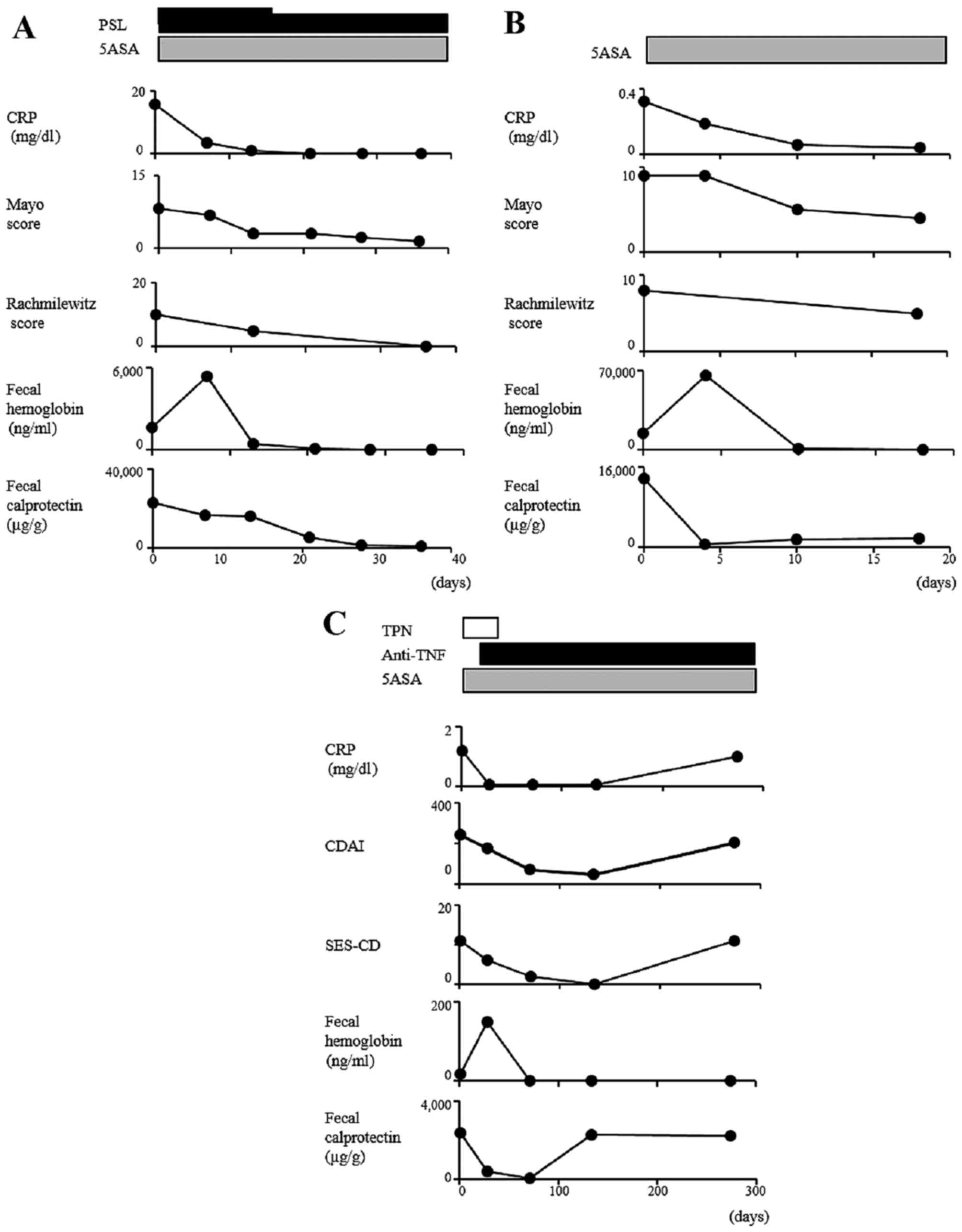
Rachmilewitz D: Coated mesalazine
(5-aminosalicylic acid) versus sulphasalazine in the treatment of
active ulcerative colitis: A randomised trial. BMJ. 298:82–86.
1989. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Schroeder KW, Tremaine WJ and Ilstrup DM:
Coated oral 5-aminosalicylic acid therapy for mildly to moderately
active ulcerative colitis. A randomized study. N Engl J Med.
317:1625–1629. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Daperno M, D'Haens G, Van Assche G, Baert
F, Bulois P, Maunoury V, Sostegni R, Rocca R, Pera A and Gevers A:
Development and validation of a new, simplified endoscopic activity
score for Crohn's disease: The SES-CD. Gastrointest Endosc.
60:505–512. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Best WR, Becktel JM and Singleton JW:
Rederived values of the eight coefficients of the Crohn's Disease
Activity Index (CDAI). Gastroenterology. 77:843–846.
1979.PubMed/NCBI
|
|
18
|
Oyaert M, Trouvé C, Baert F, De Smet D,
Langlois M and Vanpoucke H: Comparison of two immunoassays for
measurement of faecal calprotectin in detection of inflammatory
bowel disease: (pre)-analytical and diagnostic performance
characteristics. Clin Chem Lab Med. 52:391–397. 2014. View Article : Google Scholar
|
|
19
|
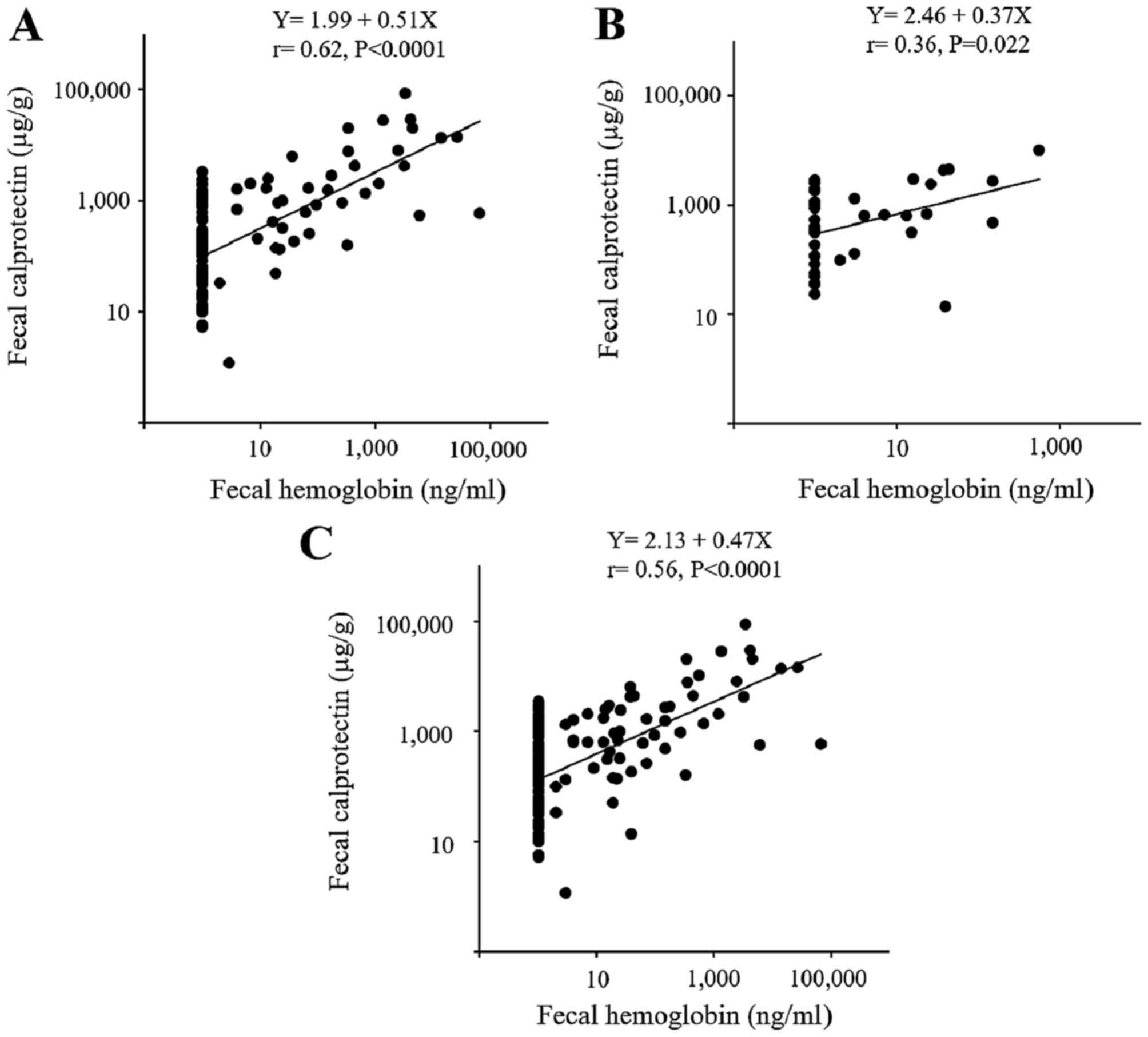
Nakarai A, Kato J, Hiraoka S, Kuriyama M,
Akita M, Hirakawa T, Okada H and Yamamoto K: Evaluation of mucosal
healing of ulcerative colitis by a quantitative fecal
immunochemical test. Am J Gastroenterol. 108:83–89. 2013.
View Article : Google Scholar
|
|
20
|
Takashima S, Kato J, Hiraoka S, Nakarai A,
Takei D, Inokuchi T, Sugihara Y, Takahara M, Harada K, Okada H, et
al: Evaluation of mucosal healing in ulcerative colitis by fecal
calprotectin vs. fecal immunochemical test. Am J Gastroenterol.
110:873–880. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Inokuchi T, Kato J, Hiraoka S, Takashima
S, Nakarai A, Takei D, Sugihara Y, Takahara M, Kawano S, Harada K,
et al: Fecal immunochemical test versus fecal calprotectin for
prediction of mucosal healing in Crohn's disease. Inflamm Bowel
Dis. 22:1078–1085. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
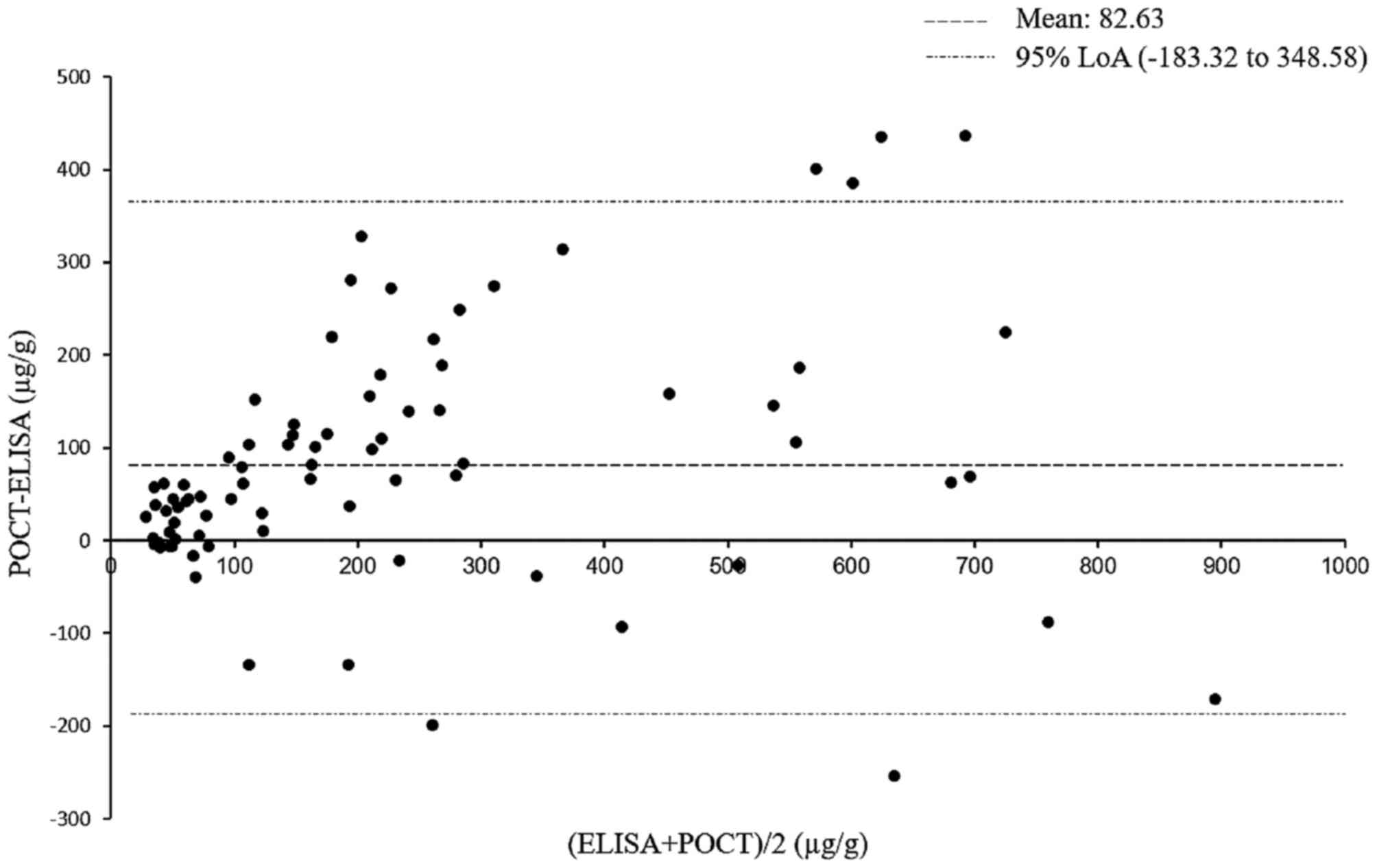
Bland JM and Altman DG: Statistical
methods for assessing agreement between two methods of clinical
measurement. Lancet. 1:307–310. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Langhorst J, Elsenbruch S, Koelzer J,
Rueffer A, Michalsen A and Dobos GJ: Noninvasive markers in the
assessment of intestinal inflammation in inflammatory bowel
diseases: Performance of fecal lactoferrin, calprotectin, and
PMN-elastase, CRP, and clinical indices. Am J Gastroenterol.
103:162–169. 2008. View Article : Google Scholar
|
|
24
|
Hanai H, Takeuchi K, Iida T, Kashiwagi N,
Saniabadi AR, Matsushita I, Sato Y, Kasuga N and Nakamura T:
Relationship between fecal calprotectin, intestinal inflammation,
and peripheral blood neutrophils in patients with active ulcerative
colitis. Dig Dis Sci. 49:1438–1443. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kawashima K, Ishihara S, Yuki T, Fukuba N,
Oshima N, Kazumori H, Sonoyama H, Yamashita N, Tada Y, Kusunoki R,
et al: Fecal calprotectin level correlated with both endoscopic
severity and disease extent in ulcerative colitis. BMC
Gastroenterol. 16:472016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Ricanek P, Brackmann S, Perminow G,
Lyckander LG, Sponheim J, Holme O, Høie O and Rydning A: Evaluation
of disease activity in IBD at the time of diagnosis by the use of
clinical, biochemical, and fecal markers. Scand J Gastroenterol.
46:1081–1091. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Jones J, Loftus EV Jr, Panaccione R, Chen
LS, Peterson S, McConnell J, Baudhuin L, Hanson K, Feagan BG,
Harmsen SW, et al: Relationships between disease activity and serum
and fecal biomarkers in patients with Crohn's disease. Clin
Gastroenterol Hepatol. 6:1218–1224. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Lin JF, Chen JM, Zuo JH, Yu A, Xiao ZJ,
Deng FH, Nie B and Jiang B: Meta-analysis: Fecal calprotectin for
assessment of inflammatory bowel disease activity. Inflamm Bowel
Dis. 20:1407–1415. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Sipponen T, Kärkkäinen P, Savilahti E,
Kolho KL, Nuutinen H, Turunen U and Färkkilä M: Correlation of
faecal calprotectin and lactoferrin with an endoscopic score for
Crohn's disease and histological findings. Aliment Pharmacol Ther.
28:1221–1229. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Kato J, Hiraoka S, Nakarai A, Takashima S,
Inokuchi T and Ichinose M: Fecal immunochemical test as a biomarker
for inflammatory bowel diseases: Can it rival fecal calprotectin.
Intest Res. 14:5–14. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ahmad R, Sorrell MF, Batra SK, Dhawan P
and Singh AB: Gut permeability and mucosal inflammation: bad, good
or context dependent. Mucosal Immunol. 10:307–317. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Haga HJ, Brun JG, Berntzen HB, Cervera R,
Khamashta M and Hughes GR: Calprotectin in patients with systemic
lupus erythematosus: Relation to clinical and laboratory parameters
of disease activity. Lupus. 2:47–50. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Soyfoo MS, Roth J, Vogl T, Pochet R and
Decaux G: Phagocyte-specific S100A8/A9 protein levels during
disease exacerbations and infections in systemic lupus
erythematosus. J Rheumatol. 36:2190–2194. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Pepper RJ, Hamour S, Chavele KM, Todd SK,
Rasmussen N, Flint S, Lyons PA, Smith KG, Pusey CD, Cook HT, et al:
Leukocyte and serum S100A8/S100A9 expression reflects disease
activity in ANCA-associated vasculitis and glomerulonephritis.
Kidney Int. 83:1150–1158. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
De Rycke L, Baeten D, Foell D, Kruithof E,
Veys EM, Roth J and De Keyser F: Differential expression and
response to anti-TNFalpha treatment of infiltrating versus resident
tissue macrophage subsets in autoimmune arthritis. J Pathol.
206:17–27. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Frosch M, Ahlmann M, Vogl T, Wittkowski H,
Wulffraat N, Foell D and Roth J: The myeloid-related proteins 8 and
14 complex, a novel ligand of toll-like receptor 4, and
interleukin-1beta form a positive feedback mechanism in
systemic-onset juvenile idiopathic arthritis. Arthritis Rheum.
60:883–891. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Hirono K, Foell D, Xing Y, Miyagawa-Tomita
S, Ye F, Ahlmann M, Vogl T, Futatani T, Rui C, Yu X, et al:
Expression of myeloid-related protein-8 and -14 in patients with
acute Kawasaki disease. J Am Coll Cardiol. 48:1257–1264. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Burkhardt K, Radespiel-Tröger M, Rupprecht
HD, Goppelt-Struebe M, Riess R, Renders L, Hauser IA and Kunzendorf
U: An increase in myeloid-related protein serum levels precedes
acute renal allograft rejection. J Am Soc Nephrol. 12:1947–1957.
2001.PubMed/NCBI
|
|
39
|
Leach ST, Yang Z, Messina I, Song C, Geczy
CL, Cunningham AM and Day AS: Serum and mucosal S100 proteins,
calprotectin (S100A8/S100A9) and S100A12, are elevated at diagnosis
in children with inflammatory bowel disease. Scand J Gastroenterol.
42:1321–1331. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Meuwis MA, Vernier-Massouille G, Grimaud
JC, Bouhnik Y, Laharie D, Piver E, Seidel L, Colombel JF and Louis
E: GETAID (Groupe d'Étude Thérapeutique Des Affections
Inflammatoires Digestives): Serum calprotectin as a biomarker for
Crohn's disease. J Crohn's Colitis. 7:e678–e683. 2013. View Article : Google Scholar
|
|
41
|
van Lent PL, Grevers LC, Schelbergen R,
Blom A, Geurts J, Sloetjes A, Vogl T, Roth J and van den Berg WB:
S100A8 causes a shift toward expression of activatory Fcγ receptors
on macrophages via toll-like receptor 4 and regulates Fcγ receptor
expression in synovium during chronic experimental arthritis.
Arthritis Rheum. 62:3353–3364. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Sunahori K, Yamamura M, Yamana J, Takasugi
K, Kawashima M, Yamamoto H, Chazin WJ, Nakatani Y, Yui S and Makino
H: The S100A8/A9 heterodimer amplifies proinflammatory cytokine
production by macrophages via activation of nuclear factor kappa B
and p38 mitogen-activated protein kinase in rheumatoid arthritis.
Arthritis Res Ther. 8:R692006. View
Article : Google Scholar : PubMed/NCBI
|
|
43
|
Loser K, Vogl T, Voskort M, Lueken A,
Kupas V, Nacken W, Klenner L, Kuhn A, Foell D, Sorokin L, et al:
The Toll-like receptor 4 ligands Mrp8 and Mrp14 are crucial in the
development of autoreactive CD8+ T cells. Nat Med.
16:713–717. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Pepper RJ, Wang HH, Rajakaruna GK,
Papakrivopoulou E, Vogl T, Pusey CD, Cook HT and Salama AD:
S100A8/A9 (calprotectin) is critical for development of
glomerulonephritis and promotes inflammatory leukocyte-renal cell
interactions. Am J Pathol. 185:1264–1274. 2015. View Article : Google Scholar : PubMed/NCBI
|