Introduction
Hepatocellular carcinoma (HCC) is the fifth most
common malignant tumor and the third most life-threatening type of
cancer worldwide. Almost 78% of global HCC cases were reported in
Asian countries each year (1).
Since the 1990s, HCC has become the third leading cause of
cancer-associated mortality in China. Liver fibrosis is associated
with HCC, with 90% of HCC cases arising from the cirrhotic liver
(2,3).
Liver fibrosis occurs as the result of the chronic
wound-healing response of the liver and is associated with major
alterations of extracellular matrix (ECM) (4). Hepatic stellate cells (HSCs) are the
main ECM-producing cell in liver fibrosis. In the normal liver,
HSCs are found in the space of Disse and are the major storage
sites of vitamin A. Following chronic injury, the HSCs are
activated and transdifferentiate into myofibroblast cells,
acquiring contractile, proinflammatory and fibrogenic properties.
The activated HSCs migrate and accumulate at sites of tissue
repair, secreting large quantities of ECM and regulating ECM
degradation (5).
Cysteine-rich 61 (CCN1/Cyr61), a member of the CCN
family, is an ECM protein and regulates multiple cellular
activities, including cell adhesion, migration, proliferation,
survival, apoptosis and angiogenesis, through binding different
integrins (6–11). Previous studies have demonstrated
that CCN1 has complex roles in cutaneous wound healing fibrosis
through binding to different integrins on the fibroblast membrane
(12–14).
Several studies have focused on the roles of CCN1 in
liver disease. A study by Kim et al (20) and our previous study showed that
level of CCN1 was elevated in the cirrhotic liver in humans and in
mice with carbon tetrachloride (CCl4)-induced liver
fibrosis, with CCN1 protein located predominantly in hepatocytes
(15). In our previous study, it
was found that the expression of CCN1 was significantly higher in
benign hepatic cirrhosis tissue and cancer-adjacent hepatic
cirrhosis tissue, compared with that in normal liver tissue
(15). These results are in
accordance with those reported by Rashid et al (16). CCN1 is involved in macrophage
infiltration and the hepatic proinflammatory response (17). In our previous study, it was also
found that CCN1 was a target gene of β-catenin in HCC and promoted
the proliferation of HepG2 cells (15). CCN1 triggers the senescence of
activated HSCs and promotes the regression of liver fibrosis
(18–20). Previous studies have demonstrated
that CCN1 induces chol-angiocyte proliferation and ductular
reactions, and identified CCN1/αvβ5/nuclear factor (NF)-κB/jagged 1
(JAG1) as a critical axis for biliary injury repair (21). CCN1 also suppresses
hepatocarcinogenesis by inhibiting epidermal growth factor receptor
(EGFR)-dependent hepatocyte compensatory proliferation (22).
In addition, several studies have found that certain
integrin subunits are located on HSC membranes and mediate the
proliferation, migration and fibrogenic activation of HSCs
(16,23–25), which suggests that CCN1 may be
involved in activated HSCs.
It is generally known that activated HSCs can
promote the progression of HCC. Clinical investigations have found
that activated HSCs in peritumoral tissues are associated with
earlier recurrence rates, mortality rates and high recurrence rates
(26). Activated HSCs are
directly involved in hepatocarcinogenesis in a transforming growth
factor (TGF)-β-dependent manner by inducing autocrine TGF-β
signaling and nuclear β-catenin accumulation in neoplastic
hepatocytes (27). Activated HSCs
stimulate the proliferation, growth and migration of HCC cells
in vitro and in vivo through cytokine secretion,
whereas ECM regulates angiogenesis and tumor immunity inhibition
(28–30). HCC cells also stimulate the growth
and migration of human HSCs (31). HCC cell-activated HSC cross-talk
in the liver promotes the progression of HCC (32). However, whether CCN1 can affect
these functions of activated HSCs remains to be elucidated. The
present study investigated whether CCN1 can activate HSCs and
whether it enhances the effect of HSCs on promoting the progression
of HCC.
Materials and methods
Ethics statement
All animals were purchased from the Experimental
Animal Center of the Third Military Medical University (Chongqing,
China). All animal protocols were approved by the Ethics Committee
of the Third Military Medical University. Animal experiments were
performed in accordance with the China Regulations for the
Administration of Affairs Concerning Experimental Animals and the
guidelines of the U.S. National Institutes of Health.
Cell lines
The human hepatic stellate cells LX-2 or human HCC
cells HepG2 were cultured in T75 flasks in DMEM (Dulbecco's
modified Eagle medium, high glucose, HyClone; GE Healthcare Life
Sciences, Logan, UT, USA) supplemented with 10% fetal calf serum
(FCS; Gibco; Thermo Fisher Scientific, Inc., Waltham, MA, USA), 100
U/ml penicillin and 10 μg/ml streptomycin at 37°C in a
humidified 5% carbon dioxide atmosphere. The HepG2 cells were used
to investigate the effects of CCN1 on HSCs in promoting the
viability and migration of the HCC cells. HepG2-LX2 cells were
co-cultured in 6-well plates and Transwell inserts.
Establishment of the mouse liver fibrosis
model and histological analyses
A total of 100 BALB/c male mice were purchased from
the Experimental Animal Center of the Third Military Medical
University (Chongqing, China). Liver fibrosis was induced in male
mice (~4 weeks of age; 17–18 g) via intraperitoneal injection of 1
ml/kg body weight of CCl4 (diluted in olive oil, 1:4; 1
ml/kg body weight) twice a week. The control animals received an
equal volume of olive oil. All mice were maintained in barrier
environment, received free access to sterile feed and water,
temperature 24–26°C, 12 h light/dark cycle. Experimental animals
were maintained in the EVC Animal Care Systems. The mice were
treated for 5 weeks and were sacrificed 3 days following injection.
Following the final injection of CCl4, mice were
sacrificed for another 3 weeks, 3 mice weekly (weeks 6–8). The
liver tissues were sectioned (1.2×1.2×0.5 cm) and fixed in 10%
formaldehyde, and were embedded in paraffin. The tissue sections (4
μm) were stained with hematoxylin and eosin (H&E),
Sirius red and immunohistochemical staining. The tissue structure
was observed using hematoxylin and eosin. The staining procedure
was performed as described previously (15).
Analysis of the expression of CCN1 was performed on
the paraffinized sections of liver tissue using immunohistochemical
staining. The staining procedure was performed as described
previously (15). The sections
were evaluated using a standard bright field microscope. Digital
images were captured using the NIS-Element Imaging Analysis system
(Nikon, Tokyo, Japan). Positive staining was defined when >10%
of cells exhibited brown staining. The degree of the staining was
digitalized automatically using the NIS-Element Imaging Analysis
system when the positive and negative points were defined. The mean
density of five randomly selected microscopic fields was
calculated, reflecting the relative expression level of CCN1. The
results are presented as the mean ± standard deviation.
The fibrotic regions were observed using Sirius red
staining. The numbers of fibers were assessed using the NIS-Element
Imaging Analysis in six randomly selected regions from each tissue
section.
Transient infection and collection of
conditioned medium (CM) from LX-2
AdCCN1 and AdRFP were acquired from Professor
Tong-Chuan He (Molecular Oncology Laboratory, Department of
Surgery, University of Chicago Medical Center, Chicago, IL, USA).
The LX-2 cells were seeded in T75 flasks. At 70% confluence, the
cells were infected with adenovirus AdCCN1 or AdRFP, respectively.
Following infection for 24 h at 37°C, the LX-2 cells were harvested
to analyze the expression of CCN1 using western blot assays.
Following infection with AdCCN1 or AdRFP for 20 h, respectively,
the LX-2 cells were washed twice with serum-free DMEM, and then
incubated for another 24 h with 12 ml serum-free DMEM; the media
were collected as CCN1-CM and control-CM, respectively (CM was 10X
concentrated). Furthermore, half of CCN1-CM was concentrated to 10X
concentration by Amicon Ultra centrifugal filter (UFC800324; Merck
Millipore) following the introductions.
Measurement of cell viability
The LX-2 cells were seeded into 96-well plates
(2,000 cells/well) in DMEM supplemented with 10% FCS. Following
infection with AdCCN1 or AdRFP for 20 h, respectively, the LX-2
cells were washed twice with serum-free DMEM and then incubated for
another 0-72 h with DMEM supplemented with 10% FCS. The viability
of cells was measured using an MTT assay.
The HepG2 cells were seeded into 96-well plates
(2,000 cells/well) in DMEM supplemented with 10% FCS. After 24 h,
the seeded HepG2 cells were washed with serum-free DMEM and were
cultured in the CM from the different LX-2 cells or the control
medium, following which an MTT assay was performed to analyze the
viability of the cells.
The HepG2 cells were cultured alone or were
co-cultured with the differently treated LX-2 cells in a 6-well
plate (1×103 cells/well) with Transwell inserts. After 5
days, colony formation of the HepG2 cells was assayed using crystal
violet staining.
Migration assays
The migration of the HepG2 cells was assessed using
two assays. For the analysis of cell invasion capability, a
Matrigel invasion assay was performed in 6-well Transwell inserts
with 8-μm pore size filters coated with Matrigel (diluted
1:6, BD Biosciences, Franklin Lakes, NJ, USA). The HepG2 cells were
harvested, resuspended in serum-free DMEM and placed in the upper
compartment (5×105 cells/well). To the lower
compartment, DMEM supplemented with CM from the activated LX-2
cells or control medium was added. Following incubation at 37°C for
30 h, the filters were collected and cells adhering to the lower
surface were fixed in formalin and stained with crystal violet. The
numbers of cells in 12 randomly selected fields in each well were
counted.
Cell migration capability was assessed using a
Boyden chamber assay. The HepG2 cells were seeded into 6-well
plates at 1×106 cells/well. The HepG2 cells were
harvested following incubation for 30 h, resuspended in serum-free
DMEM and placed in the upper compartment at 5×105
cells/well. The lower compartment contained DMEM supplemented with
CM from the activated LX-2 cells or control medium. Following
incubation for 24 h, the filters were collected and cells adhering
to the lower surface were fixed in formalin and stained with
crystal violet. Cells in 12 randomly selected fields in each well
were counted.
The LX-2 cells and HepG2 cells migration
capabilities were assessed using a monolayer scratch assay.
Following adherence, the LX-2 cells were infected with AdCCN1 or
AdRFP, followed by the same treatments as described for the
viability experiment described above. The HepG2 cells were then
washed with serum-free DMEM and were cultured in CM from the
activated LX-2 cells or control medium. Subsequently, the cell
layer was scratched using a sterile toothpick. The migration into
the space was measured at 0 and 48 h (LX-2 cells) or 72 h (HepG2
cells).
Western blot analysis
The LX-2 cells were seeded into T75 flasks at 60%
confluence in DMEM supplemented with 10% FCS. After 24 h, the LX-2
cells were infected with AdCCN1 or AdRFP for 72 h. The HepG2 cells
were washed with serum-free DMEM, and were cultured in CM from the
LX-2 cells or control medium. Following incubation for 36 h, the
HepG2 cells were harvested for subsequent analysis.
The cell lysates were prepared with cell lysis
buffer containing a protease inhibitor cocktail. Protein
concentrations of all samples were determined by Bicinchoninic acid
Protein Assay Kit (Beyotime Institute of Biotechnology, Haimen,
China). Total protein for each sample (50 μg) was loaded
onto an 8% SDS-PAGE gel for electrophoresis and transferred onto a
PVDF membrane. The membrane was then incubated with antibodies
against phosphorylated-β-catenin (cat. no 9566, 1:1,000),
total-β-catenin (cat. no. 8480, 1:1,000) (both from Cell Signaling
Technology, Inc., Danvers, MA, USA), cyclin D1 (cat. no.
60186-1-Ig, 1:1,000), VEGF (cat. no. 19003-1-AP, 1:1,000), CD34
(cat. no. 14486-1-AP, 1:1,000), CD31 (cat. no. 66065-1-Ig; 1:1,000)
(all from ProteinTech Group, Inc.), survivin (cat. no. ab76424;
1:1,000 dilution; Abcam, Cambridge, UK), and c-myc (cat. no.
MA1-980, 1:1,000; Thermo Fisher Scientific, Inc.), respectively at
4°C overnight. The blots were then incubated with horseradish
peroxidase-conjugated secondary antibodies (cat. nos. SA00001-1 and
SA00001-2, both 1:5,000; ProteinTech Group, Inc.) at room
temperature incubation for 2 h, following which the immune-reactive
signals were detected using an ECL kit (EMD Millipore, Billerica,
MA, USA).
Subcutaneous tumor models in nude
mice
Four groups of mice (n=5 per group) were used in the
following experiments, respectively. Following the infection with
AdCCN1 or AdRFP for 24 h, LX-2 cells were harvested. The flank of
4-week-old nude mice were injected subcutaneously with HepG2 cells
alone, or with HepG2 cells + LX-2 cells, HepG2 cells + LX-2-RFP
cells (LX-2 cells infected with AdRFP), or HepG2 cells + LX-2-CCN1
cells (LX-2 cells infected with AdCCN1) at 5.0×106 cells
per mouse, respectively.
The length and width of tumor masses were
dynamically measured and the tumor volume was estimated using the
formula: axb2×0.5, where a and b represent the maximal
and minimal diameters, respectively. The mice were sacrificed on
day 26, and growth curves were plotted using the tumor volumes for
each experimental group at the set points. Tumor masses were
removed and fixed in 4% formaldehyde. Paraffin-embedded consecutive
sections (5 μm) were cut for histological analysis, and
total proteins of the liver tissues were collected for western blot
analysis.
The tissue structure of the subcutaneous tumor
tissue was observed using H&E staining. Collagenous fibers in
the subcutaneous tumor were observed using Sirius red staining.
Immunohistochemical staining was performed for Ki67.
The microvessels in the subcutaneous tumor tissues
were observed by immunofluorescence staining for CD31. The sections
were visualized and images were captured using a Leica light and
fluorescence microscope (Leica Microystems, GmbH, Wetzlar,
Germany). The protein expression of VEGF was detected using western
blot analysis in the subcutaneous tumor tissues.
Statistical analysis
Data are expressed as the mean ± standard deviation.
Statistical analysis of the two mean values was performed using
Student's t-test. One-way analysis of variance was performed to
compare multiple mean values. All calculations were performed using
the SPSS 17.0 software (SPSS, Inc., Chicago, IL, USA). P<0.05
was considered to indicate a statistically significant
difference.
Results
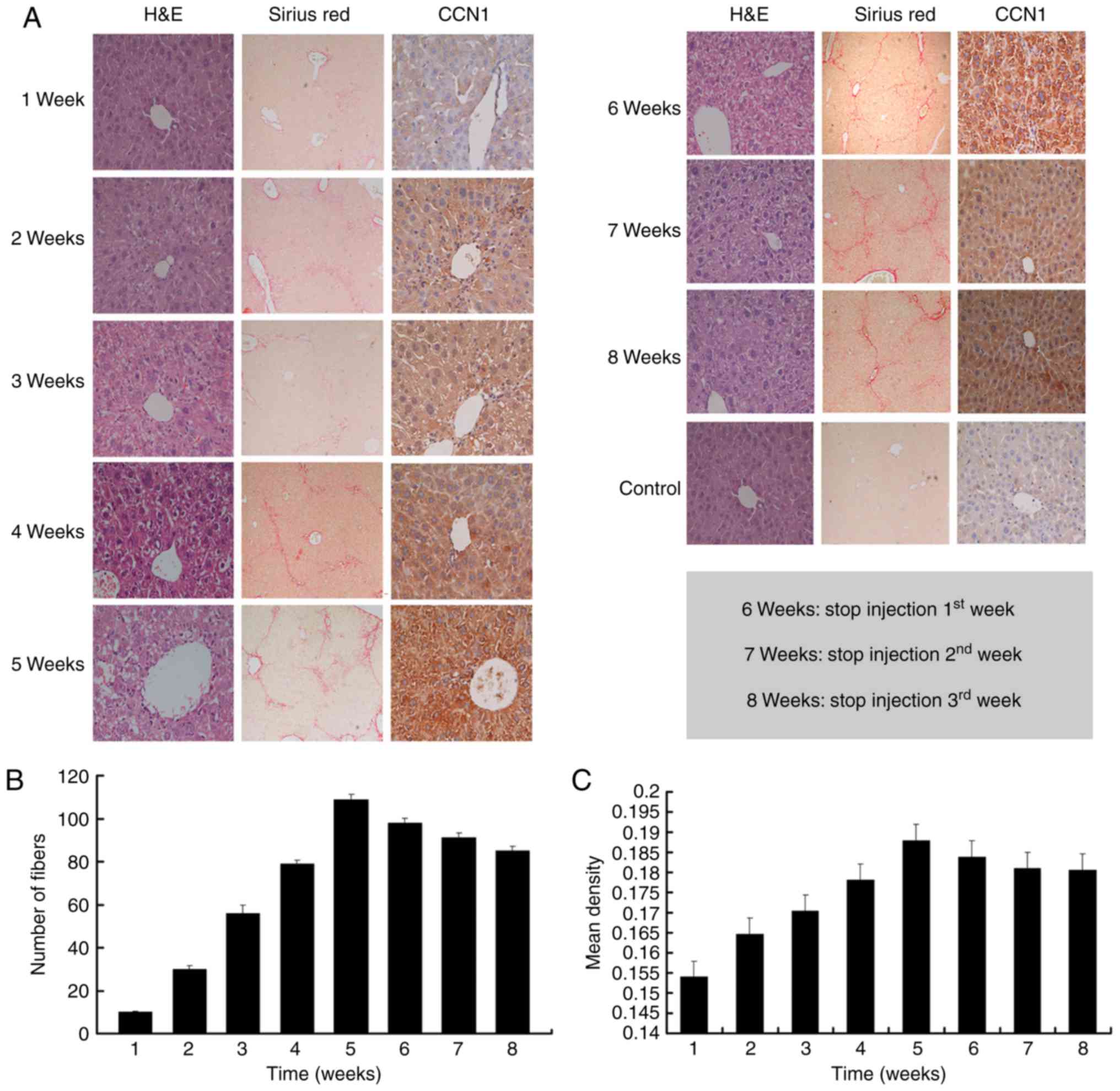
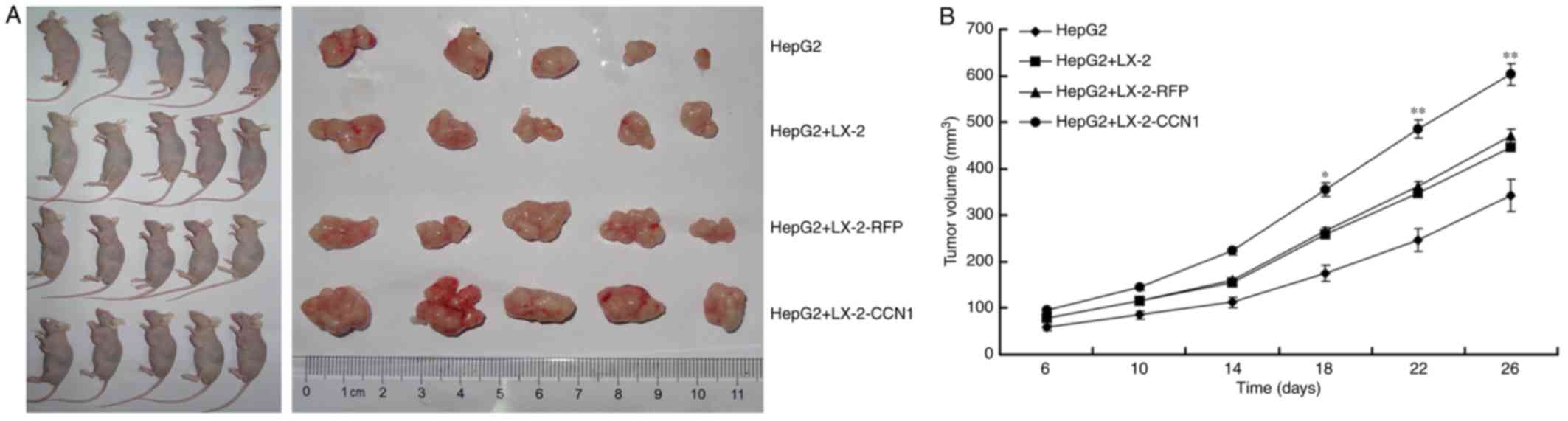
Dynamic expression of CCN1 is observed in
mouse fibrotic liver tissues
To examine the role of CCN1 in the liver
fibrosis-carcinoma axis, the present study observed the dynamic
expression of CCN1 protein in the liver fibrosis mouse model. As
shown in Fig. 1A–C, liver
fibrosis continually progressed and the expression of CCN1
continually increased as CCl4 was injected. However,
when there was no CCl4 injection, the degree of hepatic
fibrosis was alleviated, and the expression of CCN1 was also
reduced (Fig. 1). These findings
suggested that changes in the expression of CCN1 may be associated
with the severity of fibrosis during the progression of liver
fibrosis.
 | Figure 1CCN1 is expressed in mouse fibrotic
liver tissue. Liver fibrosis was induced in mice by intraperitoneal
injection of 1 ml/kg body weight of CCl4 twice a week.
(A) Liver tissue sections were stained with H&E (magnification,
×400), Sirius red (magnification, ×100) and with
immunohistochemical staining for CCN1 (magnification, ×400). (B)
Liver sections were stained with Sirius red to reveal collagen
deposition. The numbers of fibers were assessed via NIS-Element
Imaging analysis of six randomly selected regions. Data are
presented as the mean ± standard deviation. (C) Analysis of the
expression of CCN1 was performed on paraffinized sections of mice
liver tissues via immunohistochemical staining. The degree of
staining was digitalized automatically using the NIS-Element
Imaging Analysis system. The mean density of random five
microscopic fields was calculated as the relative expression level
of CCN1. Data are presented as the mean ± standard deviation; 6, 7
and 8 weeks refer to the weeks 1, 2 and 3, respectively, following
the final injection of CCl4. CCN1, cysteine-rich 61;
CCl4, carbon tetrachloride; H&E, hematoxylin and
eosin. |
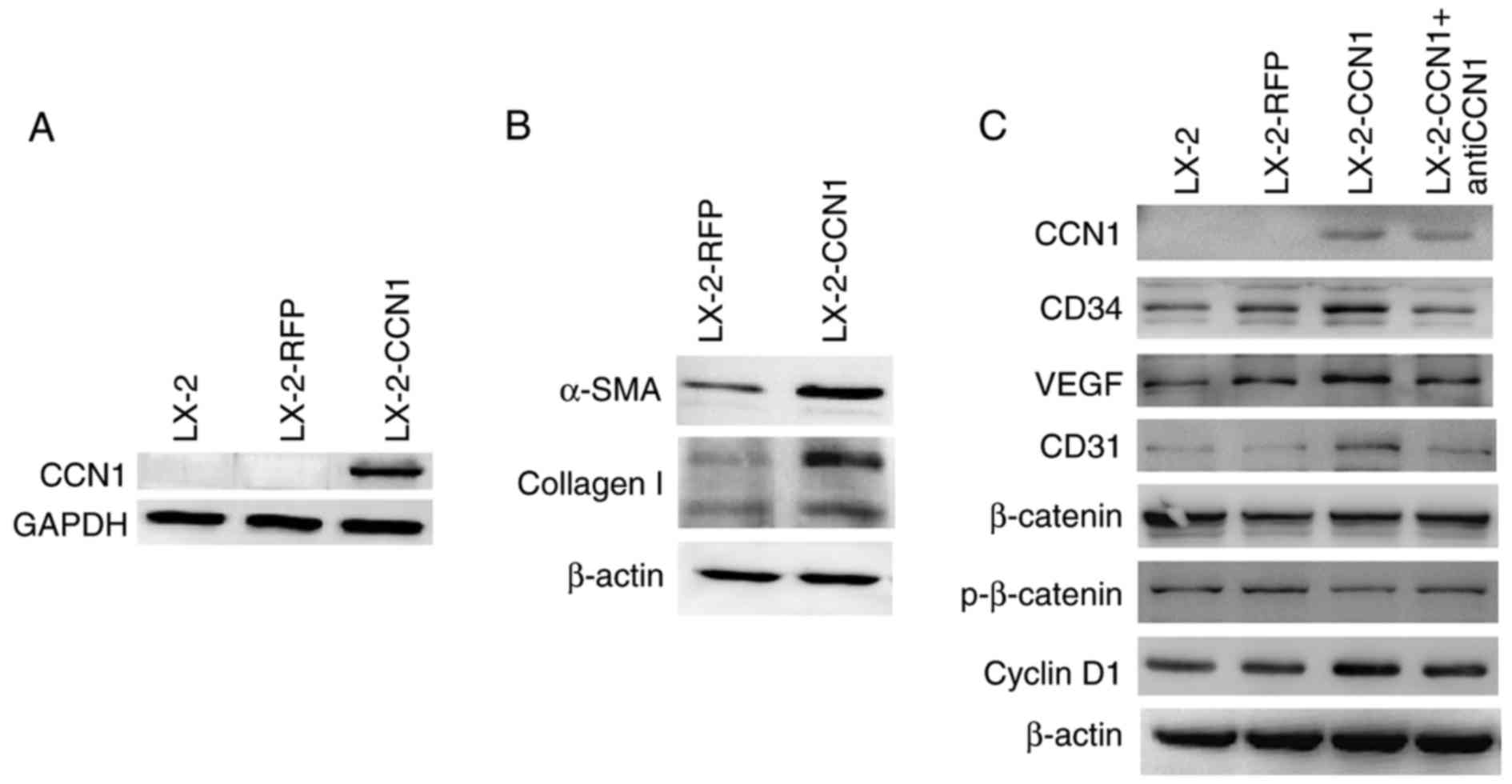
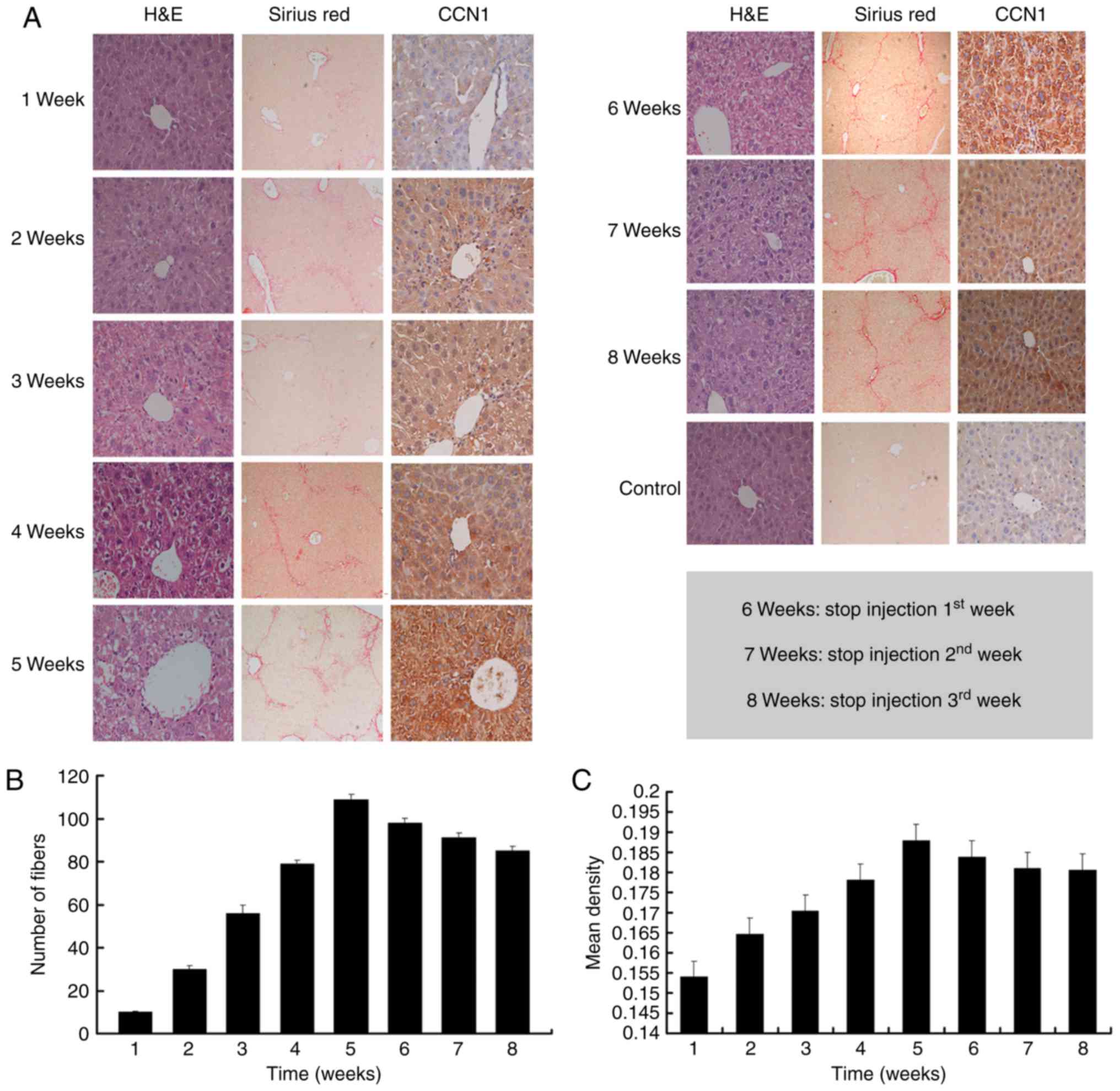
CCN1 activates HSCs and affects cell
function
CCN1 was not expressed in LX-2 cells prior to
infection with AdCCN1 (Fig. 2A).
LX-2-CCN1 cells, comprising LX-2 cells overexpressing CCN1,
expressed the markers of HSC activation and fibrosis, including
α-SMA and collagen I (Fig. 2B).
LX-2-CCN1 also exhibited cell proliferation correlated with
signaling molecules, including cyclin D1, and angiogenesis
molecules, including VEGF, CD34 and CD31 (Fig. 2C). However, the expression of
β-catenin did not alter when phosphorylated-β-catenin was
downregulated (Fig. 2C). CCN1
also promoted the viability and the migration of LX-2 cells.
However, viability and migration were inhibited in the LX-2-CCN1
cells treated by function-inhibiting monoclonal anti-CCN1, which
was obtained following recombined CCN1 protein treatment (Fig. 2D–F).
 | Figure 2CCN1 activates HSCs and affects cell
function. LX-2 cells were infected with adenovirus AdCCN1 or AdRFP,
respectively. (A) Following infection for 24 h, western blot
analysis was performed to detect the expression levels of CCN1 in
LX-2 cells, LX-2-RFP cells and LX-2-CCN1 cells. (B) Following
infection for 72 h, α-SMA and collagen I, which are markers of HSC
activation and fibrosis, were detected in the LX-2-CCN1 cells. (C)
Expression levels of p-β-catenin, β-catenin, cyclin D1, VEGF, CD31
and CD34 were analyzed. CCN1 antibody (0.5 μg/ml) was used
to neutralize CCN1 in control groups. (D) Viability of LX-2-CCN1
cells was analyzed using MTT assays. (E) Following treatment with
RCCN1 (0.6 μg/ml), LX-2 cells were analyzed using MTT
assays. CCN1 antibody (0.5 mg/ml) was used in assays. The final
concentrations were 0.5 and 2.5 μg/ml. (F) Monolayer scratch
assay was used to analyze the migration of LX-2-CCN1 cells.
*P<0.05 and **P<0.01. HSCs, hepatic
stellate cells; CCN1, cysteine-rich 61; VEGF, vascular endothelial
growth factor; SMA, smooth muscle actin; p-, phosphorylated; RCCN1,
recombined CCN1; OD, optical density. |
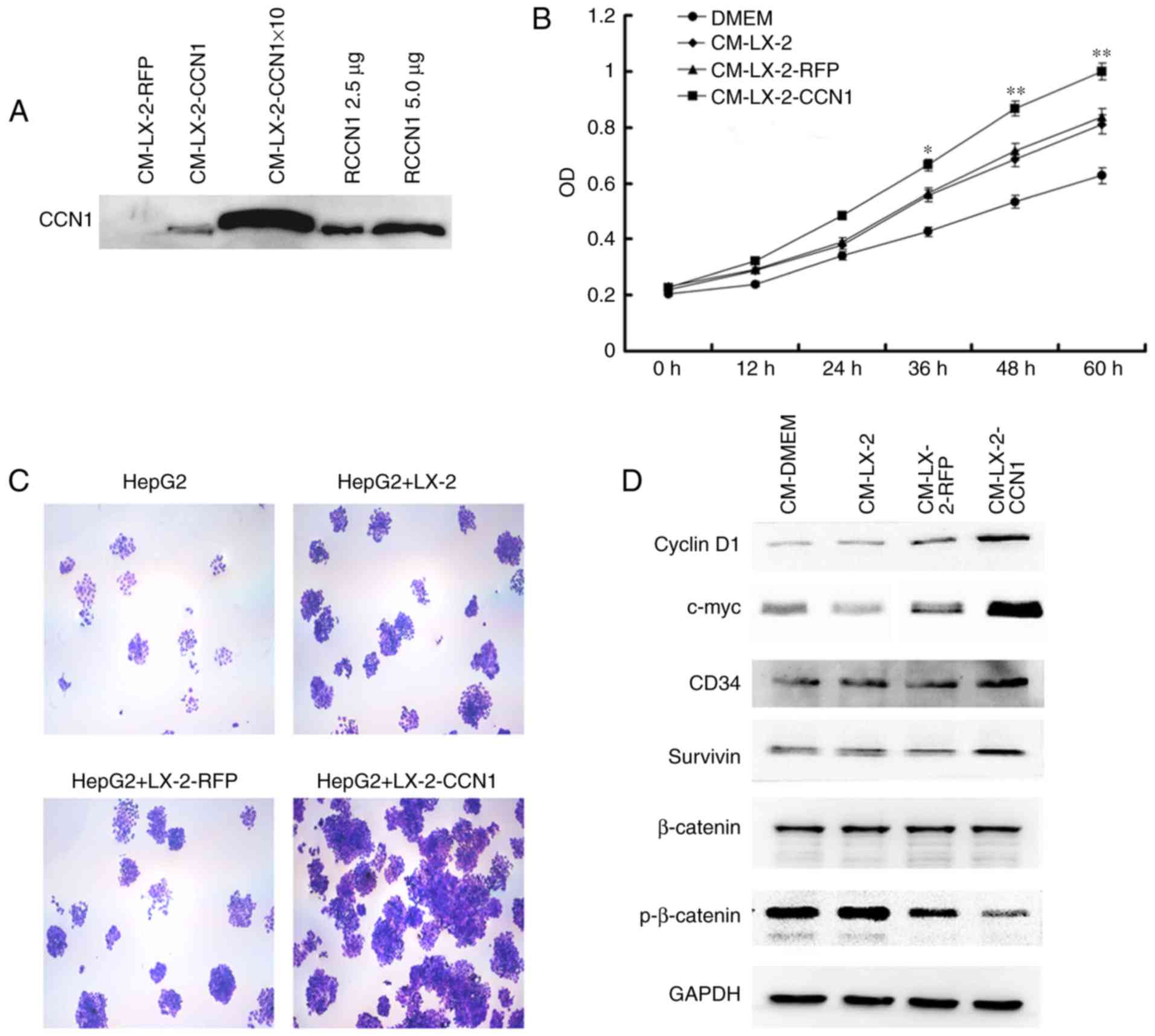
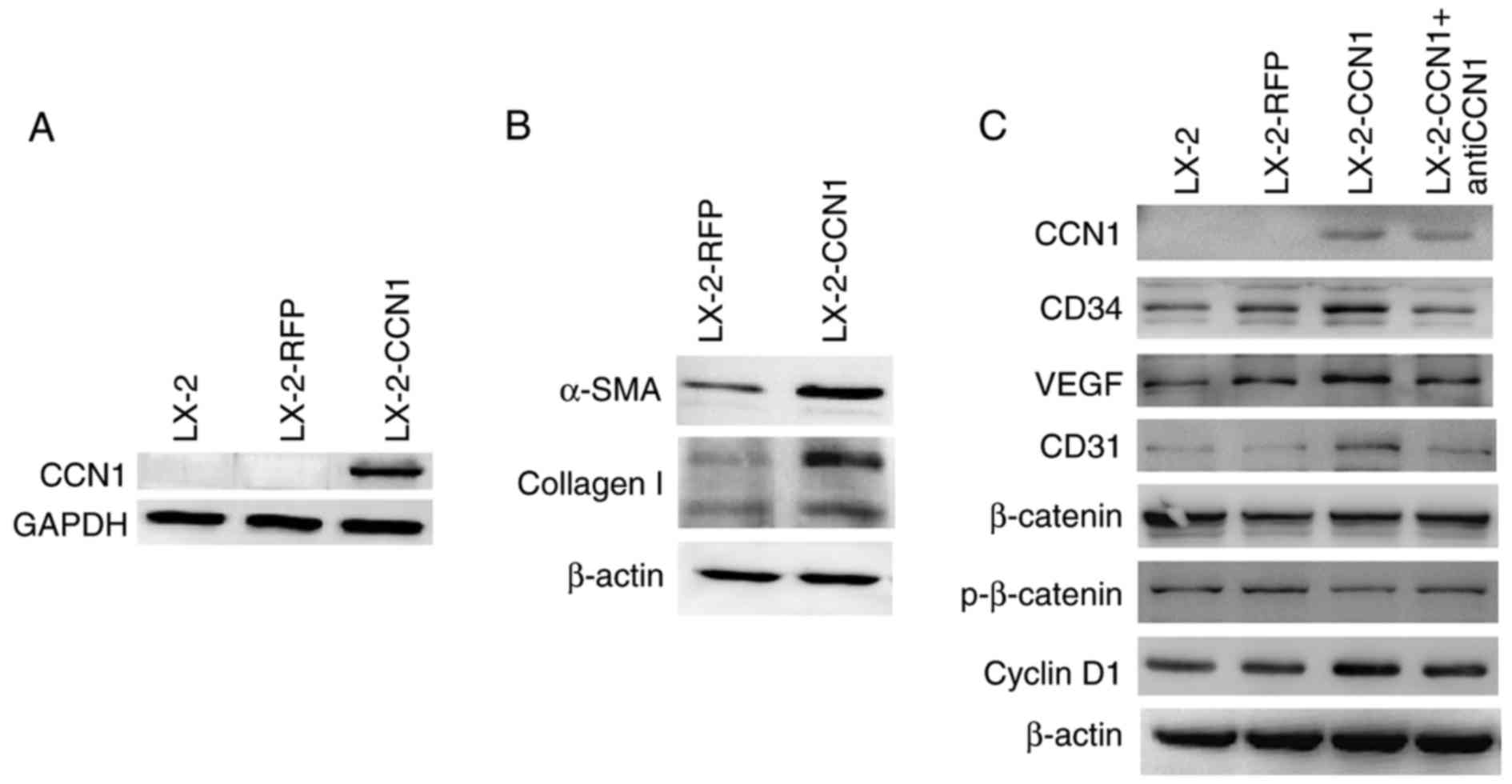
CCN1 enhances the effect of activated
HSCs on promoting the viability of HCC cells in vitro
Activated HSCs acquire fibrogenic properties but
also can promote the progression of HCC. The present study aimed to
determine whether CCN1 enhances the functions of activated HSCs.
First, the effect of CCN1 on activated HSCs in promoting the
viability of HCC cells was examined. The HepG2 cells were incubated
with CM collected from the three treatment groups of LX-2 cells.
The MTT assay revealed that the effect of CM from LX-2-CCN1 cells
on increasing HepG2 cell viability was more marked compared with
cells incubated with CM from LX-2 and LX-2-RFP cells (Fig. 3A and B). In addition, the HepG2
cells and three LX-2 cell groups were co-cultured in a Transwell
insert plate. The HepG2 cells co-cultured with LX-2-CCN1 cells
formed more clones than those cultured with the other LX-2 groups
(Fig. 3C).
 | Figure 3CCN1 enhances the function of hepatic
stellate cells in promoting the viability of HCCs. (A) Western blot
analysis was used to detect expression levels of CCN1 in the
original CM and 10X concentration CM collected from LX-2 cells
infected with AdCCN1 or AdRFP. Expression levels were also detected
following treatment with 2.5 and 5 μg. HepG2 cells were
cultured with or without CM. (B) Viability of HepG2 cells, analyzed
using MTT assays. *P<0.05 and **P<0.01
vs. the CM-LX-2-RFP group. (C) HepG2 cells were cultured alone or
were co-cultured with different LX-2 cells in a 6-well plate with
Transwell inserts. After 5 days, colony formation of HepG2 cells
was examined using crystal violet staining (magnification, ×100).
(D) Expression of p-β-catenin, β-catenin, survivin, cyclin D1 and
c-myc in HepG2 cells were analyzed using western blot analysis.
CCN1, cysteine-rich 61; CM, conditioned medium; HCCs,
hepatocellular carcinoma cells; p-, phosphorylated; RCCN1,
recombined CCN1. |
To gain insight into the molecular mechanisms
underlying the effects described above, the present study analyzed
the activation of several correlated signaling molecules, which are
known to be important in HCC. The results of the western blot
analysis revealed that stimulation with CM from LX-2-CCN1 cells
reduced the expression of phosphorylated-β-catenin in the HepG2
cells, whereas the level of total-β-catenin remained unchanged
(Fig. 3D). The expression levels
of cyclin D1 and c-myc, which are target genes of β-catenin, were
upregulated (Fig. 3D). This
indicated that stimulation of CM from LX-2-CCN1 cells significantly
induced β-catenin signaling transduction in HepG2 cells. The
western blot analysis revealed that there was a significant
increase in the expression of survivin in the HepG2 cells treated
with CM from LX-2-CCN1 cells (Fig.
3D).
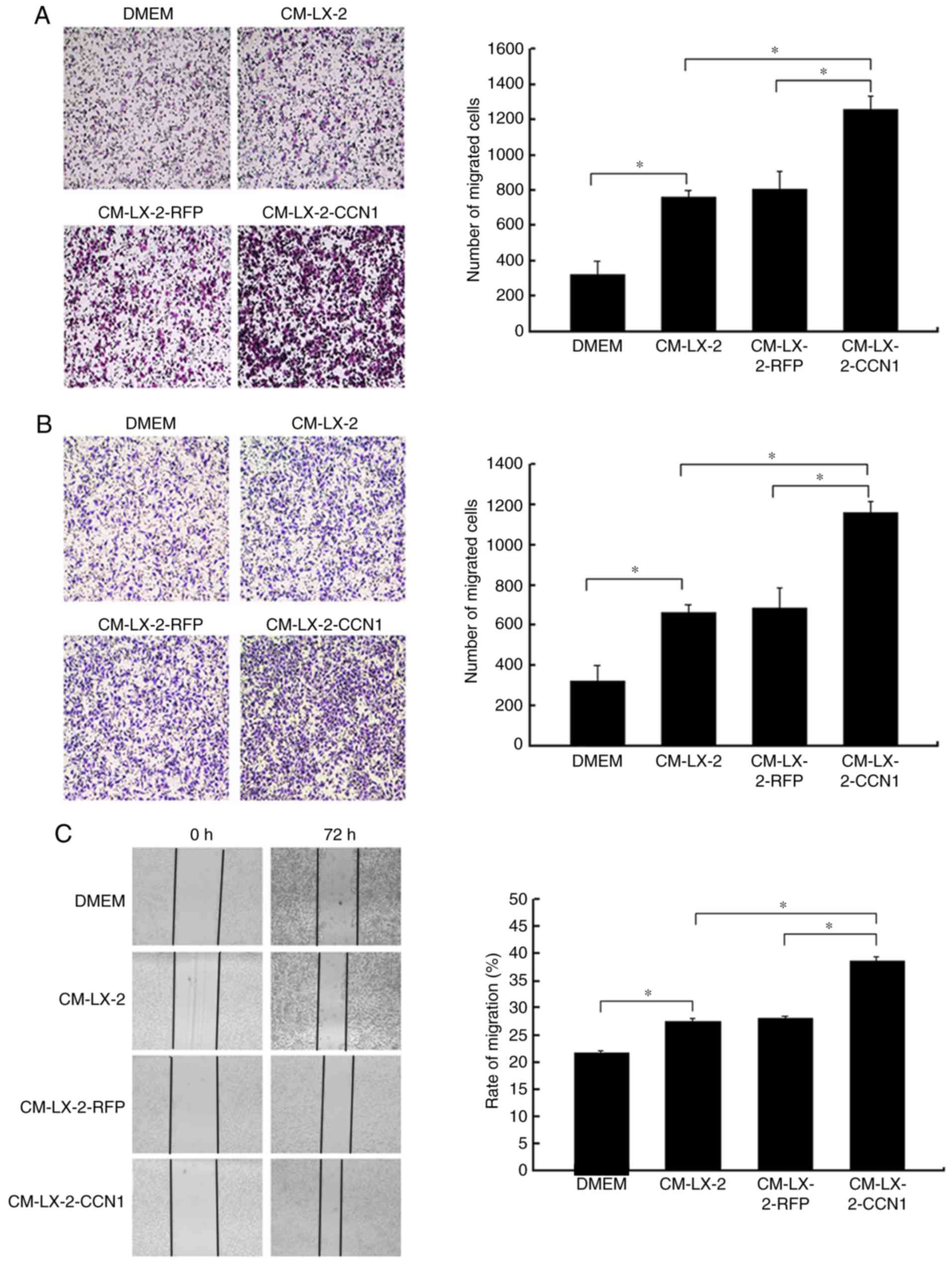
CCN1 enhances the function of activated
HSCs in promoting the migration and invasion of HCC cells
In the present study, HepG2 cells were incubated
with CM collected from the three groups of LX-2 cells, following
which the migratory activity of the HepG2 cells was analyzed. The
Boyden chamber and Matrigel invasion assays demonstrated that CM
from the LX-2-CCN1 cells significantly stimulated the migratory
potential of HepG2 cells (Fig. 4A and
B). These data were confirmed by scratch-healing assays, which
revealed significantly faster wound healing in the HepG2 cells
treated with CM from LX-2-CCN1 cells (Fig. 4C). In order to understand the
molecular mechanism of the above, the present study analyzed the
activation of ERK, and the expression of E-cadherin and MMP-9,
which are known to be important in HCC metastasis and invasion. The
results of the western blot analysis showed that stimulation with
CM from the LX-2-CCN1 cells enhanced the expression of
phosphorylated-ERK and MMP-9 in HepG2 cells., whereas the
expression of E-cadherin was reduced (Fig. 4D).
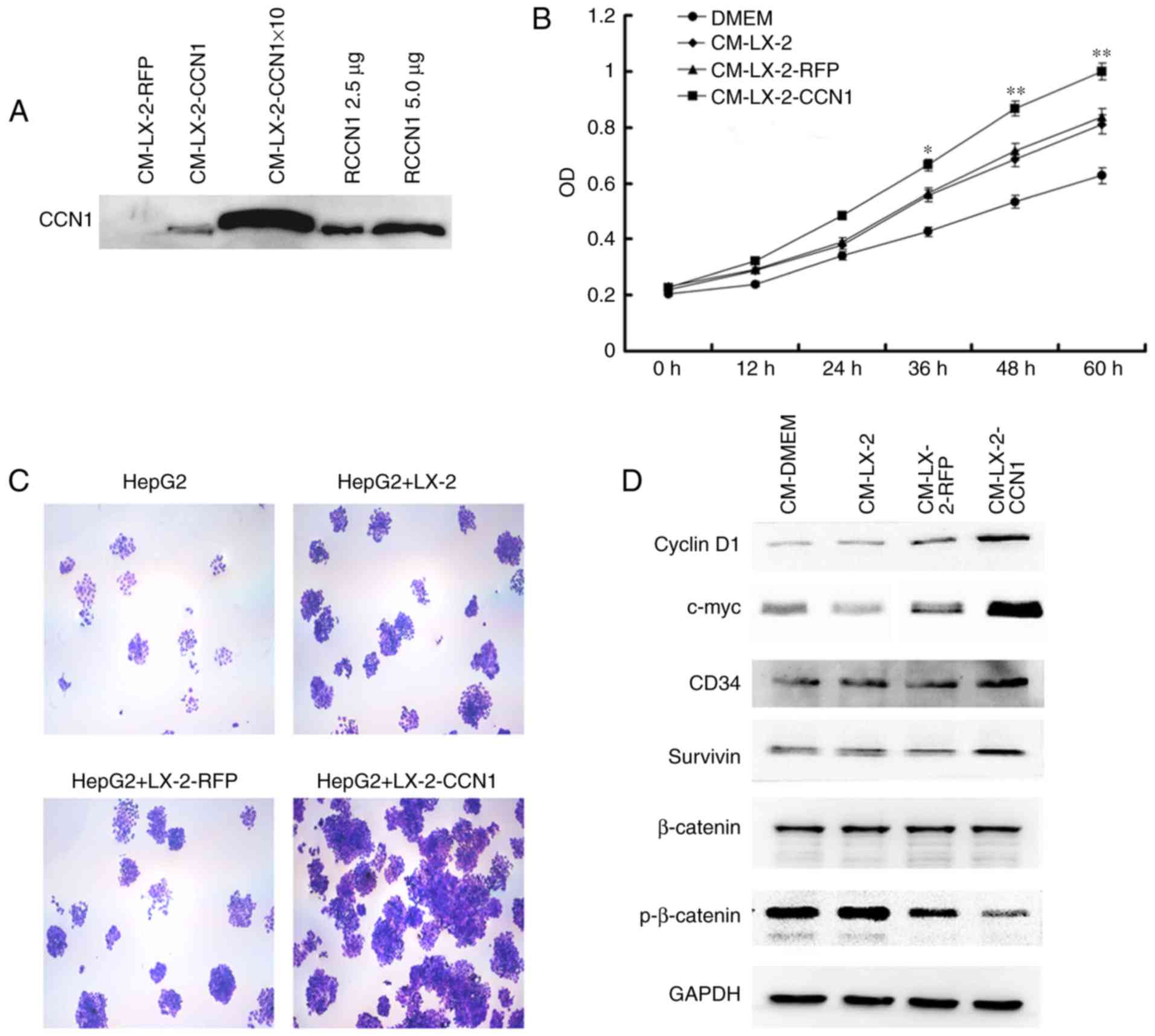
CCN1 enhances the function of HSCs in
promoting the proliferation of HCC cells in vivo
The present study also examined the effect of CCN1
on HSCs in promoting the proliferation of HCC cells in vivo.
The HepG2 cells were implanted subcutaneously into nude mice,
either alone or in combination with three different LX-2 cells
(LX-2, LX-2-RFP and LX-2-CCN1). As shown in Fig. 5A, the implantation of LX-2 cells
alone did not result in tumor formation, but all of the mice
developed tumors at the site of implantation in the other groups.
The tumor size was significantly larger in the group subjected to
subcutaneous co-implantation of LX-2 and HepG2 cells, compared with
that in the group subjected to single subcutaneous implantation of
HepG2 cells. The injection of HepG2 cells + LX-2-CCN1 cells
promoted more marked tumor growth, compared with that in the group
injected with HepG2 cells + LX-2 or HepG2 cells + LX-2-RFP
(Fig. 5B).
H&E staining of the subcutaneous tumor tissue
revealed that the tissue structure was more complex in the HepG2
cells + LX-2-CCN1 cells, compared with that in the other groups.
There was more marked hyperplasia in multinuclear tumor cells,
fibrous connective tissue and infiltration of inflammatory cells in
the HepG2 + LX-2-CCN1 cells group, compared with the other groups
(Fig. 5C).
To determine whether CCN1 promotes the proliferation
of HCC xenografts, the present study examined the expression of
Ki-67, a nuclear protein necessary for tumor cell proliferation, in
subcutaneous tumors with immunohistochemical staining. Subcutaneous
tumors from the HepG2 + LX-2-CCN1 group exhibited more marked
Ki-67-positive staining, compared with those from other groups
(Fig. 5C).
According to the results of the Sirius red staining,
collagenous fiber was significantly increased in the subcutaneous
tumors of the HepG2 + LX-2-CCN1 co-transplantation group, compared
with than that in the other groups (Fig. 5C).
Microvessel density and protein
expression of VEGF in subcutaneous tumors
The microvessel density in the subcutaneous tumor
tissues was examined by immunofluorescent staining for CD31 which
is a specific endothelial marker. As shown in Fig. 5D, CD31-positive cells and the
number of microvessels were higher in the subcutaneous tumors of
HepG2 cells + LX-2-CCN1 cells, compared with those in other groups.
In addition, the expression of VEGF, an important molecule for
angiogenesis, was examined. The western blot assay showed that the
expression of VEGF was upregulated in the subcutaneous tumors of
the HepG2 cells + LX-2-CCN1 cells (Fig. 5E). It has been reported that CCN1
can induce the expression of VEGF, EGF and other growth factors,
which is expressed by HSCs induced by CCN1, promotes the formation
of blood vessels (6). Therefore,
the above data indicated that co-transplantation of HepG2 cells and
LX-2-CCN1 cells significantly promoted tumor angiogenesis.
Discussion
It is known that CCN1 is an extracellular matrix
protein, and its involvement in tumors progression through binding
different integrins is complex (7,8,33).
Previous studies have demonstrated that CCN1 has various effects on
the fibrosis of cutaneous wound healing through binding different
integrins on the fibroblast membrane. CCN1 can stimulate skin
fibroblast migration, adhesion and proliferation through binding
integrins αvβ5 and αvβ3 (12–14). However, CCN1 also restricts
fibrosis through inducing skin fibroblast senescence and apoptosis
through binding integrin α6β1 (34).
Increasing studies have shown that CCN1 can regulate
several types of liver cell. According to a study by Bian et
al, CCN1 was expressed in the hepatocytes of mice with
non-alcoholic fatty liver disease, and was involved in macrophage
infiltration and the hepatic proinflammatory response (17). In our previous study, it was found
that the protein expression of CCN1 was not detected in the liver
tissues of healthy individuals, but its expression level was
elevated in hepatic cirrhosis tissue and markedly increased in
cancer-adjacent hepatic cirrhosis tissue (15). It was also found that CCN1 is a
target gene of β-catenin in hepatocelluar carcinoma and promotes
the proliferation of HepG2 cells (15). Kim et al demonstrated that
CCN1 triggers cellular senescence through the accumulation of
reactive oxygen species in activated HSCs, which limits
fibrogenesis and promotes the regression of liver fibrosis induced
by diverse injuries. It was suggested that chronic persistent liver
injuries might overwhelm the antifibrotic activities of CCN1
despite the elevated accumulation of CCN1 (20).
Previous studies have demonstrated that CCN1 induces
cholangiocyte proliferation and ductular reaction, and identified
CCN1/αvβ5/NF-κB/JAG1 as a critical axis for biliary injury repair
(21). CCN1 also suppresses
hepatocarcinogenesis by inhibiting EGFR-dependent hepatocyte
compensatory proliferation (22).
These results indicate that CCN1 has various effects on the liver
inflammation-fibrosis-carcinoma axis.
In liver fibrosis, activated HSCs are the main
ECM-producing cells and are important in promoting the progression
of HCC (35). Several integrin
subunits are located on the HSC membrane, mediating the
proliferation, migration and fibrogenic activation of HSCs
(16,23–25). Therefore, CCN1 may have various
effects on activated HSCs through binding to different integrins at
different stages of liver disease. In addition, proteomic analyses
of ECM from the LX-2 human hepatic stellate cell line and human
foreskin fibroblasts revealed that certain components were found in
both, but they exhibited different connectivities within each
protein-protein interaction network (16). This indicates that the role of
CCN1 in HSCs may be different from those of skin fibroblasts.
In the present study, it was shown that CCN1 was not
expressed in the liver tissues of normal mice, but was
overexpressed in the mouse model of liver fibrosis, with the
expression tendency closely associated with the severity of liver
fibrosis. Rashid et al (16) and Kim et al (20) also found that CCN1 accumulated at
higher levels in the livers of patients with cirrhosis and murine
models of hepatic injury and fibrosis. These results indicated that
CCN1 may be involved in the process of hepatic fibrosis. CCN1 is an
immediate-early gene and is transcriptionally activated on
stimulation by serum growth factors within minutes (6). Therefore, CCN1 may be a suitable
marker for diagnosing and predicting prognosis of liver
fibrosis.
The present study also found that CCN1 activated
LX-2 cells and affected their function. CCN1 promoted the viability
and migration of LX-2 cells, induced the fiber differentiation of
LX-2 cells and increased the expression of proliferation-correlated
signaling molecules and angiogenesis molecules in LX-2-CCN1 cells.
The animal experiments performed in the present study revealed that
the expression of CCN1 was directly correlated with the progression
of liver fibrosis in mice. On the basis of these findings, it was
hypothesized that CCN1 can promote HSC fibrosis, which differs from
the results reported by Kim et al (20). CCN1 may have complex effects
through binding different integrins on the HSC membrane during
liver inflammation-fibrosis-cirrhosis-cancer progression.
The activated LX-2 cells promoted the proliferation
of HepG2 cells in vitro and in vivo, and CM from the
LX-2-CCN1 cells stimulated the expression of cyclin D1, c-myc and
survivin, and the activity of β-catenin signaling in HepG2 cells.
These proteins are all factors promoting cell proliferation.
β-catenin is a key molecule in the canonical Wnt signaling pathway.
Aberrant activation of canonical Wnt/β-catenin signaling has been
shown to contribute to the development of HCC (36,37). Cyclin D1 and c-myc are known
tumor-associated signaling molecules (38,39). Survivin is an important inhibitor
of apoptosis and is overexpressed in several types of tumor; it can
promote the invasion, metastasis, growth and survival of malignant
cells, and confer resistance to specific chemotherapeutic drugs
(39,40). The present study also found that
CM from LX-2-CCN1 cells promoted the migration and invasion of
HepG2 cells, stimulated the expression of phosphorylated-ERK1/2 and
MMP-9, and inhibited the expression of E-cadherin.
Phosphorylated-ERK and MMP-9 are invasion-associated signaling
molecules and are crucial in the progression of HCC (29,41). The findings indicated that the
malignant phenotype of HepG2 cells was promoted by CM from
LX-2-CCN1, which demonstrated that CCN1 enhanced the function of
activated HSCs in promoting the progression of HCC.
Activated HSCs promote the progression of HCC in
part through regulating the formation of the tumor
microenvironment, including regulating ECM and angiogenesis
(28–30). In the present study, it was found
that CCN1 enhanced this function. Histological analysis of the
subcutaneous tumors revealed that the tissue structure was more
complex in the HepG2 + LX-2-CCN1 cell group, compared with that in
the other groups. The hyperplasia in multinuclear tumor cells,
fibrous connective tissue and infiltration of inflammatory cells
were more marked in the HepG2 + LX-2-CCN1 cell group. In addition,
increased numbers of collagenous fibers and microvessels were found
in the subcutaneous tumors of the HepG2 + LX-2-CCN1 cell group.
This indicated that CCN1 has an effect on activated HSC-regulated
tumor microenvironment formation, which is conducive to the
progression of HCC. These findings indicated that CCN1 was involved
in the progression of the hepatic cirrhosis-HCC axis through
regulating HSCs.
In conclusion, the results of the present study
indicated that CCN1/Cyr61 activated LX-2 cells and affected the
cell function. CCN1 enhanced the function of HSCs in promoting the
progression of HCC. Therefore, CCN1 may be important during the
progression of the hepatic cirrhosis-HCC axis through regulating
HSCs.
Acknowledgments
This study was supported by The National Natural
Science Foundation of China (grant no. 30672393), the Southwest
Hospital Routine Management Project of Science and Technology
Innovation Program (grant no. SWH2016JCYB-13) and the Chengdu
Military General Hospital Routine Management Project of Science
(grant no. 2016KC04).
Glossary
Abbreviations
Abbreviations:
|
CCN1/Cyr61
|
cysteine-rich 61
|
|
HSCs
|
hepatic stellate cells
|
|
HCC
|
hepatocellular carcinoma
|
|
CM
|
conditioned medium
|
References
|
1
|
Song P, Tang W, Tamura S, Hasegawa K,
Sugawara Y, Dong J and Kokudo N: The management of hepatocellular
carcinoma in Asia: A guideline combining quantitative and
qualitative evaluation. Biosci Trends. 4:283–287. 2010.
|
|
2
|
Chen W, Zheng R, Baade PD, Zhang S, Zeng
H, Bray F, Jemal A, Yu XQ and He J: Cancer statistics in China,
2015. CA Cancer J Clin. 66:115–132. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Schütte K, Bornschein J and Malfertheiner
P: Hepatocellular carcinoma-epidemiological trends and risk
factors. Dig Dis. 27:80–92. 2009. View Article : Google Scholar
|
|
4
|
Bataller R and Brenner DA: Liver fibrosis.
J Clin Invest. 115:209–218. 2005. View
Article : Google Scholar : PubMed/NCBI
|
|
5
|
Li JT, Liao ZX, Ping J, Xu D and Wang H:
Molecular mechanism of hepatic stellate cell activation and
antifibrotic therapeutic strategies. J Gastroenterol. 43:419–428.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lau LF: CCN1/CYR61: The very model of a
modern matricellular protein. Cell Mol Life Sci. 68:3149–3163.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Schmitz P, Gerber U, Jüngel E, Schütze N,
Blaheta R and Bendas G: Cyr61/CCN1 affects the integrin-mediated
migration of prostate cancer cells (PC-3) in vitro. Int J Clin
Pharmacol Ther. 51:47–50. 2013. View
Article : Google Scholar
|
|
8
|
Haseley A, Boone S, Wojton J, Yu L, Yoo
JY, Yu J, Kurozumi K, Glorioso JC, Caligiuri MA and Kaur B:
Extracellular matrix protein CCN1 limits oncolytic efficacy in
glioma. Cancer Res. 72:1353–1362. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Jun JI, Kim KH and Lau LF: The
matricellular protein CCN1 mediates neutrophil efferocytosis in
cutaneous wound healing. Nat Commun. 6:73862015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chintala H, Krupska I, Yan L, Lau L, Grant
M and Chaqour B: The matricellular protein CCN1 controls retinal
angiogenesis by targeting VEGF, Src homology 2 domain phosphatase-1
and Notch signaling. Development. 142:2364–2374. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhang F, Hao F, An D, Zeng L, Wang Y, Xu X
and Cui MZ: The matricellular protein Cyr61 is a key mediator of
platelet-derived growth factor-induced cell migration. J Biol Chem.
290:8232–8242. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Jun JI and Lau LF: Taking aim at the
extracellular matrix: CCN proteins as emerging therapeutic targets.
Nat Rev Drug Discov. 10:945–963. 2011. View
Article : Google Scholar : PubMed/NCBI
|
|
13
|
Grzeszkiewicz TM, Kirschling DJ, Chen N
and Lau LF: CYR61 stimulates human skin fibroblast migration
through integrin alpha vbeta 5 and enhances mitogenesis through
integrin alpha vbeta 3, independent of its carboxyl-terminal
domain. J Biol Chem. 276:21943–21950. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chen N, Chen CC and Lau LF: Adhesion of
human skin fibroblasts to Cyr61 is mediated through integrin alpha
6beta 1 and cell surface heparan sulfate proteoglycans. J Biol
Chem. 275:24953–24961. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Li ZQ, Ding W, Sun SJ, Li J, Pan J, Zhao
C, Wu WR and Si WK: Cyr61/CCN1 is regulated by Wnt/β-catenin
signaling and plays an important role in the progression of
hepatocellular carcinoma. PLoS One. 7:e357542012. View Article : Google Scholar
|
|
16
|
Rashid ST, Humphries JD, Byron A, Dhar A,
Askari JA, Selley JN, Knight D, Goldin RD, Thursz M and Humphries
MJ: Proteomic analysis of extracellular matrix from the hepatic
stellate cell line LX-2 identifies CYR61 and Wnt-5a as novel
constituents of fibrotic liver. J Proteome Res. 11:4052–4064. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Bian Z, Peng Y, You Z, Wang Q, Miao Q, Liu
Y, Han X, Qiu D, Li Z and Ma X: CCN1 expression in hepatocytes
contributes to macrophage infiltration in nonalcoholic fatty liver
disease in mice. J Lipid Res. 54:44–54. 2013. View Article : Google Scholar :
|
|
18
|
Borkham-Kamphorst E, Schaffrath C, Van de
Leur E, Haas U, Tihaa L, Meurer SK, Nevzorova YA, Liedtke C and
Weiskirchen R: The anti-fibrotic effects of CCN1/CYR61 in primary
portal myofibroblasts are mediated through induction of reactive
oxygen species resulting in cellular senescence, apoptosis and
attenuated TGF-β signaling. Biochim Biophys Acta. 1843:902–914.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Borkham-Kamphorst E, Steffen BT, Van de
Leur E, Haas U, Tihaa L, Friedman SL and Weiskirchen R: CCN1/CYR61
overexpression in hepatic stellate cells induces ER stress-related
apoptosis. Cell Signal. 28:34–42. 2016. View Article : Google Scholar
|
|
20
|
Kim KH, Chen CC, Monzon RI and Lau LF:
Matricellular protein CCN1 promotes regression of liver fibrosis
through induction of cellular senescence in hepatic myofibroblasts.
Mol Cell Biol. 33:2078–2090. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kim KH, Chen CC, Alpini G and Lau LF: CCN1
induces hepatic ductular reaction through integrin αvβ(5)-mediated
activation of NF-κB. J Clin Invest. 125:1886–1900. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Chen CC, Kim KH and Lau LF: The
matricellular protein CCN1 suppresses hepatocarcinogenesis by
inhibiting compensatory proliferation. Oncogene. 35:1314–1323.
2016. View Article : Google Scholar
|
|
23
|
Huang G and Brigstock DR: Integrin
expression and function in the response of primary culture hepatic
stellate cells to connective tissue growth factor (CCN2). J Cell
Mol Med. 15:1087–1095. 2011. View Article : Google Scholar
|
|
24
|
Patsenker E, Popov Y, Wiesner M, Goodman
SL and Schuppan D: Pharmacological inhibition of the vitronectin
receptor abrogates PDGF-BB-induced hepatic stellate cell migration
and activation in vitro. J Hepatol. 46:878–887. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Zhou X, Murphy FR, Gehdu N, Zhang J,
Iredale JP and Benyon RC: Engagement of alphavbeta3 integrin
regulates proliferation and apoptosis of hepatic stellate cells. J
Biol Chem. 279:23996–24006. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Ju MJ, Qiu SJ, Fan J, Xiao YS, Gao Q, Zhou
J, Li YW and Tang ZY: Peritumoral activated hepatic stellate cells
predict poor clinical outcome in hepatocellular carcinoma after
curative resection. Am J Clin Pathol. 131:498–510. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Mikula M, Proell V, Fischer AN and
Mikulits W: Activated hepatic stellate cells induce tumor
progression of neoplastic hepatocytes in a TGF-beta dependent
fashion. J Cell Physiol. 209:560–567. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zhao W, Zhang L, Yin Z, Su W, Ren G, Zhou
C, You J, Fan J and Wang X: Activated hepatic stellate cells
promote hepatocellular carcinoma development in immunocompetent
mice. Int J Cancer. 129:2651–2661. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Santamato A, Fransvea E, Dituri F,
Caligiuri A, Quaranta M, Niimi T, Pinzani M, Antonaci S and
Giannelli G: Hepatic stellate cells stimulate HCC cell migration
via laminin-5 production. Clin Sci (Lond). 121:159–168. 2011.
View Article : Google Scholar
|
|
30
|
Amann T, Bataille F, Spruss T, Mühlbauer
M, Gäbele E, Schölmerich J, Kiefer P, Bosserhoff AK and Hellerbrand
C: Activated hepatic stellate cells promote tumorigenicity of
hepatocellular carcinoma. Cancer Sci. 100:646–653. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Sancho-Bru P, Juez E, Moreno M, Khurdayan
V, Morales-Ruiz M, Colmenero J, Arroyo V, Brenner DA, Ginès P and
Bataller R: Hepatocarcinoma cells stimulate the growth, migration
and expression of pro-angiogenic genes in human hepatic stellate
cells. Liver Int. 30:31–41. 2010. View Article : Google Scholar
|
|
32
|
Coulouarn C, Corlu A, Glaise D, Guénon I,
Thorgeirsson SS and Clément B: Hepatocyte-stellate cell cross-talk
in the liver engenders a permissive inflammatory microenvironment
that drives progression in hepatocellular carcinoma. Cancer Res.
72:2533–2542. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Jandova J, Beyer TE, Meuillet EJ and Watts
GS: The matrix protein CCN1/CYR61 is required for α(V)β(5)-mediated
cancer cell migration. Cell Biochem Funct. 30:687–695. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Jun JI and Lau LF: The matricellular
protein CCN1 induces fibroblast senescence and restricts fibrosis
in cutaneous wound healing. Nat Cell Biol. 12:676–685. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Zhang DY and Friedman SL:
Fibrosis-dependent mechanisms of hepatocarcinogenesis. Hepatology.
56:769–775. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Nejak-Bowen KN and Monga SP: Beta-catenin
signaling, liver regeneration and hepatocellular cancer: Sorting
the good from the bad. Semin Cancer Biol. 21:44–58. 2011.
View Article : Google Scholar :
|
|
37
|
Monga SP: Role of Wnt/β-catenin signaling
in liver metabolism and cancer. Int J Biochem Cell Biol.
43:1021–1029. 2011. View Article : Google Scholar
|
|
38
|
Awuah PK and Monga SP: Cell cycle-related
kinase links androgen receptor and β-catenin signaling in
hepatocellular carcinoma: Why are men at a loss. Hepatology.
55:970–973. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Liu Z, Guo Y, Li J, Xu J and Liu B:
Cotransfection of survivin and CD44v3 short hairpin RNAs affects
proliferation, apoptosis, and invasiveness of colorectal cancer.
Dig Dis Sci. 58:1590–1601. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Chen L, Liang L, Yan X, Liu N, Gong L, Pan
S, Lin F, Zhang Q, Zhao H and Zheng F: Survivin status affects
prognosis and chemosensitivity in epithelial ovarian cancer. Int J
Gynecol Cancer. 23:256–263. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Jia YL, Shi L, Zhou JN, Fu CJ, Chen L,
Yuan HF, Wang YF, Yan XL, Xu YC, Zeng Q, et al: Epimorphin promotes
human hepatocellular carcinoma invasion and metastasis through
activation of focal adhesion kinase/extracellular signal-regulated
kinase/matrix metalloproteinase-9 axis. Hepatology. 54:1808–1818.
2011. View Article : Google Scholar : PubMed/NCBI
|