Introduction
Lung cancer is the most common malignancy worldwide
(accounting for ~12% of cancers) in terms of both incidence and
mortality. In addition, a tendency toward increased incidence is
estimated (1). More than 80% of
diagnosed lung cancers belong to the group of non-small cell
carcinomas (NSCLC), and the majority of these cases are diagnosed
in advanced disease stages (2). In
view of these facts, the discovery of new prognostic and predictive
factors is of high importance.
The SOX (sex-determining region on the Y
chromosome-related high mobility group box) genes encode a group of
transcription factors sharing a high-mobility group (HMG) domain,
which specifically binds to the 5′-(A/T)(A/T)CAA (A/T)G-3′ DNA
sequence motif (3,4). Through binding with DNA, whether
directly or indirectly via co-factors, SOX proteins are capable of
regulating transcription. Unlike most transcription factors, the
members of the SOX family modify the conformation of DNA by binding
to its minor groove (5). Moreover,
they are capable of sequestering other transcription factors into
complexes (5). The SOX family is
divided into ten groups (A–J) based on their amino acid homology
(5). SOX18, along with SOX7 and
SOX17, is part of the F group (SOX F) of SOX proteins (3,5).
Accumulating lines of evidence suggest that SOX18 may influence
neonatal, as well as postnatal, vascularization (6–10).
Furthermore, SOX7 and SOX17 have been shown to possess some
homology, and may complement the function of SOX18 during the
above-mentioned procesess (8,11).
It has been shown that mutations in SOX18 can lead to
defective blood and lymphatic vessel formation, what is observed in
the hypotrichosis-lymphedema-telangiectasia syndrome (12–14).
Recent findings indicate that SOX18 may play an
important role in tumour growth (15–17).
SOX18 expression has been found in cancer cell lines of various
malignancies, including breast, gastric and pancreatic cancers
(18). Recently, we found that
SOX18 expression increases in invasive ductal breast cancer (IDC)
cells, and that its expression increases with malignancy grade and
amplification of human epidermal growth factor receptor 2 (HER2)
(19). In addition, Eom et
al (20) found that SOX18,
along with SOX7 and SOX17, was overexpressed in gastric cancer
tissues, compared to corresponding normal tissues. Analysis of
SOX18 immunostained slides showed that SOX18 expression was
exclusively noted in the stromal cells (but not in the cancer
cells) of the analysed gastric cancers, and its high expression
correlated with poor patient survival (20). Evidence suggests that SOX18
expression may also be involved in cell proliferation. Inhibition
of SOX18 expression in MCF-7 breast cancer cells and in vascular
smooth muscle cells of human atherosclerotic lesions has been
observed to lead to decreased proliferation rates in both cell
lines (16,21).
To date, SOX18 expression in lung cancer cell lines
and tissues has only been studied on the mRNA level. It has been
shown that its expression is lower in NSCLC tissues and cancer cell
lines; this is associated with increased CpG island
hypermethylation of SOX18 promoter (22,23).
Moreover, the prognostic significance of SOX18 expression in NSCLC
has not yet been determined. In the present study, we therefore,
analysed SOX18 expression on the mRNA and on the protein
level in a cohort of NSCLC cases, putting emphasis on the clinical
and pathological data of the patients in order to determine its
prognostic significance.
Materials and methods
Patients and clinical samples
The present study was approved by the Bioethics
Commission at the Wroclaw Medical University and investigations
were performed after a written informed consent was obtained. The
studies were performed on archival material originating from 198
samples of NSCLC taken during surgical resections in 2007–2012 at
the Lower Silesia Centre for Pulmonary Diseases in Wroclaw. The
study group consisted of 94 adenocarcinomas (AC), 89 squamous cell
carcinomas (SQC) and 15 large cell carcinomas (LCC). All the
samples used in the present study were collected prior to
administration of chemotherapy and radiotherapy. The pTNM
classification was made according to the recommendations of the
International Association for the Study of Lung Cancer (IASLC)
(24). Clinical data were derived
from hospital archives and are summarized in Table I. The mean observation time of
patients was 27.49±37.19 months (range, 1–147). During this time,
100 (50.5%) of the patients died.
 | Table IClinical and pathological data of the
studied patients with non-small cell lung cancer. |
Table I
Clinical and pathological data of the
studied patients with non-small cell lung cancer.
| Parameters | All cases
(N=198)
n (%) | AC (N=94)
n (%) | SQC
(N=89)
n (%) | LCC
(N=15)
n (%) | Real-time PCR
(N=42)
n (%) |
|---|
| Age (years) |
| Mean | 63.45±8.6 | 62.4±9.15 | 63.13±7.21 | 64.61±8.14 | 65.17±8.37 |
| Range | (39–82) | (39–80) | (54–77) | (41–82) | (51–82) |
| Gender |
| Male | 149 (75.3) | 70 (74.5) | 69 (77.5) | 10 (66.7) | 32 (76.2) |
| Female | 49 (24.7) | 24 (25.5) | 20 (22.5) | 5 (33.3) | 10 (23.8) |
| Tumour size |
| pT1 | 59 (29.8) | 27 (28.7) | 26 (29.2) | 6 (40) | 15 (35.7) |
| pT2 | 97 (49.0) | 44 (46.8) | 46 (51.7) | 7 (46.6) | 21 (50) |
| pT3 | 19 (9.6) | 7 (7.5) | 11 (12.4) | 1 (6.7) | 5 (11.9) |
| pT4 | 23 (11.6) | 16 (17) | 6 (6.7) | 1 (6.7) | 1 (2.4) |
| Lymph nodes |
| pN0 | 97 (49.0) | 35 (37.2) | 52 (58.4) | 10 (66.7) | 25 (59.5) |
| pN1, pN2 | 101 (51.0) | 59 (62.8) | 37 (41.6) | 5 (33.3) | 17 (40.5) |
| Stage |
| IA | 45 (22.7) | 19 (20.2) | 21 (23.5) | 5 (33.3) | 11 (26.2) |
| IB | 36 (18.2) | 13 (13.8) | 20 (22.5) | 3 (20) | 7 (16.7) |
| IIA | 23 (11.6) | 11 (11.8) | 11 (12.4) | 1 (6.7) | 8 (19) |
| IIB | 17 (8.6) | 5 (5.4) | 11 (12.4) | 1 (6.7) | 5 (11.9) |
| IIIA | 53 (26.7) | 29 (30.7) | 20 (22.5) | 4 (26.6) | 9 (21.4) |
| IIIB | 14 (7.1) | 9 (9.6) | 4 (4.5) | 1 (6.7) | - |
| IV | 10 (5.1) | 8 (8.5) | 2 (2.2) | - | 2 (4.8) |
| Malignancy
grade |
| G1 | 9 (5.0) | 5 (5.3) | 4 (4.5) | - | 3 (7.1) |
| G2 | 136 (74.3) | 68 (72.4) | 68 (76.4) | - | 27 (64.3) |
| G3 | 38 (20.7) | 21 (22.3) | 17 (19.1) | - | 12 (28.6) |
In each case, the paraffin sections were stained
with hematoxylin/eosin (H&E) and assessed by two independent
pathologists to verify the utility of the samples for
immunohistochemical (IHC) studies, the diagnosis, and the degree of
tumour malignancy. In case of 42 NSCLC patients, resected tumour
fragments and additional non-malignant lung tissue (NMLT) adjacent
to the primary tumour of the same 29 patients were collected into
RNAlater RNA stabilizing fluid (Qiagen, Hilden, Germany) and stored
at −20°C until real-time PCR studies were performed. The group
consisted of 23 AC, 16 SQC and 3 LCC cases (Table I). NSCLC and NMLT tissues were also
collected and frozen in liquid nitrogen and stored at −80°C in the
case of eight patients.
Cell lines
Three NSCLC cell lines (NCI-H1703, NCI-H522 and
A549) and a normal lung fibroblast cell line (IMR-90) obtained from
the American Type Culture Collection (ATCC, Manassas, VA, USA) were
used in the present study. The NCI-H1703 cell line was derived from
stage I SQC, the NCI-H522 cell line from stage II AC and the A549
cell line from a highly malignant AC.
Both NCI-H1703 and NCI-H522 cell lines were cultured
in RPMI-1640 medium with the addition of 2 mM L-glutamine (Lonza,
Basel, Switzerland). The A549 cell line was grown in high glucose
DMEM medium and 2 mM L-glutamine, whereas the fibroblastic IMR-90
cell line in the MEM medium was supplemented with non-essential
amino acids (Sigma, St. Louis, MO, USA). All media were also
supplemented with fetal bovine serum (Sigma), up to a final
concentration of 10%. These cell lines were cultured at 37°C and at
5% CO2.
Immunhistochemistry
IHC reactions were performed using a previously
established protocol in Autostainer Link 48 (DakoCytomation,
Glostrup, Denmark) to ensure repeatable experimental conditions.
Murine monoclonal antibodies directed against SOX18 (Santa Cruz
Biotechnology, Santa Cruz, CA, USA) and Ki-67 (clone MIB-1;
DakoCytomation) were utilized.
The sections were first boiled in Target Retrieval
Solution buffer (pH 9.0 for SOX18 and pH 6.0 for Ki-67) using a
Pre-Treatment link platform (in order to deparaffinize, rehydrate,
and unmask the antigens) and subsequently cooled in a rinsing
buffer (TBS/0.1% Tween). The activity of endogenous peroxidase was
blocked by 5 min incubation with EnVision FLEX peroxidase-blocking
reagent. EnVision FLEX System was used to visualize the antigens.
After rinsing the slides in TBS/0.1% Tween buffer, the primary
antibodies were applied for 20 min at room temperature. Next, the
slides were again rinsed in buffer and incubated for 20 min with
secondary antibodies, EnVision FLEX/HRP. To visualize the reaction,
sections were incubated for 10 min with EnVision FLEX working
solution, where 3,3′-diaminobenzidine (DAB) was used as a
chromogen. All slides were counter-stained with EnVision FLEX
hematoxylin. Subsequently, the sections were dehydrated in alcohol
and xylene, and then mounted in SUB-X mounting medium. All the
equipment and reagents besides the SOX18 antibody were obtained in
DakoCytomation.
Evaluation of IHC reactions
All IHC sections were evaluated using a BX41 light
microscope (Olympus, Tokyo, Japan) by two independent pathologists
who were blinded to the patients’ clinical data. SOX18 expression
was analysed depending on the cellular localization in the NSCLC
cancer cells. Cytoplasmic SOX18 (cSOX18) expression was assessed
using the immunoreactive score (IRS) of Remmele and Stegner
(25). This scale evaluates the
percentage of cells with positive reaction (0 points, absence of
cells with positive reaction; 1 point, 1–10% cells with positive
reaction; 2 points, 11–50%; 3 points, 51–80%; 4 points, over 80%
cells with positive reaction) and the intensity of the reaction (0,
no reaction; 1, low intensity of the reaction product; 2, moderate
intensity of the reaction colour; and 3, intense colour of the
reaction). In the case of nuclear SOX18 (nSOX18) and Ki-67
expression in NSCLC cancer cells, a semi-quantitative scale based
on tumour cell positivity in the whole tissue section was employed
(26). This scale is encoded as: 0
(0% cells stained), 1 (1–10% cells stained), 2 (11–25% cells
stained), 3 (26–50% cells stained) and 4 (51–100% cells
stained).
RNA extraction and cDNA synthesis,
real-time PCR
The total RNA from the analysed cell lines
(NCI-H1703, NCI-H522, A549 and IMR-90), NSCLC, and NMLT tissues was
isolated using the RNeasy Mini kit (both Qiagen), according to the
manufacturer’s instructions. The protocol included on-column DNAse
digestion to eliminate the genomic DNA. RNA quality and integrity
were determined by an Agilent 2100 Bioanalyzer on RNA Pico Chips
(both Agilent Technologies, Santa Clara, CA, USA). First-strand
cDNA was synthesized using the QuantiTect Reverse Transcription kit
(Qiagen).
The relative levels of SOX18 mRNA expression
were determined by quantitative real-time PCR using the 7900HT Fast
Real-Time PCR System and a TaqMan Gene Expression Master Mix
(Applied Biosystems, Foster City, CA, USA), according to the
manufacturer’s protocols, as in a previous study (19). The primers used were SOX18
Hs00746079_s1 for SOX18 and SDHA Hs00188166_m1 for
SDHA (Applied Biosystems), the latter serving as a reference
for determining SOX18 expression levels (27). The reactions were carried out in
triplicate under the following conditions: initial denaturation at
94°C for 120 sec, followed by 40 cycles of denaturation at 94°C for
15 sec, and annealing and elongation at 60°C for 60 sec. The
relative mRNA expression levels of SOX18 were calculated
using the ΔΔCt method.
SDS-PAGE and western blot technique
The present study was performed using previously
established experimental protocols (19). Whole protein lysates were obtained
from the cell lines under study using a Cell Lytic buffer, and from
the sampled NSCLC and NMLT tissues using the T-Per tissue protein
extraction reagent with the addition of protease inhibitors (both
Sigma). In the case of the cell lines, the cytoplasmic and nuclear
fractions were obtained using a ProteoExtract subcellular proteome
extraction kit according to the manufacturer’s instructions. The
samples were then centrifuged again (4°C, 10 min, 10,000 × g) to
collect the nuclear extracts. Whole-cell, nuclear and cytoplasmic
proteins were quantified using the BCA protein assay (Pierce,
Rockford, IL, USA), and resolved on 10% SDS-PAGE gels using the
Laemmli method. After electrophoresis, the samples were transferred
to polyvinylidene fluoride (PVDF) membranes (Immobilon; Millipore,
Bedford, MA, USA) and incubated with anti-human SOX18 antibody
(diluted 1:100; Santa Cruz Biotechnology) overnight at 4°C. Next,
the membranes were incubated with the secondary anti-mouse antibody
conjugated with horseradish peroxidase (Jackson ImmunoResearch,
Mill Valley, CA, USA) for 1 h at room temperature, rinsed, and
treated with the Immun-Star HRP chemiluminescent kit (Bio-Rad
Laboratories, Hercules, CA, USA). β-actin, detected with anti-human
β-actin antibody (Abcam, Cambridge, UK), was used as an internal
control to normalize the amounts of SOX18 on the same membrane.
Statistical analysis
Prism 5.0 (GraphPad Software, La Jolla, CA, USA)
statistical software was used to analyse the results. The
non-parametric Mann-Whitney U test (for unpaired observations) and
the Wilcoxon signed-rank test (for paired observations) were used
to compare groups of data. The associations between clinical and
pathological parameters and the expression of the studied IHC
markers were analysed using the Fisher’s exact test, and
correlations by the Spearman’s correlation test. Survival times
were determined by the Kaplan-Meier method, and the significance of
the differences was determined by a log-rank test. For each
variable, the hazard ratio (HR) and the 95% confidence interval
(95% CI) were estimated. In all the analyses, the results were
considered statistically significant when P<0.05.
Results
Relationship between immunohistochemical
SOX18 expression in NSCLC and patients’ clinical and pathological
data
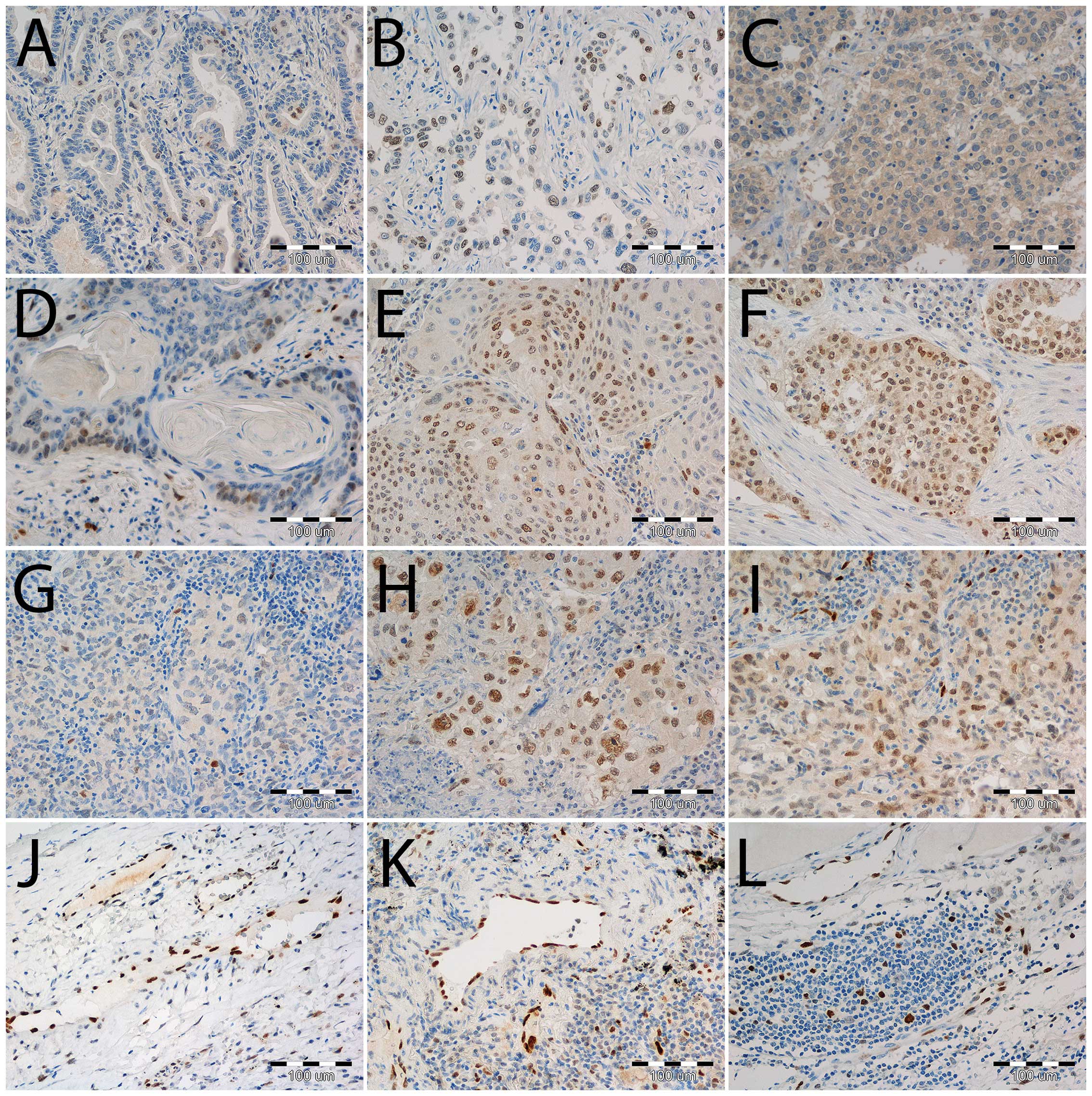
SOX18 expression was noted in cancer cell nuclei, as
well as in cytoplasm, in all of the three histological types of
NSCLC (Fig. 1). Nuclear SOX18
expression was noted in 187 out of 198 (94.4%) cases, whereas
cSOX18 expression was noted in 93 (47%) of the NSCLC cases. SOX18
expression was also observed in nuclei of vessels, and of some of
the immune cells in the tumour stroma (Fig. 1). For the purpose of statistical
analyses, and based on the median expression levels of nSOX18 and
cSOX18, the analysed cases were divided into the following groups:
Cases characterized by nSOX18 expression of 0–2 points (≤25% of
positive cells) were regarded as ‘low’, whereas those scoring 3–4
points (>25% of positive cells) were regarded as ‘high’.
Similarly, cases presenting no cSOX18 expression were classified as
negative, whereas those scoring IRS 1–12 were regarded as
positive.
A significant positive correlation was observed
between nSOX18 and cSOX18 expression in the whole study cohort
(r=0.35, P<0.0001), as well as in particular histological types:
AC (r=0.30, P=0.0038), SQC (r=0.37, P=0.0003) and LCC (r=0.56,
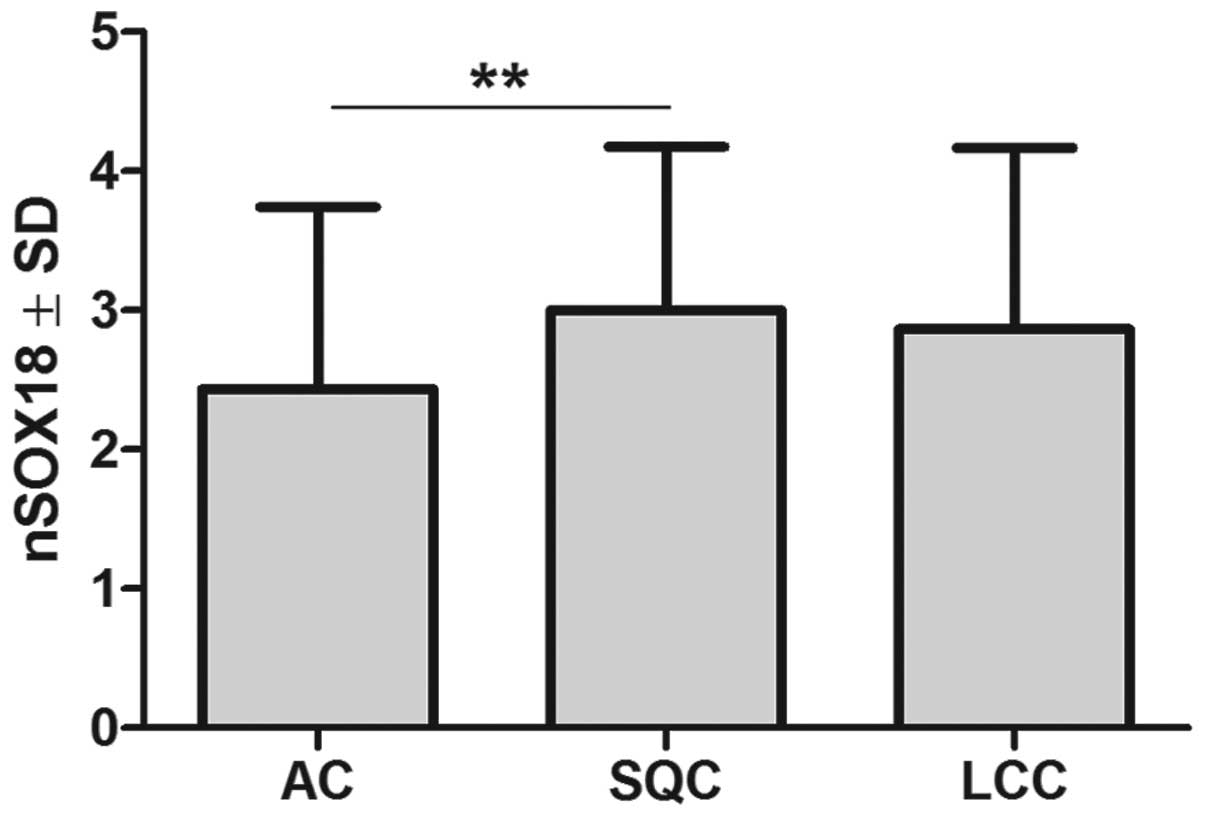
P=0.0306; Spearman correlation test, respectively). Nuclear SOX18
expression was significantly higher in the SQC (3.00±2.87) than in
the AC (2.44±2.87) cases (P=0.0021, Mann-Whitney U test; Fig. 2), however, no significant
differences were noted in regard to cSOX18 immunoreactivity between
particular NSCLC histological types (AC, IRS 1.00±1.29; SQC, IRS
1.21±1.50; and LCC, IRS 1.47±1.60). Moreover, nSOX18 expression
correlated positively with the expression of the Ki-67 antigen
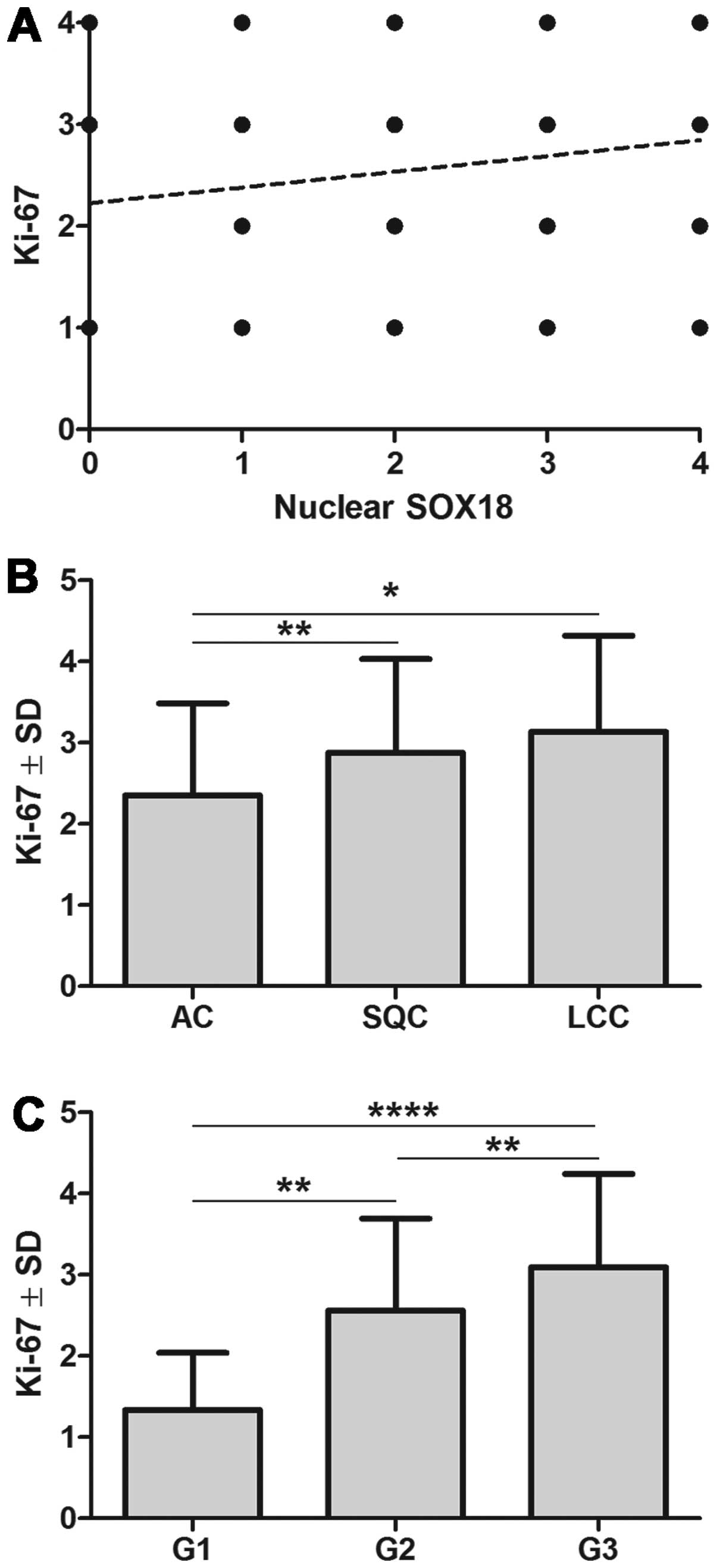
(r=0.17, P=0.0139, Spearman correlation test; Fig. 3A). It is noteworthy that Ki-67
antigen expression differed among the particular NSCLC histological
types. Significantly lower Ki-67 antigen expression was noted in
the AC cases (2.25±1.13), as compared with the SQC (2.88±1.16,
P=0.002) and LCC (3.13±1.87) cases (both Mann-Whitney U test;
Fig. 3B). Ki-67 antigen expression
increased with growing malignancy grade of the tumours (G1,
1.33±0.70; G2, 2.56±1.34; and G3, 3.09±1.15). Significant
differences were noted using the Mann-Whitney U test between G1
tumours and those of G2 and G3 (P=0.0024 and P<0.0001,
respectively). Also significant differences were observed between
G2 and G3 cancers (P=0.024, Mann-Whitney U test; Fig. 3C).
Analysis of nuclear and cytoplasmic SOX18
immunoreactivity in the whole cohort, as well as in the AC and SQC
types, revealed that higher nSOX18 expression was associated with
male gender of SQC patients (P=0.0281, Fisher’s exact test;
Table II). However, no other
association of nSOX18 and cSOX18 expression levels with the age of
the patients, gender, primary tumour size, presence of lymph node
metastasis or disease stage were noted (Tables II and III).
 | Table IIAssociation of nuclear SOX18 (nSOX18)
expression with the clinical and pathological data of patients. |
Table II
Association of nuclear SOX18 (nSOX18)
expression with the clinical and pathological data of patients.
| All cases
(N=198) | | AC (N=94) | | SQC (N=89) | |
|---|
|
| |
| |
| |
|---|
| Parameters | ≤25%
n (%) | >25%
n (%) | P-value | ≤25%
n (%) | >25%
n (%) | P-value | ≤25%
n (%) | >25%
n (%) | P-value |
|---|
| Age (years) |
| <65 | 47 (40.9) | 68 (59.1) | 0.6599 | 27 (46.6) | 31 (53.4) | 1.0000 | 16 (34.8) | 30 (65.2) | 0.6592 |
| ≥65 | 31 (37.3) | 52 (62.7) | | 16 (44.4) | 20 (55.6) | | 13 (30.2) | 30 (69.8) | |
| Gender |
| Male | 57 (38.3) | 92 (61.7) | 0.6147 | 34 (48.6) | 36 (51.4) | 0.4769 | 18 (26.1) | 51 (73.9) | 0.0281 |
| Female | 21 (42.9) | 28 (57.1) | | 9 (37.5) | 15 (62.5) | | 11 (55) | 9 (45) | |
| Tumour size |
| pT1 | 23 (39.7) | 35 (60.3) | 1.0000 | 11 (40.7) | 16 (59.3) | 0.6487 | 9 (34.6) | 17 (65.4) | 0.8077 |
| pT2–pT4 | 55 (39.3) | 85 (60.7) | | 32 (47.8) | 35 (52.2) | | 20 (31.7) | 43 (68.3) | |
| Lymph nodes |
| pN0 | 39 (40.2) | 58 (59.8) | 1.0000 | 19 (43.2) | 25 (56.8) | 0.6821 | 18 (34.6) | 34 (65.4) | 0.6543 |
| pN1, pN2 | 40 (39.2) | 62 (60.8) | | 24 (48) | 26 (52) | | 11 (29.7) | 26 (70.3) | |
| Stage |
| I | 34 (43.6) | 44 (56.4) | 0.5569 | 15 (46.9) | 17 (53.1) | 1.0000 | 15 (36.6) | 26 (63.4) | 0.5018 |
| II–IV | 47 (39.2) | 73 (60.8) | | 28 (45.2) | 34 (54.8) | | 14 (29.2) | 34 (70.8) | |
 | Table IIIAssociation of cytoplasmic SOX18
(cSOX18) expression with clinical and pathological data of the
studied patients. |
Table III
Association of cytoplasmic SOX18
(cSOX18) expression with clinical and pathological data of the
studied patients.
| All cases
(N=198) | | AC (N=94) | | SQC (N=89) | |
|---|
|
| |
| |
| |
|---|
| Parameters | IRS 0
n (%) | IRS 1–12
n (%) | P-value | IRS 0
n (%) | IRS 1–12 n (%) | P-value | IRS 0
n (%) | IRS 1–12
n (%) | P-value |
|---|
| Age (years) |
| <65 | 60 (52.2) | 55 (47.8) | 0.8853 | 33 (56.9) | 25 (43.1) | 0.5311 | 22 (47.8) | 24 (52.2) | 0.3974 |
| ≥65 | 45 (54.2) | 38 (45.8) | | 18 (50) | 18 (50) | | 25 (58.1) | 18 (41.9) | |
| Gender |
| Male | 70 (47) | 79 (53) | 0.5116 | 39 (55.7) | 31 (44.3) | 0.6434 | 35 (50.7) | 34 (49.3) | 0.6120 |
| Female | 26 (53.1) | 23 (46.9) | | 12 (50) | 12 (50) | | 12 (60) | 8 (40) | |
| Tumour size |
| pT1 | 33 (56.9) | 25 (43.1) | 0.5331 | 17 (63) | 10 (27) | 0.3616 | 13 (50) | 13 (50) | 0.8170 |
| pT2–pT4 | 72 (51.4) | 68 (48.6) | | 34 (50.7) | 33 (49.3) | | 34 (54) | 29 (46) | |
| Lymph nodes |
| pN0 | 59 (55.1) | 48 (44.9) | 0.5687 | 25 (58.1) | 18 (41.9) | 0.6765 | 28 (53.8) | 24 (46.2) | 0.8328 |
| pN1, pN2 | 46 (50.5) | 45 (49.5) | | 26 (52) | 24 (48) | | 19 (51.4) | 18 (48.6) | |
| Stage |
| I | 45 (55.6) | 36 (44.4) | 0.5660 | 18 (56.3) | 14 (43.7) | 0.8295 | 22 (53.7) | 19 (46.3) | 1.0000 |
| II–IV | 60 (51.3) | 57 (48.7) | | 33 (53.2) | 29 (46.8) | | 25 (52.1) | 23 (47.9) | |
SOX18 mRNA and protein expression in NMLT
and NSCLC with regard to patients’ clinical and pathological
characteristics
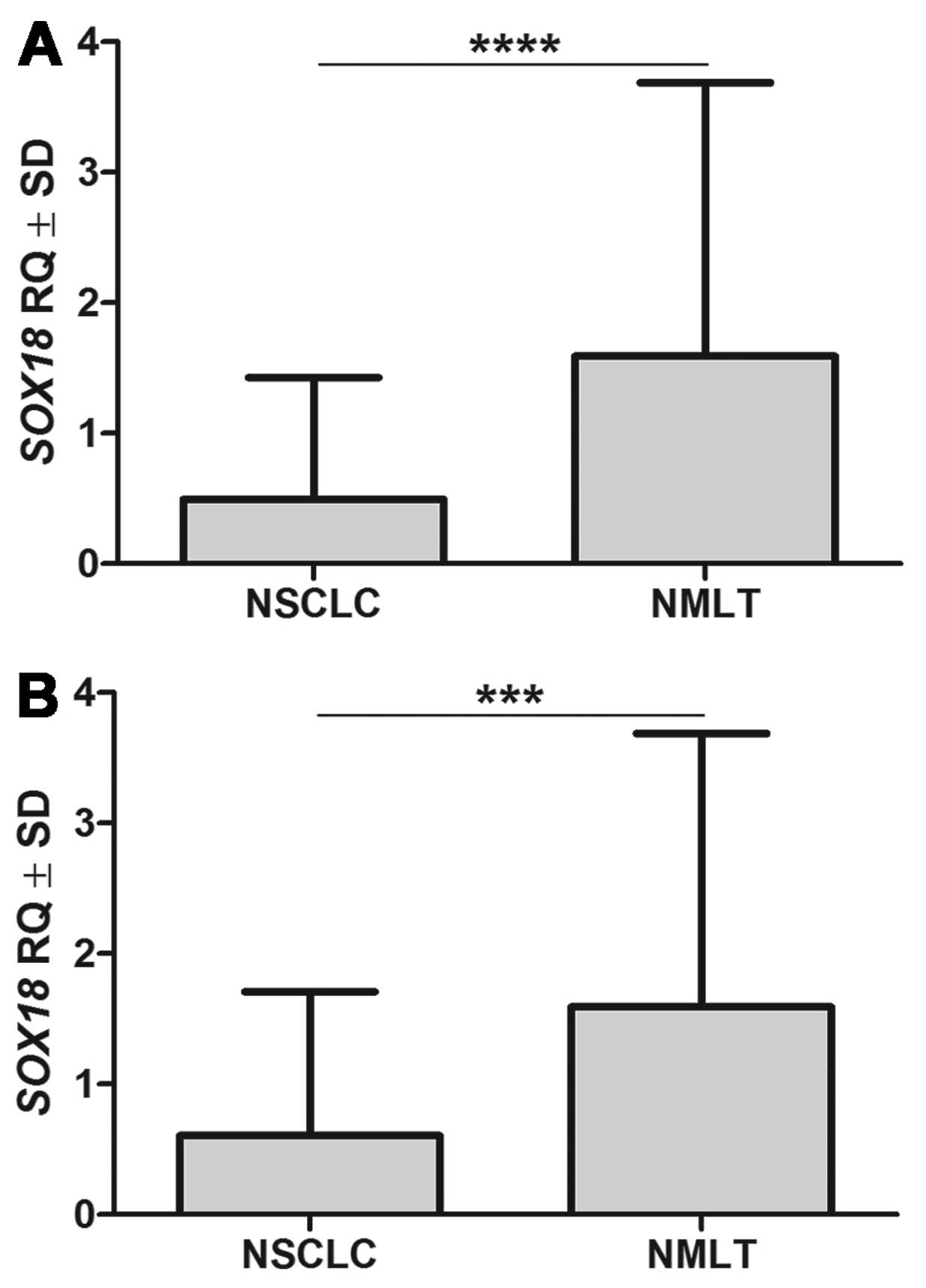
Real-time PCR analysis of SOX18 mRNA
expression was achieved in 39 out of 42 (92.9%) analysed NSCLC
samples and in all of the 29 NMLT cases. Significantly higher
SOX18 mRNA expression level was observed in NMLT (RQ
1.59±2.09) tissues than in NSCLC, both for all the analysed samples
(RQ 0.49±0.93, P<0.0001, Mann-Whitney U test) and for the paired
cases (RQ 0.60±1.10, P=0.0004, Wilcoxon signed-rank test; Fig. 4). In the paired sample analysis, a
higher SOX18 mRNA expression was noted in 27 (93.1%) cases
of NMLT, as compared with NSCLC. Statistical analysis did not
reveal any significant associations between the level of
SOX18 mRNA expression level and patients’ clinical and
pathological data (Table IV).
 | Table IVSOX18 mRNA expression, and
clinical and pathological data of non-small cell lung cancer
patients. |
Table IV
SOX18 mRNA expression, and
clinical and pathological data of non-small cell lung cancer
patients.
| Parameters | Analysed cases n
(%) | RQ ± SD | P-value |
|---|
| Age (years) |
| <65 | 26 (61.9) | 0.5585±1.158 | 0.4762 |
| ≥65 | 16 (38.1) | 0.3937±0.3521 | |
| Gender |
| Male | 32 (76.2) | 0.5353±1.053 | 0.7341 |
| Female | 10 (23.8) | 0.3688±0.3461 | |
| Malignancy
grade |
| G2 | 27 (64.3) | 0.5023±0.9666 | 0.5286 |
| G3, LCC | 15 (35.7) | 0.4837±0.9010 | |
| Tumour size |
| pT1 | 15 (35.7) | 0.7107±1.264 | 0.0929 |
| pT2–pT4 | 27 (64.3) | 0.3762±0.6857 | |
| Lymph nodes |
| pN0 | 25 (59.5) | 0.6411±1.181 | 0.7390 |
| pN1, pN2 | 17 (40.5) | 0.2818±0.2377 | |
| Stage |
| I | 18 (42.9) | 0.6160±1.175 | 0.5005 |
| II–IV | 24 (57.1) | 0.4055±0.7145 | |
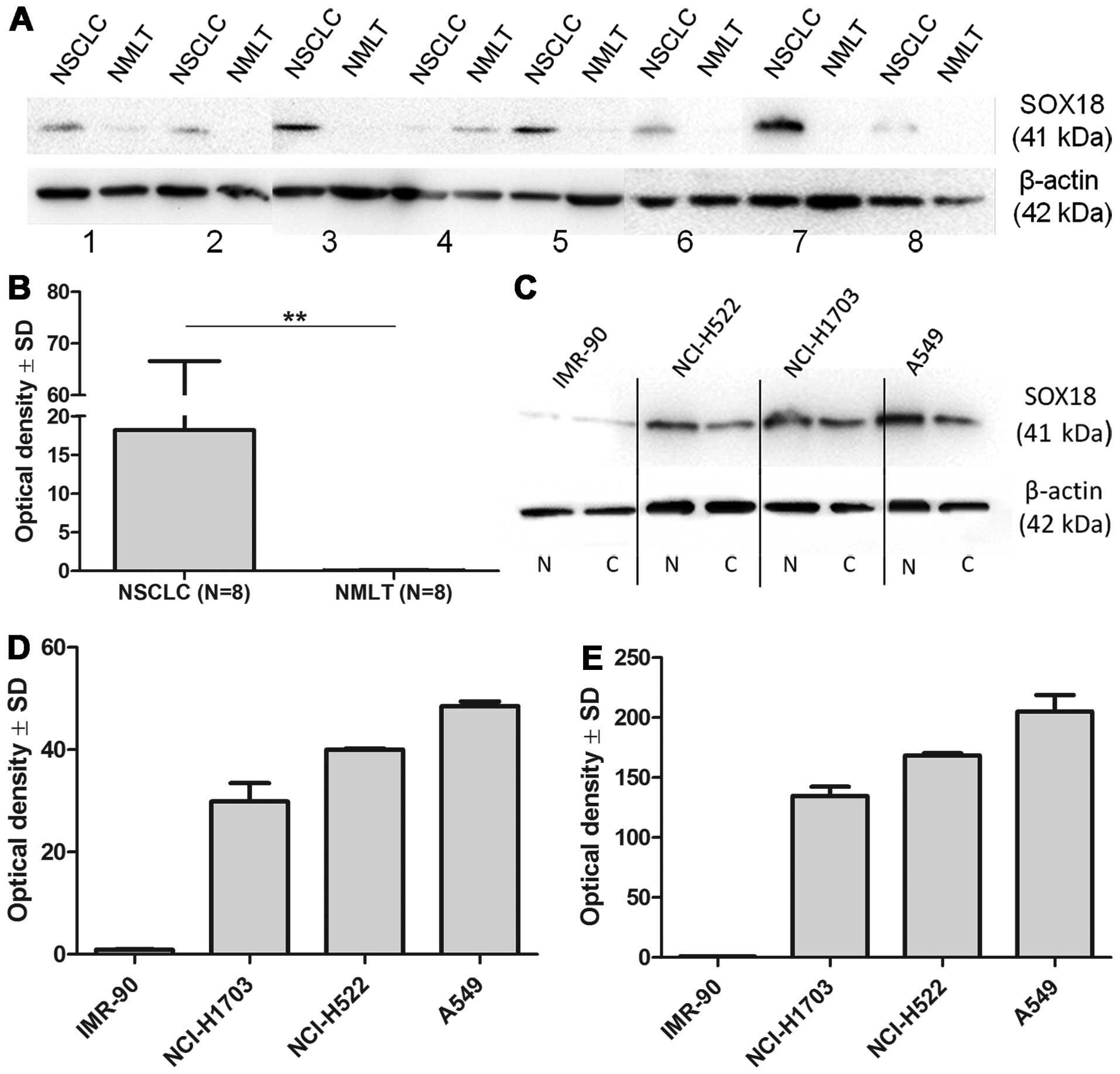
SOX18 expression determined in the paired frozen
samples of NMLT and NSCLC using the western blot technique revealed
significantly higher expression in the latter (18.18±48.44 vs.
0.05±0.06, P=0.018, Wilcoxon signed-rank test; Fig. 5A and B).
SOX18 expression in lung cancer cell
lines and normal lung fibroblasts
Analysis of SOX18 protein levels using the western
blot technique in the studied cell lines revealed increased
expression in the cytoplasmic/membranous fraction, as well as in
the nuclear fraction, of NCI-H1703, NCI-H522 and A549 cancer cell
lines (Fig. 5C–E). However, no
SOX18 expression could be noted in the corresponding cellular
fractions of the normal lung fibroblast cell line (IMR-90).
Prognostic significance of SOX18
expression in NSCLC
Univariate analysis of patient survival in the whole
study group revealed that the presence of cytoplasmic SOX18
expression was associated with poor patient outcome (P=0.0077;
Table V). From among the factors
considered in this group, AC histological type (P=0.0076), larger
primary tumour size (P=0.0056), presence of lymph node metastases
(P=0.0001), advanced disease stage (P=0.0004) and patient age
(P=0.0085) were also associated with poor prognosis. Cytoplasmic
SOX18 expression was a negative prognostic factor also in the group
of 94 AC (P=0.0048), as were larger primary tumour size (P=0.0197),
the presence of lymph node metastases (P=0.0064), advanced disease
stage (P=0.0291) and age (P=0.321) (Table V). Univariate survival analysis in
the SQC group showed that G3 malignancy grade (P=0.0436) and the
presence of lymph node metastases (P=0.0006) were associated with
poor patient survival (Table
V).
 | Table VUnivariate survival analysis of the
whole study cohort and in the adenocarcinoma and squamous cell lung
cancer patients. |
Table V
Univariate survival analysis of the
whole study cohort and in the adenocarcinoma and squamous cell lung
cancer patients.
| Overall
survival |
|---|
|
|
|---|
| Parameters | HR | 95% CI | P-value |
|---|
| All patients |
| nSOX18 (≤25 vs.
>25%) | 1.012 | 0.6765–1.513 | 0.9546 |
| cSOX18 (IRS 0 vs.
1–12) | 1.748 | 1.159–2.635 | 0.0077 |
| Ki-67 antigen (≤25
vs. >25%) | 1.017 | 0.6812–1.519 | 0.9333 |
| Histological type
(AC vs. SQC vs. LCC) | - | - | 0.0297 |
| Histological type
(AC vs. SQC and LCC) | 1.728 | 1.156–2.582 | 0.0076 |
| Malignancy grade
(G1, G2 vs. G3, LCC) | 1.553 | 0.9707–2.483 | 0.0664 |
| Tumour size (pT1
vs. pT2–pT4) | 1.837 | 1.195–2.825 | 0.0056 |
| Lymph nodes (pN0
vs. pN1, pN2) | 2.741 | 1.838–4.086 | 0.0001 |
| Stage (I vs.
II–IV) | 2.059 | 1.379–3.075 | 0.0004 |
| Gender (male vs.
female) | 1.235 | 0.7802–1.956 | 0.3673 |
| Age (≤65 vs.
>65 years) | 1.759 | 1.057–3.440 | 0.0085 |
| Adenocarcinoma
(AC) |
| nSOX18 (≤25 vs.
>25%) | 0.9724 | 0.5634–1.678 | 0.9200 |
| cSOX18 (IRS 0 vs.
1–12) | 2.267 | 1.284–4.004 | 0.0048 |
| Ki-67 antigen (≤25
vs. >25%) | 1.276 | 0.7464–2.180 | 0.3732 |
| Malignancy grade
(G1, G2 vs. G3) | 1.618 | 0.8065–3.247 | 0.1755 |
| Tumour size (pT1
vs. pT2–pT4) | 2.017 | 1.119–3.638 | 0.0197 |
| Lymph nodes (pN0
vs. pN1, pN2) | 2.137 | 1.238–3.687 | 0.0064 |
| Stage (I vs.
II–IV) | 1.861 | 1.065–3.251 | 0.0291 |
| Gender (male vs.
female) | 0.9261 | 0.4964–1.728 | 0.8093 |
| Age (≤65 vs.
>65 years) | 1.906 | 1.057–3.440 | 0.0321 |
| Squamous cell
carcinoma (SQC) |
| nSOX18 (≤25 vs.
>25%) | 1.172 | 0.5941–2.311 | 0.6476 |
| cSOX18 (IRS 0 vs.
1–12) | 1.395 | 0.7165–2.718 | 0.3272 |
| Ki-67 antigen (≤25
vs. >25%) | 0.8592 | 0.4349–1.697 | 0.6623 |
| Malignancy grade
(G1, G2 vs. G3) | 2.548 | 1.027–6.318 | 0.0436 |
| Tumour size (pT1
vs. pT2–pT4) | 1.262 | 0.6063–2.627 | 0.5337 |
| Lymph nodes (pN0
vs. pN1, pN2) | 3.262 | 1.656–6.426 | 0.0006 |
| Stage (I vs.
II–IV) | 1.864 | 0.9567–3.631 | 0.0673 |
| Gender (male vs.
female) | 1.774 | 0.8198–3.838 | 0.1456 |
| Age (≤65 vs.
>65 years) | 1.609 | 0.8249–3.139 | 0.1629 |
Discussion
Accumulating lines of evidence point to the
potential role of SOX18 transcription factor in the progression of
various cancers. Recently, we showed that high nuclear
immunoreactivity in cancer cells of IDC is associated with higher
malignancy grade and HER2 amplification (19). SOX18 expression has also been
detected in cell lines derived from melanoma, as well as from
gastric, pancreatic and breast cancer (16,18,19).
Moreover, increased SOX18 expression in gastric cancer stroma
(though not in cancer cells) was associated with poor outcome of
the patients (20). SOX18
expression has also been studied in NSCLC tissues and its derived
cancer cell lines, but only on the mRNA level (and without
addressing its prognostic value) (22,23).
To the best of our knowledge, we are the first to
assess SOX18 expression on the protein level (using both IHC and
the western blot technique) in NMLT, NSCLC specimens and cancer
cell lines. We observed SOX18 immunoreactivity in the nuclei and
cytoplasm of cancer cells in paraffin sections, as well as in the
lung cancer cell lines that we investigated (NCI-H1703, NCI-H522
and A549). The results of the present study are in line with our
previous observations regarding SOX18 expression in IDC tissues and
its cell lines (19). Moreover, in
the current study, as well as in that of Pula et al
(19), we detected no SOX18
expression in fibroblasts of immunostained paraffin sections of
NSCLC and IDC. In addition, no expression of this transcription
factor was noted in the fibroblastic cell lines IMR-90 and NHDF
which corresponds well with the results derived from the IHC
sections. The cytoplasmic expression of SOX18 in lung cancer cells
may be partly explained by the structure of this transcription
factor. The HMG domain of this transcription factor has been shown
to be capable of binding other compounds, thus mediating
protein-protein interactions (28,29).
It may be possible that SOX18 has additional unrecognized functions
in cytoplasm, such as regulating the activity of the Wnt signalling
pathway, as has been demonstrated for the other members of the SOX
F family, SOX7 and SOX17 (30,31).
We observed a discrepancy between the mRNA and
protein expression of SOX18 in NMLT and NSCLC tissues. We noted
significantly lower mRNA expression levels of this transcription
factor in the paired tissues and in all of the studied NSCLC
tissues, as compared to NMLT. This finding is in accordance with
the previous observations of Azhikina et al (23) and Dammann et al (22), who identified higher methylation
levels of SOX18 promoter in NSCLC tissues and lung cancer cell
lines. In contrast to SOX18 mRNA levels, its protein
expression increased in NSCLC tissues, as determined utilizing the
western blot technique. Due to these discrepancies, our findings
may point to the existence of a negative regulative feedback loop
in SOX18 expression. Based on the previous observations of Azhikina
et al (23) and Dammann
et al (22), it is possible
that the decreased SOX18 mRNA expression in NSCLC tissues is
caused by promoter hypermethylation, which is frequently observed
in this malignancy (32).
Transcription factors of the SOX F group have been shown to
complement their functions during angiogenesis and
lymphangiogenesis (8,10,11).
In line with the above mentioned capability, SOX7 and
SOX17 mRNA expression have also been shown to be
significantly downregulated in NSCLC as compared to NMLT (31,33,34).
In this study, we observed a positive correlation
between nuclear SOX18 immunoreactivity and that of the Ki-67
antigen in cancer cells of NSCLC. These observations may point to a
possible role of SOX18 in the regulation of the proliferation rate
of cancer cells. Previous studies have shown that SOX18 expression
influences the proliferation of MCF-7 and VSMC cell lines (16,21).
Inhibition of this protein leads to a decrease in the proliferation
of both cell lines. Moreover, the impact of SOX18 on cellular
proliferation may be indirectly supported by the results of Darby
et al (15), who showed
that SOX18 mRNA expression increased during wound healing
and diminished after the process ended.
In the present study, we have demonstrated that
cytoplasmic SOX18 expression is associated with poor patient
outcome for both the study cohort as a whole and for the AC subtype
only. Interestingly, the intensity of immunoreactivity of SOX18
nuclei did not influence patient survival, although a positive
correlation with the expression of Ki-67 antigen was recorded. The
latter also increased with the malignancy grade of the tumours, but
did not impact patients’ overall survival. The observed poor
outcome of NSCLC and AC patients characterized by increased
cytoplasmic SOX18 expression may result from its possible
regulation of the Wnt signalling pathway (30). Nevertheless, further studies are
needed to fully clarify this mechanism.
In summary, we have shown for the first time that
SOX18 is expressed in cancer cells and vessels of NSCLC. Moreover,
its expression is differentiated in regard to cellular
localization. Based on our observations, cytoplasmic expression of
SOX18 may be a new prognostic marker of poor prognosis in NSCLC.
However, further studies are needed to warrant its prognostic
utility in this malignancy.
Acknowledgements
The present study was supported by a research grant
from the Wrovasc Integrated Cardiovascular Centre Project, and
co-financed by the European Regional Development Fund within the
Innovative Economy Operational Program, 2007–2013 realized in
Regional Specialist Hospital, Research and Development Centre in
Wroclaw.
References
|
1
|
Siegel R, Naishadham D and Jemal A: Cancer
statistics, 2013. CA Cancer J Clin. 63:11–30. 2013. View Article : Google Scholar
|
|
2
|
Brandao GD, Brega EF and Spatz A: The role
of molecular pathology in non-small-cell lung carcinoma-now and in
the future. Curr Oncol. 19(Suppl 1): S24–S32. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wegner M: From head to toes: the multiple
facets of Sox proteins. Nucleic Acids Res. 27:1409–1420. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Harley VR, Lovell-Badge R and Goodfellow
PN: Definition of a consensus DNA binding site for SRY. Nucleic
Acids Res. 22:1500–1501. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wegner M: All-purpose Sox: the many roles
of Sox proteins in gene expression. Int J Biochem Cell Biol.
42:381–390. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Francois M, Koopman P and Beltrame M: SoxF
genes: key players in the development of the cardio-vascular
system. Int J Biochem Cell Biol. 42:445–448. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Cermenati S, Moleri S, Cimbro S, et al:
Sox18 and Sox7 play redundant roles in vascular development. Blood.
111:2657–2666. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hosking B, Francois M, Wilhelm D, et al:
Sox7 and Sox17 are strain-specific modifiers of the lymphangiogenic
defects caused by Sox18 dysfunction in mice. Development.
136:2385–2391. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Matsui T, Kanai-Azuma M, Hara K, et al:
Redundant roles of Sox17 and Sox18 in postnatal angiogenesis in
mice. J Cell Sci. 119:3513–3526. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Sakamoto Y, Hara K, Kanai-Azuma M, et al:
Redundant roles of Sox17 and Sox18 in early cardiovascular
development of mouse embryos. Biochem Biophys Res Commun.
360:539–544. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Herpers R, van de Kamp E, Duckers HJ and
Schulte-Merker S: Redundant roles for sox7 and sox18 in
arteriovenous specification in zebrafish. Circ Res. 102:12–15.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Downes M, Francois M, Ferguson C, et al:
Vascular defects in a mouse model of
hypotrichosis-lymphedema-telangiectasia syndrome indicate a role
for SOX18 in blood vessel maturation. Hum Mol Genet. 18:2839–2850.
2009. View Article : Google Scholar
|
|
13
|
Francois M, Caprini A, Hosking B, et al:
Sox18 induces development of the lymphatic vasculature in mice.
Nature. 456:643–647. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Irrthum A, Devriendt K, Chitayat D, et al:
Mutations in the transcription factor gene SOX18 underlie recessive
and dominant forms of hypotrichosis-lymphedema-telangiectasia. Am J
Hum Genet. 72:1470–1478. 2003. View
Article : Google Scholar : PubMed/NCBI
|
|
15
|
Darby IA, Bisucci T, Raghoenath S, et al:
Sox18 is transiently expressed during angiogenesis in granulation
tissue of skin wounds with an identical expression pattern to Flk-1
mRNA. Lab Invest. 81:937–943. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Young N, Hahn CN, Poh A, et al: Effect of
disrupted SOX18 transcription factor function on tumor growth,
vascularization, and endothelial development. J Natl Cancer Inst.
98:1060–1067. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Duong T, Proulx ST, Luciani P, et al:
Genetic ablation of SOX18 function suppresses tumor
lymphangiogenesis and metastasis of melanoma in mice. Cancer Res.
72:3105–3114. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Saitoh T and Katoh M: Expression of human
SOX18 in normal tissues and tumors. Int J Mol Med. 10:339–344.
2002.PubMed/NCBI
|
|
19
|
Pula B, Olbromski M, Wojnar A, et al:
Impact of SOX18 expression in cancer cells and vessels on the
outcome of invasive ductal breast carcinoma. Cell Oncol (Dordr).
36:469–483. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Eom BW, Jo MJ, Kook MC, et al: The
lymphangiogenic factor SOX 18: a key indicator to stage gastric
tumor progression. Int J Cancer. 131:41–48. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Garcia-Ramirez M, Martinez-Gonzalez J,
Juan-Babot JO, et al: Transcription factor SOX18 is expressed in
human coronary atherosclerotic lesions and regulates DNA synthesis
and vascular cell growth. Arterioscler Thromb Vasc Biol.
25:2398–2403. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Dammann R, Strunnikova M, Schagdarsurengin
U, et al: CpG island methylation and expression of
tumour-associated genes in lung carcinoma. Eur J Cancer.
41:1223–1236. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Azhikina T, Kozlova A, Skvortsov T and
Sverdlov E: Heterogeneity and degree of TIMP4, GATA4, SOX18, and
EGFL7 gene promoter methylation in non-small cell lung cancer and
surrounding tissues. Cancer Genet. 204:492–500. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Detterbeck FC, Boffa DJ and Tanoue LT: The
new lung cancer staging system. Chest. 136:260–271. 2009.
View Article : Google Scholar
|
|
25
|
Remmele W and Stegner HE: Recommendation
for uniform definition of an immunoreactive score (IRS) for
immunohisto-chemical estrogen receptor detection (ER-ICA) in breast
cancer tissue. Pathologe. 8:138–140. 1987.(In German).
|
|
26
|
Werynska B, Pula B, Muszczynska-Bernhard
B, et al: Metallothionein 1F and 2A overexpression predicts poor
outcome of non-small cell lung cancer patients. Exp Mol Pathol.
94:301–308. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Doroudi R, Andersson M, Svensson PA, et
al: Methodological studies of multiple reference genes as
endogenous controls in vascular gene expression studies.
Endothelium. 12:215–223. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Lefebvre V, Dumitriu B, Penzo-Mendez A, et
al: Control of cell fate and differentiation by Sry-related
high-mobility-group box (Sox) transcription factors. Int J Biochem
Cell Biol. 39:2195–2214. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Wilson M and Koopman P: Matching SOX:
partner proteins and co-factors of the SOX family of
transcriptional regulators. Curr Opin Genet Dev. 12:441–446. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Zhu Y, Li Y, Jun Wei JW and Liu X: The
role of sox genes in lung morphogenesis and cancer. Int J Mol Sci.
13:15767–15783. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Yin D, Jia Y, Yu Y, et al: SOX17
methylation inhibits its antagonism of Wnt signaling pathway in
lung cancer. Discov Med. 14:33–40. 2012.PubMed/NCBI
|
|
32
|
Tessema M, Willink R, Do K, et al:
Promoter methylation of genes in and around the candidate lung
cancer susceptibility locus 6q23-25. Cancer Res. 68:1707–1714.
2008. View Article : Google Scholar
|
|
33
|
Hayano T, Garg M, Yin D, et al: SOX7 is
down-regulated in lung cancer. J Exp Clin Cancer Res. 32:172013.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Li B, Ge Z, Song S, et al: Decreased
expression of SOX7 is correlated with poor prognosis in lung
adenocarcinoma patients. Pathol Oncol Res. 18:1039–1045. 2012.
View Article : Google Scholar : PubMed/NCBI
|