Introduction
Esophageal cancer is one of the leading causes of
cancer-related mortality in several countries. It is estimated that
200,000 individuals succumb to esophageal cancer annually (1,2).
Surgery is the main treatment modality for resectable esophageal
cancer (3). However, conventional
surgery is associated with higher mortality and postoperative
complication rates (4). In the
past, patients reported more concerns regarding the severe
postoperative complications and survival time, but appeared to be
less concerned with the overall quality of life.
An increasing number of minimally invasive surgical
techniques are currently used to reduce the incidence of
postoperative complications and the mortality rate of patients with
esophageal cancer (5,6). However, it is difficult to undertake
such surgery without video assistance. Video-assisted thoracic
surgery (VATS) has become the mainstay of minimally invasive
thoracic surgery, as it is reliable, minimizes trauma and suffering
and allows for a shorter recovery time (6,7). The
combination of VATS and conventional thoracotomy may be used to
complete the removal of lesions at an earlier stage and, thus, has
become the standard method for lymph node dissection. In 2002, the
Shandong Provincial Hospital Affiliated to Shandong University,
developed a novel technique, namely hand video-assisted
thoracoscopic surgery (HVATS), involving a surgeon operating by
hand through an abdominal incision into the chest with the
assistance of thoracoscopy. This method successfully combined
minimally invasive and conventional surgery (8,9).
The main objective of this study was to assess the
effect of HVATS and Ivor-Lewis surgery (ILS) on short-term
health-related quality of life (HRQL) of patients with esophageal
cancer using the quality of life questionnaires (QLQ)-C30 and
QLQ-OES18, published by the European Organization for Research and
Treatment of Cancer (EORTC), in order to determine the application
perspective of HVATS in the treatment of esophageal cancer.
Materials and methods
Patients
A total of 62 patients with pathologically
confirmed, newly diagnosed middle esophageal cancer, who underwent
surgery at the Shandong Provincial Hospital Affiliated to Shandong
University between January, 2005 and June, 2007, were enrolled in
this study. The eligibility criteria included Karnofsky performance
score ≥70, age 18–75 years, no adjuvant therapy, no distant
metastases, survival for >3 months after surgery, follow-up of
≥5 years after surgery and no causes of death other than esophageal
cancer.
This study was approved by the Ethics Committee of
the Shandong Provincial Hospital Affiliated to Shandong University
and written informed consent was obtained from all the
participating subjects.
Surgical techniques
HVATS
A total of 33 patients underwent HVATS under general
anesthesia, positioned on the right side of the body and rotated
45°. The key steps of HVATS included i) exploration and
mobilization of the stomach through an upper median abdominal
incision; ii) mobilizing the esophageal tumor extraperitoneally
using the left hand of the operator from the right side of the
abdominal incision under the costal arch; iii) mobilizing the
esophagus from the top of chest in the rear to the arch of the
azygos vein and drawing it from the left neck incision; iv)
performing lymph node dissection; and v) pulling the stomach into
the chest through the diaphragmatic hiatus and anastomosing with
the esophagus end-to-side under surveillance through the neck
incision.
ILS
A total of 29 patients underwent ILS under general
anesthesia, positioned on the right side of the body and rotated
45°. The key steps of ILS included i) exploring and mobilizing the
esophagus through a chest incision at the right 4th intercostal
space; ii) mobilizing the stomach through an upper median abdominal
incision; iii) performing lymph node dissection; and iv)
anastomosing with the esophagus end-to-side at the neck or right
thoracic cupola.
Quality of life evaluation
All the patients completed the QLQ-C30 and QLQ-OES18
published by EORTC. EORTC QLQ-C30 (version 3.0) is a
self-assessment questionnaire describing 5 functional indices,
including physical, role, cognitive, emotional and social
functions, 3 symptom indices, including fatigue, pain and nausea or
vomiting and 1 general score. EORTC QLQ-OES18 includes 18 indices,
namely specific symptoms, such as dysphagia, esophageal reflux and
bucking. EORTC QLQ-C30 was believed to be of superior validity and
reliability, as assessed by Hjermstad (10) in 190 untreated patients. The
combination of QLQ-C30 and QLQ-OES18 is considered to precisely
reflect the changes in the quality of life of esophageal cancer
patients and is recommended by EORTC to evaluate the quality of
life of such patients.
Survey methods
An examination was conducted 1 week prior to surgery
and at 2, 4, 12 and 24 weeks after surgery. All the questionnaires
were completed by the patients themselves. Higher functional and
general scores of EORTC QLQ-C30 indicate a better quality of life,
whereas higher symptom scores of EORTC QLQ-C30 and QLQ-OES18
reflect a worse quality of life.
Statistical analysis
Data are expressed as means ± standard deviation and
were compared by the Chi-square test. The statistical significance
of the differences in the questionnaire scores between the two
groups was determined by the Student's t-test. The logistic
regression model was used to assess the associations between
preoperative clinical characteristics and HRQL scores at 6 months
after surgery. The Chi-square test was used to evaluate the
correlation between the selection of surgical technique and
clinicopathological characteristics. The Kaplan-Meier survival
curve was applied to assess the 5-year survival rate and the
log-rank test was used to evaluate the differences in survival
distributions. P<0.05 was considered to indicate a statistically
significant difference.
Results
Clinical characteristics
The patient characteristics, grouped by surgical
procedures, are shown in Table I.
The Chi-square test revealed no significant differences in gender,
age, body mass index (BMI), substitute, TNM stage and complications
among the 62 patients. However, anastomosis location was
significantly different between patients in the HVATS and ILS
groups.
 | Table IClinical characteristics of patients
with esophageal cancer. |
Table I
Clinical characteristics of patients
with esophageal cancer.
| Total no. of patients
(n=62) | | |
|---|
|
| | |
|---|
| Characteristics | HVATS (n=33) | Ivor-Lewis
(n=29) | Chi-square | P-value |
|---|
| Gender | | | 0.111 | 0.739 |
| Male | 25 | 23 | | |
|
Female | 8 | 6 | | |
| Age, years | | | 0.295 | 0.587 |
|
<60 | 10 | 7 | | |
| ≥60 | 23 | 22 | | |
| Body mass index at
surgery | | | 0.083 | 0.773 |
|
<24.9 | 17 | 16 | | |
| ≥25 | 16 | 13 | | |
| Comorbidities | | | 0.009 | 0.924 |
| No | 11 | 10 | | |
| Yes | 22 | 19 | | |
| Tumor location | | | | |
| Upper and
middle | 33 | 29 | | |
|
Lower | 0 | 0 | | |
| Histology | | | | |
|
Adenocarcinoma | 0 | 0 | | |
| Squamous
cell carcinoma | 33 | 29 | | |
| Anastomosis
location | | | 10.452 | 0.001 |
| Neck | 33 | 21 | | |
| Upper
right chest | 0 | 8 | | |
| Substitute | | | | |
|
Stomach | 33 | 29 | | |
|
Jejunum | 0 | 0 | | |
| TNM stage | | | 0.779 | 0.854 |
| 0 | 4 | 3 | | |
| I | 18 | 17 | | |
| II | 10 | 7 | | |
| III | 1 | 2 | | |
| IV | | | | |
| Complications | | | 0.827 | 0.363 |
| No | 23 | 17 | | |
| Yes | 10 | 12 | | |
Associations between clinical
characteristics and HRQL
The 62 patients were analyzed for the associations
between clinical characteristics and QLQ-C30 functional aspects of
HRQL 6 months following esophagectomy. The results revealed that
gender and BMI were not significantly associated with the
functional aspects of HRQL at 6 months after surgery, whereas the
presence of comorbidities was significantly associated with poor
physical and role function scores (Table II). In addition, patients aged
<60 years exhibited poorer emotional function compared to
patients aged >60 years and patients with advanced tumor stage
(III-IV) exhibited an increased risk of poor role function
(Table II).
 | Table IIAssociations between clinical
characteristics and quality of life questionnaire-C30 aspects of
health-related quality of life. |
Table II
Associations between clinical
characteristics and quality of life questionnaire-C30 aspects of
health-related quality of life.
| GQL | Physical
function | Role function | Emotional
function | Social function |
|---|
|
|
|
|
|
|
|---|
| Characteristics | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI |
|---|
| Gender | | | | | | | | | | |
|
Malea | 1 | | 1 | | 1 | | 1 | | 1 | |
|
Female | 1.24 | 0.54–1.97 | 1.12 | 0.53–1.74 | 0.68 | 0.41–1.29 | 0.99 | 0.57–1.79 | 0.69 | 0.36–1.68 |
| Age, years | | | | | | | | | | |
|
<60a | 1 | | 1 | | 1 | | 1 | | 1 | |
| ≥60 | 0.61 | 0.38–1.23 | 1.03 | 0.57–1.88 | 0.59 | 0.31–1.42 | 0.61 | 0.33–0.97 | 0.54 | 0.41–1.01 |
| BMI | | | | | | | | | | |
|
<24.9a | 1 | | 1 | | 1 | | 1 | | 1 | |
|
≥25 | 0.84 | 0.71–1.03 | 0.99 | 0.86–1.32 | 0.88 | 0.73–1.25 | 0.9 | 0.66–1.13 | 0.73 | 0.59–0.97 |
| Comorbidities | | | | | | | | | | |
| Noa | 1 | | 1 | | 1 | | 1 | | 1 | |
| Yes | 1.49 | 0.97–2.52 | 1.79 | 1.21–2.83 | 1.86 | 1.07–2.89 | 1.61 | 0.87–3.01 | 1.55 | 0.92–2.34 |
| TNM stage | | | | | | | | | | |
| 0-Ia | 1 | | 1 | | 1 | 1 | | 1 | |
| II | 1.45 | 0.88–2.71 | 1.32 | 0.68–2.70 | 1.88 | 0.96–3.73 | 1.27 | 0.61–2.08 | 1.53 | 0.69–2.66 |
| III-IV | 1.71 | 0.73–2.91 | 1.58 | 0.81–3.01 | 1.98 | 1.17–3.92 | 1.54 | 0.69–2.68 | 1.34 | 0.58–2.36 |
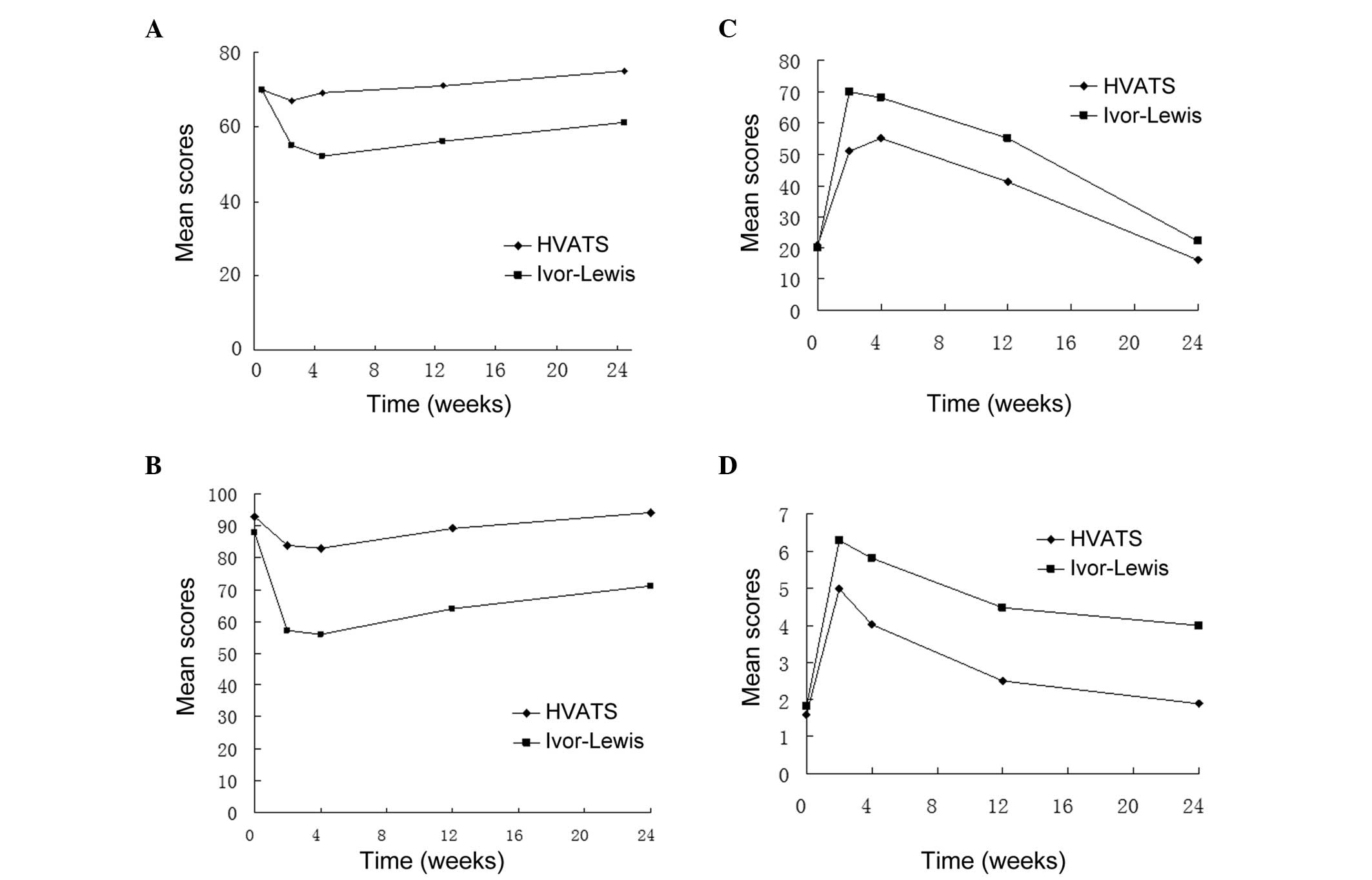
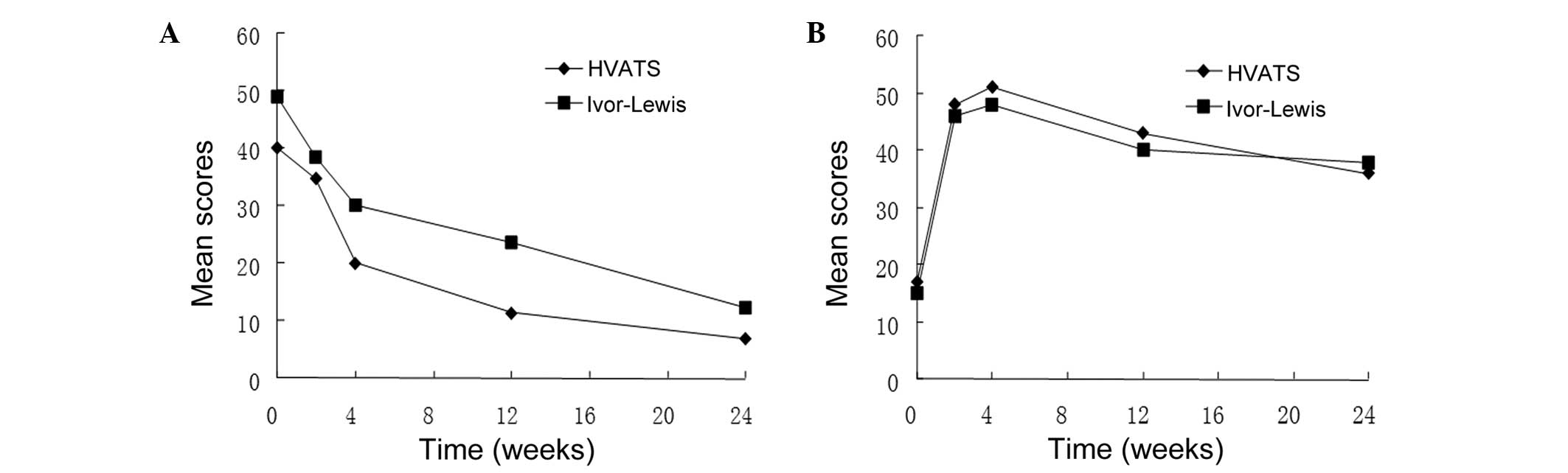
Quality of life
A total of 282 questionnaires were qualified
(282/296). According to the EORTC QLQ-C30, the general, physical,
fatigue and pain scores were significantly different between the
HVATS and ILS groups. However, the remaining scores of EORTC
QLQ-C30 and all the scores of EORTC QLQ-OES18 were not
significantly different between the two groups. The changes in all
the mean scores are presented in Figs.
1 and 2.
The portrait of the changes of EORTC QLQ-C30
revealed that the preoperative symptom and functional scores were
similar between the two groups. However, compared to the
preoperative scores, the functional scores at 2 weeks
postoperatively, such as general and physical scores, were
decreased, while the symptom scores, such as pain and fatigue
scores, were significantly increased, particularly in the ILS group
(Fig. 1). In addition, the
functional scores of the patients in the HVATS group had partially
recovered at 3 months and had reached preoperative level at 6
months. Although the functional scores of patients in the ILS group
gradually increased during the first 3 months postoperatively, they
remained significantly lower compared to the preoperative levels at
6 months (Fig. 1). The changes in
the EORTC QLQ-OES18 scores demonstrated that the postoperative
dysphagia scores of the patients in both groups were significantly
lower compared to their preoperative scores, reflecting the success
of the surgical intervention. However, the scores of dysphagia,
esophageal reflux and other specific symptoms of the two groups
were not significantly different prior to and after surgery
(P>0.05) (Fig. 2).
Furthermore, the general quality of life scores of
the patients in the HVATS group were significantly higher compared
to those of the patients in the ILS group at all the monitoring
points (P<0.05).
Discussion
There are several surgical techniques applied to the
treatment of esophageal cancer, although their survival rates are
not significantly different. The quality of life as 1 of the 3
endpoints for cancer therapy evaluation has attracted extensive
attention over the last few years. Blazeby et al (11) evaluated the quality of life of
esophageal cancer patients who received surgery or palliative
treatment using EORTC QLQ-C30 and observed that the quality of life
of the former was significantly higher compared to that of the
latter, suggesting that surgical treatment may be a preferred
choice for patients with esophageal cancer. Studies on the effect
of VATS on the quality of life are currently more focused on
patients with lung cancer (12,13).
To the best of our knowledge, this is the first study on the effect
of VATS on the quality of life of patients with esophageal
cancer.
HVATS improved the general short-term quality of
life. This study demonstrated that the general quality of life
scores of patients in the two groups were significantly higher in
the HVATS group compared to those in the ILS group at all the
monitoring points. This may be mainly attributed to the fact that
HVATS minimizes the injury to the chest wall, preserves lung
function and relieves postoperative pain; therefore, patients may
find it easier to exercise and cough following surgery compared to
ILS. Thus, HVATS may be conducive to recovery and improved overall
quality of life.
HVATS may reduce postoperative fatigue and
restrictions to physical functionality. A high proportion of
patients exhibited fatigue and decreased locomotor activity in the
two groups at all the monitoring time points. During the first 3
months, the patients in the HVATS group had higher physical and
lower fatigue scores compared to those of patients in the ILS
(P<0.05), possibly due to the fact that HVATS was associated
with less extensive injury to the chest wall and was conducive to
the recovery of physical functions.
Pain is one of the major causes of discomfort, which
may compromise rest, breathing and coughing and may also cause
pneumonia, atelectasis and other complications. This study
demonstrated that, at all the monitoring points, the patients in
the HVATS group had lower pain scores compared to patients in the
ILS group, indicating that HVATS was associated with significantly
less pain (P<0.05). HVATS, which only requires a small incision
and does not require cutting through the latissimus dorsi and
anterior serratus muscles or a rib retractor, may help avoid
injuries to the ribs, intercostal nerves and vertebral joints,
thereby minimizing postoperative pain. It was previously
demonstrated that thoracoscopic surgery reduces postoperative pain
and the amount of postoperative analgesics administered (14).
Although HVATS is associated with certain advantages
regarding the functional scores mentioned above, the EORTC
QLQ-OES18 symptomatic scores, such as dysphagia, gastroesophageal
reflux and diarrhea, were not significantly different between
patients in the HVATS and ILS groups (P>0.05).
In conclusion, HVATS for esophageal cancer patients
significantly improved the short-term quality of life compared to
ILS. However, due to the limited case number, the data may be
flawed and the conclusions may come with certain limitations. In
addition, the effect of HVATS on long-term quality of life has not
been clearly determined. Thus, further prospective studies,
including larger patient samples, are required to verify our
findings.
Acknowledgements
All the authors listed have approved the manuscript.
All the procedures were conducted in accordance with the ethical
standards of the Committee on Human Experimentation of Shandong
University. This study was supported by the Science and Technology
Foundation of Shandong Province (grant no. 2013GSF11845) and the
Science and Technology Project of Jinan (grant no. 201202023).
References
|
1
|
Jemal A, Siegel R, Ward E, Hao Y, Xu J,
Murray T and Thun MJ: Cancer statistics, 2008. CA Cancer J Clin.
58:71–96. 2008. View Article : Google Scholar
|
|
2
|
Gallo A and Cha C: Updates on esophageal
and gastric cancers. World J Gastroenterol. 12:3237–3242.
2006.PubMed/NCBI
|
|
3
|
Enzinger PC and Mayer RJ: Esophageal
cancer. N Engl J Med. 349:2241–2252. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Fabian T, Martin JT, McKelvey AA and
Federico JA: Minimally invasive esophagectomy: a teaching
hospital's first year experience. Dis Esophagus. 21:220–225.
2008.
|
|
5
|
Shichinohe T, Hirano S and Kondo S:
Video-assisted esophagectomy for esophageal cancer. Surg Today.
38:206–213. 2008. View Article : Google Scholar
|
|
6
|
Sunpaweravong S, Chewatanakornkul S and
Ruangsin S: Initial experience and result of thoracoscopic and
laparoscopic esophagectomy. J Med Assoc Thai. 91:1202–1205.
2008.PubMed/NCBI
|
|
7
|
Toker A, Eroglu O, Ziyade S, Tanju S,
Senturk M, Dilege S and Kalayci G: Comparison of early
postoperative results of thymectomy: partial sternotomy vs.
videothoracoscopy. Thorac Cardiovasc Surg. 53:110–113. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Du JJ, Meng L, Chen JH, Peng ZM, Wang L,
Zhang L and Wang XH: Hand-assisted video-thoracoscopy for resecion
of esophageal cancer. Chin J Surg. 43:351–353. 2005.(In
Chinese).
|
|
9
|
Du JJ, Meng L, Chen JH, Peng ZM, Wang L,
Zhang L and Wang XH: Clinical therapeutic effect of esophageal
carcinoma with hand video assisted surgery. Chin J Surg.
45:822–824. 2007.(In Chinese).
|
|
10
|
Hjermstad MJI, Fossa SD, Bjordal K and
Kaasa S: Test/retest study of the European Organization for
Research and Treatment of Cancer Core Quality-of-Life
Questionnaire. J Clin Oncol. 13:1249–1254. 1995.PubMed/NCBI
|
|
11
|
Blazeby JM, Williams MH, Brookes ST, et
al: Quality of life measurement in patients with oesophageal
cancer. Gut. 37:505–508. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Nakata M, Saeki H, Yokoyama N, et al:
Pulmonary function after lobectomy: video-assisted thoracic surgery
versus thoracotomy. Ann Torac Surg. 70:938–941. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Walker WS, Codispoti M, Soon SY, et al:
Long-term outcomes following VATS lobectomy for non-small cell
bronchogenic carcinoma. Eur J Cardiothorac Surg. 23:397–402. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Paiva JM and Wright GM: Hand-assisted
thoracoscopic surgery causes less postoperative pain than limited
thoracotomy after cessation of epidural analgesia. Heart Lung Circ.
13:374–378. 2004. View Article : Google Scholar
|