Introduction
Head and neck squamous cell carcinoma (HNSCC) is the
sixth most common type of cancer worldwide (1), with an increasing trend in incidence. In
2014, 12,000 mortalities were expected to occur from head and neck
cancer (2). Several factors affect
survival and locoregional tumor control in patients with HNSCC
(3–6).
In order to better define the risks, analyses of prognostic factors
and outcomes have been performed in a number of trials.
Systemic inflammation and immunity have recently
been investigated in the context of HNSCC. The inflammatory
response is crucial for the development and progression of this
type of cancer. The neutrophil to lymphocyte ratio (NLR) is a
marker reflecting systemic inflammation and it may be easily
calculated from the white blood cell counts. NLR was reported to be
an independent prognostic factor for patients with various types of
cancer. An increase in NLR has been shown to be associated with
adverse overall survival (OS) in several solid tumors (3); a high NLR was associated with adverse
outcomes of nasopharyngeal carcinoma, castration-resistant
metastatic prostate carcinoma, breast cancer, non-small-cell lung
cancer (NSCLC), local and advanced esophageal squamous carcinoma
and renal cell carcinoma (7–14).
In the present study, we aimed to determine whether
NLR is a prognostic factor for the survival of patients with
recurrent or metastatic HNSCC.
Patients and methods
Patient characteristics
The clinicopathological characteristics and outcome
data of 79 patients with recurrent or metastatic HNSCC were
collected and retrospectively reviewed using the Akdeniz University
database between 2003 and 2013. Age, gender, Eastern Cooperative
Oncology Group performance status (ECOG PS), primary tumor site,
stage, curative treatment protocol performed for local disease at
diagnosis, induction chemotherapy, type of chemotherapy in the
first-line setting and metastatic site at recurrence were imported
into the Statistical Package for the Social Sciences software,
version 16.0 (SPSS 16.0; SPSS, Inc., Chicago, IL, USA). Staging was
performed according to the American Joint Committee on Cancer
(AJCC) staging manual (15).
NLR
The neutrophil and lymphocyte counts at diagnosis of
metastatic disease and at recurrence for local or locally advanced
disease were recorded into SPSS 16.0. NLR was calculated as the
ratio of absolute neutrophil count to absolute lymphocyte count in
blood samples.
Survival
The date of diagnosis for patients with metastatic
HNSCC or the date of recurrence for patients with recurrent HNSCC,
time to progression and date of death of patients with recurrent
and metastatic HNSCC were imported into the SPSS 16.0 statistical
program. Progression-free survival (PFS) was defined as the time
from treatment initiation to first evidence of disease progression.
OS was defined as the time from treatment initiation to death from
any cause.
Statistical analysis
Statistical analyses were performed using SPSS 16.0.
To determine the characteristics of the patients, a frequency
analysis was performed. The optimum cut-off value of NLR at
recurrence or diagnosis was identified according to the receiver
operating characteristic (ROC) curve and all 79 patients were
divided into two groups based on the NLR value. According to the
cut-off value of 2.93, the effect of NLR on the PFS and OS of
patients with metastatic or recurrent HNSCC was calculated by the
log-rank test. Kaplan-Meier survival probability estimates were
also calculated. A P-value of <0.05 was considered to indicate a
statistically significant difference. The prognostic effect of NLR
on survival (PFS and OS) in patients with recurrent or metastatic
HNSCC was assessed by univariate and multivariate analyses.
Results
Patient characteristics
The characteristics of the two groups are summarized
in Table I. The median age of the
patients was 59 years (range, 28–85 years) and the majority of the
patients were male (89.9%). In terms of ECOG PS, 43% of the
patients had a PS of 0, 32.9% had 1, 22.8% had 2 and 1.3% had 3.
The most common primary tumor localization was the larynx. A total
of 59 (74.6%) patients had stage 4 disease, whereas 25.3% had local
or locally advanced (stage I-II or III) disease. The most commonly
used local treatment modality was surgery plus radiotherapy
(39.2%). In 16.5% of the patients, induction chemotherapy was
performed. The most commonly used chemotherapeutic regimen (64.6%)
in the first-line setting was docetaxel 75 mg/m2 on day
1, with cisplatin 75 mg/m2 on day 1 and 5-fluorouracil
1,000 mg/m2 on days 1–5. Local or nodal recurrence was
the most common recurrence site in patients with recurrent
HNSCC.
 | Table I.Characteristics of the study patients
(n=79). |
Table I.
Characteristics of the study patients
(n=79).
| Characteristics | Patient no. (%)
(n=79) |
|---|
| Age, years [median
(range)] | 59 (28–85) |
| Gender |
|
|
Female | 8 (10.1) |
| Male | 71 (89.9) |
| ECOG PS |
|
| 0 | 34 (43.0) |
| 1 | 26 (32.9) |
| 2 | 18 (22.8) |
| 3 | 1 (1.3) |
| Primary tumor
localization |
|
|
Larynx | 46 (58.3) |
|
Hypopharynx | 4 (5.1) |
| Base of
tongue | 9 (11.4) |
|
Tonsils | 5 (6.3) |
| Paranasal
or maxillary sinuses | 5 (6.3) |
| Oral
cavity | 2 (2.5) |
|
Other | 8 (10.1) |
| TNM stage at
diagnosis |
|
| 1 | 1 (1.3) |
| 2 | 3 (3.8) |
| 3 | 16 (20.2) |
| 4 | 59 (74.7) |
| Local treatment
modality |
|
| None | 13 (16.5) |
|
Radiotherapy | 25 (31.6) |
|
Surgery | 10 (12.7) |
| Surgery +
radiotherapy | 31 (39.2) |
| Prior induction
chemotherapy |
|
| Yes | 13 (16.5) |
| No | 66 (83.5) |
| Type of
chemotherapy |
|
|
TCFa | 51 (64.6) |
|
CFb + cetuximab | 19 (24.0) |
|
Other | 9 (11.4) |
| Recurrence site |
|
| Local or
nodal | 35 (44.3) |
| Lung | 32 (40.5) |
| Viscera
other than lung | 12 (15.2) |
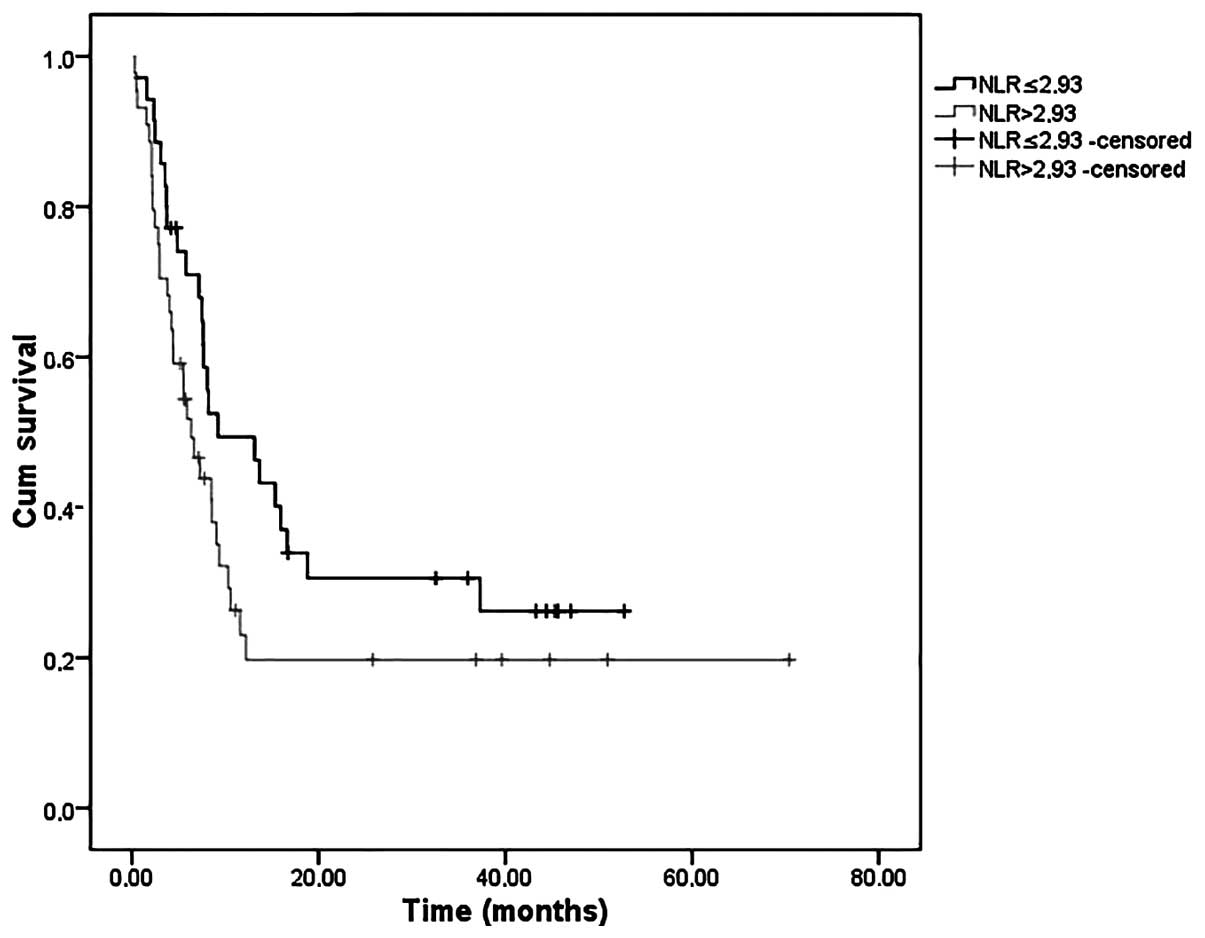
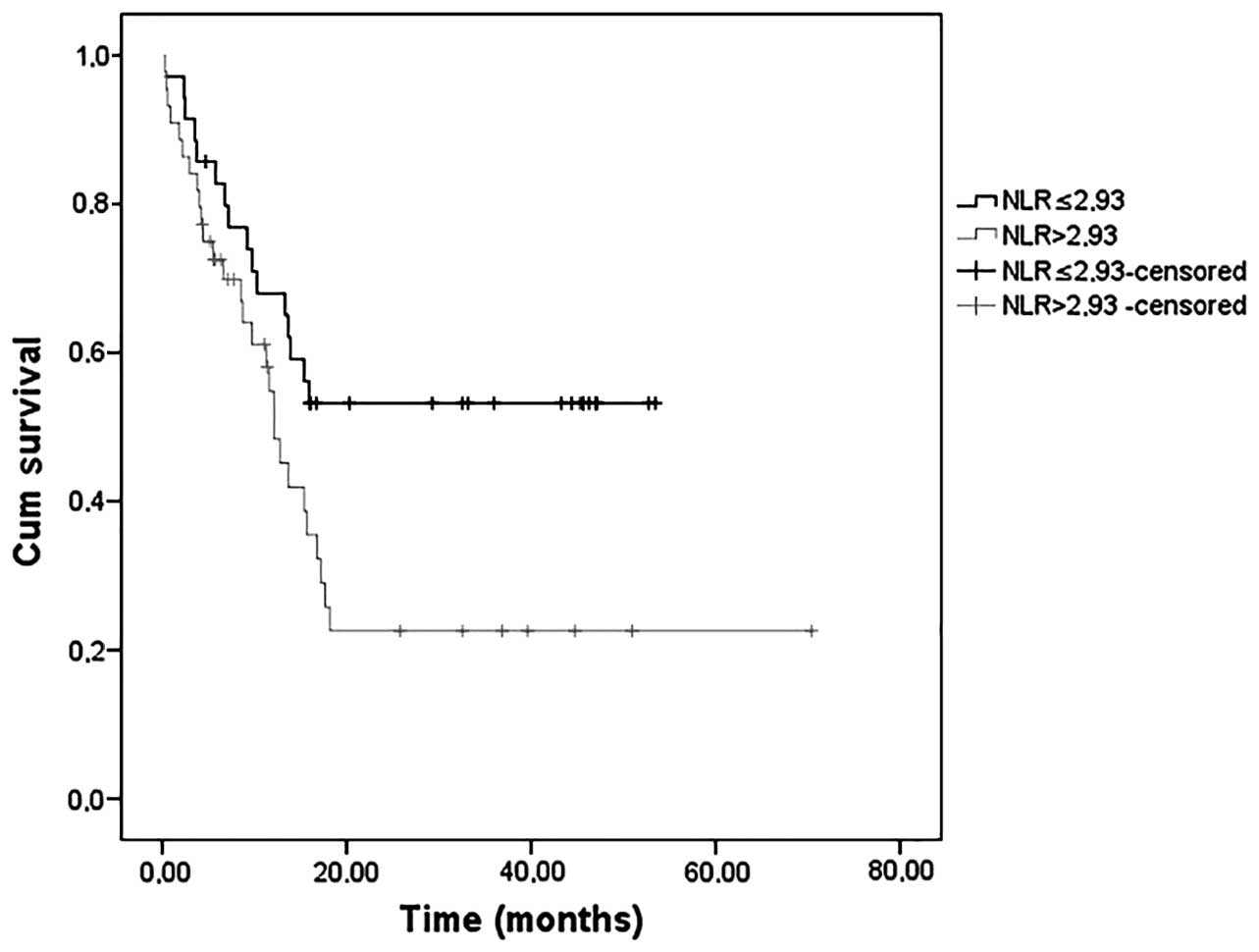
OS and PFS by NLR
Following ROC curve analysis, the optimum cut-off
value of NLR was set at 2.93. The patients were divided into two
groups, those with NLR >2.93 (n=44) and those with NLR ≤2.93
(n=35). When the groups were evaluated in terms of PFS, there was
no significant difference between the groups (P=0.109). However,
the median OS was significantly higher in patients with NLR ≤2.93
(P=0.027). The median PFS and OS values are presented in Table II. PFS and OS curves are shown in
Figs. 1 and 2, respectively.
 | Table II.Survival analysis. |
Table II.
Survival analysis.
| Median survival
(months) | NLR >2.93
(n=44) | NLR ≤2.93 (n=35) | P-value |
|---|
| PFS | 6.34 (95% CI
3.55–9.12) | 9.19 (95% CI
1.53–16.8) | 0.109 |
| OS | 12.1 (95% CI
9.75–14.4) | NR | 0.027 |
Survival analysis
Age, gender, primary tumor site, prior curative
treatment protocol, prior induction chemotherapy, type of
chemotherapy in the first-line setting, metastatic site at
recurrence and NLR were evaluated in a univariate analysis
regarding their effect on PFS and OS. As regards PFS, recurrence or
metastatic site and prior induction chemotherapy were included in
the multivariate analysis. Following Cox's regression analysis,
only recurrence or metastatic site were identified as an
independent factor affecting PFS (P=0.001) (data not shown).
Following univariate analysis for OS, ECOG PS,
recurrence or metastatic site, prior induction chemotherapy and NLR
were included in the multivariate analysis (P=0.138, P=0.004,
P=0.128 and P=0.061, respectively) (data not shown). Following
Cox's regression analysis, only NLR and recurrence or metastatic
site were found to be independent significant prognostic factors
affecting OS (P=0.014 and P=0.002, respectively) (data not
shown).
Discussion
In the present study, we investigated the prognostic
effect of NLR on OS and PFS in recurrent or metastatic HNSCC. Our
results revealed that NLR is an independent significant prognostic
factor for OS (P=0.002) in patients with recurrent or metastatic
HNSCC.
Cancer-related inflammation has been shown to
negatively affect cancer prognosis. Neutrophilia may be a marker of
inflammation-related aggressive biological behaviour of the tumor
(18). Absolute neutrophil and
lymphocyte counts may be affected by various physiological,
pathological and physical factors, although NLR may remain stable
with respect to these factors. Therefore, NLR may be prognostically
superior to leukocyte subtype and high NLR values resulting from
inflammation are considered to be associated with poor prognosis
(16). The exact association of high
NLR and poor outcome in cancer patients has not been fully
elucidated. Neutrophilia may inhibit the immune system by
suppressing lymphocytes, activated T cells and natural killer cells
(3,17). The prognostic role of the NLR has been
evaluated in >60 studies on a number of solid tumors (7–14,16,18).
In a systemic review analyzing cancer-specific
survival, a high NLR was found to be associated with worse OS
(3). A retrospective review of
patients with esophageal squamous cell carcinoma demonstrated that
a preoperative NLR of ≥2.5 may be predictive of poor prognosis
following radical resection. In the same study, NLR was found to be
an independent prognostic risk factor (12). In another retrospective study, NLR was
suggested to be a predictor of chemosensitivity in advanced
esophageal cancer patients receiving neoadjuvant chemotherapy
(10). Wang et al (11) demonstrated that elevated NLR at
recurrence of NSCLC indicates poor prognosis and suggested it may
be a significant independent prognostic factor in patients with
recurrent NSCLC following curative resection. Nakano et al
(9) investigated the association
between NLR and survival outcome in preoperative local and locally
advanced breast cancer and concluded that it may be an independent
prognostic factor for disease-free survival and breast
cancer-specific survival in patients with breast cancer. It has
also been demonstrated that increased pretreatment NLR is an
independent prognostic factor in patients with metastatic renal
cell carcinoma who received tyrosine kinase inhibitors (14).
When evaluating the association between NLR and
HNSCC, it was previously demonstrated that high pretreatment
peripheral NLR was significantly associated with poor PFS among
patients with advanced clinical stage (III and IV) nasopharyngeal
carcinoma (7). However, there was no
significant association between NLR and PFS in the present study.
Apart from the limited number of studies on nasopharyngeal
carcinoma, there are no studies in the literature demonstrating the
prognostic significance of NLR in head and neck carcinomas, mainly
laryngeal carcinoma. In another study on oral cavity cancer
patients, it was observed that NLR increased in parallel with the
advancement of clinical stage and T stage, but it was not
significantly associated with survival (18). Furthermore, the opposite finding has
also been reported, namely better survival associated with higher
NLR in HNSCC patients, suggesting an antitumorigenic role of NLR
(19). Rassouli et al
(20) reported that NLR ≥4.2 predicts
a higher recurrence rate (P<0.0001, log-rank test) and concluded
that NLR may be used as an independent predictor of recurrence and
survival. A retrospective study on pretreatment NLR and
disease-spesific survival in patients with oral cancer undergoing
preoperative chemoradiotherapy indicated that NLR is a significant
independent predictor of poor cancer-specific survival (21). In accordance with the literature
regarding cancer types other than HNSCC, our results also
identified NLR as an independent prognostic factor in patients with
recurrent or metastatic HNSCC.
NLR derived from a single blood sample at initial
diagnosis of metastatic disease or at recurrence may be a useful
laboratory marker for recurrent or metastatic HNSCC. This simple,
cost-effective, non-invasive and rapidly available test may be
easily used in clinical practice.
Combined with other markers, NLR may be used in
decision-making and the selection of treatment modality in patients
with recurrent or metastatic HNSCC. Although the present study was
a retrospective, single-center study, it indicates the potential
benefit of a novel prognostic marker in HNSCC. However, our
findings require confirmation by larger, prospective, randomized
studies.
References
|
1
|
Hunter KD, Parkinson EK and Harrison PR:
Profiling early head and neck cancer. Nat Rev Cancer. 5:127–135.
2005. View
Article : Google Scholar : PubMed/NCBI
|
|
2
|
Siegel R, Ma J, Zou Z and Jemal A: Cancer
statistics, 2014. CA Cancer J Clin. 64:9–29. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Templeton AJ, McNamara MG, Šeruga B, et
al: Prognostic role of neutrophil-to-lymphocyte ratio in solid
tumors: a systematic review and meta-analysis. J Natl Cancer Inst.
106:dju1242014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Huang AT, Tang C, Bell D, et al:
Prognostic factors in adenocarcinoma of salivary glands. Oral
Oncol: Apr. 2:2015.(Epub ahead of print).
|
|
5
|
Iyer NG, Dogan S, Palmer F, et al:
Detailed analysis of clinicopathologic factors demonstrate distinct
difference in outcome and prognostic factors between surgically
treated HPV-positive and negative oropharyngeal cancer. Ann Surg
Oncol. Mar 24–2015.(Epub ahead of print).
|
|
6
|
Krestevska V, Stojkovski I,
Zafirova-Ivanovska B and Crvenkova S: Prognostic factors in
patients with advanced hypopharyngeal squamous cell carcinoma
treated with concurrent chemoradiotherapy. J BUON. 17:327–336.
2012.PubMed/NCBI
|
|
7
|
He JR, Shen GP, Ren ZF, et al:
Pretreatment levels of peripheral neutrophils and lymphocytes as
independent prognostic factors in patients with nasopharyngeal
carcinoma. Head Neck. 34:1769–1776. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Templeton AJ, Pezaro C, Omlin A, et al:
Simple prognostic score for metastatic castration-resistant
prostate cancer with incorporation of neutrophil-to-lymphocyte
ratio. Cancer. July 3–2014.(Epub ahead of print).
|
|
9
|
Nakano K, Hosoda M, Yamamoto M and
Yamashita H: Prognostic significance of pre-treatment
neutrophil:lymphocyte ratio in Japanese patients with breast
cancer. Anticancer Res. 34:3819–3824. 2014.PubMed/NCBI
|
|
10
|
Sato H, Tsubosa Y and Kawano T:
Correlation between the pretherapeutic neutrophil to lymphocyte
ratio and the pathologic response to neoadjuvant chemotherapy in
patients with advanced esophageal cancer. World J Surg. 36:617–622.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wang X and Li K: Neutrophil-to-lymphocyte
ratio predicts the survival in patients with post-operative
recurrence of non-small cell lung cancer. Chin J Oncol. 36:298–302.
2014.(In Chinese).
|
|
12
|
Chen H and He J: Preoperative
neutrophil-to-lymphocyte ratio as a prognostic predictor after
radical resection of esophageal squamous cell carcinoma. Chin J
Oncol. 36:294–297. 2014.(In Chinese).
|
|
13
|
Yoo EJ, Park JC, Kim EH, et al: Prognostic
value of neutrophil-to-lymphocyte ratio in patients treated with
concurrent chemoradiotherapy for locally advanced oesophageal
cancer. Dig Liver Dis. 46:846–853. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gunduz S, Mutlu H, Uysal M, Coskun HS and
Bozcuk H: Prognostic value of hematologic parameters in patients
with metastatic renal cell carcinoma using tyrosine kinase
inhibitors. Asian Pac J Cancer Prev. 15:3801–3804. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Edge S, Byrd DR, Compton CC, et al: AJCC
Cancer Staging Manual. 7th. Springer; New York, NY: pp. 41–113.
2010
|
|
16
|
Dirican A, Kucukzeybek BB, Alacacioglu A,
et al: Do the derived neutrophil to lymphocyte ratio and the
neutrophil to lymphocyte ratio predict prognosis in breast cancer?
Int J Clin Oncol. February 18–2014.(Epub ahead of print).
|
|
17
|
el-Hag A and Clark RA: Immunosuppression
by activated human neutrophils. Dependence on the myeloperoxidase
system. J Immunol. 139:2406–2413. 1987.PubMed/NCBI
|
|
18
|
Tsai YD, Wang CP, Chen CY, et al:
Pretreatment circulating monocyte count associated with poor
prognosis in patients with oral cavity cancer. Head Neck.
36:947–953. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Millrud CR, Månsson Kvarnhammar A, Uddman
R, Björnsson S, Riesbeck K and Cardell LO: The activation pattern
of blood leukocytes in head and neck squamous cell carcinoma is
correlated to survival. PLoS One. 7:e511202012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Rassouli A, Saliba J, Castano R, Hier M
and Zeitouni AG: Systemic inflammatory markers as independent
prognosticators of head and neck squamous cell carcinoma. Head
Neck. December 13–2013.(Epub ahead of print).
|
|
21
|
Perisanidis C, Kornek G, Pöschl PW,
Holzinger D, Pirklbauer K, Schopper C and Ewers R: High
neutrophil-to-lymphocyte ratio is an independent marker of poor
disease-specific survival in patients with oral cancer. Med Oncol.
30:3342013. View Article : Google Scholar : PubMed/NCBI
|