Introduction
Unclassified renal cell carcinoma (RCC) does not
belong to a specific RCC subtype with unique diagnostic
histological findings or characteristic genetic changes. The
frequency of this type of RCC is quite variable, accounting for
0.7–5.7% of all RCCs (1). Previous
reports suggested that unclassified RCC is associated with
unfavourable histological characteristics and aggressive behavior
(1,2).
Spontaneous regression of metastases of RCC is rare,
but well-documented in the course of clear cell RCC. However, there
are no reports on spontaneous regression of unclassified RCC to
date. We herein present the rare case of spontaneous regression of
pulmonary nodules in a patient with unclassified RCC following
laparoscopic partial nephrectomy.
Case report
A 56-year old woman underwent medical examination by
a physician. The patient was asymptomatic prior to hospitalization.
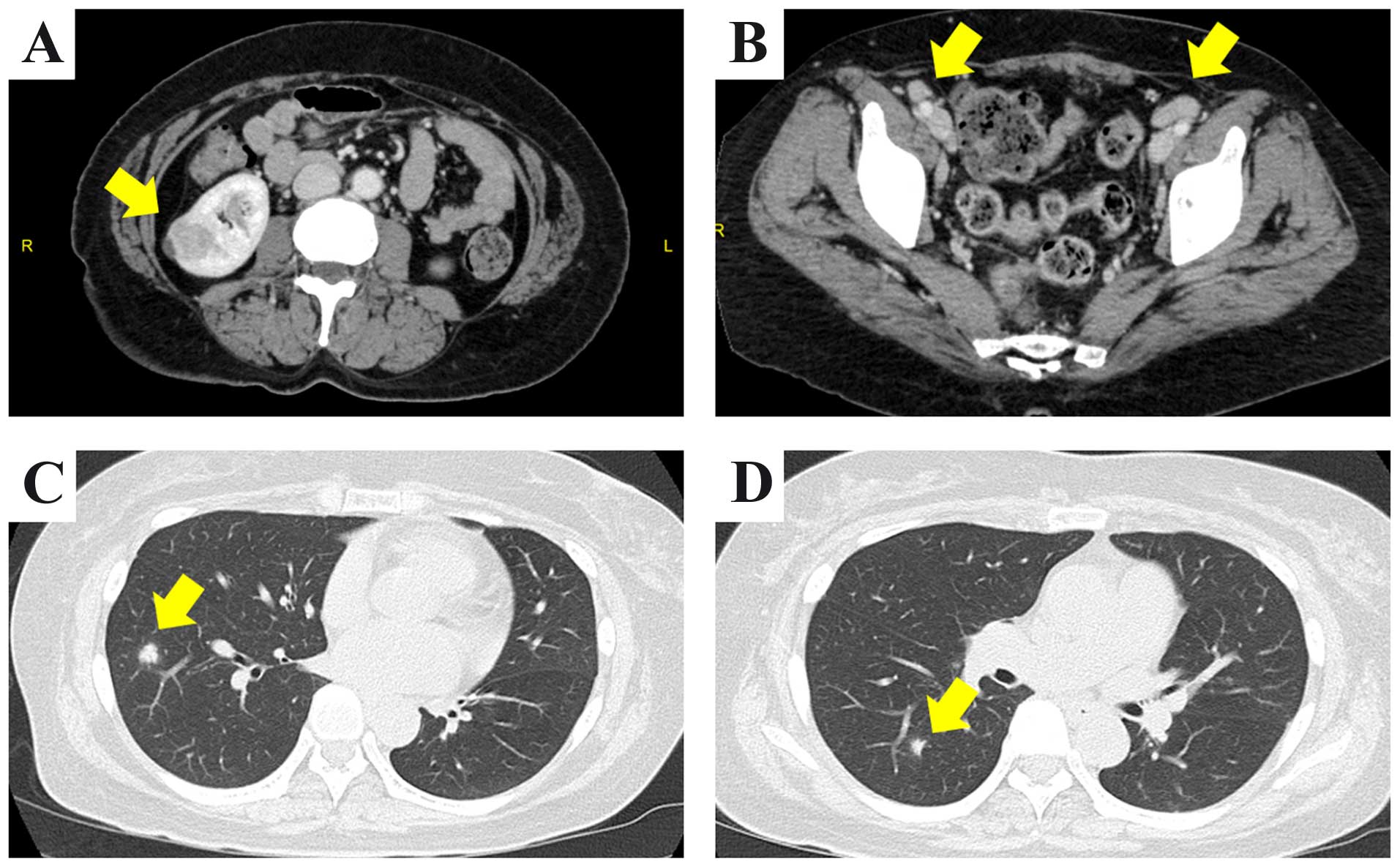
Computed tomography (CT) was performed. Abdominal CT revealed a
22-mm mass with a cystic area in the right kidney and multiple
enlarged lymph nodes in the common iliac, external iliac and groin
areas bilaterally (Fig. 1A and B).
The chest CT revealed multiple pulmonary nodules bilaterally, the
largest measuring 15 mm (Fig. 1C and
D). The laboratory tests revealed mild elevation of the
C-reactive protein levels to 1.16 mg/dl (normal range, ≤0.14
mg/dl). The levels of tumor markers, such as squamous cell
carcinoma antigen, carbohydrate antigen 19-9, carcinoembryonic
antigen (CEA), cytokeratin 19 fragment and pro-gastrin-releasing
peptide, were within the normal range. The serum concentration of
soluble interleukin-2 receptor (sIL-2R) was increased to 914 U/ml
(reference range, 122–496 U/ml). [18F]
2-fluoro-2-deoxy-d-glucose (18F-FDG) positron emission
tomography showed high FDG uptake by multiple enlarged lymph nodes,
whereas the right kidney mass and the pulmonary nodules exhibited
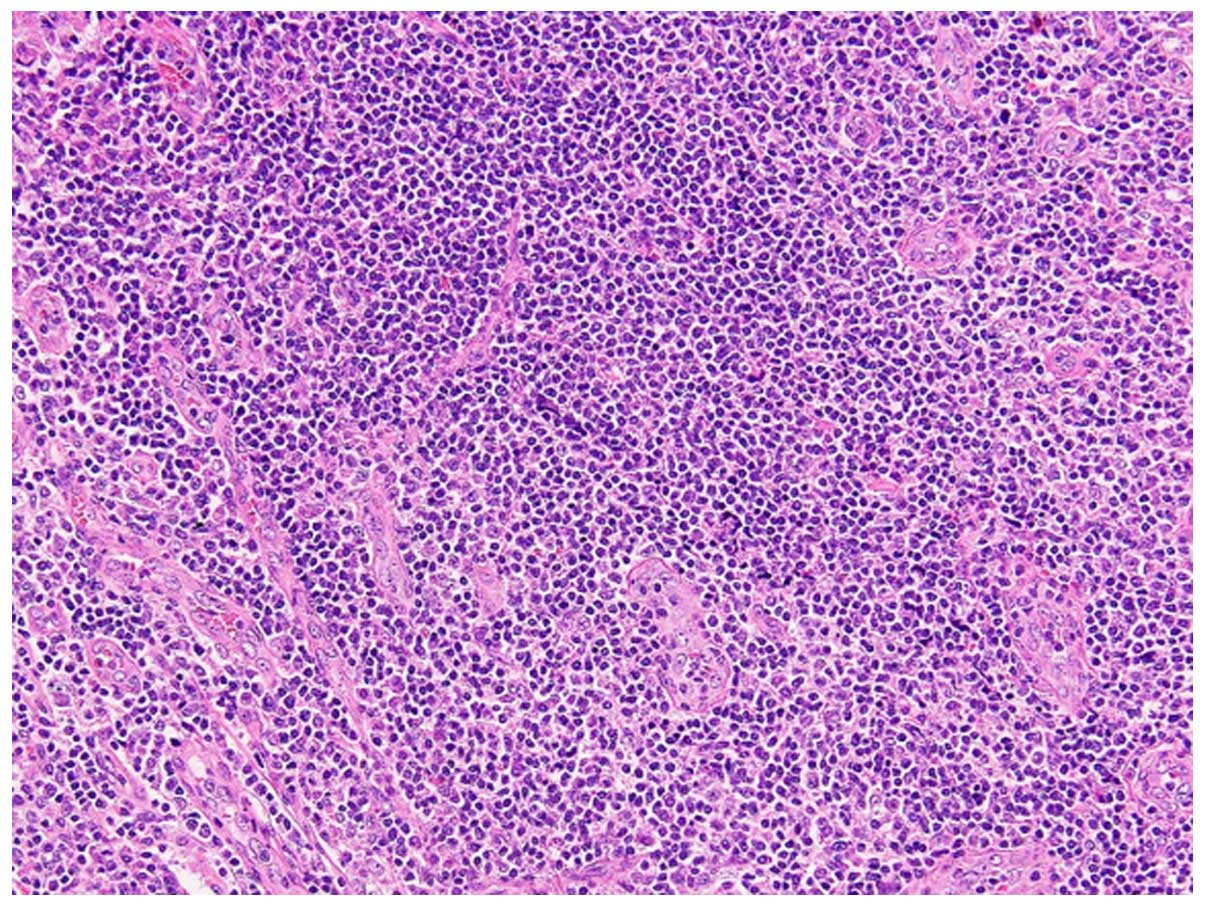
no increased uptake. A right inguinal lymph node biopsy was first
performed, since malignant lymphoma was suspected. On microscopic
examination, there were sheets of lymphoid cells and numerous
lymphoid follicles; however, there was no evidence of tumor cells
(Fig. 2) and the lymph node
enlargement was diagnosed as reactive lymphoid hyperplasia. Since
the right renal tumor was suspected to be RCC, laparoscopic partial
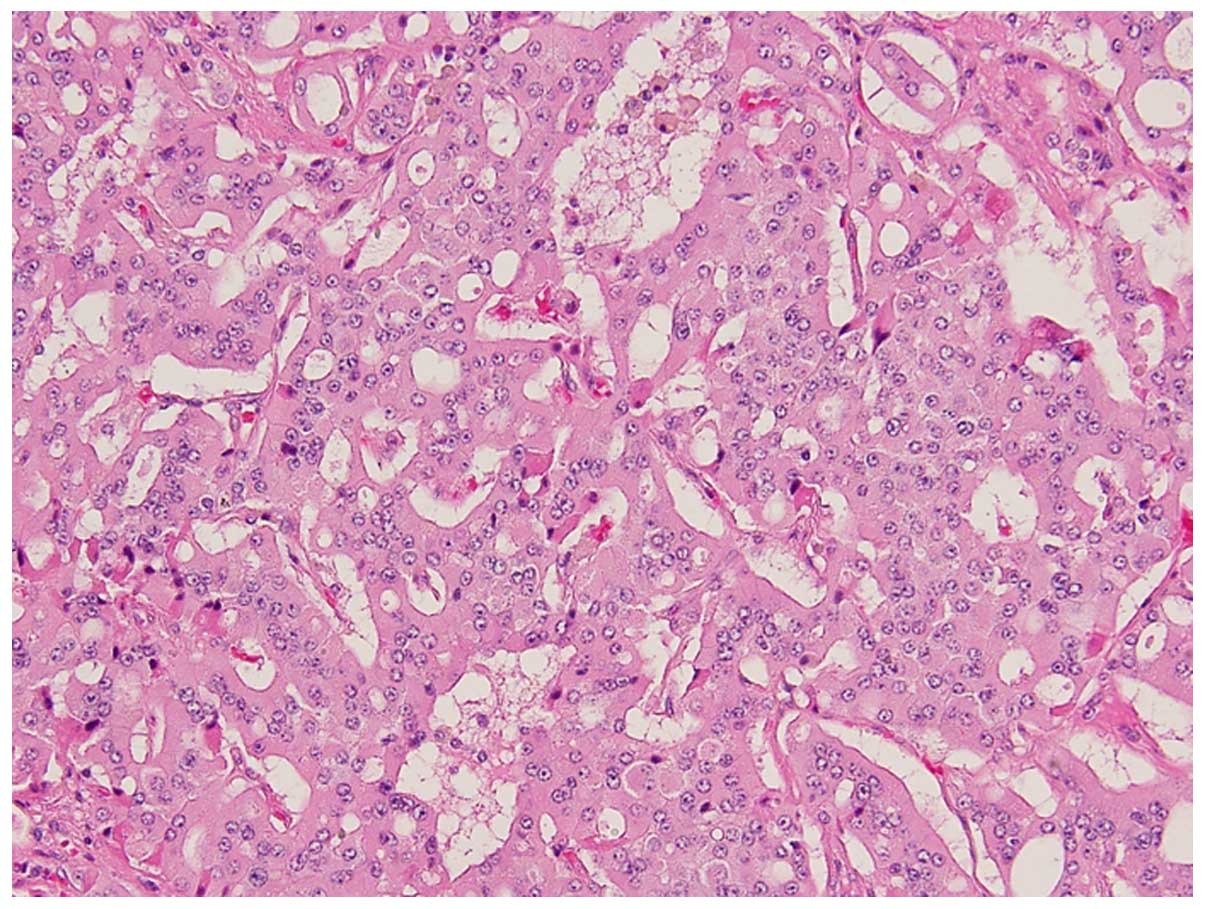
nephrectomy was performed, without any complications. The resected
tumor was sized 25 mm and was well-circumscribed; histologically,
it was composed of cells with eosinophilic cytoplasm arranged in
glandular and cribriform patterns (Figs.
3 and 4). Immunohistochemically,
almost all the tumor cells were diffusely positive for
pancytokeratin (AE1/AE3), cytokeratin 7 and E-cadherin.
Immunoreactivity for CD10, α-methylacyl-CoA racemase, 34βE12,
c-kit, anaplastic lymphoma kinase, thyroid transcription factor-1,
p63 and CEA was not detected in the tumor cells. These findings
suggested that the tumor was a RCC with distal tubular
characteristics. However, the findings were not typical. The case
was referred for expert consultation, and the final pathological
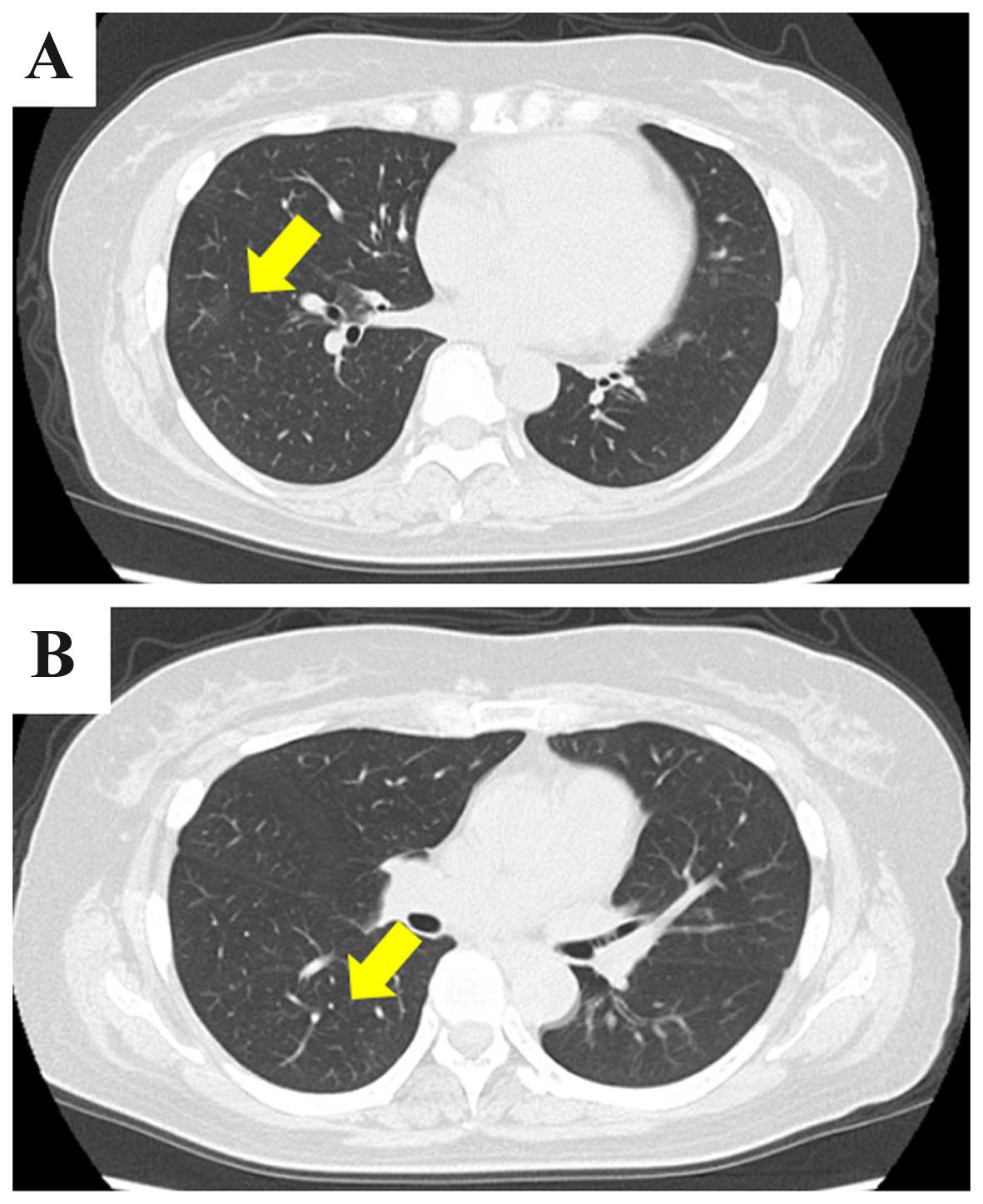
diagnosis was unclassified RCC. One month after surgery, a thoracic
CT scan revealed spontaneous regression of the pulmonary nodules
(Fig. 5). However, the enlargement of
the lymph nodes did not subside. Surveillance CT scans at 3 months
revealed no evidence of recurrence or progression of the pulmonary
nodules and lymph nodes. In addition, the level of sIL-2R had
decreased to 511 U/ml.
Discussion
RCC accounts for 3% of all cancers and its incidence
is steadily increasing. RCC is the most common among renal tumors
in adults, accounting for 85% of neoplasms arising in the kidney
(3). Approximately one-fourth of RCC
patients are known to have metastatic disease at the initial
diagnosis (4). The lungs (50%), bones
(49%), lymph nodes (6–32%), skin (11%), liver (8%) and brain (3%)
are the most frequent sites of clinical metastases (5), and these patients generally have a poor
prognosis, with a reported 5-year survival of 3–11% for unoperated
patients (6).
In the era of immunotherapy, cytoreductive
nephrectomy followed by interferon-α treatment increased overall
survival (OS) in RCC patients compared with immunotherapy alone
(7,8).
In this era of molecular-targeted therapy, it was also reported
that cytoreductive nephrectomy may provide an OS benefit in
patients with metastatic RCC (9).
Spontaneous regression of metastases in RCC is rare,
occurring in <1% of all cases (10). In 1928, Bumpus described the first
reported case of spontaneous regression of metastatic RCC (11). It was previously reported that a
number of these cases are associated with surgical removal of the
primary tumor, but regression may also occur in association to
radiation or embolization of the primary tumor (12). Different hypotheses of this rare
phenomenon have been documented. The suggested mechanism of
spontaneous regression is considered to be an immune response,
which may be evoked by surgery, tumor necrosis, infection,
radiotherapy and other treatments (13,14). In
our case, spontaneous regression of multiple pulmonary nodules was
observed following nephrectomy. Malignant lymphoma was first
suspected on preoperative assessment, due to multiple lymph node
enlargement and the increased sIL-2R level. However,
histopathological examination of a lymph node biopsy specimen
revealed reactive lymphoid hyperplasia, while the renal tumor was
diagnosed as RCC. It has been reported that pulmonary infarcts
caused by, e.g., emboli, may mimic pulmonary metastases on
radiographic scans (15,16). Several reports have also demonstrated
that IgG4-related diseases and Epstein-Barr virus-associated
lymphoproliferative diseases occasionally cause inflammatory
pseudotumors (17–19). The examinations of these diseases
revealed contradictory findings.
Previous reports demonstrated that the majority of
unclassified RCCs are aggressive, mainly because in the majority of
the cases they are at an advanced stage at presentation (1,2). Our
patient has a good clinical course, without disease recurrence or
progression. Most previous reports of spontaneous regression were
of clear cell RCC. To the best of our knowledge, this is the first
case of spontaneous regression of pulmonary nodules in a patient
with unclassified RCC following partial nephrectomy. However, the
main limitation of this study is the lack of histological
confirmation from the pulmonary nodules in our case. Adequate
histological confirmation of metastases has been estimated to be
available in only 20% of cases with spontaneous regression
(20). Although there is no evidence
of the pulmonary nodules being metastatic in our case, this
clinical phenomenon is rare in unclassified RCC. As regards disease
recurrence, long-term follow-up is required.
References
|
1
|
Lopez-Beltran A, Kirkali Z, Montironi R,
Blanca A, Algaba F, Scarpelli M, Yorukoglu K, Hartmann A and Cheng
L: Unclassified renal cell carcinoma: A report of 56 cases. BJU
Int. 110:786–793. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Karakiewicz PI, Hutterer GC, Trinh QD,
Pantuck AJ, Klatte T, Lam JS, Guille F, de La Taille A, Novara G,
Tostain J, et al: Unclassified renal cell carcinoma: An analysis of
85 cases. BJU Int. 100:802–808. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Landis SH, Murray T, Bolden S and Wingo
PA: Cancer statistics, 1999. CA Cancer J Clin. 49:8–31.1. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hock LM, Lynch J and Balaji KC: Increasing
incidence of all stages of kidney cancer in the last 2 decades in
the United States: An analysis of Surveillance, Epidemiology and
End Results program data. J Urol. 167:57–60. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Pagano S, Franzoso F and Ruggeri P: Renal
cell carcinoma metastases. Review of unusual clinical metastases,
metastatic modes and patterns and comparison between clinical and
autopsy metastatic series. Scand J Urol Nephrol. 30:165–172. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kavolius JP, Mastorakos DP, Pavlovich C,
Russo P, Burt ME and Brady MS: Resection of metastatic renal cell
carcinoma. J Clin Oncol. 16:2261–2266. 1998.PubMed/NCBI
|
|
7
|
Flanigan RC, Salmon SE, Blumenstein BA,
Bearman SI, Roy V, McGrath PC, Caton JR Jr, Munshi N and Crawford
ED: Nephrectomy followed by interferon alfa-2b compared with
interferon alfa-2b alone for metastatic renal-cell cancer. N Engl J
Med. 345:1655–1659. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Mickisch GH, Garin A, van Poppel H, de
Prijck L and Sylvester R: European Organisation for Research and
Treatment of Cancer (EORTC) Genitourinary Group: Radical
nephrectomy plus interferon-alfa-based immunotherapy compared with
interferon alfa alone in metastatic renal-cell carcinoma: A
randomised trial. Lancet. 358:966–970. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Heng DY, Wells JC, Rini BI, Beuselinck B,
Lee JL, Knox JJ, Bjarnason GA, Pal SK, Kollmannsberger CK, Yuasa T,
et al: Cytoreductive nephrectomy in patients with synchronous
metastases from renal cell carcinoma: Results from the
International Metastatic Renal Cell Carcinoma Database Consortium.
Eur Urol. 66:704–710. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
de Riese W, Goldenberg K, Allhoff E, Stief
C, Schlick R, Liedke S and Jonas U: Metastatic renal cell carcinoma
(RCC): Spontaneous regression, long-term survival and late
recurrence. Int Urol Nephrol. 23:13–25. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bumpus HC: The apparent disappearance of
pulmonary metastasis in a case of hypernephroma following
nephrectomy. J Urol. 20:181–191. 1928.
|
|
12
|
Lokich J: Spontaneous regression of
metastatic renal cancer. Case report and literature review. Am J
Clin Oncol. 20:416–418. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ishiyama H, Teh BS, Ren H, Chiang S, Tann
A, Blanco AI, Paulino AC and Amato R: Spontaneous regression of
thoracic metastases while progression of brain metastases after
stereotactic radiosurgery and stereotactic body radiotherapy for
metastatic renal cell carcinoma: Abscopal effect prevented by the
blood-brain barrier? Clin Genitourin Cancer. 10:196–198. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ricci SB and Cerchiari U: Spontaneous
regression of malignant tumors: Importance of the immune system and
other factors (Review). Oncol Lett. 1:941–945. 2010.PubMed/NCBI
|
|
15
|
Janiszewska AD, Poletajew S and
Wasiutyński A: Spontaneous regression of renal cell carcinoma.
Contemp Oncol (Pozn). 17:123–127. 2013.PubMed/NCBI
|
|
16
|
Wagner JR, Merino MJ, Pass HI, Linehan WM
and Walther MM: Pulmonary infarcts can mimic pulmonary metastases
from renal cancer. J Urol. 158:1688–1690. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Miura H and Miyachi Y: IgG4-related
retroperitoneal fibrosis and sclerosing cholangitis independent of
autoimmune pancreatitis. A recurrent case after a 5-year history of
spontaneous remission. JOP. 10:432–437. 2009.PubMed/NCBI
|
|
18
|
McCabe MG, Hook CE and Burke GA:
Spontaneous regression of an EBV-associated monoclonal large B-cell
proliferation in the mastoid of a young child following surgical
biopsy. Pediatr Blood Cancer. 51:557–559. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Park SH, Kim CG, Kim JY and Choe JY:
Spontaneous regression of EBV-associated diffuse
lymphoproliferative disease in a patient with rheumatoid arthritis
after discontinuation of etanercept treatment. Rheumatol Int.
28:475–477. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Chan BP, Booth CM, Manduch M and Touma NJ:
Spontaneous regression of metastatic pulmonary renal cell carcinoma
in the setting of sarcomatoid differentiation of the primary
tumour. Can Urol Assoc J. 7:E587–E589. 2013. View Article : Google Scholar : PubMed/NCBI
|