Introduction
Esophageal carcinoma is a life-threatening disease.
Despite adequate initial treatment, patients remain at high risk of
recurrence. Even after esophagectomy following neoadjuvant
chemoradiotherapy, ~30% of patients develop recurrent disease
(1). Recurrences predominantly occur
in the regional lymph nodes or in distant organs, including the
lung, liver, bone, brain, kidney, adrenal glands and skin (2). The liver is the most frequent site of
distant recurrence (3,4).
The role of surgical resection in the treatment of
liver metastases from esophageal carcinoma is controversial.
Complete surgical resection is a well-accepted treatment for
metastatic liver disease from colorectal cancer, with 5-year
survival rates of 25–40% (5). Huddy
et al reported on four patients who underwent successful
resection of recurrent liver metastases from esophageal cancer
(6). Cryosurgical ablation,
transarterial embolization, and radiofrequency ablation also remain
as options for management of liver metastases in patients who are
unsuitable for surgery.
Stereotactic body radiation therapy (SBRT) can also
be considered an effective, safe, and non-invasive therapeutic
option for unresectable liver metastases (7). We selected SBRT to treat
oligo-recurrence in the liver in a patient with relapsed esophageal
cancer, who had a remarkable clinical response without severe
adverse events.
Case report
A 60-year-old Japanese man presented with a chief
complaint of dysphagia in December 2012. His alcohol consumption
was 60 g/day and he had smoked 20 cigarettes per day for the
previous 40 years. Gastrointestinal fiberscopy revealed a Borrmann
type II lesion invading the full circumference of the esophagus at
21–28 cm from the incisor teeth. The mucosa was biopsied and the
diagnosis was moderately to poorly differentiated squamous cell
carcinoma. A computed tomography (CT) scan showed a thickened
upper-middle thoracic esophageal wall that was broadly attached to
the membranous wall of the trachea and an absence of the fat plane,
indicating tumor invasion. The CT scan also showed enlarged right
upper thoracic paraesophageal and left paratracheal lymph nodes.
The patient was staged clinically as T4bN1M0 according to the 7th
edition of the American Joint Committee on Cancer TNM staging
system.
The patient received definitive concurrent
chemoradiotherapy consisting of four 28-day cycles of chemotherapy
(nedaplatin 80 mg/m2 on day 1 and S-1 120 mg/body orally
on days 1–14) and radiotherapy (four-field oblique box, parallel
opposed pair, 10 MV X-ray beams; 50 Gy in daily fractions of 2 Gy).
He experienced acute adverse events, including grade 2 fatigue,
grade 2 esophagitis, grade 1 anemia, grade 3 leukopenia, and grade
3 thrombocytopenia (Common Terminology Criteria for Adverse Events
version 4.0). After the chemoradiotherapy, a CT scan showed
improvement of the thickened esophageal wall and that the swollen
lymph nodes had markedly reduced in volume. Gastrointestinal
fiberscopy revealed no obvious abnormalities, except for a
scar-like lesion at the site of the primary lesion in the
esophagus. Accordingly, this treatment was deemed to have resulted
in a complete response. Follow-up investigations included a
physical examination, assessment of laboratory data, and a CT
scan.
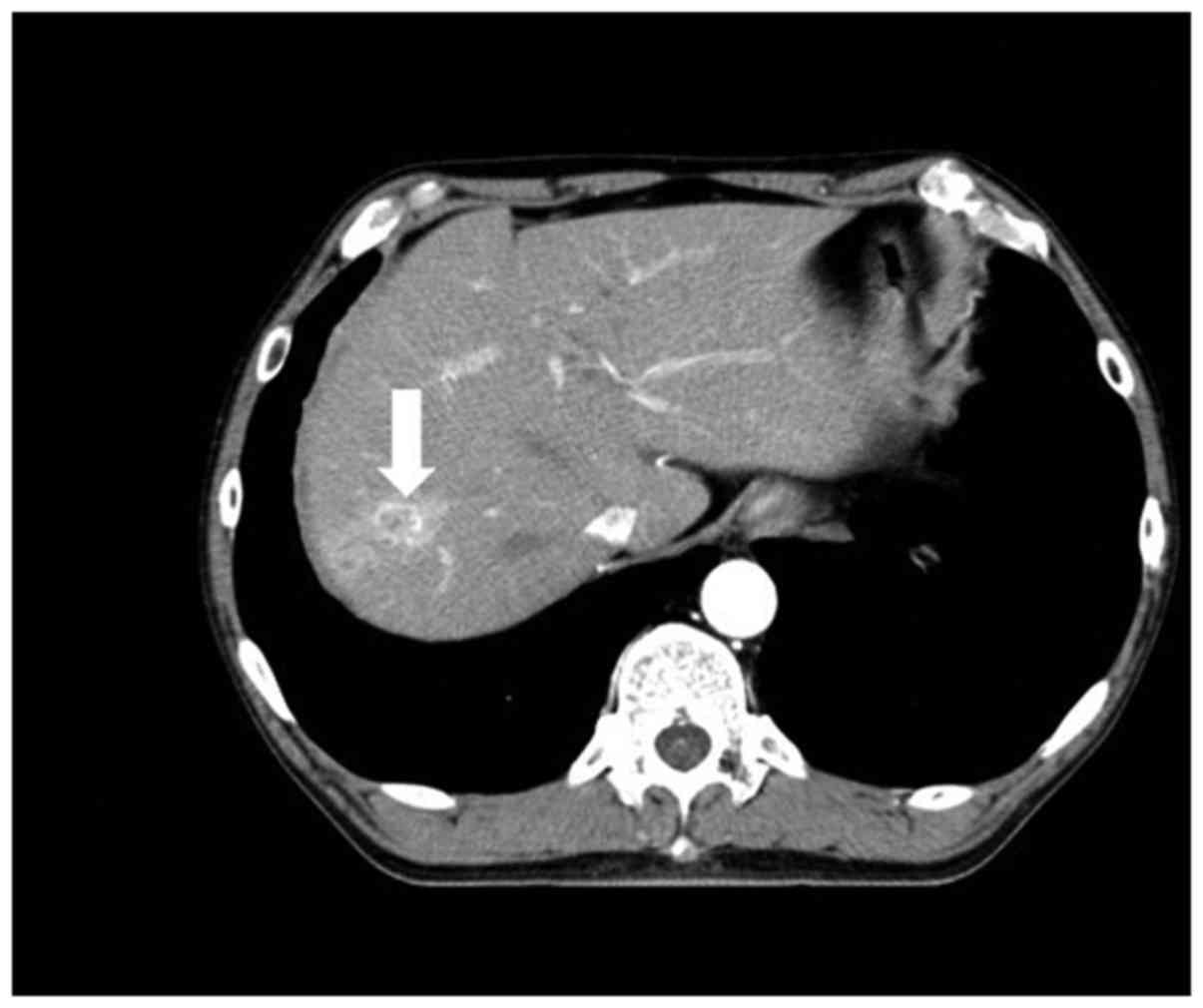
In December 2013, an abdominal CT scan revealed a
solitary nodule measuring 18 mm in diameter in segment 8 of the
liver (Fig. 1) that was
pathologically confirmed by a needle biopsy to be squamous cell
carcinoma and was compatible with metastasis from the esophageal
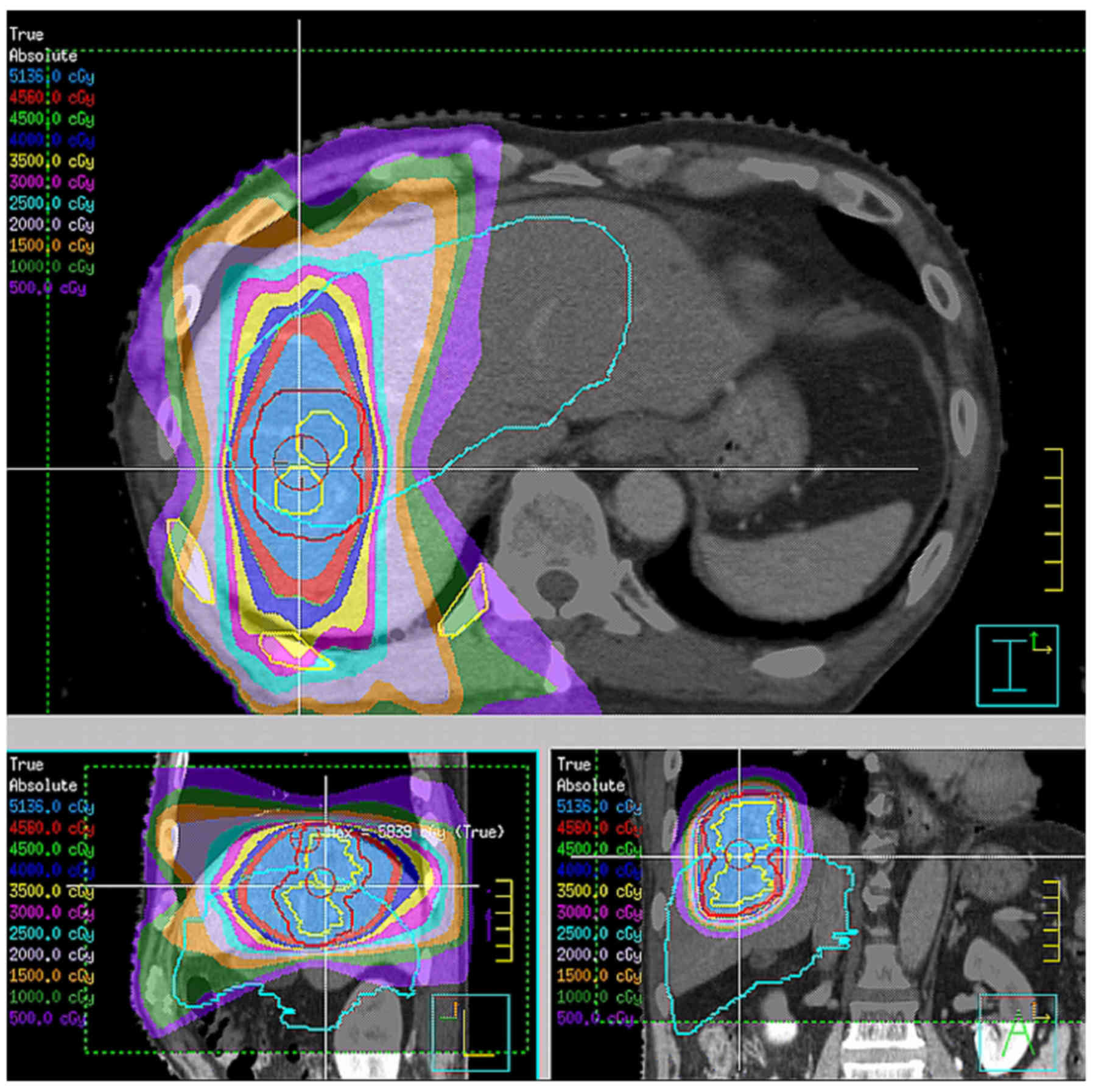
cancer. The patient elected to receive SBRT (Fig. 2) followed by two 28-day cycles of
adjuvant combination chemotherapy (nedaplatin 80 mg/m2
on day 1 and S-1 100 mg/body orally on days 1–14). The SBRT
consisted of eleven 6 MV X-ray beams including a non-coplanar beam
arrangement and 48 Gy in once-daily fractions of 12 Gy delivered to
95% of the planning target volume.
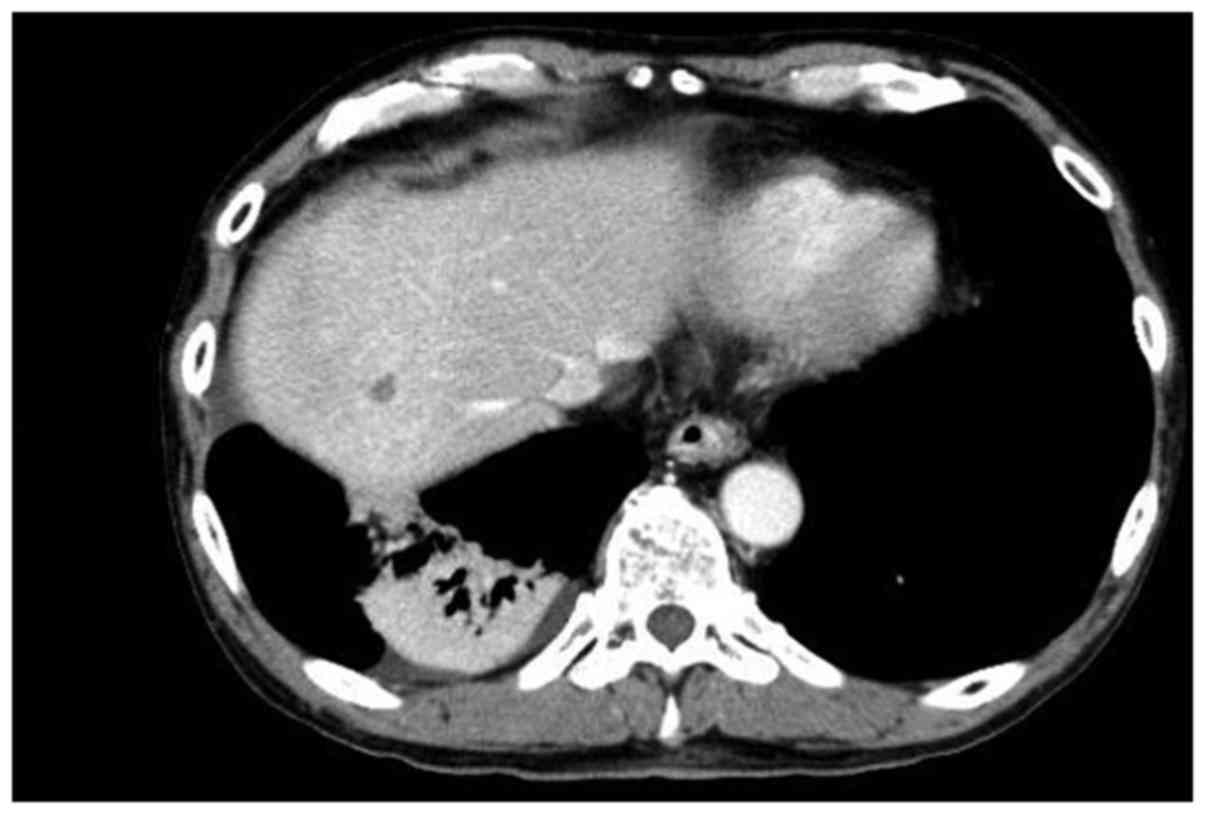
A CT scan showed that the nodular lesion in segment
8 of the liver was markedly reduced in volume (Fig. 3). The patient showed no signs of
recurrence for ~3 years. However, in January 2017, he noticed
dysphagia and a CT scan revealed a large lesion located on the
right lateral wall of the oropharynx and another intrahepatic
lesion, which were considered a recurrence of esophageal cancer. He
underwent salvage chemotherapy consisting of docetaxel 70
mg/m2 intravenously at 3-week intervals and palliative
irradiation (30 Gy in daily fractions of 3 Gy) to the oropharynx
and the metastatic liver lesion.
Discussion
Metastatic recurrence is associated with poor
clinical outcome in cancer treatment. However, as in our case,
there is a preliminary state during which patients with cancer have
a limited number of relapsed sites with a controlled primary
lesion. The term for this state is ‘oligo-recurrence’, which was
defined by Niibe et al (8,9). It
originates from Hellman and Weichselbaum's hypothesis of
oligometastases, that is, a clinical disease state in which tumors
early in the evolution of metastatic progression produce metastases
that are limited in number and location (10). Appropriate local treatment could be
efficacious for these ‘oligometastatic’ lesions. Indeed, Iitaka
et al have reported long-term survival in a patient with a
recurrence of esophageal cancer that was treated by a multimodal
combination of appropriate systemic and local therapy (11).
SBRT is a safe and locally effective treatment for
patients with inoperable oligometastases (12,13). A
retrospective study of 51 patients with metastatic liver tumors in
Japan reported that SBRT was associated with a local control rate
of 64.2% and an overall survival rate of 72% at 2 years, with no
significant (over grade 2) elevation of liver enzymes during
treatment (14). These outcomes
confirm that SBRT has a beneficial effect in patients who are
unsuitable for surgery.
However, the indication for SBRT in the management
of oligometastases should be considered carefully. Although the
response rate in patients treated by SBRT is high, intrahepatic
recurrence has been observed in a proportion of patients. Milano
et al reported that 45% of their patients with initial
oligometastases confined to the liver developed local recurrence
after SBRT (15).
Appropriate management of an oligometastatic state
has a significant role in the management of cancer patients. Egawa
et al reported successful control of liver metastasis from
esophageal cancer for 1 year following SBRT (16). SBRT might be considered as a good
treatment option for liver oligo-recurrence of esophageal
carcinoma.
References
|
1
|
Meguid RA, Hooker CM, Taylor JT, Kleinberg
LR, Cattaneo SM II, Sussman MS, Yang SC, Heitmiller RF, Forastiere
AA and Brock MV: Recurrence after neoadjuvant chemoradiation and
surgery for esophageal cancer: Does the pattern of recurrence
differ for patients with complete response and those with partial
or no response? J Thorac Cardiovasc Surg. 138:1309–1317. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Quint LE, Hepburn LM, Francis IR, Whyte RI
and Orringer MB: Incidence and distribution of distant metastases
from newly diagnosed esophageal carcinoma. Cancer. 76:1120–1125.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Mariette C, Balon JM, Piessen G, Fabre S,
Van Seuningen I and Triboulet JP: Pattern of recurrence following
complete resection of esophageal carcinoma and factors predictive
of recurrent disease. Cancer. 97:1616–1623. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hulscher JB, van Sandick JW, Tijssen JG,
Obertop H and van Lanschot JJ: The recurrence pattern of esophageal
carcinoma after transhiatal resection. J Am Coll Surg. 191:143–148.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Abbas S, Lam V and Hollands M: Ten-year
survival after liver resection for colorectal metastases:
Systematic review and meta-analysis. ISRN Oncol.
2011:7632452011.PubMed/NCBI
|
|
6
|
Huddy JR, Thomas RL, Worthington TR and
Karanjia ND: Liver metastases from esophageal carcinoma: Is there a
role for surgical resection? Dis Esophagus. 28:483–487. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Scorsetti M, Arcangeli S, Tozzi A, Comito
T, Alongi F, Navarria P, Mancosu P, Reggiori G, Fogliata A,
Torzilli G, et al: Is stereotactic body radiation therapy an
attractive option for unresectable liver metastases? A preliminary
report from a phase 2 trial. Int J Radiat Oncol Biol Phys.
86:336–342. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Niibe Y and Hayakawa K: Oligometastases
and oligo-recurrence: The new era of cancer therapy. Jpn J Clin
Oncol. 40:107–111. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Niibe Y and Chang JY: Novel insights of
oligometastases and oligo-recurrence and review of the literature.
Pulm Med. 2012:2610962012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hellman S and Weichselbaum RR:
Oligometastases. J Clin Oncol. 13:8–10. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Iitaka D, Shiozaki A, Fujiwara H, Ichikawa
D, Okamoto K, Komatsu S, Murayama Y, Ikoma H, Kuriu Y, Nakanishi M,
et al: Case involving long-term survival after esophageal cancer
with liver and lung metastases treated by multidisciplinary
therapy: Report of a case. Surg Today. 43:556–561. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Almaghrabi MY, Supiot S, Paris F, Mahé MA
and Rio E: Stereotactic body radiation therapy for abdominal
oligometastases: A biological and clinical review. Radiat Oncol.
7:1262012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
de Vin T, Engels B, Gevaert T, Storme G
and De Ridder M: Stereotactic radiotherapy for oligometastatic
cancer: A prognostic model for survival. Ann Oncol. 25:467–471.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yamashita H, Onishi H, Matsumoto Y,
Murakami N, Matsuo Y, Nomiya T and Nakagawa K: Japanese
Radiological Society multi-institutional SBRT study group
(JRS-SBRTSG): Local effect of stereotactic body radiotherapy for
primary and metastatic liver tumors in 130 Japanese patients.
Radiat Oncol. 9:1122014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Milano MT, Katz AW and Okunieff P:
Patterns of recurrence after curative-intent radiation for
oligometastases confined to one organ. Am J Clin Oncol. 33:157–163.
2010.PubMed/NCBI
|
|
16
|
Egawa T, Okubo Y, Kemmochi T, Mori T, Sato
S, Nishiya S, Mihara K, Ito Y, Makino H and Nagashima A: A case of
liver metastasis from esophageal cancer treated with stereotactic
body radiation therapy. Gan To Kagaku Ryoho. 40:1850–1852. 2013.(In
Japanese). PubMed/NCBI
|