Introduction
Endobronchial ultrasound (EBUS) bronchoscopy has
been well described in the diagnosis of pulmonary diseases,
particularly lung cancer, due to its usefulness in the evaluation
of hilar and mediastinal lymph nodes as a diagnostic and staging
method (1). Recently, EUS-FNA
qualified as a surgical mediastinal staging procedure due to its
safety and minimal invasiveness, and is recommended by
international guidelines (2). To
date, numerous publications have established the value of EUS-FNA
in the assessment of mediastinal nodes, as well as the adrenal
glands (3–6). Although accumulating evidence has
confirmed the efficacy of EUS in the staging of mediastinal nodes,
the application of EUS-FNA is not yet widely applied in the
diagnosis of patients with lung cancer (7,8). We
herein report a case of stage IV lung adenocarcinoma metastatic to
the left adrenal gland, which was finally diagnosed by EUS-FNA
biopsy. To the best of our knowledge, the present case may be the
first to affirm the validity of the use of EUS-FNA as a first-line
minimally invasive staging procedure for non-small-cell lung cancer
(NSCLC) in China.
Case report
A 62-year-old Han Chinese woman was admitted to the
Department of Respiratory Medicine, Shanghai East Hospital, Tongji
University School of Medicine (Shanghai, China) in May 2017, with
complaints of a non-productive cough persisting for 3 months and a
history of passive smoking. No abnormalities were found on routine
physical examination. The laboratory tests demonstrated that the
serum carcinoembryonic antigen and carbohydrate antigen-125 levels
were elevated to 156.7 ng/ml (normal range, 0–5.2 ng/ml) and 85.23
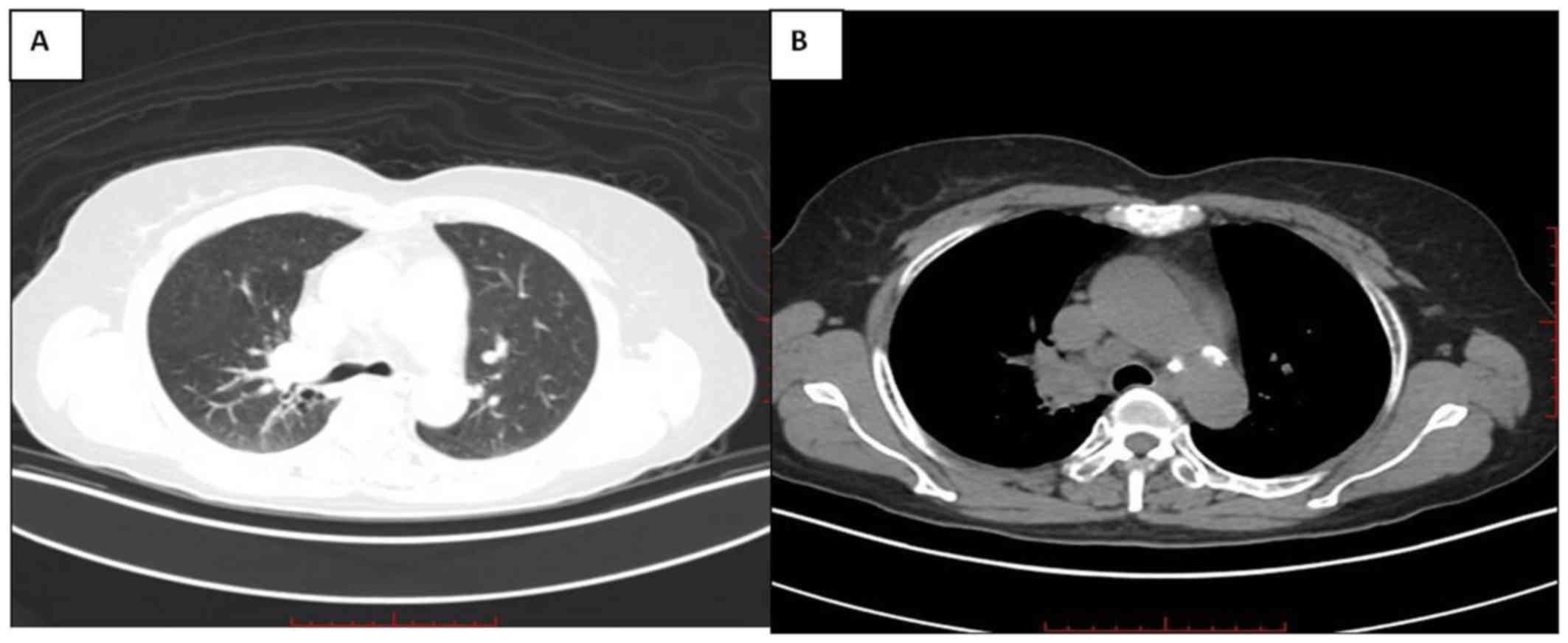
ng/ml (normal range, 0–35 ng/ml), respectively. A computed
tomography (CT) scan of the chest revealed a hypodense soft mass
(size, 2.3×2.2 cm) with the spicule sign in the right upper lobe;
an enlarged paratracheal lymph node in the superior mediastinum
(4R) was also identified (Fig. 1A and
B). The patient was then scheduled to undergo a
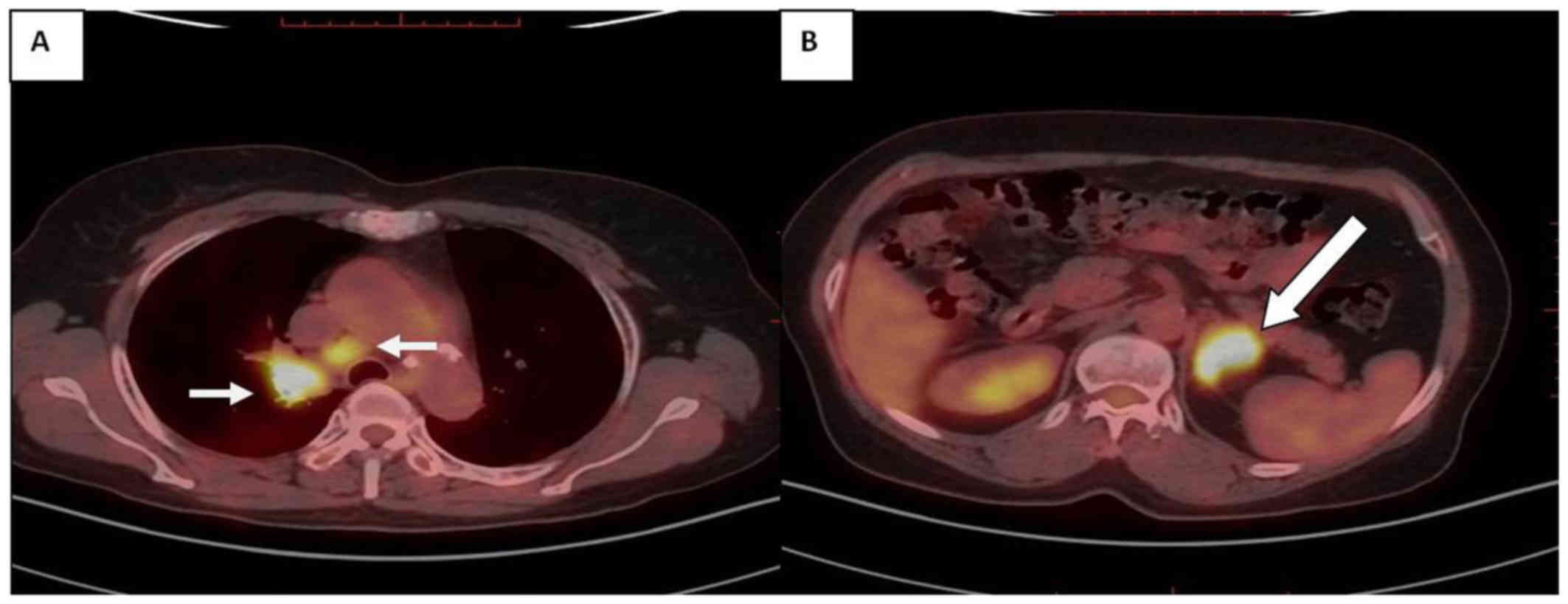
18F-fluorodeoxyglucose positron emission tomography
(18FDG-PET) scan and the results demonstrated abnormal
18FDG uptake by the pulmonary mass of the right upper
lobe [maximum standardized uptake value (SUVmax) 13.5],
the right paratracheal lymph node (4R) (SUVmax, 13.0)
(Fig. 2A), as well as the left
adrenal gland (SUVmax, 13.6) (Fig. 2B). Furthermore, irregular shape of
the left adrenal gland, with dimensions 3.8×2.7 cm, was also
observed (Fig. 2B). These findings
strongly indicated that the pulmonary lesion was a malignant tumor.
Moreover, the enlarged and 18FDG-PET-positive left
adrenal gland was also highly likely to be a metastatic site.
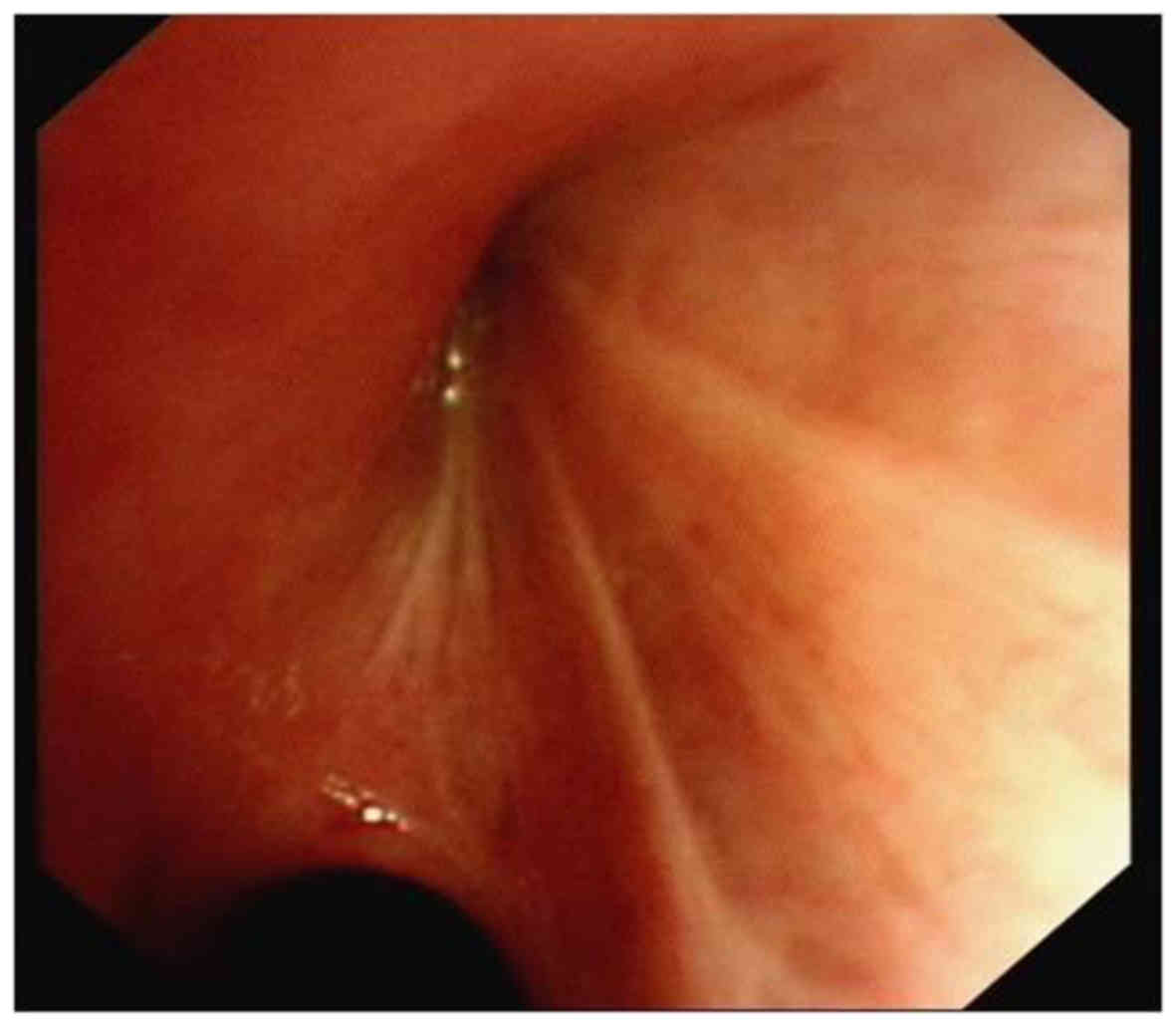
Routine bronchoscopy was initially performed to assess the airways,
and it revealed an obstruction of the bronchus opening at the
apical segment of the right upper lobe, without detection of any
neoplasm (Fig. 3). Subsequently,
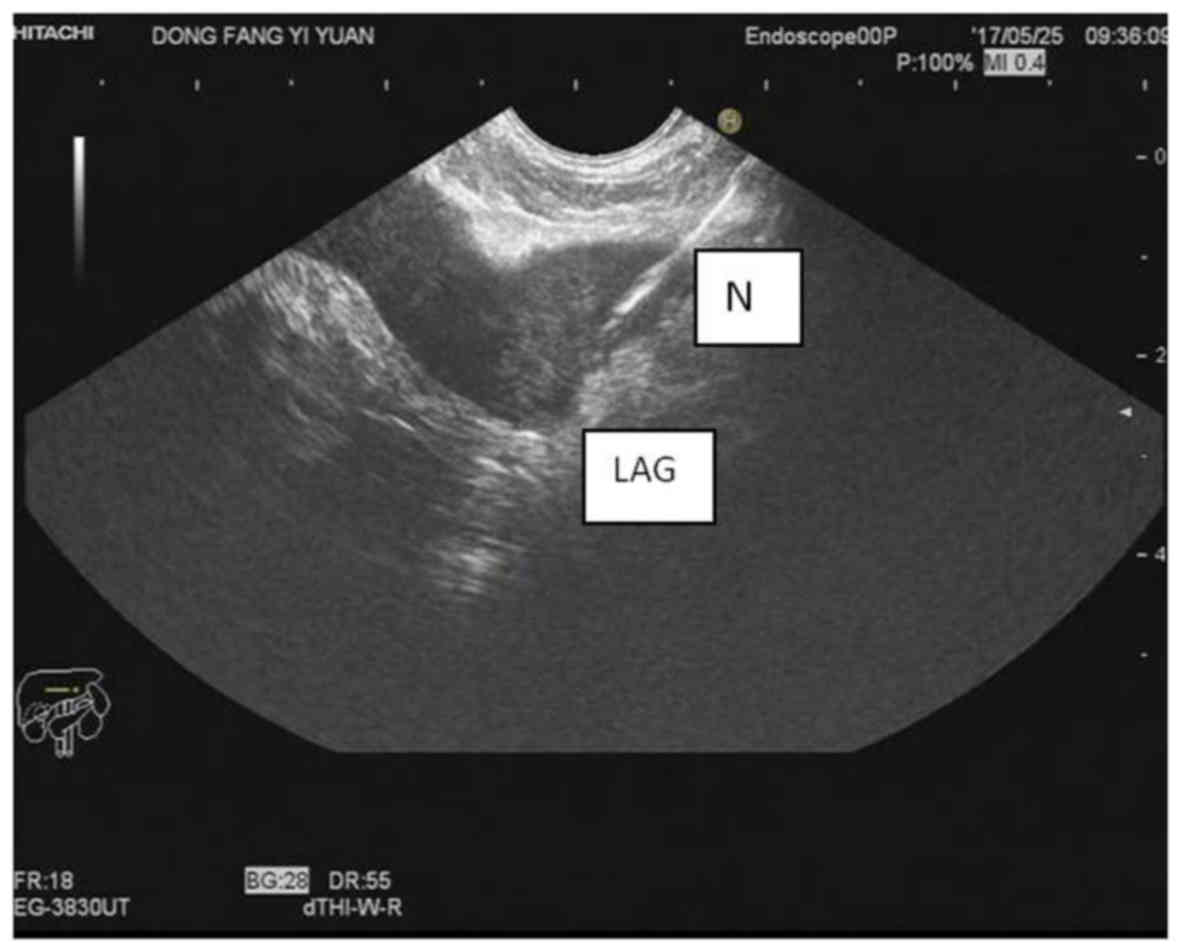
EUS-FNA was suggested as a minimally invasive test for the
confirmation of suspected metastasis to the left adrenal gland. EUS
was conducted in a standardized manner at an endoscopy room under
conscious sedation using propofol (9). The vessels surrounding the left adrenal
were evaluated with color flow Doppler; then, the optimal lesion
site (hypoechoic involvement in the left adrenal gland) was
punctured using a 22-gauge needle, guided by real-time ultrasound
imaging (Fig. 4). FNA was repeated
until sufficient tissue samples were obtained. Subsequently, the
samples were processed and stained for cytological analysis.
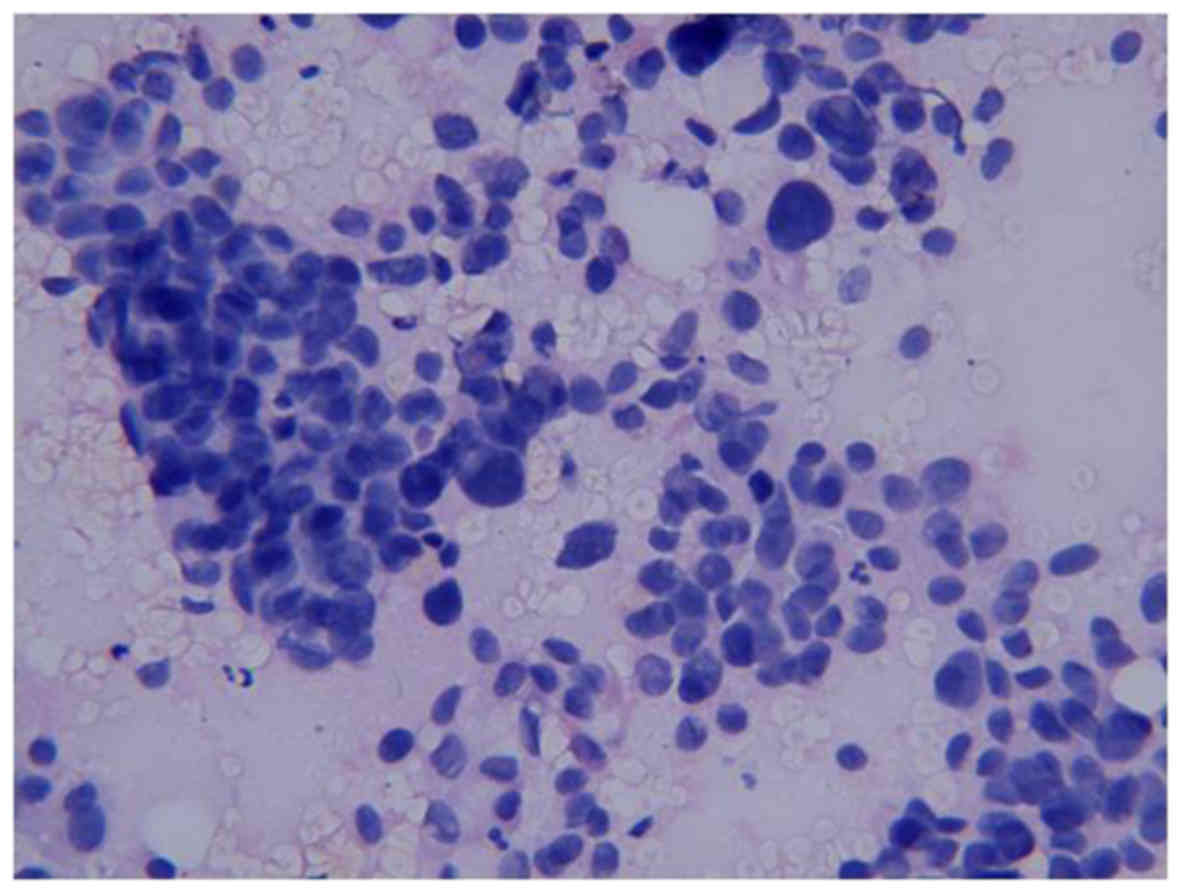
Histopathological examination of the EUS-FNA samples demonstrated
an adenocarcinoma. The results of immunohistochemical examination
indicated metastatic adenocarcinoma from the primary lung cancer
(Fig. 5). Consequently, our patient
was treated with gefitinib due to the presence of epidermal growth
factor receptor gene mutation. The physical status of the patient
has currently been under control since the treatment with gefitinib
for ~10 months.
Discussion
Lung cancer is the leading cause of cancer-related
mortality worldwide (10). The
majority of new cases of lung cancer (≤80%) are NSCLCs (11). Chest CT and integrated PET scans are
widely available non-invasive methods for the assessment of
suspected NSCLC; however, their efficacy is limited by their
relatively low sensitivity (58 and 74%, respectively) and
specificity (85% for both) (12).
Bronchoscopy is usually required to diagnose or evaluate pulmonary
lesions. In terms of minimally invasive techniques, EBUS has the
best yield regarding hilar, intrapulmonary, anterior and superior
mediastinal lymph nodes. Hence, EBUS is suitable for lymph nodes
located in the anterosuperior mediastinum, as well as paratracheal
regions (13). On the contrary,
patients with enlarged posteroinferior mediastinal or subcarinal
lymph nodes may benefit from EUS as a primary staging procedure.
The selection of EUS or EBUS is mainly determined by the location
of the lymph nodes (14). For
mediastinal staging, these two invasive methods may complement each
other. Furthermore, compared with EBUS, EUS may detect distant
metastatic lesions to subdiaphragmatic organs, including the left
adrenal gland and the liver, which adds another advantage with
respect to metastatic lung cancer (15).
In the present case, routine bronchoscopy was
initially performed, but no mass was detected in the trachea.
Accordingly, transbronchial lung biopsy could not be performed.
Thus, it was crucial to verify the suspected malignant involvement
for the definitive diagnosis. The paratracheal lymph node (4R) and
the left adrenal gland were both found to harbor metastatic lesions
on CT and 18FDG-PET imaging. In theory, EBUS-guided
transbronchial needle aspirate (EBUS-TBNA) and EUS-FNA may be
applied to perform a biopsy of the target lesion. However, the
mediastinal nodes are surrounded by elements of the cardiopulmonary
system, vasculature and skeletal components, which makes tissue
sampling challenging (16). It was
reported that EBUS-TBNA may be associated with occasional serious
complications, such as pneumothorax and respiratory failure
requiring ventilation (17). In
addition, unlike the trachea, the esophagus is flexible. Using
magnified real-time imaging, the operator may approach the adrenal
gland, easily avoiding the pancreas and local great vessels and
reducing the risk of injuring the pleural space under EUS
examination. In this manner, biopsy of the adrenal lesion is safer
and simpler. A meta-analysis of 18 studies including a total of
1,201 patients reported that the rate of complications caused by
EUS-FNA was as low as 0.8% (only 10 cases) (18). In conclusion, EUS-FNA was considered
as a superior technique for the assessment of the metastatic
lesions, and a definitive diagnosis of the metastasis to the left
adrenal from the primary lung adenocarcinoma was finally
confirmed.
As previously reported, the adrenal glands are the
fourth most common metastatic site in lung cancer (19). Of note, metastases to left adrenal
gland are significantly more common compared with those to the
right adrenal (20). In the present
case, the PET findings were consistent with those of previous
reports. Given that the left adrenal is easily accessible through
the stomach and may be easily visualized and real-time sampled by
EUS, EUS may be considered as the preferred approach to the biopsy
of left adrenal lesions (6). The
utility of EUS-FNA has been broadened to provide tissue evidence of
suspected left adrenal metastases in lung malignancies (21). Schuurbiers et al demonstrated
that EUS-FNA has a relatively high sensitivity (86%) and positive
predictive value (70%) for malignant lesions in the left adrenal
gland (22). Thus, EUS-FNA is a
staging tool valuable for identifying metastases to the left
adrenal gland in patients with lung cancer.
Although EUS may serve as a replacement for EBUS in
assessing mediastinal lymph nodes, the application of EUS-FNA for
diagnosing lung malignancies remains limited and controversial.
Reddy et al reported that the majority of oncologists in the
US did not consider EUS to be helpful for NSCLC staging, with very
few (<20%) selecting this procedure as a diagnostic tool
(23). Therefore, it is crucial to
ameliorate the application of EUS in the staging of lung cancer. In
the present case, the diagnostic value of EUS-FNA in lung cancer
with suspected left adrenal metastasis was confirmed and, although
performing EBUS may be possible, EUS-FNA may also be utilized as
the first-line approach to detecting suspected lung malignancy,
improving the application of EUS-FNA in the diagnosis of lung
cancer with nodal or distant metastases.
From this case study of primary lung adenocarcinoma
with mediastinal lymph node and left adrenal metastases described
above, left adrenal biopsy via EUS-FNA was found to be an efficient
approach to obtaining a final definitive diagnosis. The feasibility
and validity of EUS-FNA in the diagnosis and staging of NSCLC was
also demonstrated. Even when EBUS is not difficult to perform,
EUS-FNA may also be an alternative option for first-line staging in
NSCLC.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of materials and data
Not applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for publication of this case report and any accompanying
images.
Authors' contributions
ML analyzed the clinical data and drafted the
manuscript. YS provided the imaging data. HL performed the
bronchoscopy. MX was the gastroenterologist who performed the
EUS-FNA. QZ conducted follow-up on the patient in the outpatient
clinic. ZG contributed to critical review and supervised the entire
work. All the authors have read and approved the final version of
this manuscript.
Competing interests
The authors declare that they have no competing
interests to disclose.
References
|
1
|
Yasufuku K, Chiyo M, Koh E, Moriya Y,
Iyoda A, Sekine Y, Shibuya K, Iizasa T and Fujisawa T:
Endobronchial ultrasound guided transbronchial needle aspiration
for staging of lung cancer. Lung Cancer. 50:347–354. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Detterbeck FC, Jantz MA, Wallace M,
Vansteenkiste J and Silvestri GA: American College of Chest
Physicians: Invasive mediastinal staging of lung cancer: ACCP
evidence-based clinical practice guidelines (2nd edition). Chest.
132 3 Suppl:202S–220S. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
ASGE Standards of Practice Committee, .
Jue TL, Sharaf RN, Appalaneni V, Anderson MA, Ben-Menachem T,
Decker GA, Fanelli RD, Fukami N, Ikenberry SO, et al: Role of EUS
for the evaluation of mediastinal adenopathy. Gastrointest Endosc.
74:239–245. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hwangbo B, Lee GK, Lee HS, Lim KY, Lee SH,
Kim HY, Lee HS, Kim MS, Lee JM, Nam BH and Zo JI: Transbronchial
and transesophageal fine-needle aspiration using an ultrasound
bronchoscope in mediastinal staging of potentially operable lung
cancer. Chest. 138:795–802. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ang TL, Chua TS, Fock KM, Tee AK, Teo EK
and Mancer K: EUS-FNA of the left adrenal gland is safe and useful.
Ann Acad Med Singapore. 36:954–957. 2007.PubMed/NCBI
|
|
6
|
Eloubeidi MA, Seewald S, Tamhane A, Brand
B, Chen VK, Yasuda I, Cerfolio RJ, Omar S, Topalidis T, Wilcox CM
and Soehendra N: EUS-guided FNA of the left adrenal gland in
patients with thoracic or GI malignancies. Gastrointest Endosc.
59:627–633. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hernandez LV, Geenen JE, Schmalz MJ and
Catalano MF: The underutilization of EUS-guided FNA in the
lymph-node staging of non-small-cell lung cancer: Perceptions of
chest physicians in Wisconsin. Gastrointest Endosc. 62:517–520.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Walsh PR and Williams DB: Mediastinal
adenopathy: Finding the answer with endoscopic ultrasound-guided
fine-needle aspiration biopsy. Intern Med J. 35:392–398. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Peric R, Schuurbiers OC, Veseliç M, Rabe
KF, van der Heijden HF and Annema JT: Transesophageal endoscopic
ultrasound-guided fine-needle aspiration for the mediastinal
staging of extrathoracic tumors: A new perspective. Ann Oncol.
21:1468–1471. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Alberg AJ, Ford JG and Samet JM: American
College of Chest Physicians: Epidemiology of lung cancer: ACCP
evidence-based clinical practice guidelines (2nd edition). Chest.
132 3 Suppl:29S–55S. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Silvestri GA, Gould MK, Margolis ML,
Tanoue LT, McCrory D, Toloza E and Detterbeck F: American College
of Chest Physicians: Noninvasive staging of non-small cell lung
cancer: ACCP evidenced-based clinical practice guidelines (2nd
edition). Chest. 132 3 Suppl:178S–201S. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Herth FJ, Eberhardt R, Vilmann P, Krasnik
M and Ernst A: Real-time endobronchial ultrasound guided
transbronchial needle aspiration for sampling mediastinal lymph
nodes. Thorax. 61:795–798. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gill KR, Ghabril MS, Jamil LH, Hasan MK,
McNeil RB, Woodward TA, Raimondo M, Hoffman BJ, Hawes RH,
Romagnuolo J and Wallace MB: Endosonographic features predictive of
malignancy in mediastinal lymph nodes in patients with lung cancer.
Gastrointest Endosc. 72:265–271. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lankarani A and Wallace MB: Endoscopic
ultrasonography/fine-needle aspiration and endobronchial
ultrasonography/fine-needle aspiration for lung cancer staging.
Gastrointest Endosc Clin N Am. 22(207–219): viii2012.
|
|
16
|
Hasan MK, Gill KR, Wallace MB and Raimondo
M: Lung cancer staging by combined endobronchial ultrasound (EBUS)
and endoscopic ultrasound (EUS): The gastroenterologist's
perspective. Dig Liver Dis. 42:157–162. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Varela-Lema L, Fernández-Villar A and
Ruano-Ravina A: Effectiveness and safety of endobronchial
ultrasound-transbronchial needle aspiration: A systematic review.
Eur Respir J. 33:1156–1164. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Micames CG, McCrory DC, Pavey DA, Jowell
PS and Gress FG: Endoscopic ultrasound-guided fine-needle
aspiration for non-small cell lung cancer staging: A systematic
review and metaanalysis. Chest. 131:539–548. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Abrams HL, Spiro R and Goldstein N:
Metastases in carcinoma; Analysis of 1,000 autopsied cases. Cancer.
3:74–85. 1950. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ettinghausen SE and Burt ME: Prospective
evaluation of unilateral adrenal masses in patients with operable
non-small-cell lung cancer. J Clin Oncol. 9:1462–1466. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Bodtger U, Vilmann P, Clementsen P, Galvis
E, Bach K and Skov BG: Clinical impact of endoscopic
ultrasound-fine needle aspiration of left adrenal masses in
established or suspected lung cancer. J Thorac Oncol. 4:1485–1489.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Schuurbiers OC, Tournoy KG, Schoppers HJ,
Dijkman BG, Timmers HJ, de Geus-Oei LF, Grefte JM, Rabe KF,
Dekhuijzen PN, van der Heijden HF and Annema JT: EUS-FNA for the
detection of left adrenal metastasis in patients with lung cancer.
Lung Cancer. 73:310–315. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Reddy NK, Markowitz AB, Abbruzzese JL and
Bhutani MS: Knowledge of indications and utilization of EUS: A
survey of oncologists in the United States. J Clin Gastroenterol.
42:892–896. 2008. View Article : Google Scholar : PubMed/NCBI
|