Introduction
Extraskeletal osteosarcoma (ESOS) is a rare soft
tissue sarcoma defined as a malignant mesenchymal neoplasm composed
of cells producing osteoid, bone and/or chondroid material, with no
attachment to the bone or periosteum (1). ESOS accounts for 1–2% of all soft
tissue sarcomas and 2–4% of all osteosarcomas (1,2). ESOS
occurs most frequently in the deep tissues of the thighs, followed
by the buttocks and trunk (1). ESOS
originating in the superficial (cutaneous-subcutaneous) tissue is
extremely rare (3). To the best of
our knowledge, only 17 cases of subcutaneous ESOS have been
reported in detail to date. The prognosis of ESOS is reported to be
worse compared with that of skeletal osteosarcoma (4). However, there are reports of long-term
survival among the 17 cases of subcutaneous ESOS (5,6).
Furthermore, our patient with subcutaneous ESOS survived for 3
years with treatment. Therefore, superficial ESOS may have a better
prognosis compared with deep-seated ESOS.
In this report, a new case of subcutaneous ESOS of
the lower leg is presented, and previous reports of subcutaneous
ESOS are reviewed, focusing on the clinical characteristics,
including the MIB-1 labeling index, treatment methods and
prognosis.
Case report
In April 2015, a 79-year-old healthy man presented
with a painful, slowly growing mass in his lower right leg
measuring ~5 cm in greatest dimension. The mass had been present
for ~3 years, and the patient had initially consulted another
hospital. There was no reported history of trauma or radiation to
this area. Plain radiographs revealed an irregular calcification
pattern of ~5 cm in the soft tissue of the lower right leg
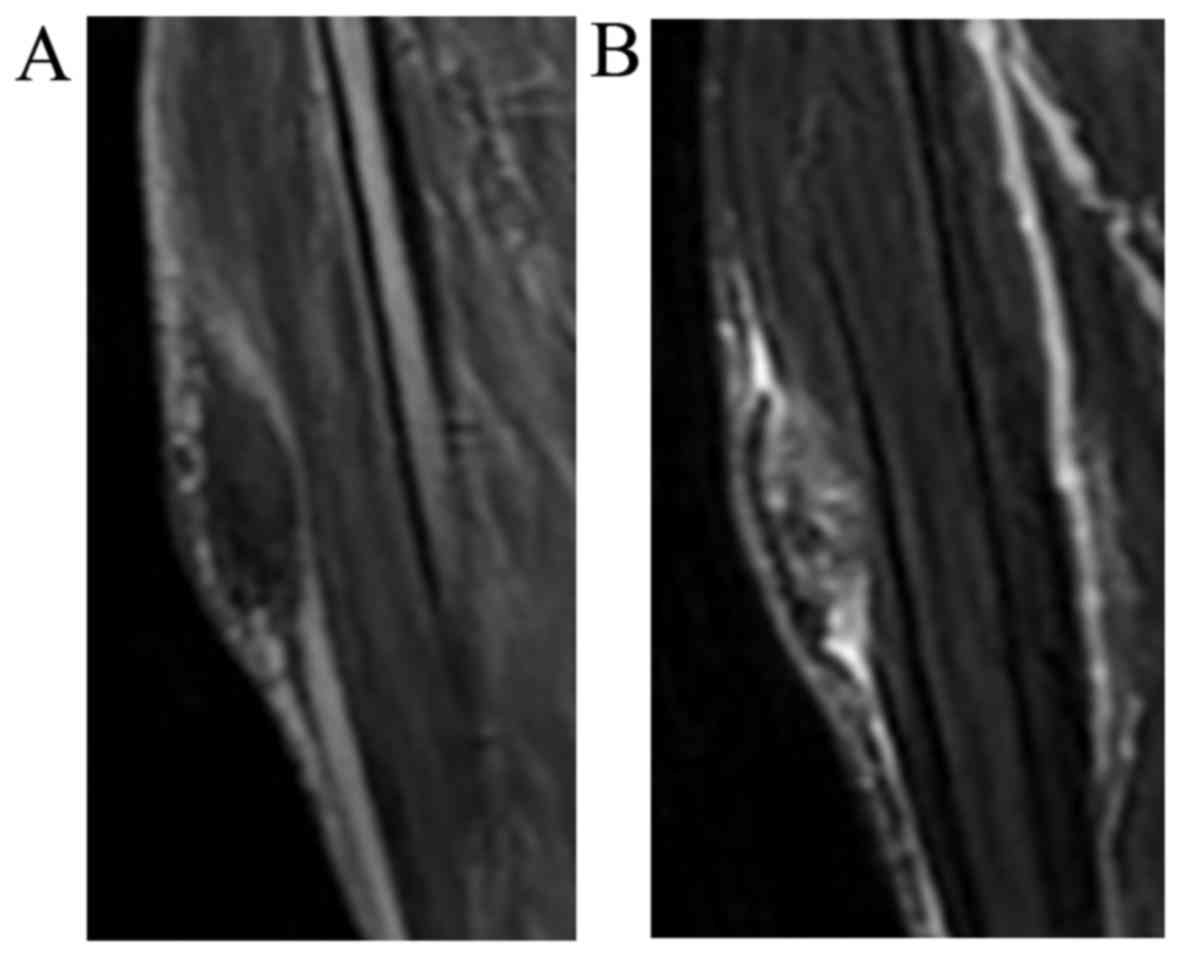
(Fig. 1). Magnetic resonance imaging
(MRI) revealed a 5×2-cm subcutaneous mass, superficial to the
fascia of the tibialis anterior muscle. The mass was hypointense on
T1-weighted images and exhibited a heterogeneous high-intensity
signal on fat-suppressed T2-weighted images (Fig. 2). Computed tomography (CT) of the
chest revealed no pulmonary lesions. Since the mass had been
growing slowly, the differential diagnosis included a low-grade
soft tissue sarcoma with bone mineralization, or a benign tumor.
Marginal resection of the mass was performed in the previous
hospital and the excised tumor was histopathologically diagnosed as
ESOS; the patient was then referred to our institution for further
treatment. Since the patient was elderly, it was decided not to
administer chemotherapy, but to follow him up regularly.
One year after tumor resection in the previous
hospital, the patient noticed a 2-cm mass in the surgical wound.
Plain radiographs revealed a mass with calcification in the soft
tissue of the lower leg. MRI revealed a 1×1-cm mass in the previous
surgical scar that was hypointense on T1-weighted images and
exhibited a heterogeneous high-intensity signal on the
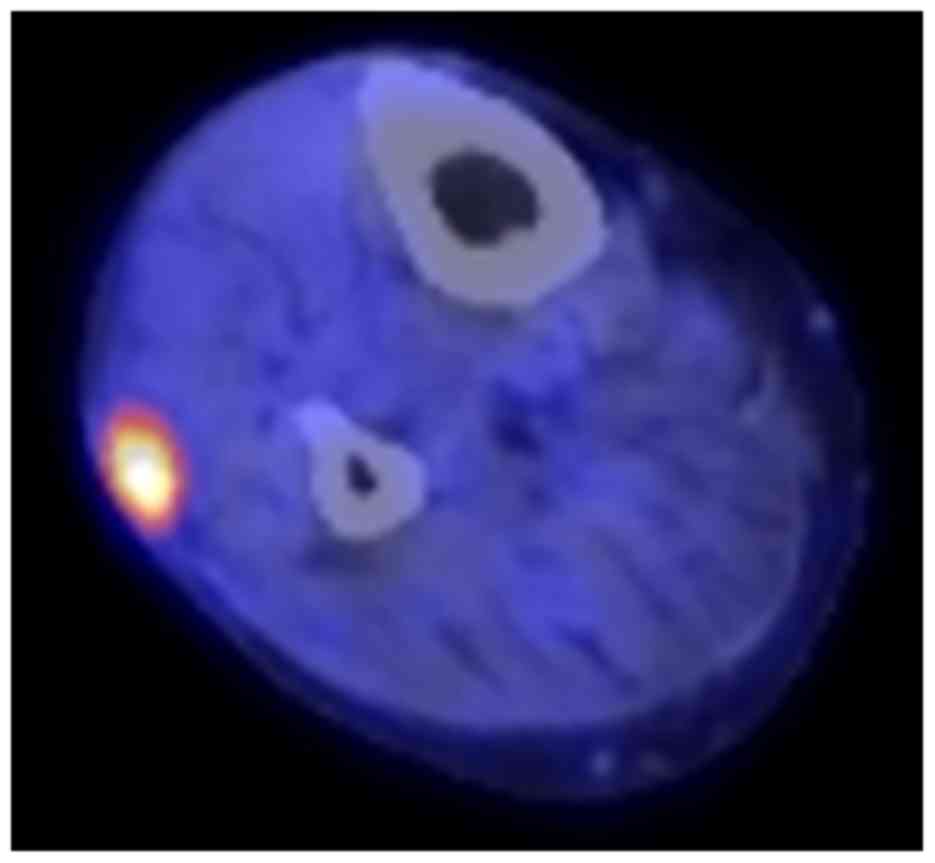
fat-suppressed T2-weighted images. F-18 2-fluoro-2-deoxy-glucose
positron emission tomography (FDG-PET)/CT revealed accumulation of
FDG only in the palpable mass of the lower leg, with a maximum
standardized uptake value of 6.7 (Fig.
3). Local recurrence of ESOS was diagnosed, and a wide
resection was performed, with skin grafting from the inguinal area.
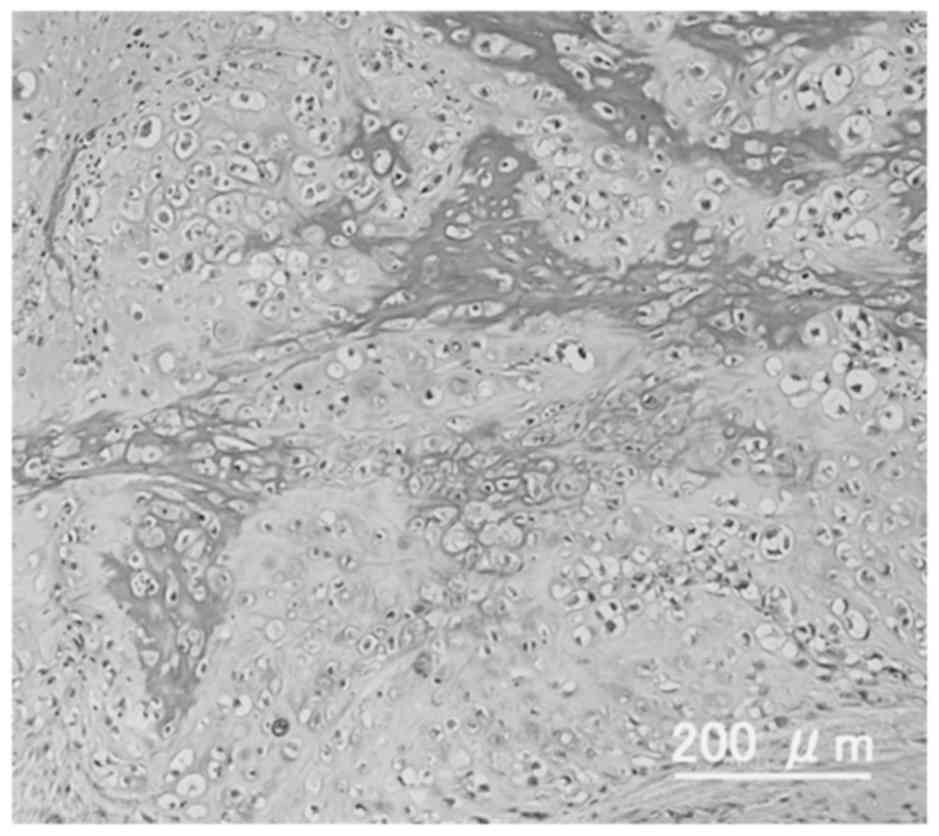
On histopathological examination, the resected tumor was composed
of proliferating chondrocytic cells with nuclear atypia producing
coarse lace-like neoplastic bone (Fig.
4). Immunohistochemical staining for Ki-67 revealed a high
proliferative index of 35%. These findings led to a diagnosis of
the chondroblastic type of ESOS. Since the patient was elderly, no
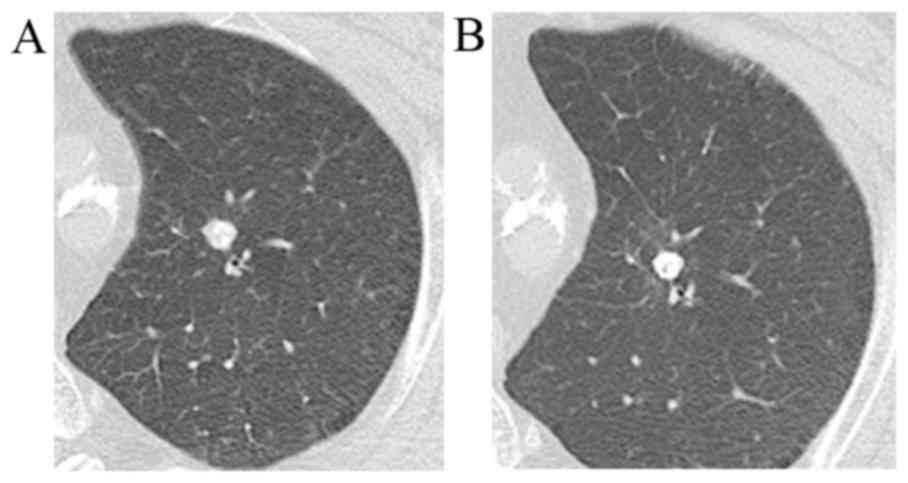
postoperative chemotherapy was administered. A solitary lung
metastasis appeared 6 months after resection of the recurrent tumor
(Fig. 5A), and stereotactic
radiotherapy (SRT; 60 Gy/4 fractions/5 days) was delivered to the
lung metastasis. There were no complications, such as radiation
pneumonitis, after SRT. Since the metastatic pulmonary lesion did
not increase in size for 2 years after SRT, the lesion was
considered to have undergone scarification by SRT (Fig. 5B). The patient had no evidence of
local recurrence or new distant metastasis for 2 years after the
second surgery at the latest follow-up date of May 14, 2018.
Discussion
ESOS mostly arises in deep soft tissues. The
superficial subcutaneous tissue is rarely involved, accounting for
<10% of ESOS cases (1). A PubMed
search was performed to identify cases of ESOS arising in
subcutaneous tissues. The search term was ‘extraskeletal
osteosarcoma AND subcutaneous’. A total of 34 papers were
identified, only 10 of which reported the clinical characteristics
of primary subcutaneous ESOS in detail (3,5–13). A total of 17 cases were included in
these 10 papers. The clinical characteristics of the 17 cases and
the case presented herein are summarized in Table I. These cases were of primary ESOS
arising in subcutaneous tissue, rather than occurring secondarily
at the site of trauma or radiotherapy. The mean age of the 18 cases
was 56.3 years (range, 15–80 years). Although ESOS is common in the
fifth to seventh decades of life at diagnosis (1), 30% of cases of subcutaneous ESOS were
aged <40 years (6,9,11,12).
Subcutaneous ESOS may develop in younger adults compared with
deep-seated ESOS. The 18 patients included 9 men and 9 women. The
mean tumor size of the 18 subcutaneous ESOS cases was 4.95 cm
(range, 1.5–15 cm), and 11 tumors (61%), including the present
case, were <5 cm in greatest dimension (3,6–9,12,13). In
the largest series of ESOS cases (n=266), ~80% were tumors sized
>5 cm (14). Generally, it is
considered that ESOS are >5 cm, but since subcutaneous ESOS are
located more superficially, a number of patients may visit the
hospital for the first time while the tumor is relatively small.
The sites of tumor origin were non-extremities in 10 cases and
extremities in 8 cases (6 lower and 2 upper extremities). Although
the majority of ESOS cases were reported to involve the extremities
(14), subcutaneous ESOS may also
involve the trunk.
 | Table I.Clinical characteristics of primary
subcutaneous extraskeletal osteosarcomas. |
Table I.
Clinical characteristics of primary
subcutaneous extraskeletal osteosarcomas.
| Author, year | Age (years), sex | Location | Size (cm) | Method of biopsy | Treatment | Histological
subtype | MIB1- LI (%) | Recurrence | Metastasis | Outcome | Follow-up time
(months) | Refs. |
|---|
| Frang et al,
1995 | 59, F | Abdominal wall | 15 | None | WR | ND | ND | – | – | CDF | 187 | (5) |
| Dubec et al,
1997 | 71, F | Lower leg | 5.5 | Needle | WR (amputation) | TA | ND | – | – | CDF | 10 | (7) |
|
| 75, F | Lower leg | 2.5 | Needle | CT, WR | TA | ND | – | – | CDF | 12 |
|
| Lidang Jensen et
al, 1998 | 39, F | Shoulder | 4 | ND | WR, RT, CT | OB | 23 | – | – | CDF | 162 | (6) |
|
| 40, M | Scapula | 6 | ND | WR | OB | 24 | ND | ND | DOD | 35 |
|
|
| 35, M | Chest | 2.8 | ND | WR, CT | OB | 21 | – | – | CDF | 5 |
|
|
| 79, F | Scapula | 2 | ND | WR | OB | 19 | ND | ND | DOD | 11 |
|
|
| 75, M | Shoulder | 8 | ND | WR | OB | 28 | ND | ND | DOC | 54 |
|
|
| 50, M | Axilla | 1.5 | ND | WR | OB | 26 | – | – | CDF | 7 |
|
|
| 73, M | Scapula | 10 | ND | RT | FB | 15 | ND | ND | DOC | 7 |
|
| Oonuma et
al, 2001 | 55, F | Buttock | 1 |
Excisionala | WRa, CT | GC | ND | – | – | CDF | 48 | (8) |
| Hatano et
al, 2005 | 25, M | Jaw | 1.5 | Excisional | CT, WR | ND | ND | – | – | CDF | 16 | (9) |
| Nakamura et
al, 2011 | 79, M | Upper arm | 4 | None | WR | GC | ND | – | – | CDF | 12 | (3) |
| Papachristou et
al, 2012 | 54, M | Lower leg | 8 |
Excisionala | CT, WRa | GC | ND | – | Lung | AWD | 12 | (10) |
| Sarsilmaz et
al, 2012 | 31, F | Lower leg | 8 | Needle | CT, WR, RT | ND | ND | – | – | CDF | 60 | (11) |
| Zreik et al,
2016 | 15, F | Thigh | 2.8 | Core | RT, WR | OB | ND | – | – | CDF | 9 | (12) |
| Healy et al,
2016 | 80, F | Forearm | 1.5 | Excisional | WR | ND | 60 | + | – | CDF | 36 | (13) |
| Present case | 79, M | Lower leg | 5 |
Excisionala | WRa | CB | 35 | – | Lung | AWD | 36 |
|
A preoperative diagnosis of subcutaneous ESOS was
made in 9 patients; 2 cases were not diagnosed preoperatively; and
there was no description in 7 cases. The preoperative diagnostic
methods for 9 patients were 5 excisional biopsies, 3 needle
biopsies and 1 core biopsy. With ESOS originating in the
subcutaneous tissue rather than intramuscularly, the tumor is thin,
and needle biopsy is difficult, even if the long axis is large.
Therefore, excisional biopsy is often performed. Even in the
present case, since the long diameter was 5 cm, but the thickness
was only 2 cm, excisional biopsy was performed, and the diagnosis
was obtained.
Similar to ESOS occurring in the deep soft tissue,
wide resection is also the gold standard of treatment for
subcutaneous ESOS (13). The
effectiveness of neoadjuvant or adjuvant chemotherapy for ESOS is
controversial. Treatment of subcutaneous ESOS includes surgery,
chemotherapy or radiotherapy (RT), alone or in combination
(3,6,11). Wide
resection was performed in all but one of the 18 reported cases,
including the present case. In the one case that did not undergo
surgery, no chemotherapy was administered, and the patient only
received RT (6). Chemotherapy was
performed in 7 (38.9%) of the 18 patients, 4 of whom received
neoadjuvant chemotherapy and 3 postoperative adjuvant chemotherapy.
RT as adjuvant therapy was performed in only 3 cases. A recent
study of ESOS with the largest number of cases reported that the
5-year disease-free survival and overall survival (OS) were
significantly better in patients treated with chemotherapy compared
with those not administered chemotherapy, with a 5-year OS rate of
62 and 38%, respectively (14).
Although the number of ESOS patients was small, it was reported
that the effect of chemotherapy was limited. Fan et al
reported that chemotherapy with doxorubicin and ifosfamide had a
positive effect on local recurrence for patients with stage III
disease, but had no effect on disease-specific survival (15). The outcome of patients with
subcutaneous ESOS was continuously disease-free (CDF) or alive with
disease (AWD) in 14 patients [7 who received chemotherapy (6–11) and 7
who did not (3,5–7,12,13];
thus, the effectiveness of chemotherapy remains unclear. Further
investigation of the usefulness of chemotherapy is required.
RT was performed in 4 patients (22%). RT was
administered postoperatively in 2 cases, preoperatively in 1 case
and palliatively in 1 case. The role of adjuvant RT for ESOS is
debatable. Choi et al reported that there was no significant
difference in disease-free survival between patients treated and
those not treated with radiation (16). Longhi et al also reported that
RT for ESOS decreased the incidence of local relapse for patients
with tumors sized >5 cm and R0 margins, but no significant
difference in local relapse rate was observed for patients with
tumors >5 cm and R1 margins (14). However, RT for patients with stage
III (>5 cm) exerted a positive effect on local control, but not
on disease-specific survival (15).
In the present review of subcutaneous ESOS, since the number of
patients who received RT was small, its effectiveness is unclear.
In the present case, postoperative adjuvant chemotherapy was not
performed due to the patient's age. In addition, the patient did
not receive postoperative adjuvant RT, as the histopathological
assessment of the resected recurrent tumor was R0.
ESOS tends to cause local recurrence and distant
metastases, and localized ESOS is reported to relapse in 40–50% of
the cases (4,14,16).
Choi et al reported that the local recurrence rate was 19%
and that of distant metastatic recurrence 38.1% among patients with
localized ESOS, all of whom had lung metastasis (16). Longhi et al also reported that
the local recurrence rate was 24.6%, and that the distant
metastatic recurrence rate was 41.7% among patients with localized
ESOS (14). In the present review,
only 1 case developed local recurrence 8 months after surgery
(13). In these subcutaneous ESOS
series, the local recurrence rate was 5.6%, which was lower than
the recurrence rate of previous ESOS cases. Furthermore, distant
metastasis was confirmed in 2 cases (11.1%) of subcutaneous ESOS
[case reported in (10) and the
present case], and its frequency was low compared with the
frequency of distant metastasis in previous ESOS cases. The reports
with larger numbers of cases with localized ESOS demonstrated that
the 5-year survival rate was relatively poor, ~50–60% (4,14,16).
Thus far, only few reports have examined the prognosis of ESOS
separately for ESOS cases occurring in subcutaneous tissue and
those in deep tissue. In this review of patients with subcutaneous
ESOS, the outcome at the final follow-up observation was relatively
good: CDF in 13, AWD in 1, dead of disease in 1, and dead of other
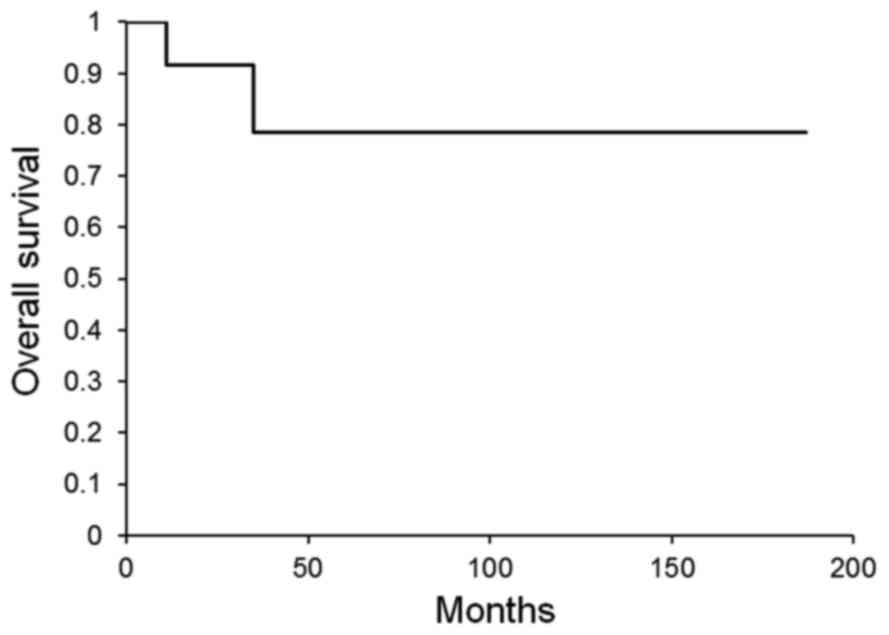
cause (DOC) in 2. The 5-year survival rate was calculated by the
Kaplan-Meier method for 16 patients, excluding 2 DOC cases, among
the subcutaneous ESOS cases reviewed. The 5-year survival rate of
patients with subcutaneous ESOS was 78.6%, which was better
compared with that of the previous ESOS cases (Fig. 6). To the best of our knowledge, this
is the first report of the survival rate only for subcutaneous ESOS
cases, and the prognosis may be better for subcutaneous ESOS rather
than for deep-seated ESOS. There are a few reports on the
prognostic factors for ESOS. Thampi et al reported that
adverse prognostic factors on multivariate analysis were axial
tumor site and larger tumor size (≥10 cm) (4). Choi et al also demonstrated that
the prognostic factors for event-free survival of localized ESOS
were significantly associated with the tumor being located
superficially and having achieved R0 resection (16). The MIB-1 labeling index evaluated by
immunohistochemical staining using Ki-67 was also reported to be a
prognostic factor associated with survival, and it was estimated
that a value of <24% would reflect a good prognosis (6). The mean MIB-1 labeling index with
subcutaneous ESOS was 24% (range, 15–60%, n=9). The MIB-1 labeling
index of the present case was 35%, which was higher than the mean
in the subcutaneous ESOS series. This value of the MIB-1 labeling
index corresponds to a poor prognostic factor for previous ESOS
cases, but our patient has survived for 3 years as CDF.
Subcutaneous ESOS is considered to be highly
malignant histopathologically (1),
but it is rare for a superficial tumor to invade into the deep
tissue, and it is often found at a size of ≤10 cm, so that wide
resection can be performed; thus, the prognosis of subcutaneous
ESOS is considered to be better compared with that of ESOS arising
from deeper tissues. Therefore, further information on the
necessity of chemotherapy and the prognosis of subcutaneous ESOS is
required.
In summary, a new case of ESOS arising in the
subcutaneous tissue of the lower leg was reported. The diagnosis of
subcutaneous ESOS was made by excisional biopsy, and wide resection
was performed at the time of tumor recurrence. The tumor was 5 cm
in greatest dimension, and the MIB-1 labeling index was 35%.
Although the patient developed a solitary lung metastasis, the
lesion was successfully controlled by SRT without chemotherapy, and
the patient survived for 3 years as CDF. Furthermore, the previous
subcutaneous ESOS cases were reviewed herein, focusing on the
clinical characteristics, MIB-1 labeling index and outcomes.
Patients with subcutaneous ESOS may have a better prognosis
compared with those with ESOS arising from deeper soft tissue,
although the mean MIB-1 labeling index of subcutaneous ESOS was
24%.
Acknowledgements
The authors are grateful to Professor Joji Imura,
Department of Pathology, University of Toyama (Toyama, Japan), for
discussion of histopathological diagnosis.
Funding
The present study was supported by the Japan Society
for the Promotion of Science (JSPS; grant no. JP17K16681).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
TT and KS made substantial contributions to the
conception and design. TY was responsible for the acquisition or
analysis and interpretation of data. KW provided advice on the data
analysis. KS, TY and SN were involved in surgical treatment. MK and
TK were involved in drafting the manuscript or revising it
critically for important intellectual content. KS made a critical
revision of the article for important intellectual content. All
authors have read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
This report was approved by the Ethics Committee of
the University of Toyama (Toyama, Japan), and clinical research
number ‘21-22’ was granted.
Patient consent for publication
Written informed consent was obtained from the
patient for publication of this report and accompanying images. A
copy of the written consent is available for review upon
request.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
ESOS
|
extraskeletal osteosarcoma
|
|
MRI
|
magnetic resonance imaging
|
|
CT
|
computed tomography
|
|
FDG-PET
|
F-18 2-fluoro-2-deoxy-glucose positron
emission tomography
|
|
SUV
|
standardized uptake value
|
|
SRT
|
stereotactic radiotherapy
|
|
OS
|
overall survival
|
|
CDF
|
continuously disease-free
|
|
AWD
|
alive with disease
|
|
RT
|
radiotherapy
|
|
DOC
|
died of other cause
|
References
|
1
|
Rosenberg AE: Extraskeletal
osteosarcomaWHO classification of tumours of soft tissue and bone.
Fletcher CDM, Bridge JA, Hogendoorn PCW and Mertens F: IARC; Lyon:
pp. 161–162. 2013
|
|
2
|
Chung EB and Enzinger FM: Extraskeletal
osteosarcoma. Cancer. 60:1132–1142. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Nakamura T, Matsumine A, Nishimura K,
Yokoyama H, Murata T, Uchida A and Sudo A: Extraskeletal
subcutaneous osteosarcoma of the upper arm: A case report. Oncol
Lett. 2:75–77. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Thampi S, Matthay KK, Boscardin WJ,
Goldsby R and DuBois SG: Clinical features and outcomes differ
between skeletal and extraskeletal osteosarcoma. Sarcoma.
2014:9026202014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Fang Z, Yokoyama R, Mukai K, Beppu Y and
Fukuma H: Extraskeletal osteosarcoma: A clinicopathologic study of
four cases. Jpn J Clin Oncol. 25:55–60. 1995.PubMed/NCBI
|
|
6
|
Jensen Lidang M, Schumacher B, Jensen
Myhre O, Nielsen Steen O and Keller J: Extraskeletal osteosarcomas:
A clinicopathologic study of 25 cases. Am J Surg Pathol.
22:588–594. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Dubec JJ, Munk PL, O'Connell JX, Lee MJ,
Janzen D, Connell D, Masri B and Logan PM: Soft tissue osteosarcoma
with telangiectatic features: MR imaging findings in two cases.
Skeletal Radiol. 26:732–736. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Oonuma M, Hatori M, Hosaka M and Kokubun
S: Extraskeletal osteosarcoma arising in the buttock. Ups J Med
Sci. 106:211–215. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hatano H, Morita T, Kobayashi H, Ito T,
Segawa H and Hasegawa S: Extraskeletal osteosarcoma of the jaw.
Skeletal Radiol. 34:171–175. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Papachristou DJ, Goodman M, Cieply K and
Rao UN: Extraskeletal osteosarcoma of subcutaneous soft tissue with
lymph node and skin metastasis: A case report with fluorescence in
situ hybridization analysis. Pathol Oncol Res. 18:107–110. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Sarsilmaz A, Argin M, Sezak M, Altay C and
Erdogan N: Primary osteosarcoma arising from subcutaneous tissue:
5-year follow-up. Clin Imaging. 36:402–405. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zreik RT, Meyer RG, Jenkins RB, Norambuena
GA and Fritchie KJ: A rare pediatric example of subcutaneous
extraskeletal osteosarcoma: A case report and review of the
morphologic differential diagnosis. Am J Dermatopathol. 38:e44–e48.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Healy C, Kahn LB and Kenan S: Subcutaneous
extraskeletal osteosarcoma of the forearm: A case report and review
of the literature. Skeletal Radiol. 45:1307–1311. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Longhi A, Bielack SS, Grimer R, Whelan J,
Windhager R, Leithner A, Gronchi A, Biau D, Jutte P, Krieg AH, et
al: Extraskeletal osteosarcoma: A European Musculoskeletal Oncology
Society study on 266 patients. Eur J Cancer. 74:9–16. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Fan Z, Patel S, Lewis VO, Guadagnolo BA
and Lin PP: Should high-grade extraosseous osteosarcoma be treated
with multimodality therapy like other soft tissue sarcomas? Clin
Orthop Relat Res. 473:3604–3611. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Choi LE, Healey JH, Kuk D and Brennan MF:
Analysis of outcomes in extraskeletal osteosarcoma: A review of
fifty-three cases. J Bone Joint Surg Am. 96(e2): 1–8.
2014.PubMed/NCBI
|