Introduction
Benign prostatic hyperplasia (BPH), also commonly
termed benign prostatic hypertrophy, can be described clinically or
pathologically. Clinical BPH presents as benign enlargement of the
prostate, which contributes to an array of voiding difficulties
that can range from bothersome to significantly impacting quality
of life in older men (1). Due to
the high prevalence of BPH in elderly men, BPH has been suggested
to be a ubiquitous sign of aging (2). The concept that androgens are
important for the maintenance of prostate disease dictates the
standard of care for BPH (3).
Although aging and androgens are two established factors that
contribute to the development of BPH, recent novel findings
highlight the importance of inflammation (4). Upon histological examination, almost
all BPH specimens exhibit inflammatory infiltrates; however, the
link to bacterial or other foreign antigens remains to be
elucidated. Auto-reactive T cells recognize prostate secretion
products and animal models of experimental prostatitis have
demonstrated an autoimmune component of chronic inflammation
(5). Therefore, reducing
inflammation may serve a crucial role in the treatment of BPH and
may lead to improved clinical outcomes. Various types of
pharmaceutical therapies are in use for the treatment of BPH,
including alternative herbal-based therapies (6). Typical herbal therapies recommended
for BPH with certain clinical evidence of efficacy include saw
palmetto (Serenoa repens), stinging nettle (Urtica
dioica) and Pygeum africanum (7). Bee pollen extract (cernilton) has
also been used; however, less evidence of its efficacy against BPH
exists. Lower urinary tract symptoms provide a complex but common
connection between BPH and chronic prostatitis. Therefore,
alternative agents can be used alone or in combination for
treatment of BPH.
The herbal liquor, musulju (MSJ), has been
traditionally used in Korean medicine to strengthen virility. The
Korean medicine book called the Dongui Bogam reported MSJ to be
effective in elderly men for alleviating urinary system
dysfunction. Although MSJ may be a potential therapeutic for BPH,
the molecular mechanisms supporting its clinical claims remain
elusive. Therefore, to understand the mechanisms underlying its
clinical effect, the present study evaluated the anti-proliferative
effect of MSJ and determined the molecular mechanisms of MSJ in a
testosterone-induced rat model of BPH.
Materials and methods
Chemicals and reagents
Testosterone, phenylmethylsulfonyl fluoride,
Triton-X-100 and the protein inhibitor cocktail were purchased from
Sigma-Aldrich (St. Louis, MO, USA). Finasteride, a type II
5-reductase inhibitor, was obtained from Merck & Co., Inc.
(Whitehouse Station, NJ, USA). 5α-Reductase 2 and
glyceraldehyde-3-phosphate dehydrogenase (GAPDH)
oligonucleotide primers were purchased from Bioneer Corporation
(Daejeon, Republic of Korea), and SYBR Premix Ex Taq was purchased
from Takara Bio., Inc. (Otsu, Japan). Antibodies against inducible
nitric oxide synthase (iNOS; M-19; cat. no. sc-650), cyclooxygenase
2 (COX-2; C-20; cat. no. sc-1745), poly (ADP-ribose) polymerase-1
(PARP-1; F-2; cat. no. sc-25780), caspase-3 (E-8; cat. no.
sc-7272), Bcl-2 (C-2; cat. no. sc-7382), Bcl-xL (H-5; cat. no.
sc-8392), Bax (B-9; cat. no. sc-7480) and β-actin (ACTBD11B7; cat.
no. sc-81178) were purchased from Santa Cruz Biotechnology, Inc.
(Dallas, TX, USA). An antibody for proliferating cell nuclear
antigen (PCNA; cat. no. sc-56) was purchased from BD Biosciences
(San Jose, CA, USA). Horseradish peroxidase-conjugated secondary
antibody was purchased from Jackson ImmunoResearch Laboratories,
Inc. (West Grove, PA, USA).
Preparation of MSJ. The muscle of
Canis familiaris L
(1.5 kg) was purchased from the Moran traditional
market, (Sung-nam, Korea), and it was cleansed. It was boiled for
24 h and the oil, which forms on the top, was removed. It was
subsequently mixed with hard-steamed glutinous rice (24 kg) and
malt made of barley flour (120 g), and it was brewed for 14 days.
MSJ was filtered through Whatman No. 1 filter paper and the
filtrate was evaporated to dryness under reduced pressure on an
EYELAN-1000 rotary evaporator (EYELA Riakikai Co., Ltd, Tokyo,
Japan) at 40°C. Finally, MSJ extracts were obtained and stored at
−20°C for later use.
Animals
Male Wistar rats (n=24; 10-weeks-old; weight, 200±20
g) were purchased from Daehan Biolink (Daejeon, Korea). The animals
were housed under conditions specified in the guide for the Care
and Use of Laboratory Animals, as adopted and promulgated by the
Institutional Animal Care Committee, Sangji University (Reg. no.
2014-08; Wonju-si, Korea). Prior to the start of the experiment,
the rats were adapted to the modified conditions for 2 weeks. Rats
were randomly distributed into four groups (n=6/group): i)
Sham-operated group (Con); ii) BPH model group (BPH); iii)
finasteride-administrated group (Fina); and iv) Musulju-treated
group (MSJ). The rats were castrated, with the exception of those
in the Con group, and BPH was induced in castrated animals by
subcutaneous injection of testosterone, as described previously
(8). Throughout the experiment,
the animals were provided free access to food and water for 4
weeks, and they were maintained under a 12 h light/dark cycle at a
constant temperature of 22±2°C with a relative humidity of 55±9%.
At the end of the 4-week period, the body weight of the rats was
recorded and all animals were fasted for 12 h. The following day,
the rats were sacrificed by anesthesis with Zoletil® 50
(intraperitoneal, 20 mg/kg; Virbac, CarrosCedex, France), and blood
samples were collected by cardiac puncture. The prostatic tissue
was excised, rinsed, weighed and stored at −70°C until further
analysis.
Administration and dosage
Testosterone propionate (Wako Pure Chemical
Industries, Ltd., Osaka, Japan) was diluted with corn oil and
injected subcutaneously (10 mg/kg) into rats in the BPH, Fina and
MSJ groups to induce BPH (9,10).
Finasteride (Merck & Co., Inc.) and MSJ were dissolved in
distilled water. Fina and MSJ were orally administered at a dose of
5 and 200 mg/kg, respectively.
Prostate weight to body weight ratio
(PW/BW)
Prostatic tissues were excised, rinsed and weighed
immediately after removal. The PW/BW ratio was calculated using the
following equation: PW/BW ratio = (prostate weight of each animal
from experimental group / body weight of each animal from
experimental group) × 1,000.
Growth inhibition of prostate
weight
The percentage of growth inhibition was calculated
as follows: 100 - [(treated group - control group) / (BPH group -
control group) × 100].
Serum concentrations of testosterone
analysis
The serum concentrations of testosterone were
determined using commercial enzyme linked immunosorbent assay
(ELISA) kits (Cayman Chemical Company, Ann Arbor, MI, USA). The
assays were performed according to the manufacturer's protocol.
Histological analysis
The prostatic tissue in each group was fixed in 4%
formalin, embedded in paraffin and the tissue was then cut into
4-µm sections. The sections were stained with hematoxylin and eosin
for histological examination. Images were captured using a SZX10
microscope (Olympus Corporation, Tokyo, Japan). The thickness of
epithelium tissue from prostate (TETP) was measured using Leica
Application Suite (ver.3.3.0) software (Leica Biosystems, Wetzlar,
Germany) for histological analysis.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
The prostatic tissue from each animal was
homogenized and the total RNA was isolated using
Easy-Blue® reagent (iNtRON Biotechnology, Inc.,
Gyeonggi-do, Republic of Korea), according to the manufacturer's
protocol. The total RNA was quantified using an Epoch®
microvolume spectrophotometer system (BioTek Instruments, Inc.,
Winooski, VT, USA). Total RNA from the prostate was reverse
transcribed into cDNA using a high-capacity cDNA reverse
transcription kit (Life Technologies, Grand Island, NY, USA). PCR
amplification was performed with the incorporation of SYBR green
(Life Technologies; Thermo Fisher Scientific, Inc., Waltham, MA,
USA). The oligonucleotide primers for designed from rat were as
follows: 5α-reductase 2, forward: 5′-ATGGGGACCCTGATCCTGTG-3′ and
reverse: 5′-CGACACCACAAAGGAAGGCA-3′; GAPDH, a housekeeping
gene, forward: 5′-TGATTCTACCCACGGCAAGT-3′ and
5′-AGCATCACCCCATTTGATGT-3′. RT was performed with a thermo cycler
(Gene Amp® PCR system 9700; Life Technologies; Thermo
Fisher Scientific, Inc.) and the results were expressed as the
ratio of optimal density against that of GAPDH.
Western blot analysis
The prostatic tissue from each animal was
homogenized in PRO-PREP® lysis buffer (iNtRON
Biotechnology, Inc., Seoul, South Korea) and incubated for 25 min
on ice to induce cell lysis. Tissue extracts were centrifuged at
13,000 rpm (4°C) for 20 min and the supernatants were transferred
to clean tubes. Aliquots of each protein sample (30 µg) were
resolved on 8–12% sodium dodecyl sulfate-polyacrylamide gel
electrophoresis gels and were transferred onto a polyvinylidene
fluoride membrane. The membranes were incubated for 1 h with
blocking solution and were subsequently incubated with a 1:1,000
dilution of primary antibodies, including anti-PCNA, anti-iNOS,
anti-COX-2, anti-PARP-1, anti-caspase-3, anti-Bcl-xL, anti-Bax, and
anti-β-actin, overnight at 4°C. The membranes were washed three
times with 0.1% Tween-20/TBS, followed by incubation with the
corresponding secondary antibodies (1:2,000 dilution) for 1 h at
room temperature. The membranes were washed as before, and the
immunoreactive protein bands were visualized using enhanced
chemiluminescence and exposure to X-ray film (GE Healthcare
Bio-Sciences, Piscataway, NJ, USA). Density of protein band was
measured using Bio-Rad Quantity One Software (version 4.6.3;
Bio-Rad Laboratories, Inc., Hercules, CA, USA).
Statistical analysis
The data are expressed as the mean ± standard error
of the mean of 6 rats. The data were analyzed by one-way analysis
of variance with Dunnett's test. Statistical analysis was performed
using SPSS version 19.0 (IBM Corporation, Armonk, NY, USA).
Results
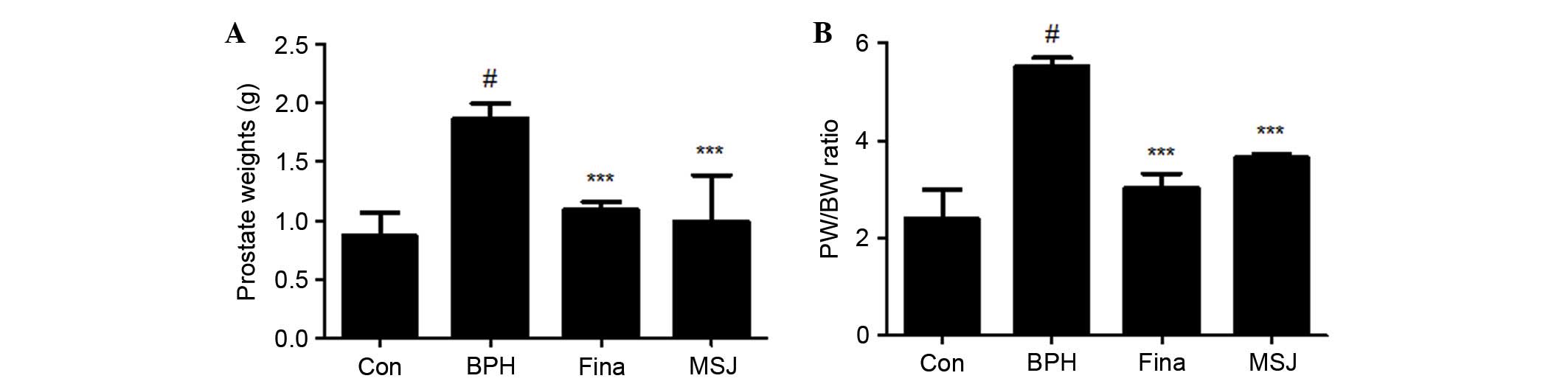
Effects of MSJ on prostate weight in
BPH model rats
As shown in Fig.
1A, the mean prostate weight of rats in the BPH group was
significantly higher compared with that of rats in the other
groups, suggesting that testosterone successfully induced BPH in
the castrated rats. The prostate weight of the rats in the Fina and
MSJ groups significantly decreased compared with that of rats in
the BPH group (Fig. 1A). The
prostate weight in the BPH-induced group was 2.16-fold higher
compared with that of the Con group. In the Fina and MSJ groups,
the prostate weights were 1.25- and 1.14-fold higher, respectively,
compared with the Con group. In addition, the PW/BW ratio in BPH
group was 2.31-fold higher compared with that in the Con group
(Fig. 1B). The PW/BW ratios in the
Fina and MSJ groups were 1.26- and 1.53-fold higher, respectively,
compared with that in the Con group. In addition, the growth
inhibition ratio of prostate growth in each group is demonstrated
in Table I. In the Fina and MSJ
groups, the prostate growth inhibition ratio was recorded to be
almost 85% and 68%, respectively.
 | Table I.Effect of treatments on prostate
growth in rats treated with testosterone. |
Table I.
Effect of treatments on prostate
growth in rats treated with testosterone.
| Group | Prostate weight
(g) | Inhibition ratio
(%) |
|---|
| Control | 0.87±0.20 | – |
| BPH |
1.87±0.13a | – |
| Finasteride |
1.09±0.07b | 85.34 |
| MSJ |
0.99±0.39b | 68.26 |
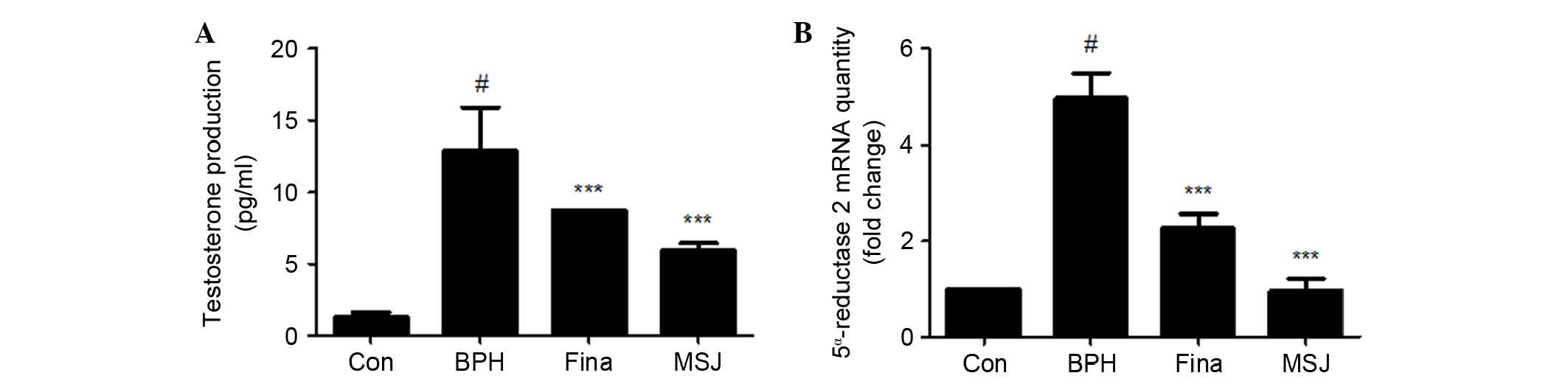
Effects of MSJ on serum testosterone
levels and 5α-reductase 2 mRNA expression in BPH model rats
Circulating testosterone acts locally in the
prostate via production of growth factors that act in an autocrine
or a paracrine manner to influence prostate cell growth, survival
or apoptosis (11). As shown in
Fig. 2A, serum testosterone levels
in the testosterone-induced BPH group (12.88±3.00 pg/ml) were
significantly higher compared with that in the Con group (1.28±0.36
pg/ml). However, serum testosterone levels in the Fina group
(8.70±0.00 pg/ml) and the MSJ group (5.93±0.51 pg/ml) significantly
decreased compared with that in the BPH group. In the prostate,
testes and hair follicles, circulating testosterone is converted by
5α-reductase to dihydrotestosterone (DHT), which serves a key role
in the development of male reproductive organs, and these hormones
are commonly associated with BPH (12). To determine if the effect of MSJ
was associated with the synthesis of DHT from testosterone by
5α-reductase, the present study examined the mRNA expression levels
of 5α-reductase 2 in prostatic tissue. As shown in Fig. 2B, similar to the results in the
Fina group, MSJ treatment significantly decreased
testosterone-induced mRNA expression of 5α-reductase 2 in
the prostate tissue compared with that in the BPH group.
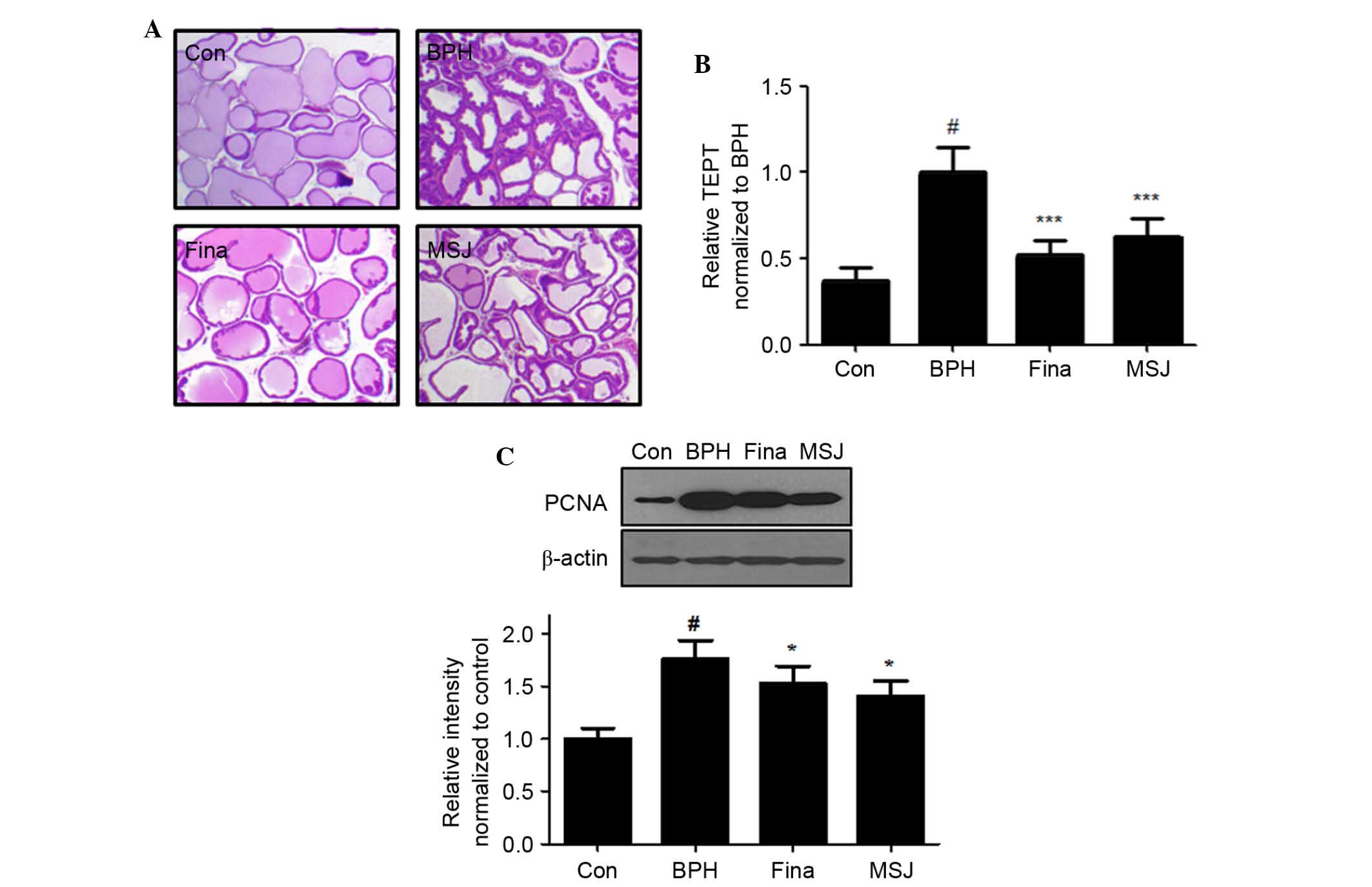
Effects of MSJ on histological
parameters and cell proliferation in BPH model rats
Histological analysis revealed changes in
characteristics of glandular hyperplasia with epithelial
proliferation and decreased glandular luminal area in the BPH model
rats (Fig. 3A). However, Fina and
MSJ treatment suppressed these typical hyperplastic patterns, which
represent the histological change of normal prostatic tissue into
tissue with prostatic hyperplasia. As shown in Fig. 3B, TETP analysis revealed that the
thickness of the epithelium tissue was maximal in rats in the BPH
group and that Fina and MSJ treatment significantly reduced the
thickness of the epithelium tissue of the prostate.
In order to evaluate the effects of MSJ on the
proliferation of prostatic epithelial cells, the present study
examined the protein expression levels of PCNA, a proliferation
marker, in the prostatic tissue of BPH model rats. As shown in
Fig. 3C, PCNA protein levels, as
detected by western blotting, increased in the BPH group relative
to the levels in the Con group. Compared with the BPH group,
however, the Fina and MSJ groups exhibited a slight increase in the
protein levels of PCNA, consistent with the antiproliferative
effects in BPH.
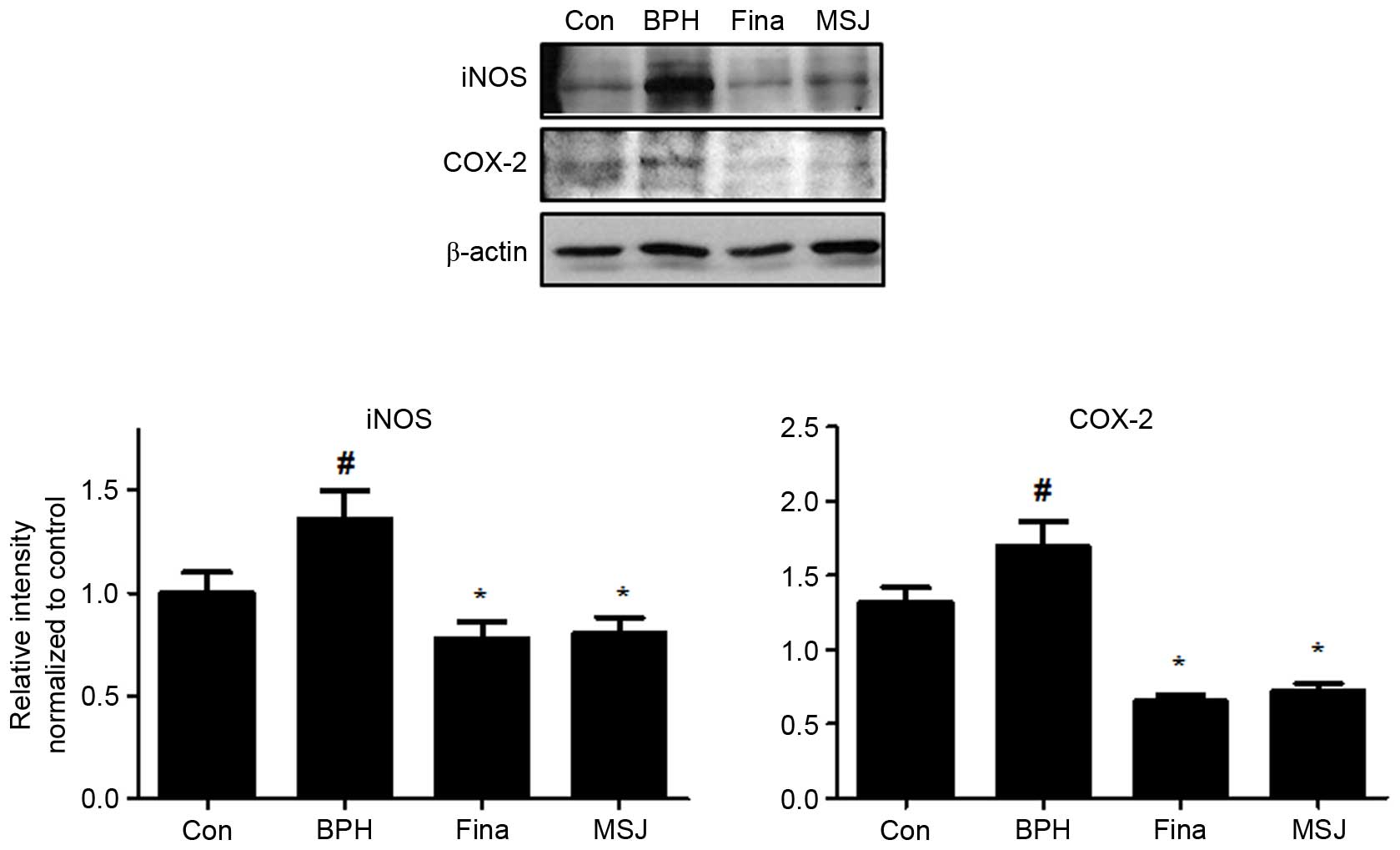
Effects of MSJ on inflammatory
proteins in BPH model rats
Inflammatory factors serve a crucial role in
proliferation of prostatic cells in BPH. As shown in Fig. 4, treatment with testosterone
markedly increased the protein expression levels of iNOS and COX-2
in the BPH group compared with that of the control group. The Fina
and MSJ groups, however, exhibited reduced expression levels of
these inflammatory proteins.
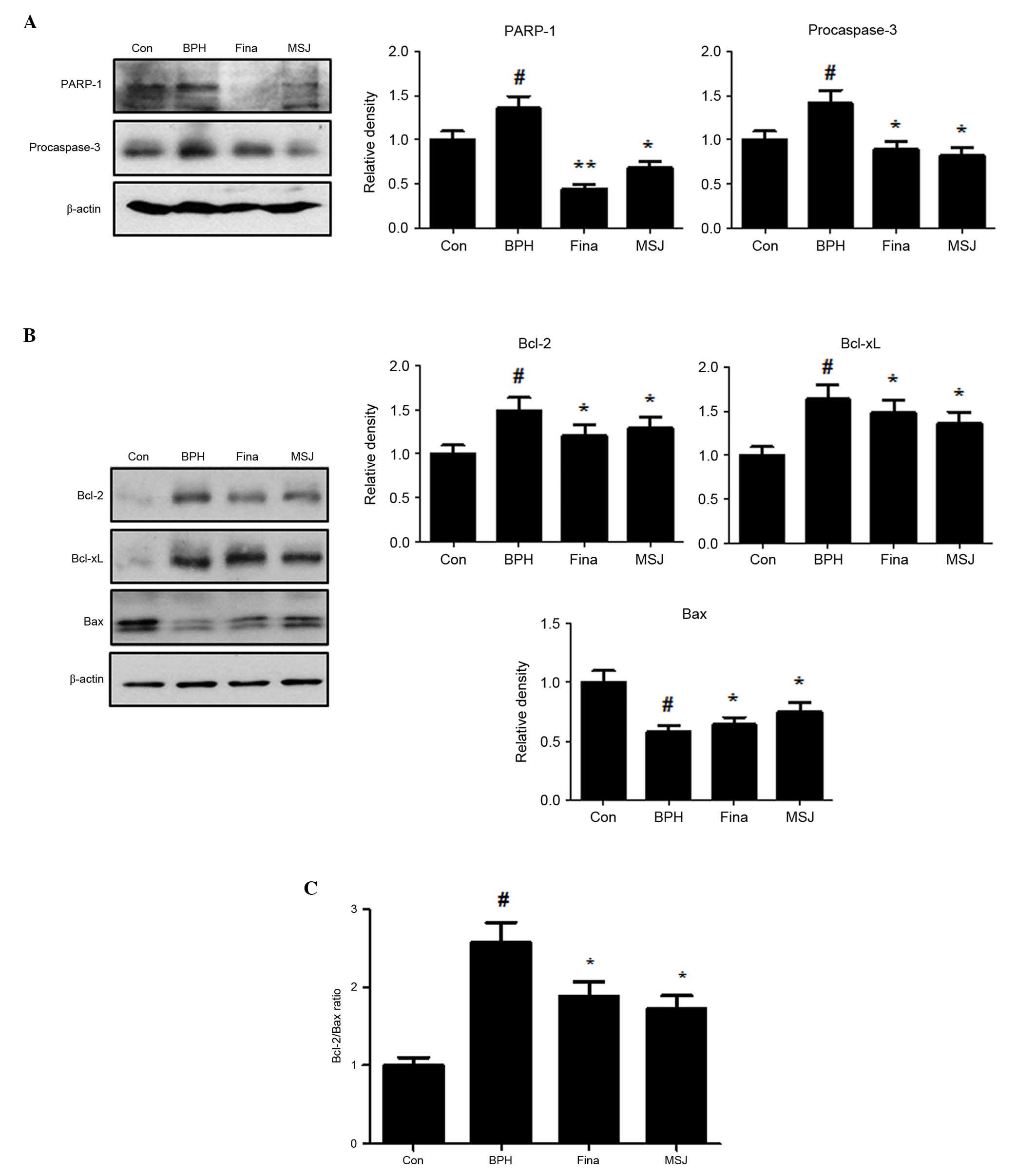
Effects of MSJ on apoptotic proteins
in BPH model rats
Apoptotic activity has been suggested to be a key
cofactor in the development and progression of BPH. In the present
study, treatment with testosterone upregulated the protein
expression levels of PARP-1 and procaspase-3 in the BPH group
(Fig. 5A). Treatment with MSJ,
however, markedly suppressed the protein expression levels of
PARP-1 and procaspase-3, suggesting the involvement of
caspase-mediated apoptotic pathways in BPH. In addition, the
MSJ-treated group exhibited decreased levels of the antiapoptotic
proteins, Bcl-2 and Bcl-xL, but increased expression of
proapoptotic Bax compared with the BPH group (Fig. 5B). Therefore, the ratio of Bcl-2 to
Bax significantly decreased following treatment with MSJ, which
suggested a role of the Bcl-2 family of proteins (Fig. 5C), an important mediator of the
intrinsic apoptotic pathway, in MSJ-induced apoptosis in the BPH
model. Therefore, MSJ-induced apoptosis was mediated by the
regulation of the expression levels of the caspase and Bcl-2 family
proteins.
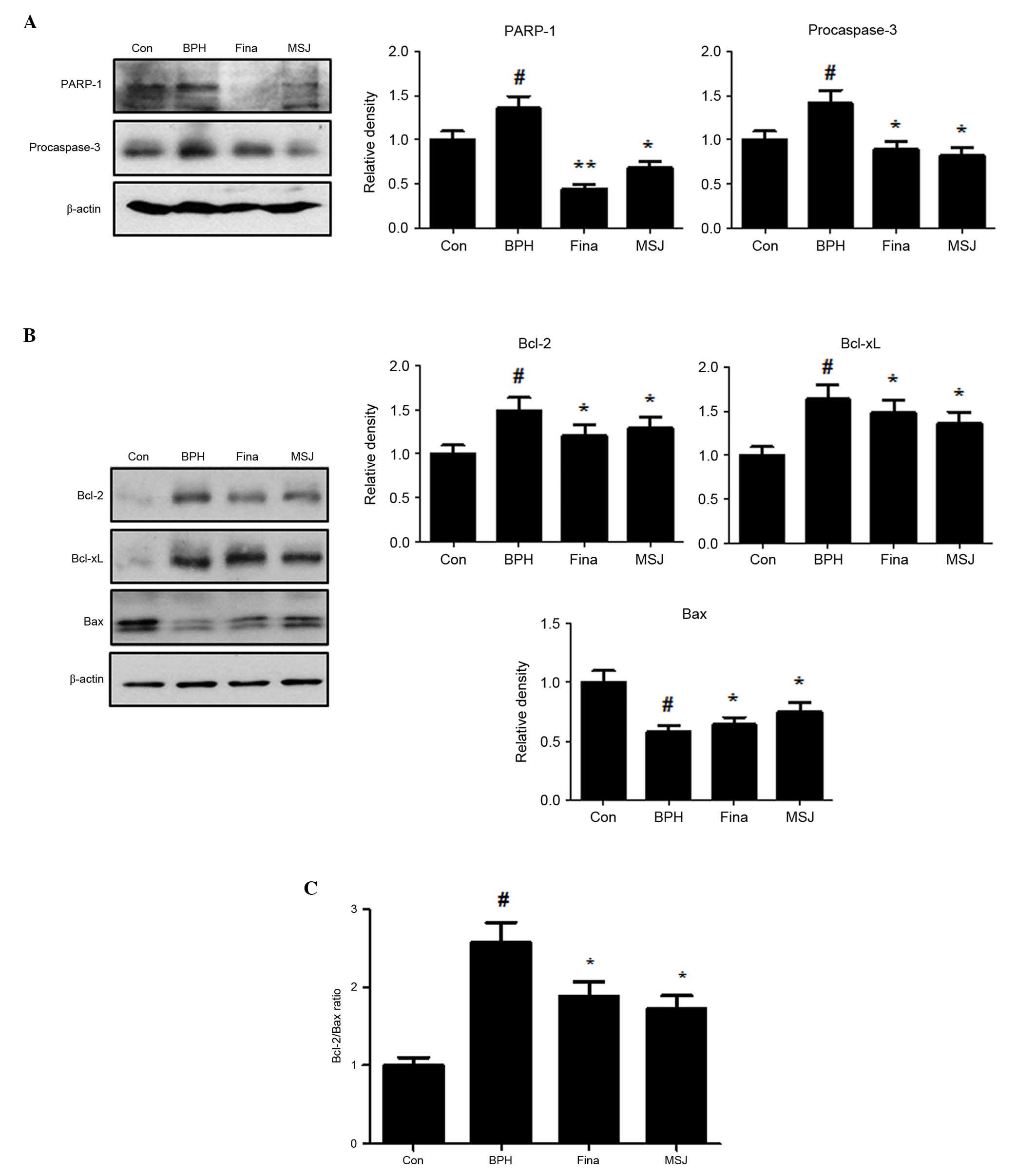 | Figure 5.Effect of MSJ administration on the
expression of apoptosis-related proteins in prostate tissues of
BPH-induced rat models. (A) The expression levels of (A) PARP-1 and
procaspase-3, and (B) Bcl-2 family were determined by western
blotting using specific antibodies. β-actin was used as internal
controls. The protein band densities were determine by
densitometric analysis. (C) The densitometric analysis of Bcl-2 and
Bax bands was performed, and the data were plotted as the Bcl-2/Bax
ratio. Densitometric analysis was performed using Bio-rad Quantity
One® Software. The data are presented as the mean ±
standard error of the mean of 6 rats per group
(#P<0.05 vs. Con group; *P<0.05, **P<0.01 vs.
BPH group). BPH, benign prostatic hyperplasia; Fina, BPH-induced
group treated with finasteride 5 mg/kg/day; MSJ, BPH-induced group
treated with musulju 200 mg/kg/day; Con, control; PARP, poly
(ADP-ribose) polymerase-1; Bcl, B-cell lymphoma; Bax,
Bcl-2-associated X protein. |
Discussion
BPH is the most common benign proliferative disease
in males, with ~8 million new patients diagnosed with primary or
secondary BPH annually (13). BPH
is the major cause of lower urinary tract symptoms, and is
characterized by enlargement of the transitional zone and increased
population of stromal cells (14).
Numerous factors have been implicated in the pathogenesis of BPH,
including an imbalance in cell proliferation and cell death
(15). In the present study, the
testosterone-induced BPH group demonstrated increased prostate
weight and PW/BW ratio compared with the Con group, and treatment
of BPH model rats with 200 mg/kg MSJ orally for 4 weeks
significantly inhibited this increase in prostate weight and PW/BW
ratio. In addition, histological analysis and assessment of
epithelial thickness confirmed that MSJ was effective in reversing
typical hyperplastic patterns, as previously shown. Based on these
data, a dose of 200 mg/kg MSJ was efficacious in protecting against
testosterone-induced BPH and this dose was used for further
investigation.
Androgens serve an essential role in the development
and growth of the entire male genital tract, in particular, the
prostate, stimulating the differentiation and proliferation of both
the epithelial and the stromal compartments of the gland (16). Development and maintenance of the
normal prostate, as well as development of BPH, depend on a
functional androgen-signaling axis, components that include: i)
Testosterone synthesis in the testes and the adrenal glands; ii)
conversion of testosterone to DHT by 5α-reductase; iii) transport
of DHT to target tissues; and iv) binding of DHT to the androgen
receptor with consequent modulation of genes (17). 5α-reductase is responsible for the
conversion of testosterone into its active form, DHT, and its
activity is correlated with the occurrence and progression of BPH
(18). In the present study, it
was revealed that treatment with MSJ inhibited serum testosterone
production in BPH model rats. Consistent with this reduction in
serum testosterone levels, the mRNA expression of 5α-reductase 2
was upregulated in rats with BPH, but was decreased in the animals
receiving MSJ treatment.
Inflammation is extremely common in the prostates of
aging men and is diagnosed histologically by the presence of
inflammatory cells infiltrating the prostatic stroma, epithelium
and/or ductal lumen (16).
Prostatic inflammation involves both an inflammatory cell
infiltrate and local tissue responses. A variety of inflammatory
mediators, such as cytokines, chemokines, histamine, prostanoids,
reactive oxygen species, growth factors, neuropeptides, and
neurotrophins, may produce these effects (19). In the present study, MSJ markedly
suppressed the expression of iNOS and COX-2, and these data
suggested that MSJ may be a potent alternative medicine for the
treatment of BPH via the regulation of the expression of
inflammation-associated proteins.
Changes in the expression levels of Bcl-2 and
caspase-3 have been observed in BPH relative to healthy prostates.
In normal prostatic tissue, Bcl-2 and caspase-3 expression in
epithelial cells was either undetectable or only weakly detected.
Therefore, it was suggested that lowering apoptosis rate in BPH may
be associated with alterations in the balance between Bcl-2 and
caspase-3 (20). Bcl-2 is an inner
mitochondrial membrane protein, and its predominant effect is to
prolong cell survival by inhibiting apoptosis. This increase in the
expression of Bcl-2 may balance the death cascade by inhibiting the
mitochondrial release of cytochrome c, which activates
caspases. The caspase family of proteases is central to the cell
death pathway. The extrinsic and intrinsic cell death pathways
converge to activate caspase-3 for the final execution of apoptosis
(21). Activation of caspase-3
cleaves a broad range of cellular substrates and promotes
activation of a DNA endonuclease required for internucleosomal DNA
fragmentation, a widely accepted hallmark of apoptosis. In the
present study, it was revealed that MSJ activated effector
caspase-3 and decreased the protein expression of its substrate,
PARP-1, in the BPH group. Additionally, MSJ markedly reduced the
level of Bcl-2 protein expression and increased the level of Bax
protein expression in the rat BPH model. These data suggested that
MSJ induced apoptosis through an antiapoptotic mechanism involving
a decrease in the ratio of Bcl-2 to Bax, leading to a
caspase-dependent pathway involving a caspase-3 activation.
In conclusion, the present study demonstrated that
MSJ decreased prostate weight and testosterone production in
BPH-induced rats. These effects may be due to the anti-inflammatory
and apoptotic effects of MSJ. Accordingly, the use of MSJ as a
potential therapeutic agent for the treatment of BPH must be
further explored.
References
|
1
|
Roehrborn CG: Male lower urinary tract
symptoms (LUTS) and benign prostatic hyperplasia (BPH). Med Clin
North Am. 95:87–100. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ho CK and Habib FK: Estrogen and androgen
signaling in the pathogenesis of BPH. Nat Rev Urol. 8:29–41. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Huggins C and Hodges CV: Studies on
prostatic cancer. I. The effect of castration, of estrogen and of
androgen injection on serum phosphatases in metastatic carcinoma of
the prostate. 1941. J Urol. 168:9–12. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Izumi K, Li L and Chang C: Androgen
receptor and immune inflammation in benign prostatic hyperplasia
and prostate cancer. Clin Investig (Lond). 4:935–950. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kramer G, Mitteregger D and Marberger M:
Is benign prostatic hyperplasia (BPH) an immune inflammatory
disease? Eur Urol. 51:1202–1216. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Shoskes DA: Phytotherapy in chronic
prostatitis. Urology. 60:(Suppl 6). S35–S37; discussion 37. 2002.
View Article : Google Scholar
|
|
7
|
Hirsch IH: Integrative urology: A spectrum
of complementary and alternative therapy. Urology. 56:185–189.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Guo QL, Ding QL and Wu ZQ: Effect of
baicalein on experimental prostatic hyperplasia in rats and mice.
Biol Pharm Bull. 27:333–337. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Rick FG, Schally AV, Block NL, Nadji M,
Szepeshazi K, Zarandi M, Vidaurre I, Perez R, Halmos G and
Szalontay L: Antagonists of growth hormone-releasing hormone (GHRH)
reduce prostate size in experimental benign prostatic hyperplasia.
Proc Natl Acad Sci USA. 108:3755–3760. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Maggi CA, Manzini S, Giuliani S and Meli
A: Infravesical outflow obstruction in rats: A comparison of two
models. Gen Pharmacol. 20:345–349. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Marinese D, Patel R and Walden PD:
Mechanistic investigation of the adrenergic induction of ventral
prostate hyperplasia in mice. Prostate. 54:230–237. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Miller J and Tarter TH: Combination
therapy with dutasteride and tamsulosin for the treatment of
symptomatic enlarged prostate. Clin Interv Aging. 4:251–258.
2009.PubMed/NCBI
|
|
13
|
Wei JT, Calhoun E and Jacobsen SJ:
Urologic diseases in America project: Benign prostatic hyperplasia.
J Urol. 173:1256–1261. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Izumi K, Mizokami A, Lin WJ, Lai KP and
Chang C: Androgen receptor roles in the development of benign
prostate hyperplasia. Am J Pathol. 182:1942–1949. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Pawlicki B, Zielinski H and Dabrowski M:
Role of apoptosis and chronic prostatitis in the pathogenesis of
benign prostatic hyperplasia. Pol Merkur Lekarski. 17:307–310.
2004.(In Polish). PubMed/NCBI
|
|
16
|
Corona G, Vignozzi L, Rastrelli G, Lotti
F, Cipriani S and Maggi M: Benign prostatic hyperplasia: A new
metabolic disease of the aging male and its correlation with sexual
dysfunctions. Int J Endocrinol. 2014:329–456. 2014. View Article : Google Scholar
|
|
17
|
Carson C III and Rittmaster R: The role of
dihydrotestosterone in benign prostatic hyperplasia. Urology.
61(4): Suppl 1. S2–S7. 2003. View Article : Google Scholar
|
|
18
|
Steers WD: 5alpha-reductase activity in
the prostate. Urology. 58(6): Suppl 1. S17–S24; discussion 24.
2001. View Article : Google Scholar
|
|
19
|
Meyer-Siegler KL and Vera PL: Substance P
induced release of macrophage migration inhibitory factor from rat
bladder epithelium. J Urol. 171:1698–1703. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zhang X, Zhang Q, Zhang Z, Na Y and Guo Y:
Apoptosis profiles in benign prostatic hyperplasia: Close
associations of cell kinetics with percent area density of
histologic composition. Urology. 68:905–910. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Nuñez G, Benedict MA, Hu Y and Inohara N:
Caspases: The proteases of the apoptotic pathway. Oncogene.
17:3237–3245. 1998. View Article : Google Scholar : PubMed/NCBI
|