Introduction
Berberine (BBR) is an isoquinoline derivative
alkaloid isolated from Chinese herbs, such as those from the
Berberis and Coptis genera (1). Aside from its traditional use as a
treatment for gastrointestinal disorders, BBR has been demonstrated
to exhibit inhibitory functions in a number of additional diseases,
including cancer (2), microbial
infection (3), inflammatory and
autoimmune diseases (such as cardiovascular disease) (4), collagen-induced arthritis (5), experimental type I diabetes in mice
(6) and experimental autoimmune
encephalomyelitis (EAE) (7).
Numerous reports have demonstrated that BBR may suppress the Th17
response in certain autoimmune diseases (6–8).
However, it remains unclear whether BBR exerts this function by
suppressing the Th17 response in Behcet's disease.
Behcet's disease is a multi-system inflammatory
disorder characterized by recurrent uveitis, oral aphthae, genital
ulcers or skin lesions (9). Ocular
Behcet's disease (OBD) is one of the most common causes of uveitis
in China (9). A number of studies
have indicated that Th17 cells, a subset of interleukin-17
(IL-17)-producing CD4+ T helper cells, and their
relevant cytokines, serve important roles in the pathogenesis of
experimental autoimmune uveitis (EAU), as well as in clinical
uveitis (including OBD) (10–12).
IL-17, the characteristic cytokine produced by Th17 cells, has been
observed to be upregulated in patients with active OBD, and
neutralization of IL-17 using a specific antibody or through the
inhibition of Th17 cells, led to the amelioration of EAU (10,13).
Corticosteroids and cyclosporin A, which are frequently used as
effective immunosuppressive drugs to treat clinical uveitis, may
significantly downregulate the Th17 cell response in patients with
OBD (14).
The signal transducer and activator of transcription
3 (STAT3) serves a critical role in Th17 differentiation and IL-17
production (15). STAT3 activation
is characterized by STAT3 phosphorylation, and previous studies
have demonstrated that patients with active Behcet's disease
exhibit elevated levels of STAT3 phosphorylation (16,17).
The aim of the present study was to investigate the
effect of BBR on the Th17 response in OBD. The results demonstrated
that patients with active OBD exhibited an increased Th17 response.
In vitro experiments revealed that BBR significantly
downregulated the expression of IL-17 and the number of Th17 cells
in patients with active OBD, and BBR could inhibit the
phosphorylation of STAT3. This suggests that BBR may suppress
intraocular inflammation in Behcet's disease, likely through
downregulating the phosphorylation of STAT3, thereby inhibiting the
Th17 response.
Materials and methods
BBR
BBR was purchased from Sigma-Aldrich; Merck
Millipore (Darmstadt, Germany), and was dissolved in dimethyl
sulfoxide (DMSO) before the stock solution (50 mM) was stored at
−20°C.
Patients and healthy controls
A total of 16 patients with active OBD, who were
admitted to The Second Xiangya Hospital of Central South University
(Changsha, China) from June 2014 to April 2015 (9 males and 7
females; average age, 34.8 years), and 18 healthy controls (HC; 10
males and 8 females; average age, 36.4 years) were included in the
present study. Behcet's disease was diagnosed according to the
diagnostic criteria of the International Study Group for Behcet's
Disease (18). The patients
presented with active uveitis, as evidenced by the presence of: i)
Intraocular inflammation, which was characterized by the presence
of floating cells in the anterior chamber or vitreous (100%); and
ii) retinal vasculitis, which was characterized by fundus
fluorescein angiography (100%). The extraocular systemic findings
included recurrent oral aphthous ulcers (100%), recurrent genital
ulcers (43.8%), skin lesions (56.3%) and arthritis (18.8%). The
present study was approved by the Ethics Committee of the Second
Xiangya Hospital of Central South University (Changsha, China). All
procedures complied with the Declaration of Helsinki (19), and informed consent was obtained
from all healthy individuals and patients with Behcet's disease
that were included in the study.
Isolation and culture of cells
Anticoagulated whole blood samples were obtained
from HCs and patients with active OBD. PBMCs were isolated using
Ficoll-Hypaque density gradient centrifugation. Blood cells were
diluted 1:1 with PBS. Ficoll-Hypaque solution (3–4 ml) was added
into 15-ml centrifuge tubes, and the diluted blood cells (6–8 ml)
were slowly layered on top of the Ficoll-Hypaque solution. The tube
was centrifuged at 4°C at 800 × g for 25 min without the
break. Following centrifugation, the PBMC layer appeared as a
white, cloudy band between the blood cell and Ficoll-Hypaque
layers, and was transferred to a new centrifuge tube and washed in
PBS three times. Peripheral CD4+ T cells were isolated
using human CD4 microbeads followed by magnetic-activated cell
sorting according to the manufacturer's instructions (Miltenyi
Biotec, Inc., San Diego, CA, USA). The purity of isolated cells
identified by flow cytometry was >94%. PBMCs and CD4+
T cells were resuspended in RPMI 1640 medium (Gibco; Thermo Fisher
Scientific, Inc., Waltham, MA, USA) containing L-glutamine (2 mM),
penicillin/streptomycin (100 U/ml), and 10% fetal calf serum
(Gibco; Thermo Fisher Scientific, Inc.), to a final concentration
of 1×106 cells/ml. Cells were cultured for 3 days in the
presence of BBR (5 µM) or DMSO and anti-CD3 (catalog no.
130-093-387) and anti-CD28 (catalog no. 130-093-375) antibodies
(0.5 and 0.1 µg/ml, respectively; Miltenyi Biotec, Inc.) at 37°C,
100% humidity and 5% CO2.
Enzyme-linked immunosorbent assay
(ELISA)
The levels of IL-17 in PBMCs and CD4+ T
cell sample supernatants were measured using DuoSet ELISA
Development Systems assay kits with a detection limit of 15.6 pg/ml
according to the manufacturer's protocol (catalog no. DY317;
R&D Systems, Inc., Minneapolis, MN, USA).
Cell viability assay
The PBMC suspension was seeded onto a 96-well plate
(1×106 cells/ml), and treated with BBR (5 µM) or DMSO,
and cultured for 3 days in the presence of anti-CD3 (0.5 µg/ml) and
anti-CD28 (0.1 µg/ml) antibodies. Cell viability was measured using
the Cell Counting kit-8 (Sigma-Aldrich; Merck Millipore).
Absorbance was read at 450 nm using an ELISA plate reader.
Flow cytometry
CD4+ T cells were cultured in the
presence of BBR or DMSO, and anti-CD3 (0.5 µg/ml) and anti-CD28
antibodies (0.1 µg/ml). In order to determine the number of
IL-17+ cells, CD4+ T cell samples were
stimulated with phorbol 12-myristate 13-acetate (100 ng/ml) and
ionomycin (1 µg/ml; Sigma-Aldrich; Merck Millipore) for 5 h. During
the final 4 h, brefeldin A (10 µg/ml; Sigma-Aldrich; Merck
Millipore) was added. Fixation/Permeabilization Concentrate (1
part; catalog no. 00-5123-43; eBioscience; Affymetrix, Inc., Santa
Clara, CA, USA) was mixed with Fixation/Permeabilization Diluent (3
parts; catalog no. 00-5223-56; eBioscience; Affymetrix, Inc.), and
1 ml of this Fixation/Permeabilization solution was added to
stimulated cells for 30 min at 4°C. Subsequently, 2 ml 1X
Permeabilization Buffer (catalog no. 00-8333; eBioscience;
Affymetrix, Inc.) was added to wash the cells. Cells were
resuspended in 100 µl 1X Permeabilization Buffer, and stained with
a fluorescein isothiocyanate (FITC)-conjugated mouse anti-human
IL-17 antibody (catalog no. 11-7179-41; eBioscience; Affymetrix,
Inc.) or a FITC-conjugated mouse IgG1 κ isotype control (catalog
no. 11-4714-41; eBioscience; Affymetrix, Inc.). The
IL-17+ cells in the CD4+ T cell population
were defined as Th17 cells.
Detection of phosphorylated (p)-STAT3 expression in
CD4+ T cells was achieved by culturing cells in the
presence of BBR (5 µM) or DMSO, together with anti-CD3 (0.5 µg/ml)
and anti-CD28 antibodies (0.1 µg/ml) for 30 min. Cells were
subsequently fixed and permeabilized as described above, and
stained with a phycoerythrin (PE)-conjugated mouse anti-human
pSTAT3 antibody (catalog no. 558557; BD Biosciences, San Jose, CA,
USA) or a PE-conjugated mouse IgG1 isotype control (catalog no.
12-4714; eBioscience; Affymetrix, Inc.).
Flow cytometry analysis was performed using a
FACSAria cytometer (BD Biosciences) and analyzed using FlowJo
software (Tree Star, Inc., San Carlos, CA, USA).
Statistical analysis
Data are expressed as the mean ± standard deviation.
Statistical analysis was performed using SPSS (version 13.0; SPSS,
Inc., Chicago, IL, USA). Differences between sample groups were
analyzed using Student's t-test, Mann-Whitney U-test and the
Wilcoxon signed-rank test. P<0.05 was considered to indicate a
statistically significant difference.
Results
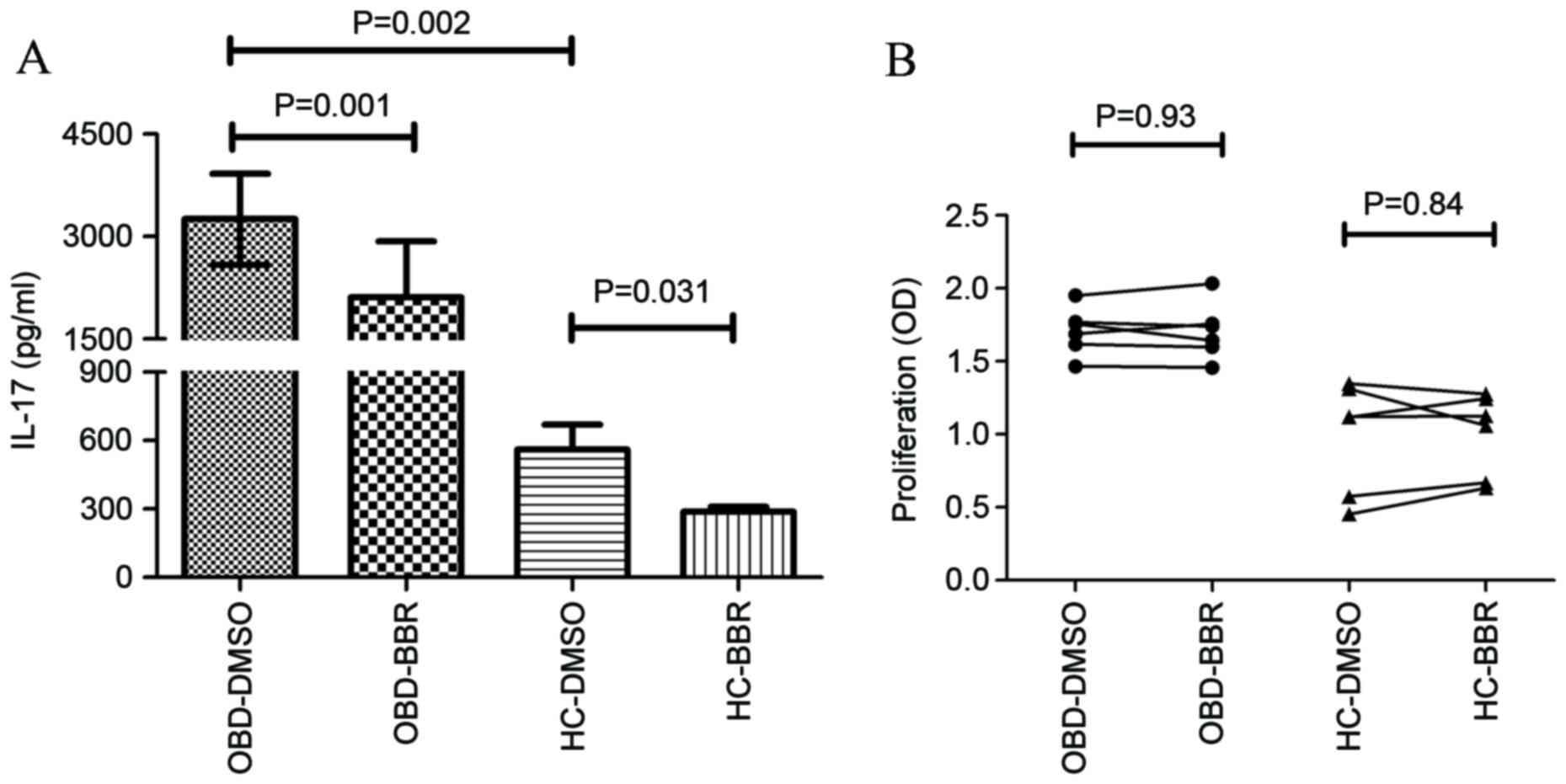
BBR inhibited the production of IL-17
but had no effect on the viability of PBMCs
PBMCs obtained from HC and patients with active OBD
were cultured in the presence of BBR (5 µM) or DMSO, together with
anti-CD3 and anti-CD28 antibodies for 3 days, in order to
investigate the effect of BBR on IL-17 production. Patients with
active OBD demonstrated a significant increase in IL-17 expression
compared with HC (3,251.98±666.02 vs. 561.61±108.37 pg/ml; P=0.002;
Fig. 1A). As shown in Fig. 1A, BBR significantly inhibited the
expression of IL-17 in PBMCs from patients with active OBD (from
3,251.98±666.02 to 2,113.63±815.07 pg/ml; P=0.0001) and HC (from
561.61±108.37 to 287.66±23.67 pg/ml; P=0.031). In order to
investigate whether BBR inhibited IL-17 production by reducing PBMC
cell viability, the effect of BBR exposure on PBMC cell viability
was then examined. As shown in Fig.
1B, BBR did not have a significant effect on the viability of
PBMC cells in HC or OBD groups at a concentration of 5 µM.
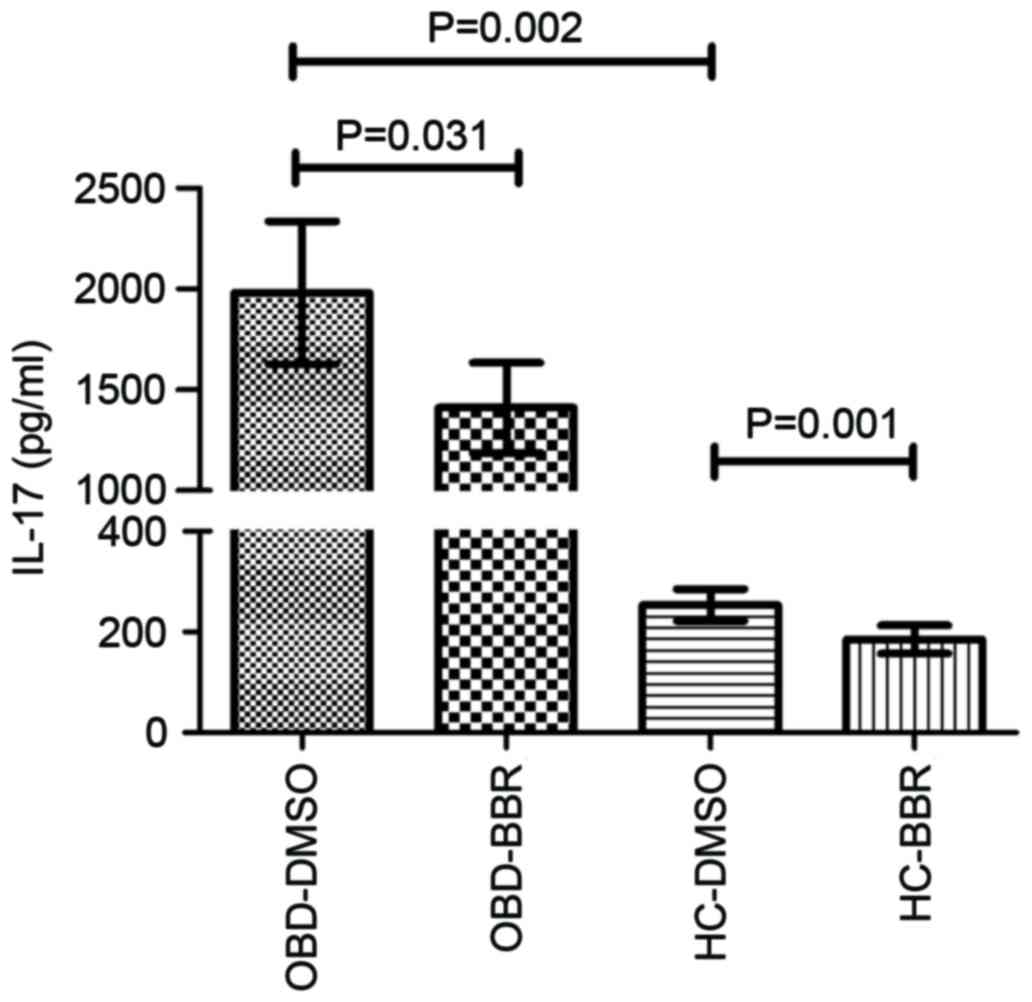
BBR inhibited the production of IL-17
in CD4+ T cells from HCs and patients with active
OBD
The expression of IL-17 in CD4+ T cells
was significantly higher upon stimulation with anti-CD3 and
anti-CD28 antibodies in patients with active OBD compared with HCs
(1,981.73±869.59 vs. 253.31±77.15 pg/ml; P=0.002; Fig. 2). Exposure to BBR significantly
decreased the production of IL-17 by CD4+ T cells in
active OBD patients (from 1,981.73±869.59 to 1,410.39±545.41 pg/ml;
P=0.031) and HCs (from 253.31±77.15 to 185.11±67.80 pg/ml; P=0.001;
Fig. 2).
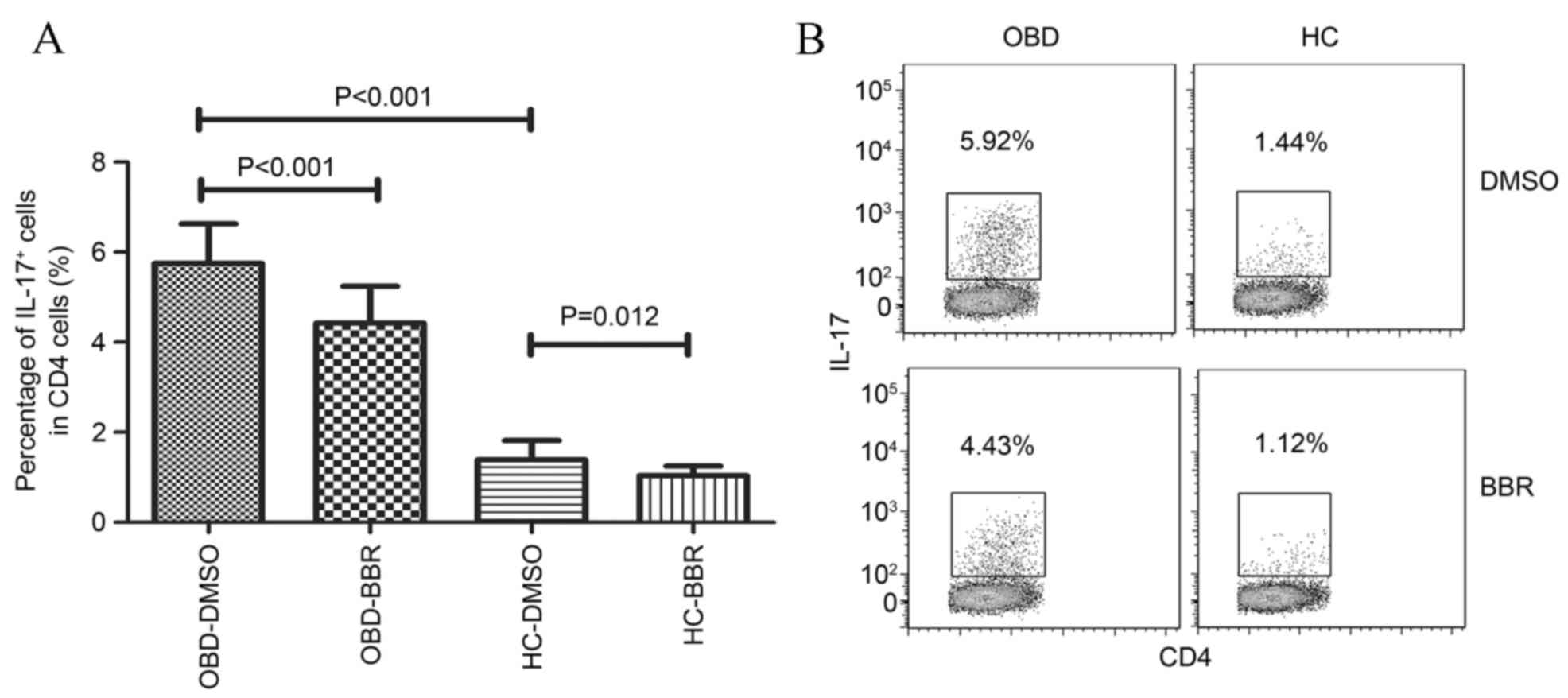
BBR inhibited the number of Th17 cells
in patients with active OBD and healthy controls
As shown in Fig. 3,
the number of Th17 cells (IL-17-producing CD4+ T cells)
was significantly higher in patients with active OBD compared with
HCs (5.75±0.88 vs. 39±0.43%; P<0.001). In addition, exposure to
BBR significantly inhibited the number of Th17 cells in patients
with active OBD (from 5.75±0.88 to 4.42±0.82%; P<0.001) and HCs
(from 1.39±0.43 to 1.03±0.22%; P=0.012; Fig. 3).
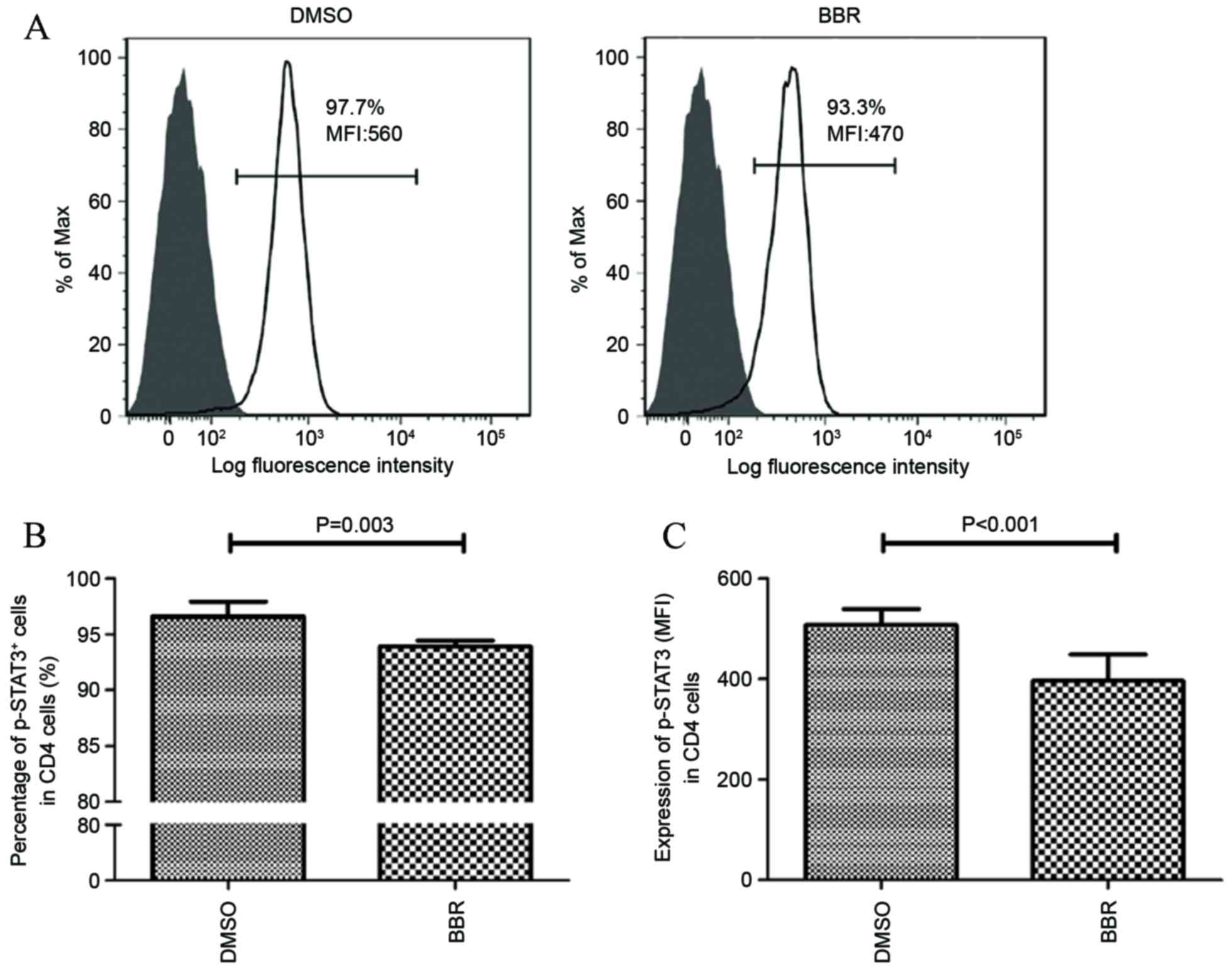
BBR inhibited the activation of
STAT3
Due to the observation that STAT3 activation is an
important factor involved in the differentiation of Th17 cells and
the production of IL-17 (15), the
effect of BBR on modulating STAT3 phosphorylation was investigated.
As shown in Fig. 4A and B,
exposure of CD4+ T cells, obtained from HCs, to BBR
significantly decreased the number of p-STAT3-positive cells from
96.6±1.24 to 93.9±0.54% (P=0.0.003). The expression of p-STAT3 was
then determined using the mean fluorescence intensity (MFI)
parameter. The results demonstrated that the MFI value of p-STAT3
expression in BBR-treated CD4+ T cells was significantly
lower compared with that of the DMSO-treated cells (506.67±32.75
vs. 396.33±58.49; P<0.001; Fig.
4C).
Discussion
In the present study the potential role of BBR as a
potential therapeutic agent for OBD was investigated. The results
demonstrated that BBR suppressed IL-17 expression and the number of
Th17 cells in PBMCs obtained from patients with active OBD and HCs.
In addition, BBR inhibited the activation of STAT3. These results
suggest that BBR may suppress the Th17 response in patients with
OBD by downregulating the phosphorylation of STAT3, and therefore
provides a rationale for investigating the potential use of BBR for
the treatment of patients with OBD in a clinical setting.
BBR is an isoquinoline alkaloid isolated from
certain Chinese herbs, such as Berberis, Hydrastis
canadensis and Coptidis rhizoma (1). The role of BBR in the treatment of a
number of inflammatory and autoimmune disorders has been reported
previously (4,6,7,20,21).
In addition, the role of BBR in uveitis has been investigated; in
endotoxin-induced uveitis, Berberis aristata, whose primary
components include BBR, inhibited ocular inflammation (22). Furthermore, BBR demonstrated an
immunoregulatory role in the Vogt-Koyanagi-Harada ocular autoimmune
disease (8). These studies support
a role for BBR as an anti-inflammatory agent.
As Th17 cell-associated inflammatory responses are
critically involved in the pathogenesis of OBD (23), the present study was designed to
investigate the effect of BBR on the function of Th17 cells in OBD.
The effect of BBR on the secretion of IL-17 by PBMCs was first
investigated. Consistent with Chi et al (24), a significant increase in the
expression of IL-17 was observed in patients with active OBD
compared with HCs. Following exposure to BBR, IL-17 expression in
PBMCs was significantly suppressed. Cell viability is an important
parameter that can influence cytokine production (25). Therefore, we investigated whether
BBR-mediated suppression of IL-17 expression was due to the
suppression of T-cell viability. The results demonstrated that BBR
did not influence T cell viability when exposed to a concentration
of 5 µM. This result is largely consistent with a previous report,
in which 50 µM BBR did not increase the death rate of lymphocytes
(26).
The results of the present study indicate a
suppressive effect of BBR on the secretion of IL-17 by PBMCs. As
Th17 cells primarily produce IL-17, CD4+ T cells were
purified from PBMCs in order to verify the suppressive effect of
BBR on IL-17 secretion by Th17 cells. The results revealed that BBR
may inhibit the secretion of IL-17 by Th17 cells.
Previous studies have demonstrated that STAT3
activation is critical for Th17 differentiation and IL-17
production (15). STAT3 activation
is characterized by its phosphorylation, which leads to the
regulation of downstream target genes that mediate intrinsic and
extrinsic cellular functions (15). In the present study STAT3
phosphorylation was significantly inhibited in CD4+ T
cells following BBR exposure, which may have been responsible for
the suppressive effect of BBR on the function of Th17 cells. This
result is consistent with those presented by Qin et al
(7), which used a mouse model of
EAE, and demonstrated that Th17 cell differentiation was markedly
inhibited by BBR treatment in vivo and in vitro, and
that this was associated with decreased phosphorylation of STAT3 in
Th17 cells.
Despite these observations, a number of important
questions for the use of BBR as a potential treatment for OBD
remain. Namely, the selection of a safe but effective dose of BBR
for the treatment of OBD. Our results demonstrate that BBR is not a
cytotoxic or a general immunosuppressive agent that affects T cell
survival in vitro. In addition, BBR is currently used for
the treatment of numerous gastrointestinal diseases in China, and
to the best of our knowledge, no unexpected safety concerns have
yet been identified. A recent randomized, placebo-controlled,
double-blind trial concerning the effects of BBR gelatin on
recurrent aphthous stomatitis, has demonstrated that the use of BBR
gelatin is safe and effective (27). Although there is no evidence to
suggest that increasing the dose of BBR may cause severe adverse
effects, there have been no reports on the safety of BBR treatment
in large doses and in the long-term, thus, the appropriate dose of
BBR for the treatment of OBD in vivo remains a critical
factor that requires further investigation. In addition, the
concentration of BBR in the plasma is an important aspect for
improving the symptoms of autoimmune disease (28). Therefore further studies are
required to define the optimal plasma BBR concentrations for the
treatment of OBD in vivo.
Another important consideration for the use of BBR
as a treatment for OBD, is based on the observation that BBR did
not completely suppress the Th17 cell response in the present
study. According to these results, the decreased levels of IL-17
expression and Th17 cell number following exposure of PBMCs
obtained from OBD patients to BBR, were not as low as observed in
the HC group. This suggests that BBR treatment alone may be
insufficient to control the disease. Therefore, further studies are
required to investigate whether BBR in combination with other
currently used immunosuppressive agents may modulate an aberrant
immune response, and may be a more suitable therapeutic approach
for the treatment of patients with OBD and additional autoimmune
diseases mediated by an abnormal Th17 immune response.
In conclusion, the results of the present study
indicate that BBR exhibits an inhibitory effect on the Th17 cell
response. BBR-mediated suppression of STAT3 activation abrogates
downstream signaling events, and results in the decreased
expression of IL-17 and the number of Th17 cells, which is one of
the potential mechanisms underlying the immunosuppressive effects
of BBR.
Acknowledgements
The authors would like to thank all of the patients
and healthy donors enrolled in the study. The present study was
supported by the Development Program of Hunan Provincial Science
& Technology Department (grant no. 2014FJ3006).
Glossary
Abbreviations
Abbreviations:
|
BBR
|
berberine
|
|
OBD
|
ocular Behcet's disease
|
|
PBMC
|
peripheral blood mononuclear cells
|
|
STAT3
|
signal transducer and activator of
transcription 3
|
|
DMSO
|
Dimethyl sulfoxide
|
|
ELISA
|
Enzyme-linked immunosorbent assay
|
|
EAE
|
experimental autoimmune
encephalomyelitis
|
|
EAU
|
experimental autoimmune uveitis
|
|
HC
|
healthy controls
|
|
MFI
|
mean fluorescence intensity
|
References
|
1
|
Ye M, Fu S, Pi R and He F:
Neuropharmacological and pharmacokinetic properties of berberine: A
review of recent research. J Pharm Pharmacol. 61:831–837. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Song YC, Lee Y, Kim HM, Hyun MY, Lim YY,
Song KY and Kim BJ: Berberine regulates melanin synthesis by
activating PI3K/AKT, ERK and GSK3β in B16F10 melanoma cells. Int J
Mol Med. 35:1011–1016. 2015.PubMed/NCBI
|
|
3
|
Saha P, Bhattacharjee S, Sarkar A, Manna
A, Majumder S and Chatterjee M: Berberine chloride mediates its
anti-leishmanial activity via differential regulation of the
mitogen activated protein kinase pathway in macrophages. PLoS One.
6:e184672011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chi L, Peng L, Pan N, Hu X and Zhang Y:
The anti-atherogenic effects of berberine on foam cell formation
are mediated through the upregulation of sirtuin 1. Int J Mol Med.
34:1087–1093. 2014.PubMed/NCBI
|
|
5
|
Hu Z, Jiao Q, Ding J, Liu F, Liu R, Shan
L, Zeng H, Zhang J and Zhang W: Berberine induces dendritic cell
apoptosis and has therapeutic potential for rheumatoid arthritis.
Arthritis Rheum. 63:949–959. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Cui G, Qin X, Zhang Y, Gong Z, Ge B and
Zang YQ: Berberine differentially modulates the activities of ERK,
p38 MAPK, and JNK to suppress Th17 and Th1 T cell differentiation
in type 1 diabetic mice. J Biol Chem. 284:28420–28429. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Qin X, Guo BT, Wan B, Fang L, Lu L, Wu L,
Zang YQ and Zhang JZ: Regulation of Th1 and Th17 cell
differentiation and amelioration of experimental autoimmune
encephalomyelitis by natural product compound berberine. J Immunol.
185:1855–1863. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yang Y, Qi J, Wang Q, Du L, Zhou Y, Yu H,
Kijlstra A and Yang P: Berberine suppresses Th17 and dendritic cell
responses. Invest Ophthalmol Vis Sci. 54:2516–2522. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yang P, Fang W, Meng Q, Ren Y, Xing L and
Kijlstra A: Clinical features of chinese patients with Behçet's
disease. Ophthalmology. 115:312–318. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Amadi-Obi A, Yu CR, Liu X, Mahdi RM,
Clarke GL, Nussenblatt RB, Gery I, Lee YS and Egwuagu CE: TH17
cells contribute to uveitis and scleritis and are expanded by IL-2
and inhibited by IL-27/STAT1. Nat Med. 13:711–718. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chi W, Yang P, Li B, Wu C, Jin H, Zhu X,
Chen L, Zhou H, Huang X and Kijlstra A: IL-23 promotes
CD4+ T cells to produce IL-17 in Vogt-Koyanagi-Harada
disease. J Allergy Clin Immunol. 119:1218–1224. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Peng Y, Han G, Shao H, Wang Y, Kaplan HJ
and Sun D: Characterization of IL-17+ interphotoreceptor
retinoid-binding protein-specific T cells in experimental
autoimmune uveitis. Invest Ophthalmol Vis Sci. 48:4153–4161. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Luger D, Silver PB, Tang J, Cua D, Chen Z,
Iwakura Y, Bowman EP, Sgambellone NM, Chan CC and Caspi RR: Either
a Th17 or a Th1 effector response can drive autoimmunity:
Conditions of disease induction affect dominant effector category.
J Exp Med. 205:799–810. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Liu X, Yang P, Lin X, Ren X, Zhou H, Huang
X, Chi W, Kijlstra A and Chen L: Inhibitory effect of Cyclosporin A
and corticosteroids on the production of IFN-gamma and IL-17 by T
cells in Vogt-Koyanagi-Harada syndrome. Clin Immunol. 131:333–342.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Mathur AN, Chang HC, Zisoulis DG,
Stritesky GL, Yu Q, O'Malley JT, Kapur R, Levy DE, Kansas GS and
Kaplan MH: Stat3 and Stat4 direct development of IL-17-secreting Th
cells. J Immunol. 178:4901–4907. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tulunay A, Dozmorov MG, Ture-Ozdemir F,
Yilmaz V, Eksioglu-Demiralp E, Alibaz-Oner F, Ozen G, Wren JD,
Saruhan-Direskeneli G, Sawalha AH and Direskeneli H: Activation of
the JAK/STAT pathway in Behcet's disease. Genes Immun. 16:170–175.
2014.PubMed/NCBI
|
|
17
|
Qi J, Yang Y, Hou S, Qiao Y, Wang Q, Yu H,
Zhang Q, Cai T, Kijlstra A and Yang P: Increased Notch pathway
activation in Behçet's disease. Rheumatology (Oxford). 53:810–820.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Criteria for diagnosis of Behçet's
disease, . International Study Group for Behçet's Disease. Lancet.
335:1078–1080. 1990.PubMed/NCBI
|
|
19
|
Rickham PP: Human experimentation. Code of
ethics of the world medical association. Declaration of Helsinki.
Br Med J. 2:1771964. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ma X, Jiang Y, Wu A, Chen X, Pi R, Liu M
and Liu Y: Berberine attenuates experimental autoimmune
encephalomyelitis in C57 BL/6 mice. PLoS One. 5:e134892010.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Marinova EK, Nikolova DB, Popova DN,
Gallacher GB and Ivanovska ND: Suppression of experimental
autoimmune tubulointerstitial nephritis in BALB/c mice by
berberine. Immunopharmacology. 48:9–16. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Gupta SK, Agarwal R, Srivastava S, Agarwal
P, Agrawal SS, Saxena R and Galpalli N: The anti-inflammatory
effects of Curcuma longa and Berberis aristata in endotoxin-induced
uveitis in rabbits. Invest Ophthalmol Vis Sci. 49:4036–4040. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Na SY, Park MJ, Park S and Lee ES:
Up-regulation of Th17 and related cytokines in Behçet's disease
corresponding to disease activity. Clin Exp Rheumatol. 31(3): Suppl
77. 32–40. 2013.PubMed/NCBI
|
|
24
|
Chi W, Yang P, Zhu X, Wang Y, Chen L,
Huang X and Liu X: Production of interleukin-17 in Behcet's disease
is inhibited by cyclosporin A. Mol Vis. 16:880–886. 2010.PubMed/NCBI
|
|
25
|
Hedegaard CJ, Krakauer M, Bendtzen K,
Sorensen PS, Sellebjerg F and Nielsen CH: The effect of
beta-interferon therapy on myelin basic protein-elicited
CD4+ T cell proliferation and cytokine production in
multiple sclerosis. Clin Immunol. 129:80–89. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Xu L, Liu Y and He X: Inhibitory effects
of berberine on the activation and cell cycle progression of human
peripheral lymphocytes. Cell Mol Immunol. 2:295–300.
2005.PubMed/NCBI
|
|
27
|
Jiang XW, Zhang Y, Zhu YL, Zhang H, Lu K,
Li FF and Peng HY: Effects of berberine gelatin on recurrent
aphthous stomatitis: A randomized, placebo-controlled, double-blind
trial in a Chinese cohort. Oral Surg Oral Med Oral Pathol Oral
Radiol. 115:212–217. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Pang B, Zhao LH, Zhou Q, Zhao TY, Wang H,
Gu CJ and Tong XL: Application of berberine on treating type 2
diabetes mellitus. Int J Endocrinol. 2015:9057492015.PubMed/NCBI
|