Introduction
Adult onset Still's disease (AOSD) is a rare
multi-systemic inflammatory disease of unknown etiology and
pathogenesis, which predominantly affects young adults, and most
commonly occurs before the age of 35 years old (1–4). Its
main features are high spiking fever, evanescent rash,
lymphadenopathy, hepatosplenomegaly, leukocytosis, elevated liver
enzymes, erythrocyte sedimentation rate, and serum ferritin.
However, due to non-specific clinical performance, laboratory and
imaging examinations, the diagnosis of AOSD first requires the
exclusion of other diseases including infectious, inflammatory and
malignant diseases (5–7). Thus, it is important to rule out a
wide range of other diseases, including malignant, infectious and
rheumatic diseases before the definite diagnosis of AOSD (2,6,8).
Numerous clinical studies have demonstrated that the
important roles of 18F-fluorodeoxyglucose positron
emission tomography/computed tomography (18F-FDG PET/CT)
examinations in obtaining differential diagnoses of malignant vs.
benign diseases. In addition, 18F-FDG PET/CT scanning is
more effective in evaluating the involved extent of the disease. At
present, the majority of knowledge concerning 18F-FDG
PET/CT imaging in patients with AOSD is limited to sporadic case
reports (2,9–15)
and few previous studies (16,17).
Thus, the purpose of the present study was to summarize the imaging
characteristics of 18F-FDG PET/CT and evaluate the
potential efficacy of using PET/CT in patients with AOSD.
Materials and methods
Patients
Between November 2010 and March 2015, 32 patients
with definite AOSD were enrolled from Zhongshan Hospital (Shanghai,
China) to this retrospective analysis based on the criteria of
Yamaguchi et al (18). It
contains 4 major (fever, rash, arthritis and leukocytosis) and 5
minor (sore throat, lymphadenopathy, hepatomegaly/splenomegaly,
altered liver function test and negative for antinuclear antibodies
and rheumatoid arthritis) criteria. A total of 5 or more criteria
with at least 2 major criteria are required to make the diagnosis.
All procedures performed involving human participants were in
accordance with the ethical standards of the Institutional Review
Board of Zhongshan Hospital, Fudan University, and with the 1964
Helsinki Declaration and its later amendments or comparable ethical
standards. The present study was approved by the Ethics Committee
of Zhongshan Hospital, Fudan University (Shanghai, China) and
informed consent was obtained from all individual participants
included in the study.
18F-FDG PET/CT scan
18F-FDG PET/CT scanning was performed on
a Discovery VCT 64 System (GE Healthcare Biosciences, Milwaukee,
WI, USA) with a 15.7 cm axial field view. Patients were required to
fast for a minimum of 6 h prior to imaging, and serum glucose
levels were maintained under 7.4 mmol/l. PET/CT images were
obtained approximately 60 min subsequent to intravenous
administration of 3.7–5.6 MBq of 18F-FDG per kilogram of
body weight. A total of 6 or 7 bed positions (dependent on the
patient's height) from the vertex of skull to middle of the thighs
were imaged. PET images were acquired for 2.5 min per bed position.
CT was performed on the same scanner without contrast
administration. The CT scan data were collected with 140 kV, 200
mAs (adjusted by auto mA) and a gantry rotation speed of 0.8 sec.
All CT scans were obtained using 3.75-mm-thick axial slices.
Integrated PET and CT images were obtained automatically on Xeleris
(GE Healthcare Biosciences) or Advantage workstations (GE
Healthcare Biosciences).
Visual and semi-quantitative
analysis
PET/CT results were analyzed and interpreted by two
experienced Nuclear Medicine physicians who were blind to the
patients' clinical information, other conventional imaging findings
and the pathology results. Increased 18F-FDG uptake by
spleen and/or bone marrow was defined as that was greater than
liver. This method has been previously used to evaluate spleen and
bone marrow uptake in lymphoma and leukemia (19,20).
In cases of discrepancy regarding PET/CT results, a consensus was
reached after mutual discussion between two physicians. Areas of
focally increased accumulation known to represent physiological
18F-FDG uptake, such as brown fat, were excluded. For
semi-quantitative analysis, the maximal standardized uptake value
(SUVmax) was analyzed as published previously (21). SUVmax was calculated as
decay-corrected maximum activity concentration in the lesion
divided by administered activity divided by body weight in
kilograms. The SUVmax of a region of interest located in the right
lobe of the liver served as the reference. Associated results,
including splenomegaly, lymph node swelling and other lesions, were
additionally evaluated. In cases of multiple lymph nodes, SUVmax
was calculated for all lesions, and the highest SUVmax was
selected.
Pathology
Pathological examinations were performed: 26 cases
on bone marrow, and 9 cases on lymph node biopsies. The pathology
was reviewed by 2 experienced board-certified pathologists and all
cases were clinically monitored a minimum of 1 year.
Statistical analysis
All data are expressed as the means and standard
deviations. Statistical analysis was performed using Student's
t-test using SPSS software, version 18.0 (SPSS Inc., Chicago, IL,
USA). P<0.05 was considered to indicate a statistically
significant difference.
Results
Clinical data
A total of 32 patients with AOSD, comprising 25
female and 7 male patients with an average age of 39±15 years
(range, 19–80 years) took part in the present study. The patients
were admitted to the hospital with various non-specific clinical
features, including fever, rash, joint pain, sore throat, fatigue,
skin itching, and lymphadenopathy. Fever (32/32, 100.0%) with the
range of the maximum temperature (Tmax) from 39–41°C, rash (18/32,
56.3%) and joint pain (16/32, 50.0%) were the top three clinical
symptoms.
18F-FDG PET/CT imaging
As presented in Table
I, among 32 patients, no normal case was observed. Diffusely
abnormal FDG accumulation by the spleen and bone marrow was the
main observation on PET/CT images, followed by lymphadenopathy with
abnormal FDG uptake. A total of 27 cases out of the 32 patients
were identified with diffusely elevated FDG uptake by the spleen,
and the average SUVmax was 4.2±1.1 (range, 2.5–6.7), and 19 of 27
cases exhibited swelling of the spleen. The remaining 5 cases were
without abnormal FDG uptake, and only two patients were identified
to present with marginal spleen swelling. The mean SUVmax of these
5 spleens was 2.1±0.6 (range, 1.5–2.8), which was significantly
lower than that of 27 cases (P<0.05).
 | Table I.Imaging characteristics of 32 patients
with adult onset Still's disease demonstrated with
18F-FDG PET/CT. |
Table I.
Imaging characteristics of 32 patients
with adult onset Still's disease demonstrated with
18F-FDG PET/CT.
| Organs and
tissues | Positive cases | Negative cases |
|---|
| Spleen | 27 | 5 |
| SUVmax
range | 2.5–6.7 | 1.5–2.8 |
| Mean ±
standard deviation | 4.2±1.1a | 2.1±0.6a |
| Bone marrow | 26 | 6 |
| SUVmax
range | 2.8–7.0 | 1.3–3.4 |
| Mean ±
standard deviation | 4.6±0.6a | 2.6±0.7a |
| Lymph nodes | 20 | 5 |
| SUVmax
range | 2.2–13.9 | – |
| Mean ±
standard deviation | 5.9±3.1 | – |
| Skin | 1 | 31 |
| Joint | 1 | 31 |
| Serous effusion | 7 | 25 |
In addition, 26 of 32 patients presented with
diffuse and homogeneous glucose accumulation by bone marrow of
whole body, with the mean SUVmax of 4.6±0.6 (range, 2.8–7.0). The
remaining 6 cases were observed without FDG uptake, and the mean
SUVmax was 2.6±0.7 (range, 1.3–3.4). There was significant
difference between the abovementioned two groups (P<0.05).
Among 32 cases, 20 patients were identified with
lymphadenopathy with positive FDG uptake on PET/CT images. The
performance of FDG metabolism by lymph nodes was mixed, with an
SUVmax range from 2.2–13.9, and the mean SUVmax was 5.9±3.1. The
range of maximum diameter of lymph nodes was from 9.3–24.2 mm, and
the mean diameter was 15.3–4.2 mm. The lymph node swelling in 2
cases was limited to local lymph nodes (one in mediastinum, the
other in bilateral necks), and the remaining 18 cases displayed
varied lymph node involvement (neck, clavicle, axillary,
mediastinum, lung hilar, abdominal, retroperitoneal, pelvic and
inguinal regions). The most involved lymph nodes were located in
the neck (19/32) and chest (18/32), the abdomen and pelvic regions
were secondary (13/32).
In addition, 1 case presented with marginally
increased FDG uptake by the skin of the neck, shoulders and chest,
which was caused by the skin rash of the corresponding part
(Fig. 1). Another case displayed
elevated FDG activity in the right shoulder joint, but the patient
had no history of joint diseases. A total of 7 cases presented with
effusion on the PET/CT images, including 4 cases with diffuse
effusion (pleural, pericardial, abdominal and pelvic effusion;
Fig. 2) and 3 cases with local
effusion (2 patients with pericardial effusion and 1 patient with
pelvic effusion). However, in the present study, no case of liver
swelling and/or abnormal glucose metabolism was observed, and the
mean SUVmax of the liver was 2.5±0.5 (range, 1.7–3.5).
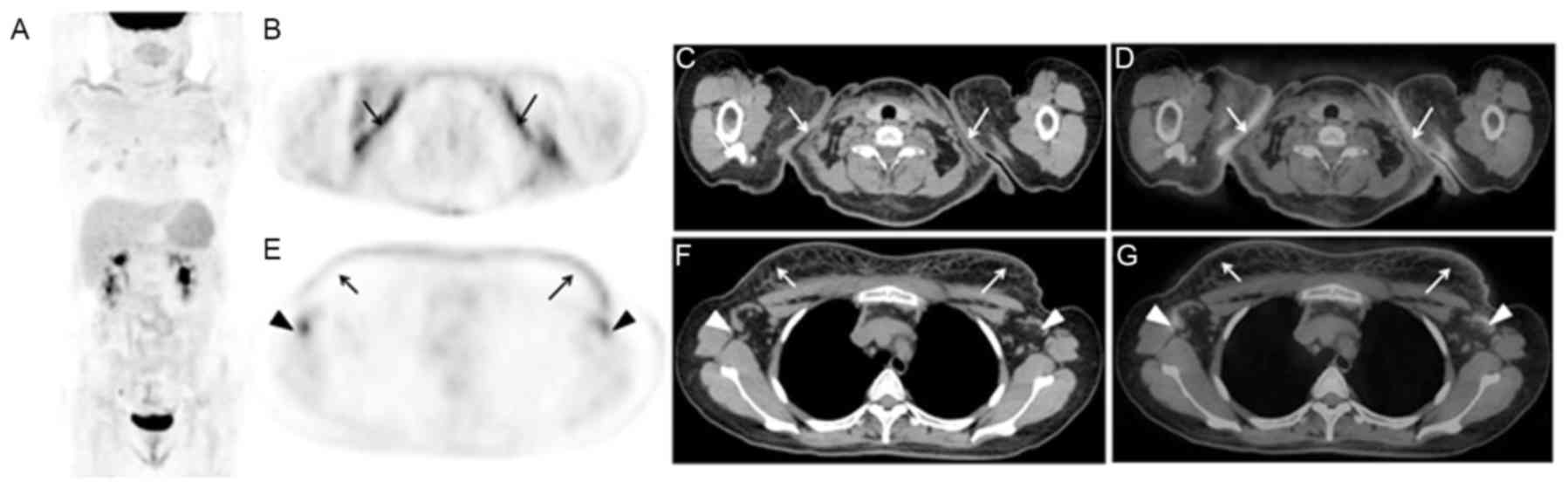
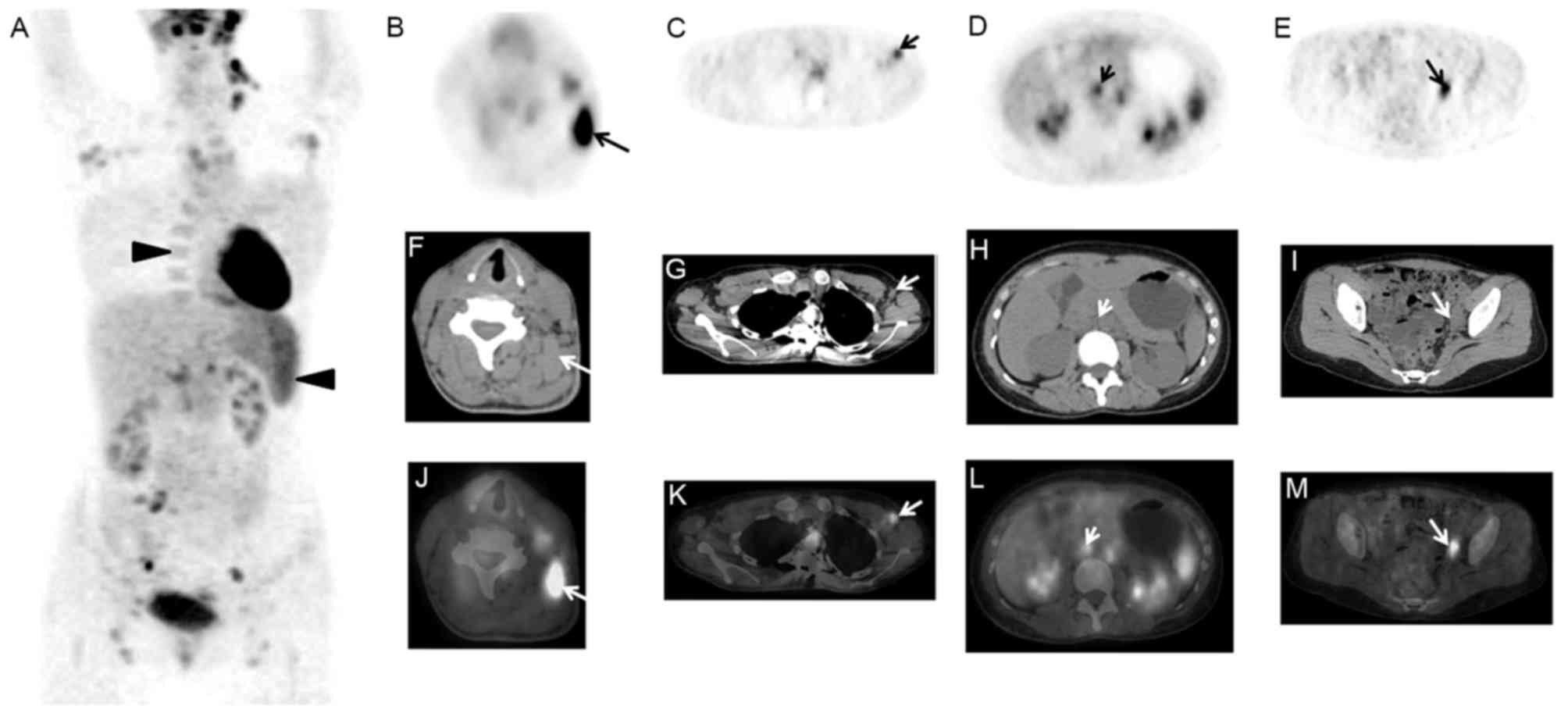
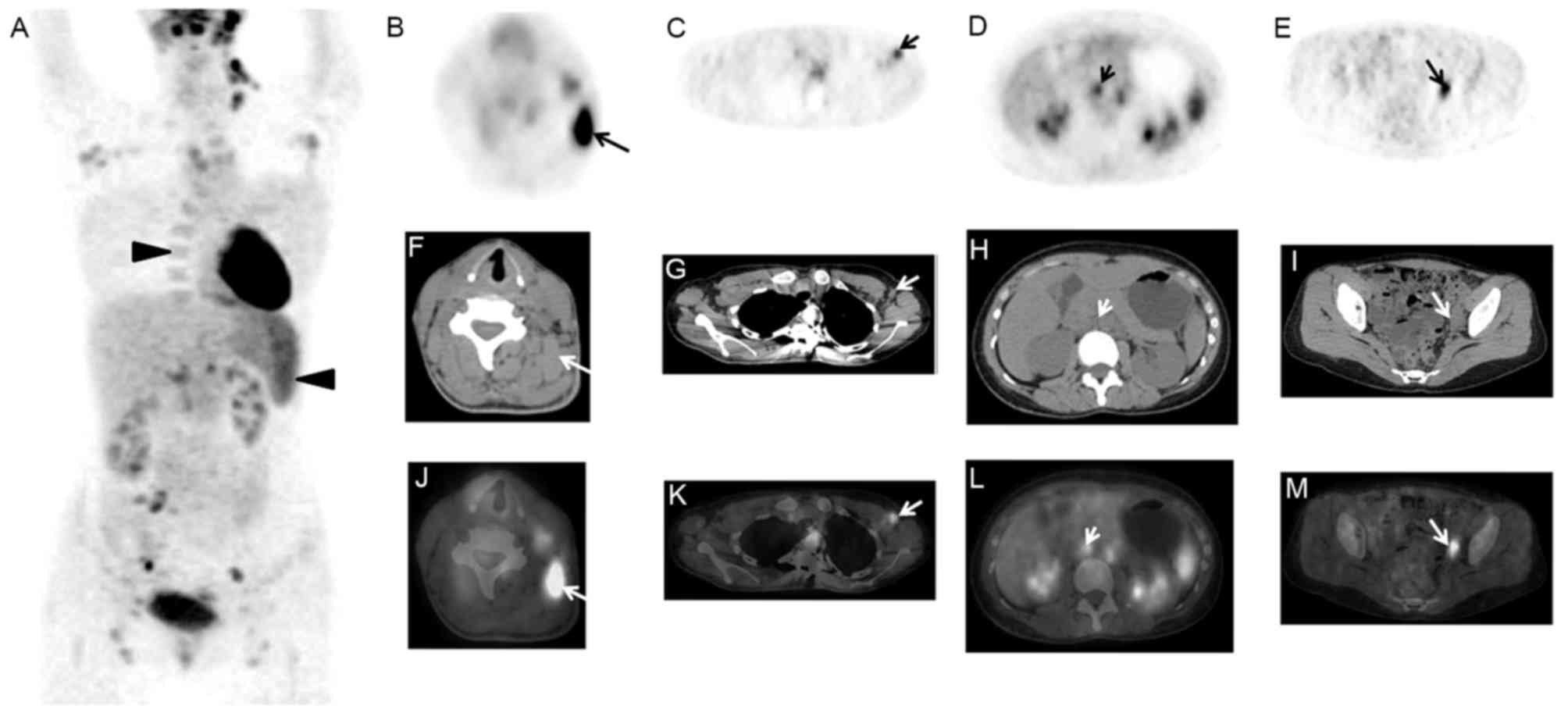
 | Figure 1.A 36-year-old female patient presented
with intermittent fever (Tmax of 39.6°C) and rash for almost 1
year. AOSD was diagnosed 10 months ago, and the patient received
the therapy of CSs. The rash was worsened after the reduction of
CSs, and was widely located in the skin of trunk and limbs.
18F-FDG PET/CT images are presented: (A) MIP, (B) PET,
(C) CT, (D) PET/CT, (E) PET, (F) CT, (G) PET/CT. These images
indicated diffusely increased FDG uptake by the skin of the neck,
shoulders and chest (arrows), with an SUVmax of 3.1. In addition,
marginal swelling of the spleen was observed with diffuse FDG
uptake. Lymph nodes of the left cervical, bilateral axillary
(triangle arrows), lung hilar and abdominal regions were enlarged
with mildly increased radioactivity, of which the SUVmax was 2.2.
AOSD, adult onset Still's disease; CSs, corticosteroids;
18F-FDG, fluorodeoxyglucose; PET, positron emission
tomography; CT, computerized tomography; MIP, maximum intensity
projection; SUV, standardized uptake value. |
Pathology and clinical follow-up
Among 32 patients, 26 cases underwent bone marrow
biopsy: 9 cases displayed normal bone marrow biopsies, 15 cases
showed the non-specific reactive hyperplasia of hematopoietic
cells, 1 case presented with non-specific low bone marrow
hyperplasia, and 1 case with non-specific increased granulocyte
ratio. Lymph node biopsies were conducted in 9 patients out of 32,
and the results demonstrated non-specific inflammation in 8 cases,
and a normal result in 1 case. With the exception of 1 case, the
remaining 31 patients responded well to corticosteroids (CSs) and
the symptoms were markedly improved. The symptom of this case
returned, and was finally improved under the control of
methotrexate and methylprednisolone.
Discussion
AOSD is a chronic systemic inflammatory disease,
first described by Bywaters in 1971 (10,22).
Due to the non-specific features in clinical performance,
laboratory tests and imaging modalities, AOSD remains difficult to
diagnose. In the present study, all 32 patients were admitted to
the hospital based on fever of unknown origin. In order to exclude
malignancy, 18F-FDG PET/CT scans were performed, and the
imaging characteristics of AOSD on PET/CT imaging were summarized
and analyzed.
Previous studies have indicated that the results of
18F-FDG PET/CT for AOSD are mixed. Funauchi et al
(10) presented a case of AOSD
with increased FDG activity in the liver and spleen alone. Roy
et al (9) reported elevated
FDG level in the joints of whole body associated with AOSD in a
28-year-old patient. In another case reported by de Graaff et
al (14), increased FDG
accumulation by the carotids, the wrist and the large vessels of
the legs was demonstrated. Yamashita et al (17) reported that in 7 cases with AOSD,
FDG uptake was additionally positive in the pericardium, pleura,
salivary glands, eyelids and muscles. Other cases reported
increased FDG uptake was identified in multiple lymph nodes across
the whole body (2,12,16,17),
which could not lead to differential diagnosis with malignant
lymphoma. In agreement with previous studies, the
18F-FDG PET/CT images in patients with AOSD presented
with varied results. Increased FDG activity in the spleen (84.4%),
bone marrow (81.3%) and lymphadenopathy (62.5%) were the most
common observations. In addition, 21.9% of patients were exhibited
with effusion without FDG uptake, and another 2 cases showed
abnormal FDG uptake by the skin and joint, respectively. Notably,
no elevated FDG uptake in the liver and vessels were observed in
the present study.
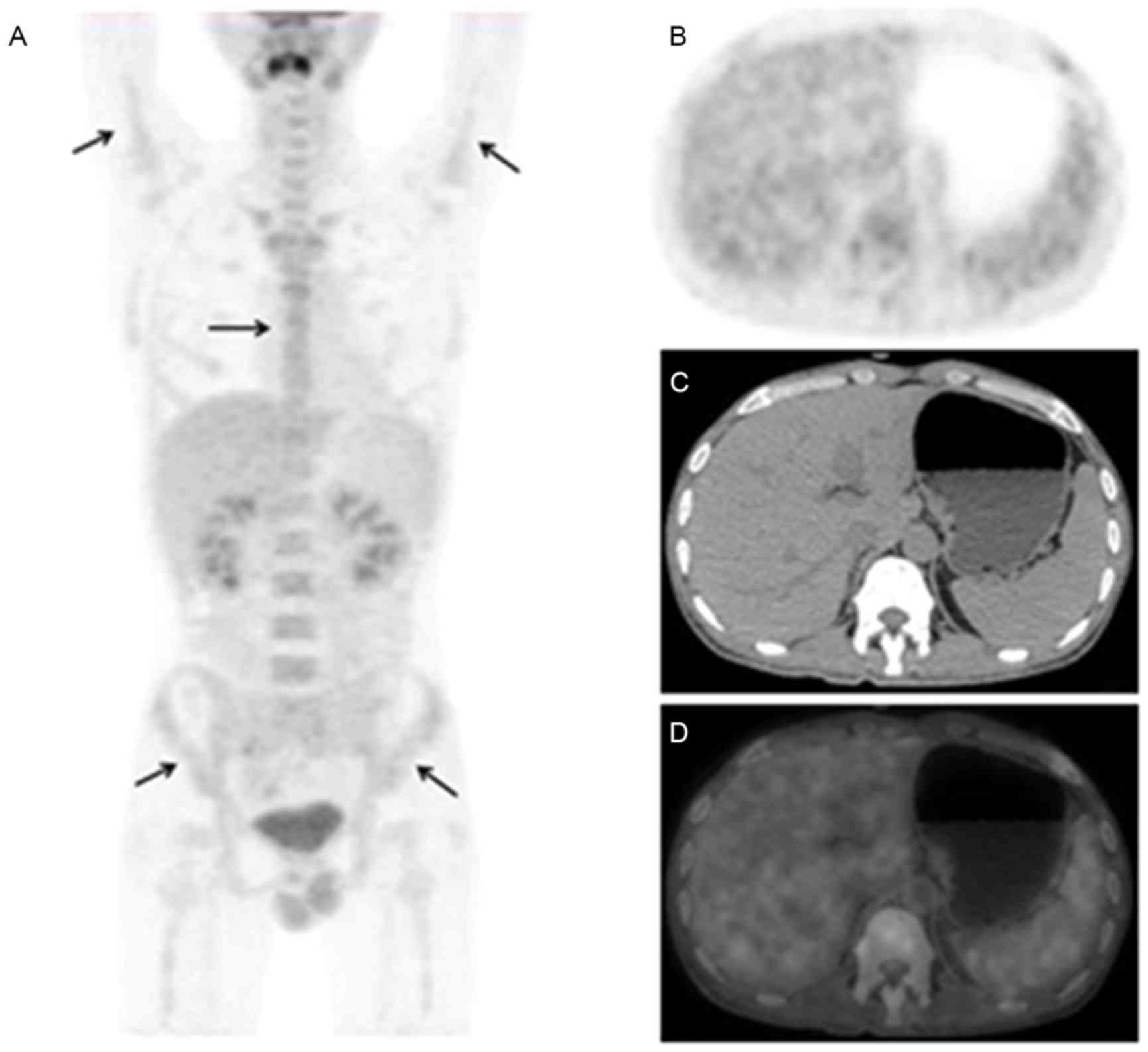
Based on the imaging features of this study, the
roles of 18F-FDG PET/CT in AOSD were retrospectively
investigated. Firstly, 18F-FDG PET/CT could display both
anatomic and functional changes of AOSD, and evaluated the involved
extent of AOSD. For example, as presented in Fig. 3, the case only displayed diffusely
elevated FDG activity in bone marrow of whole body on PET/CT
images. The case in Fig. 4
demonstrated that although multiple enlarged lymph nodes of the
whole body with mildly increased radioactivity were displayed on
PET/CT images, the benign diseases of lymph nodes such as
inflammation rather than malignancies were diagnosed based on the
size, morphology, density, and SUVmax of the lymph nodes in this
case. However, for other cases, as presented in Figs. 5 and 6, which was difficult to make
differential diagnosis with lymphoma. Secondly, it could guide the
biopsy of tissues with abnormal FDG accumulation including lymph
nodes, bone marrow, skin and other tissues. Regarding the cases in
Figs. 5 and 6, the biopsies of the lymph nodes were
performed under the guide of 18F-FDG PET/CT imaging,
which contributed to suggest the proper lymph node applied for the
biopsy. Finally, 18F-FDG PET/CT is helpful in the
post-treatment evaluation of AOSD. Although these data weren't
investigated in the present study, Choe et al (2) and Yamashita et al (17) identified significant improvements
(decreased SUV level) in the initially abnormally sized radioactive
lesions in the follow-up images of PET/CT.
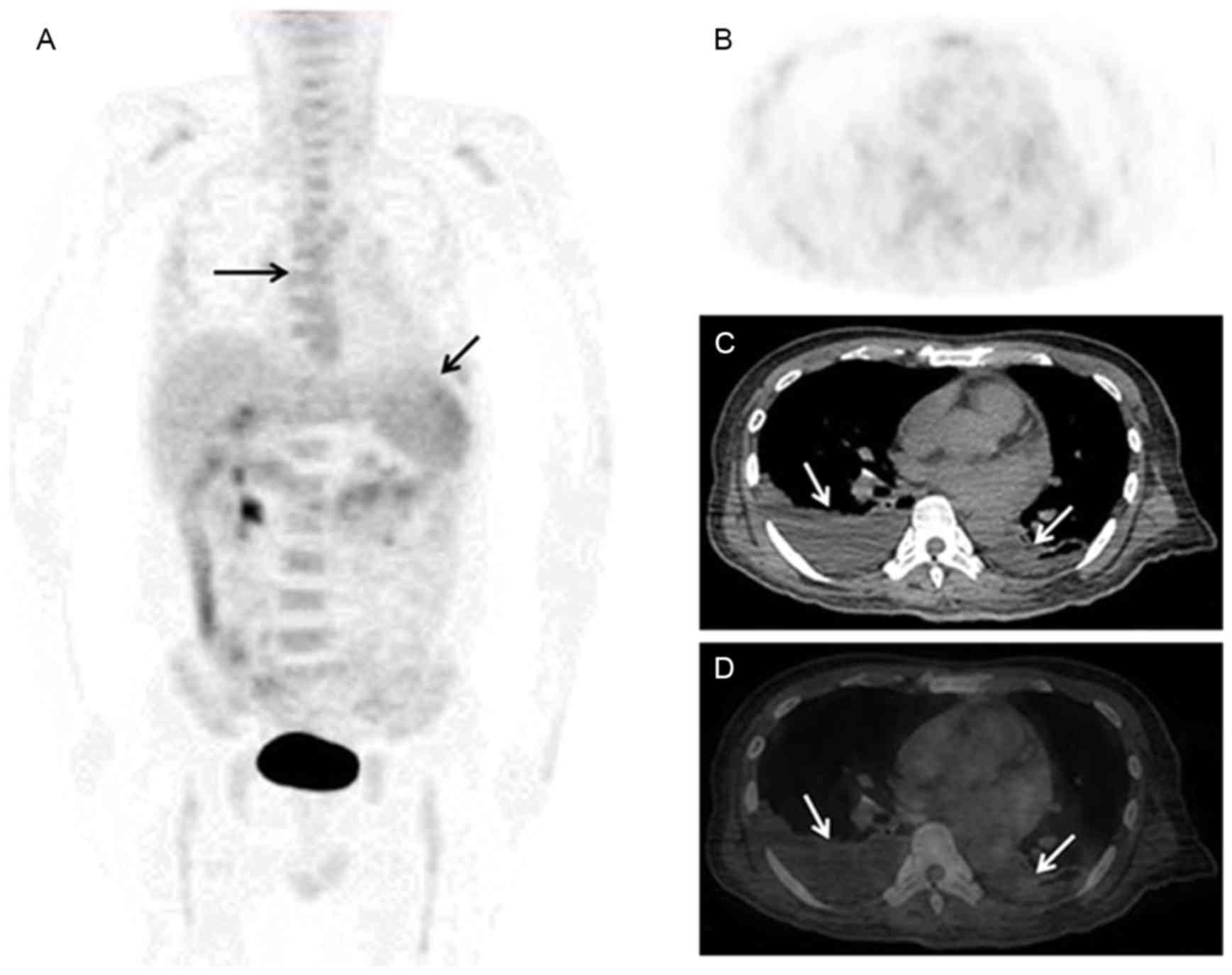
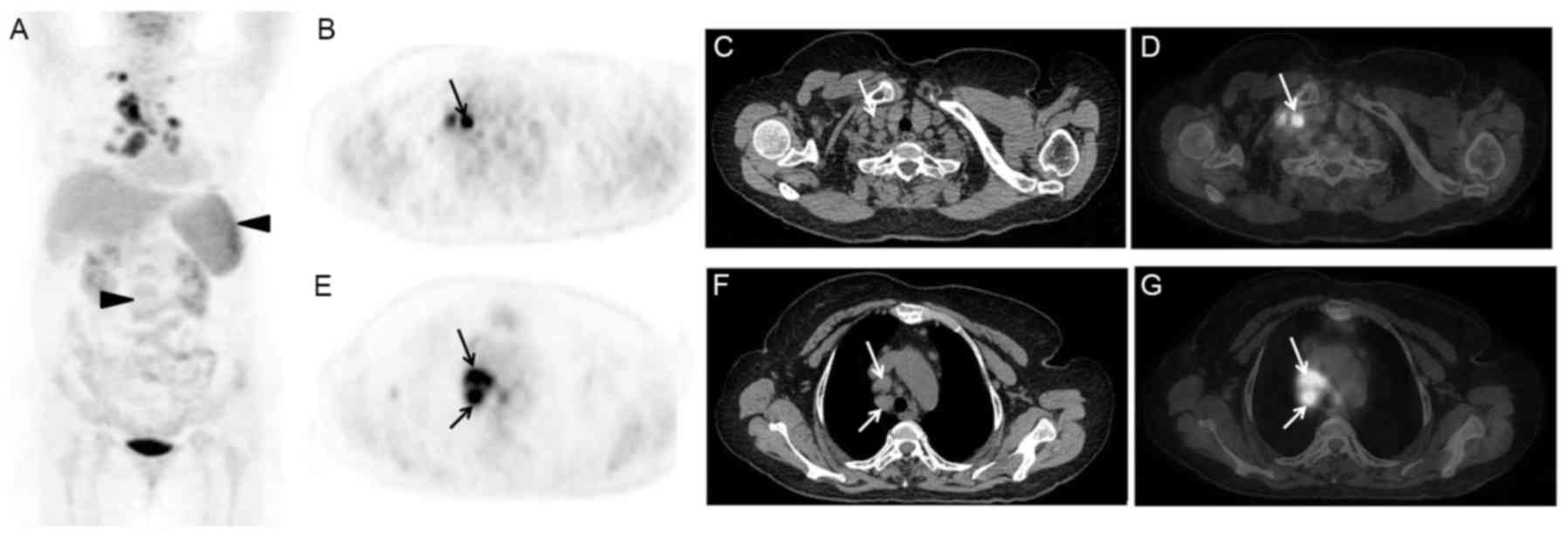
 | Figure 4.A 28-year-old female presented with
intermittent fever, bilateral knee joints pain, and rash for 1
month, and Tmax was 40.4°C. The treatment of antibiotics was
invalid, and local CT displayed multiple enlarged lymph nodes of
cervical and axillary regions. 18F-FDG PET/CT scan
indicated that the spleen was markedly enlarged with FDG
accumulation, with SUVmax of 5.2, and diffuse radioactivity uptake
was observed in the bone marrow with an SUVmax of 5.0 (A: MIP,
triangle arrows). In addition, multiple lymph nodes of cervical,
supraclavicle, mediastina, axillary, abdominal, retroperitoneal,
pelvic and inguinal regions were enlarged with increased
radioactivity (B-D: PET, E-G: CT, and H-J: PET/CT, arrows). CT,
computerized tomography; 18F-FDG, fluorodeoxyglucose;
PET, positron emission tomography; SUV, standardized uptake value;
MIP, maximum intensity projection. |
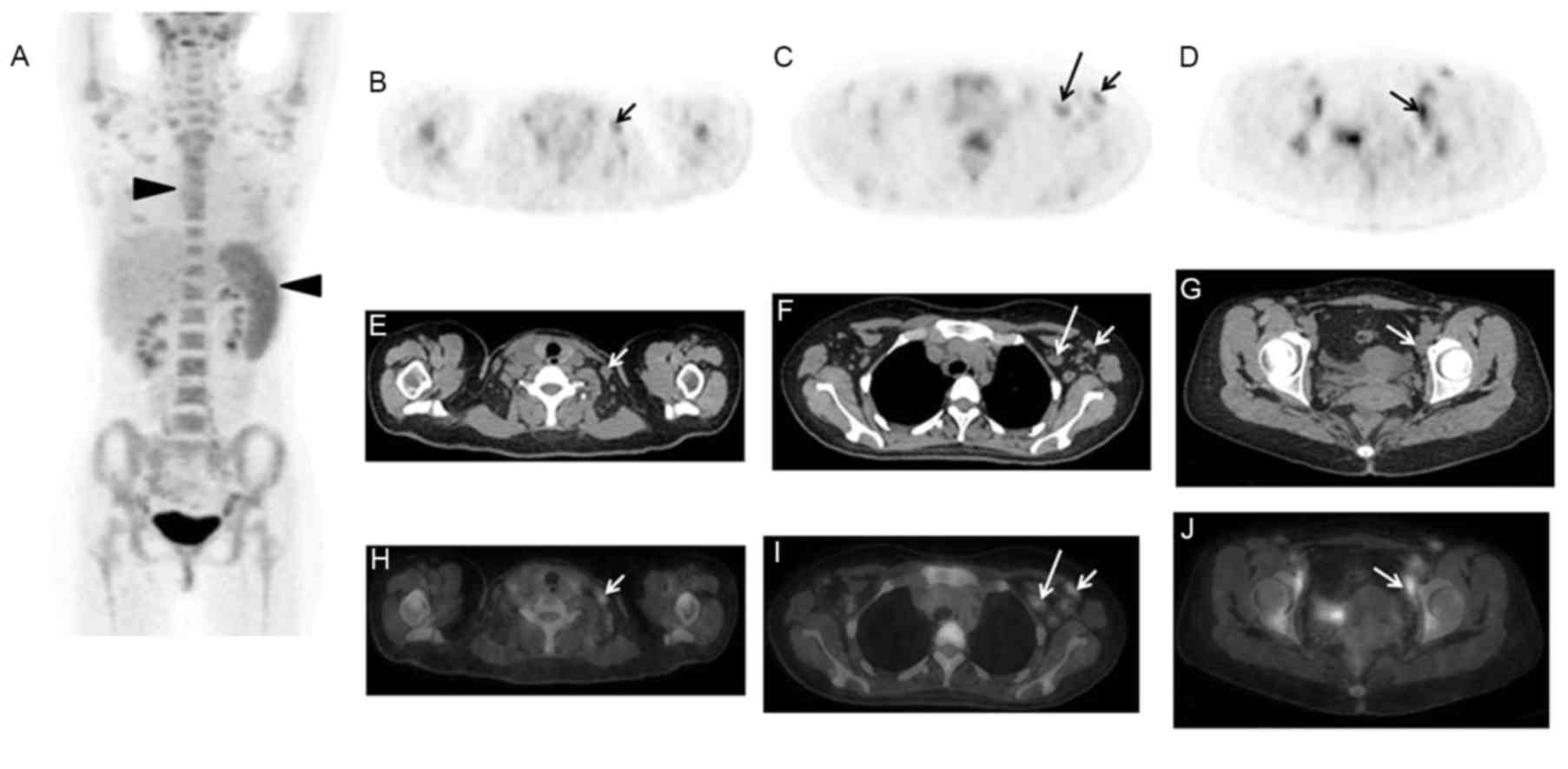
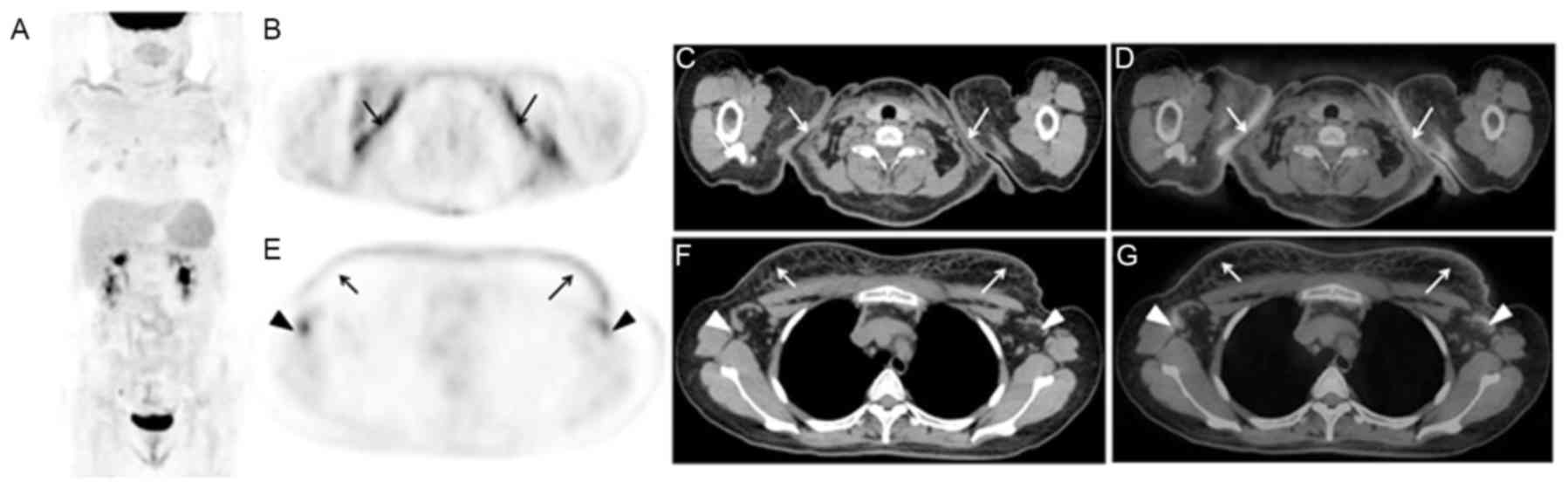
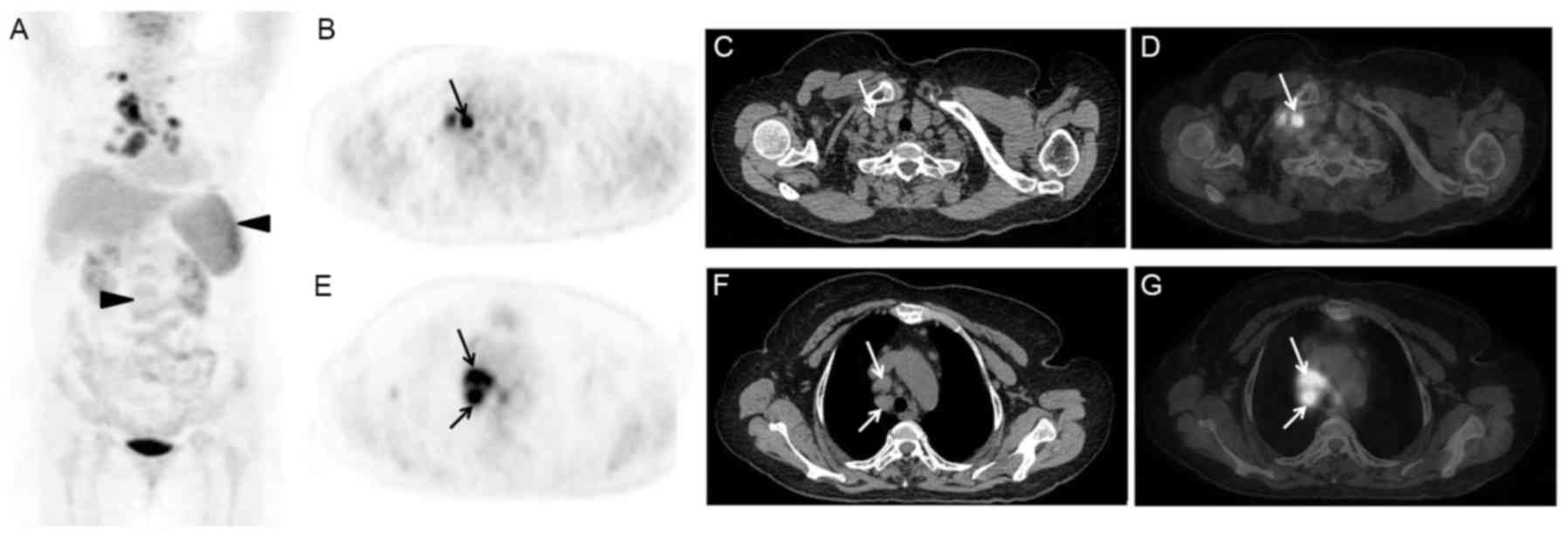
 | Figure 5.A 25-year-old female presented with a
mass located in the left cervical region for 1 month, fever (Tmax
of 40.0°C) and joint pain for 3 weeks. The patient had history of
corrective operation for deformities of the spine 10 years ago.
18F-FDG PET/CT imaging displayed that in addition to
diffuse FDG uptake by the spleen and bone marrow (A: MIP, triangle
arrows), multiple lymphadenopathy with abnormal FDG uptake (arrows)
was observed (B-E, PET; F-I, CT; and J-M, PET/CT). The biopsy of
left cervical lymph node (B, F and G; arrows) was taken and the
pathology was non-specific inflammation. The biopsy of bone marrow
was non-specific reactive hyperplasia of hematopoietic cells. After
the therapy of CSs for 1 month, ultrasound displayed that the lymph
nodes of left neck and axillary obviously shrine.
18F-FDG, fluorodeoxyglucose; PET, positron emission
tomography; CT, computerized tomography; MIP, maximum intensity
projection. |
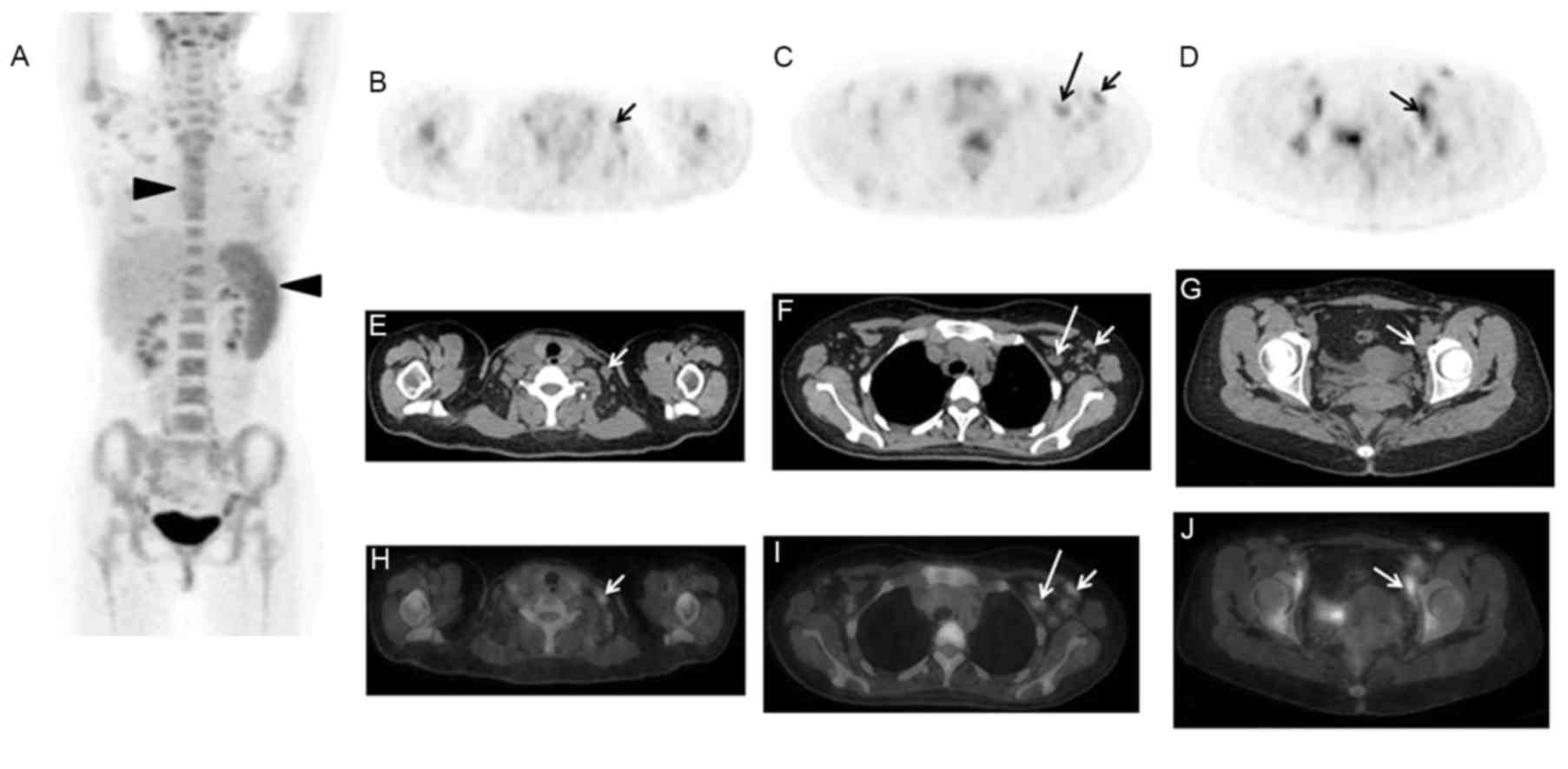
 | Figure 6.A 67-year-old female presented with
fever (Tmax of 39.0°C) for 4 weeks, and anti-inflammatory therapy
was invalid. 18F-FDG PET/CT imaging observed that
diffuse FDG uptake by the spleen and bone marrow (A: MIP, triangle
arrows), and multiple lymphadenopathy with abnormal FDG uptake in
the cervical, supraclavicle, mediastinum and lung hilar regions (B
and E, PET; C and F, CT; D and G, PET/CT; arrows). The pathology
after the biopsy of the right supraclavicle lymph node (B-D;
arrows) led to the diagnosis of non-specific inflammation. The bone
marrow biopsy indicated non-specific and mild hyperplasia of
hematopoietic cells, predominantly myeloid, and lymphocytes and
plasma cells within normal range. During the follow-up, the lymph
nodes of supraclavicle, mediastinum and lung hilar regions were
significantly decreased or disappeared on chest CT images.
18F-FDG, fluorodeoxyglucose; PET, positron emission
tomography; CT, computerized tomography; MIP, maximum intensity
projection. |
There were several limitations in the present study.
i) As a retrospective study, there may have been a substantial
selection bias on the basis of the physicians' decisions to request
18F-FDG PET/CT examinations; ii) Due to the small size
of the population in the present study, the imaging characteristics
of AOSD on 18F-FDG PET/CT could not be fully
investigated; iii) the majority of patients with AOSD respond well
to CS treatment, and other imaging modalities including ultrasound
and local CT are commonly conducted to monitor AOSD, therefore,
there is a lack of data and information concerning the follow-up
PET/CT images following the appropriate therapy for AOSD.
In conclusion, due to the non-specific imaging
features on 18F-FDG PET/CT examinations,
18F-FDG PET/CT scans could not directly aid in the
diagnosis of AOSD. The final diagnosis of AOSD is based on clinical
performance, laboratory and imaging examinations, and pathology.
However, for AOSD, 18F-FDG PET/CT serves important roles
in evaluating the involved extent, and guiding the biopsy of the
lymph nodes, bone marrow or other tissues, which may aid in the
development of novel strategies for clinical management.
Acknowledgements
The study was in part supported by the National
Science Foundation for Scholars of China (grant nos. 81271608 to Dr
Hongcheng Shi and 81571703 to Dr Lei Jiang), and funding sponsored
by Shanghai Pujiang Program (grant no. 2015PJD006) and Zhongshan
Hospital Outstanding Youth Talent Program (grant no. 2015ZSYXQN17).
The abstract of the present study was presented and published at
the Society of Nuclear Medicine and Molecular Imaging (SNMMI)
conference held in San Diego, CA, USA in June, 2016.
References
|
1
|
Efthimiou P, Paik PK and Bielory L:
Diagnosis and management of adult onset Still's disease. Ann Rheum
Dis. 65:564–572. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Choe JY, Chung DS, Park SH, Kwon HH and
Kim SK: Clinical significance of
18F-fluoro-dexoxyglucose positron emission tomography in
patients with adult-onset Still's disease: Report of two cases and
review of literatures. Rheumatol Int. 30:1673–1676. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Senthilvel E, Papadakis A, McNamara M and
Adebambo I: Adult-Onset Still Disease (AOSD). J Am Board Fam Med.
23:418–422. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Mamun AA, Sutradhar SR, Alam MB and
Bhattacharjee M: Management of adult Still's disease-an update.
Mymensingh Med J. 20:520–527. 2011.PubMed/NCBI
|
|
5
|
Fautrel B, Zing E, Golmard JL, Le Moel G,
Bissery A, Rioux C, Rozenberg S, Piette JC and Bourgeois P:
Proposal for a new set of classification criteria for adult-onset
still disease. Medicine (Baltimore). 81:194–200. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gerfaud-Valentin M, Maucort-Boulch D, Hot
A, Iwaz J, Ninet J, Durieu I, Broussolle C and Sève P: Adult-onset
still disease: Manifestations, treatment, outcome, and prognostic
factors in 57 patients. Medicine (Baltimore). 93:91–99. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Riera E, Olive A, Narváez J, Holgado S,
Santo P, Mateo L, Bianchi MM and Nolla JM: Adult onset Still's
disease: Review of 41 cases. Clin Exp Rheumatol. 29:331–336.
2011.PubMed/NCBI
|
|
8
|
Kádár J and Petrovicz E: Adult-onset
Still's disease. Best practice & research. Clin Rheumatol.
18:663–676. 2004.
|
|
9
|
Roy SG, Karunanithi S, Dhull VS, Bal C and
Kumar R: 18F-FDG PET/CT aids the diagnosis of adult
onset Still's disease in a patient with fever of unknown origin.
Rev Esp Med Nucl Imagen Mol. 33:392–393. 2014.PubMed/NCBI
|
|
10
|
Funauchi M, Ikoma S, Kishimoto K, Shimazu
H, Nozaki Y, Sugiyama M and Kinoshita K: A case of adult onset
Still's disease showing marked accumulation in the liver and
spleen, on positron emission tomography-CT images. Rheumatol Int.
28:1061–1064. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kato T, Fujii K, Wakabayashi T, Tanaka A
and Hidaka Y: A case of cutaneous polyarteritis nodosa manifested
by spiking high fever, arthralgia and macular eruption like
adult-onset Still's disease. Clin Rheumatol. 25:419–421. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Cai L, Chen Y and Huang Z: Elevated FDG
activity in lymph nodes as well as the spleen and liver in a
patient with adult-onset still disease. Clin Nucl Med.
37:1009–1010. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ahn BC, Lee SW and Lee J: Intense
accumulation of F-18 FDG in colonic wall in adult onset still
disease with pseudomembranous colitis. Clin Nucl Med. 33:806–808.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
de Graaff LC, ten Broek MR and Schweitzer
DH: Is Still's disease still one disease? A case of Adult-onset
Still's disease showing accumulation in the carotids and the large
vessels of the legs on positron emission tomography: CT images.
Rheumatol Int. 32:2487–2490. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yazisiz V and Yazisiz H: Comment on: Is
Still's disease still one disease? A case of adult-onset Still's
disease showing accumulation in the carotids and the large vessels
of the legs on positron emission tomography: CT images. Rheumatol
Int. 33:1373–1374. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Dong MJ, Wang CQ, Zhao K, Wang GL, Sun ML,
Liu ZF and Xu L: 18F-FDG PET/CT in patients with
adult-onset Still's disease. Clin Rheumatol. 34:2047–2056. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Yamashita H, Kubota K, Takahashi Y,
Minamimoto R, Morooka M, Kaneko H, Kano T and Mimori A: Clinical
value of 18F-fluoro-dexoxyglucose positron emission
tomography/computed tomography in patients with adult-onset Still's
disease: A seven-case series and review of the literature. Mod
Rheumatol. 24:645–650. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yamaguchi M, Ohta A, Tsunematsu T,
Kasukawa R, Mizushima Y, Kashiwagi H, Kashiwazaki S, Tanimoto K,
Matsumoto Y, Ota T, et al: Preliminary criteria for classification
of adult Still's disease. J Rheumatol. 19:424–430. 1992.PubMed/NCBI
|
|
19
|
Arimoto MK, Nakamoto Y, Nakatani K,
Ishimori T, Yamashita K, Takaori-Kondo A and Togashi K: Increased
bone marrow uptake of 18F-FDG in leukemia patients: Preliminary
findings. Springerplus. 4:5212015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Carr R, Barrington SF, Madan B, O'Doherty
MJ, Saunders CA, van der Walt J and Timothy AR: Detection of
lymphoma in bone marrow by whole-body positron emission tomography.
Blood. 91:3340–3346. 1998.PubMed/NCBI
|
|
21
|
Jiang L, Tan H, Panje CM, Yu H, Xiu Y and
Shi H: Role of 18F-FDG PET/CT imaging in intrahepatic
cholangiocarcinoma. Clin Nucl Med. 41:1–7. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Bywaters EG: Still's disease in the adult.
Ann Rheum Dis. 30:121–133. 1971. View Article : Google Scholar : PubMed/NCBI
|