Introduction
The number of patients suffering from burn injuries
has increased over time (1); this
type of chronic and non-healing wound, and its associated
treatment, is considered a major medical and economic issue
(2,3). Natural and synthetic drugs have been
used to treat burn injuries, in order to identify an efficient
method to control the damage. Natural remedies are considered safe
and cheap therapeutic alternatives; therefore, the demand for them
is increasing in developing countries, as well as in certain
developed countries. Various plants or animals with antibacterial
and healing properties have been identified as effective treatments
for burn injuries (4–6), including Lucilia sericata
maggots.
L. sericata maggots have been clinically used
to treat decubital necrosis; gastrointestinal problems, such as
indigestion and malnutrition; ecthyma and burn injuries since the
Ming/Qing dynasty (1368 AD) in China. This therapeutic method
became popular worldwide for the treatment of chronic and infected
wounds in the 1930s (7). Maggot
debridement therapy (MDT) is a therapeutic method that has proven
effective for the cleansing of non-healing wounds. Previous
comparative clinical trials have investigated the efficacy of MDT
(8,9), and demonstrated that MDT is more
effective compared with conventional therapies in terms of
debridement (8). Paul et al
(10) used MDT to clinically treat
diabetic foot ulcers; the findings revealed that MDT was effective
when used as a debridement technique. In addition, the ward stay
time and amputation rate were reduced in MDT-treated patients
(10). Maggots have been reported
to exert several beneficial effects on wounds, including cleansing,
disinfection, debridement and healing (11,12).
Maggot therapy has been adopted as an effective
debridement technique for the management of chronic wounds
(13,14); however, it remains cosmetically
unappealing to the majority of patients and nursing staff, and the
maggots themselves have a limited shelf life (15). For more fields to benefit from the
use of maggots, a switch to contemporary biosurgery, involving the
application of maggot-derived substances instead of live insects,
should be investigated for future treatments. A previous study
isolated and characterized the beneficial molecules in maggot
secretions, with the aim of producing them synthetically or as
recombinant proteins that may be applied as topical formulations
(15). However, a limited number
of studies have investigated the beneficial molecules in maggot
secretions and the underlying molecular mechanisms (16,17).
In the present study, antimicrobial proteins were
extracted and purified from the body of maggots and their
biological activity was investigated in vivo. In addition,
the underlying molecular mechanisms of action on second-degree burn
injury were evaluated.
Materials and methods
Sterile larvae and crude protein
extract
A laboratory colony of L. sericata flies was
obtained from Xi'an Furulin Biological Technology Co., Ltd. (Xi'an,
China) and sterile maggots were reared in our laboratory, according
to a previously described method by Mumcuoglu et al
(18). The maggots were 4–5 days
old prior to extraction of the proteins.
To extract the active ingredients from the maggots,
the maggots were frozen in liquid nitrogen and homogenized using a
mortar, subsequently the homogenate was lyophilized and the
pulverized material was dissolved in 0.1 µg/ml aprotinin in 0.1%
trifluoroacetic acid (1:10 v/v); the suspension was maintained on
ice in the dark for 1 h and centrifuged 3 times at 20,000 × g at
4°C for 30 min to remove residues. The supernatant was collected
and stored at −80°C until further use.
Purification of the crude protein
extract
To purify the crude extract, the Sephadex G-50 fine
column (26×1,000 mm; GE Healthcare Life Sciences, Chalfont, UK) was
used and the extract was eluted at 2 ml/min. Eluted components were
collected corresponding to the absorbance at 280 nm and
lyophilized. To analyze the proteins, SDS-PAGE was conducted; MAE
samples were separated on a 5.0% stacking gel and 12.5% separation
gel, followed by Coomassie staining (Nanjing Jiancheng
Bioengineering Institute). To determine the antibacterial activity
of the extract, and for the performance of other bioassays, the
fractions were dissolved in water to 50 µg/ml.
Antibacterial tests
Antibacterial activity was tested using a method
described by Huberman (19).
Briefly, Escherichia coli (ATCC 25922) was purchased from
the China Center of Type Culture Collection (Wuhan, China). E.
coli was cultured in 20 ml tryptic soy broth (TSB; BD
Biosciences, Franklin Lakes, NJ, USA) at 30°C for 17 h.
Subsequently, 100 µl culture was mixed with 10 ml TSB and incubated
for a further 4 h (density ~2×108/ml). Nutrient agar
(Oxoid, Ltd., Basingstoke, UK) was inoculated with 10 µl bacterial
culture, at a final density of 4×104/ml. After gentle
mixing, the agar was immediately distributed into Petri dishes
(85-mm). After cooling and solidification, holes (4-mm-diameter)
were bored into the agar, and 10 µl samples [aqueous extract of
maggots (MAE) P1-P7] were loaded into the holes. Sterile ultrapure
water was included as a control. Plates were incubated at 30°C
overnight and the diameters of bacterial growth inhibition were
measured.
Burn injury model and drug
administration
Male Wistar rats (n=100; age, 20±1 weeks; weight,
200–250 g) were provided by the Experimental Animal Center of the
Fourth Military Medical University (Xi'an, China). Animals were
housed in a room at a controlled temperature (25°C) under a 12 h
light/dark cycle with free access to food and water. The present
study was approved by the Ethics Committee of the Fourth Military
Medical University.
Rats were attached to a homemade wooden support and
anesthetized by 100 mg/kg ketamine and 8 mg/kg xylazine through
intraperitoneal injection. Back hair was removed and the exposed
skin was immersed in 98°C water for 15 sec to induce a
second-degree burn. A group of animals (n=8) was not burned and
served as controls. Jingwanhong ointment (JWH; Tianjin Darentang
Jingwanhong Pharmaceutical Co., Ltd., Tianjin, China) was used as a
positive control. The animals were divided into the following four
groups (n=8/group): i) Control group; ii) burn group (model); iii)
burn + MAE (0.2 g per wound) group; and iv) burn + JWH (0.2 g per
wound) group. All the tested medicines were applied on the surface
of the wound slowly. The wounds were treated every 24 h for 14
days. To evaluate effects of MAE-P1-P7 on burn wound, MAE-P1-P7
(0.2 g per wound; n=8 rats/treatment) was administered to rats in
the burn + MAE group. In some experiments, LY294002 (Sigma-Aldrich;
Merck KGaA, Darmstadt, Germany) was intraperitoneally administered
together with MAE-P6, at a dose of 0.3 mg/kg. The burn wound area
was observed after all treatments on the 14th day and the rats were
anesthetized with ketamine (75 mg/kg) and sacrificed by
decapitation. Blood was subsequently collected, and wound tissues
were collected and frozen at −80°C until use.
Determination of hydroxyproline
levels
A hydroxyproline assay was used to quantify collagen
deposition in the wound area. Tissue samples (7 mg) were obtained,
subcutaneous fat was removed, and they were incubated at 60°C in
open microtubes for 20 h to obtain the dry weight. Subsequently,
the samples were hydrolyzed with 6 mol/l HCl by stirring for 15 h
at 120°C. The lysate was diluted with deionized water and
neutralized with NaOH. Subsequently, the lysate was centrifuged at
1,000 × g at 25°C for 15 min, and the supernatant was collected for
hydroxyproline assay. The hydroxyproline levels were quantified
using the hydroxyproline assay kit (catalog no. A030-1; Nanjing
Jiancheng Bioengineering Institute), according to the
manufacturer's protocol. Hydroxyproline levels were expressed as
mg/g of tissue.
Determination of malondialdehyde (MDA)
levels
MDA is an index of lipid peroxidation. The MDA level
was quantified using a commercial kit (catalog no. A003; Nanjing
Jiancheng Bioengineering Institute), which results in the formation
of thiobarbituric acid-reactive substances during an acid-heating
reaction. To precipitate proteins, tissue samples were mixed with
600 µl 10% (w/v) trichloroacetic acid and then centrifuged at 1,000
× g for 10 min at 25°C. Supernatants were collected and treated
with an equal volume of 0.67% thiobarbituric acid in a boiling
water bath for 15 min. After cooling for 5 min the reaction
products were measured at 535 nm. MDA
(nmol/mg)=(ODtest-ODblank)/(ODstandard-ODblank)x10/protein
concentration, where OD refers to optical density. The level of MDA
was expressed as nmol/mg of protein.
Determination of superoxide dismutase
(SOD) levels
The enzyme activity of SOD was quantified using a
spectrophotometric assay kit (catalog no. A001-3; Nanjing Jiancheng
Bioengineering Institute), according to the manufacturer's
protocol. Briefly, the proteins in the tissue samples were
extracted using a protein extraction kit (catalog no. P0033;
Beyotime Institute of Biotechnology, Nanjing, China). The protein
samples were incubated with the provided radical detector reagent
and xanthine oxidase was subsequently added to initiate the
reaction. Following incubation at room temperature for 20 min with
agitation, the reaction system was measured at 450 nm. SOD (U/mg
prot)=(ODstandard-ODtest)/ODstandard/0.5/protein
concentration, where OD refers to optical density. The levels of
SOD were expressed as U/mg of protein.
Determination of serum levels of tumor
necrosis factor-α (TNF-α) and interleukin-6 (IL-6)
Blood samples were collected 14 days after burns. To
separate serum, blood samples were maintained at room temperature
for 1 h, and were centrifuged at 1,000 × g for 10 min at 25°C.
Serum levels of TNF-α and IL-6 were quantified using rat TNF-α
ELISA kit (catalog no. PT516) and rat IL-6 ELISA kit (catalog no.
PI328; Beyotime Institute of Biotechnology), according to the
manufacturer's protocols. The level was expressed as ng/l.
Western blot analysis
Proteins in excised tissues were homogenized using a
protein extraction kit (catalog no. P0033; Beyotime Institute of
Biotechnology) and were centrifuged at 12,000 × g for 15 min at
4°C. Protein concentration was determined using a bicinchoninic
acid kit (catalog no. A045-3; Nanjing Jiancheng Bioengineering
Institute). The supernatant was then collected, mixed with 2X SDS
loading buffer and denatured at 100°C for 5 min. Equal amounts of
protein (40 µg) were separated by 10% SDS-PAGE. Subsequently the
proteins were transferred to nitrocellulose membranes (Pall
Corporation, New York, NY, USA), which were blocked with 5% non-fat
dry milk in 1X Tris-buffered saline. The membranes were then
incubated with Akt (catalog no. ab79360), phosphorylated (p)-Akt
(catalog no. ab81283), nuclear factor (NF)-κB (catalog no. ab28856)
and vascular endothelial growth factor A (VEGFA; catalog no.
ab51745) rabbit anti-rat monoclonal antibodies (1:1,000; Abcam,
Cambridge, UK) at 4°C for 8 h and were then incubated with
horseradish peroxidase-conjugated anti-rabbit secondary antibody
(catalog no. sc-2357; 1:5,000; Santa Cruz Biotechnology, Inc.,
Dallas, TX, USA) or horseradish peroxidase-conjugated anti-mouse
secondary antibody (catalog no. ab97255; 1:5,000; Abcam). β-actin
(1:1,000; catalog no. ab8226; Abcam) was used as a control. All
bands were detected by enhanced chemiluminescence (ECL) using the
ECL Western Blot detection kit (GE Healthcare Life Sciences).
Western blots were semi-quantified by densitometric analysis using
Quantity One 1-D software (Bio-Rad Laboratories, Inc., Hercules,
CA, USA).
Analysis of microvessel density (MVD)
and VEGFA expression
After the rats were anesthetized with ketamine, 4%
paraformaldehyde was routinely perfused through left ventricle for
1 h, and wound tissue was collected and fixed in 4%
paraformaldehyde for 24 h. Sections (5.0 µm) were obtained from
paraffin-embedded tissues, and were then deparaffinized and
rehydrated. To block endogenous peroxidase activity, sections were
treated with 3% 2O2 methanol solution for 10
min at room temperature. For antigen retrieval, sections were
boiled in 0.01 mol/l citric acid for 20 min and blocked with 3%
skim milk powder solution for 30 min at 37°C. The sections were
then washed with PBS and incubated with cluster of differentiation
(CD)31 monoclonal antibody (catalog no. sc-376764) or rabbit
anti-rat VEGFA (catalog no. sc-152) monoclonal antibody (1:10;
Santa Cruz Biotechnology, Inc.) at 37°C for 1 h. Sections were
washed with PBS, incubated with biotinylated goat anti-mouse
(1:100; catalog no. BA1001) and biotinylated goat anti-rabbit
secondary antibody (1:100; catalog no. BA1003; Boster Biological
Technology Co., Ltd., Zhongshan, China) for 30 min at 37°C and were
subsequently incubated with horseradish peroxidase-labeled
streptavidin (catalog no. BA1088; Boster Biological Technology Co.,
Ltd.) for 30 min at 37°C. Sections were stained with
3,3′-diaminobenzidine/H2O2 and hematoxylin,
dehydrated, cleared and mounted for viewing. The quantity of
CD31-positive small vessels was observed under a microscope (×400
magnification; DM2500; Leica Microsystems GmbH, Wetzlar, Germany)
to determine MVD. The number of counted microvessels per
mm2 was considered the MVD. MVD of a sample was
calculated as the average MVD of five selected areas. An additional
five areas were randomly selected for VEGFA analysis. To calculate
VEGFA expression, integrated optical density and density mean of
positive expression were used; the images were analyzed with Image
Pro Plus version 6.0 (Media Cybernetics, Inc., Rockville, MD, USA).
Data were recorded as fold-change.
Statistical analysis
Each experiment was repeated at least three times.
Data are presented as the mean ± standard deviation. SPSS version
18.0 (SPSS Inc., Chicago, IL, USA) was used to analyze the data.
Statistically significant differences between treatment groups were
determined by one-way analysis of variance, followed by Tukey test
for multiple comparisons between groups. P<0.05 was considered
to indicate a statistically significant difference.
Results
MAE reduces the size of the wound
area
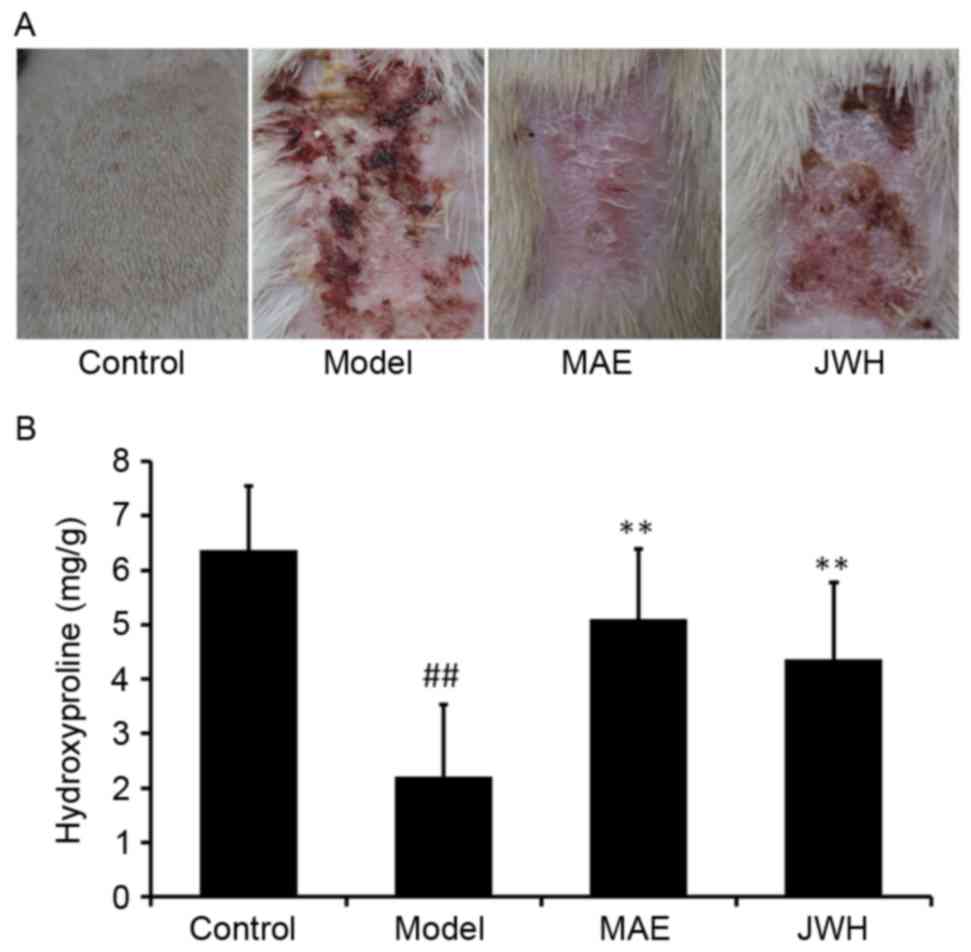
To evaluate the effects of MAE treatment on burn
wound closure, wound contraction was measured. As presented in
Fig. 1A, an increase in
wound-healing activity was observed in the rats treated with MAE
and JWH, as compared with the burn model rats that did not receive
treatment. In addition, it was demonstrated that the wound-healing
activity of MAE was greater compared with JWH.
Hydroxyproline, which is integral to collagen
fibers, may promote wound healing in tissue injury (20). In various wound models, an increase
in hydroxyproline content may indicate increased collagen
synthesis. In the burn wound model, the level of hydroxyproline in
granulation tissue was significantly reduced compared with in the
control group (Fig. 1B;
P<0.05). However, MAE and JWH treatment significantly increased
the hydroxyproline level compared with the model group (P<0.05).
These findings suggested that MAE may be an effective treatment
option for second-degree burns.
Partial purification and
characterization of the antibacterial components of MAE
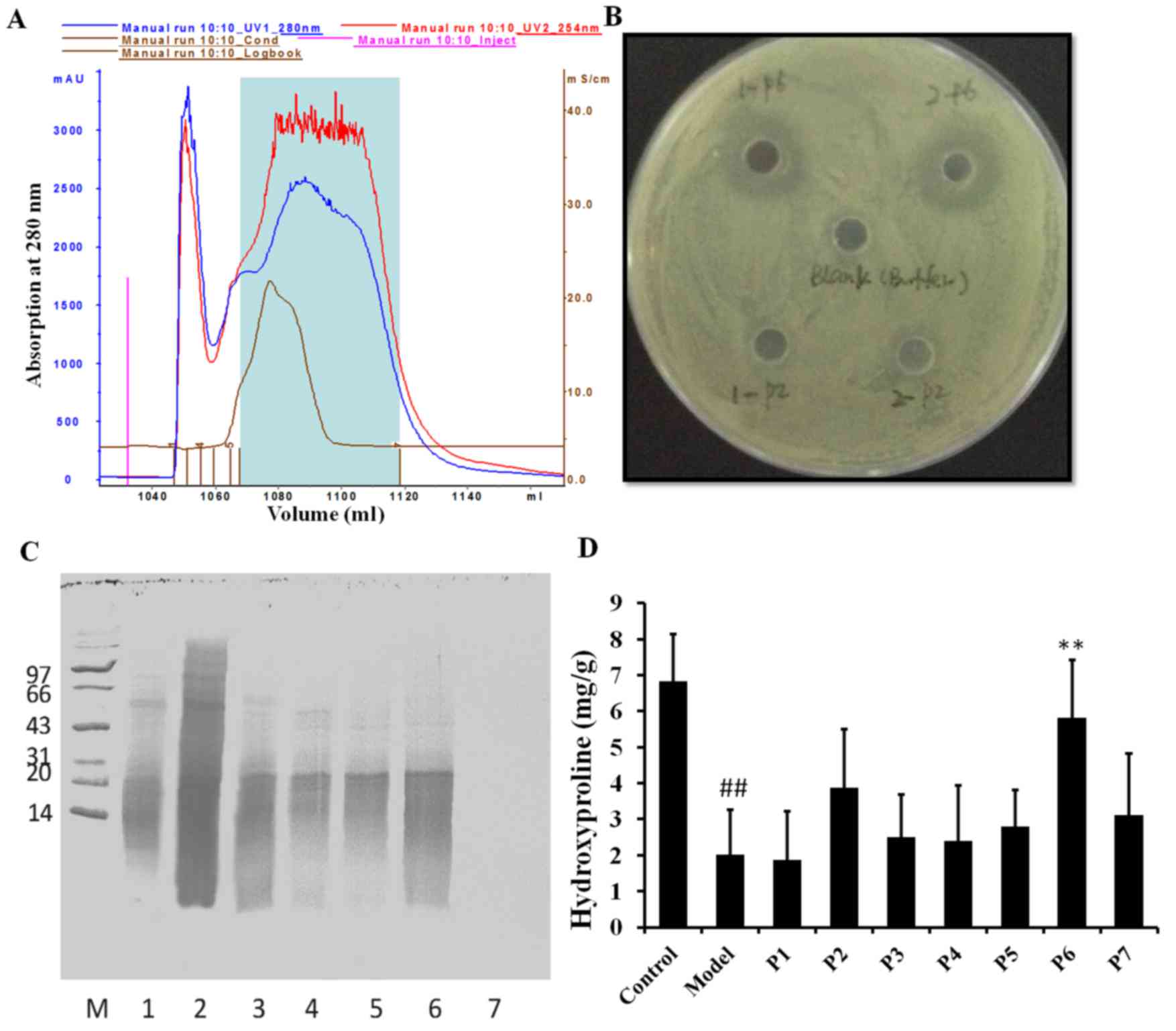
In order to identify the major active ingredients in
MAE, Sephadex G-50 fine column was previously used (21). Different components were identified
according to their UV absorption characteristics (Fig. 2A). Finally, a total of 7 compounds
were collected. Antibacterial tests demonstrated that compound 6
(MAE-P6) had a high antibacterial activity, whereas the remaining
compounds had little or no antibacterial activity (Fig. 2B). Examination of these fractions
by SDS-PAGE revealed that the majority of proteins in the MAE-P6
were <20 kDa molecular weight (Fig.
2C). In order to determine if the various compounds exert
anti-burn activity, MAE-P1-P7 were used to treat rats in the burn
wound model group. The results demonstrated that MAE-P6 treatment
significantly increased hydroxyproline levels compared with the
burn model (P<0.05); however, no significant difference was
identified between the remaining compounds and the burn model
(Fig. 2D). Therefore, MAE-P6 may
be responsible for the antibacterial activity and healing
properties of MAE. MAE-P6 was used for the subsequent
experiments.
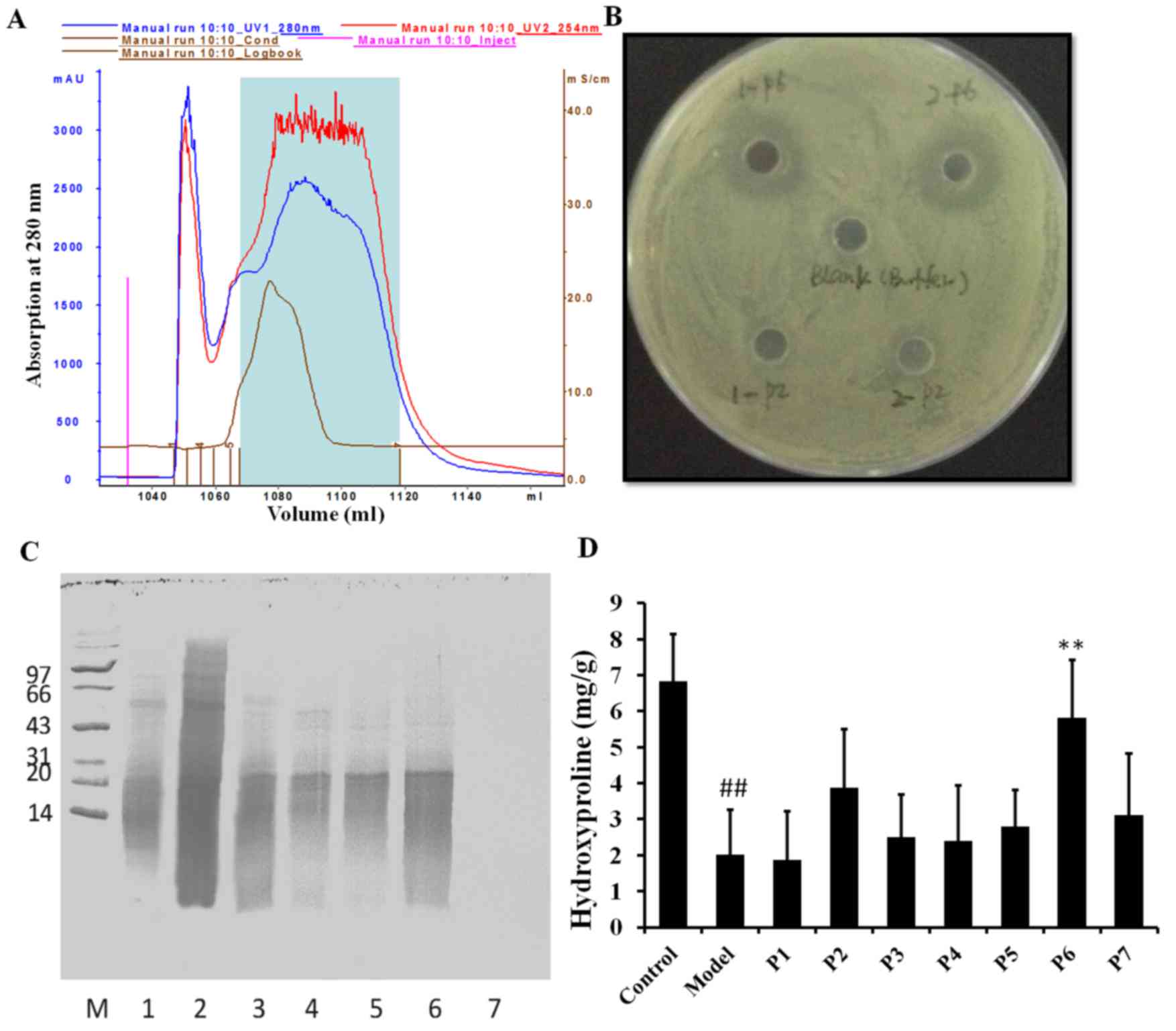 | Figure 2.Partial purification and
characterization of antibacterial components of MAE. (A) UV
absorption characteristics of the various components. (B)
Antibacterial tests. Various components (P1-P7) were tested on
Escherichia coli (dose, 50 µg/ml). The antibacterial
activity of P2 and P6 is presented. (C) SDS-PAGE analysis of the
different components. Lane 1, P1; lane 2, P2; lane 3, P3; lane 4,
P4; lane 5, P5; lane 6, P6; lane 7, P7. (D) Effects of MAE P1-P7 on
hydroxyproline levels in the burn wound model. Data are expressed
as the mean ± standard deviation. ##P<0.05 vs. the
control group, **P<0.05 vs. the model group. MAE, aqueous
extract of maggots. |
Effects of MAE on oxidative damage and
inflammation
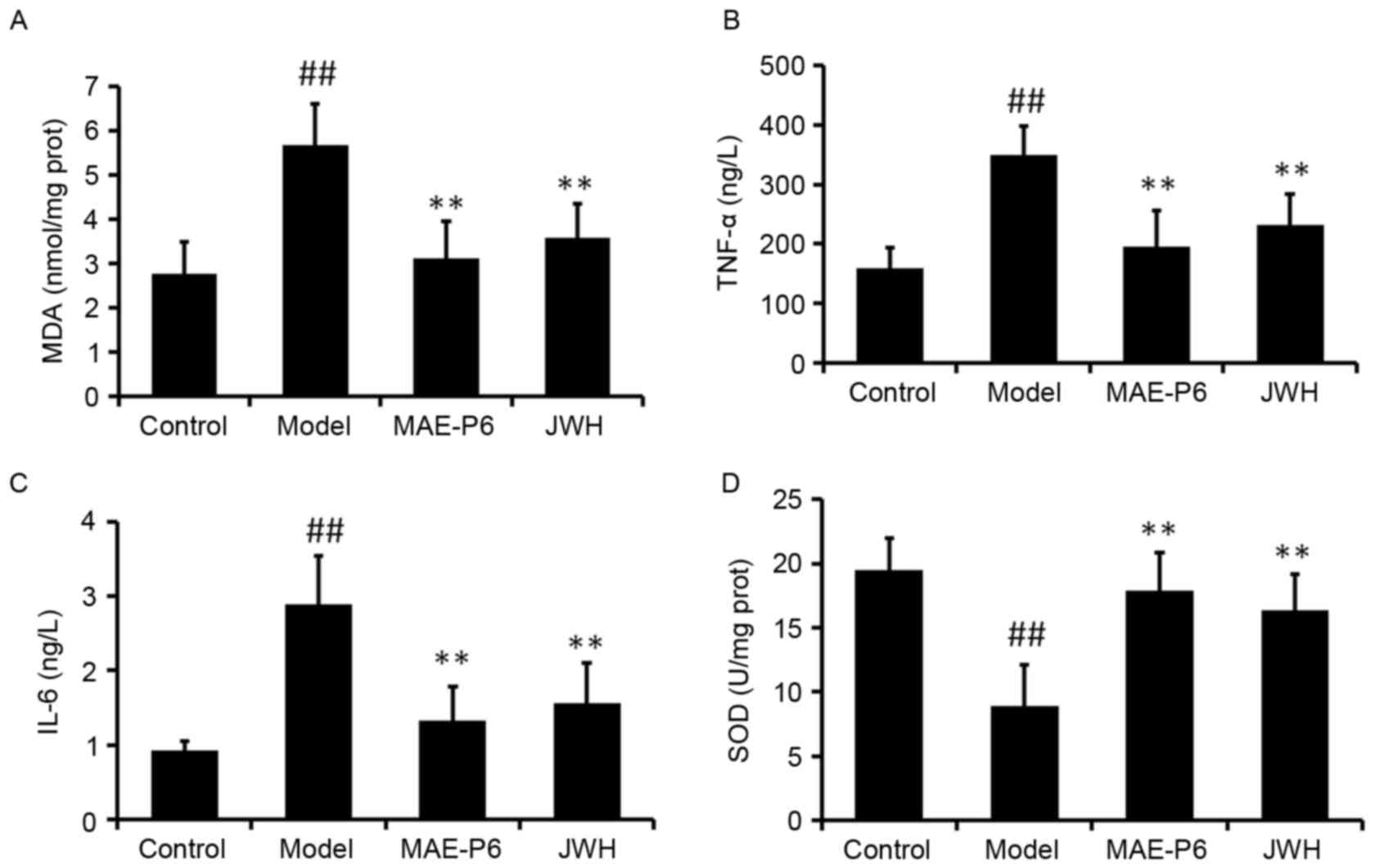
High intracellular levels of reactive oxygen species
(ROS), which occur during the initial stages following a burn
injury, have been identified as the inducers of oxidative damage. A
previous study suggested that topical application of antioxidants
may provide a photoprotective effect and may be considered an
effective strategy for reducing burn-induced oxidative damage to
the skin (22). The level of MDA
is an indication of lipid peroxidation in tissues. The findings of
the present study demonstrated that treatment with MAE-P6
significantly reduced the burn-mediated increase of epidermal MDA
when compared with the model group (Fig. 3A; P<0.05). Following a burn
injury, inflammatory cells are recruited to the wound site,
initiating the inflammatory stage of the healing process (23). The present study examined the
effects of MAE-P6 on burn-induced expression levels of cytokines
TNF-α and IL-6. A significant increase in the levels of TNF-α and
IL-6 was observed following the administration of the burn compared
with the control group (Fig. 3B and
C; P<0.05). However, topical application of MAE-P6 for 14
days post-burn significantly reduced the levels of IL-6 and TNF-α
compared with in the burn model group (Fig. 3B and C; P<0.05). SOD acts as the
first line of defense against superoxide anions (O2•),
by dismutating these anions to H2O2. SOD
activity was significantly reduced in the burn model group compared
with the control group (Fig. 3D;
P<0.05). However, this activity was significantly increased
following 14 days of treatment with MAE-P6 when compared with the
burn model group (Fig. 3D;
P<0.05). These findings revealed that MAE-P6 was able to reduce
levels of oxidative stress in the rats, potentially limiting the
damaging effect of ROS following burn administration.
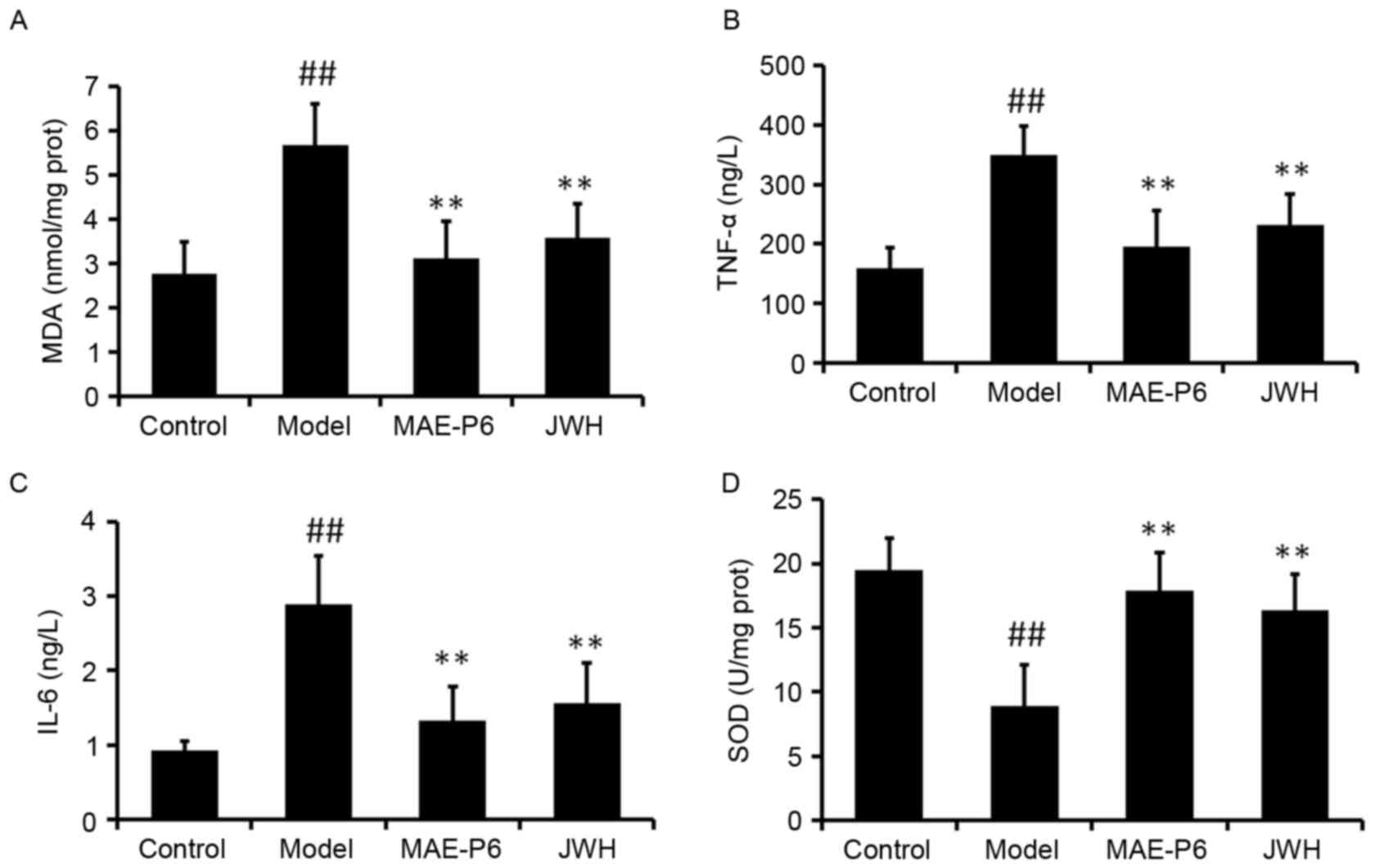 | Figure 3.Effects of MAE-P6 on oxidative damage
and inflammation. The levels of (A) MDA, (B) TNF-α and (C) IL-6
were increased, whereas the levels of (D) SOD were decreased in the
burn model. Application of MAE-P6 following burn treatment led to a
significant increase in the activity of SOD and a reduction in the
levels of MDA, TNF-α and IL-6 after 14 days of treatment. Data are
expressed as the mean ± standard deviation. ##P<0.05
vs. the control group, **P<0.05 vs. the model group. MDA,
malondialdehyde; MAE-P6, aqueous extract of maggots-compound 6;
JWH, Jingwanhong ointment; TNF-α, tumor necrosis factor-α; IL-6,
interleukin-6; SOD, superoxide dismutase. |
Effects of MAE on MVD and VEGFA
expression
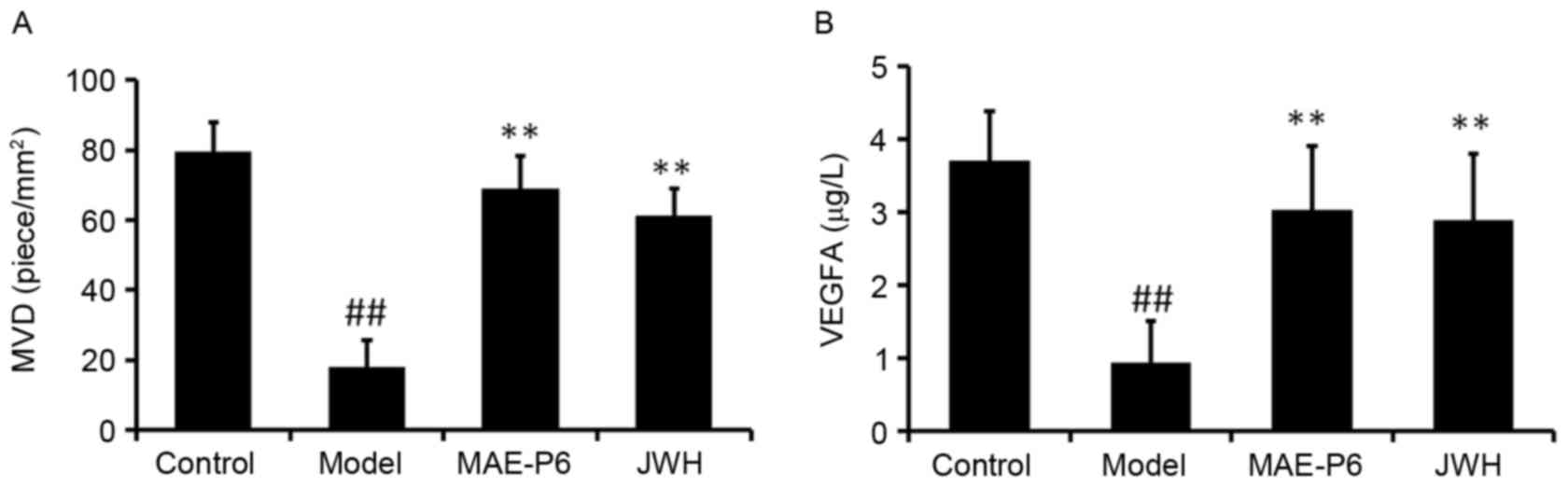
MVD and VEGFA levels in the model group were
significantly reduced compared with in the control group 14 days
after the burn was administered (Fig.
4; P<0.05). MVD and VEGFA levels in the MAE-P6 and JWH
groups were significantly higher compared with in the model group
(Fig. 4; P<0.05). In addition,
the MVD and VEGFA levels in the MAE-P6 group were slightly higher
when compared with the JWH group, but had no significant
difference.
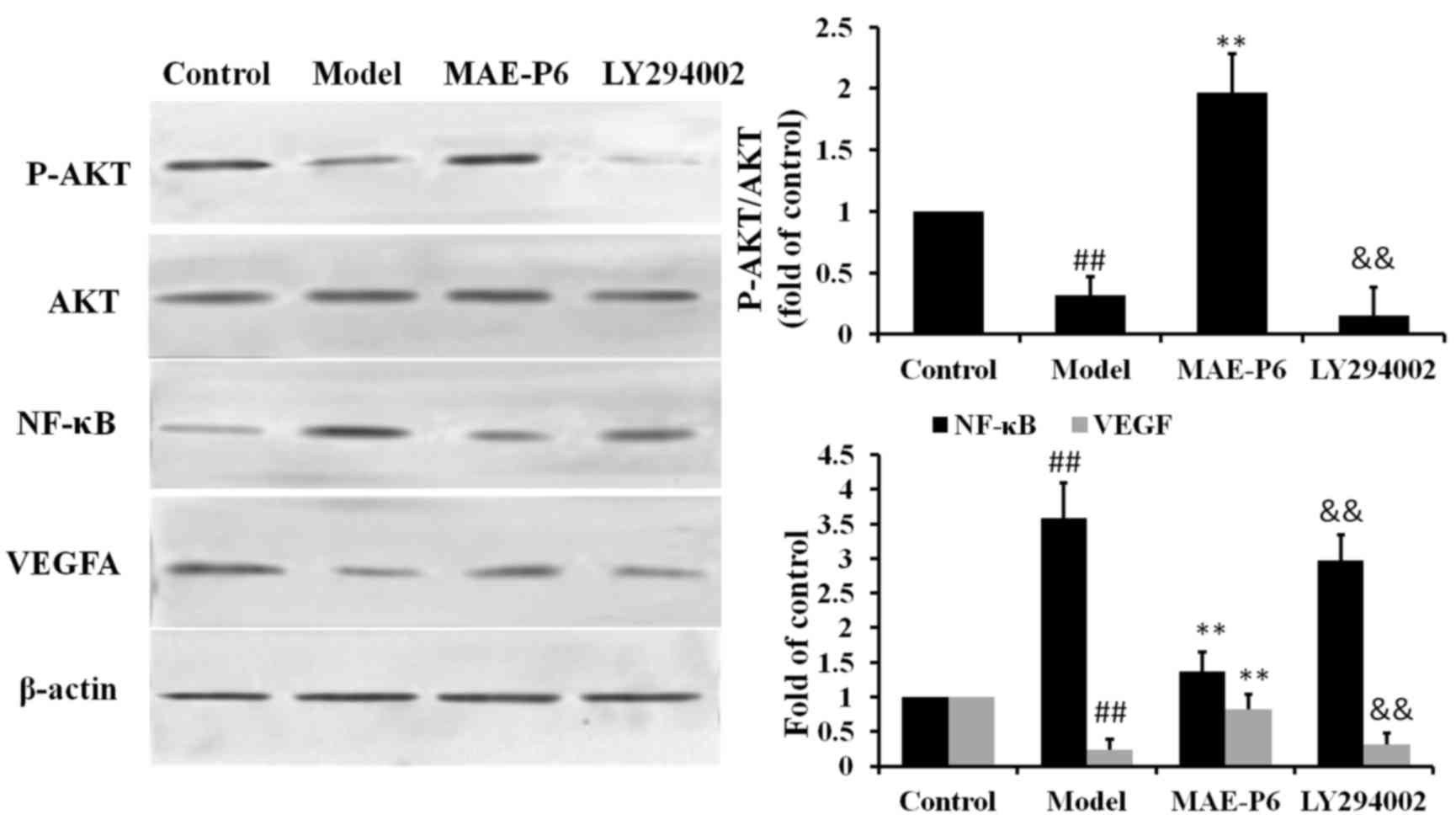
Effects of MAE on the expression
levels of Akt, NF-κB and VEGFA
The Akt signaling pathway regulates numerous
physiological processes associated with apoptosis, oxidative stress
and inflammation (24). Therefore,
the present study determined the effects of topical administration
of MAE-P6 on the phosphorylation of Akt following burn
administration using western blot analysis. The findings indicated
that phosphorylation of Akt was significantly reduced post-burn, as
compared with in the control group (Fig. 5; P<0.05). Conversely, MAE-P6
treatment significantly increased phosphorylation of Akt compared
with the burn model group (Fig. 5;
P<0.05).
NF-κB is a downstream target of the Akt signal
transduction pathway. Western blot analysis indicated that the
expression of NF-κB was significantly increased in the burn model
group compared with in the control group (Fig. 5; P<0.05). Topical application of
MAE-P6 significantly reduced the burn-induced increase in NF-κB
expression. In addition, the effects of MAE-P6 on the possible
regulation of VEGFA signaling were investigated. MAE-P6 reversed
the downregulation of VEGFA protein expression, which occurred
following burn exposure (Fig. 5).
Furthermore, inhibition of Akt by LY294002 eliminated these
effects. These findings indicated that MAE-P6 possibly inhibited
NF-κB expression and increased VEGFA expression via phosphorylation
of the Akt signaling pathway.
Discussion
Burns represent a devastating form of trauma, which
are associated with severe pain, distress and reduced quality of
life for numerous patients worldwide. Thermal injury may severely
compromise the skin barrier, affecting important functions, such as
protection against infection, thermoregulation and body fluid
homeostasis (25,26). Effective treatments associated with
wound infection control and wound healing are important for a
successful recovery (27). Burn
wound healing is categorized into three overlapping stages: i)
Inflammation; ii) granulation tissue formation; and iii) remodeling
(19). Therefore, acceleration of
the rate of tissue regeneration, inhibition of inflammation or
oxidative stress, and prevention of wound infection are crucial
procedures for burn treatment (28). Natural products, such as insects or
plants, may be considered promising for the treatment of burn
injuries, and may be used worldwide. A particularly interesting
therapeutic strategy in traditional Chinese medicine is the use of
maggots, which are the larvae of insects and terrestrial
arthropods; however, only a small number of studies regarding this
treatment strategy are available (13,14).
The present study aimed to determine the burn wound healing and
antibacterial properties of MAE in rats, and observed that MAE
treatment accelerated wound contraction 14 days after burn
administration, indicating the beneficial effects of this
therapeutic agent.
Fibroblasts, which are responsible for the
deposition, synthesis and remodeling of the extracellular matrix,
are the primary cell type involved in the wound healing process
(29). At the initiation of wound
repairing, fibroblasts undergo in situ proliferation and
differentiation, then migrate from the edges of the wound to the
wound site, proliferate again and begin to produce collagen
(30). In the healing phase,
collagen content in the granulation tissue may be quantified by
monitoring the concentration of hydroxyproline, which is a marker
of collagen biosynthesis (31).
Therefore, the levels of hydroxyproline represent the rate of
collagen synthesis. In the present study, 14 days after treatment,
an increase in hydroxyproline content was observed in the MAE group
(5.11±1.28 mg/g dry weight of tissue), which was significantly
higher compared with in the model group (2.21±1.32 mg/g). These
findings indicated that collagen synthesis was improved by
treatment with MAE. Therefore, the wound healing effects of MAE
treatment may be due to increases in collagen content.
Bacterial infections may occur at the early stages
of wound healing, which may delay healing, and lead to failure of
healing or wound deterioration (31). Pathogenic microorganisms delay
wound healing via various mechanisms, including persistent
production of inflammatory mediators, induction of tissue hypoxia,
production of cytolytic enzymes and free oxygen radicals, and
competitive inhibition of nutrient and oxygen levels (32). Therefore, keeping the wound clean
in order to avoid infection or maintaining a good bioburden is
necessary for successful wound healing. The present study
identified seven compounds isolated from MAE and their
bacteriostatic action on Gram-negative bacterial growth was
evaluated. As the findings of the present study demonstrated,
compound P6 (MAE-P6) exerted a significantly greater antibacterial
effect compared with the remaining six compounds. Further
investigation revealed that MAE-P6 may increase the levels of
hydroxyproline in the wound healing model. Therefore, the
antibacterial activity of MAE-P6 may reduce the number of pathogens
growing on the skin, thus promoting wound healing.
Exposure to a pathogenic microorganism may activate
neutrophils, which produce ROS and lead to oxidative stress. In
burns, oxidative stress is a pathogenic factor in the inflammatory
response; the excessive production of free radicals recruits
inflammatory cells and may lead to endothelial dysfunction
(33). However, antioxidants, such
as SOD, catalase and glutathione, may eliminate free radicals and
accelerate the process of burn wound healing. So it is necessary to
estimate these antioxidants in granulation tissues. Significant
alterations in the antioxidant profile, combined with elevated
levels of MDA, which is a marker of fatty acid oxidation, may lead
to impaired wound healing in rats (34). In the present study, the levels of
SOD and MDA were quantified in the granulation tissue. The results
demonstrated that treatment with MAE-P6 significantly increased the
activity of SOD, and reduced the levels of MDA compared with in the
burn model group. Notably, MAE-P6 treatment also inhibited the
expression levels of the inflammatory cytokines IL-6 and TNF-α.
The surface of burn wounds may be anoxic or hypoxic;
both conditions limit the growth of ulcerated or injured tissues.
Therefore, treatment that may improve the microcirculation of the
burn wound may also improve partial ischemia and hypoxia, and
promote healing. VEGFA has previously been described as an
important stimulator of angiogenesis and vasopermeability, and is
produced by macrophages in the hypoxic burn environment, in order
to stimulate the migration and proliferation of endothelial cells
(35,36). In the present study, the increase
in VEGF and MVD levels coincided with a faster decrease of the
wound area (Fig. 4), thus
suggesting the importance of angiogenic stimulation by MAE-P6 in
the overall acceleration of wound healing.
The possible signaling molecules were also
investigated in the present study, in order to determine the
potential regulatory targets associated with MAE-P6. The
phosphorylation of Akt, which is considered a crucial node of the
phosphoinositide 3-kinase-Akt pathway, may be regarded as a cell
survival factor via the inhibition of apoptosis and downstream
NF-κB, resulting in the inhibition of inflammation and oxidative
stress (37,38). The findings of the present study
revealed that the post-burn reduction in p-Akt was accompanied by
an increased release of IL-6 and TNF-α, and an increase in the
expression levels of NF-κB. Conversely, MAE-P6 administration led
to increased expression levels of p-Akt and reduced NF-κB
expression levels. Inhibition of Akt with LY294002 attenuated the
expression of p-Akt and increased the expression of NF-κB.
Therefore, it may be hypothesized that the Akt/NF-κB signaling
pathway contributes to MAE-P6-induced inflammatory regulation in
burn wounds. Furthermore, inhibition of Akt with LY294002 also
inhibited the expression of VEGFA, whereas rats treated with MAE-P6
only exhibited increased expression of VEGFA.
In conclusion, to the best of our knowledge, the
present study was the first to demonstrate the beneficial effects
of MAE on burn wound healing via its antibacterial, antioxidative
and anti-inflammatory activities. It is possible that MAE-P6
functions via the Akt/NF-κB signaling pathway to regulate the
release of inflammatory cytokines and free radicals. MAE-P6 may
also regulate angiogenesis and vasopermeability via the Akt/VEGFA
pathway. The findings of the present study suggested that MAE-P6
has multi-target mechanisms for improving burn wound healing, and
may provide useful information for the development of burn wound
healing treatments.
Acknowledgements
The present study was supported by the National
Science Foundation of China (grant nos. 81470174, 81173514,
81303264, 81403134, 81403135 and 81403182) and the Xijing Research
Boosting Program (grant no. XJZT14D06).
References
|
1
|
Mogoşanu GD and Grumezescu AM: Natural and
synthetic polymers for wounds and burns dressing. Int J Pharm.
463:127–136. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Lay-flurrie K: Honey in wound care:
Effects, clinical application and patient benefit. Br J Nurs.
17:S30–S36. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Riedel K, Ryssel H, Koellensperger E,
Germann G and Kremer T: Pathogenesis of chronic wounds. Chirurg.
79:526–534. 2008.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ghasemi Pirbalouti A: Medicinal plants
used in Chaharmahal and Bakhtyari districts. Iran Herba Pol.
55:34–38. 2009.
|
|
5
|
Nayak BS, Isitor G, Davis EM and Pillai
GK: The evidence-based wound healing activity of Lawsonia inermis
Linn. Phytother Res. 21:827–831. 2007. View
Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bahramsoltani R, Farzaei MH and Rahimi R:
Medicinal plants and their natural components as future drugs for
the treatment of burn wounds: An integrative review. Arch Dermatol
Res. 306:601–617. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hou L, Shi Y, Zhai P and Le G:
Antibacterial activity and in vitro anti-tumor activity of the
extract of the larvae of the housefly (Musca domestica). J
Ethnopharmacol. 111:227–231. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sherman RA: Maggot versus conservative
debridement therapy for the treatment of pressure ulcers. Wound
Repair Regen. 4:208–214. 2002. View Article : Google Scholar
|
|
9
|
Dumville JC, Worthy G, Bland JM, Cullum N,
Dowson C, Iglesias C, Mitchell JL, Nelson EA, Soares MO and
Torgerson DJ: VenUS II team: Larval therapy for leg ulcers (VenUS
II): Randomised controlled trial. BMJ. 338:b7732009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Paul AG, Ahmad NW, Lee HL, Ariff AM,
Saranum M, Naicker AS and Osman Z: Maggot debridement therapy with
Lucilia cuprina: A comparison with conventional debridement in
diabetic foot ulcers. Inter Wound J. 6:39–46. 2009. View Article : Google Scholar
|
|
11
|
Wollina U, Liebold K, Schmidt WD, Hartmann
M and Fassler D: Biosurgery supports granulation and debridement in
chronic wounds-clinical data and remittance spectroscopy
measurement. Int J Dermatol. 41:635–639. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Huberman L, Gollop N, Mumcuoglu KY, Block
C and Galun R: Antibacterial properties of whole body extracts and
haemolymph of Lucilia sericata maggots. J Wound Care. 16:123–127.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Pinheiro MA, Ferraz JB, Junior MA, Moura
AD, da Costa ME, Costa FJ, Neto VF, Neto RM and Gama RA: Use of
maggot therapy for treating a diabetic foot ulcer colonized by
multidrug resistant bacteria in Brazil. Indian J Med Res.
141:340–342. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Nigam Y and Morgan C: Does maggot therapy
promote wound healing? The clinical and cellular evidence. J Eur
Acad Dermatol. 30:776–782. 2016. View Article : Google Scholar
|
|
15
|
Vilcinskas A: From traditional maggot
therapy to modern biosurgeryInsect Biotechnology. Vilcinskas A:
Dordrecht, Netherlands: Springer; pp. 67–755. 2011, View Article : Google Scholar
|
|
16
|
Bohova J, Majtan J, Majtan V and Takac P:
Selective antibiofilm effects of Lucilia sericata larvae
secretions/excretions against wound pathogens. Evid Based
Complement Alternat Med. 2014:8573602014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hultmark D: Techniques in Insect
Immunology. Weisner A, Dunphy GB, Marmaras VJ, Morishima I,
Sugumaran M and Yamakawa M: SOS Publications; New Jersey: pp.
103–1075. 1998
|
|
18
|
Mumcuoglu KY, Ingber A, Gilead L, Stessman
J, Friedmann R, Schulman H, Bichucher H, Ioffe-Uspensky I, Miller
J, Galun R and Raz I: Maggot therapy for the treatment of
intractable wounds. Int J Dermatol. 8:623–627. 1999. View Article : Google Scholar
|
|
19
|
Huberman L, Gollop N, Mumcuoglu KY, Block
C and Galun R: Antibacterial properties of whole body extracts and
haemolymph of Lucilia sericata maggots. J Wound Care. 16:123–127.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Morellini NM, Giles NL, Rea S, Adcroft KF,
Falder S, King CE, Dunlop SA, Beazley LD, West AK, Wood FM and Fear
MW: Exogenous metallothionein-IIA promotes accelerated healing
after a burn wound. Wound Repair Regen. 16:682–690. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Lu J and Chen ZW: Isolation,
characterization and anti-cancer activity of SK84, a novel
glycine-rich antimicrobial peptide from Drosophila virilis.
Peptides. 31:44–50. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Sen CK: The general case for redox control
of wound repair. Wound Repair Regen. 11:431–438. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Guo S and Dipietro LA: Factors affecting
wound healing. J Dent Res. 89:219–229. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Hassan B, Akcakanat A, Holder AM and
Meric-Bernstam F: Targeting the PI3-kinase/Akt/mTOR signaling
pathway. Surg Oncol Clin N Am. 22:641–664. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Hettiaratchy S and Dziewulski P: ABC of
burns. BMJ. 328:1366–1368. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Church D, Elsayed S, Reid O, Winston B and
Lindsay R: Burn wound infections. Clin Microbiol Rev. 19:403–434.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
DeSanti L: Pathophysiology and current
management of burn injury. Adv Skin Wound Care. 18:323–332. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Rowan MP, Cancio LC, Elster EA, Burmeister
DM, Rose LF, Natesan S, Chan RK, Christy RJ and Chung KK: Burn
wound healing and treatment: Review and advancements. Critical
Care. 19:2432015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Hinz B: The myofibroblast: Paradigm for a
mechanically active cell. J Biomech. 43:146–155. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Werner S, Krieg T and Smola H:
Keratinocyte-fibroblast interactions in wound healing. J Invest
Dermatol. 127:998–1008. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Guo S and Dipietro LA: Factors affecting
wound healing. J Dent Res. 89:219–229. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Macri L and Clark RA: Tissue engineering
for cutaneous wounds: Selecting the proper time and space for
growth factors, cells and the extracellular matrix. Skin Pharmacol
Physiol. 22:83–93. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Richelle M, Sabatier M, Steiling H and
Williamson G: Skin bioavailability of dietary vitamin E,
carotenoids, polyphenols, vitamin C, zinc and selenium. Br J Nutr.
96:227–238. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Gupta A, Singh RL and Raghubir R:
Antioxidant status during cutaneous wound healing in
immunocompromised rats. Mol Cell Biochem. 241:1–7. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Mast BA and Schultz GS: Interactions of
cytokines, growth factors and proteases in acute, and chronic
wounds. Wound Repair Regen. 4:411–420. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Distler JH, Hirth A, Kurowska-Stolarska M,
Gay RE, Gay S and Distler O: Angiogenic and angiostatic factors in
the molecular control of angiogenesis. Q J Nucl Med. 41:149–161.
2003.
|
|
37
|
Baehrecke EH: Autophagy: Dual roles in
life and death? Nat Rev Mol Cell Biol. 6:505–510. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Sarkar S: Regulation of autophagy by
mTOR-dependent and mTOR-independent pathways: Autophagy dysfunction
in neurodegenerative diseases and therapeutic application of
autophagy enhancers. Biochem Soc Trans. 41:1103–1130. 2013.
View Article : Google Scholar : PubMed/NCBI
|