Introduction
Myocardial ischemia-reperfusion (IR) injury often
occurs following cardiovascular surgery (1). This results from coronary blood
supply, which is produced by thrombosis or coronary atherosclerotic
plaques (2). The imbalance between
oxygen supply and demand from the ischemic organ facilitates the
production of oxygen free radicals, inflammatory cytokines and
other proinflammatory mediators, which leads to severe tissue
damage (3,4).
During cardiac surgery, myocardial protection
techniques, such as cardioplegia and hypothermia, are applied to
reduce the severity of the myocardial IR injury. The lowered
temperature protects the ischemic heart by reducing cellular
metabolism and the oxygen demand of the tissue. It also increases
tolerance of metabolic waste accumulation (5). However, there still remains the
problem of IR injury-related cardiac dysfunction.
GV1001 is a novel vaccine peptide derived from the
human telomerase reverse transcriptase (hTERT) corresponding to
amino acids 611–626 of hTERT (6).
It is a 16-amino acid peptide with the following sequence;
Glu-Ala-Arg-Pro-Ala-Leu-Leu-Thr-Ser-Arg-Leu-Arg-Phe-Ile-Pro-Lys
(7). Since hTERT is a well-known
cancer target that is overexpressed in most human cancer tissues
(8), GV1001 was initially
developed as an anticancer drug. It has been proved to be effective
for various cancer treatments, such as non-small cell lung cancer
(9,10), pancreatic cancer (8,11),
hepatocellular carcinoma (12),
melanoma (13,14) and B-cell chronic lymphocytic
leukemia (15). Since GV1001 has
been also known to possess anti-inflammatory effects, various
pre-clinical studies are ongoing to evaluate the anti-inflammatory
effects and their underlying mechanisms from disease models. It was
reported that GV1001 decreases the pro-inflammatory cytokines
[tumor necrosis factor (TNF)-α, interleukin (IL)-1β and IL-6] by
suppressing p38 mitogen-activated protein kinase (MAPK) and nuclear
factor (NK)-κB activation following enolase 1 (ENO1) stimulation
(16). ENO1 induces inflammation
through p38 MAPK and NF-κB signaling pathway activation. NF-κB
regulates inflammation through transcription regulation.
Furthermore, p38 MAPK is the key regulator of proinflammatory
cytokine.
The authors previously identified the
anti-inflammatory effect of GV1001 on IR injury in a rat lung
transplantation model (17). Koo
et al (18) also studied
the protective effects of GV1001 against renal IR injury model. In
the present study, focusing on modulating the inflammatory
response, the authors investigated the myocardial protective
effects of GV1001 in an IR injury rat model.
Materials and methods
Animals
The study protocols were approved by the
Institutional Animal Care and Use Committee of Seoul National
University Bundang Hospital (BA1307-133/060-01; Seoul, Korea). A
total of 105 10-week old male Sprague-Dawley rats (Orient Bio Inc.,
Seongnam, Korea) weighing 300–350 g were used in the study. All
animals were housed in a 12 h light-dark cycle and allowed water
and food ad libitum.
Chemicals
GV1001 was a gift from GemVax & KAEL Co., Ltd.
(Seongnam, Korea).
Cardiac ischemia-reperfusion injury
model
The cardiac ischemia-reperfusion injury model was
induced based on the previous study (19). The rats were anesthetized by an
intraperitoneal injection of Rompun (23.3 mg/ml) and Zoletil (50
mg/ml) (1:2; 1 ml/kg) mixture. During the experiments, the body
temperature was monitored via a rectal thermometer probe and
maintained at 37±0.5°C by a heating pad and lamp. Then, the rat was
intubated through a tracheostomy with a 14-gauge intravenous
catheter (B. Braun Melsungen, Melsungen, Germany) and tied with 4-0
silk ligature (Ethicon Inc., Cornelia, GA, USA). The ventilator
(Harvard Apparatus, Holliston, MA, USA) was connected at a
respiratory rate of 60 breaths/min, a tidal volume of 10 ml/kg, a
positive end-expiratory pressure of 2 cm H2O, and a
fraction of inspired oxygen of 1.0. The chest was opened by midline
sternotomy and the heart was exposed. Before the induction of IR
injury, normal saline (control) or the determined concentration
(0.001, 0.01, 0.1, 1, 5 or 10 mg/kg) of GV1001 was injected
directly through the right ventricle anterior wall using a 30-gauge
needle and a 1 ml syringe (BD Biosciences, Franklin Lakes, NJ,
USA), for a total of 7 different treatment groups. Around the
mid-to-distal third of the left anterior descending (LAD) coronary
artery was identified with 6-0 polyprophylene suture (Ethicon Inc.)
for subsequent snaring. Then, the suture was passed through a tube
using a tourniquet and ischemic injury was achieved by tightening
the snare and clamping the tube with a mosquito clamp. The ischemic
zone was confirmed by its pale color. At 40 min, following
induction of ischemic injury, reperfusion was performed by
releasing the snare for 10 min.
Assessment of area at risk
At the end of the reperfusion, the LAD coronary
artery was religated and 0.5 ml 5% Evans blue solution was infused
through the inferior vena cava to visualize the area at risk (AAR).
The rat was sacrificed and the heart was excised, transversely
sliced into 2 mm-thick sections from the apex to the base. The
slices were incubated in 1% triphenyltetrazolium chloride (TTC) at
37°C for 20 min to identify the infarct area. Then the samples were
kept in 10% formalin solution to enhance the color contrast. The
AAR and the left ventricle area (LA) were analyzed by computerized
planimetry (Image J, version 1.48; National Institutes of Health,
Bethesda, MD, USA), respectively (n=3 for each group). All reagents
were purchased from Sigma-Aldrich; Merck KGaA (Darmstadt,
Germany).
Histological analysis
Hematoxylin and eosin (H&E) staining was
performed for the histological analysis. As stated previously, the
rat was euthanized following reperfusion and the heart was excised
immediately and rinsed twice with cold normal saline. The central
regions of the AAR from the left ventricle were separated and fixed
in 10% formalin. Then the samples were embedded in paraffin and
sectioned into 5 µm-thick slices. The severity of hemorrhage was
compared.
Detection of apoptotic cells
The apoptotic cells were determined by terminal
deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) assay.
The paraffin block samples, which were prepared from H&E stain
step, were used for the assay. The analysis was performed to label
the apoptotic cells with a commercial kit (S7100; EMD Millipore,
Billerica, MA, USA) following the manufacturer's protocol.
Counterstaining was performed with 2% methyl green. Terminal
deoxynucleotidyl transferase (TdT)-positive nuclei were stained
dark brown while TdT-negative nuclei showed a light green color. A
pathologist who was blind to the study randomly selected and
examined four fields per each slide. TUNEL positive cells
(TdT-stained nuclei) were determined and divided by the total
amount of cells under a light microscope (BX43; Olympus
Corporation, Tokyo, Japan; n=4 for each group).
Myeloperoxidase determination
The myeloperoxidase (MPO) assay was performed to
detect neutrophil accumulation. Following reperfusion, the rat was
sacrificed and the heart was removed immediately and rinsed twice
with cold normal saline. The central regions of the AAR from the
left ventricle were rapidly frozen in liquid nitrogen and stored at
−80°C. Neutrophils were determined using an MPO assay kit (ab9535;
Abcam, Cambridge, MA, USA) according to the manufacturer's protocol
(n=4 for each group).
Cytokine analysis
The heart was removed immediately, as before, and
rinsed twice with cold normal saline. The central regions of the
AAR from the left ventricle were frozen in liquid nitrogen and
stored at −80°C. The concentrations of TNF-α and IL-6 were measured
by commercial ELISA kit (RTA00 and R6000B; R&D Systems, Inc.,
Minneapolis, MN, USA; n=4 for each group).
Statistical analysis
All data were presented as means ± standard
deviation. The statistical significance between the two groups was
determined by using Student's t-test. P<0.05 was considered to
indicate a statistically significant difference.
Results
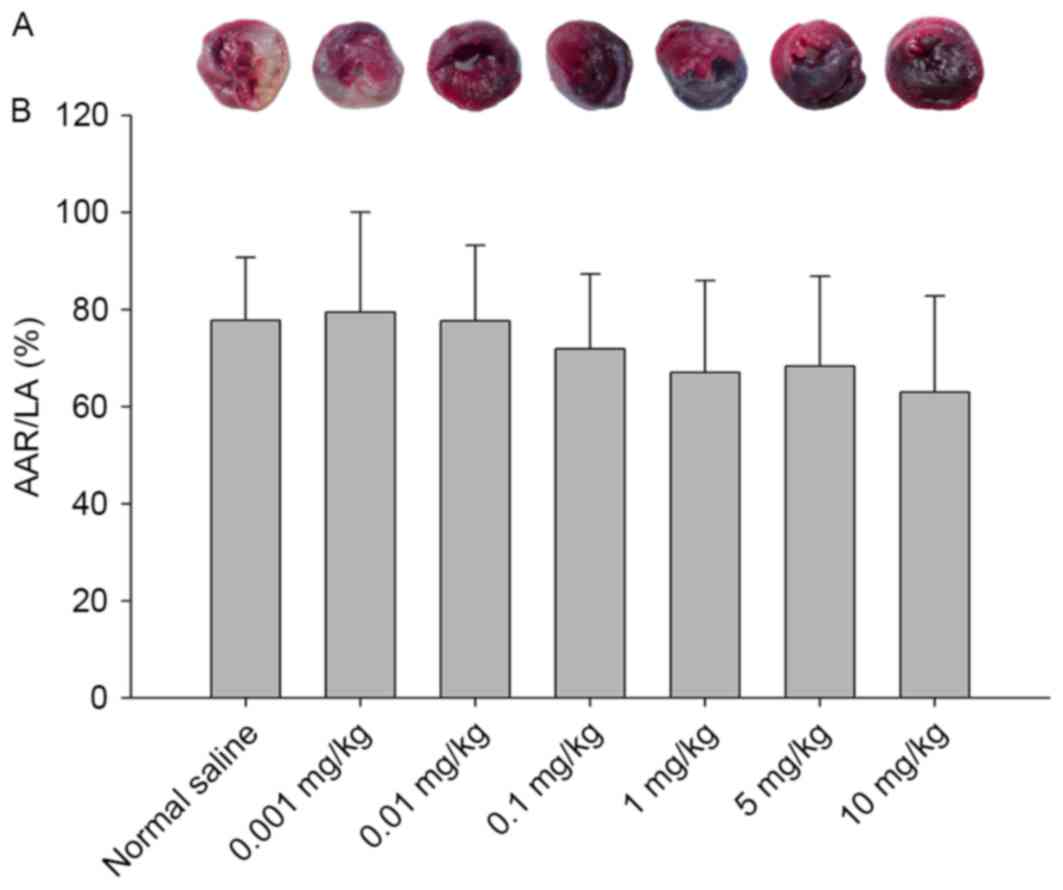
Determination of AAR
To determine the prevention effect of GV1001 on
cardiac IR injury, Evans blue and TTC staining were applied.
Representative images of heart sections are presented in Fig. 1A. The dark blue stained area
indicates the Evans blue solution-perfused region, which denotes
the non-ischemic region. The red area indicates the non-perfused,
ischemic region, which denotes the AAR. The pale white area within
the AAR represents infarcted, necrotic region, where the
cardiomyocytes have died. The infarct area was identified only in
the control and the 0.001 mg/kg GV1001-treated group.
The percentage of AAR/LA was calculated for each
group (Fig. 1B). AAR was protected
by a high concentration of GV1001 (0.01 mg/kg or higher). The
control group indicated 77.77±13.01% AAR/LA, while the 10 mg/kg
GV1001-treated group reported the most decreased value
(63.03±19.82%). No significant difference was observed between the
control group and any other experimental groups.
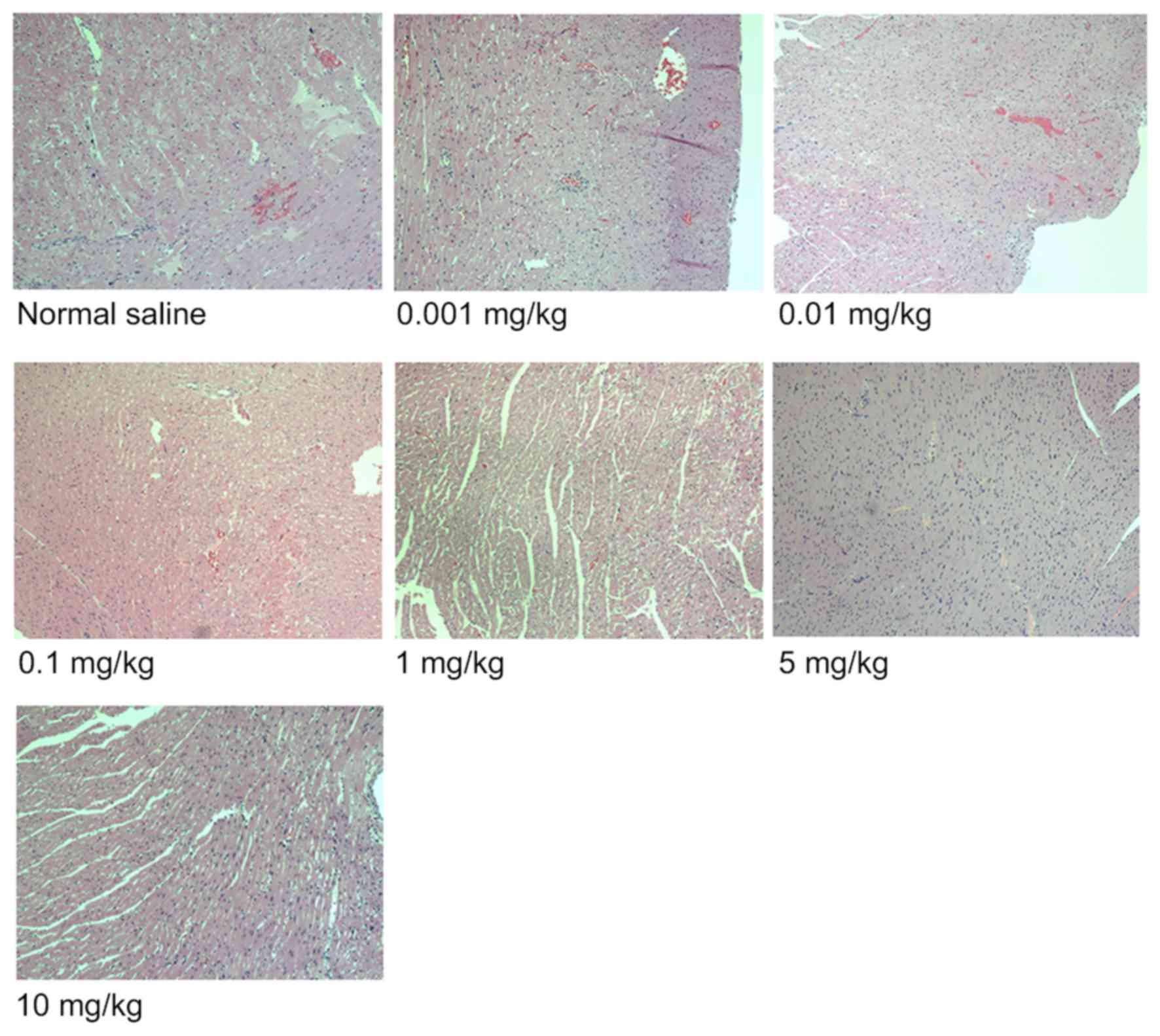
Histological analysis
The representative images of H&E stained AAR
sections are presented in Fig. 2.
GV1001-treated groups displayed a reduced degree of hemorrhage
compared with the normal saline-treated group, which demonstrated a
high degree of hemorrhage.
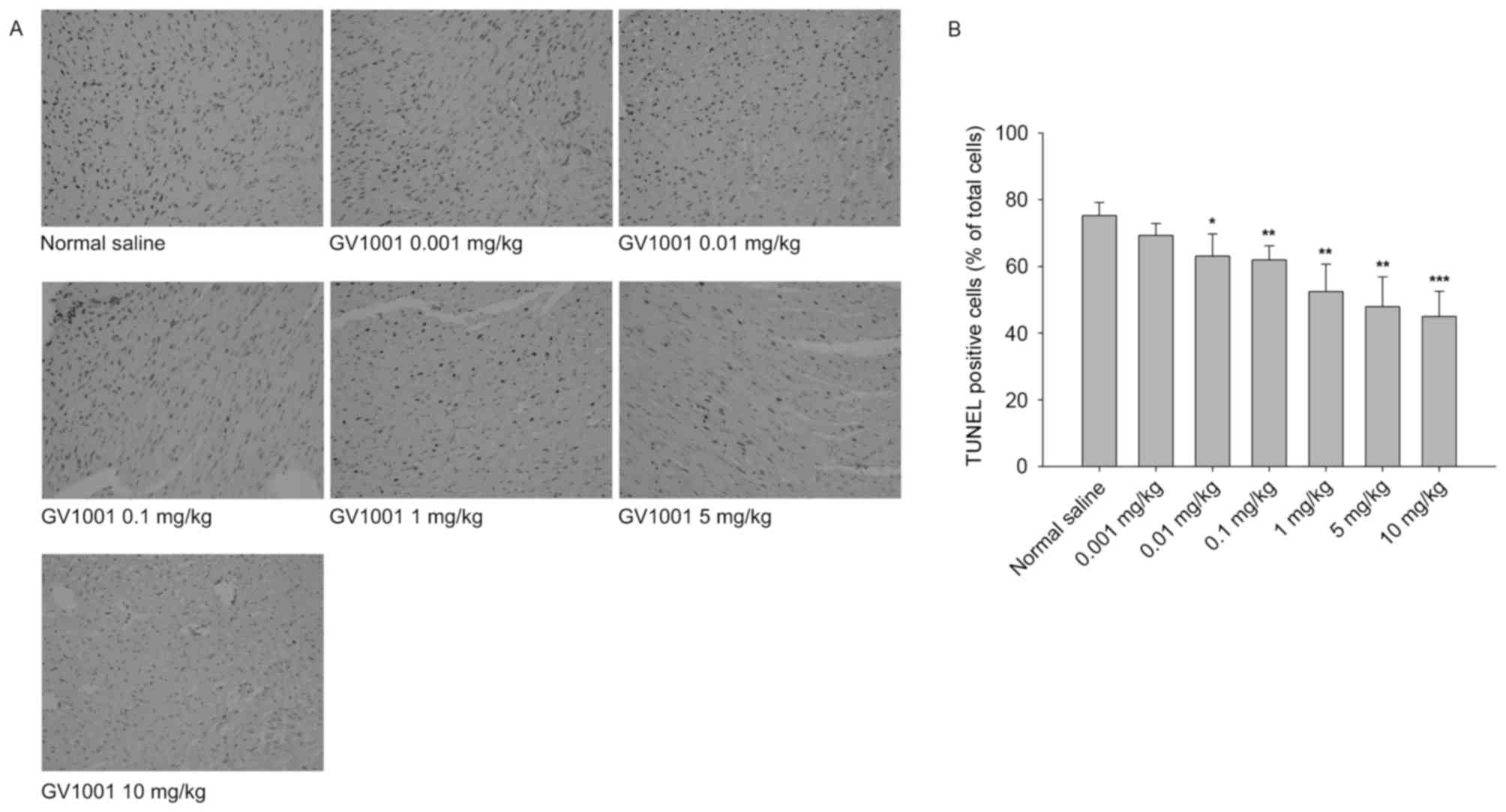
Cardiomyocyte apoptosis assay
A TUNEL stain assay was performed to determine the
apoptotic cells in the IR injury induced heart tissue. The TUNEL
positive cells were stained with dark brown and considered to be
apoptotic cells (Fig. 3A). The
apoptotic cells were quantitatively counted and expressed as % of
total cell counts (Fig. 3B).
Compared with the control group (75.25±3.91%), GV1001-treated
groups reported dose-dependent decreased levels of the TUNEL
positive cells. The 0.01 mg/kg (63.06±6.64%; P<0.05), 0.1 mg/kg
(61.93±4.26%; P<0.01), 1 mg/kg (52.44±8.22%; P<0.01), 5 mg/kg
(47.95±8.93%; P<0.01), and 10 mg/kg (44.95±7.59%; P<0.001)
GV1001-treated groups reported significantly decreased apoptotic
cells in the IR injury-induced heart.
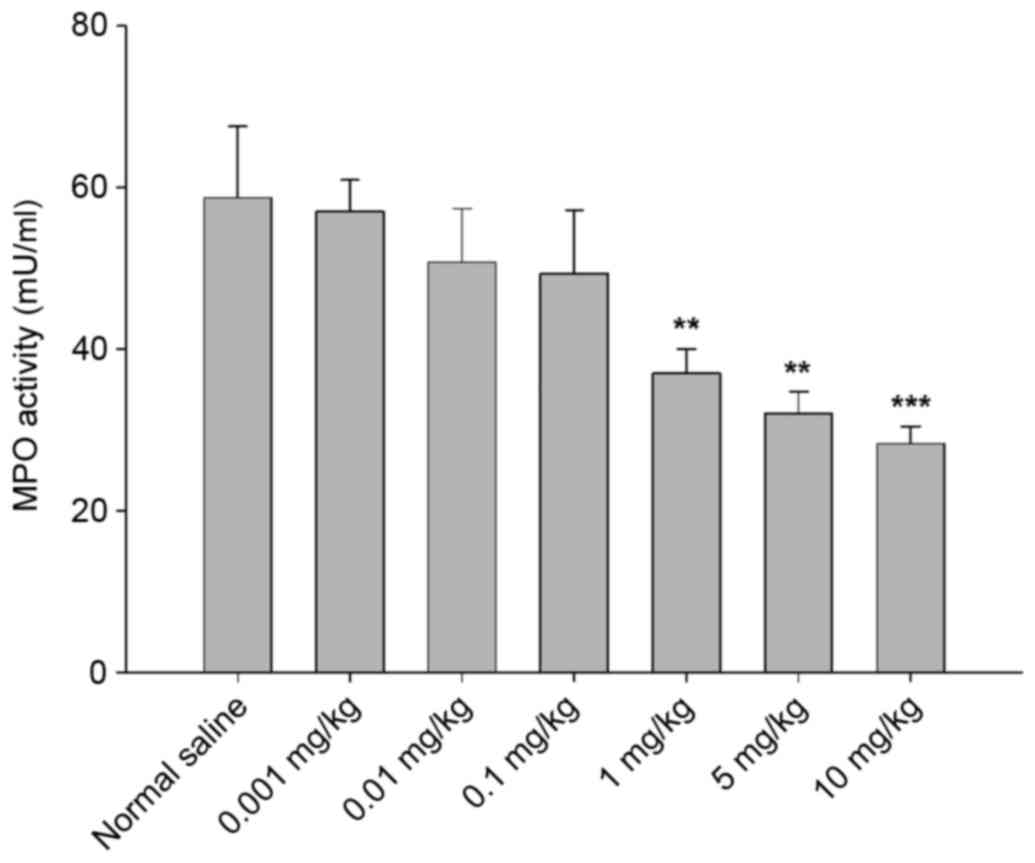
Determination of neutrophil contents
in cardiac tissue
To evaluate the anti-inflammatory effect of GV1001
on cardiac IR injury, MPO activity was measured as a marker of
neutrophil expression. The authors determined the MPO activity from
the excised AAR tissue samples. As displayed in Fig. 4, MPO activities decreased in a
GV1001 dose-dependent manner compared with the control group
(58.75±8.83 mU/ml). 1 mg/kg (37.04±2.97 mU/ml; P<0.01), 5 mg/kg
(32.08±2.63 mU/ml; P<0.01) and 10 mg/kg (28.28±2.18 mU/ml;
P<0.001) GV1001 treated group reported significantly decreased
neutrophil contents in the IR injury-induced heart.
Cytokine analysis
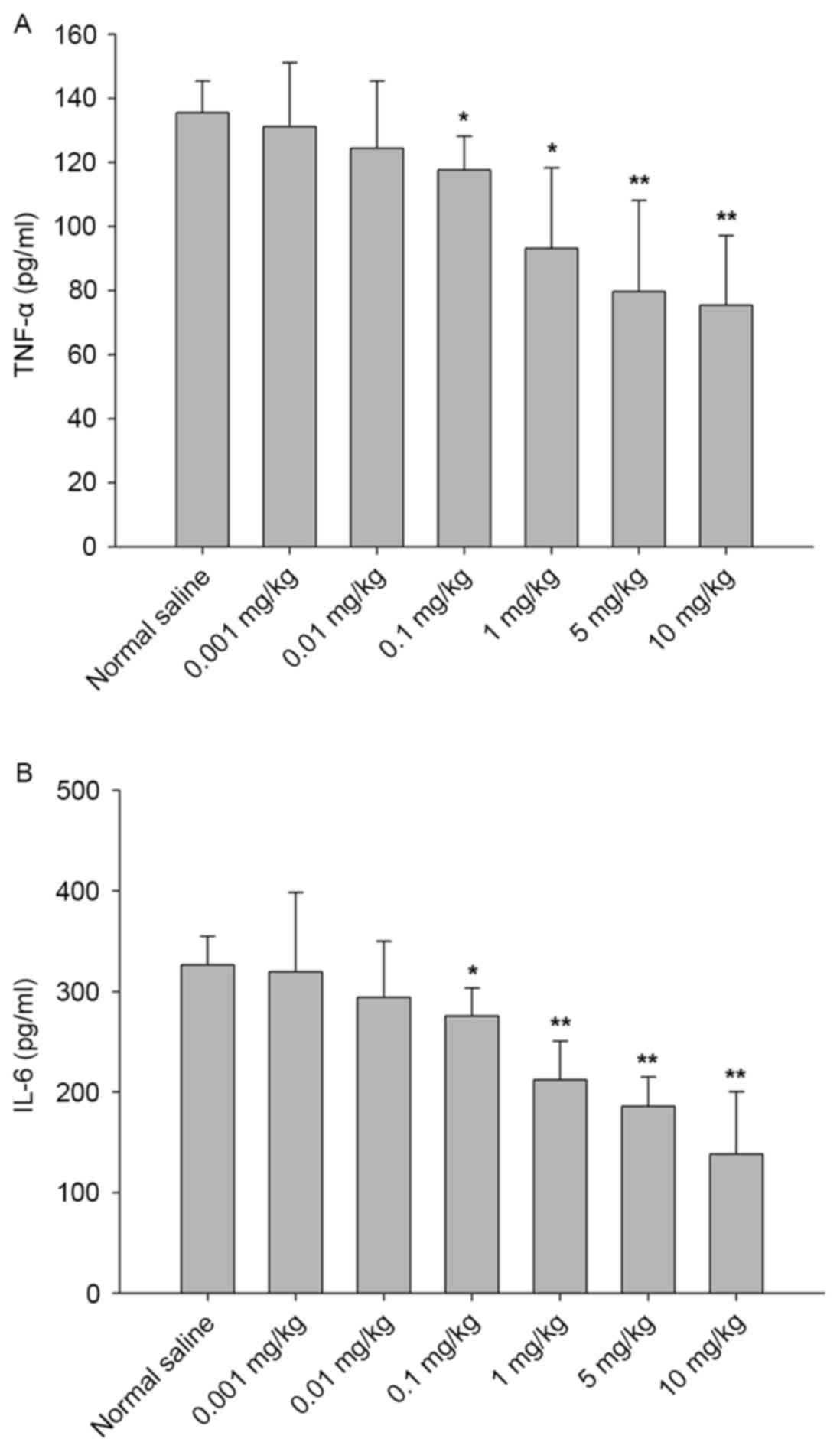
For further other confirmation of the
anti-inflammatory effects of GV1001 on cardiac IR injury,
inflammatory cytokines from the excised AAR zone were analyzed.
Fig. 5A and B present a GV1001
dose-dependent decrease in the levels of TNF-α and IL-6. For TNF-α
analysis (Fig. 5A), the 0.1 mg/kg
(117.62±10.55 pg/m; P<0.05), 1 mg/kg (93.21±25.12 pg/ml;
P<0.05), 5 mg/kg (79.68±28.47 pg/ml; P<0.01) and 10 mg/kg
(75.41±21.76 pg/ml; P<0.01) GV1001 treated groups presented
significantly decreased levels compared with the control group
(135.56±9.86 pg/ml).
For IL-6 analysis (Fig.
5B), significantly decreased levels were identified in the 0.1
mg/kg (275.71±27.62 pg/ml; P<0.05), 1 mg/kg (211.97±38.74 pg/m;
P<0.01), 5 mg/kg (185.76±29.25 pg/ml; P<0.01) and 10 mg/kg
(138.20±62.13 pg/ml; P<0.01) GV1001-treated groups compared with
the control group (326.34±28.67 pg/ml).
Discussion
To overcome the limitations of present
cardioprotective techniques, various pre-clinical approaches have
been made. Some research has focused on modulating the inflammatory
response. Shimamoto et al (20) evaluated the effect of eritoran, a
specific Toll-like receptor 4 (TLR4) antagonist, on myocardial IR
injury. TLR4 was suggested as a proinflammatory receptor in IR
injury. TLR2 also serves a key role in myocardial IR injury and
Arslan et al (21) studied
the effect of anti-TLR2 antibody. The four transmembrane adenosine
receptors (A1, A2A, A2B and
A3) are associated with cardiac protection. These
receptors are expressed in the immune system and modulate the
effects of adenosine (22).
Adenosine was studied to reduce myocardial IR injury using
adenosine-receptor-based therapy (23,24).
In the present study, the authors confirmed the
myocardial protective effect of the novel vaccine peptide GV1001 on
an IR injury animal model. This was conducted by establishing a
stable myocardial IR injury model by performing 40 min of ischemic
injury and 10 min of reperfusion in Sprague-Dawley rats. When the
ischemic time was shorter than 40 min, the ischemic injury was
insufficient for evaluation. In addition, when the ischemic time
was longer than 40 min, cardiac arrest occurred leading to death.
It was important to determine the proper ischemic and reperfusion
time providing the appropriate damage. To maintain the constant
strength when tightening the snare was also a critical point in
preparing the uniform myocardial IR injury models. 10 min of
reperfusion time was the maximum stable survival periods in the
established model. Due to the strong ischemia induction, the
reperfusion time was not too long. However, according to these
data, our myocardial IR injury model was damaged enough to express
apoptotic cells, neutrophils and inflammatory cytokines from the
ischemic zone.
To evaluate the cardioprotective effects of GV1001
on IR injury, AAR analysis, histological analysis, TUNEL assay, MPO
assay and inflammatory cytokine analysis were performed. Since the
recommended dose of GV1001 for inflammation has not yet been
determined, the authors tried various concentrations (0.001, 0.01,
0.1, 1, 5 and 10 mg/kg) GV1001 for the study.
The AAR and the infarct area were determined by
Evans blue and TTC staining (Fig.
1). The infarct area was only identified in the normal saline
and the 0.001 mg/kg GV1001 treated groups as the authors speculat
that the induced myocardial IR injury was not severe enough to
express complete infarction. Furthermore, induced mild infarction
was prevented by a high concentration of GV1001 (0.01 mg/kg or
higher).
When severe damage occurs to the endothelium,
extravasation of blood into the interstitum leads to
intramyocardial hemorrhage (25).
Though the quantitative analysis was not easy, based on the
representative images, 0.1 mg/kg and higher concentrations of
GV1001 presented attenuated congestion, while severe bleeding was
observed in the control group (Fig.
2).
Interestingly, apoptotic cells (Fig. 3), MPO activity (Fig. 4) and inflammatory cytokines (TNF-α
and IL-6; Fig. 5) reported GV1001
dose-dependent decreased levels. The 10 mg/kg GV1001 pre-treated
group presented 59.73% apoptotic cells, 48.14% neutrophil contents,
55.63% TNF-α and 42.35% IL-6 levels compared with the control
group. The inflammatory cytokines, such as TNF-α and IL-6, are well
known mediators of inflammation in early IR injury, which regulates
myocyte survival or apoptosis (26). In previous studies, pretreatment
with eritoran (TLR4 antagonist) in a myocardial IR injury model
attenuated ~29.37% TNF-α and 28.50% IL-6 compared with the control
group (20). When the Toll/IL-1R
(TIR)/BB-loop mimetic AS-1 is administered in myocardial IR injury
model, TNF-α and IL-6 were reduced by 30.0 and 38.7%, respectively,
compared with the control group (27). Though the animal models and the
protocols that were adopted in the studies were not identical,
GV1001 presented the most attenuated inflammatory cytokine levels
compared with the previous reports. As the proinflammatory
cytokines are the index of inflammation induced by IR injury, these
data suggested that GV1001 effectively protects against myocardial
IR injury.
Protein/peptide-based cancer vaccines are known to
stimulate immune response (28).
Since the hTERT participates in telomere length maintenance, it
serves as an attractive therapeutic target in cancer, anti-aging,
and various diseases (29,30). The anti-inflammatory effect of
GV1001 has been proved by previous studies. The GV1001 treatment
reduced neutrophil and macrophage infiltration in renal IR
injury-induced mice (19). The
inhibitory effect of GV1001 in rheumatoid arthritis mice model was
also evaluated (31). In a
previous report of the authors, adding GV1001 to the lung
preservation and flushing solutions also provided potential
protective effects against IR injury in a rat lung transplantation
model (18). In the present study,
neutrophils, reperfusion edema, and inflammatory cytokines were
significantly decreased in the GV1001 pre-treated lungs compared
with the non-treated lungs. These results strongly support the
anti-inflammatory effects of GV1001.
However, the current study has some limitations.
First, the reperfusion time was short. For further investigation,
pigs should be used for the myocardial IR injury models to increase
the reperfusion time. Secondly, the distribution of GV1001 in the
heart was not clearly verified. The drug administration was
performed through the right ventricle anterior wall. This
transmyocardial injection was made for the vascular distribution of
the drug with avoiding any direct damage to the left ventricle
surface. However, further analysis of drug distribution should be
performed.
In conclusion, the novel vaccine peptide GV1001
provided myocardial protective effects against IR injury and
therefore it can be considered as an alternative potential
anti-inflammatory agent for myocardial IR injury.
Acknowledgements
The present study was supported by a GemVax &
KAEL Co., Ltd. Research fund (grant no. 800-20130369). The authors
would also like to thank J. Patrick Barron, Professor Emeritus,
Tokyo Medical University and Adjunct Professor, Seoul National
University Bundang Hospital for his pro bono editing of this
manuscript.
References
|
1
|
Boyle EM, Pohlman TH, Cornejo CJ and
Verrier ED: Ischemia-reperfusion injury. Ann Thorac Surg. 64
Suppl:S24–S30. 1997. View Article : Google Scholar
|
|
2
|
Buja LM: Myocardial ischemia and
reperfusion injury. Cardiovasc Pathol. 14:170–175. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Jordan JE, Zhao ZQ and Vinten-Johansen J:
The role of neutrophils in myocardial ischemia-reperfusion injury.
Cardiovasc Res. 43:860–878. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Liu Q, Li J, Jubair S, Wang D, Luo Y, Fan
D and Janicki JS: Sparstolonin B attenuates hypoxia-induced
apoptosis, necrosis and inflammation in cultured rat left
ventricular tissue slices. Cardiovasc Drugs Ther. 28:433–439. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hale SL and Kloner RA: Mild hypothermia as
a cardioprotective approach for acute myocardial infarction:
Laboratory to clinical application. J Cardiovasc Pharmacol Ther.
16:131–139. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Inderberg-Suso EM, Trachsel S, Lislerud K,
Rasmussen AM and Gaudernack G: Widespread CD4+ T-cell
reactivity to novel hTERT epitopes following vaccination of cancer
patients with a single hTERT peptide GV1001. Oncoimmunology.
1:670–686. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Stevenson CL: Advances in peptide
pharmaceuticals. Curr Pharm Biotechnol. 10:122–137. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Bernhardt SL, Gjertsen MK, Trachsel S,
Møller M, Eriksen JA, Meo M, Buanes T and Gaudernack G: Telomerase
peptide vaccination of patients with non-resectable pancreatic
cancer: A dose escalating phase I/II study. Br J Cancer.
95:1474–1482. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Brunsvig PF, Aamdal S, Gjertsen MK,
Kvalheim G, Markowski-Grimsrud CJ, Sve I, Dyrhaug M, Trachsel S,
Møller M, Eriksen JA and Gaudernack G: Telomerase peptide
vaccination: A phase I/II study in patients with non-small cell
lung cancer. Cancer Immunol Immunother. 55:1553–1564. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Brunsvig PF, Kyte JA, Kersten C, Sundstrøm
S, Møller M, Nyakas M, Hansen GL, Gaudernack G and Aamdal S:
Telomerase peptide vaccination in NSCLC: A phase II trial in stage
III patients vaccinated after chemoradiotherapy and an 8-year
update on a phase I/II trial. Clin Cancer Res. 17:6847–6857. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Middleton G, Ghaneh P, Costello E,
Greenhalf W and Neoptolemos JP: New treatment options for advanced
pancreatic cancer. Expert Rev Gastroenterol Hepatol. 2:673–696.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Greten TF, Forner A, Korangy F, N'Kontchou
G, Barget N, Ayuso C, Ormandy LA, Manns MP, Beaugrand M and Bruix
J: A phase II open label trial evaluating safety and efficacy of a
telomerase peptide vaccination in patients with advanced
hepatocellular carcinoma. BMC Cancer. 10:2092010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kyte JA, Gaudernack G, Dueland S, Trachsel
S, Julsrud L and Aamdal S: Telomerase peptide vaccination combined
with temozolomide: A clinical trial in stage IV melanoma patients.
Clin Cancer Res. 17:4568–4580. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hunger RE, Lang K Kernland, Markowski CJ,
Trachsel S, Møller M, Eriksen JA, Rasmussen AM, Braathen LR and
Gaudernack G: Vaccination of patients with cutaneous melanoma with
telomerase-specific peptides. Cancer Immunol Immunother.
60:1553–1564. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kokhaei P, Palma M, Hansson L, Osterborg
A, Mellstedt H and Choudhury A: Telomerase (hTERT 611–626) serves
as a tumor antigen in B-cell chronic lymphocytic leukemia and
generates spontaneously antileukemic, cytotoxic T cells. Exp
Hematol. 35:297–304. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Choi J, Kim H, Kim Y, Jang M, Jeon J,
Hwang YI, Shon WJ, Song YW, Kang JS and Lee WJ: The
anti-inflammatory effect of GV1001 mediated by the downregulation
of ENO1-induced pro-inflammatory cytokine production. Immune Netw.
15:291–303. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chang JE, Kim HJ, Yi E, Jheon S and Kim K:
Reduction of ischaemia-reperfusion injury in a rat lung
transplantation model by low-concentration GV1001. Eur J
Cardiothorac Surg. 50:972–979. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Koo TY, Yan JJ and Yang J: Protective
effect of peptide GV1001 against renal ischemia-reperfusion injury
in mice. Transplant Proc. 46:1117–1122. 2014; View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yaoita H, Ogawa K, Maehara K and Maruyama
Y: Attenuation of ischemia/reperfusion injury in rats by a caspase
inhibitor. Circulation. 97:276–281. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Shimamoto A, Chong AJ, Yada M, Shomura S,
Takayama H, Fleisig AJ, Agnew ML, Hampton CR, Rothnie CL, Spring
DJ, et al: Inhibition of Toll-like receptor 4 with eritoran
attenuates myocardial ischemia-reperfusion injury. Circulation. 114
1 Suppl:I270–I274. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Arslan F, Smeets MB, O'Neill LA, Keogh B,
McGuirk P, Timmers L, Tersteeg C, Hoefer IE, Doevendans PA,
Pasterkamp G and de Kleijn DP: Myocardial ischemia/reperfusion
injury is mediated by leukocytic Toll-like receptor-2 and reduced
by systemic administration of a novel anti-Toll-like receptor-2
antibody. Circulation. 121:80–90. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Haskó G, Linden J, Cronstein B and Pacher
P: Adenosine receptors: Therapeutic aspects for inflammatory and
immune diseases. Nat Rev Drug Discov. 7:759–770. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Pitarys CJ II, Virmani R, Vildibill HD Jr,
Jackson EK and Forman MB: Reduction of myocardial reperfusion
injury by intravenous adenosine administered during the early
reperfusion period. Circulation. 83:237–247. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Janier MF, Vanoverschelde JL and Bergmann
SR: Adenosine protects ischemic and reperfused myocardium by
receptor-mediated mechanisms. Am J Physiol. 264:H163–H170.
1993.PubMed/NCBI
|
|
25
|
Hausenloy DJ and Yellon DM: Myocardial
ischemia-reperfusion injury: A neglected therapeutic target. J Clin
Invest. 123:92–100. 2013. View
Article : Google Scholar : PubMed/NCBI
|
|
26
|
Nian M, Lee P, Khaper N and Liu P:
Inflammatory cytokines and postmyocardial infarction remodeling.
Circ Res. 94:1543–1553. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Cao Z, Hu Y, Wu W, Ha T, Kelley J, Deng C,
Chen Q, Li C, Li J and Li Y: The TIR/BB-loop mimetic AS-1 protects
the myocardium from ischaemia/reperfusion injury. Cardiovasc Res.
84:442–451. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Disis ML: Mechanism of action of
immunotherapy. Semin Oncol. 41 Suppl 5:S3–S13. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Mazzola P, Radhi S, Mirandola L, Annoni G,
Jenkins M, Cobos E and Chiriva-Internati M: Aging, cancer, and
cancer vaccines. Immun Ageing. 9:42012. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Martínez P and Blasco MA: Telomeric and
extra-telomeric roles for telomerase and the telomere-binding
proteins. Nat Rev Cancer. 11:161–176. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Choi I, Choi J, Kim J, Oh SY, Kim S and
Lee E: AB0125 the effect of Gv1001, a peptide vaccine, in animal
model of rheumatoid arthritis. Annals Rheumat Dis. 73:8452014.
View Article : Google Scholar
|