Introduction
Target immunotherapies have been suggested to be
important in the termination of tumor initiation, development,
progression and deterioration, via immunologic cytotoxicity and
personalized adoptive cellular immunotherapy (1,2). It
has previously been demonstrated that various target molecules
specific to tumor antigens may be used to suppress tumor growth,
migration, invasion or metastasis via targeting
metastasis-associated pivotal proteins, and may act as potential
therapeutic strategies with tumor-inhibition and anti-metastatic
properties in human cancer treatments (3,4).
Cafarotti et al (5)
reported that the personalized target therapy era ideally involves
therapeutically treating each individual human disease case,
including cancers, infections and hereditary diseases, in different
ways that are most efficient and in accordance with the patient's
unique genome.
Lung cancer is a primary public health concern and
the leading cause of cancer-associated mortalities worldwide
(6). Non-small cell lung cancer
(NSCLC) and small cell lung cancer (SCLC) are two particular
variations of lung cancer, which account for ~85 and 15% of the
incidence rate, respectively, in human cancer clinical statistical
analysis (7). NSCLC includes large
cell carcinoma, squamous cell carcinoma and adenocarcinoma that
additionally present an increasing trend and incidence rate
(8–10). Various investigations regarding
therapeutic treatments for NSCLC have previously been conducted,
however the overall 5-year survival rate is <15% in patients
with NSCLC, and this is of primary clinical concern (9,11,12).
NSCLC is one of the most frequently occurring
cancers resulting from poor air quality and high levels of air
contamination (13). Migration and
invasion are the predominant features of tumor metastasis and
development. The migratory, invasive and metastatic capabilities of
NSCLC result in the poor survival rate during treatment and
subsequent recurrence of the disease in patients (14,15).
Therefore, the development and identification of effective agents
for inhibition of migration and invasion, and individualized
medication for NSCLC, is of primary concern regarding treatment of
cancer patients (16,17). Lung cancer spectral histopathology
statistical analysis indicates that standard bio-therapy protocols,
including cell therapy and target therapy, results in beneficial
outcomes in 95% of patients, compared with traditional treatments
(7). A previous study suggested
that bio-therapy stiffness modulates lung cancer cell migration via
focal adhesion signaling as opposed to epithelial mesenchymal
transition (EMT) signaling (18).
Significant advances have been made, particularly
with the discovery of targeted agents. Metastasis-associated in
colon cancer-1 (MACC-1) is a protein that promotes human lung
cancer cell metastasis and is associated with poor patient
prognosis in NSCLC (19).
Expression levels of MACC-1 have been observed to be increased in
human colorectal cancer, and promote tumor migration and metastasis
through transactivating the metastasis-inducing hepatocyte growth
factor/MET proto-gene, receptor tyrosine kinase (HGF/MET) signaling
pathway (20).
The present study investigated if targeting of
MACC-1 is a reliable strategy for the inhibition of NSCLC migration
and metastasis in vitro and in vivo. Furthermore, the
regulatory pathway of MACC-1 and its functional role in NSCLC was
investigated. Overall, the results of the present study suggest
that targeting of MACC-1 may act as a promising potential
therapeutic strategy for intervention in metastasis formation and
treatment of NSCLC.
Materials and methods
Ethics statement
The present study was carried out in strict
accordance with the recommendations in the Guide for the Care and
Use of Laboratory Animals of the First Affiliated Hospital of
Soochow University (Suzhou, China). The study was approved by the
ethics committee of the Third People's Hospital of Yancheng
(Yancheng, China). All surgery and euthanasia were performed under
sodium pentobarbital anesthesia, and all efforts were made to
minimize suffering. The animals were anesthetized with 35 mg/kg
sodium pentobarbital by tail vein injection.
Cell culture
CHO-K1SV, NCI-H520, A549, H358 and MRC-5 cells were
purchased from American Type Culture Collection (Manassas, VA,
USA). NCI-H520, A549 and H358 cells were cultured in Dulbecco's
modified Eagle's medium, supplemented with 10% fetal bovine serum
(Gibco; Thermo Fisher Scientific, Inc., Waltham, MA, USA). MRC-5
cells were cultured in RPMI-1640 supplemented with 10% fetal bovine
serum (Gibco; Thermo Fisher Scientific, Inc.). All cells were
cultured at 37°C in an environment containing 5%
CO2.
Lung cancer tissues
Lung cancer tissue samples of large cell carcinoma,
squamous cell carcinoma and adenocarcinoma were obtained from
patients that underwent tumorectomies in the First Affiliated
Hospital of Soochow University. The ethical committee members
reviewed the experimental designs and protocols and gave ethical
approval. A total of 9 male lung cancer patients were enrolled in
the study during May 2015 to July 2015, with large cell carcinoma
(n=3), squamous cell carcinoma (n=3) and adenocarcinoma (n=3). The
mean age of the patients was 48.3 years old (range, 35.6–68.4). All
patients agreed to participate in the present study and gave
written informed consent.
Construction of full length
Anti-MACC-1 antibody
The mouse anti-human MACC-1 monoclonal antibody was
constructed using a conventional approach. The chimeric antibody
(Chanti)-MACC-1 was constructed as previously described (21) The single chain variable fragments
of the MACC-1 monoclonal antibody were cloned and inserted into the
Pklight vector (Hengfei Bioscience, Inc., Shanghai China). The
constant domain heavy chain (CH)-Fc and light chain (CL) fragments
were subcloned into the Pklight-anti-MACC-1 vector, which were
subcloned into the Peedual 12.4 vector (Hengfei Bioscience, Inc.).
Subsequently, this was transfected into CHO-K1SV cells using
Lipofectamine® 2000 (Sigma-Aldrich; Merck KGaA) at room
temperature for 20 min. The production of Chanti-MACC-1extracted
from the CHO-K1SV cells was confirmed by using SDS-PAGE western
blotting.
Enzyme-linked immunosorbent assay
(ELISA)
The affinity of Chanti-MACC-1 for its target
antigens mouse-MACC-1 (m MACC-1) and human-MACC-1 (hMACC-1) was
determined using ELISA kit (cat. no. bs-4293R; BIOSS, Beijing
China). A total of 0.2–1.2 mg/ml mMACC-1 and hMACC-1 protein was
added into a microplate and incubated with Chanti-MACC-1 at 4°C for
12 h. Chanti-MACC-1 (3 µg/ml) was subsequently added to the mMACC-1
and hMACC-1 microplate and incubated for 120 min at 37°C and PBS
was used as a control. The protocol was conducted as previously
described (22) and the results
were analyzed at a wavelength of 450 nm by an ELISA plate reader
(Bio-Rad Laboratories, Inc., Hercules, CA, USA).
MTT assay
A549 cells were cultured in 6-well plates and grown
to ~90% monolayer cells. Subsequently, Chanti-MACC-1 was added into
the 6-well plates for 12 h. A total of 10 µl MTT was used, and
formazan crystals were subsequently dissolved in 100 µl dimethyl
sulfoxide, then the procedure was conducted as previously described
(23). The results were determined
by a spectrophotometer (Bio-Rad Laboratories, Inc.) at a wavelength
of 570 nm.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
Total RNA was obtained from NCI-H520, A549, H358 and
MRC-5 cells prior or the tumor tissues with Chanti-MACC-1 by using
RNAeasy Mini kit (24) (Qiagen
Sciences, Inc., Gaithersburg, MD, USA). A total of 1 µg total RNA
was then transcribed into cDNA using the PrimeScript™ RT Master mix
(Perfect Real Time; Takara Biotechnology Co., Ltd.) in an ABI PRISM
7900 real time system (Applied Biosystems; Thermo Fisher
Scientific, Inc.). The quality of the synthetic cDNA was verified
by electrophoresis. Subsequently, the synthetic cDNA (10 ng) was
subjected to RT-qPCR using SYBR-Green Master Mix system (Bio-Rad
Laboratories, Inc). The protocol of thermos cycling was as follows:
Denaturation, 95°C for 2 min; annealing, 40 repetitions of 95°C for
30 sec and 60°C for 60 sec; and final extension, 72°C for 10 min.
The primers used in the present study were synthesized by Shanghai
Shenggong Biology Engineering Technology Service, Ltd., Shanghai,
China. MACC-1 forward, 5′-AGTGGGATTGTGGAGACGGTGT-3′ and reverse,
5′-AGGTAAAAGGAACTGGCAACGC-3′; GAPDH forward,
5′-GTGGACATCCGCAAAGAC-3′ and reverse, 5′-AAAGGGTGTAACGCAACTA-3′.
GAPDH was included as an internal control. Differences in mRNA
expression alterations were calculated by 2−ΔΔCq
(25). The results are expressed
as the n-fold way compared with control.
Cell invasion assay
A549 cells were treated with Chanti-MACC-1 and
non-treated cells served as control. Cultured cells were suspended
at a density of 5×106 in 1,000 µl serum-free DMEM medium
for 12 h in the upper chamber of a BD BioCoat Matrigel chamber (BD
Biosciences, Franklin Lakes, NJ, USA) whereas the lower chamber was
filled with 600 µl cultural medium supplied with 10% FBS. According
to the manufacturer's protocol. Following incubation for 12 h at
37°C, cells in each group were fixed with ice-cold methanol for 10
min and stained with crystal violet for 5 min at room temperature.
Images were captured under a light microscope (magnification, ×200;
Nikon Corp., Tokyo, Japan). A549 cell invasion was determined in at
least three randomly stained-fields using a microscope for each
sample.
SDS-PAGE and western blot
analysis
The supernatant of serum-free CHO-K1SV cells was
harvested. Proteins were resolved by 12% SDS-PAGE under reducing
conditions with β-mercaptoethanol (Yuanmu Bioscience Inc.,
Shanghai, China). A549 cells were treated with Chanti-MACC-1 at a
concentration of 100 ng/ml for 12 h. Protein samples from
colorectal tumors and A549 cells and were homogenized using
radioimmunoprecipitation assay lysis buffer (Invitrogen; Thermo
Fisher Scientific, Inc.) and samples were centrifuged at 7,103 × g
at 4°C for 10 min. The protein concentrations of the cell extracts
were then measured using Bradford protein dye reagent (Bio-Rad
Laboratories, Inc., Hercules, CA, USA). A total of 30 µg/lane
protein was loaded and separated by 12% SDS-PAGE and transferred to
nitrocellulose membranes. The membranes were blocked with 5%
skimmed milk for 1 h at room temperature, washed in Tris-buffered
saline containing 0.1% Tween-20 (TBST) and incubated with the
following primary antibodies at 4°C overnight: Anti-MACC-1
(1:2,000; cat. no. ab106579; Abcam, Cambridge, UK), anti-HGF
(1:1,000; cat. no. ab83760; Abcam), anti-Met (1:2,000; cat. no.
ab216574; Abcam), anti-Vimentin (1:2,000; cat. no. ab8978; Abcam),
anti-E-cadherin (1:2,000; cat. no. ab11512; Abcam), anti-slug
(1:2,000; cat. no. ab27568; Abcam), anti-MMP-1 (1:2,000; cat. no.
ab52631; Abcam), anti-CT-1 (1:2,000; cat. no. ab13975; Abcam),
anti-fibronectin (1:2,000; cat. no. ab2413; Abcam), A5 anti-rabbit
primary IgG (1:1,500; cat. no. ab6721; Abcam) conjugated to
horseradish peroxidase. The protein bands labeled with the
antibodies were visualized using the SuperSignal West Pico
Chemiluminescent Substrate Trial kit (Pierce; Thermo Fisher
Scientific, Inc.). Images were obtained using the ChemiDoc XRS
system with BandScan 5.0 software (Glyko, Inc., Novato, CA,
USA).
Immunofluorescence
A549 cells or tumors from NSCLC xenograph mice were
fixed by using 10% formaldehyde for 30 min at 4°C in the dark,
embedded in paraffin and then the wax blocks were cut into sections
(4 µm thickness). The sections were dewaxed by conventional methods
and underwent microwave antigen retrieval at 95°C for 10 min. After
cooling, they were washed with distilled water and blocked in
normal 10% fetal bovine serum (Gibco; Thermo Fisher Scientific,
Inc.) at room temperature for 30 min. A549 cells and tumor sections
were incubated for 1 h at room temperature with MACC-1 antibodies
(1:2,000; cat. no. ab106579; Abcam). Subsequently, the cells and
sections were incubated with fluorophore-labeled secondary antibody
(1:300; cat. no. ab150117; Abcam) for 15 min at room temperature.
Sections were stained using 4′,6-diamidino-2-phenylindole (Hengfei
Bioscience, Shanghai, China) for 2 min, and sealed using glycerol
after being washed. Then the sections were placed under the
fluorescence microscope (Olympus Corporation, Tokyo, Japan) for
observation in the dark.
Animal studies
A total of 60 specific pathogen-free female C57BL/6
mice (6-week old and weight 16–22 g) were purchased from Shanghai
SLAC Laboratory Animal Co., Ltd (Shanghai, China). All mice were
housed at a specific temperature (22–24°C) in a pathogen-free room
at 40–70% humidity with a 12 h light/dark cycle and free access to
clean water and standard food. Mice were subcutaneously implanted
with A549 tumor cells and were divided into 2 groups (n=30 per
group). Treatments were started on day 6 following tumor
implantation when the tumor diameter reached 5–6 mm. Xenograft mice
were intravenously injected Chanti-MACC-1 (100 µg) and PBS as
control. The treatment was continued for 14 days at a frequency of
everyday. The tumor volumes were calculated as previously described
(26).
Statistical analysis
All data were presented as the mean ± standard error
of the mean of three independent replicates. Analysis was performed
using SPSS software version 20.0 (IBM Corp., Armonk, NY, USA).
Unpaired data was determined by Student's t-test and comparisons of
data between multiple groups were analyzed by analysis of variance
followed by a Student-Newman-Keuls test. A Kaplan-Meier test was
used to estimate the survival rate during a 150-day observation.
*P<0.05 and **P<0.01 were considered to indicate a
statistically significant difference.
Results
MACC-1 expression increases in NSCLC
cells and tissues
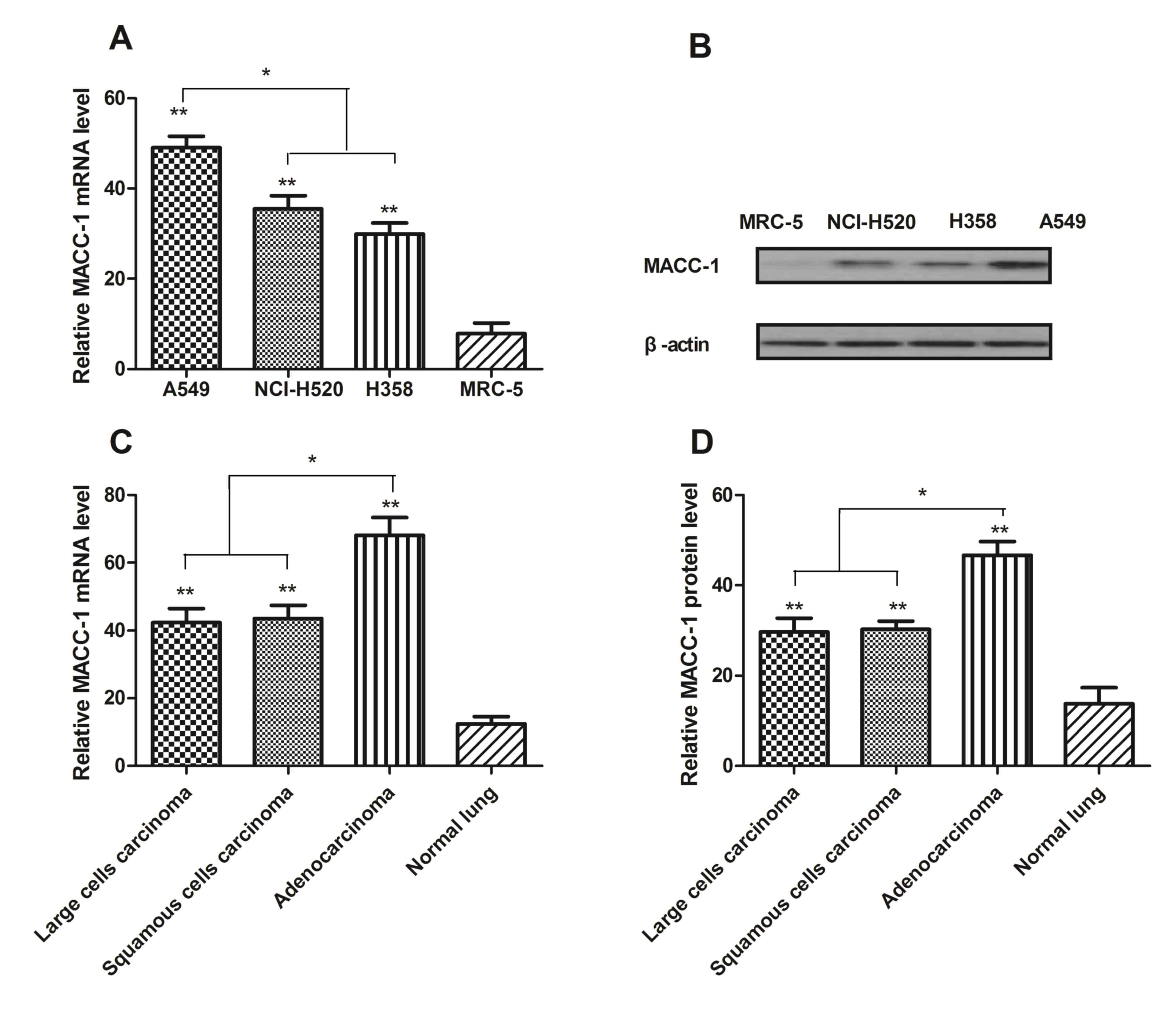
In order to investigate the role of MACC-1 in NSCLC
and normal lung cells, RT-qPCR was used to analyze expression
levels. The results in Fig. 1A and
B demonstrated that mRNA and protein expression of MACC-1 was
increased in NCI-H520, A549 and H358 cells compared with normal
lung MRC-5 cells. In addition, relative mRNA and protein expression
levels were additionally studied from patients with large cell
carcinoma, squamous cell carcinoma and adenocarcinoma. It was
observed that MACC-1 expression levels were upregulated at the mRNA
and protein level in NSCLC tumor tissues (Fig. 1C and D). MACC-1 expression in A549
cells was the greatest in all cell lines. These results suggested
that MACC-1 expression was upregulated in NSCLC, and expressed at a
low level in MRC-5 cells.
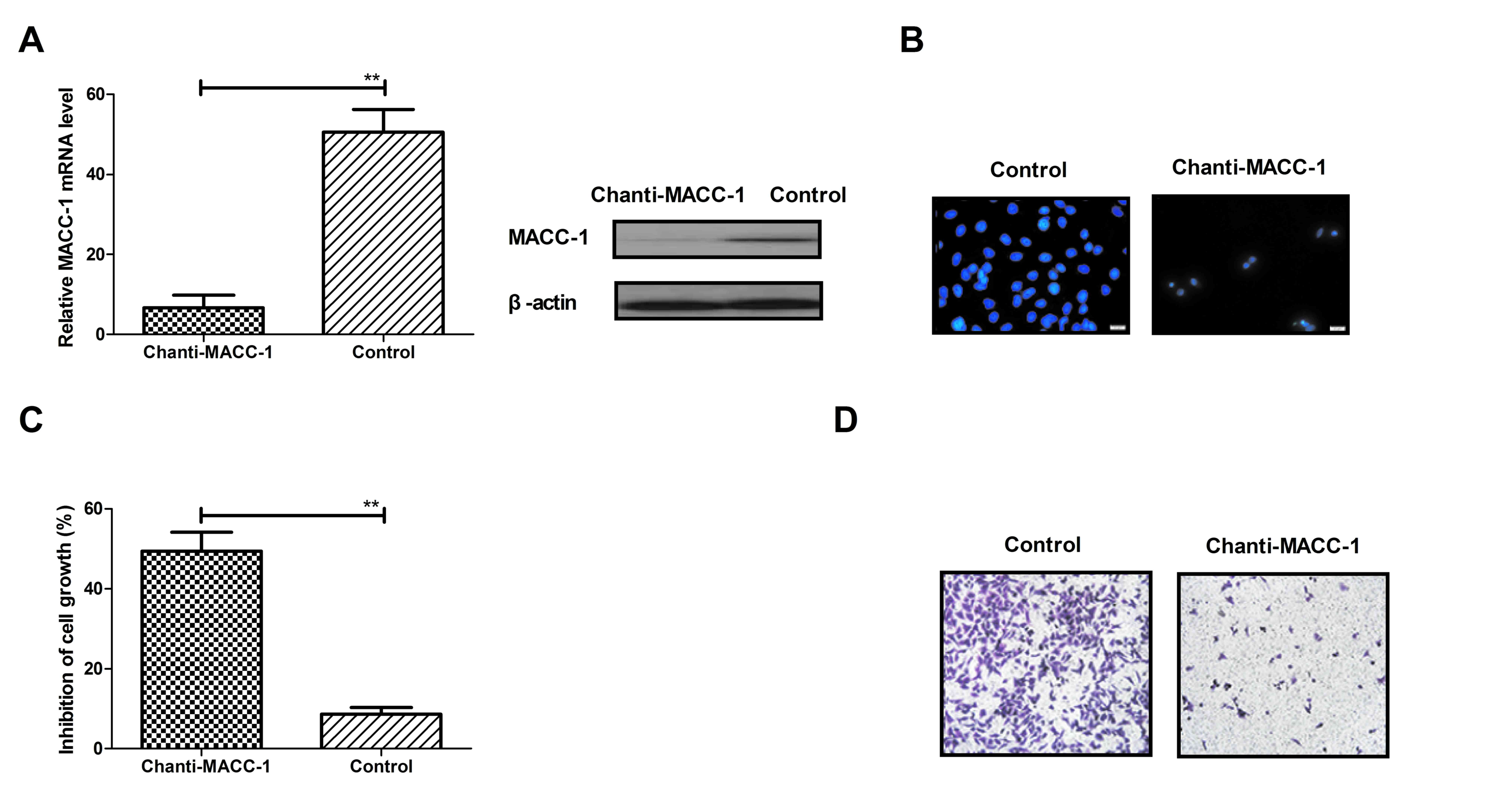
Chanti-MACC-1 directly targets MACC-1
in NSCLC cells
In consideration of the increased expression of
MACC-1 in NSCLC cells, the authors hypothesized that targeting of
MACC-1 was beneficial for NSCLS tumor cell inhibition. As presented
in Fig. 1, MACC-1 expression in
A549 cells was the greatest among NSCLS cells. Therefore, A549
cells were used to further study the efficacy of Chanti-MACC-1in
NSCLC cells. The results in Fig.
2A demonstrated that Chanti-MACC-1 efficiently decreased MACC-1
mRNA expression levels. The immunofluorescence assay revealed that
MACC-1 expression was suppressed in A549 cells following treatment
with Chanti-MACC-1 (Fig. 2B). In
addition, the present study further investigated the efficient
effects of Chanti-MACC-1 on NSCLS tumor cell growth and migration.
The results in Fig. 2C
demonstrated that A549 cell growth was significantly inhibited in
the Chanti-MACC-1-treated group. However, it was observed that
MACC-1 greatly promoted A549 cell growth compared with non-treated
control. Chanti-MACC-1 treatment efficiently suppressed A549 cell
migration, whereas MACC-1 significantly promoted A549 cell
migration (Fig. 2D). These data
indicated that Chanti-MACC-1 directly targets MACC-1 in NSCLC
cells.
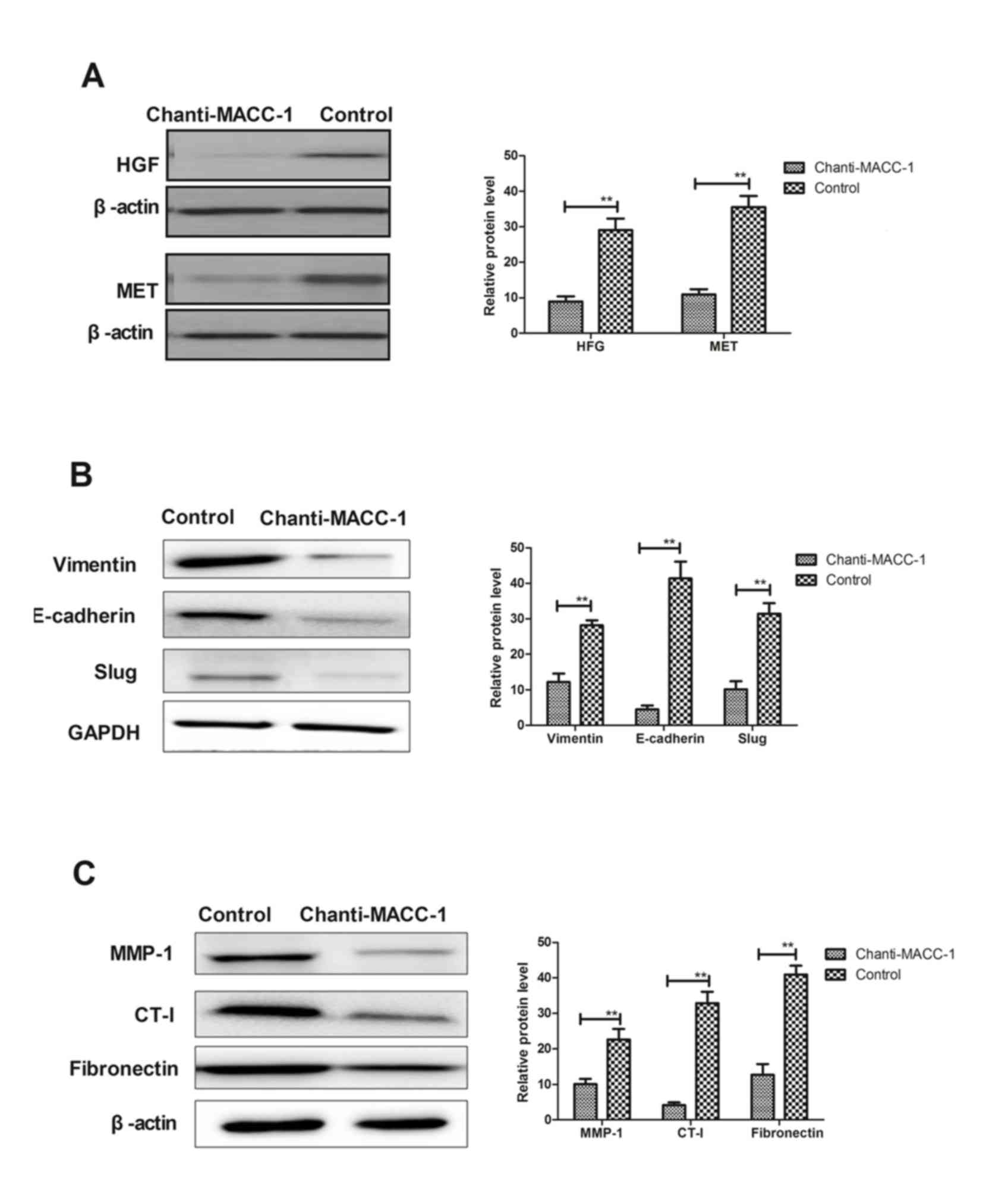
Chanti-MACC-1 inhibits the EMT process
via the HGF/MET signaling pathway
A previous study indicated that MACC-1 is
significantly associated with the EMT and tumor progression
(27). The MACC-1-induced EMT
signaling pathway was first analyzed, and observed to be blocked by
Chanti-MACC-1. Therefore, the underlying mechanism of the effects
of Chanti-MACC-1 on HGF/MET and EMT marker expression levels were
analyzed, including Vimentin, E-cadherin and Slug. The results in
Fig. 3A demonstrated that HGF/MET
expression was downregulated in A549 cells following Chanti-MACC-1
treatment. In addition, EMT marker expression was analyzed and
Fig. 3B demonstrated that
Chanti-MACC-1 treatment decreased Vimentin, E-cadherin and Slug
expression in A549 cells. Furthermore, migration-associated matrix
metalloproteinase (MMP)-1 proteins, collagen type I (CT-I) and
fibronectin were studied in A549 cells. The data presented in
Fig. 3C revealed that MMP-1
proteins, CT-I and fibronectin protein expression levels appeared
to be markedly decreased following treatment with Chanti-MACC-1 in
A549 cells. These results suggested that Chanti-MACC-1 suppressed
the migration-promoting proteins in the MACC-1-induced EMT process,
which may be beneficial to treatment of cancer cell migration in
the HGF/MET pathway.
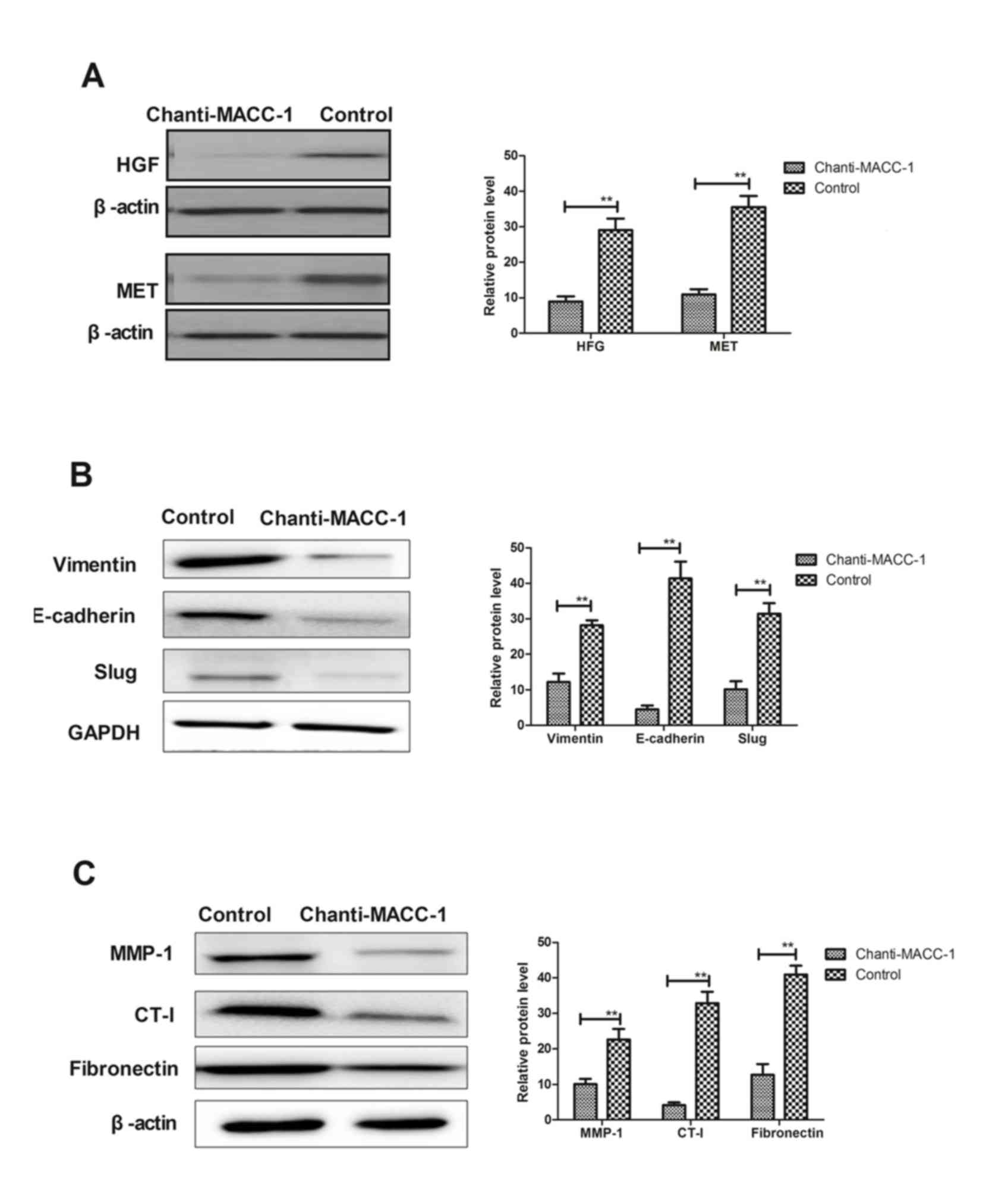 | Figure 3.Chanti-MACC-1 induces downregulation
of EMT and HGF/MET. (A) Representative image and quantification of
HGF and MET protein expression levels in A549 cells, following
Chanti-MACC-1 treatment. (B) Representative image and
quantification of EMT markers Vimentin, E-cadherin and Slug protein
expression analyzed in A549 cells, following Chanti-MACC-1
treatment. (C) Proteins that promoted tumor migration alterations
were analyzed in A549 cells following Chanti-MACC-1 treatment.
Student's t-test revealed a significant difference. **P<0.01 vs.
control. MACC-1, metastasis-associated in colon cancer-1;
Chanti-MACC-1, chimeric antibody-MACC-1; HGF/MET, hepatocyte growth
factor/MET proto-gene, receptor tyrosine kinase; EMT,
epithelial-mesenchymal transition; MMP-1, matrix metalloproteinase;
CT-I, collagen type I. |
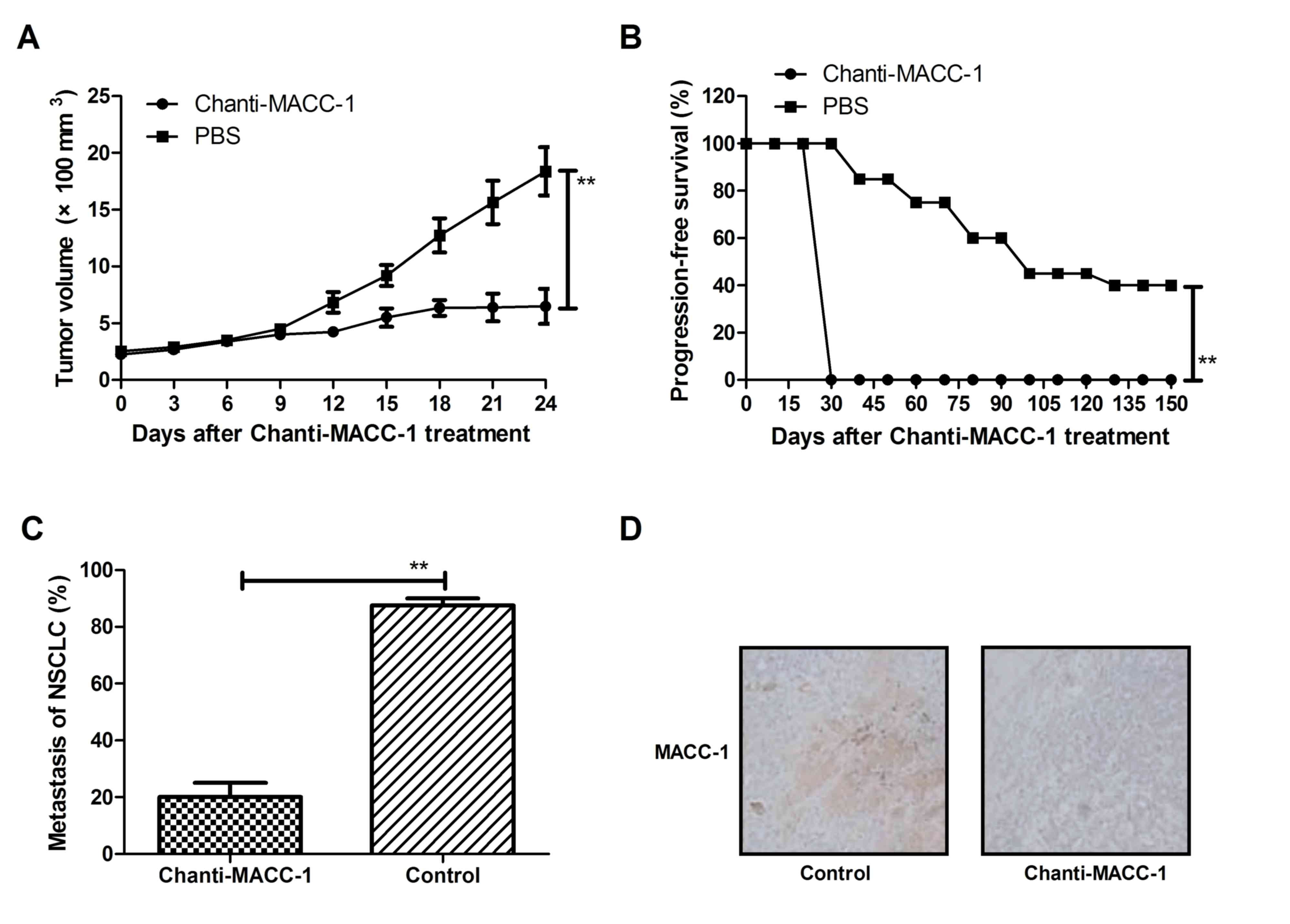
Chanti-MACC-1 exhibits a therapeutic
effect in tumor-bearing mice
Following confirmation of the in vitro
effects and mechanism, the present study proceeded to analyze the
in vivo effects of Chanti-MACC-1 in xenogeneic NSCLC in
C57BL/6 mice. As presented in Fig.
4A, tumor growth was significantly decreased in
Chanti-MACC-1-treated xenograft mice, compared with those treated
with PBS. In addition, the results in Fig. 4B demonstrated that Chanti-MACC-1
treatment prolonged the survival of NSCLC-bearing mice in a 150-day
observation, compared with control mice (n=30 in each group). Tumor
metastasis was additionally observed and Fig. 4C demonstrated that Chanti-MACC-1
treatment inhibited 80% metastasis tumor-bearing mice compared to
control group. Furthermore, the data in Fig. 4D indicated that MACC-1, HGF/MET
expression levels were significantly downregulated in tumors
following treatment with Chanti-MACC-1. These data suggested that
inhibition of tumor metastasis in NSCLC-bearing mice was enhanced
due to Chanti-MACC-1 therapy.
Discussion
The occurrence of lung cancer has previously been
demonstrated to be associated with industrial pollution and
destruction of the ecological environment in developing countries
(28). NSCLC is the primary
manifestation of human lung cancer (accountable for >80% of lung
cancer cases) that are frequently diagnosed at an advanced stage.
Therefore, numerous patients with NSCLC are informed of the limited
survival time associated with the diagnosis (29). In addition, the relative increased
morbidity and mortality rates of NSCLC among human cancers is
currently of primary concern (28). Previous studies have demonstrated
that NSCLC is exhibiting a significantly increasing trend in recent
years, and is gradually becoming the focus of public opinion and a
significant hazard to human health maintenance (30).
Currently, curative treatment of NSCLC is limited to
surgical resection or orthotopic lung transplantation. However, not
all patients with NSCLC benefit from a surgical approach and suffer
from increased recurrence rates. Furthermore, conventional
radiation and chemotherapy demonstrate little efficacy for NSCLC
and more frequent recurrence and metastasis occurs. Patients
generally exhibit a poor response to chemotherapy and surgery, and
as of yet, no targeted therapy has been established. In addition,
the poor survival rate of NSCLC patients is <15% following the
overall 5-year census (31).
Therefore, identification of novel therapeutic protocols to cure
patients with NSCLC is of primary concern.
A previous study suggested that migration and
metastasis are associated with a poor prognosis of patients with
NSCLC (32). Numerous reports have
indicated that migration and metastasis contribute to the
short-term survival period and are important contributing factors
to the relapse and retreatment of patients with NSCLC (33,34).
Therefore, anti-tumor agents targeting metastasis-promoting factors
are currently of great research interest for the treatment of
patients with NSCLC.
MACC-1 is human colon cancer cell metastasis gene
located on human chromosome 7 (35). Increased expression of MACC-1 is
positively correlated with patient disease progression and
prognosis in colorectal cancer (36). Previous biostatistics have revealed
that the majority of NSCLC patients observed exhibit an increased
expression of MACC-1 in tumors, that may contribute to a short-term
survival period (37). Clinical
studies have additionally demonstrated that MACC-1 is overexpressed
in colorectal cancer (38). In
addition, a previous study indicated that targeted therapy for
MACC-1 in patients with NSCLC has been investigated in various
human tumor cells (39–44). Furthermore, MACC-1 may be useful in
the identification of poor prognosis subjects with NSCLC in
clinical diagnosis, and may act as a potential molecular target for
intervention in metastasis formation. However, the mechanism of the
signaling pathway of MACC-1 in the growth, migration and metastasis
of NSCLC remains to be elucidated.
The results of the present study verified those of a
previous study, identifying MACC-1 as a tumorigenesis and
developmental metastasis-associated gene, which enhances NSCLC cell
proliferation, migration and invasion (45). The data from the present study
demonstrated that MACC-1 regulated proliferation, migration and
invasion through HGF-induced scattering and the metastasis-inducing
HGF/Met signaling pathway in tumor cells and xenograft models.
MACC-1 was reported as a regulator of HGF/Met/mitogen-activated
protein kinase pathway and induces proliferation, migration and
metastasis. In the present study, migration and invasion-associated
MMP-3, CT-I and fibronectin were studied and were demonstrated to
be significantly decreased both in vitro and in vivo,
following treatment with Chanti-MACC-1.
In conclusion, the results of the present study
suggested that MACC-1 was overexpressed in NSCLC cells and induced
the EMT signaling pathway to enhance growth, migration and
metastasis. The data additionally indicated that MACC-1 was
associated with a poor prognosis of mice with NSCLC. In addition,
Chanti-MACC-1 targeting MACC-1 revealed beneficial outcomes for
NSCLC-bearing mice, through inhibition of the
HGF/Met/mitogen-activated protein kinase pathway. Furthermore, the
results have identified the potential of Chanti-MACC-1 to suppress
growth, migration and metastasis via regulating
metastasis-associated genes, and to act as a novel therapeutic in
anti-metastasis treatment strategies.
References
|
1
|
Trautmann L, Said EA, Halwani R, Janbazian
L, Chomont N, El-Far M, Breton G, Haddad EK and Sekaly RP:
Programmed death 1: A critical regulator of T-cell function and a
strong target for immunotherapies for chronic viral infections.
Curr Opin HIV AIDS. 2:219–227. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Tanzarella S, Lionello I, Valentinis B,
Russo V, Lollini PL and Traversari C: Rhabdomyosarcomas are
potential target of MAGE-specific immunotherapies. Cancer Immunol
Immunother. 53:519–524. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Selvan SR, Dowling JP, Kelly WK and Lin J:
Indoleamine 2,3-dioxygenase (IDO): Biology and target in cancer
immunotherapies. Curr Cancer Drug Targets. 16:755–764. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Pier GB: Rationale for development of
immunotherapies that target mucoid Pseudomonas aeruginosa infection
in cystic fibrosis patients. Behring Inst Mitt. 1–360. 1997.
|
|
5
|
Cafarotti S, Lococo F, Froesh P, Zappa F
and Andrè D: Target therapy in lung cancer. Adv Exp Med Biol.
893:127–136. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Magnuson WJ, Yeung JT, Guillod PD,
Gettinger SN, Yu JB and Chiang VL: Impact of deferring radiation
therapy in patients with epidermal growth factor receptor-mutant
non-small cell lung cancer who develop brain metastases. Int J
Radiat Oncol Biol Phys. 95:673–679. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhukovsky M, Varaksin A and Pakholkina O:
Statistical analysis of observational study of the influence of
radon and other risk factors on lung cancer incidence. Radiat Prot
Dosimetry. 160:108–111. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Brody H: Lung cancer. Nature. 513
Suppl:S12014. View
Article : Google Scholar : PubMed/NCBI
|
|
9
|
Moro-Sibilot D, Smit E, de Castro Carpeño
J, Lesniewski-Kmak K, Aerts JG, Villatoro R, Kraaij K, Nacerddine
K, Dyachkova Y, Smith KT, et al: Non-small cell lung cancer
patients with brain metastases treated with first-line
platinum-doublet chemotherapy: Analysis from the European FRAME
study. Lung Cancer. 90:427–432. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Barnett SA, Downey RJ, Zheng J, Plourde G,
Shen R, Chaft J, Akhurst T, Park BJ and Rusch VW: Utility of
routine PET imaging to predict response and survival after
induction therapy for non-small cell lung cancer. Ann Thorac Surg.
101:1052–1059. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Xie FJ, Lu HY, Zheng QQ, Qin J, Gao Y,
Zhang YP, Hu X and Mao WM: The clinical pathological
characteristics and prognosis of FGFR1 gene amplification in
non-small-cell lung cancer: A meta-analysis. Onco Targets Ther.
9:171–181. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lim SH, Sun JM, Lee SH, Ahn JS, Park K and
Ahn MJ: Pembrolizumab for the treatment of non-small cell lung
cancer. Expert Opin Biol Ther. 16:397–406. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lupo B, Vialard J, Sassi F, Angibaud P,
Puliafito A, Pupo E, Lanzetti L, Comoglio PM, Bertotti A and
Trusolino L: Tankyrase inhibition impairs directional migration and
invasion of lung cancer cells by affecting microtubule dynamics and
polarity signals. BMC Biol. 14:52016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Müller B, Bovet M, Yin Y, Stichel D, Malz
M, González-Vallinas M, Middleton A, Ehemann V, Schmitt J, Muley T,
et al: Concomitant expression of far upstream element (FUSE)
binding protein (FBP) interacting repressor (FIR) and its splice
variants induce migration and invasion of non-small cell lung
cancer (NSCLC) cells. J Pathol. 237:390–401. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zhao Q, Yue J, Zhang C, Gu X, Chen H and
Xu L: Inactivation of M2 AChR/NF-κB signaling axis reverses
epithelial-mesenchymal transition (EMT) and suppresses migration
and invasion in non-small cell lung cancer (NSCLC). Oncotarget.
6:29335–29346. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhang H, Zhu X, Li N, Li D, Sha Z, Zheng X
and Wang H: miR-125a-3p targets MTA1 to suppress NSCLC cell
proliferation, migration, and invasion. Acta Biochim Biophys Sin
(Shanghai). 47:496–503. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Roth MT, Ivey JL, Esserman DA, Crisp G,
Kurz J and Weinberger M: Individualized medication assessment and
planning: Optimizing medication use in older adults in the primary
care setting. Pharmacotherapy. 33:787–797. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Shukla VC, Higuita-Castro N, Nana-Sinkam P
and Ghadiali SN: Substrate stiffness modulates lung cancer cell
migration but not epithelial to mesenchymal transition. J Biomed
Mater Res A. 104:1182–1193. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Shirahata A, Fan W, Sakuraba K, Yokomizo
K, Goto T, Mizukami H, Saito M, Ishibashi K, Kigawa G, Nemoto H, et
al: MACC 1 as a marker for vascular invasive hepatocellular
carcinoma. Anticancer Res. 31:777–780. 2011.PubMed/NCBI
|
|
20
|
Shirahata A, Sakata M, Kitamura Y,
Sakuraba K, Yokomizo K, Goto T, Mizukami H, Saito M, Ishibashi K,
Kigawa G, et al: MACC 1 as a marker for peritoneal-disseminated
gastric carcinoma. Anticancer Res. 30:3441–3444. 2010.PubMed/NCBI
|
|
21
|
Bai F, Tian H, Niu Z, Liu M, Ren G, Yu Y,
Sun T, Li S and Li D: Chimeric anti-IL-17 full-length monoclonal
antibody is a novel potential candidate for the treatment of
rheumatoid arthritis. Int J Mol Med. 33:711–721. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Lanyon SR and Reichel MP: Pretreatment of
serum samples to reduce interference of colostrum-derived specific
antibodies with detection of Bovine viral diarrhea virus antigen by
ELISA in young calves. J Vet Diagn Invest. 28:345–349. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Trino S, Iacobucci I, Erriquez D,
Laurenzana I, De Luca L, Ferrari A, Di Rorà A Ghelli Luserna,
Papayannidis C, Derenzini E, Simonetti G, et al: Targeting the
p53-MDM2 interaction by the small-molecule MDM2 antagonist
Nutlin-3a: A new challenged target therapy in adult Philadelphia
positive acute lymphoblastic leukemia patients. Oncotarget.
7:12951–12961. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ma J, Ma J, Meng Q, Zhao ZS and Xu WJ:
Prognostic value and clinical pathology of MACC-1 and c-MET
expression in gastric carcinoma. Pathol Oncol Res. 19:821–832.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-tie quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zhuang T, Djemil T, Qi P, Magnelli A,
Stephans K, Videtic G and Xia P: Dose calculation differences
between Monte Carlo and pencil beam depend on the tumor locations
and volumes for lung stereotactic body radiation therapy. J Appl
Clin Med Phys. 14:40112013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wang L, Lin L, Chen X, Sun L, Liao Y,
Huang N and Liao W: Metastasis-associated in colon cancer-1
promotes vasculogenic mimicry in gastric cancer by upregulating
TWIST1/2. Oncotarget. 6:11492–11506. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Lee YT, Liu CJ, Hu YW, Teng CJ, Tzeng CH,
Yeh CM, Chen TJ, Lin JK, Lin CC, Lan YT, et al: Incidence of second
primary malignancies following colorectal cancer: A distinct
pattern of occurrence between colon and rectal cancers and
association of Co-morbidity with second primary malignancies in a
population-based cohort of 98,876 patients in Taiwan. Medicine
(Baltimore). 94:e10792015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Kim DS, Park KM, Won YS, Kim JY, Lee JK,
Kim JG, Oh ST, Jung SS and Kang WK: Occurrence and prognosis of
symptomatic venous thromboembolism in colorectal cancer surgery
patients. Vasc Specialist Int. 30:49–55. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Wink KC, Belderbos JS, Dieleman EM, Rossi
M, Rasch CR, Damhuis RA, Houben RM and Troost EG: Improved
progression free survival for patients with diabetes and locally
advanced non-small cell lung cancer (NSCLC) using metformin during
concurrent chemoradiotherapy. Radiother Oncol. 118:453–459. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Charvat H, Sasazuki S, Inoue M, Iwasaki M,
Sawada N, Shimazu T, Yamaji T and Tsugane S: JPHC Study Group:
Prediction of the 10-year probability of gastric cancer occurrence
in the Japanese population: The JPHC study cohort II. Int J Cancer.
138:320–331. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Gold M, Dunn LB, Phoenix B, Paul SM,
Hamolsky D, Levine JD and Miaskowski C: Co-occurrence of anxiety
and depressive symptoms following breast cancer surgery and its
impact on quality of life. Eur J Oncol Nurs. 20:97–105. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Arora S, Ranade AR, Tran NL, Nasser S,
Sridhar S, Korn RL, Ross JT, Dhruv H, Foss KM, Sibenaller Z, et al:
MicroRNA-328 is associated with (non-small) cell lung cancer
(NSCLC) brain metastasis and mediates NSCLC migration. Int J
Cancer. 129:2621–2631. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Han L, Liang XH, Chen LX, Bao SM and Yan
ZQ: SIRT1 is highly expressed in brain metastasis tissues of
non-small cell lung cancer (NSCLC) and in positive regulation of
NSCLC cell migration. Int J Clin Exp Pathol. 6:2357–2365.
2013.PubMed/NCBI
|
|
35
|
Sun L, Duan J, Jiang Y, Wang L, Huang N,
Lin L, Liao Y and Liao W: Metastasis-associated in colon cancer-1
upregulates vascular endothelial growth factor-C/D to promote
lymphangiogenesis in human gastric cancer. Cancer Lett.
357:242–253. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Lederer A, Herrmann P, Seehofer D, Dietel
M, Pratschke J, Schlag P and Stein U: Metastasis-associated in
colon cancer 1 is an independent prognostic biomarker for survival
in Klatskin tumor patients. Hepatology. 62:841–850. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Stein U, Walther W, Arlt F, Schwabe H,
Smith J, Fichtner I, Birchmeier W and Schlag PM: MACC1, a newly
identified key regulator of HGF-MET signaling, predicts colon
cancer metastasis. Nat Med. 15:59–67. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Boardman LA: Overexpression of MACC1 leads
to downstream activation of HGF/MET and potentiates metastasis and
recurrence of colorectal cancer. Genome Med. 1:362009. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Shimokawa H, Uramoto H, Onitsuka T,
Chundong G, Hanagiri T, Oyama T and Yasumoto K: Overexpression of
MACC1 mRNA in lung adenocarcinoma is associated with postoperative
recurrence. J Thorac Cardiovasc Surg. 141:895–898. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Migliore C, Martin V, Leoni VP, Restivo A,
Atzori L, Petrelli A, Isella C, Zorcolo L, Sarotto I, Casula G, et
al: miR-1 downregulation cooperates with MACC1 in promoting MET
overexpression in human colon cancer. Clin Cancer Res. 18:737–747.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Yang T, Kong B, Kuang YQ, Cheng L, Gu JW,
Zhang JH, Shu HF, Yu SX, He WQ, Xing XM and Huang HD:
Overexpression of MACC1 protein and its clinical implications in
patients with glioma. Tumour Biol. 35:815–819. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Wang Z, Li Z, Wu C, Wang Y, Xia Y, Chen L,
Zhu Q and Chen Y: MACC1 overexpression predicts a poor prognosis
for non-small cell lung cancer. Med Oncol. 31:7902014. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Wang G, Fu Z and Li D: MACC1
overexpression and survival in solid tumors: A meta-analysis.
Tumour Biol. 36:1055–1065. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Li H, Zhang H, Zhao S, Shi Y, Yao J, Zhang
Y, Guo H and Liu X: Overexpression of MACC1 and the association
with hepatocyte growth factor/c-Met in epithelial ovarian cancer.
Oncol Lett. 9:1989–1996. 2015.PubMed/NCBI
|
|
45
|
Nakamura K, Nozawa K, Aoyagi Y, Ishihara
S, Matsuda K, Fukushima J and Watanabe T: A case report of thyroid
gland metastasis associated with lung metastasis from colon cancer.
Tumori. 97:229–232. 2011.PubMed/NCBI
|