Introduction
The role of the immune system in the origin,
development and metastasis of cancer is gradually being elucidated
(1–3) and is being taken into consideration
in anticancer treatment (4–6). For
example, the predictive and prognostic value of tumor-infiltrating
lymphocytes (TILs) in various tumors, especially breast cancer
(BC), was recently investigated (7–9). The
main infiltrating cells of the immune system in BC are T cells, and
accumulating evidence suggests that immune activity mediated by T
cells is critical for a sustained and effective antitumor response
(10). A previous study involving
semi-quantitative hematoxylin-eosin staining demonstrated that
triple-negative breast cancer (TNBC) exhibited a high infiltration
of cluster of differentiation (CD)4+T cells,
CD8+T cells and regulatory T cells (Tregs) (11). However, the exact numbers of these
cells and discrepancies between tumor, and healthy tissue are
seldom reported. Therefore, a more accurate and detailed analysis
is needed to determine the distribution of tumor-infiltrating T
cells in BC.
Tregs are a subset of CD4+T cells that
regulate immune responses to pathogens and maintain self-tolerance.
The forkhead box P3 protein (FOXP3) controls immune system
development and function, and serves a crucial role in the
generation of Tregs (12). The
infiltration of Tregs was reported in a variety of malignancies,
including BC and can effectively inhibit anti-tumor responses
(13–15). However, tumors are highly
heterogeneous and the way in which Tregs influence other immune
cells in BC remains unknown.
Mahmoud et al (16) demonstrated that tumor-infiltrating
CD8+ T lymphocytes exhibited antitumor activity, as
evidenced by their favorable effect on patient survival. However,
Matkowski et al (17)
demonstrated that the presence of CD8+ and
CD4+ cells correlated with lymph node involvement and
unfavorable prognosis in early BC. Similarly, Merlo et al
(18) demonstrated that FOXP3
expression in tumors was associated with worse overall survival in
BC. However, Ladoire et al (19) demonstrated that FOXP3 expression in
tumor cells predicted a better survival in human epidermal growth
factor receptor (HER)2-overexpressing BC patients treated with
neoadjuvant chemotherapy. These data identified the controversy
surrounding the prognostic value of tumor-infiltrating T cell
subsets and demonstrated that further research is required to fully
understand it.
Therefore, the present study aimed to assess the
distribution and interaction of tumor-infiltrating T cell subsets
in BC. Additionally, the prognostic value of CD4, CD8A and
FOXP3 expression in BC was evaluated using The Cancer Genome
Atlas (TCGA) database.
Materials and methods
Patient samples
The present study comprised 72 female BC patients
who underwent breast-conserving surgery or mastectomy without
neoadjuvant chemotherapy in the First People's Hospital of Yunnan
Province between October 2016 and July 2017 (Kunming, China). All
patient samples were diagnosed as invasive breast carcinoma by core
needle biopsy prior to surgery. Patient characteristics are
presented in Table I. The present
study was approved by the Ethics Committee of The First People's
Hospital of Yunnan Province and written informed consent was
provided by each patient. All methods were performed in accordance
with relevant guidelines and regulations.
 | Table I.Association of tumor infiltrating
lymphocytes with clinicopathological characteristics of breast
cancer patients. |
Table I.
Association of tumor infiltrating
lymphocytes with clinicopathological characteristics of breast
cancer patients.
|
Characteristics | Total N | TILs low N (%) | TILs high N
(%) | P-value |
|---|
| Age |
|
|
| 0.976 |
| <50
years | 26 | 18 (69.2) | 8
(30.8) |
|
| ≥50
years | 46 | 32 (69.6) | 14 (30.4) |
|
| Tumor size |
|
|
| 0.100 |
| <2
cm | 30 | 24 (80.0) | 6
(20.0) |
|
| ≥2
cm | 42 | 26 (61.9) | 16 (38.1) |
|
| Lymph node |
|
|
| 0.409 |
|
Negative | 38 | 28 (73.7) | 10 (26.3) |
|
|
Positive | 34 | 22 (64.7) | 12 (35.3) |
|
| Histological
grade |
|
|
| 0.030 |
| Low (I
and II) | 40 | 32 (80.0) | 8
(20.0) |
|
| High
(III) | 32 | 18 (56.3) | 14 (43.8) |
|
| ER |
|
|
| 0.006 |
|
Negative | 23 | 11 (47.8) | 12 (52.2) |
|
|
Positive | 49 | 39 (79.6) | 10 (20.4) |
|
| HER2 status |
|
|
| 0.047 |
|
Negative | 48 | 37 (77.1) | 11 (22.9) |
|
|
Positive | 24 | 13 (54.2) | 11 (45.8) |
|
| Ki-67 |
|
|
| 0.113 |
|
<20% | 33 | 26 (78.8) | 7
(21.2) |
|
|
≥20% | 39 | 24 (61.5) | 15 (38.5) |
|
| Molecular
subtype |
|
|
| 0.012 |
|
Luminal | 37 | 31 (83.8) | 6
(16.2) |
|
|
Her2+ | 24 | 13 (54.2) | 11 (45.8) |
|
|
Triple-negative | 11 | 5
(45.5) | 6
(54.5) |
|
Breast cancer subtypes
The St. Gallen Expert Consensus (20) was used to classify BC subtypes and
was optimised as: Luminal type [estrogen receptor (ER)+
and/or progesterone receptor (PR)+ and
HER2–], HER2+ (any ER status, any PR status
and HER2+), and triple negative (ER–,
PR– and HER2–). For ER and PR, cases with ≥1%
positive staining as performed according to a previously published
protocol (11) were considered
positive, and patients with HER2 3+ or the presence of
HER2 amplification were considered HER2-positive. The Ki67
index was also determined in all patients (11).
Processing of genomic data from
TCGA
Publicly available TCGA data including 1,085 BC
patients was downloaded from http://www.cbioportal.org and used in this study
(21). Gene Expression Profiling
Interactive Analysis (21), an
interactive web server, was used for cancer and normal gene
expression profiling and interactive analysis. A total of 69 BC
patients who are male, presented with distant metastasis or
received neoadjuvant chemotherapy were excluded in the further
survival analysis. The best cut-off for CD4, CD8A and FOXP3 mRNA
expression was 10.32, 7.47 and 6.55 separately which was defined by
the receiver operating characteristic curve. Information regarding
the 291 normal patients referred to as healthy women without
infectious disease in the last 6 months was also obtained from this
site.
Hematoxylin and eosin (H&E)
staining
Sections (4 µm) were deparaffinized with 2 changes
of xylene for 10 min each. The BC sections were hydrated by passing
through decreasing alcohol series (100, 95 and 70%). Slides were
stained in hematoxylin for 8 min at room temperature and then
washed in running tap water for 5 min. 1% acidified alcohol was
used for differentiation (1% HCl in 70% alcohol) for 2 min.
Sections were washed in running tap water until the sections were
blue again by dipping in an alkaline solution followed by another
tap water wash. Then the sections were stained in 1% eosin Y for 5
min at room temperature. Sections were washed in tap water for 3
min and dehydrated in increasing concentration of alcohols and
cleared in xylene.
Quantification of TILs
A semi-quantitative H&E method was used to
evaluate the TILs (22).
Histopathological analysis of the lymphocyte infiltrate was
performed on H&E-stained sections (22). All tumor H&E-stained slides
were observed at ×100 or ×400 magnification (OLYMPUS CX23; Olympus
Corporation, Tokyo, Japan). Stromal TILs were defined as the
percentage of tumor stroma area containing a lymphocytic infiltrate
without direct contact to tumor cells. In heterogenous tumors,
different regions were evaluated and the average percentages of
TILs were reported. During H&E evaluation, the cutoff
percentages for low TILs and high TILs were <60% and >60% in
BC tissue, respectively.
Flow cytometry
Flow cytometry was used to evaluate the density of
TILs. This was evaluated as the average number of CD45+
cells per gram. In the present study the H&E slides with 60%
TILs from the 72 patients were chosen for subsequent analysis, and
the TIL density of the same patient was calculated by flow
cytometry. Low and high groups were defined as CD45+
events/g tissue <300,000 and ≥300,000, respectively.
Freshly resected tissue was manually minced and then
incubated for 60 min at 37°C in a rocking table bed (120 rpm/min)
with 1.0 mg/ml collagenase type IV (Gibco; Thermo Fisher
Scientific, Inc., Waltham, MA, USA) and 100 µg/ml DNase I
(Sigma-Aldrich; Merck KGaA, Darmstadt, Germany) diluted in RPMI
Medium (HyClone; GE Healthcare Life Sciences, Logan, UT, USA)
without fetal bovine serum (FBS). Single cell suspensions were
prepared by filtering through 70-µm nylon strainers (BD
Biosciences, Franklin Lakes, NJ, USA). Zombie Yellow (BioLegend,
Inc., San Diego, CA, USA) was used to discriminate live and dead
cells according to the manufacturer's suggested dilutions (1:1,000)
prior to surface marker staining for 30 min at 4°C.
For surface staining, filtered single cells were
incubated for 30 min on ice with Fc Receptor Binding Inhibitor
(eBioscience; Thermo Fisher Scientific, Inc.) diluted 1:10 in PBS.
Cells were then incubated for 15 min in PBS containing 1.0 mM EDTA
and 5% FBS (Gibco; Thermo Fisher Scientific, Inc.) together with
the manufacturer's suggested dilutions of the following antibodies
at room temperature: Alexa Fluor 700 anti-human CD3 (1:500; cat.
no. 300324; Biolegend, Inc.), fluorescein isothiocyanate anti-human
CD4 (1:500; cat. no. 317408; Biolegend, Inc.), PerCP/Cy5.5
anti-human CD8 (1:500; cat. no. 300924; Biolegend, Inc.),
phycoerythrin anti-human CD25 (1:500; cat. no. 302606; Biolegend,
Inc.), PE/Cy5 anti-human CD45 (1:500; cat. no. 304010; Biolegend,
Inc.) and Brilliant Violet 650 anti-human CD127 (IL-7Rα; 1:500;
cat. no. 351326; Biolegend, Inc.).
For cytokine staining, filtered single cells were
incubated for 5 h with phorbol-12-myristate-13-acetate (50 ng/ml),
ionomycin (1 µg/ml) and Brefeldin A (1:1,000) diluted in RPMI
Medium (HyClone; GE Healthcare Life Sciences) containing 10% FBS
and penicillin-streptomycin (1:100). Surface markers were stained
as described above. Cells were fixed with fixation/permeabilization
buffer (eBioscience; Thermo Fisher Scientific, Inc.) for 20 min at
4°C according to the manufacturer's protocol. Then the
intracellular staining plate containing Pacific Blue-conjugated
anti-human IFN-γ (1:500; cat. no. 502517; Biolegend, Inc.),
PECy7-conjugated anti-human IL-4 (1:500; cat. no. 500817;
Biolegend, Inc.) and Brilliant Violet 510-conjugated anti-human
IL-17 (1:500; cat. no. 512307; Biolegend, Inc.) was placed at 4°C
for 30 min, washed twice with fixation/permeabilization buffer
(eBioscience; Thermo Fisher Scientific, Inc.) diluted in PBS
(1:1,000) and stored at 4°C until required for analysis with the
CytoFLEX flow cytometer (Beckman Coulter, Inc., Brea, CA, USA).
Results were analyzed using FlowJo software v9.3.2 (Tree Star,
Inc., Ashland, OR, USA).
Statistical analysis
All statistical analysis was conducted using IBM
SPSS Statistics software (version 22.0; IBM Corp, Armonk, NY, USA).
Continuous data are presented as the mean ± standard deviation.
Non-continuous data were compared by the Chi-square test or
Fisher's exact (two-sided) test and continuous data were analyzed
by the Mann-Whitney U test (two groups) or Kruskal-Wallis test
followed by Tukey's post hoc test (>two groups). Kaplan-Meier
curves and the log-rank test were used for survival analysis.
Pearson's correlation analysis was used to evaluate the correlation
between two variables. Univariate and multivariate Cox regression
analyses were used to evaluate the significance of various
parameters for survival. P<0.05 was considered to indicate a
statistically significant difference. All experiments were repeated
three times.
Results
TILs are closely associated with the
clinicopathological characteristics of BC patients
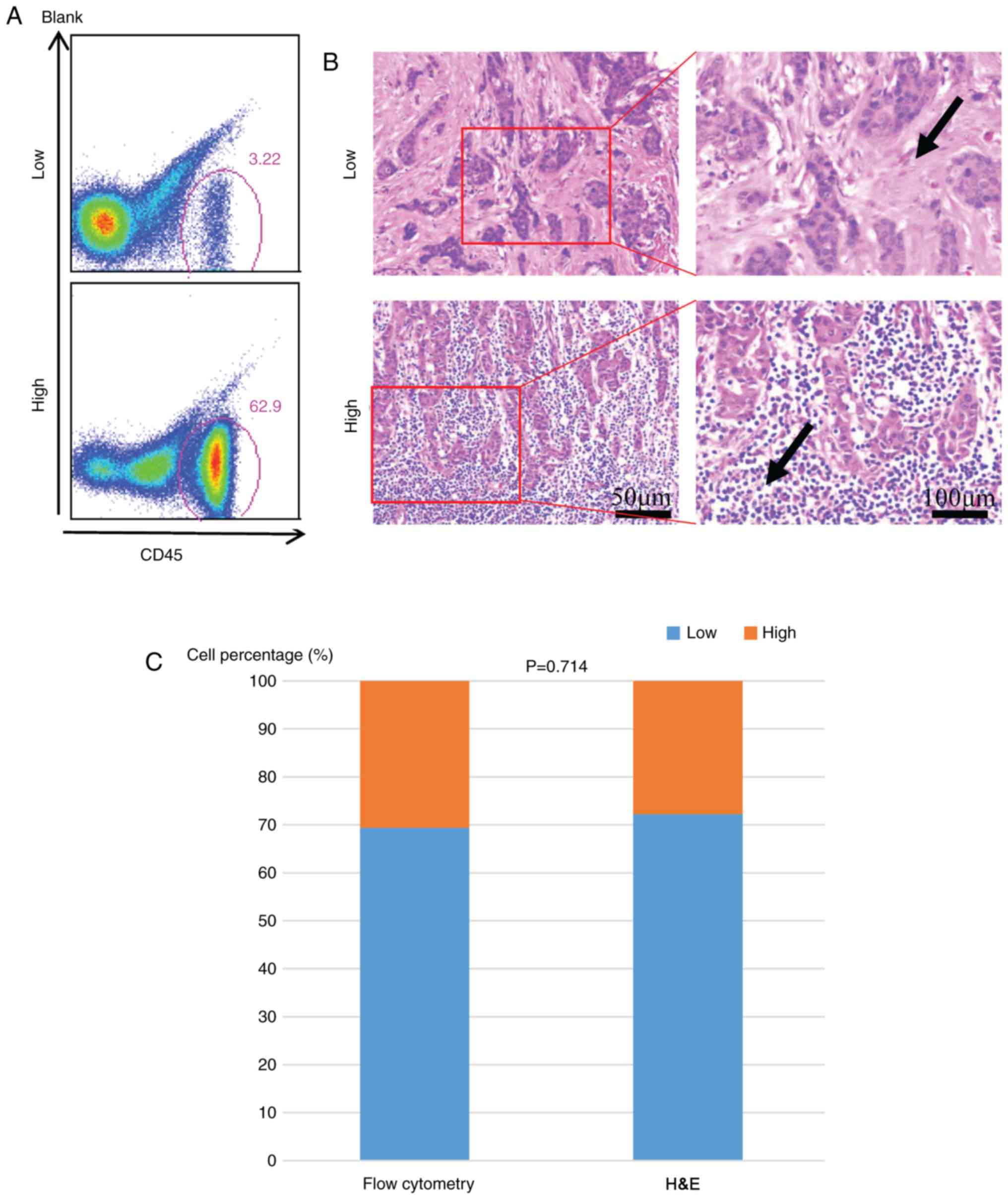
A total of 72 patients were divided into two groups
(low and high) according to their TIL density. There were 22
patients with high TILs using the quantitative method and this
number was 20 when using the semiquantitative H&E staining. The
result was comparable in evaluating the TILs by flow cytometry
(Fig. 1A) and hematoxylin-eosin
staining evaluation (Fig. 1B and
C). The association between TIL infiltration (low vs. high) and
various clinicopathological parameters of BC patients are presented
in Table I. A high infiltration of
TILs was significantly associated with histological grade (P=0.03),
ER negativity (P=0.006), HER2 positivity (P=0.047) and BC molecular
subtypes (P=0.012). The infiltration of lymphocytes demonstrated no
correlation with age, tumor size, lymph node status, or Ki-67
proliferation index (Table I).
Expression of tumor infiltrating T
cell genes in BC
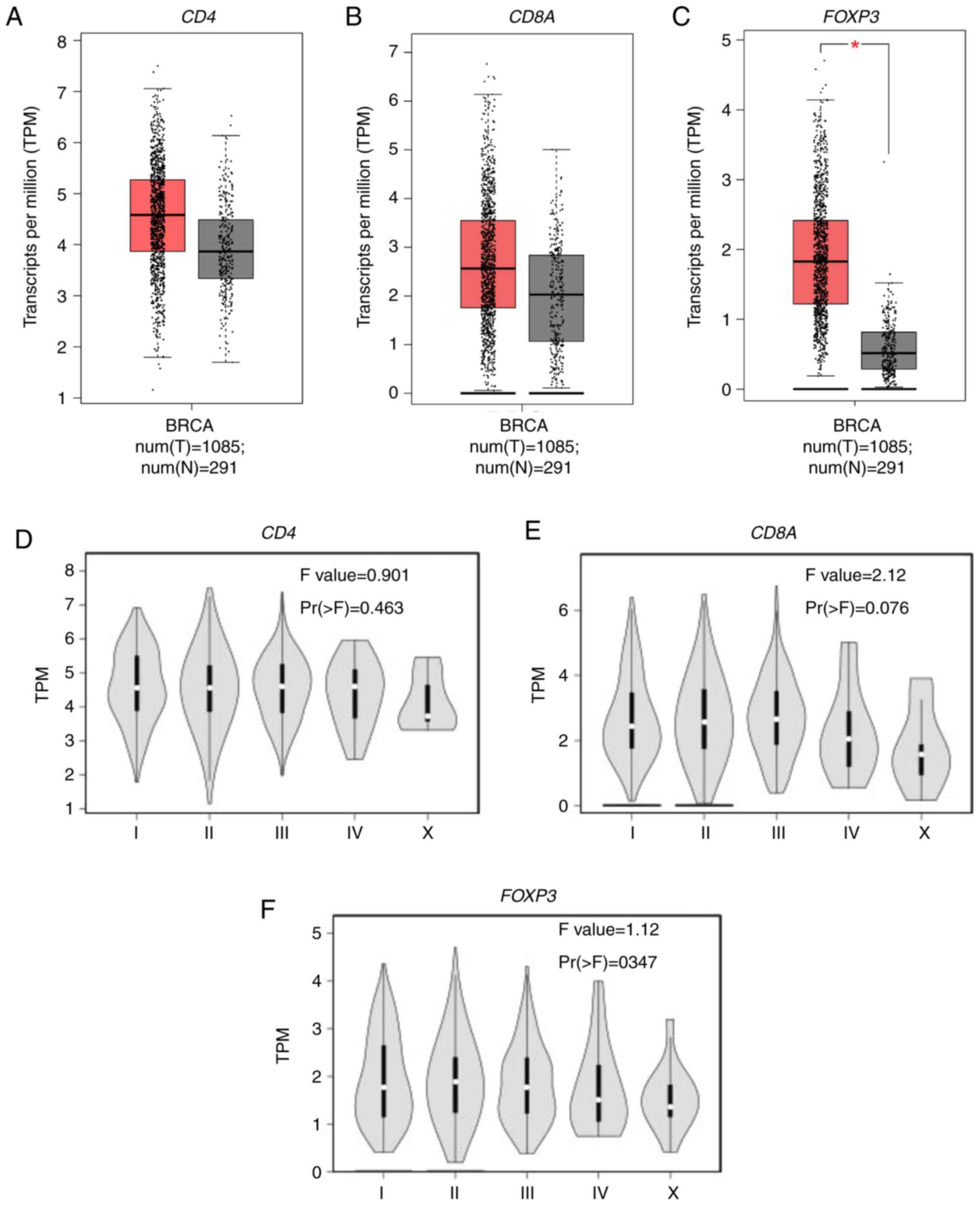
The expression of CD4, CD8A and FOXP3
mRNA as measured by transcripts per million, reflects the
infiltration of CD4+T cells, CD8+T cells, and
Tregs, respectively. A total of 1,085 BC samples and 291 healthy
breast tissue samples were analyzed, and increased CD4,
CD8A, and significantly increased FOXP3 mRNA expression
(P<0.01) was detected in BC samples compared with the healthy
breast tissue (Fig. 2A-C). The
association between CD4, CD8A and FOXP3 mRNA
expression and clinical stage of BC patients was also evaluated as
determined by the American Joint Committee on Cancer staging
system. There was no significant difference in the mRNA expression
of CD4 (P=0.463; Fig. 2D)
or FOXP3 (P=0.347; Fig. 2F)
in BC patients with different clinical stages. However, stage IV BC
patients tended to exhibit decreased CD8A mRNA expression
compared with early BC patients (P=0.076; Fig. 2E).
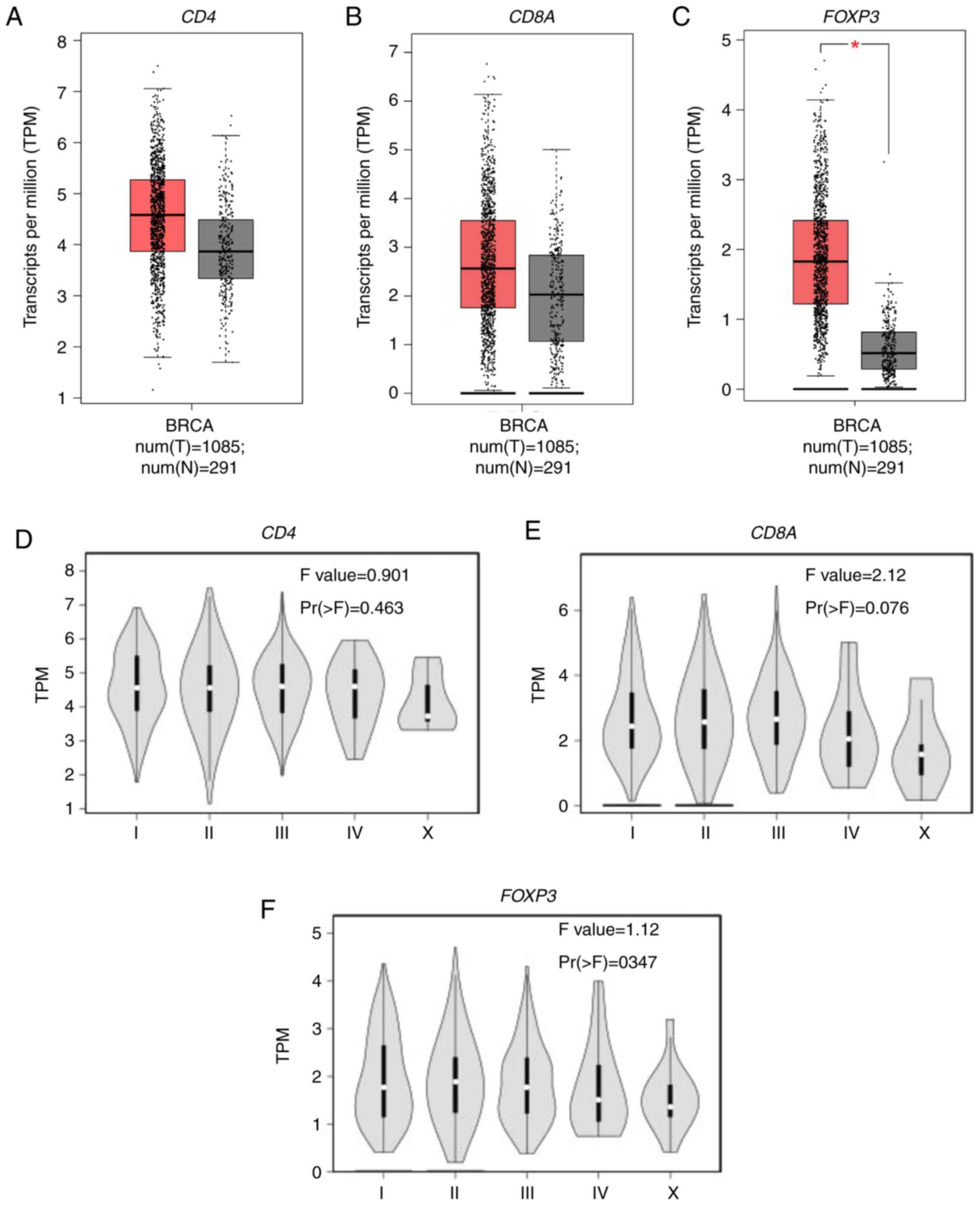 | Figure 2.CD4, CD8A and FOXP3
mRNA expression in breast cancer. TPM of (A) CD4, (B)
CD8A and (C) FOXP3 obtained from The Cancer Genome
Atlas database were compared between BC and healthy breast tissue
samples. TPM of (D) CD4, (E) CD8A and (F)
FOXP3 were compared among BC patients at different clinical
stages. *P<0.01. All experiments were repeated three times. CD,
cluster of differentiation; BRCA, Breast invasive carcinoma; BC,
breast cancer; FOXP3, forkhead box protein P3; TPM, transcripts per
million; num(T), number of tumor samples; num(N), number of normal
tissue samples. |
Distribution of tumor-infiltrating T
cells in different molecular subtypes of BC patients
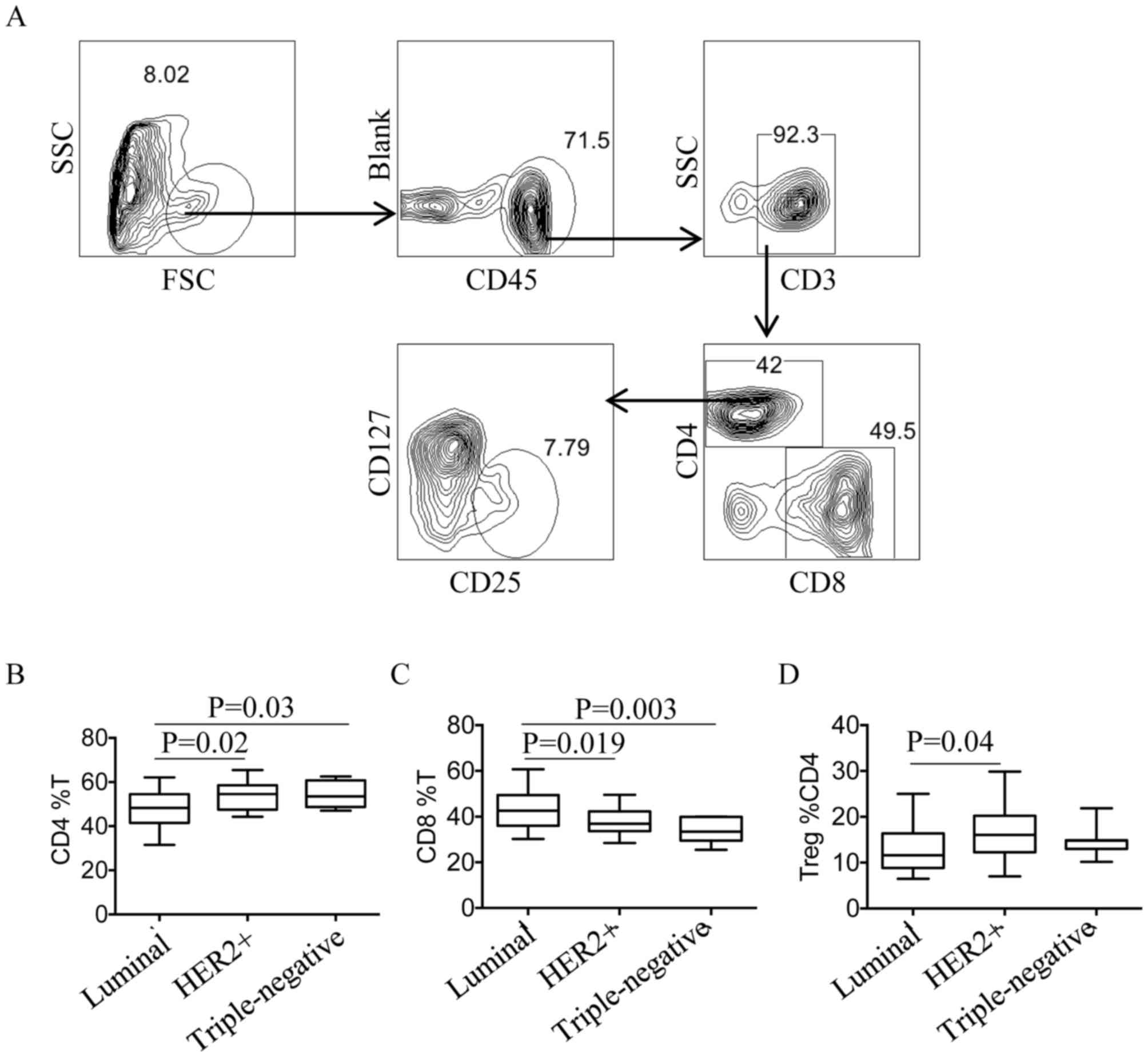
Flow cytometry was used to quantify CD4+T
cells, CD8+T cells and Tregs, and the gating strategy is
presented in Fig. 3A. First, total
lymphocytes were gated, then CD3+T cells were
distinguished from CD45+T cells. Tregs were defined as
CD4+CD25+CD127low T cells. The quantity of
CD4+T cells, CD8+T cells and Tregs was
compared between different subtypes of BC, and the percentage of
CD4+T cells was demonstrated to be significantly
increased in HER2+ and TNBC compared with the luminal
subtype (P=0.02 and P=0.03 respectively; Fig. 3B. However, the percentage of
CD8+T cells was significantly reduced in
HER2+ and TNBC patients compared with patients with the
luminal subtype (P=0.019 and P=0.003, respectively; Fig. 3C). The percentage of Tregs was also
significantly increased in HER2+ patients compared with
patients with the luminal subtype (P=0.04, Fig. 3D).
Tregs inhibit T cell cytokine
secretion in BC
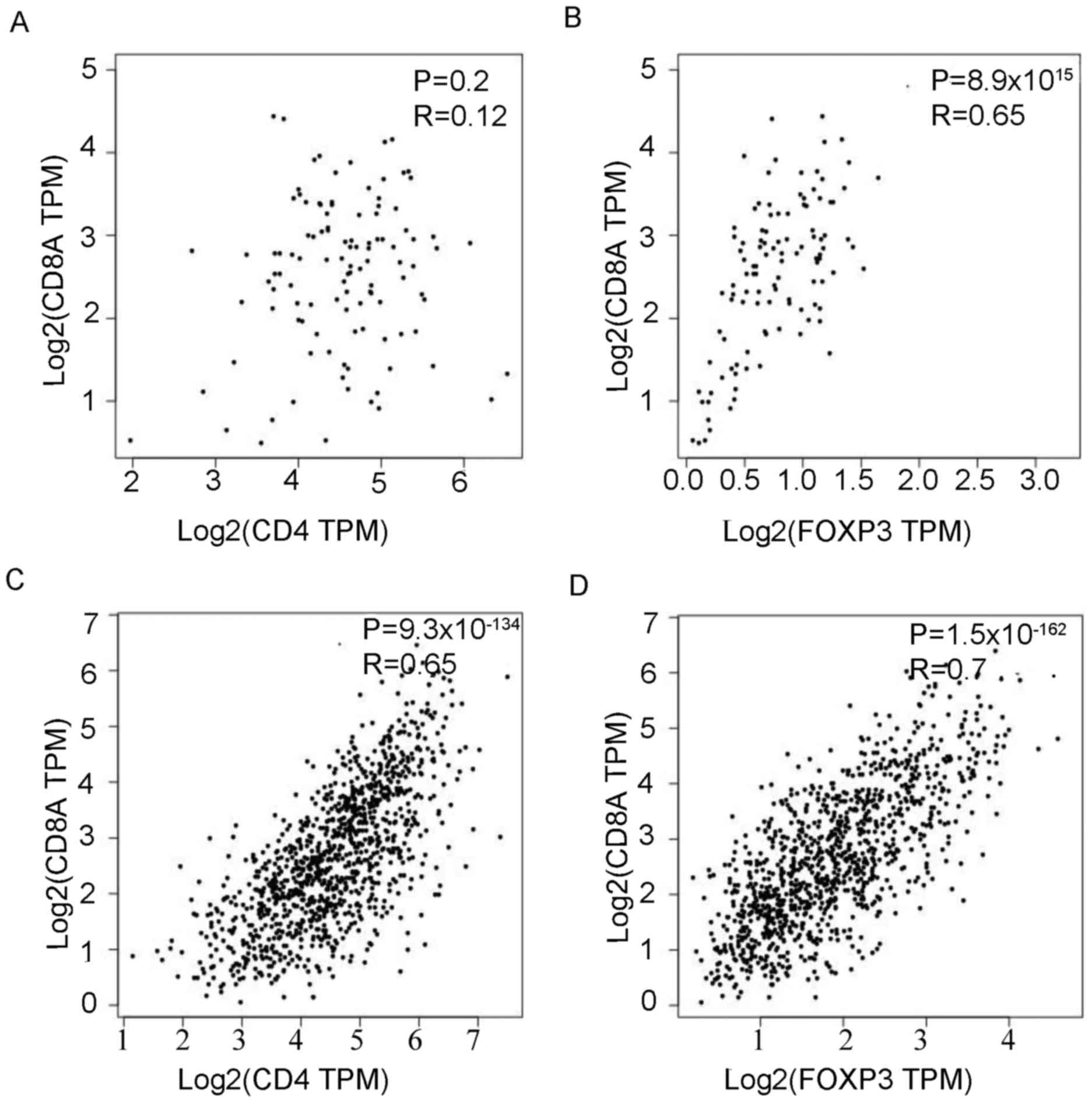
The correlation of mRNA expression in
CD4+T cells, CD8+T cells and Tregs in BC and
healthy breast tissue was next evaluated. In healthy breast tissue,
there was no association between CD4 and CD8A mRNA
expression (P=0.2; Fig. 4A).
However, CD8A mRNA expression was significantly, positively
correlated with FOXP3 expression (P=8.9×10−15;
Fig. 4B). In BC, CD8A mRNA
expression was significantly, positively correlated with CD4
(P=9.3×10−134; R=0.65; Fig.
4C) and FOXP3 (P=1.5×10−162; R=0.7; Fig. 4D) mRNA expression. Furthermore, the
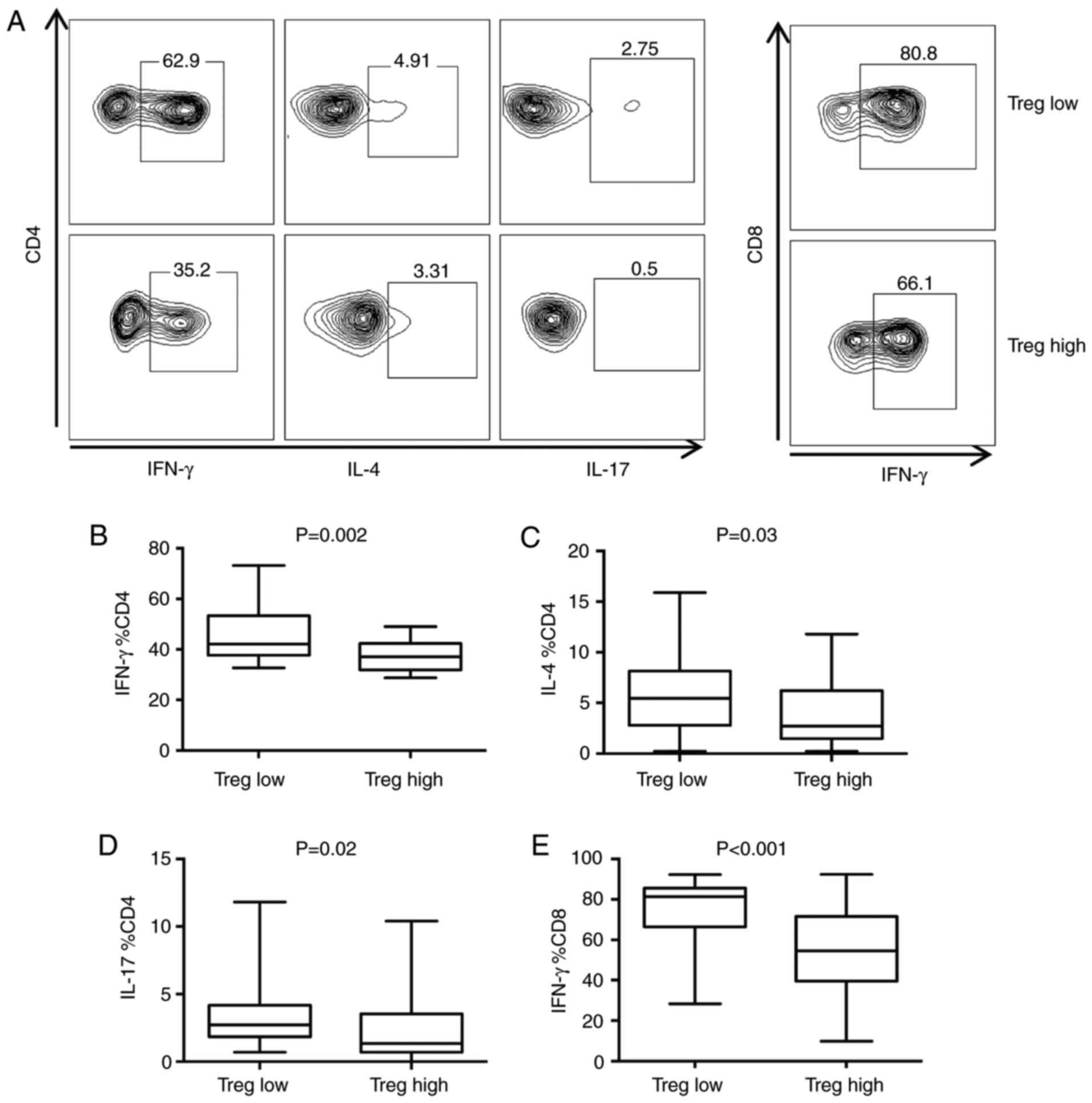
association between the number of Tregs and cytokine secretion of T
cells was studied (Fig. 5A). The
median number of Tregs was used as the cutoff to divide cells into
Tregs high and Tregs low groups. CD4+T cells secreted
significantly more interferon (IFN)-γ (P=0.002; Fig. 5B), IL-4 (P=0.03; Fig. 5C) and IL-17 (P=0.02; Fig. 5D), while CD8+T cells
secreted significantly more IFN-γ (P<0.001; Fig. 5E) in the Tregs low group compared
with the Tregs high group.
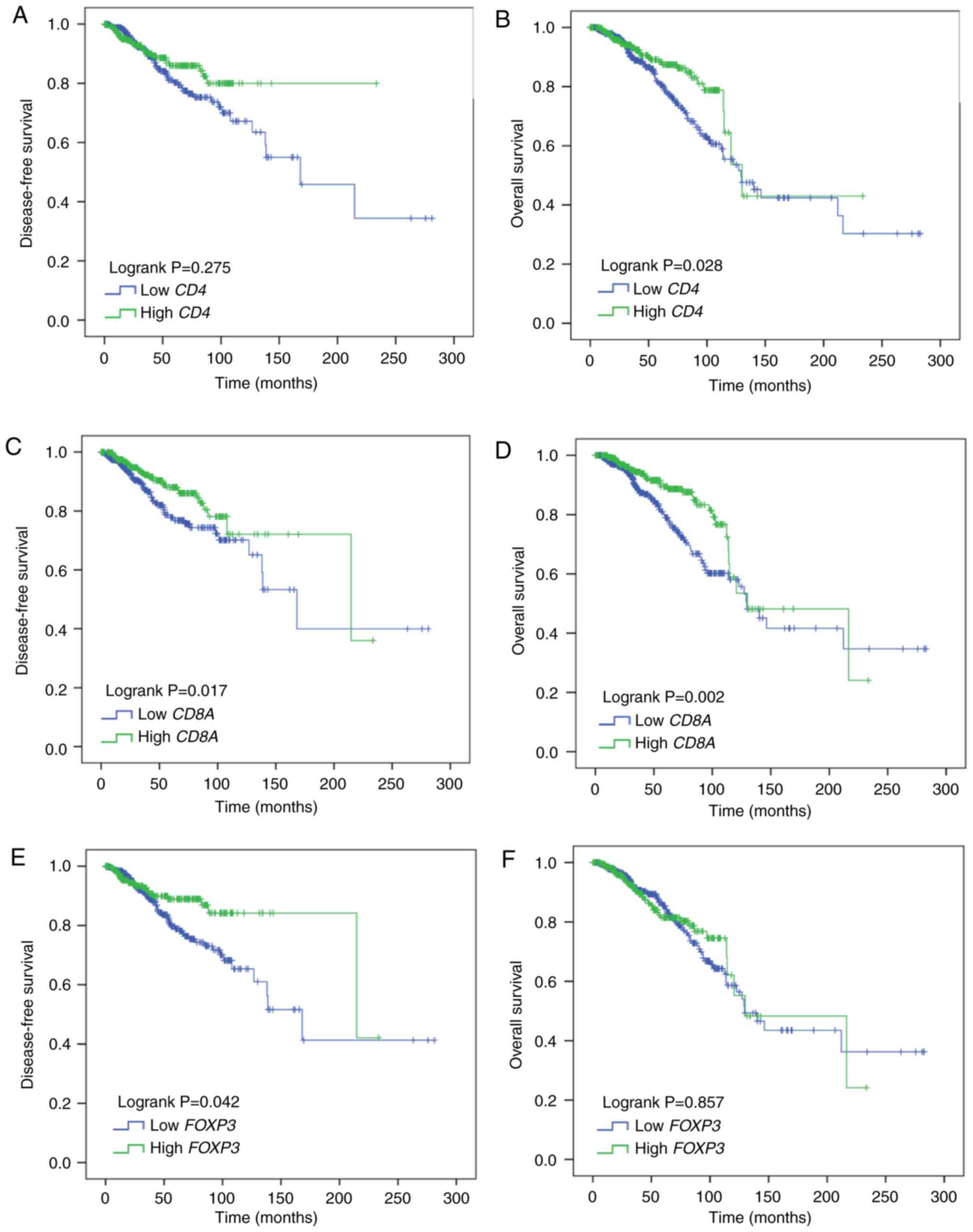
CD8A and FOXP3 mRNA expression as
prognostic markers in BC
A total of 1,029 BC patients were evaluated for
disease-free survival (DFS) and overall survival (OS). CD4
mRNA expression was not correlated with DFS (Log rank P=0.275;
Fig. 6A); however, it was
significantly, positively correlated with OS (Log rank P=0.028;
Fig. 6B). CD8A mRNA
expression was both significantly, positively correlated with DFS
(Log rank P=0.017; Fig. 6C) and OS
(Log rank P=0.002; Fig. 6D). As
for FOXP3 mRNA, its expression was significantly, positively
correlated with DFS (Log rank P=0.042; Fig. 6E) and had no correlation with OS
(Log rank P=0.857; Fig. 6F). In
univariate analysis, correlations between DFS, OS and each
clinicopathological parameter were examined for BC patients. CD8A,
FOXP3 demonstrated a significant association with DFS (P=0.018 and
0.044) and CD4. CD8A demonstrated a significant association with OS
(P=0.029 and 0.003; Table II). In
multivariate analysis, CD8A, FOXP3 remained statistically
significant (P=0.013 and 0.028) in the analysis for DFS and CD8A
remained statistically significant (P=0.028) in the analysis for OS
(Table II). These data indicate
that CD8A and FOXP mRNA expression could serve as independent
prognosis markers in BC patients.
 | Table II.Univariate and multivariate Cox
regression analyses of DFS and OS in patients with breast
cancer. |
Table II.
Univariate and multivariate Cox
regression analyses of DFS and OS in patients with breast
cancer.
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|---|
| Covariates | HR (95% CI) | P-value | HR (95% CI) | P-value |
|---|
|
|---|
| A, DFS |
|---|
| Age |
| 41–65
vs. ≤40 years old | 0.434
(0.257–0.734) | 0.002 | 0.518
(0.299–0.895) | 0.018 |
| >65
vs. ≤40 years old | 0.625
(0.339–1.151) | 0.131 | 0.717
(0.377–1.366) | 0.312 |
| Menopause status
(post vs. pre) | 1.002
(0.635–1.582) | 0.992 |
|
|
| Histology |
| ILC vs.
IDC | 1.297
(0.8–2.105) | 0.292 |
|
|
| Others
vs. IDC | 1.667
(0.83–3.349) | 0.151 |
|
|
| pT stage |
| T2 vs.
T1 | 1.794
(1.041–3.093) | 0.035 | 1.678
(0.957–2.942) | 0.071 |
| T3 vs.
T1 | 2.579
(1.338–4.97) | 0.005 | 2.408
(1.194–4.855) | 0.014 |
| T4 vs.
T1 | 7.541
(3.068–18.531) | 0.000 | 3.784
(1.447–9.899) | 0.007 |
| pN stage (positive
vs. negative) | 1.969
(1.295–2.993) | 0.002 | 1.808
(1.159–2.822) | 0.009 |
| ER (positive vs.
negative) | 0.535
(0.351–0.815) | 0.004 | 0.782
(0.418–1.464) | 0.443 |
| PR (positive vs.
negative) | 0.514
(0.342–0.771) | 0.001 | 0.574
(0.316–1.041) | 0.068 |
| HER2 (positive vs.
negative) | 0.781
(0.412–1.484) | 0.451 |
|
|
| CD4 expression
level (high vs. low) | 0.794
(0.525–1.202) | 0.276 |
|
|
| CD8A expression
level (high vs. low) | 0.608
(0.403–0.918) | 0.018 | 0.575
(0.371–0.891) | 0.013 |
| FOXP3 expression
level (high vs. low) | 0.634
(0.406–0.988) | 0.044 | 0.595
(0.374–0.947) | 0.028 |
|
| B, OS |
|
|
| Univariate
analysis | Multivariate
analysis |
|
|
|
|
|
Covariates | HR (95%
CI) | P-value | HR (95%
CI) | P-value |
|
| Age |
| 41–65
vs. ≤40 years old | 0.58
(0.331–1.016) | 0.057 | 0.553
(0.284–1.076) | 0.081 |
| >65
vs. ≤40 years old | 1.785
(1.021–3.123) | 0.042 | 1.73
(0.806–3.71) | 0.159 |
| Menopause status
(post versus pre) | 2.135
(1.246–3.661) | 0.006 | 1.638
(0.831–3.23) | 0.154 |
| Histology |
| ILC vs.
IDC | 1.082
(0.688–1.699) | 0.734 |
|
|
| Others
vs. IDC | 1.521
(0.812–2.849) | 0.191 |
|
|
| pT stage |
| T2 vs.
T1 | 1.361
(0.875–2.116) | 0.172 | 1.35
(0.851–2.141) | 0.203 |
| T3 vs.
T1 | 1.559
(0.884–2.749) | 0.125 | 1.347
(0.736–2.467) | 0.334 |
| T4 vs.
T1 | 3.277
(1.524–7.046) | 0.002 | 1.945
(0.861–4.39) | 0.109 |
| pN stage (positive
vs. negative) | 1.884
(1.301–2.727) | 0.001 | 1.852
(1.244–2.757) | 0.002 |
| ER (positive vs.
negative) | 0.631
(0.427–0.933) | 0.021 | 0.574
(0.381–0.865) | 0.008 |
| PR (positive vs.
negative) | 0.733
(0.506–1.062) | 0.101 |
|
|
| HER2 (positive vs.
negative) | 1.391
(0.852–2.271) | 0.187 |
|
|
| CD4 expression
level (high vs. low) | 0.649
(0.440–0.957) | 0.029 | 0.781
(0.522–1.169) | 0.229 |
| CD8A expression
level (high vs. low) | 0.562
(0.385–0.82) | 0.003 | 0.637
(0.426–0.953) | 0.028 |
| FOXP3 expression
level (high vs. low) | 0.967
(0.668–1.398) | 0.857 |
|
|
Discussion
Immune cells that infiltrate in BC maintain tissue
homeostasis by continuous immunosurveillance and the initiation of
inflammatory reactions (10,23).
The assessment of TILs and their subsets in BC patients by
histological methods (hematoxylin-eosin or immunohistochemistry
staining) has been widely used in previous studies (7–9,11,16),
and suggestions have been made to improve their evaluation
(22). Although flow cytometry was
seldom used to determine the distribution of TILs and their
subsets, it has the advantage of being a quantitative technique
that emphasizes the relative percentages of immune cell subsets.
This value may be as important as the absolute number of immune
cell subsets given that immune cells interact with each other in
the tissue.
A number of studies have focused on the distribution
of TILs and demonstrated that they are particularly prevalent in
ductal carcinoma and in ER negative, high Ki67 BC patients with a
high histological grade (24,25).
Similar results were observed in the present study. TIL recruitment
is influenced by a number of factors including C-X-C motif
chemokine 9 expression (26,27),
HLA class I histocompatibility antigen (28), the presence of high endothelial
venules in the tissue (29),
indoleamine 2,3-dioxygenase levels (30) and epithelial-mesenchymal transition
(11).
TIL subsets also have a particular distribution in
BC. Seo et al (11)
analyzed the correlation between absolute CD4+T cells,
CD8+T cells and FOXP3+ TIL numbers, and the
clinicopathological characteristics of tumors. In the present
study, it was demonstrated that the percentage of
tumor-infiltrating T cell subsets was associated with the BC
molecular subtype. However, further study is required to determine
the specific mechanism influencing the distribution of T cell
subsets. CD4, CD8A and FOXP3 mRNA expression was also
demonstrated to be increased in BC compared with healthy breast
tissue, indicating the important role of tumor-infiltrating T cells
in BC.
The prognostic value of tumor-infiltrating T cells,
especially Tregs, in tumors is controversial. Tregs are usually
considered an unfavorable factor because of their inhibitory
function on other effector T cells. However, a high infiltration of
Tregs was associated with a pathological complete response in BC
(31,32). Seo et al (11) postulated that the suppression of
Treg inhibitory function by chemotherapy facilitated the
CD8+ cytotoxic T cell attack on the tumor, aiding the
achievement of pathologic complete response. In the present study,
the prognostic value of FOXP3 mRNA expression was evaluated
in 1,029 BC patients and it was demonstrated to be positively
correlated with DFS but not OS. Therefore, the prognostic value of
Tregs remains to be validated.
There are certain limitations in the present study.
This was only a preliminary study and more patients are required to
validate the conclusion. In addition, more studies are needed to
investigate how the tumor-infiltrating T cells serve a positive
role in BC.
In conclusion, the present study elucidated the
distribution and interaction of TILs and their subsets in BC
patients. The results of the present study also suggest that
CD8+T cells and Tregs may be used as reliable predictors
of prognosis in BC, although further study is needed to determine
the underlying mechanism. The present study identified potential
targets for BC treatments that may provide more clinical choice in
the future.
Acknowledgements
The authors would like to thank Sarah Williams for
language editing this manuscript.
Funding
This study was supported by the Science and
Technology Planning Project of Yunnan Province (grant no.
2015FB093).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
KY designed the study. SM and LL performed the
experiments, SM, LL, MZ, WJ and HN analyzed the data. SM, LL and KY
wrote the manuscript. All authors reviewed the manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of The First People's Hospital of Yunnan Province and
written informed consent was provided by each patient. All methods
were performed in accordance with relevant guidelines and
regulations.
Patient consent for publication
Written informed consent was provided by each
patient.
Competing interests
The authors declare they have no competing
interests.
References
|
1
|
Coffelt SB, Kersten K, Doornebal CW,
Weiden J, Vrijland K, Hau CS, Verstegen NJM, Ciampricotti M,
Hawinkels LJAC, Jonkers J and de Visser KE: IL-17-producing γδ T
cells and neutrophils conspire to promote breast cancer metastasis.
Nature. 522:345–348. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Jia Y, Xu L, Lin Q, Zhu M, Ding L, Wu K
and Lu Y: Levels of lymphocyte subsets in peripheral blood prior
treatment are associated with aggressive breast cancer phenotypes
or subtypes. Med Oncol. 31:9812014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Koh CH, Bhoo-Pathy N, Ng KL, Jabir RS, Tan
GH, See MH, Jamaris S and Taib NA: Utility of pre-treatment
neutrophil-lymphocyte ratio and platelet-lymphocyte ratio as
prognostic factors in breast cancer. Br J Cancer. 113:150–158.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Liu L, Mayes PA, Eastman S, Shi H,
Yadavilli S, Zhang T, Yang J, Seestaller-Wehr L, Zhang SY, Hopson
C, et al: The BRAF and MEK inhibitors dabrafenib and trametinib:
Effects on immune function and in combination with immunomodulatory
antibodies targeting PD-1, PD-L1, and CTLA-4. Clin Cancer Res.
21:1639–1651. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
von Minckwitz G, Eidtmann H, Rezai M,
Fasching PA, Tesch H, Eggemann H, Schrader I, Kittel K, Hanusch C,
Kreienberg R, et al: Neoadjuvant chemotherapy and bevacizumab for
HER2-negative breast cancer. N Engl J Med. 366:299–309. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tan W, Zhang W, Strasner A, Grivennikov S,
Cheng JQ, Hoffman RM and Karin M: Tumour-infiltrating regulatory T
cells stimulate mammary cancer metastasis through RANKL-RANK
signalling. Nature. 470:548–553. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Denkert C, Loibl S, Noske A, Roller M,
Müller BM, Komor M, Budczies J, Darb-Esfahani S, Kronenwett R,
Hanusch C, et al: Tumor-associated lymphocytes as an independent
predictor of response to neoadjuvant chemotherapy in breast cancer.
J Clin Oncol. 28:105–113. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Denkert C, von Minckwitz G, Brase JC, Sinn
BV, Gade S, Kronenwett R, Pfitzner BM, Salat C, Loi S, Schmitt WD,
et al: Tumor-infiltrating lymphocytes and response to neoadjuvant
chemotherapy with or without carboplatin in human epidermal growth
factor receptor 2-positive and triple-negative primary breast
cancers. J Clin Oncol. 33:983–991. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Loi S, Sirtaine N, Piette F, Salgado R,
Viale G, Van Eenoo F, Rouas G, Francis P, Crown JP, Hitre E, et al:
Prognostic and predictive value of tumor-infiltrating lymphocytes
in a phase III randomized adjuvant breast cancer trial in
node-positive breast cancer comparing the addition of docetaxel to
doxorubicin with doxorubicin-based chemotherapy: BIG 02–98. J Clin
Oncol. 31:860–867. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ruffell B, Au A, Rugo HS, Esserman LJ,
Hwang ES and Coussens LM: Leukocyte composition of human breast
cancer. Proc Natl Acad Sci USA. 109:2796–2801. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Seo AN, Lee HJ, Kim EJ, Kim HJ, Jang MH,
Lee HE, Kim YJ, Kim JH and Park SY: Tumour-infiltrating CD8+
lymphocytes as an independent predictive factor for pathological
complete response to primary systemic therapy in breast cancer. Br
J Cancer. 109:2705–2713. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Coffer PJ and Burgering BM: Forkhead-box
transcription factors and their role in the immune system. Nat Rev
Immunol. 4:889–899. 2004. View
Article : Google Scholar : PubMed/NCBI
|
|
13
|
Winerdal ME, Marits P, Winerdal M, Hasan
M, Rosenblatt R, Tolf A, Selling K, Sherif A and Winqvist O: FOXP3
and survival in urinary bladder cancer. BJU Int. 108:1672–1678.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Jensen HK, Donskov F, Nordsmark M,
Marcussen N and von der Maase H: Increased intratumoral
FOXP3-positive regulatory immune cells during interleukin-2
treatment in metastatic renal cell carcinoma. Clin Cancer Res.
15:1052–1058. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kang MJ, Kim KM, Bae JS, Park HS, Lee H,
Chung MJ, Moon WS, Lee DG and Jang KY: Tumor-infiltrating
PD1-positive lymphocytes and FoxP3-positive regulatory T cells
predict distant metastatic relapse and survival of clear cell renal
cell carcinoma. Transl Oncol. 6:282–289. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Mahmoud SM, Paish EC, Powe DG, Macmillan
RD, Grainge MJ, Lee AH, Ellis IO and Green AR: Tumor-infiltrating
CD8+ lymphocytes predict clinical outcome in breast cancer. J Clin
Oncol. 29:1949–1955. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Matkowski R, Gisterek I, Halon A, Lacko A,
Szewczyk K, Staszek U, Pudelko M, Szynglarewicz B, Szelachowska J,
Zolnierek A and Kornafel J: The prognostic role of
tumor-infiltrating CD4 and CD8 T lymphocytes in breast cancer.
Anticancer Res. 29:2445–2451. 2009.PubMed/NCBI
|
|
18
|
Merlo A, Casalini P, Carcangiu ML,
Malventano C, Triulzi T, Mènard S, Tagliabue E and Balsari A: FOXP3
expression and overall survival in breast cancer. J Clin Oncol.
27:1746–1752. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ladoire S, Arnould L, Mignot G, Coudert B,
Rébé C, Chalmin F, Vincent J, Bruchard M, Chauffert B, Martin F, et
al: Presence of Foxp3 expression in tumor cells predicts better
survival in HER2-overexpressing breast cancer patients treated with
neoadjuvant chemotherapy. Breast Cancer Res Treat. 125:65–72. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Goldhirsch A, Wood WC, Coates AS, Gelber
RD, Thürlimann B and Senn HJ; Panel members, : Strategies for
subtypes-dealing with the diversity of breast cancer: Highlights of
the St. Gallen International expert consensus on the primary
therapy of early breast cancer 2011. Ann Oncol. 22:1736–1747. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Tang Z, Li C, Kang B, Gao G, Li C and
Zhang Z: GEPIA: A web server for cancer and normal gene expression
profiling and interactive analyses. Nucleic Acids Res. 45:W98–W102.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Salgado R, Denkert C, Demaria S, Sirtaine
N, Klauschen F, Pruneri G, Wienert S, van den Eynden G, Baehner FL,
Penault-Llorca F, et al: The evaluation of tumor-infiltrating
lymphocytes (TILs) in breast cancer: Recommendations by an
International TILs working group 2014. Ann Oncol. 26:259–271. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Demaria S, Pikarsky E, Karin M, Coussens
LM, Chen YC, El-Omar EM, Trinchieri G, Dubinett SM, Mao JT, Szabo
E, et al: Cancer and inflammation: promise for biologic therapy. J
Immunother. 33:335–351. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Tung NM and Winer EP: Tumor-infiltrating
lymphocytes and response to platinum in triple-negative breast
cancer. J Clin Oncol. 33:969–971. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Mohammed ZM, Going JJ, Edwards J,
Elsberger B, Doughty JC and McMillan DC: The relationship between
components of tumour inflammatory cell infiltrate and
clinicopathological factors and survival in patients with primary
operable invasive ductal breast cancer. Br J Cancer. 107:864–873.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Walser TC, Ma X, Kundu N, Dorsey R,
Goloubeva O and Fulton AM: Immune-mediated modulation of breast
cancer growth and metastasis by the chemokine Mig (CXCL9) in a
murine model. J Immunother. 30:490–498. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ohtani H, Jin Z, Takegawa S, Nakayama T
and Yoshie O: Abundant expression of CXCL9 (MIG) by stromal cells
that include dendritic cells and accumulation of CXCR3+ T cells in
lymphocyte-rich gastric carcinoma. J Pathol. 217:21–31. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Dong DD, Yie SM, Li K, Li F, Xu Y, Xu G,
Song L and Yang H: Importance of HLA-G expression and tumor
infiltrating lymphocytes in molecular subtypes of breast cancer.
Hum Immunol. 73:998–1004. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Martinet L, Garrido I, Filleron T, Le
Guellec S, Bellard E, Fournie JJ, Rochaix P and Girard JP: Human
solid tumors contain high endothelial venules: Association with T-
and B-lymphocyte infiltration and favorable prognosis in breast
cancer. Cancer Res. 71:5678–5687. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Jacquemier J, Bertucci F, Finetti P,
Esterni B, Charafe-Jauffret E, Thibult ML, Houvenaeghel G, van den
Eynde B, Birnbaum D, Olive D and Xerri L: High expression of
indoleamine 2,3-dioxygenase in the tumour is associated with
medullary features and favourable outcome in basal-like breast
carcinoma. Int J Cancer. 130:96–104. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Oda N, Shimazu K, Naoi Y, Morimoto K,
Shimomura A, Shimoda M, Kagara N, Maruyama N, Kim SJ and Noguchi S:
Intratumoral regulatory T cells as an independent predictive factor
for pathological complete response to neoadjuvant paclitaxel
followed by 5-FU/epirubicin/cyclophosphamide in breast cancer
patients. Breast Cancer Res Treat. 136:107–116. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Lee HJ, Seo JY, Ahn JH, Ahn SH and Gong G:
Tumor-associated lymphocytes predict response to neoadjuvant
chemotherapy in breast cancer patients. J Breast Cancer. 16:32–39.
2013. View Article : Google Scholar : PubMed/NCBI
|