Introduction
Knee osteoarthritis (KOA), also known as
degenerative arthropathy and hypertrophic arthritis, is one of the
most common degenerative diseases. Its basic pathological changes
include degeneration, loss of articular cartilage and osteophyte
formation in the articular cartilage and the lower border of the
cartilage that manifests as joint pain, tenderness, stiffness,
joint swelling, limited mobility and joint deformities, usually
involving the finger joints, knees, spine and hip (1). Kinesitherapy may provide therapeutic
effects in the treatment of KOA (2–3). The
current study used kinesitherapy to treat patients with KOA and
explored its mechanism of action by concurrently measuring knee
function and the levels of tumor necrosis factor-α (TNF-α), high
sensitivity C-reactive protein (hs-CRP) and matrix
metalloproteinase 3 (MMP-3) in the synovial fluid.
Materials and methods
Clinical design
Study sample
Patients (n=100, 38 male and 62 female, aged 41–63
years) were diagnosed with KOA in the First People’s Hospital of
Yancheng City from January 2010 to December 2011. All patients
provided their informed consent. The patients were randomly divided
into the treatment and control groups according to the order of
their diagnosis times. The patients in the treatment group received
daily oral diclofenac sodium (Difene®) and
kinesitherapy. The patients in the control group received only
daily oral diclofenac sodium. The treatment group contained 50
patients (20 males and 30 females, aged 44–62 years, mean
53.0±5.6). The numbers of patients having disease durations of
<3 months, 3 months to 1 year, 1–2 years and 2–3 years were 9,
13, 18 and 10, respectively. The control group contained 50
patients (18 males and 32 females, aged 41–63 years, mean
52.3±7.0). The numbers of patients having disease durations of
<3 months, 3 months to 1 year, 1–2 years and 2–3 years were 8,
15, 20 and 7, respectively. The patients in the two groups were
comparable in gender distribution, age and disease duration without
any statistically significant differences (P<0.05). The study
was approved by the ethics committee of Yancheng Health Vocational
and Technical College, Yancheng, China.
Diagnostic criteria
The knee osteoarthritis diagnostic criteria were as
defined by the American Rheumatism Association (4): a) knee joint disease (pain duration
≥14 days within one month prior to treatment); b) X-ray showing
osteophyte formation at the joint margins; c) clear, sticky
synovial fluid with a leukocyte count <2,000 cells/ml; d)
absence of synovial fluid index, age >40 years; e) knee morning
stiffness <30 min; and f) crepitation during knee motion.
Patients with a,b, or a,c,e,f, or a,d,e,f combinations of the above
criteria were confirmed.
Inclusion and exclusion criteria
Inclusion criteria included: diagnostic criteria of
KOA; not receiving other treatment methods or medication; age 40–70
years; and a disease classification of I-III by X-ray. Exclusion
criteria included: significant stenosis of the joint space or bone
bridge connection between the joints manifested as bony ankylosis;
disease classification IV by X-ray; primary disease of the knee
affecting joint structures; active gastrointestinal diseases and/or
esophageal or peptic ulcer within 30 days of the trial; concurrent
cardiovascular, cerebrovascular, liver, kidney or hematopoietic
system diseases; mental illness; pregnancy and lactation; and known
allergy to diclofenac.
Experimental methods
Treatment methods
The patients in the control group received oral
diclofenac sodium (75 mg, twice daily). Patients in the treatment
group received oral diclofenac sodium (75 mg, twice daily) and
kinesitherapy. Kinesitherapy included knee joint flexion and
extension (active exercise) followed by isometric contraction of
the quadriceps femoris at angles of 0° and 90° from the knee joint.
Contractions were held continuously for 10 sec followed by 10 sec
of relaxation, repeated 10 times for one exercise circle. The
patients also performed 5 circles at each angle, with 1 min between
circles. Isometric exercises were performed in the sitting position
to avoid the effects of weight-bearing on the knee joints. Patients
carried out the exercises twice per day in the morning and
afternoon, 4 days per week (5).
The two groups received treatment for 4 consecutive weeks.
Functional evaluation of the knee
joint
The joint function index refers to the sum of the
evaluation scores for rest pain, activity pain, tenderness,
swelling and joint function. Rest pain was scored as: painless;
mild pain, no effect on life and work; moderate pain, effect on
life and work; or severe pain, effect on sleep. The activity pain
was scored as: painless; mild pain, pain during forced activity;
moderate pain, pain during common activity; or severe pain, pain
during light activity. Tenderness was scored as: no tenderness;
mild tenderness, no effect on activity; moderate tenderness, frown;
or severe tenderness, retreat. Swelling was scored as: no swelling;
light swelling, limited to local sites of the joints; moderate
swelling, in the joint range; or severe swelling, diffusing to the
surrounding tissue. Joint function was scored as: normal; mild
limitation, no effect on life and work; moderate limitation, effect
on life and work; or severe limitation, sitting and/or lying
position, unable to take care of themselves. For all parameters,
the four possible scores were 0, 1, 2 and 3 (6).
Outcome measures
Synovial fluid (1.5 ml) was extracted from the
medial compartment of the knee prior to and following 4 weeks of
treatment and was stored at −20°C until further analysis. An
enzyme-linked immunosorbent assay (ELISA) was used to evaluate the
TNF-α, hs-CRP and MMP-3 levels in the synovial fluid. The ELISA
kits were acquired from Wuhan Boster Biological Engineering, Ltd.
(Wuhan, China). The assays were performed according to the
manufacturer’s instructions.
Therapeutic effect criteria
The therapeutic effect was determined using the
Clinical Guideline of New Drugs for Traditional Chinese Medicine
(7). The therapeutic effects were
divided into four grades: clinically-controlled; significantly
effective; effective; and ineffective.
Statistical analysis
SPSS 17.0 software was used for analysis. The
independent Student’s t-test was used to compare the ages of the
two groups and the χ2 test was used to compare gender
and disease duration difference. Efficacies were compared using the
Mann-Whitney U test. The knee function index scores and cytokine
levels prior to and following treatment were compared by
repeat-measures analysis of variance. The above analyses were
two-sided and P<0.05 was considered to indicate a statistically
significant result.
Results
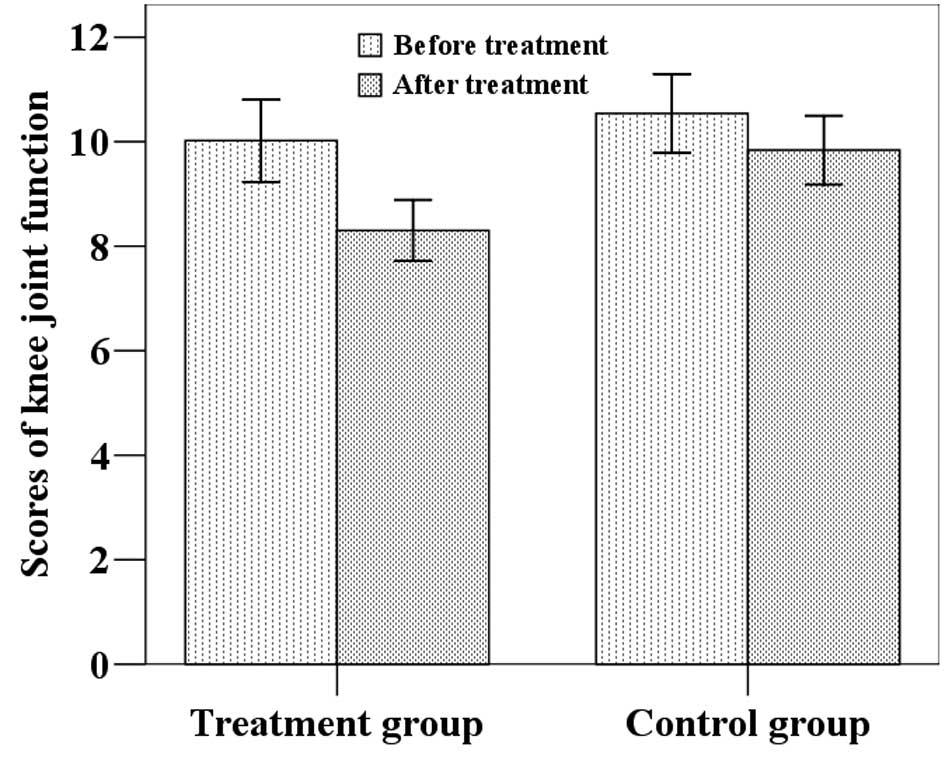
Knee function index scores
The mean knee function index scores (±SD) of the
patients in the treatment group were 10.0 (±2.8) at baseline and
8.3 (±2.1) following treatment, while the scores of the patients in
the control group were 10.5 (±2.7) at baseline and 9.8 (±2.3)
following the 4-week study (Fig.
1). Statistical analysis revealed that the post-treatment knee
function index scores of the patients in the two groups were
significantly lower than those before treatment (P<0.05). The
score in the treatment group was significantly lower than that in
the control group (F=4.695, P=0.033).
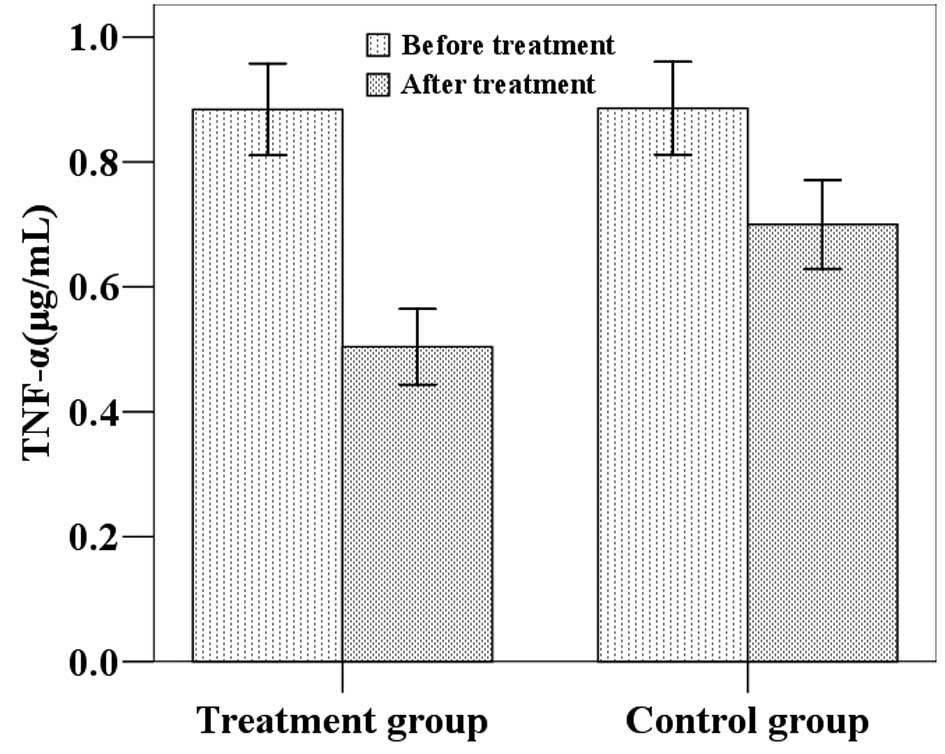
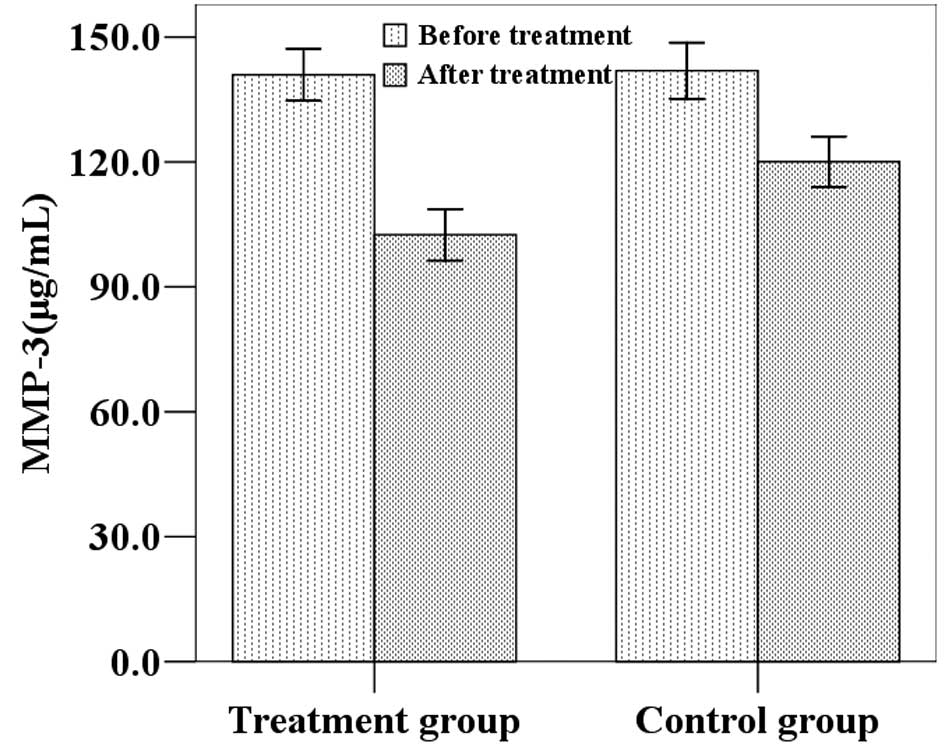
TNF-α, hs-CRP and MMP-3 expression in
synovial fluid
The mean (±SD) TNF-α, hs-CRP and MMP-3 levels in the
treatment group were 0.88 (0.26), 11.33 (0.90) and 140.94 (22.02)
μg/ml at baseline and 0.50 (0.21), 6.01 (1.13) and 102.51 (21.84)
μg/ml following treatment. The mean (±SD) TNF-α, hs-CRP and MMP-3
levels in the control group were 0.89 (0.26), 11.46 (0.84) and
141.92 (23.78) μg/ml at baseline and 0.70 (0.25), 8.69 (1.36) and
120.06 (21.53) μg/ml following the four-week study period (Figs. 2–4). Statistical analysis demonstrated that
the post-treatment TNF-α, hs-CRP and MMP-3 levels were
significantly lower than the baseline values in the two groups. In
addition, post-treatment TNF-α, hs-CRP and MMP-3 levels in the
treatment group were significantly lower than in the control group
(P<0.05).
Clinical efficacy comparison
The efficacy rate was 90.0% (45/50) in the treatment
group and 84% (42/50) in the control group, as shown in Table I. Statistical analysis showed that
the therapeutic effect in the kinesitherapy treatment group was
significantly improved compared with that in the control group
(Z=2.736, P=0.006).
 | Table IComparison of the therapeutic efficacy
between groups [n(%)]. |
Table I
Comparison of the therapeutic efficacy
between groups [n(%)].
| Groups | Cases |
Clinically-controlled | significantly
effective | effective | ineffective |
|---|
| Treatment group | 50 | 11 (22.0) | 21 (42.0) | 13 (26.0) | 5 (10.0) |
| Control group | 50 | 3 (6.0) | 16 (32.0) | 23 (46.0) | 8 (16.0) |
| Total | 100 | 14 (14.0) | 37 (37.0) | 36 (36.0) | 13 (13.0) |
Discussion
KOA primarily affects the physical functions and
activities of patients, particularly daily activities related to
walking and transferring that are essential for the maintainance of
daily independence and the quality of life (8). Maly et al(9) found that the pain and limited
activity of KOA reduces patients’ evaluations of self-worth.
Therefore, researchers continue to search for safe and reliable
treatment methods to effectively treat KOA and reduce its adverse
effects on the quality of life.
Kinesitherapy has previously been proposed as the
treatment of choice for KOA in certain countries (10). In this study, kinesitherapy was
used to treat KOA and its effects on knee function and the levels
of TNF-α, hs-CRP and MMP-3 in synovial fluid were observed. The
results revealed a gradual improvement in knee function following
treatment. The combination of kinesitherapy and diclofenac was able
to improve joint function and movement and may support healthy
cartilage metabolism and repair.
KOA pathogenesis is an inflammatory process
involving multiple cytokines and inflammatory mediators (11). TNF-α selectively inhibits the
generation of cartilage collagen and proteoglycan synthesis and
promotes its degradation. Increased cytokine levels in the knee
joint synovial fluid are closely related to KOA severity (12). hs-CRP is a highly sensitive marker
of inflammation and Spector et al found that hs-CRP levels
were significantly higher in the serum of KOA patients than that of
healthy controls and that hs-CRP levels positively correlated with
osteoarthritis disease activity (13). It is considered that the
pathogenesis of knee osteoarthritis primarily involves the
degeneration and degradation of articular cartilage, while the main
cause of cartilage degeneration is the abnormal degradation of the
extracellular matrix on which chondrocytes are dependent.
MMPs are involved in the degradation of the
extracellular matrix. MMP-3 is an important member of the MMP
family that is able to degrade extracellular proteoglycans, type IV
collagen and a number of other matrix protein substrates. Type IV
collagen is a non-indigenous fibrosis collagen primarily located at
the articular cartilage surface. MMP-3 is also involved in the
activation of interstitial collagenase. Interstitial collagenase
degrades type II collagen and so MMP-3 is indirectly involved in
type II collagen degradation. Studies have revealed that the serum
and synovial fluid MMP-3 levels of patients with osteoarthritis are
significantly higher than those of normal controls and are related
to the severity of the joint disease (14). Therefore, detection of TNF-α,
hs-CRP and MMP-3 levels in the synovial fluid of KOA patients may
be used for comprehensive diagnosis and for the evaluation of
disease severity and prognosis. The results of this study show that
kinesitherapy significantly reduces TNF-α, hs-CRP and MMP-3 levels
in the synovial fluid of KOA patients. This mechanistic effect may
inhibit inflammatory damage to chondrocytes and the cartilage
matrix, delay articular cartilage degeneration and improve the
therapeutic effect and knee function.
References
|
1
|
Page CJ, Hinman RS and Bennell KL:
Physiotherapy management of knee osteoarthritis (Review). Int J
Rheum Dis. 14:145–151. 2011. View Article : Google Scholar
|
|
2
|
Topp R, Woolley S, Hornyak J III, Khuder S
and Kahaleh B: The effect of dynamic versus isometric resistance
training on pain and functioning among adults with osteoarthritis
of the knee. Arch Phys Med Rehabil. 83:1187–1195. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Deyle GD, Allison SC, Matekel RL, Ryder
MG, Stang JM, Gohdes DD, Hutton JP, Henderson NE and Garber MB:
Physical therapy treatment effectiveness for osteoarthritis of the
knee: a randomized comparison of supervised clinical exercise and
manual therapy procedures versus a home exercise program. Phys
Ther. 85:1301–1317. 2005.
|
|
4
|
Altman R, Asch E, Bloch D, et al:
Development of criteria for the classification and reporting of
osteoarthritis. Classification of osteoarthritis of the knee
Diagnostic and Therapeutic Criteria Committee of the American
Rheumatism Association. Arthritis Rheum. 29:1039–1049. 1986.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Yang YH, Su GH, Luo JM, et al: Overall
acupotome zonulolysis in combination of kinesitherapy in treatment
of 44 cases of knee osteoarthritis. Academic Journal of Anhui
University of Traditional Chinese Medicine. 28:43–45. 2009.(In
Chinese).
|
|
6
|
Kang XP and Ye YJ: The effect of articular
injection of chitosan on knee function and inflammatory factors in
synovial fluid. Chinese Clinical Rehabilitation. 9:42–43. 2008.(In
Chinese).
|
|
7
|
Zheng XY: Clinical Guideline of New Drugs
for Traditional Chinese Medicine in Treatment of Osteoarthritis.
Clinical Guideline of New Drugs for Traditional Chinese Medicine
China. Medical Science and Technology Press; Beijing: pp. 350–353.
2002, (In Chinese).
|
|
8
|
Kuptniratsaikul V, Tosayanonda O,
Nilganuwong S and Thamalikitkul V: The efficacy of a muscle
exercise program to improve functional performance of the knee in
patients with osteoarthritis. J Med Assoc Thai. 85:33–40.
2002.PubMed/NCBI
|
|
9
|
Maly MR and Krupa T: Personal experience
of living with knee osteoarthritis among older adults. Disabil
Rehabil. 29:1423–1433. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
O’Reilly SC, Muir KR and Doherty M:
Effectiveness of home exercise on pain and disability from
osteoarthritis of the knee: a randomised controlled trial. Ann
Rheum Dis. 58:15–19. 1999.PubMed/NCBI
|
|
11
|
Lin MN and Liu XX: Synergistic effect of
cytokines in osteoarthritis. Academic Journal of Fujian College of
Traditional Chinese Medicine. 16:69–70. 2006.(In Chinese).
|
|
12
|
Wang DH, Bao F, Wu ZH, Sun H and Zhang YX:
Influence of acupuncture on IL-1beta and TNF-alpha expression in
the cartilage of rats with knee osteoarthritis. Zhongguo Gu Shang.
24:775–778. 2011.(In Chinese).
|
|
13
|
Spector TD, Hart DJ, Nandra D, Doyle DV,
Mackillop N, Gallimore JR and Pepys MD: Low-level increases in
serum C-reactive protein are present in early osteoarthritis of the
knee and predict progressive disease. Arthritis Rheum. 40:723–727.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Aktas E, Sener E and Gocun PU:
Mechanically induced experimental knee osteoarthritis benefits from
anti-inflammatory and immunomodulatory properties of simvastatin
via inhibition of matrix metalloproteinase-3. J Orthop Traumatol.
12:145–151. 2011. View Article : Google Scholar
|