Introduction
Septic shock is a result of severe sepsis, which is
produced by microorganisms and their toxins. These cause low blood
pressure, hypoxemia, metabolic acidosis, systemic inflammatory
reaction and multiple organ dysfunctions characteristic of complex
pathophysiological processes. Septic shock affects critical care
patients and is one of the main causes of mortality (1). Myocardial dysfunction is a common
complication during sepsis and significantly contributes to the
mortality of patients with septic shock (2). Previous studies on septic shock have
concentrated on the generation of inflammatory mediators, including
tumor necrosis factor-α (TNF-α) and interleukin-1β (IL-1β) and
damage to liver, lung and kidney tissues (3). Myocardial depression is a
well-recognized manifestation of organ dysfunction in sepsis.
However, the various mechanisms underlying septic cardiac
dysfunction remain unclear and none of the current therapeutic
strategies designed specifically to target myocardial dysfunction
have proven to be effective in patients with septic shock (4).
The janus kinase-signal transduction and activator
of transcription (JAK-STAT) signaling pathway is one of the best
understood signal transduction cascades and is essential for
cytokine receptor signaling involved in immune and inflammatory
responses. JAK-STAT signaling molecules bind specific nucleotide
sequences in the gene promoter region of cytokines and inflammatory
cytokines, including TNF-α, IL-1β and IL-6, inducing gene
expression (5,6). Our previous study revealed that the
JAK/STAT signaling pathway was activated and the expression of
TNF-α and IL-6 increased in rat lung tissue with sepsis (7). Inhibition of the JAK/STAT pathway
attenuated multiple organ dysfunction in rats with sepsis (8). These observations indicate that the
activation of the JAK/STAT signaling pathway is associated with the
occurrence and development of systemic inflammatory reaction. Thus,
preventing the activation of JAK/STAT signaling pathways to reduce
inflammation may have clinical benefits for patients suffering from
septic shock.
OMT, the major active component of the traditional
Chinese medicine, kushen, has been well studied and its
anti-inflammatory activity has been demonstrated in experimental
animal models and clinical studies (9,10).
OMT exhibits a variety of biological activities, including
clearance of heat and toxic material, anti-inflammatory, inhibition
of liver fibrosis, elevation of white blood cells, coxsackie virus
resistance and regulation of immunity and other aspects of
pharmacological action (11,12).
It has been reported that OMT may reduce the generation of oleic
acid in rats induced by acute lung injury by inhibiting the p38
MAPK signaling pathway and the expression of TNF-α (13). Lung tissue damage in mice with
endotoxemia has been identified to be inhibited by OMT and this
mechanism is associated with regulation of the LPS recognition
receptor expression and downregulation of the expression of
downstream inflammatory factors (14). These observations indicate that OMT
plays a vital role in anti-inflammatory reactions and are
consistent with our hypothesis that OMT may prevent myocardial
damage with infectious shock by inhibiting the activation of
JAK/STAT signaling pathways.
In the present study, cecal ligation and puncture
(CLP) was performed in a rat model to examine the effect of OMT on
inhibition of the JAK/STAT signaling pathway in cardiac muscle
injury with septic shock.
Materials and methods
Chemicals
Oxymatrine was purchased from Ningxia Qi Yuan
Pharmaceutical Co. (Yinchuan, China). Dexamethasone was from Hubei
Day Drug Pharmaceutical Co. (Hubei, China). Coomassie Brilliant
Blue protein quantification kit was purchased from Nanjing
Jiancheng Bioengineering Company (Nanjing, China). The
125I tumor necrosis factor-α and 125I
interleukin-1β radiation immunoassay kits were purchased from the
Beijing Chemclin Bioengineering Company (Beijing, China). TRIzol
was obtained from Invitrogen Life Technologies (Carlsbad, CA. USA).
PrimeScript RT reagent kit was from Takara Bio (Takara Bio, Inc.,
Dalian, China). RT-PCR kit was from Promega (Promega Corporation,
Madison, WI, USA). Rat monoclonal antibodies against JAK2 and STAT3
were from Santa Cruz Biotechnology, Inc. (Santa Cruz, CA, USA) and
IP cell lystates and the BCA protein concentration assay kit were
from Jiangsu Green Biotechnology Company (Jiangsu, China).
Animals
Animal studies were approved by the Ningxia Medical
University Animal Care Committee (Ningxia, China). Male
Sprague-Dawley rats, specific pathogen free, weighing 200–250 g,
were obtained from the Animal Center of Ningxia Medical University
[SCXK (Ning) 2005-001]. Rats were randomly divided into 7 groups
(n=8): sham surgery, OMT control, CLP model, positive control [CLP
+ dexamethasone (DEX), 10 mg/kg] and CLP + OMT 52, 26 and 13 mg/kg.
The septic shock model was induced by CLP as described previously
(15). Rats received tail vein
injection with drugs (volume, 5 ml/kg). In the sham-operated and
OMT control groups, the rats received intravenous injection with
normal saline and OMT (26 ml/kg) and the CLP group received normal
saline (26 ml/kg) only. Following treatment, the cecum was exposed
under sterile conditions. Postoperative monitoring rat tail artery
pressure was performed, and rat blood pressure dropped to 2/3 of
base blood pressure and pulse pressure <20 mmHg was the standard
used to judge the success of the sepsis model.
Cardiac function and histological
analyses
To examine cardiac function, the right common
carotid artery was used to determine the rat heart rate (HR), mean
arterial pressure (MAP), left intraventricular pressure change rate
(LVdp/dt max), left ventricular end systolic pressure (LVESP) and
left ventricular end diastolic pressure (LVEDP) by inserting the
cardiac catheterization. The heart was then removed for
histological analysis. Apical tissue blocks (~2 mm3)
were collected and fixed in 10% formalin, then embedded in
paraffin. Following haematoxylin-eosin staining, pathological
changes of myocardial tissue were observed under the light
microscope. Additional myocardial tissues ~2 mm3 were
placed in 2% glutaraldehyde and sectioned as electron microscopy
specimens to determine ultrastructural changes.
RT-PCR analysis
Total RNA was prepared using TRIzol and was
reverse-transcribed to cDNA using a PrimeScript RT reagent kit.
RT-PCR was performed using a commercially available kit as follows:
35 cycles of denaturation at 94°C for 60 sec, annealing at 58°C for
60 sec and extension at 72°C for 50 sec. β-actin was used as an
internal control to evaluate relative expression of TNF-α and
IL-1β. The primers used were: TNF-α (355 bp)
5′-CAATGGCATGGATCTCAAAG-3′ and 5′-CAGAGCAATGACTCCAAAGT-3′, IL-1β
(399 bp) 5′-AGAAGCTGTGGCAGCTACCT-3′ and 5′-TTGGGA
TCCACACTCTCCAG-3′, β-actin (299 bp) 5′-AGGTGAGAG GGAAATCGTGCG-3′
and 5′-GTGCCACCAGACAGC ACTGTGC-3′.
Western blot analysis
Total protein concentration was measured using a BCA
kit. Equal amounts of protein (40 μg) were separated
electrophoretically using 10% SDS-PAGE and the gel was then
transferred to a 0.45 μm PVDF membrane. Blots were soaked in
blocking buffer (5% non-fat milk) and then incubated with primary
antibodies (anti-JAK, 1:200; anti-STAT3, 1:200; anti-β-actin,
1:1,000) overnight at 4°C. Following thorough washing with TBST
buffer, horseradish peroxidase conjugated secondary antibodies
(1:10,000) were applied and immune complexes were then visualized
using the enhanced chemiluminescence detection system.
Radioimmunoassay
Levels of TNF-α and IL-1β in myocardial tissue were
determined by radioimmunoassay. Myocardial tissue (100 mg) was
mixed with a 3-fold volume of PBS and homogenized, then centrifuged
at 12900 x g for 20 min at 4°C. Protein levels of TNF-α and IL-1β
in the supernatant were quantified using a radioimmunoassay assay
kit.
Statistical analysis
Results were presented as the mean ± SEM of at least
three separate experiments. Data were analyzed by one-way ANOVA,
followed by the Student-Newman-Keuls post hoc test. P<0.05 was
considered to indicate a statistically significant difference.
Results
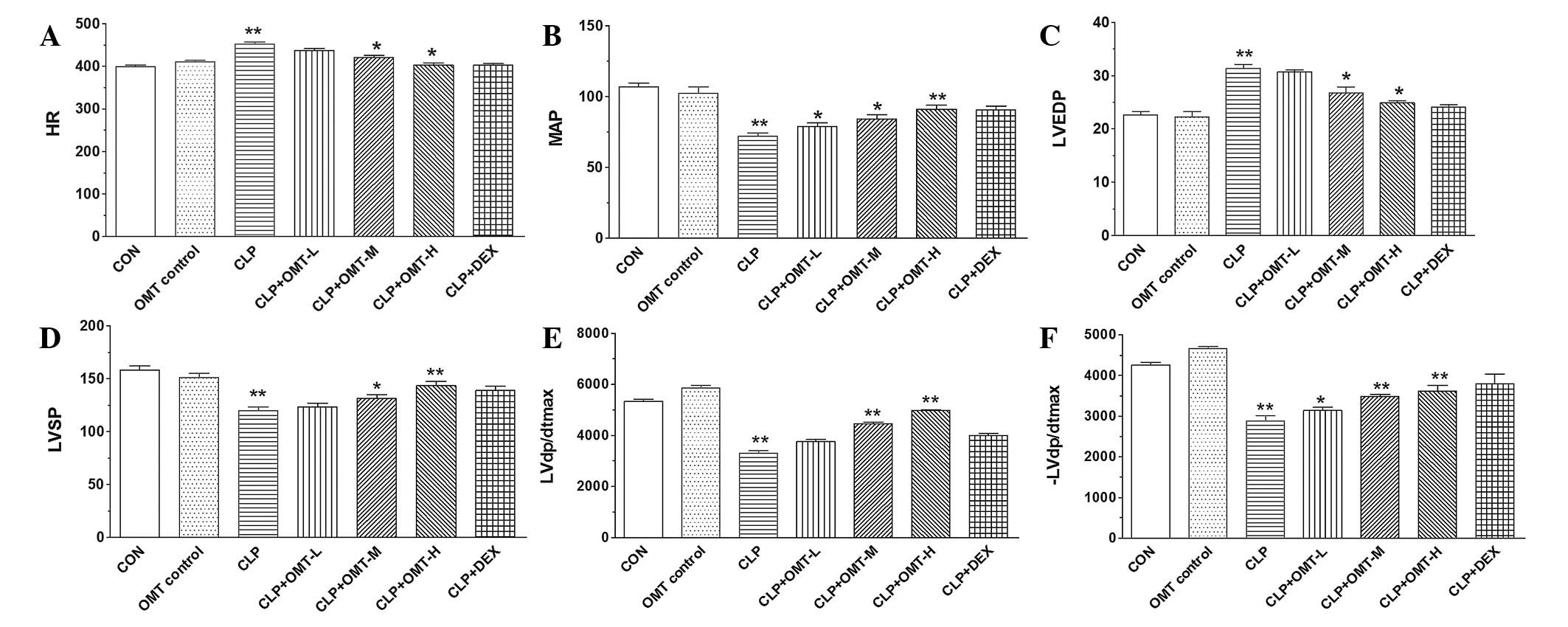
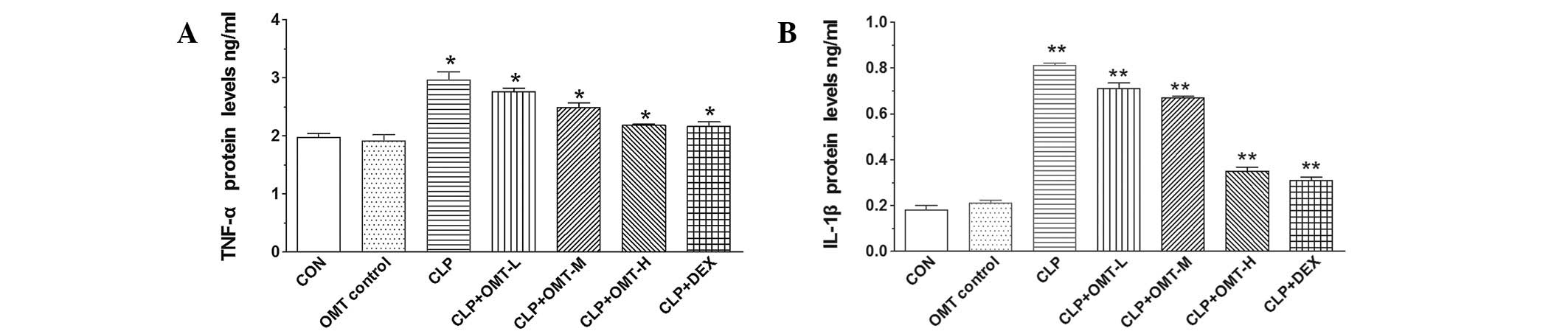
Cardiac function assay
Changes in myocardial diastolic function are an
important characteristic of septic shock (16). A rat model of CLP was used to
evaluate the effect of OMT on cardiac function in rats with septic
shock. As demonstrated in Table I
and Fig. 1, cardiac function
parameters, including HR, MAP, LVSP, LVEDP, LVdp/dtmax and
-LVdp/dtmax indices were not affected in the OMT control group
compared with the control (CON) group. In the CLP group,
significant changes in all indices were identified (P<0.01)
compared with CON. HR increased by 15%, MAP reduced by 33%, LVSP
reduced by 24%, LVEDP increased by 47%, LVdp/dtmax reduced by 38%
and -LVdp/dtmax reduced by 32%. Following treatment with various
doses of OMT, the CLP + high-dose OMT group was observed to reduce
HR by 11% (P<0.05), increase MAP by 26% (P<0.01), increase
LVSP by 20% (P<0.01), reduce LVEDP by 20% (P<0.01) and
increase LVdp/dtmax by 50% (P<0.01) and -LVdp/dtmax by 25%
(P<0.01) compared with CLP. The CLP + middle dose OMT group was
observed to have a reduced HR by 7% (P<0.05), increased MAP by
17% (P< 0.05), increased LVSP in 10% (P<0.05), reduced LVEDP
by 14% (P<0.05) and increased LVdp/dtmax by 35% (P<0.01) and
-LVdp/dtmax by 25% (P<0.01). HR was reduced by 3% (P>0.05),
MAP was increased by 9% (P<0.05), LVSP was increased by 3%
(P>0.05), LVEDP was reduced by 2% (P>0.05), LVdp/dtmax was
increased by 13% (P<0.05) and -LVdp/dtmax was increased by 9%
(P<0.05) in the CLP + low-dose OMT group. The positive control
CLP + DEX group did not reveal marked differences in various
indices compared with CON, CLP + high-dose OMT and CLP +
middle-dose OMT, however a significant difference in all indices
was found when compared with CLP and CLP + low-dose OMT.
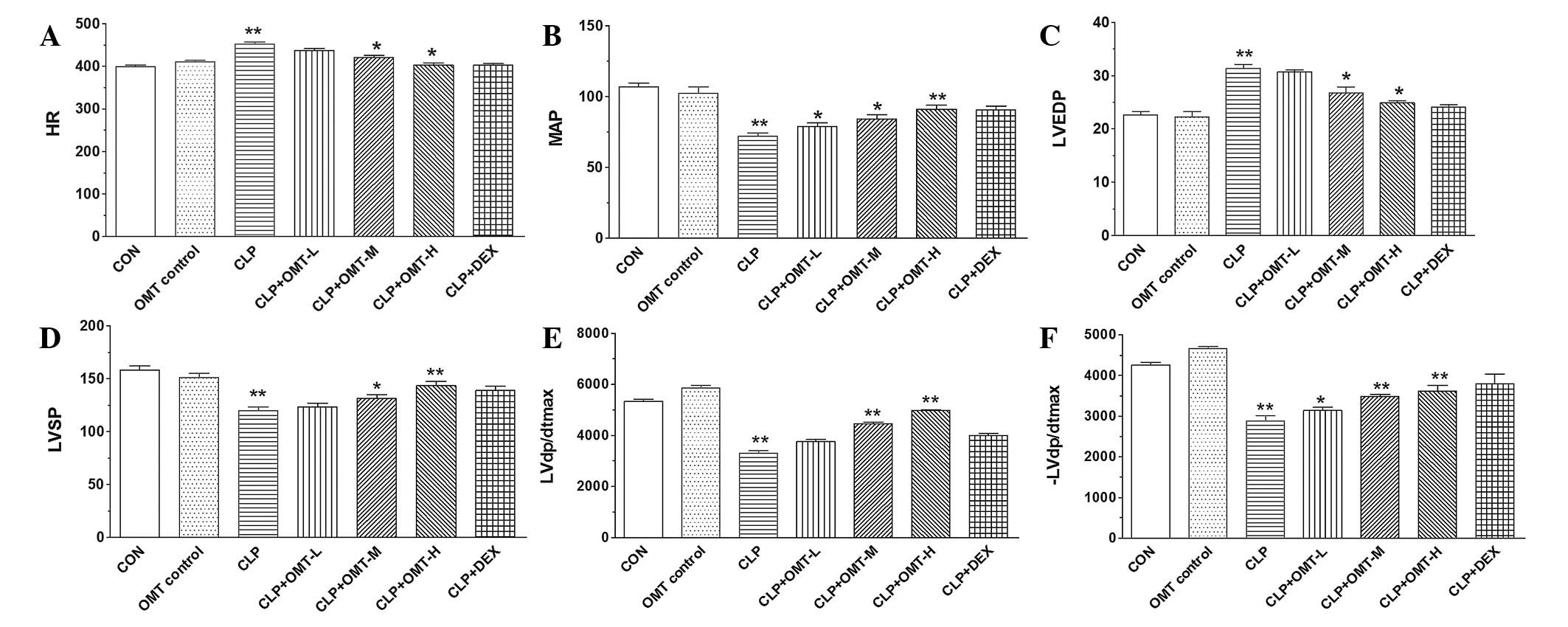 | Figure 1Effect of OMT on cardiac function in
rats with septic shock (n=8). Indexes (A) HR, (B) MAP, (C) LVEDP,
(D) LVSP, (E) LVdp/dtmax and (F) -LVdp/dtmax indices were measured
by inserting the cardiac catheterization in all animal groups,
including CON, OMT CON, CLP, CLP + L, CLP + M, CLP + H, CLP + DEX
group. *P<0.05 and **P<0.01, vs. CON.
OMT, oxymatrine; CLP, cecal ligation and puncture; DEX,
dexamethasone; HR, heart rate; MAP, mean arterial pressure; LVdp/dt
max, left intraventricular pressure change rate; LVESP, left
ventricular end systolic pressure; LVEDP, left ventricular end
diastolic pressure; CON, control. |
 | Table IEffect of OMT on cardiac function in
rats with septic shock (mean ± SD; n=8) |
Table I
Effect of OMT on cardiac function in
rats with septic shock (mean ± SD; n=8)
| Group | Dose (mg/kg) | HR | MAP | LVSP | LVEDP | ± LVdp/dtmax |
|---|
| CON | | 398.61±11.30 | 106.80±8.04 | 157.90±11.27 | 22.64±1.78 |
5352.41±220.30/−4254.40±184.02 |
| OMT control | 26 | 410.30±10.66 | 102.41±12.52 | 150.92±11.76 | 22.21±3.01 |
5876.43±237.64/−4658.64±129.54 |
| CLP | | 452.42±12.34 | 72.11±6.02 | 119.74±10.63 | 31.32±2.24 |
3310.70±296.08/−2879.22±375.54 |
| CLP + OMT-L | 13 | 437.60±11.59 | 78.80±7.32 | 123.6±9.73 | 30.7±1.16 |
3755.91±228.40/−3134.20±225.34 |
| CLP + OMT-M | 26 | 420.54±13.42 | 84.11±9.09 | 131.42±10.36 | 26.80±2.93 |
4459.41±146.35/−3481.04±148.30 |
| CLP + OMT-H | 52 | 402.61±15.39 | 91.10±8.14 | 143.31±11.58 | 24.90±1.16 |
4967.21±101.53/−3605.70±415.43 |
| CLP + DEX | 10 | 409.31±12.22 | 90.52±8.06 | 139.10±10.74 | 24.11±1.25 |
4010.70±184.02/−3795.70±652.99 |
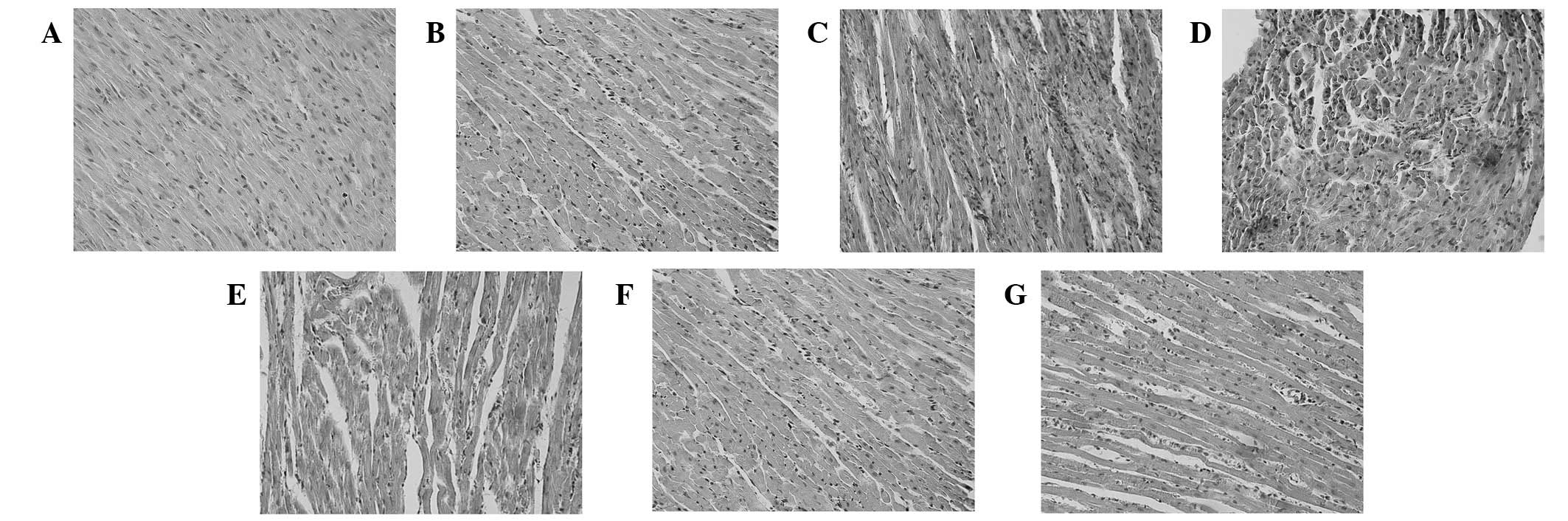
Myocardial histological assay
Differences in myocardial tissue were not identified
between the CON and OMT control group. The endocardial membrane was
complete, with no edema and fibrous connective tissue hyperplasia.
The myocardial stripes were clear, the nucleus centered and no
vasodilation and inflammatory cell infiltration were observed.
Epicardial membrane demonstrated integrity in the stroma without
inflammatory exudate (Fig. 2A and
B). As shown in Fig. 2C, CLP
rat myocardial tissue revealed marked subendocardial myocardial
structural disorder compared with the CON group. Infiltration of a
number of inflammatory cells with a considerable number of
mononuclear cells and a few lymphocytes and neutrophils and
telangiectasia and bleeding were observed. The CLP group also
exhibited interstitial edema, fibroblast proliferation and cell
necrosis and fibrosis to various degrees. Following various doses
of OMT treatment, myocardial tissue damage in the CLP + OMT-L group
was reduced compared with CLP, however, low levels of disorganized
myocardial structures with inflammatory cell infiltration,
telangiectasia and bleeding, as well as cell necrosis and fibrosis
were identified (Fig. 2D).
However, myocardial tissue damage in the CLP + OMT-M and CLP +
OMT-H groups was markedly reduced and a normal basic cardiac
structure was observed (Fig. 2E and
F). Edema, degeneration and necrosis were significantly reduced
but remained accompanied by a small amount of inflammatory cell
infiltration and exudative changes. Compared with the CLP group,
myocardial injury was significantly reduced in the CLP + DEX group
and myocardial cells were organized in rows, accompanied by a small
amount of inflammatory cell infiltration. However, no significant
changes in cell swelling, degeneration and necrosis were identified
(Fig. 2G).
The results indicate that OMT may reduce myocardial
injury and have a protective effect on cardiac structure and
function in rats with septic shock. Results in the CLP + OMT groups
with high and middle doses and the positive control (CLP + DEX
group) were consistent.
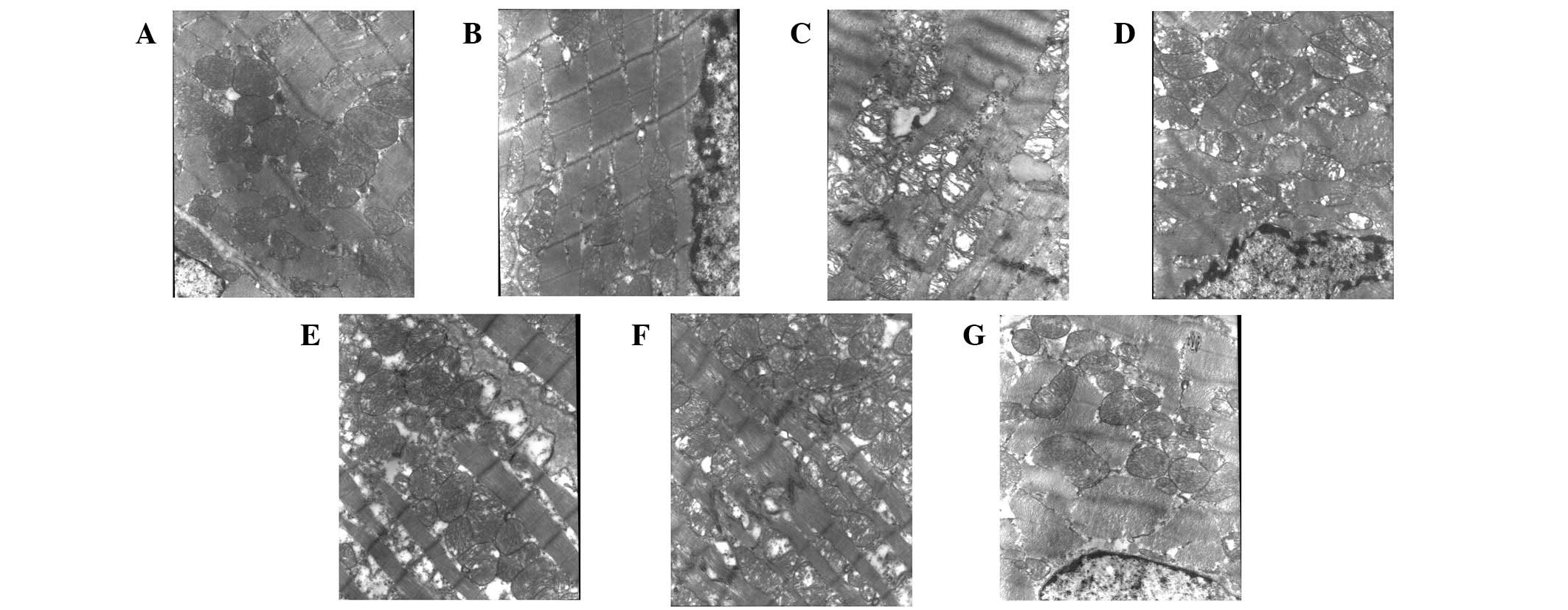
Myocardial ultramicro-histological
changes
Compared with CON, myocardial tissue, including
myofilaments, sarcomere, capillaries, mitochondrion, sarcoplasmic
reticulum and nucleolus in the OMT control group were observed to
exhibit no significant changes and all had normal shapes and clear
structures (Fig. 3A and B).
Myofilaments and sarcomere arrangement was normal and blood flow
volume was normal. Mitochondrial structure was normal and clear
with complete membranes, dense ridges and a clear matrix. The
intercalated disc was in order and successive. The sarcoplasmic
reticulum was smooth and continuous. The nucleolus was clear with
visible light nucleus pycnosis and the chromatin was uniform.
However, the ultramicro-histological myocardial tissue of the CLP
group was observed to be significantly damaged. As is evident in
Fig. 3C, mitochondria were
markedly swollen, leading to membrane damage and disordered
cristae. In addition, myofilaments were dissolved and sarcomeres
were disordered, leading to vacuoles. The nucleus was significantly
reduces in size and the chromatin margination was observed.
Dissolution of intercalated disc demonstrated discontinuity and
uneven distribution. However, compared with the CLP, the injuries
of ultramicro-histological myocardial tissue in CLP + OMT groups
were significantly reduced (Fig.
3D-F). Myocardial fiber arrangement was normal, the majority of
the mitochondrial structure was complete and ridge dense
arrangement had a regular pattern. Although a section of the ridge
was undefined, the arrangement was still regular, mitochondrial
swelling was reduced and specific incidences of damage were not
recovered fully. The CLP + OMT-L group was found to exhibit the
highest levels of damage. The ultramicro-histological myocardial
tissue in the CLP + DEX group was almost normal and rarely injured
(Fig. 3G). Myocardial fibers were
aligned, the majority of mitochondrial structures were complete,
ridges were dense, regions of the ridge were undefined, fibers were
arranged in an organized manner, specific incidences of damage were
not recovered fully and intercalated disc demonstrated clear
continuity. The sarcoplasmic reticulum was smooth and continuous.
The nucleolus was clear with light nucleus pycnosis and the
chromatin was uniform.
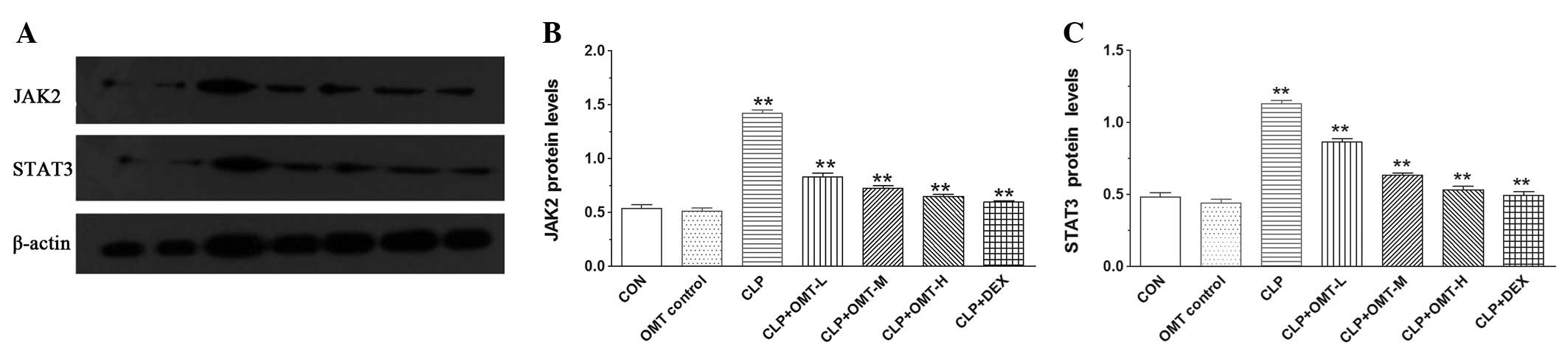
Effect of OMT on JAK2 and STAT3 protein
expression
Western blot analysis revealed that JAK2 and STAT3
protein levels in OMT control myocardial tissue was similar to that
of the CON group but was observed to be significantly higher in the
CLP group (P<0.05). However, JAK2 and STAT3 protein levels in
CLP + OMT and positive control groups were markedly decreased
compared with CLP (P<0.05; Fig.
4).
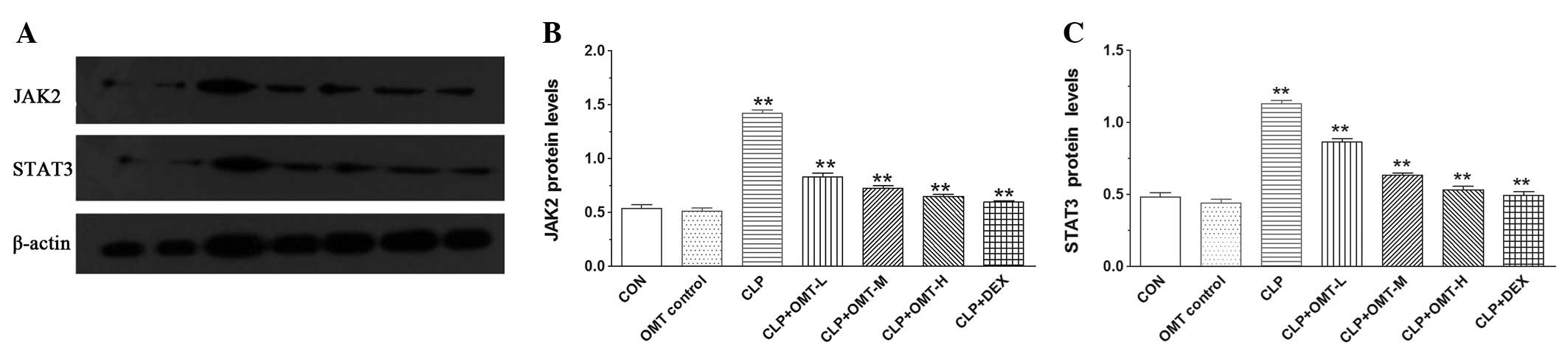 | Figure 4Effect of OMT on JAK2 and STAT3
protein expression in rat cardiac muscle with septic shock. (A)
Western blot analysis of JAK2 and STAT3 protein expression, with
β-actin as the internal control. Quantification of (B) JAK2 and (C)
STAT3 protein expression. Lanes 1–7 show CON, OMT control, CLP, CLP
+ OMT-L, CLP + OMT-M, CLP + OMT-H and CLP + DEX groups,
respectively. *P<0.05 and **P<0.01 vs.
CON. OMT, oxymatrine; CLP, cecal ligation and puncture; DEX,
dexamethasone; JAK-STAT, janus kinase-signal transducer and
activator of transcription; CON, control. |
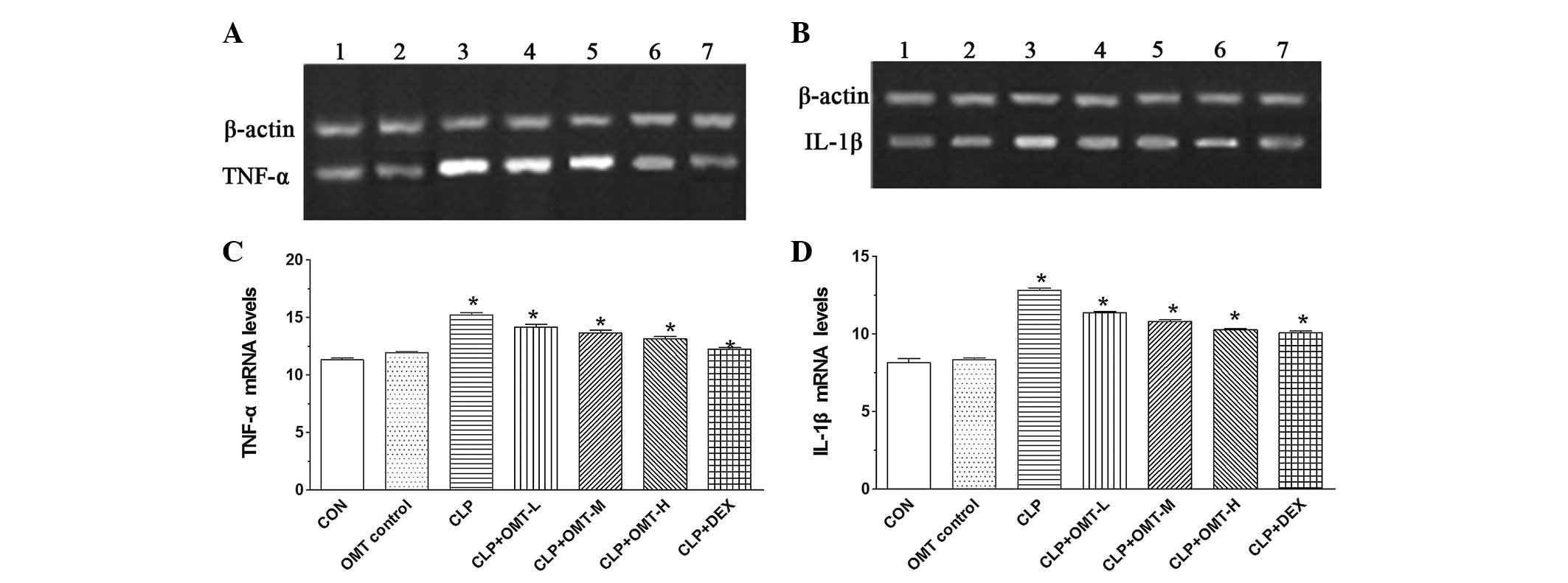
Effect of OMT on TNF-α and IL-1β protein
expression
Radioimmunoassay revealed that TNF-α and IL-1β
protein levels in the CLP group was significantly increased
compared with the CON and OMT control (P<0.05). However,
compared with the CLP group, TNF-α and IL-1β protein levels in CLP
+ OMT and the positive control were found to be significantly
decreased (P<0.05; Fig. 5).
Effect of OMT on TNF-α and IL-1β mRNA
expression
TNF-α and IL-1β mRNA levels in OMT control and CON
myocardial tissue were normal, however, levels were identified to
be significantly increased in the CLP group (P<0.05). Compared
with the CLP group, TNF-α and IL-1β mRNA levels in CLP + OMT and
the positive control were markedly decreased (P<0.05; Fig. 6).
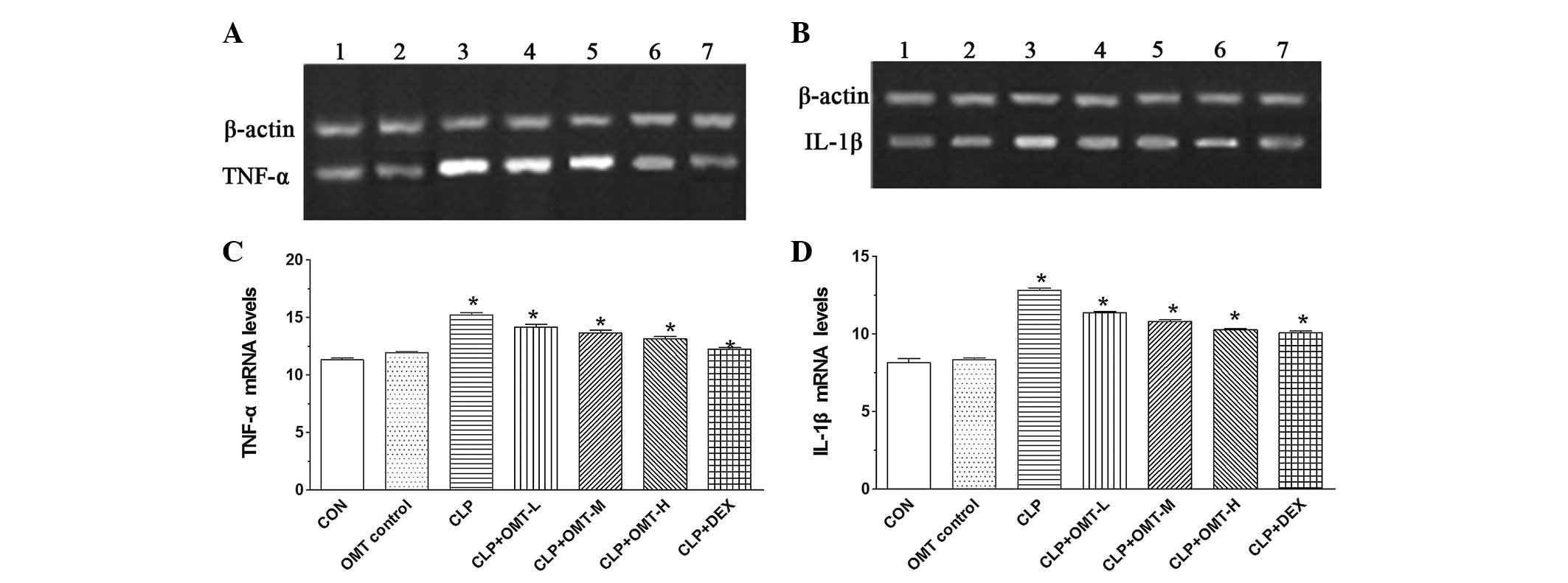 | Figure 6Effect of OMT on TNF-α and IL-1β mRNA
expression in rat cardiac muscle with septic shock. RT-PCR of (A)
TNF-α and (B) IL-1β mRNA expression. M, marker; lanes 1–7, CON, OMT
control, CLP, CLP + OMT-L, CLP + OMT-M, CLP + OMT-H and CLP + DEX
groups, respectively. Length of PCR product for TNF-α, IL-1β and
β-actin were 355, 399 and 662 bp, respectively. Quantification of
(C) TNF-α and (D) IL-1β mRNA levels. *P<0.05 vs. CON.
OMT, oxymatrine; CLP, cecal ligation and puncture; DEX,
dexamethasone; TNF-α, tumor necrosis factor-α; IL-1β,
interleukin-1β; CON, control. |
Discussion
Septic shock is a serious complication in acutely
ill patients suffering from severe trauma, burns, shock, infection
and major surgery. The widespread activation of cells in septic
shock results in the release of a number of inflammatory mediators,
including cytokines, chemokines, prostaglandins, lipid mediators
and reactive oxygen species. Excess production of inflammatory
mediators in sepsis is associated with numerous signaling pathways,
including MAPK and NF-κB and in particular, JAK/STAT (17–22).
JAK2 and STAT1/3 promote the release of cytokines, including TNF-α
and IL-1β and are markedly associated with the uncontrolled
inflammatory response, septic shock and acute organ injury
(23). Wang et al reported
that IL-2 and IFN-γ are directly associated with the JAK/STAT
pathway activation and inhibition of this pathway reduces
dysfunction of vital organs in septic shock in rats (16). An extremely limited number of
studies have analyzed the role of the JAK/STAT signaling pathway in
septic shock.
OMT is an alkaloid extracted from the Sophora
flavescens Ait and its bioactivities have been studied
extensively (24–26). OMT has been found to attenuate
hepatic fibrosis via targeting hepatic stellate cells and reducing
bleomycin-induced pulmonary fibrosis in mice via inhibition of the
inducible nitric oxide synthase expression and the TGF-β/Smad
signaling pathway (24–26). In addition, OMT was found to
exhibit a neuroprotective effect in cerebral ischemia/reperfusion.
However, the pharmacological effects of OMT on cardiac tissues and
the mechanisms remain unknown.
Our previous study revealed that OMT significantly
inhibited JAK2 and STAT3 activity in septic rat lung tissue,
decreased TNF-α and IL-6 levels, W/D ratio and pulmonary
coefficient and reduced lung tissue congestion, edema, neutrophil
infiltration, hyaline membrane formation and other lesions
(7). In the present study, septic
shock rat models were developed to examine the effect of OMT on
cardiac tissue injuries and the JAK/STAT signaling pathway by
detecting JAK2 and STAT3 expression and the release of TNF-α and
IL-6. Histological analysis revealed that OMT intervention markedly
reduced septic shock in rats caused by increases in HR and LVSP.
Decreased ±LVdp/dtmax increased myocardial compliance, reduced
myocardial stiffness, improved heart function, enhanced myocardial
contraction force, corrected ventricular end-diastolic pressure
increases and reduced preload. These cardiac protective effects are
associated with activation of the JAK/STAT signaling pathway.
Western blot analysis and RT-PCR revealed that OMT inhibits the
activation of JAK2 and STAT3 leading to a reduced expression of
proinflammatory cytokines, TNF-α and IL-6. These results are
consistent with our previous study (27).
This is the first study to demonstrate that cardiac
injuries are associated with the JAK/STAT signaling pathway and OMT
has the ability to suppress the activation of this signaling
pathway. Activation of JAK2 and STAT3 leads to the upregulation of
TNF-α and IL-6. Release of TNF-α and IL-6 has marked effects on
cardiac tissue. Current observations indicate that OMT protects
myocardial injury and is associated, at least in part, with
significant inhibition of JAK2/STAT3 signaling in rats with septic
shock and may be a potential therapeutic agent for the treatment of
septic shock.
In summary, the present results provide valuable
insight into the mechanisms underlying the cardiac protective
effects of OMT and the possible application of OMT for the
treatment of inflammatory diseases accompanied by septic shock.
Acknowledgements
The present study was supported by grants from the
Natural Science Foundation of Ningxia (NZ1194), National Natural
Science Foundation of China (30960108, 31060140 and 31260243), 2012
Yinchuan Key Scientific and Technological Project for Minghao
Zhang, Key Project of Department of Public Health of Ningxia
(2012004) and the project-sponsored by SRF for ROCS, SEM for Yin
Wang.
References
|
1
|
Van Amersfoort ES, Van Berkel TJC and
Kuiper J: Receptors, mediators and mechanisms involved in bacterial
sepsis and septic shock. Clin Microbiol Rev. 16:379–414.
2003.PubMed/NCBI
|
|
2
|
Kumar A, Haery C and Parrillo JE:
Myocardial dysfunction in septic shock. Crit Care Clin. 16:251–287.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Cao W, Wang Y, Lv X, Yu X, Li X, Li H,
Wang Y, Lu D, Qi R and Wang H: Rhynchophylline prevents cardiac
dysfunction and improves survival in lipopolysaccharide-challenged
mice via suppressing macrophage I-κBα phosphorylation. Int
Immunopharmacol. 14:243–251. 2012.PubMed/NCBI
|
|
4
|
Celes MR, Prado CM and Rossi MA: Sepsis:
going to the heart of the matter. Pathobio. 80:70–86. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mao YJ, Li HH, Li JF and Shen JS: Signal
transduction by protein tyrosine kinases and antitumor agents. Yao
Xue Xue Bao. 43:323–334. 2008.(In Chinese).
|
|
6
|
Liu X, Ye L, Bai Y, Mojidi H, Simister NE
and Zhu X: Activation of the JAK/STAT-1 signaling pathway by
IFN-gamma can down-regulate functional expression of the MHC class
I-related neonatal Fc receptor for IgG. J Immunol. 181:449–463.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhang MH, Li GZ and Cao J: Effect of
oxymatrine on JAK/STAT iteral in rat lung tissue with sepsis.
Zhongguo Zhong Yao Za Zhi. 35:103–107. 2010.(In Chinese).
|
|
8
|
Matsukawa A: STAT proteins in innate
immunity during sepsis lessons from gene knockout mice. Acta Med
Okayama. 5:239–245. 2007.PubMed/NCBI
|
|
9
|
Yuan X, Wang Y, Du D, Hu Z, Xu M, Xu M and
Liu Z: The effects of the combination of sodium ferulate and
oxymatrine on lipopolysaccharide-induced acute lung injury in mice.
Inflammation. 35:1161–1168. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Cui HL, Wang YF, Li XL and Kang QX:
Clinical observation of matrine injection in the treatment of 51
cases of various types of cancers. Shanxi Med J. 22:232–233.
1993.
|
|
11
|
Shi GF and Li Q: Effects of oxymatrine on
experimental hepatic fibrosis and its mechanism in vivo. World J
Gastroenterol. 11:268–271. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zheng P, Niu FL, Liu WZ, Shi Y and Lu LG:
Anti-inflammatory mechanism of oxymatrine in dextran sulfate
sodium-induced colitis of rats. World J Gastroenterol.
11:4912–4915. 2005.PubMed/NCBI
|
|
13
|
Xu GL, Yao L, Rao SY, Gong ZN, Zhang SQ
and Yu SQ: Attenuation of acute lung injury in mice by oxymatrine
is associated with inhibition of phosphorylated p38
mitogen-activated protein kinase. J Ethnopharmacol. 98:177–183.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Han Y, Zhou Y and Liu Q: Antiendotoxic
effects of Sophora alopecuroides L. Zhong Yao Cai.
29:1066–1068. 2006.(In Chinese).
|
|
15
|
Jing HM: A model of sepsis in rat after a
cecal ligation and puncture. Chin J Pathophysiol. 6:126–127.
1990.(In Chinese).
|
|
16
|
Wang SB, Yao YM and Chen JS: Relationship
between activation of Janus kinase/signal transducer and activator
of transcription pathway and multiple organ dysfunction in rats
with sepsis. Infection Inflammation Repair. 29:42–44. 2004.(In
Chinese).
|
|
17
|
Risco A, del Fresno C, Mambol A,
Alsina-Beauchamp D, MacKenzie KF, Yang HT, Barber DF, Morcelle C,
Arthur JS, Ley SC, Ardavin C and Cuenda A: p38γ and p38δ kinases
regulate the Toll-like receptor 4 (TLR4)-induced cytokine
production by controlling ERK1/2 protein kinase pathway activation.
Proc Natl Acad Sci USA. 109:11200–11205. 2012.
|
|
18
|
Oishi H, Takano K, Tomita K, Takebe M,
Yokoo H, Yamazaki M and Hattori Y: Olprinone and colforsin daropate
alleviate septic lung inflammation and apoptosis through
CREB-independent activation of the Akt pathway. Am J Physiol Lung
Cell Mol Physiol. 303:130–140. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lee C, Lim HK, Sakong J, Lee YS, Kim JR
and Baek SH: Janus kinase-signal transducer and activator of
transcription mediates phosphatidic acid-induced interleukin
(IL)-1beta and IL-6 production. Mol Pharmacol. 69:1041–1047.
2006.PubMed/NCBI
|
|
20
|
Qian F, Deng J, Gantner BN, Flavell RA,
Dong C, Christman JW and Ye RD: Map kinase phosphatase 5 protects
against sepsis-induced acute lung injury. Am J Physiol Lung Cell
Mol Physiol. 302:866–874. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Krüttgen A and Rose-John S: Interleukin-6
in sepsis and capillary leakage syndrome. J Interferon Cytokine
Res. 32:60–65. 2012.PubMed/NCBI
|
|
22
|
Hui L, Yao Y, Wang S, Yu Y, Dong N, Li H
and Sheng Z: Inhibition of Janus kinase 2 and signal transduction
and activator of transcription 3 protect against cecal ligation and
puncture-induced multiple organ damage and mortality. J Trauma.
66:859–865. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Gu XB, Yang XJ, Hua Z, Lu ZH, Zhang B, Zhu
YF, Wu HY, Jiang YM, Chen HK and Pei H: Effect of oxymatrine on
specific cytotoxic T lymphocyte surface programmed death receptor-1
expression in patients with chronic hepatitis B. Chin Med J (Engl).
125:1434–1438. 2012.PubMed/NCBI
|
|
24
|
Fan DL, Zhao WJ, Wang YX, Han SY and Guo
S: Oxymatrine inhibits collagen synthesis in keloid fibroblasts via
inhibition of transforming growth factor-β1/Smad signaling pathway.
Int J Dermatol. 51:463–472. 2012.PubMed/NCBI
|
|
25
|
Liu L, Lu W, Ma Z and Li Z: Oxymatrine
attenuates bleomycin-induced pulmonary fibrosis in mice via the
inhibition of inducible nitric oxide synthase expression and the
TGF-β/Smad signaling pathway. Int J Mol Med. 29:815–822.
2012.PubMed/NCBI
|
|
26
|
Chai NL, Fu Q, Shi H, Cai CH, Wan J, Xu SP
and Wu BY: Oxymatrine liposome attenuates hepatic fibrosis via
targeting hepatic stellate cells. World J Gastroenterol.
18:4199–4206. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zhang MH, Wang XY and Zhang Y: The
preventive and therapeutic effects of oxymatrine on cardiac muscle
injury in rats with septic shock. J Ningxia Med Univ. 32:876–879.
2012.(In Chinese).
|