Introduction
Esophageal carcinoma is the eighth most common
cancer worldwide, responsible for 481,600 new cases in 2008, and
the sixth most common cause of mortality from cancer with 406,500
deaths (1). Geographic variation in
incidence is extremely striking, with China being high-risk and
western Africa being low-risk. In China, ~210,000 patients succumb
to esophageal squamous cell carcinoma (ESCC) per year, accounting
for 52% of the worldwide mortality due to ESCC (1). Although various treatments, such as
surgery with preoperative treatments of radiotherapy, chemotherapy
and hyperthermia, have been used, esophageal carcinoma has the
poorest prognosis among digestive tract malignancies and the 5-year
survival rate of advanced esophageal carcinoma is <25% (2,3). However,
the 5-year survival rate of early esophageal carcinoma can reach
86–100% (4,5). Thus, early detection of ESCC appears to
be the most promising method of improving the 5-year survival.
In recent decades, esophageal Lugol chromoendoscopy
has become a common clinical approach in China, particularly in
high-risk regions. Lugol chromoendoscopy has been demonstrated to
improve endoscopic visualization of squamous dysplasia and
carcinoma of the esophagus in Linxian, a high-risk ESCC region in
the Henan Province in China (6).
However, the diagnostic value of Lugol chromoendoscopy in low-risk
regions is unknown. Beijing is a low-risk ESCC region; the
morbidity (9.2/100,000) and mortality (7.5/100,000) is lower than
the average level in China (19.3/100,000 and 15.4/100,000) and is
similar to the global average level (1,7). Our
previous study demonstrated that Lugol chromoendoscopy elevates the
detection rate of early ESCC/dysplasia in high-risk individuals in
Beijing (8); additionally, patients
with esophageal symptoms, such as reflux, dysphagia, and globus
sensation, were often observed to have esophageal dysplasia or
early esophageal carcinoma. It has been previously reported that
61.9% patients with early stage esophageal carcinoma exhibit
subjective symptoms (9). Therefore,
the aim of the present study was to conduct a prospective study to
evaluate whether Lugol chromoendoscopy improves the detection of
squamous dysplasia/early carcinoma of the esophagus in patients
with esophageal symptoms in Beijing, China.
Materials and methods
Subjects
The study was carried out at the Endoscopic Center
of Beijing Friendship Hospital, Capital Medical University
(Beijing, China). Patients with reflux, dysphagia, and globus
sensation were included consecutively between January 2002 and May
2004, with the exception of the following: i) Patient had thyroid
disease; ii) was hypersensitive to iodine; iii) was pregnant or
lactating; iv) had chronic nephropathy; v) had esophageal varices,
polypus, ulcer, hiatus hernia, diverticulum, and leiomyoma; vi) had
any malignancies including esophageal advanced carcinoma; vii)
lived in Beijing <10-years; or viii) had coagulation
defects.
Patients were randomly divided into routine
endoscopy and chromoendoscopy groups according to odd or even
numbers prior to endoscopy examinations. Patients in the routine
endoscopy group only received routine endoscopy examinations;
patients in the chromoendoscopy group received routine endoscopy
examinations, followed by iodine staining. At recruitment, each
subject was interviewed to collect detailed information with regard
to their history of alcohol and tobacco use. Alcohol use was
defined as over 100 g per week over one year in this study. Light
or heavy tobacco use were categorized by the approximate 50th
percentile pack-years value among patients (as our previous study)
(10); i.e. <25 or 25 pack-years
[(cigarettes per day/20)x(years smoked)]. This study was conducted
in accordance with the declaration of Helsinki. This study was
conducted with approval from the Ethics Committee of Beijing
Friendship Hospital, Capital Medical University. Written informed
consent was obtained from all participants.
Endoscopic procedures
All subjects were given 5 ml of 1% lidocaine for
local anesthesia 2–5 min prior to endoscopy. Endoscopic examination
was performed by an experienced endoscopist using a videoendoscope
(GIF-XQ240; Olympus Optical Co., Ltd, Tokyo, Japan). In the routine
endoscopy group, the entire esophagus and upper gastrointestine was
examined and between one and five biopsies were collected for
pathology from any areas with abnormal lesions (Table I) (7).
In the chromoendoscopy group, following routine endoscopic
examination, the tip of the endoscope was placed in the distal part
of the esophagus and 10 ml of 2.5% Lugol's solution (25 g I+50 g KI
in 1000 ml distilled water; 2.5% weight/weight iodine) was sprayed
onto the esophageal surface from the gastroesophageal junction to
the upper esophageal sphincter using the dye-spraying catheter
(PW-5L-1, Olympus Optical Co., Ltd) through the biopsy channel.
From each unstained or light-stained area of >0.5 cm in
diameter, between one and five biopsies were collected for
pathology. All characteristics, size and location in visually
abnormal areas or unstained areas in the chromoendoscopy group were
described and photographed.
 | Table I.Abnormal lesions of esophagus under
routine endoscopy. |
Table I.
Abnormal lesions of esophagus under
routine endoscopy.
| Abnormal lesions | Characteristics |
|---|
| Irregular | Mucosa was focally or
diffusely irregular, with prominent wrinkling |
| Small white
patch | Focal raised or flat
white patch, with smooth distinct borders, usually <1 cm in
greatest dimension |
| Focal red area | Focal flat red area
not caused by mucosal contact |
| Erosion | Focal defect in the
mucosa, the erosions were subcatergorized as linear, punched-out,
or broad-based, depending on their shape and size |
| Plaque | Mucosa was focally
thickened and raise, with irregular indistinct borders and
occasional shallow surface erosions, usually were >1 cm in
greatest dimension |
Histological examination
The biopsies were fixed in 10% formalin, embedded in
paraffin, cut into 5 µm sections, and examined after staining with
hematoxylin and eosin. An experienced pathologist analyzed the
histology samples. Dysplasia was defined as an atypia of the
epithelium with a basophilic matrix, a high matrix-core ratio, and
a hyperheterochromatin. It was histologically classified into three
grades: Mild (abnormalities confined to the lower one-third of the
epithelium); moderate (abnormalities in the lower two-thirds); and
severe grade (immature cells occupied more than two-thirds of the
epithelium), according to the degree of atypical epithelium in
comparison with the basal zone (11).
Early esophageal carcinoma was defined as a tumor not beyond
mucosal 2 (11,12). When several lesions were observed in a
patient, only the most severe lesion was considered.
Statistical analysis
Numerical data is presented as the mean ± standard
deviation (SD) and categorical data is expressed as percentage.
Difference was evaluated by AVOVA, t-test or χ2
tests. P<0.05 was considered to indicate a statistically
significant difference. All tests were two-sided tests and all
analyses were conducted using Statistical Analysis System Software
(version 6.12, SAS Institute, Cary, NC, USA).
Results
General information
In total, 900 patients were randomized to receive
routine endoscopy (450 patients) and chromoendoscopy (450 patients)
examinations. Due to polypus, ulcer, hiatus hernia, diverticulum,
or leiomyoma, 55 and 33 patients were eliminated in the routine
endoscopy and chromoendoscopy group, respectively. A total of 812
patients who fulfilled the inclusion and exclusion criteria were
enrolled. The baseline characteristics of the 395 patients in the
routine endoscopy group and 417 patients in the chromoendoscopy
group are summarized in Table II.
The patients in the chromoendoscopy group and the control group
were comparable in age, gender, symptoms and smoking and alcohol
status. The mean age was 57.08±12.43 years for the chromoendoscopy
group and 55.66±13.30 years for the control group (P=0.12). The
number of patients >45 years of age for the two groups was
determined, and no significant difference was identified (86.6 vs.
75.2%; P=0.12). Additionally, no significant difference was
identified in gender distribution (P=0.89), smoking and alcohol
status (P=0.53), and symptoms (P=0.27).
 | Table II.Baseline characteristics of
demographic, smoking, alcohol status and symptoms between the
routine endoscopy and chromoendoscopy groups. |
Table II.
Baseline characteristics of
demographic, smoking, alcohol status and symptoms between the
routine endoscopy and chromoendoscopy groups.
|
| Chromoendoscopy
(n=417) | Routine endoscopy
(n=395) |
|
|---|
|
|
|
|
|
|---|
| Variable | n | % | n | % | Pa |
|---|
| Gender |
|
|
|
| 0.89 |
| Male | 243 | 58.3 | 232 | 58.7 |
|
|
Female | 174 | 41.7 | 163 | 41.3 |
|
| Age structure |
|
|
|
| 0.12 |
| ≥45 | 362 | 86.8 | 297 | 75.2 |
|
|
<45 | 55 | 13.2 | 98 | 24.8 |
|
| Smoking status |
|
|
|
| 0.90 |
|
Never | 331 | 79.4 | 315 | 79.7 |
|
| Ever | 86 | 20.6 | 80 | 20.3 |
|
| <25
pack-year | 46 | 53.5 | 36 | 45.0 | 0.27 |
| ≥25
pack-year | 40 | 46.5 | 44 | 55.0 |
|
| Alcohol status |
|
|
|
| 0.53 |
| Yes | 48 | 11.5 | 40 | 10.0 |
|
| No | 369 | 88.5 | 355 | 90.0 |
|
| Symptoms |
|
|
|
| 0.27 |
|
Reflux | 272 | 68.9 | 308 | 73.9 |
|
|
Dysphagia | 54 | 13.7 | 45 | 10.8 |
|
| Globus
sensation | 69 | 17.5 | 64 | 15.3 |
|
Detection of dysplasia/early
carcinoma
A total of 86 patients had dysplasia/early
carcinoma, and the detection rate was 10.6% (86/812). In the
routine endoscopy group, 29 patients (7.3%, 29/395) had
dysplasia/early ESCC. The detection rates of mild, moderate and
severe dysplasia/early ESCC in the routine endoscopy group were
3.3% (13/395), 2.8% (11/395) and 1.3% (5/395), respectively. In the
chromoendoscopy group, 57 (13.7%, 57/417) dysplasia/early carcinoma
patients were identified, among whom, 31 (7.4%, 31/417) patients
exhibited mild dysplasia, 12 (2.9%, 12/417) patients had moderate
dysplasia and 14 (3.4%, 14/417) patients exhibited severe
dysplasia/early ESCC. A significant difference was observed in the
detection rates of dysplasia/early ESCC between the two groups
(χ2=8.58, P=0.003; Table
III). Among the 57 cases of dysplasia/early ESCC in
chromoendoscopy group, 18 cases of esophagitis were revealed
endoscopically; mild, moderate and severe dysplasia were present in
11, 6 and 1 cases, respectively. In the chromoendoscopy group, the
most common appearance of severe dysplasia/early ESCC (64.3%, 9/14)
was rugged or rough surface under routine endoscopy, also showing
irregular unstained areas after staining with Lugol's solution
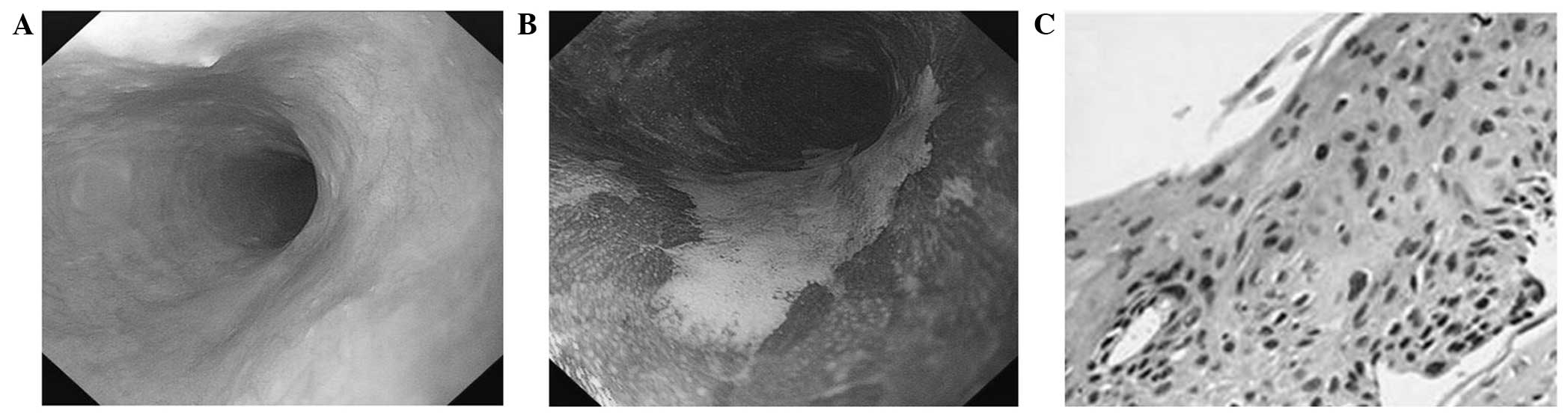
(100%, 14/14; Fig. 1).
 | Table III.Detection rates of mild, moderate and
severe grade dysplasia/early ESCC. |
Table III.
Detection rates of mild, moderate and
severe grade dysplasia/early ESCC.
|
|
|
| Dysplasia/early
carcinoma (%) |
|
|
|---|
|
|
|
|
|
|
|
|---|
| Groups | No | Mild | Moderate | Severe/early
ESCC | Total | Othersa (%) |
|---|
| Chromoendoscopy | 417 | 31 (7.4) | 12 (2.9) | 14 (3.4) | 57 (13.7) | 360 (86.3) |
| Routine
endoscopy | 395 | 13 (3.3) | 11 (2.8) | 5 (1.3) | 29 (7.3) | 366 (92.7) |
| Pb |
| 0.009 | 0.936 | 0.049 | 0.003 |
|
Association between the
dysplasia/early ESCC and esophageal symptoms
Patients were divided into three groups according to
symptoms. Overall, 580 cases had reflux, 99 cases had dysphagia,
and 133 cases had globus sensation. The detection of mild, moderate
and severe grade dysplasia/early ESCC in the three groups was 8.3%
(48/580), 17.2% (17/99), and 16.5% (22/133), respectively (Table IV).
 | Table IV.Association between the detection
rates of dysplasia/early ESCC and esophageal symptoms. |
Table IV.
Association between the detection
rates of dysplasia/early ESCC and esophageal symptoms.
| Histological
findings | Reflux (%) | Dysphagia (%) | Globus sensation
(%) | Total (%) |
|---|
| Dysplasia/early
ESCC | 48 (8.3) | 17 (17.2) | 22 (16.5) | 86 (10.6) |
|
Mild | 28 (4.8) | 7 (0.07) | 10 (7.5) | 44 (5.4) |
|
Moderate | 9 (1.6) | 6 (0.06) | 8 (0.06) | 23 (2.8) |
|
Severe/early ESCC | 11 (1.9) | 4 (0.04) | 4 (0.03) | 19 (2.3) |
| Others | 532 (91.7) | 82 (82.8) | 112 (84.2) | 726 (89.4) |
| Total | 580 (71.4) | 99 (12.2) | 133 (16.4) | 812 |
Association between the detection
rates and the length of unstained lesions (USLs)
USLs were observed in 213 patients (>0.5 cm). The
patients were divided into two groups according to the length of
USLs. If one patient had more than one USL, the largest lesion was
selected to group. In total, 76 cases had USLs of 0.5–1.0 cm in
diameter. Among these cases, 4 patients had dysplasia/early ESCC (4
mild dysplasia cases). USLs of >1.0 cm were observed in 137
seven cases and the number of mild, moderate and severe grade
dysplasia/early ESCC was 27, 10 and 14, respectively. A significant
difference was identified between the two groups
(χ2=21.46, P<0.001; Table
V).
 | Table V.Association between the detection
rates and the length of unstained lesions in chromoendoscopy
group. |
Table V.
Association between the detection
rates and the length of unstained lesions in chromoendoscopy
group.
|
|
| Dysplasia (%) |
|
|---|
|
|
|
|
|
|---|
| Groups | No | Mild | Moderate | Severe/early
carcinoma | Total |
|---|
| 0.5–1.0 cm | 76 | 4 (5.3) | 0 (0) | 0 (0) | 4 (5.3) |
| ≥1.0 cm | 137 | 27 (19.7) | 10 (7.3) | 14 (10.2) | 51 (37.2) |
| P |
| 0.04 | 0.22 | 0.04 | <0.001 |
Discussion
Lugol chromoendoscopy is an important diagnostic
tool and has been widely used to detect esophageal carcinomas or
precancerous lesions as it can make the borders of visible lesions
more clear or reveal lesions that cannot be observed by routine
endoscopy examinations. It was reported that 27% of moderate/severe
dysplasia of the esophagus were not identified in routine endoscopy
examinations (6). In previous
studies, Lugol chromoendoscopy was predominantly used in high-risk
populations or high-risk regions to screen esophageal carcinomas or
precancerous lesions (6,13–15). The
current study screens esophageal dysplasia/early carcinoma in
low-risk regions using Lugol chromoendoscopy to evaluate whether
this technology may improve the detection rates of esophageal
dysplasia/early carcinoma. The results revealed that the detection
rate of dysplasia/early carcinoma in chromoendoscopy group was
markedly higher than that of the routine endoscopy group. The
result suggested that Lugol chromoendoscopy was also important in
low-risk regions for the detection of esophageal dysplasia/early
carcinoma.
In the current study, patients were selected with
esophageal symptoms and 86 (10.6%) patients were observed to have
dysplasia/early carcinoma, among whom 19 (2.3%, 19/812) cases had
severe dysplasia/early carcinoma. The detection rate of severe
dysplasia/early carcinoma almost reached that of the high-risk
population (13–17). In this study, these patients were
divided into three groups according to symptoms, and 8.3% patients
who had reflux, 17.2% patients who had dysphagia, and 15.8%
patients who had globus sensation, were also observed to have
dysplasia/early ESCC. The results indicated that increased
attention must be given to the patients with esophageal symptoms,
and Lugol chromoendoscopy should be recommended as a routine
procedure in patients with esophageal symptoms, similarly to those
high-risk patients with head and neck, or tracheobronchial squamous
cell carcinomas, or had an alcohol or tobacco addiction, or lived
in a high-risk region (13–17).
Previous studies have identified a positive
correlation between USL size and the probability of clinically
significant neoplasia (6,18,19). In
high-risk regions, high grade dysplasia/carcinoma is identified in
31% (46/149) patients with USLs of <1 cm (6). The current study found that only 4
(5.3%) patients with mild dysplasia had USLs of 0.5–1.0 cm, while
51 patients with dysplasia/early ESCC had USLs >1.0 cm,
including 14 cases with severe dysplasia/early ESCC. The results
indicated that the probability of USLs <1.0 cm being severe
dysplasia/early ESCC was low in low-risk regions. As it is
challenging to conduct biopsies for USLs of <0.5 cm, and due to
the current results regarding the correlation between USL size and
the probability of dysplasia/early ESCC, it does not appear that
biopsies are required for USLs of <0.5 cm in diameter.
The Japanese Society for Esophageal Disease defined
superficial esophageal carcinoma as lesions in which infiltration
does not go beyond the submucosal layer, and subclassified these
into the six categories: Mucosal 1, mucosal 2, mucosal 3,
submucosal 1, submucosal 2 and submucosal 3 (20). It has previously been reported that
mucosal 1 and mucosal 2 carcinomas have no lymph node and distal
metastasis (21). In the current
study, we defined early carcinoma as a tumor not beyond submucosal
2. As esophageal severe dysplasia and early ESCC have a similar
treatment and prognosis, these were grouped together.
The current study also found that it is extremely
important to rinse the mucosa prior to staining and it not
necessary to pretreat the mucosa with a mucolytic agent (9). The formula of the iodine solution that
we used was stronger than the Lugol's solution used in other
studies (8,9). This formula ensured that the USLs were
clearly visible for 5–9 min, allowing enough time for photographs
to be recorded and biopsies to be conducted. If the stain did begin
to fade prior to the biopsy, restaining was easily accomplished and
effective.
In total, 20% patients experienced discomfort in
this study. The predominant discomfort was a sensation of
esophageal burning and pain, which appeared to be caused by gastric
distention and/or reflux of iodine, and was minimized by careful
suction of air and iodine from the stomach prior to the removal of
the endoscope.
In conclusion, Lugol chromoendoscopy improves the
detection of dysplasia/early ESCC in patients with esophageal
symptoms in low-risk regions. Lugol chromoendoscopy must therefore
be considered in addition to routine endoscopy in patients with
esophageal symptoms.
Acknowledgements
This study was supported in part by grants from the
Municipal science and technology commission of China (grant no.
Z101100055610031).
References
|
1
|
Ferlay J, Shin HR, Bray F, et al:
Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int
J Cancer. 127:2893–2917. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sant M, Aareleid T, Berrino F, et al:
EUROCARE-3: survival of cancer patients diagnosed 1990–94-results
and commentary. Ann Oncol. 14:v61–v118. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Jemal A, Siegel R, Ward E, Hao Y, Xu J,
Murray T and Thun MJ: Cancer statistics, 2008. CA Cancer J Clin.
58:71–96. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Inoue H and Endo M: Endoscopic esophageal
mucosal resection using a transparent tube. Surg Endosc. 4:189–201.
1990. View Article : Google Scholar
|
|
5
|
Wang LD, Zhou Q and Yang CS: Esophageal
and gastric cardia epithelial cell proliferation in northern
Chinese subjects living in a high-incidence area. J Cell Biochem
Suppl. 28–29:159–165. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Dawsey SM, Fleischer DE, Wang GQ, et al:
Mucosal iodine staining improves endoscopic visualization of
squamous dysplasia and squamous cell carcinoma of the esophagus in
Linxian, China. Cancer. 83:220–231. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhang SW, Zhang M, Li GL, et al: An
analysis of incidence and mortality of esophageal cancer in China,
2003–2007. China Cancer. 21:241–244. 2012.
|
|
8
|
Shao Y, Ji M, Wu YD, et al: The clinical
study of detection of dysplasia and early esophageal squamous cell
carcinoma (ESCC) by using 2.5% lugol chromoendoscopy. J Clin Intern
Med. 23:534–536. 2006.
|
|
9
|
Sugimachi K, Ohno S, Matsuda H, Mori M,
Matsuoka H and Kuwano H: Clinicopathologic study of early stage
esophageal carcinoma. Br J Surg. 76:759–763. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shao Y, Tan W and Zhang S: P53 gene codon
72 polymorphism and risk of esophageal squamous cell carcinoma: a
case-control study in a Chinese population. Dis Esophagus.
21:139–143. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dawsey SM, Lewin KJ, Liu FS, Wang GQ and
Shen Q: Esophageal morphology from Linxian, China: squamous
histologic findings in 754 patients. Cancer. 73:2027–2037. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kodama M and Kakegawa T: Treatment of
superficial cancer of the esophagus: a summary of responses to a
questionnaire on superficial cancer of the esophagus in Japan.
Surgery. 123:432–439. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kaneko K, Murakami Y, Katagiri A, et al:
Does daily alcohol and/or cigarette consumption cause low-grade
dysplasia, a precursor of esophageal squamous cell carcinoma? J
Clin Gastroenterol. 44:173–179. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Boller D, Spieler P, Schoenegg R, et al:
Lugol chromoendoscopy combined with brush cytology in patients at
risk for esophageal squamous cell carcinoma. Surg Endosc.
23:2748–2754. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Dubuc J, Legoux J, Winnock M, et al:
Endoscopic screening for esophageal squamous-cell carcinoma in
high-risk patients: a prospective study conducted in 62 french
endoscopy centers. Endoscopy. 38:690–695. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Fukuhara T, Hiyama T, Tanaka S, et al:
Characteristics of esophageal squamous cell carcinomas and
lugol-voiding lesions in patients with head and neck squamous cell
carcinoma. J Clin Gastroenterol. 44:e27–e33. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Fagundes RB, de Barros SG, Pütten AC, et
al: Occult dysplasia is disclosed by Lugol chromoendoscopy in
alcoholics at high risk for squamous cell carcinoma of the
esophagus. Endoscopy. 31:281–285. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Dawsey SM, Wang GQ, Weinstein WM, et al:
Squamous dysplasia and early esophageal cancer in the Linxian
region of China: distinctive endoscopic lesions. Gastroenterology.
105:1333–1340. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hori K, Okada H, Kawahara Y, Takenaka R,
Shimizu S, et al: Lugol-voiding lesions are an important risk
factor for a second primary squamous cell carcinoma in patients
with esosphageal cancer or head and neck cancer. Am J
Gastroenterol. 106:858–866. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Comprehensive Registry of Esophageal
Cancer in Japan (1998,1999) & Long Term Results of
Esophagectomy in Japan (1988–1997). 3rd. Japanese Society for
Esophageal Disease; 2002
|
|
21
|
Tachibana M, Yoshimura H, Kinugasa S, et
al: Clinicopathological features of superficial squamous cell
carcinoma of the esophagus. Am J Surg. 174:49–53. 1997. View Article : Google Scholar : PubMed/NCBI
|