Introduction
The risk of esophageal cancer is reported to be
strongly associated with alcohol flushing and drinking, which is
associated with inactive aldehyde dehydrogenase-2, smoking and
dietary habits (1–3). These risk factors are well known and
screening via endoscopy is extremely useful for the detection of
esophageal cancer in high-risk groups. Esophageal cancer has a poor
prognosis if advanced cancer is diagnosed, but the prognosis of
patients with superficial esophageal cancer is acceptable. The
5-year survival rate has been reported to be 80.7% for stage I
patients and 8.5% for stage IV patients (4).
As an initial treatment, curative endoscopic
resection (ER) may be selected if the esophageal cancer is
superficial, which is associated with extremely low risk
complications, while radical surgery or definitive
chemoradiotherapy (CRT) is used in advanced esophageal cancer cases
to achieve a cure. Due to the high rate of surgical complications,
CRT or radiotherapy (RT) is often used for esophageal cancer as a
non-surgical treatment option (5,6). Previous
studies have demonstrated that definitive CRT for esophageal cancer
is associated with a high response and survival rate (7–9), although
local failure following CRT or RT remains a major challenge in
achieving a cure. A standard treatment strategy for local failure
following CRT or RT has not yet been determined, although a salvage
esophagectomy is generally indicated for these cases. However, due
to the technical challenge of radical surgery and the high rate of
complications, salvage surgery has not yet been accepted as a
standard treatment strategy for local failure. For local disease
control, salvage ER may be utilized if the depth of invasion is
limited to the mucosa or submucosa. Salvage ER is associated with a
low risk of complications and may be used to achieve a cure if
recurrences are local and superficial (10). The present authors have performed ER
for such locoregional lesions and metachronous lesions appearing
following CRT or RT. The present study reviewed the
clinicopathological records and follow-up data for 37 patients that
underwent salvage ER following CRT or RT for esophageal cancer to
identify the outcome of these patients.
Patients and methods
Patients
Between January 2001 and December 2012, 37 patients
with esophageal cancer (total of 78 lesions) underwent salvage
endoscopic treatment for recurrences or residual/metachronous
lesions following definitive CRT or RT at the Department of
Surgery, Keio University Hospital (Tokyo, Japan). The
clinicopathological records of these patients, including
pretreatment diagnoses, methods used for initial therapy,
pre-salvage endoscopic treatment diagnoses, methods used for
endoscopic treatment, complications, histological features of
resected specimens and outcomes, were examined by the present
study.
Results
Clinicopathological diagnoses and
initial treatment methods
The histopathological features of the patients are
presented in Table I. The stage
distribution of the patients was as follows, according to the
tumor-node-metastasis (TNM) classification defined by the UICC
(11): Stage I, 28 patients (75.6%);
stage II, 2 patients (5.4%); stage III, 4 patients (10.8%); and
stage IV, 3 patients (8.1%). The depth of tumor invasion of the
patients was as follows, according to diagnosis by endoscopy and
fluoroscopy: Epithelial (EP)/lamina propria (LPM), 9 patients
(24.3%); muscularis mucosa (MM)/submucosal (SM) 1, 7 patients
(18.9%); SM2/SM, 8 patients (21.6%); and muscularis propria
(MP)/deeper than MP, 8 patients (21.6%). Table II reveals the initial methods of
treatment of the patients; 27 patients (72.9%) underwent CRT and 10
patients (27.0%) underwent RT. Overall, 22 patients (59.4%)
exhibited a complete response (CR) and 15 patients (40.5%)
exhibited a partial response.
 | Table I.Histopathological characteristics of
37 patients with esophageal cancer. |
Table I.
Histopathological characteristics of
37 patients with esophageal cancer.
| Characteristics | Value |
|---|
| Total, n (%) | 37
(100.0) |
| Gender, n (%) |
|
| Male | 36 (97.3) |
|
Female | 1 (2.7) |
| Age, years |
|
|
Median | 71.5 |
|
Range | 53–85 |
| TNM stage, n (%) |
|
| I | 28 (75.7) |
| II | 2 (5.4) |
| III | 4
(10.8) |
| IV | 3 (8.1) |
| Depth of tumor
invasion, n (%) |
|
| EP | 3 (8.1) |
| LPM | 6
(16.2) |
| MM | 5
(13.5) |
| SM1 | 2 (5.4) |
| SM2 | 3 (8.1) |
| SM3 | 5
(13.5) |
| SM | 5
(13.5) |
| MP | 1 (2.7) |
| AD | 3 (8.1) |
| AI | 4
(10.8) |
| Initial treatment
method, n (%) |
|
| CRT | 27 (73.0) |
| RT | 10 (27.0) |
| Effect of initial
treatment, n (%) |
|
| CR | 22 (59.5) |
| PR | 15 (40.5) |
 | Table II.Final pathological findings of all
locoregional lesions that underwent ER, including depth of
invasion. |
Table II.
Final pathological findings of all
locoregional lesions that underwent ER, including depth of
invasion.
| A, Endoscopic
therapy |
|---|
|
|---|
| Method | Lesions, n (%) |
|---|
| Total | 78
(100.0) |
| EMR/ESD | 67 (85.9) |
| APC | 11 (14.1) |
|
| B, Tumor
invasion |
|
| Characteristic | Lesions, n (%) |
|
| Total | 67
(100.0) |
| Diagnosis |
|
|
Dysplasia | 6 (8.9) |
| EP | 26 (38.8) |
| LPM | 17 (25.3) |
| MM | 5 (7.4) |
| SM1 | 6 (8.9) |
|
SM2 | 5 (7.4) |
|
SM3 | 1 (1.4) |
| SM | 1 (1.4) |
|
Lymphatic/vascular
invasion | 2 (2.9) |
| Positive
margin | 15 (22.3) |
| Lateral
(+) | 13 (19.4) |
|
Vertical (+) | 2 (2.9) |
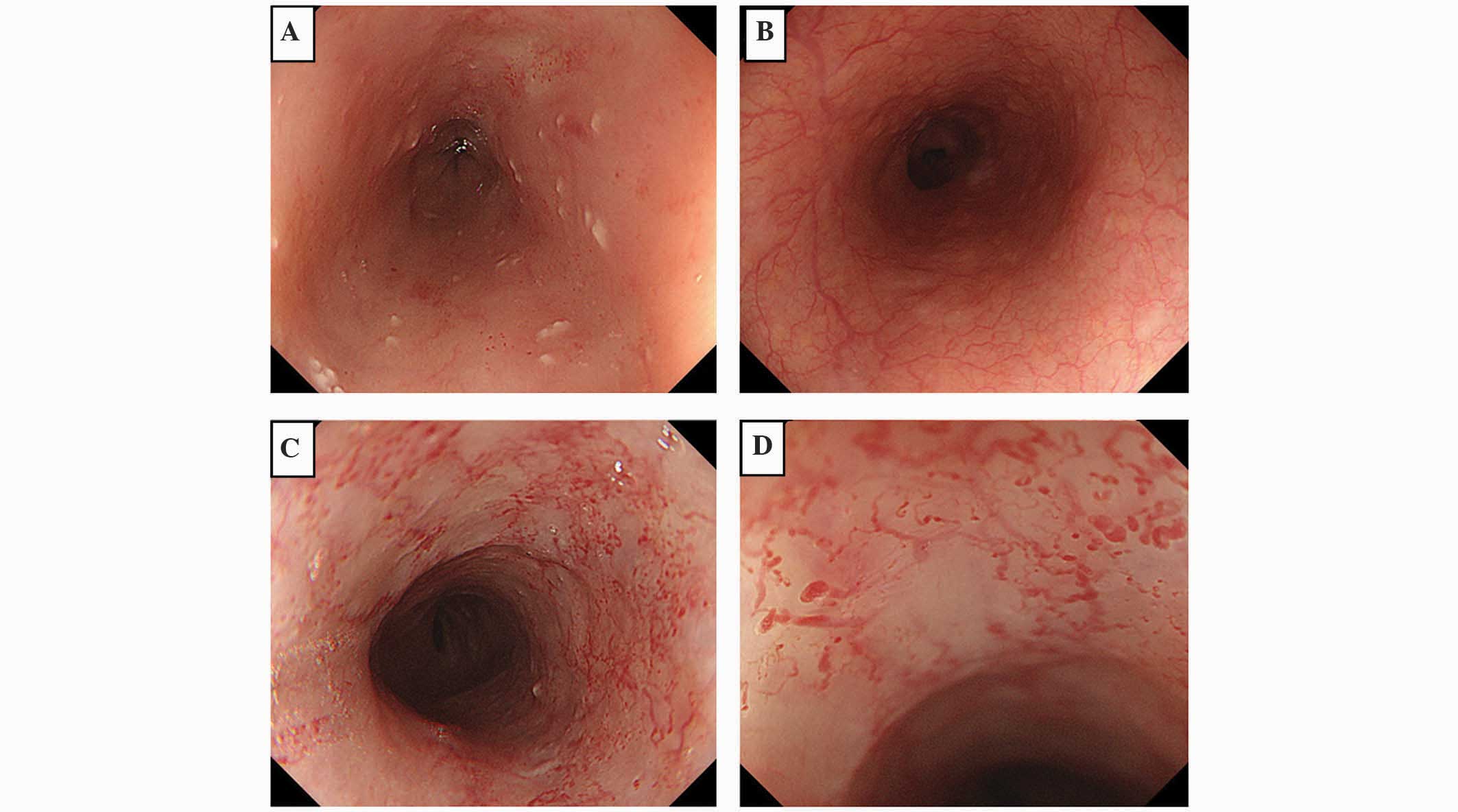
Characteristics of locoregional
failure or recurrence
The esophageal mucosa following CRT or RT is often
characterized by a thick epithelium and the disappearance of normal
superficial vessels in the mucosa (Fig.
1A) compared with normal esophageal mucosa (Fig. 1B). Radiation esophagitis causes the
appearance of abnormal vessels in the esophageal mucosa (Fig. 1C and D) and renders the detection of
cancer lesions, using white light imaging or narrow band imaging
(NBI), relatively challenging. In the present study, almost all the
lesions were detected using iodine staining, and the most important
characteristic was the speed of tumor growth following the first
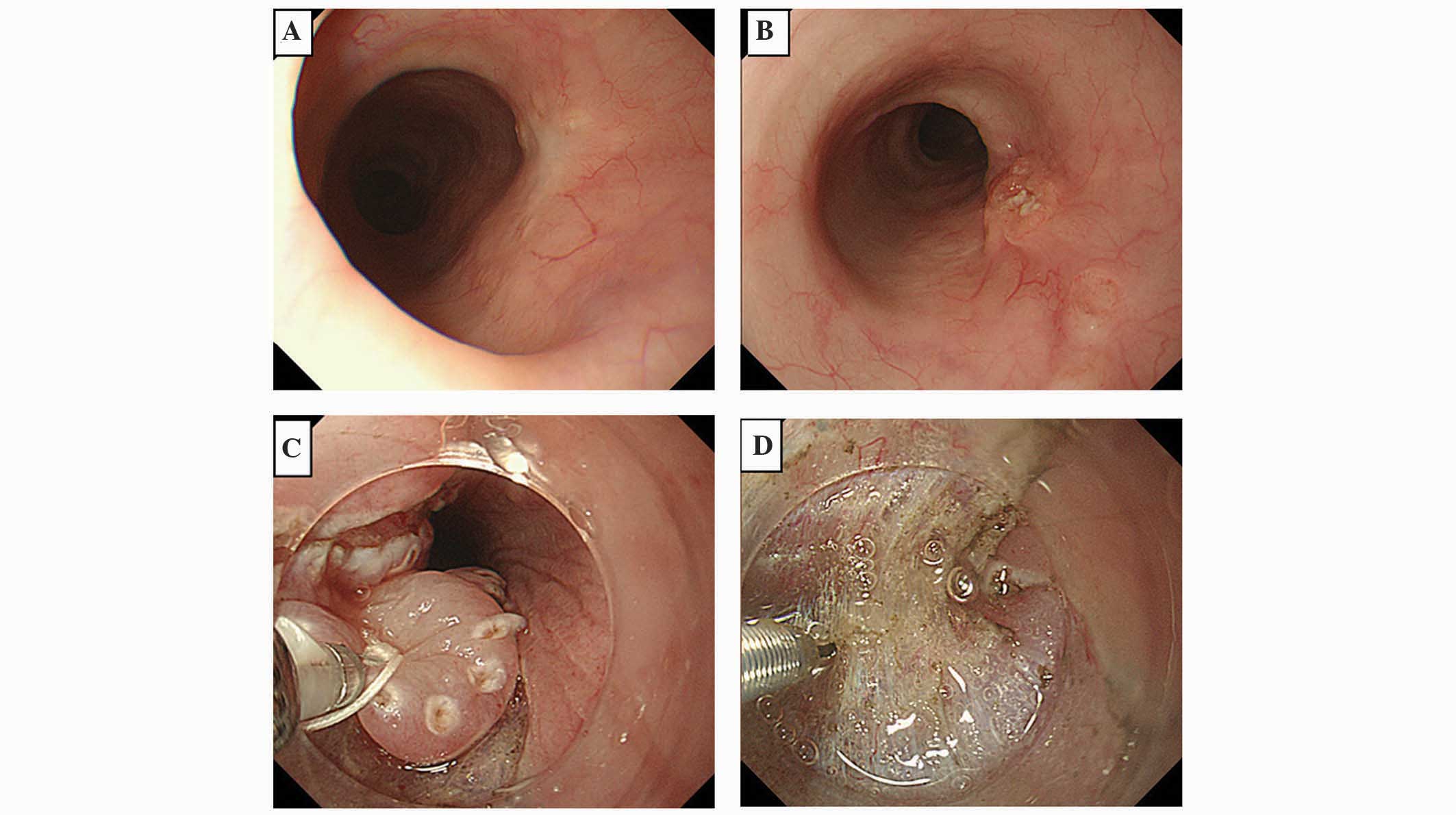
detection of cancer lesions, which was evaluated by endoscopy. If
lesions that could not be confirmed as cancer were detected, a
re-examination was performed within a relatively short period (2–3
months later) (Fig. 2A and B).
Methods of treatment for locoregional
failure or recurrence following CRT or RT
A total of 78 lesions were detected and treated in
the 37 patients following CRT or RT. Endoscopic mucosal resection
(EMR) or endoscopic submucosal dissection (ESD) was performed for
67 lesions (85.8%), and argon plasma coagulation was performed for
11 lesions (14.1%) (Table IIA). No
serious complications occurred post-treatment.
Challenges associated with endoscopic
therapy for locoregional failure or recurrence
Severe fibrous alterations of the submucosa may
render the resection of the submucosa challenging and may increase
the risk of perforation during ER in numerous cases (10). Furthermore, the total thickness due to
radiation or ablation therapy may mean the cancer lesion is not
detected definitively; therefore, residual cancer may occasionally
recur and invade to a deeper layer (10). Consequently, the ESD technique
requires a high level of endoscopic proficiency. Fig. 2C and D reveals treatment with ESD for
a locoregional failure lesion following CRT for esophageal and
hypopharyngeal duplication cancer. In this patient, the esophageal
lesion exhibited a high-grade of CRT-induced fibrosis, making it
challenging to detect the submucosal layer. To overcome this
difficulty, the use of a ‘clip with line’ device developed by Oyama
(11) simplified the dissection of
the submucosa by providing a counter-traction for the cutting
layer. This device not only improves the safety of the submucosa
dissection, but also shortens the time required to perform the
submucosal dissection during ESD.
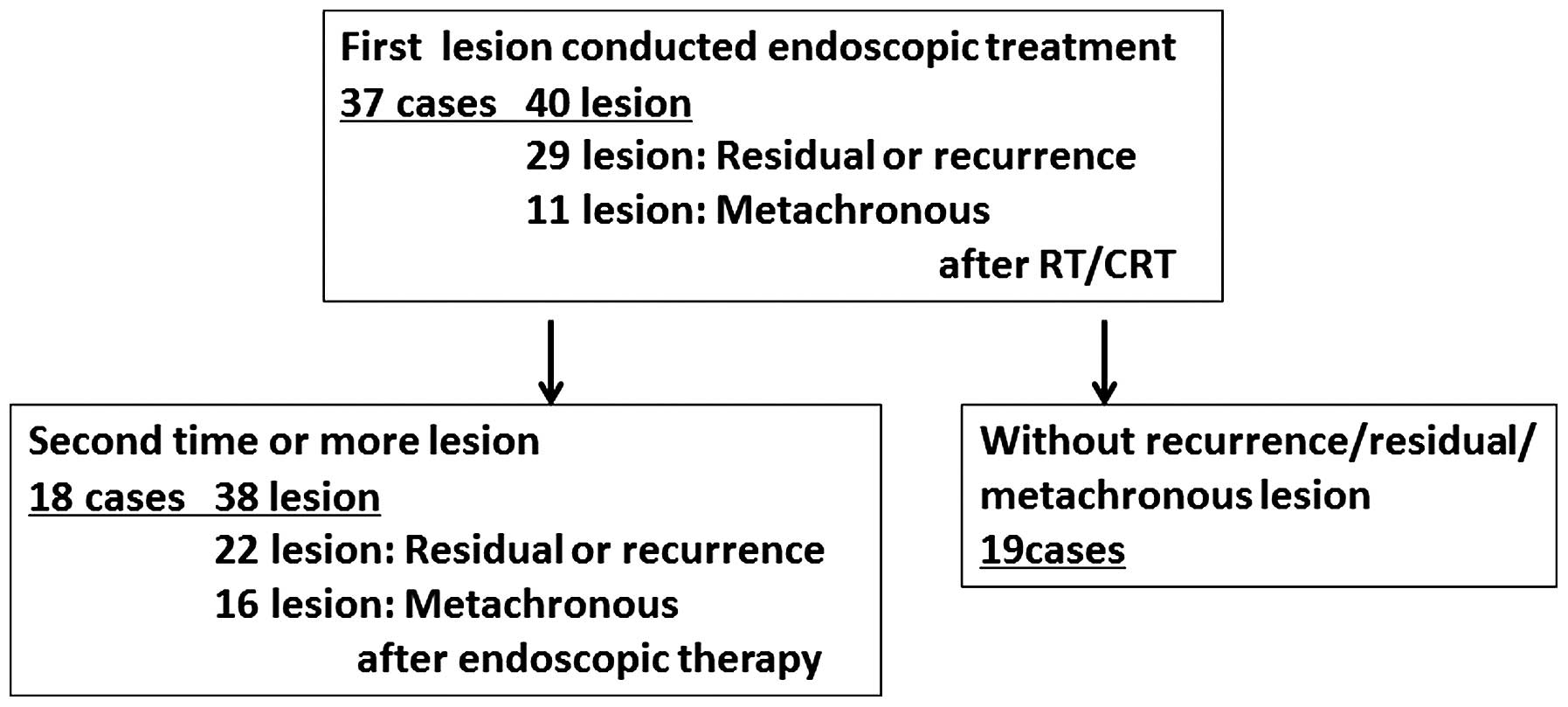
Treatment courses for locoregional
lesions following CRT and RT
Fig. 3 shows the
treatment courses administered to patients for locoregional lesions
following CRT/RT. Initial salvage ER was conducted for 40 lesions
in 37 patients; 29 of these lesions were residual or recurrent
lesions, and 11 were metachronous. Second-line or greater ER was
conducted for 38 lesions occurring following initial ER in 18
patients; 22 of these lesions were residual or recurrent lesions
and 16 were metachronous. In total, 19 patients did not develop
recurrent, residual or metachronous lesions after initial salvage
ER during the follow-up period.
Pathological diagnoses of ER-conducted
specimens
Table IIB shows the
pathological findings for all the locoregional lesions that were
treated with ER, including the depth of invasion. A total of 49
lesions (62.8%) were confirmed to exhibit dysplasia or EP/LPM, 11
lesions (14.1%) were confirmed as MM/SM1, and 7 lesions (8.9%) were
confirmed as SM2/SM3 or SM, according to the TNM staging
classification (12). The majority of
the lesions were T1a (mucosal lesion, early cancer of esophagus),
and ER was a useful method for achieving a cure in patients with
these lesions.
Patient outcomes following salvage
ER
Table III shows the
patient outcomes of 37 salvage ER cases. In total, 16 patients
(43.2%) were alive at the last follow-up and 11 patients survived
for ≥5 years. Only 4 patients succumbed to esophageal cancer, while
9 patients succumbed to other causes. Among the 4 patients that
succumbed to esophageal cancer, the pretreatment diagnoses prior to
CRT or RT were T1b for 3 patients and T3 for 1 patient, while the
tumor depths at ER were 2 EP, 1 SM1 and 1 SM2. A total of 8
patients were lost to follow-up.
 | Table III.Outcomes of 37 patients that
underwent salvage endoscopic resection. |
Table III.
Outcomes of 37 patients that
underwent salvage endoscopic resection.
| Outcome | n (%) |
|---|
| Total | 37
(100.0) |
| Alive | 16 (43.2) |
| ≥5
years | 11 (29.7) |
| <5
years | 5
(13.5) |
| Succumbed | 13 (35.1) |
|
Esophageal cancer | 4
(10.8) |
| Other
disease | 9
(24.3) |
| Lost to
follow-up | 8
(21.6) |
Discussion
Esophageal cancer has a good prognosis if the
disease is detected as a superficial lesion that may be treated
with ER and has an EP or LPM depth of invasion. However,
chemotherapy is recommended for local advanced lesions or patients
with regional lymph node or distant metastases, since this type of
disease is known to be aggressive (13). Patients with unresectable advanced
cancer that have never been referred for surgical resection, have
refused surgery or have characteristics that make them ineligible
for surgery, including poor performance status, are candidates for
definitive CRT or RT. However, the frequency of a pathological CR
to CRT ranges between 30 and 62% (7–9,14,15), and
the majority of recurrences reportedly occur within the radiation
field when examined either retrospectively or prospectively
(16–18). Additionally, esophageal cancer often
occurs as metachronous or multiple cancers (19). At the Keio University Hospital,
regular endoscopic examinations are performed to detect not only
recurrent lesions following RT or CRT, but also novel superficial
cancer lesions in radiation fields. As discussed, in the majority
of CRT or RT cases, normal regular vessels are not visible through
the mucosa and cancer lesions cannot be detected as brown areas
using NBI. However, iodine dyeing is extremely useful for detecting
lesions; therefore, it should be included in regular examinations
of patients that have undergone CRT or RT. In cases where
superficial lesions are detected and no distant metastases are
apparent, ER treatment appears to be a useful method for obtaining
local control.
Salvage esophagectomy is one option for the
treatment of local recurrence or locoregional lesions, although a
salvage esophagectomy following CRT reportedly has a high risk of
complications, a high mortality rate and there is an increased
challenge of treatment for recurrences following salvage surgery
(20,21). Regarding complications, the incidence
of conduit necrosis has been reported to be as high as 25%
following salvage esophagectomy (22,23), and
the creation of an anastomosis within the radiated field in the
chest has been demonstrated to result in a higher than acceptable
leakage rate (24). Regarding patient
outcome, previous studies have reported long-term survival rates of
50% at 3 years and 30–35% at 5 years (25,26)
following salvage esophagectomy.
By contrast, the major complications of salvage
endoscopic treatments are bleeding and perforation, and the
majority of those complications are treated by endoscopy or careful
observation with conservative follow-up care. No severe
complications were experienced in the present patient series, and
none of the patients required surgery due to a complication or
succumbed to a complication. However, the mucosa exhibits severe
scarring following RT or CRT, making it challenging to identify the
submucosal layer and to cut the appropriate layer when performing
an ER. Thus, this strategy requires a high level of technical
proficiency and should only be performed by experienced surgeons,
and careful follow-up is required.
According to the present results, among the 37
patients that underwent endoscopic treatment, the pretreatment
diagnoses indicated that 75% of the patients were classified as
stage I and 78% were estimated to have a T1 depth of SM tumor
invasion. Pathologically, 80% of the resected specimens
demonstrated EP to SM1 invasion. Salvage ER was well suited to the
pretreatment diagnoses of T1 esophageal cancer, while 22% of the
T2-T4 patients were able to undergo endoscopic treatment following
tumor reduction by CRT or RT in cases where the tumor invasion of
the final resected specimen proved to be T1 invasion.
At Keio University Hospital, CRT is conducted for
patients that cannot undergo or have refused surgery. The aim is to
avoid surgery as much as possible if recurrent, residual or
metachronous lesions are detected following CRT. Salvage endoscopic
treatment is conducted only in cases where local control is thought
to be probable; thus, cases with distant metastases or lesions that
have invaded deeper than the submucosal layer are not candidates
for salvage ER. Regardless of the pathological results, typical
follow-up care includes endoscopic and computed tomography
examinations to confirm the absence of local lesions and distant
metastases.
In addition, 48% of patients required second-line or
additional endoscopic treatment following salvage ER of the first
lesion; therefore, the regular examination for the early detection
of cancer lesions and the early ER of these types of lesions is
essential. Regardless of whether recurrent or metachronous cancer
is present, early detection is the most important factor for good
patient outcome.
Certain cases in the current patient series had
laryngopharyngeal cancer in addition to esophageal cancer; 3 of
these patients were diagnosed prior to CRT or RT for esophageal
cancer, 4 patients were diagnosed at the same time as CRT or RT and
6 patients were diagnosed following CRT or RT. In addition, 6
patients were diagnosed with gastric cancer. Such high-risk cases
often do not undergo surgery for esophageal cancer, and the
esophageal cancer lesions do not necessarily affect the outcome of
these patients. Similarly, surgery may not be performed in elderly
patients, and the median age of the patients in this study was
>70 years old. Therefore, salvage ER is well suited to cases
with two or more cancers and elderly patients in whom surgery may
not be well tolerated. In the present study, only 4 patients
(10.8%) succumbed to esophageal cancer and 11 patients (29.7%)
survived for ≥5 years following their first endoscopic treatment.
These results are thought to be acceptable for salvage treatment
following the presence of recurrent or metachronous lesions.
Certain authors have reported excellent long-term
survival without severe complications following salvage endoscopic
treatment subsequent to CRT; 5-year survival rates following
salvage endoscopic treatment have been reported as 36–49% (10,27). In
the present study, no severe complications occurred following
salvage endoscopic treatment, and only 4 patients succumbed to
esophageal cancer, while 11 patients (29.7%) survived for ≥5 years.
While salvage ER requires a high quality of diagnostic capability
and advanced techniques, it should be considered as a treatment
option for esophageal cancer to achieve a cure without surgery.
The present results demonstrated that salvage ER is
an excellent strategy for obtaining long-term survival following
local recurrence or metachronous lesions subsequent to CRT or RT
for esophageal cancer. This technique may be used to excise the
lesions completely, has a low risk of complications and is less
stressful for patients, compared with salvage surgery. This
strategy is well suited for patients whose treatment strategy may
be uncertain, including patients with two or more cancers, a
history of surgery or elderly patients. The present results were
acceptable in terms of curability, patients' quality of life and
patient outcome.
Glossary
Abbreviations
Abbreviations:
|
RT
|
radiotherapy
|
|
CRT
|
chemoradiotherapy
|
|
ER
|
endoscopic resection
|
|
NBI
|
narrow band imaging
|
|
EMR
|
endoscopic mucosal resection
|
|
ESD
|
endoscopic submucosal dissection
|
|
APC
|
argon plasma coagulation
|
|
CR
|
complete response
|
|
PR
|
partial response
|
References
|
1
|
Cui R, Kamatani Y, Takahashi A, Usami M,
Hosono N, Kawaguchi T, Tsunoda T, Kamatani N, Kubo M, Nakamura Y
and Matsuda K: Functional variants in ADH1B and ALDH2 coupled with
alchol and smoking synergistically enhance esophageal cancer risk.
Gastroenterology. 137:1768–1775. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Yokoyama T, Yokoyama A, Kato H, Tsujinaka
T, Muto M, Omori T, Haneda T, Kumagai Y, Igaki H, Yokoyama M, et
al: Alcohol flushing, alcohol and aldehyde dehydrogenase genotypes,
and risk for esophageal squamous cell carcinoma in Japanese men.
Cancer Epidemiol Biomarkers Prev. 12:1227–1233. 2003.PubMed/NCBI
|
|
3
|
Mitsumori T, Matsusaka T, Wakasugi K,
Takenaka M, Kume K, Fujinaga Y, Teraoka H and Iwashita A: A
clinicopathological study of gastric cancer with special reference
to age of the patients: An analysis of 1,630 cases. World J Surg.
13:225–230; discussion 230–231. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Japanese Society of Esophageal Diseases:
Comprehensive registry of esophageal cancer in Japan, 1999.
Esophagus. 2:43–69. 2005. View Article : Google Scholar
|
|
5
|
Ohtsu A: Chemoradiotherapy for esophageal
cancer: Current status and perspectives. Int J Clin Oncol.
9:444–450. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ajani J, Bekaii-Saab T, D'Amico TA, Fuchs
C, Gibson MK, Goldberg M, Hayman JA, Ilson DH, Javle M, Kelley S,
et al: Esophageal Cancer Clinical Practice Guidelines. J Natl Compr
Canc Netw. 4:328–347. 2006.PubMed/NCBI
|
|
7
|
Ishihara R, Yamamoto S, Lishi H, Takeuchi
Y, Sugimoto N, Higashino K, Uedo N, Tatsuta M, Yano M, Imai A and
Nishiyama K: Factors predictive of tumor recurrence and survival
after initial complete response of esophageal squamous cell
carcinoma to definitive chemoradiotherapy. Int J Radiat Oncol Biol
Phys. 76:123–129. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kato K, Muto K, Minashi K, Ohtsu A,
Ishikura S, Boku N, Takiuchi H, Komatsu Y, Miyata Y and Fukuda H:
Gastrointestinal Oncology Study Group of the Japan Clinical
Oncology Group (JCOG): Phase II study of chemoradiotherapy with
5-fluorouracil and cisplatin for stage II–III esophageal squamous
cell carcinoma: JCOG trial (JCOG 9906). Int Radiat Oncol Biol Phys.
81:684–690. 2011. View Article : Google Scholar
|
|
9
|
Suzuki A, Xiao L, Hayashi Y, Blum MA,
Welsh JW, Lin SH, Lee JH, Bhutani MS, Weston B, Maru DM, et al:
Nomograms for prognostication of outcome in patients with
esophageal and gastroesophageal carcinoma undergoing definitive
chemoradiotherapy. Oncology. 82:108–113. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yano T, Muto M, Hattori S, Minashi K,
Onozawa M, Nihei K, Ishikura S, Ohtsu A and Yoshida S: Long-term
results of salvage endoscopic mucosal resection in patients with
local failure after definitive chemoradiotherapy for esophageal
squamous cell carcinoma. Endoscopy. 40:717–721. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Oyama T: Counter traction makes endoscopic
submucosal dissection easier. Clin Endosc. 45:375–378. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Edge SB, Byrd DR, Compton CC, Fritz AG and
Greene FL: AJCC Cancer Staging Manual (7th). Springer-Verlag. New
York, NY: 2010.
|
|
13
|
Kato H and Nakajima M: Treatments for
esophageal cancer: A review. Gen Thorac Cardiovasc Surg.
61:330–335. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Michel P, Adenis A, Di Fiore F, Boucher E,
Galais MP, Dahan L, Mirabel X, Hamidou H, Raoul JL, Jacob JH, et
al: Induction cisplatin-irinotecan followed by concurrent
cisplatin-irrinotecan and radiotherapy without surgery in
oesophageal cancer: Multicenter phase II FFCD trial. Br J Cancer.
95:705–709. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Conroy T, Yataghène Y, Etienne PL, Michel
P, Senellart H, Raoul JL, Mineur L, Rives M, Mirabel X, Lamezec B,
et al: Phase II randomised trial of chemoradiotherapy with FOLFOX4
or cisplatin plus fluorouracil in oesophageal cancer. Br J Cancer.
103:1349–1355. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Minsky BD, Pajak TF, Ginsberg RJ, Pisansky
TM, Martenson J, Komaki R, Okawara G, Rosenthal SA and Kelsen DP:
INT 0123 (Radiation Therapy Oncology Group 94-05) Phase III trial
of combined-modality therapy for esophageal cancer: High-dose
versus standard-dose radiation therapy. J Clin Oncol. 20:1167–1174.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Crosby TD, Brewster AE, Borley A, Perschky
L, Kehagioglou P, Court J and Maughan TS: Definitive chemoradiation
in patients with inoperable oesophageal carcinoma. Br J Cancer.
90:70–75. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Welsh J, Settle SH, Amini A, Xiao L,
Suzuki A, Hayashi Y, Hofstetter W, Komaki R, Liao Z and Ajani JA:
Failure patterns in patients with esophageal cancer treated with
definite chemoradiation. Cancer. 118:2632–2640. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kudou M, Shiozaki A, Fujiwara H, Kosuga T,
Konishi H, Morimura R, Murayama Y, Komatsu S, Kuriu Y, Ikoma H, et
al: Clinical analysis of esophageal cancer patients with a history
of metachronous primary cancer. Gan To Kagaku Ryoho. 41:2030–2032.
2014.PubMed/NCBI
|
|
20
|
Swisher SG, Wynn P, Putnam JB, Mosheim MB,
Correa AM, Komaki RR, Ajani JA, Smythe WR, Vaporciyan AA, Roth JA
and Walsh GL: Salvage esophagectomy for recurrent tumors after
definitive chemotherapy and radiotherapy. J Thorac Cardiovasc Surg.
123:175–183. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Meunier B, Raoul J, Le Prisé E, Lakéhal M
and Launois B: Salvage esophagectomy agter unsuccessful curative
chemoradiotherapy for squamous cell cancer of the esophagus. Dig
Surg. 15:224–226. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Nakamura T, Hayashi K, Ota M, Eguchi R,
Ide H, Takasaki K and Mitsuhashi N: Salvage esophagectomy after
definitive chemotherapy and radiotherapy for advanced esophageal
cancer. Am J Surg. 188:261–266. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Amimi A, Ajani J, Komaki R, Allen PK,
Minsky BD, Blum M, Xiao L, Suzuki A, Hofstetter W, Swisher S, et
al: Factors associated with local-regional failure after definitive
chemoradiation for locally advanced esophageal cancer. Ann Surg
Oncol. 21:306–314. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Juloori A, Tucker SL, Komaki R, Liao Z,
Correa AM, Swisher SG, Hofstetter WL and Lin SH: Influence of
preoperative radiation field on postoperative leak rates in
esophageal cancer patients after trimodality therapy. J Thorac
Oncol. 9:534–540. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Gardner-Thorpe J, Hadwick RH and
Dwerryhous SJ: Salvage esophagectomy after local failure of
definitive chemoradiotherapy. Br J Surg. 94:1059–1066. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
D'Journo XB, Michelet P, Dahan L, Doddoli
C, Seitz JF, Giudicelli R, Fuentes PA and Thomas PA: Indications
and outcome of salvage surgery for esophageal cancer. Eur J
Cardiothrorac Surg. 33:1117–1123. 2008. View Article : Google Scholar
|
|
27
|
Yano T, Muto M, Minashi K, Onozawa M,
Nihei K, Ishikura S, Kaneko K and Ohtsu A: Long-term results of
salvage photodynamic therapy for patients with local failure after
chemoradiotherapy for esophageal squamous cell carcinoma.
Endoscopy. 43:657–663. 2011. View Article : Google Scholar : PubMed/NCBI
|