Introduction
Over the past few years, the five-year survival rate
of patients with osteosarcoma has remarkably improved with the
widespread use of neoadjuvant chemotherapy, and limb salvage
surgery is now the mainstay in the treatment of this malignancy
(1–3).
Currently, several options are available for limb reconstruction
following the resection of malignant tumors, including tumor
prostheses, allografts, and vascularized, autologous osseous
grafts. However, reconstruction of large tibial bone defects
resulting from the resection of osteosarcomas remains challenging
(4–6).
Bone transport distraction osteogenesis is widely used in the
reconstruction of large bone defects following trauma, but its use
has rarely been reported in defects resulting from the removal of
bone tumors (7). This is primarily
due to concerns regarding the possible detrimental effects of
chemotherapy administered for osteosarcoma on bone transport
osteogenesis and bone union.
The current case report presents two cases in which
the bone transport technique was successfully used for the
reconstruction of large tibial bone defects caused by the resection
of osteosarcomas. Written informed consent was obtained from each
patient for publication of this study.
Case report
Case 1
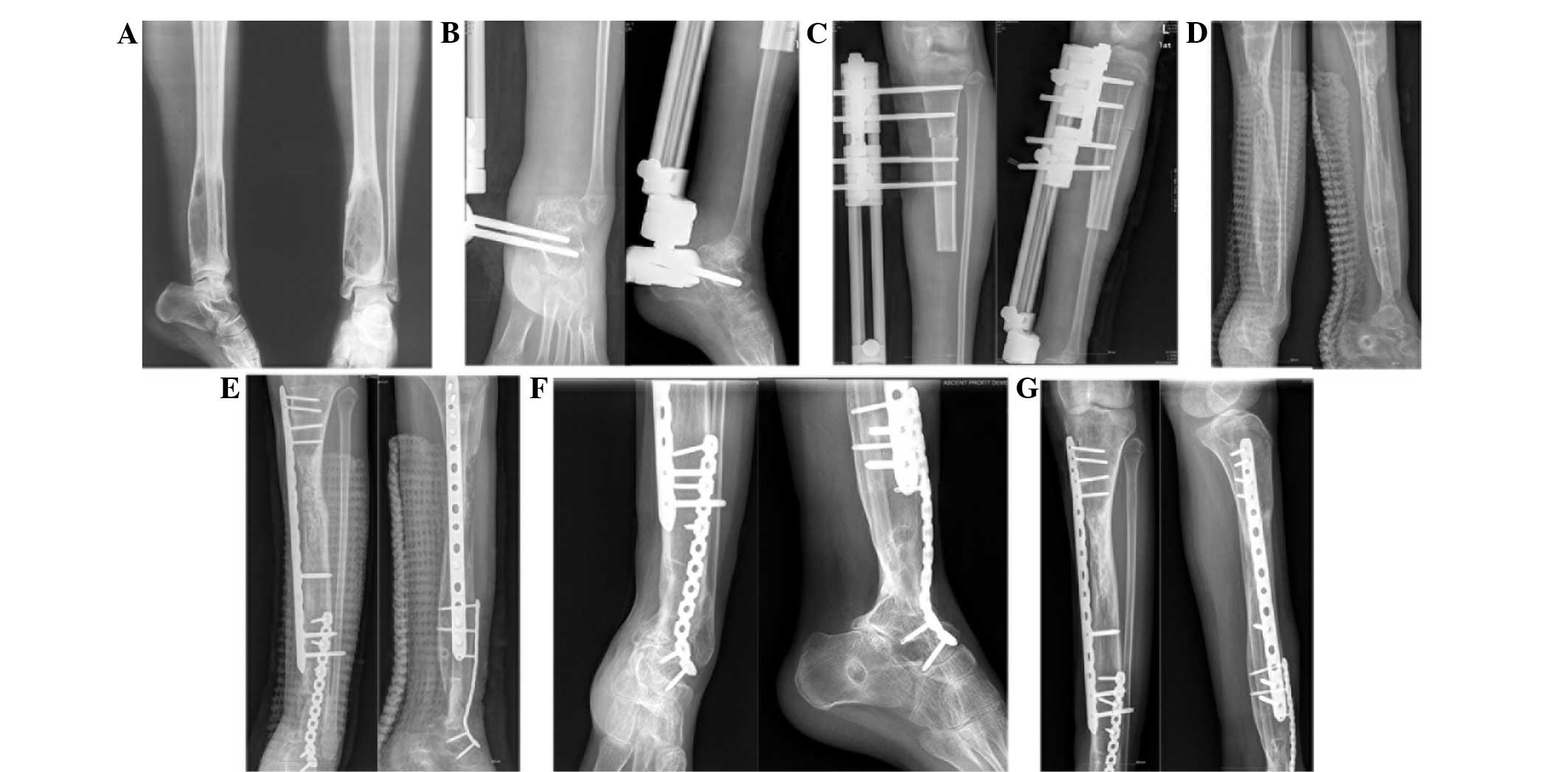
A 29-year-old man was admitted to the Second
Affiliated Hospital (Hangzhou, Zhejiang, China) in April 2009 due
to pain in the right proximal tibial region, which had been ongoing
for 4 months. Biopsy of the tissue sample collected from the
affected site revealed that the lesion was a parosteal
osteosarcoma. Subsequently, the lesion was surgically resected. No
evidence of metastasis was detected during the surgery. The tibial
defect was 11 cm in length and fixed with a Orthofix Limb
Reconstruction System via an external fixator (Orthofix,
Lewisville, TX, USA) (Fig. 1).
Post-surgery, the patient was administered with two cycles of
chemotherapy. Each cycle consisted of methotrexate (8
g/m2) on days 1 and 8, cisplatin (120 mg/m2)
on day 15 and doxorubicin (60 mg/m2) on day 17. The
second cycle of chemotherapy was started after 2 weeks. Bone
transport distraction osteogenesis was initiated on postoperative
day 14 at a distraction rate of 2.0×0.5 mm per day. The callus to
diameter ratio (CDR) was calculated as the diameter of the callus
divided by the diameter of the original diaphysis (8). The distraction rate was reduced to 0.50
or 0.25 mm per day if the CDR was <80%. Distraction was allowed
to continue for 16 months. Subsequently, autologous bone grafts
were harvested from the ilium and implanted at the non-union site.
Bone union was observed for 3 months following the implantation,
and the external fixator was removed. Over a follow-up period of 51
months, the patient exhibited no signs of recurrence or metastasis,
and at the last follow-up visit in July 2013, the patient's
Musculoskeletal Tumor Society functional score (9) was 22. There were no complications during
the postoperative course.
Case 2
A 16-year-old girl was admitted to the Second
Affiliated Hospital in September 2008 with a history of pain in the
left ankle, which had been ongoing for 3 months. The lesion was
identified at the distal tibial end and no signs of metastasis were
noted in the preoperative examination. Pathological examination
revealed that the lesion was an osteosarcoma. The patient received
preoperative and postoperative chemotherapy each for 2 cycles. Each
cycle consisted of methotrexate (8 g/m2) on days 1 and
8, cisplatin (120 mg/m2) on day 15 and doxorubicin (60
mg/m2) on day 17. The second cycle of chemotherapy was
started after 2 weeks. Following the resection of the tumor, the
tibial defect was observed to be 15-cm long and was fixed with an
Orthofix Limb Reconstruction System via an external fixator
(Orthofix) (Fig. 2). Bone transport
was initiated on postoperative day 14 at a distraction rate of
2.0×0.5 mm per day. As with case 1, the distraction rate was
reduced to 0.5 mm or even 0 mm per day if the CDR <80%.
Distraction was continued for 28 months. Subsequently, the external
fixator was removed, and 4 weeks later autologous bone grafts were
harvested from the ilium and implanted at the non-union site, along
with an internal fixator. Bone union was observed 3 months later.
The patient was followed up for 56 months, at the end of which (in
May 2013) the patient exhibited no signs of recurrence or
metastasis, and had a Musculoskeletal Tumor Society functional
score (9) of 18. There were no
complications during the postoperative course.
Discussion
Several options are now available for the
reconstruction of large tibial bone defects following resection of
osteosarcoma, including tumor prostheses, allografts, and
vascularized, autologous osseous grafts. However, tumor prostheses
and allografts are prone to cause infections (4–6,10), and vascularized fibular grafting is a
complex procedure that has poor biomechanical strength (11). By contrast, bone transport distraction
osteogenesis has been demonstrated to be a low-risk procedure with
a beneficial outcome for large bone defects (7,12).
Compared to the other available methods for bone
reconstruction, bone transport distraction osteogenesis is a
simpler procedure with a shorter operation time and, consequently,
lowers the risk of complications. The use of bone transport
distraction generally precludes the requirement for internal
fixation and prosthesis implantation; therefore, this significantly
minimizes the chances of wound infection. The reconstructed bone
formed following distraction osteogenesis has good biomechanical
performance and sufficient rigidity to allow for the execution of
daily activities (13). However,
there are certain drawbacks to bone transport distraction. One
significant limitation of this method is the long duration required
for the completion of distraction, which is a severe test of
patient compliance. Furthermore, chemotherapy administered to
patients may inhibit the osteogenesis process and reduce the rate
of distraction, which may lead to failure of the consolidation of
the callus (7). In the two present
cases, the distraction rate was adjusted according to the CDR in
order to ensure sound formation and consolidation of the
callus.
In addition, it is extremely important to select the
optimal bone transport rate. Previous studies have demonstrated
that bone transport at a rate of 1 mm per day is optimal for the
reconstruction of bone defects caused by trauma (13,14). A low
distraction rate of 0.5 mm per day may lead to premature bone
consolidation, whereas a high rate of 2 mm per day results in the
formation of fibrous tissue without osteogenesis. Furthermore, a
fixed distraction rate of 1 mm per day may not be beneficial for
patients with osteosarcoma, due to the inhibitory effect of
chemotherapy on osteogenesis. CDR is an index that reflects the
quality of the callus formation during distraction osteogenesis
(8). In the two present cases, the
rate of bone transport distraction was reduced to 0.5 or 0.25 mm
per day when the CDR was <80%. This approach inevitably
prolonged the duration of distraction, thereby challenging patient
compliance.
Although a few cases (7) have been reported using bone transport
distraction osteogenesis for the defects resulting from the removal
of bone tumors, the studies have not been concerned with the
effects of chemotherapy. The present 2 cases focused on the
osteosarcoma, discussing the effects of chemotherapy for bone
transport and providing an overview of the whole experience of bone
transport distraction osteogenesis. The study was primarily
concerned with the effects of chemotherapy for the bone transport
distraction osteogenesis of osteosarcoma.
In conclusion, the current study presents two cases
in which bone transport was successfully used for the
reconstruction of large tibial bone defects following osteosarcoma
resection. An important concern associated with this method is the
challenge of patient compliance for the entire treatment duration,
and measures should be taken to encourage the patient to complete
the treatment for successful reconstruction. The current study only
presents information on two cases; therefore, a larger case series
is required to provide treatment recommendations concerning this
type of method for the treatment of tibial bone defects following
osteosarcoma resection.
References
|
1
|
Messerschmitt PJ, Garcia RM, Abdul-Karim
FW, Greenfield EM and Getty PJ: Osteosarcoma. J Am Acad Orthop
Surg. 17:515–527. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ottaviani G and Jaffe N: The epidemiology
of osteosarcoma. Cancer Treat Res. 152:3–13. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Simon MA: Limb salvage for osteosarcoma in
the 1980s. Clin Orthop Relat Res. 264–270. 1991.PubMed/NCBI
|
|
4
|
Natarajan MV, Annamalai K, Williams S,
Selvaraj R and Rajagopal TS: Limb salvage in distal tibial
osteosarcoma using a custom mega prosthesis. Int Orthop.
24:282–284. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Muscolo DL, Ayerza MA, Aponte-Tinao L,
Ranalletta M and Abalo E: Intercalary femur and tibia segmental
allografts provide an acceptable alternative in reconstructing
tumor resections. Clin Orthop Relat Res. 97–102. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ramseier LE, Malinin TI, Temple HT,
Mnaymneh WA and Exner GU: Allograft reconstruction for bone sarcoma
of the tibia in the growing child. J Bone Joint Surg Br. 88:95–99.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Watanabe K, Tsuchiya H, Yamamoto N, Shirai
T, Nishida H, Hayashi K, Takeuchi A, Matsubara H and Nomura I: Over
10-year follow-up of functional outcome in patients with bone
tumors reconstructed using distraction osteogenesis. J Orthop Sci.
18:101–109. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Nakamura K, Matsushita T, Mamada K,
Okazaki H, Ou W, Okuma Y and Kurokawa T: Changes of callus diameter
during axial loading and after fixator removal in leg lengthening.
Arch Orthop Trauma Surg. 117:464–467. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Enneking WF, Dunham W, Gehardt MC, Malawer
M and Pritchard DJ: A system for the functional evaluation of
reconstructive procedures after surgical treatment of tumors of the
musculoskeletal system. Clin Orhtop Relat Res. 241–246. 1993.
|
|
10
|
Shekkeris AS, Hanna SA, Sewell MD,
Spiegelberg BG, Aston WJ, Blunn GW, Cannon SR and Briggs TW:
Endoprosthetic reconstruction of the distal tibia and ankle joint
after resection of primary bone tumours. J Bone Joint Surg Br.
91:1378–1382. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ebeid W, Amin S, Abdelmegid A, Refaat Y
and Ghoneimy A: Reconstruction of distal tibial defects following
resection of malignant tumours by pedicled vascularised fibular
grafts. Acta Orthop Belg. 73:354–359. 2007.PubMed/NCBI
|
|
12
|
Tsuchiya H and Tomita K: Distraction
osteogenesis for treatment of bone loss in the lower extremity. J
Orthop Sci. 8:116–124. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ilizarov GA: The tension-stress effect on
the genesis and growth of tissues: Part II. The influence of the
rate and frequency of distraction. Clin Orthop Relat Res. 263–285.
1989.PubMed/NCBI
|
|
14
|
Ilizarov GA: Clinical application of the
tension-stress effect for limb lengthening. Clin Orthop Relat Res.
8–26. 1990.PubMed/NCBI
|