Introduction
Colon cancer is a major cause of mortality
worldwide, and is the leading cause of cancer-associated mortality
in a number of developed countries (1). The number of colon cancers requiring
surgical intervention continues to increase due to the prolongation
of life expectancy in many nations (2). Recently, multi-port laparoscopic surgery
(MLS) has been adopted more frequently worldwide for the treatment
of colon cancer. Compared with open surgery, MLS has been
associated with less pain, a quicker recovery of gastrointestinal
function, improved pulmonary function, shorter hospital stays and a
better postoperative quality of life (3). In addition, single-incision laparoscopic
surgery (SLS) has been successfully introduced for colon cancer
treatment (4–8), and has become a more commonly used
surgical option.
These procedures, when used for elderly patients,
must be selected with care, considering the magnitude of the
surgery and the predicted risk of hospital mortality (9,10);
however, postoperative morbidity and mortality increase with age
(11–15). Several studies have reported that MLS
demonstrates oncological results and surgical outcomes comparable
to that of open surgery (16–23). However, in the elderly, although MLS
is reported to be non-inferior to the open procedure and may be an
acceptable alternative in elderly patients with colorectal cancer
(24), no study has investigated the
feasibility of SLS in elderly patients with colon cancer, with the
exception of one small study (10).
Therefore, the critical issue of whether SLS can benefit colon
cancer patients of advanced age as an alternative to MLS remains to
be elucidated. The purpose of this retrospective study was thus to
determine the feasibility of SLS in the elderly.
Materials and methods
Patients
Between January 2011 and September 2014, 378
patients underwent laparoscopic surgery for colon cancer at Yao
Municipal Hospital (Yao, Japan); 129 were aged ≥70 years. A
retrospective case-control study of these 129 patients who
underwent elective surgical intervention for colon cancer was
conducted. The MLS group consisted of 79 patients in the first half
of this period, and the SLS group consisted of 50 patients in the
latter half of this period. All procedures were performed by staff
colorectal surgeons who were highly experienced in MLS or SLS. Data
on patient demographics, body mass index (BMI), American Society of
Anesthesiologists (ASA) class, tumor location, tumor size, personal
history of prior surgery, surgery time, estimated blood loss,
number of lymph nodes harvested, length of the resected margin,
conversion to open surgery, insertion of an additional port,
perioperative complications, morbidity and length of hospital stay
were compared. The present study was approved by the research
ethics committee of Yao Municipal Hospital. Written informed
consent was obtained from the patients for publication of the
present study and accompanying images.
Surgical technique
MLS required five ports, with the first 12-mm trocar
in the umbilicus or a Lap Protector (LP; Hakko, Co., Ltd., Nagano,
Japan) as a camera port, another 12-mm trocar, and three 5-mm
trocars. The trocars were inserted in the upper and lower abdominal
quadrants on the right and left sides, under laparoscopic guidance.
The camera port was expanded to extract the specimen through an
incision of 4–5 cm, as previously described (17,25).
For SLS, an LP was inserted through a 30-mm incision
at the umbilicus. Following this, an EZ Access (Hakko Co., Ltd.)
was mounted on the LP, and three 5 mm ports were placed in the EZ
Access. The surgical procedures and instruments were the same as
those used for standard laparoscopic surgery with a flexible 5 mm
scope (EndoEye Flex HD; Olympus Corporation, Tokyo, Japan). An
additional incision or trocar port was placed without hesitation,
if necessary, to complete the procedure, and conversion to open
laparotomy was maintained as an option. The decision to use an
additional trocar or to convert to open laparotomy depended on the
staff surgeon. For lymphadenectomy, a complete mesocolic excision
(CME) with central vascular ligation (CVL) was performed (26–28). The
final incision was extended to a length comparable to the size of
the specimen.
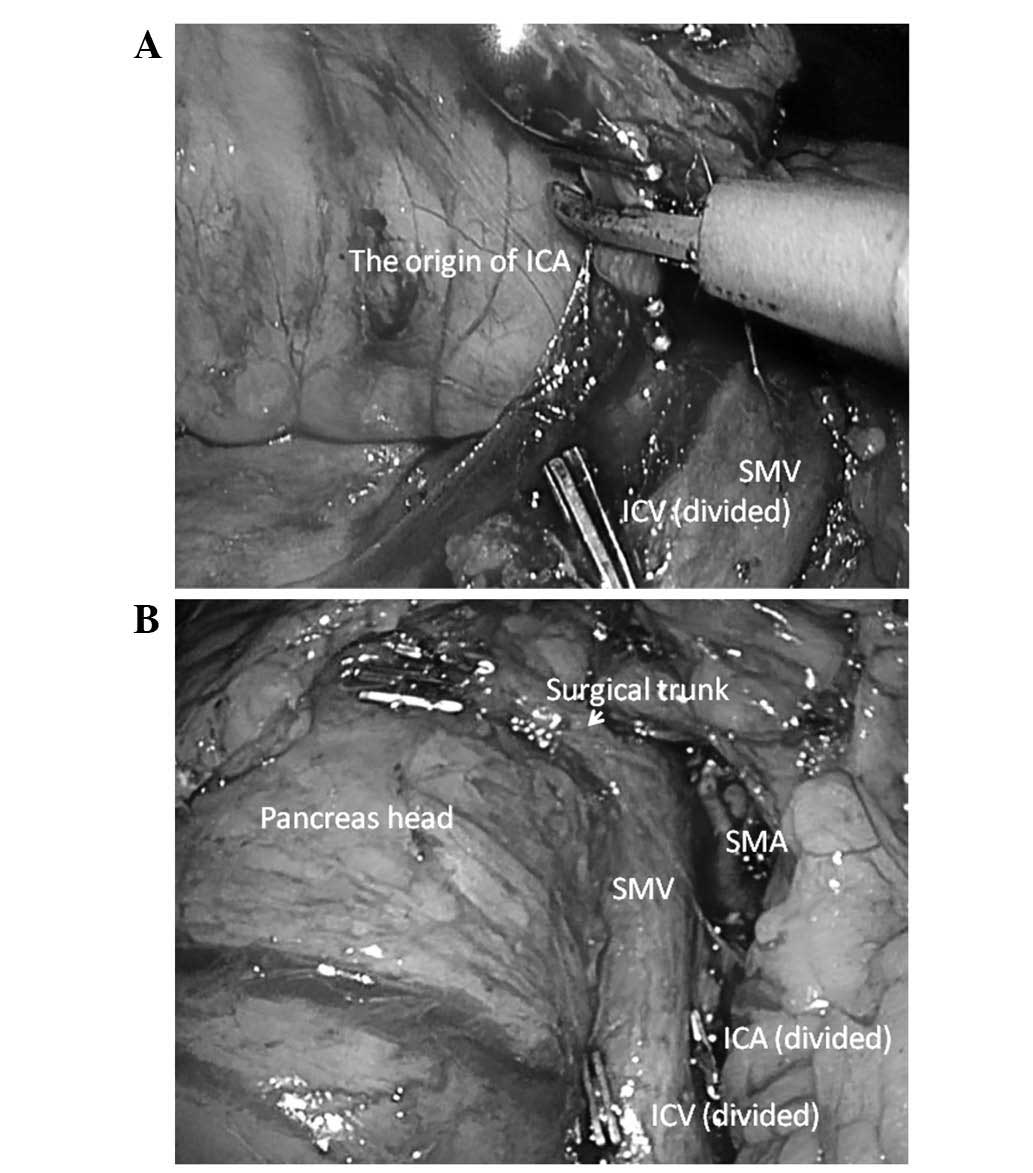
Right hemicolectomy
The patient was placed in the Trendelenburg
semi-left lateral position (29). The
surgeon and camera operator stood on the left side of the patient.
For MLS, the assistant stood between the patient's legs. In both
groups, the procedure was performed via an inferior approach, with
initial peritoneal dissection between the mesoileum and the
retroperitoneum. Following mesocolic plane resection, the duodenum
and pancreas were sufficiently exposed, and the ileocolic, right
colic (if necessary) and middle colic vessels were ligated and
dissected between clips at their origin to allow CME and CVL
(Fig. 1). Following the dissection of
the greater omentum, the hepatic flexure was mobilized. The
specimen was retrieved through the incision of the umbilicus, after
which an extracorporeal, functional end-to-end anastomosis was
performed.
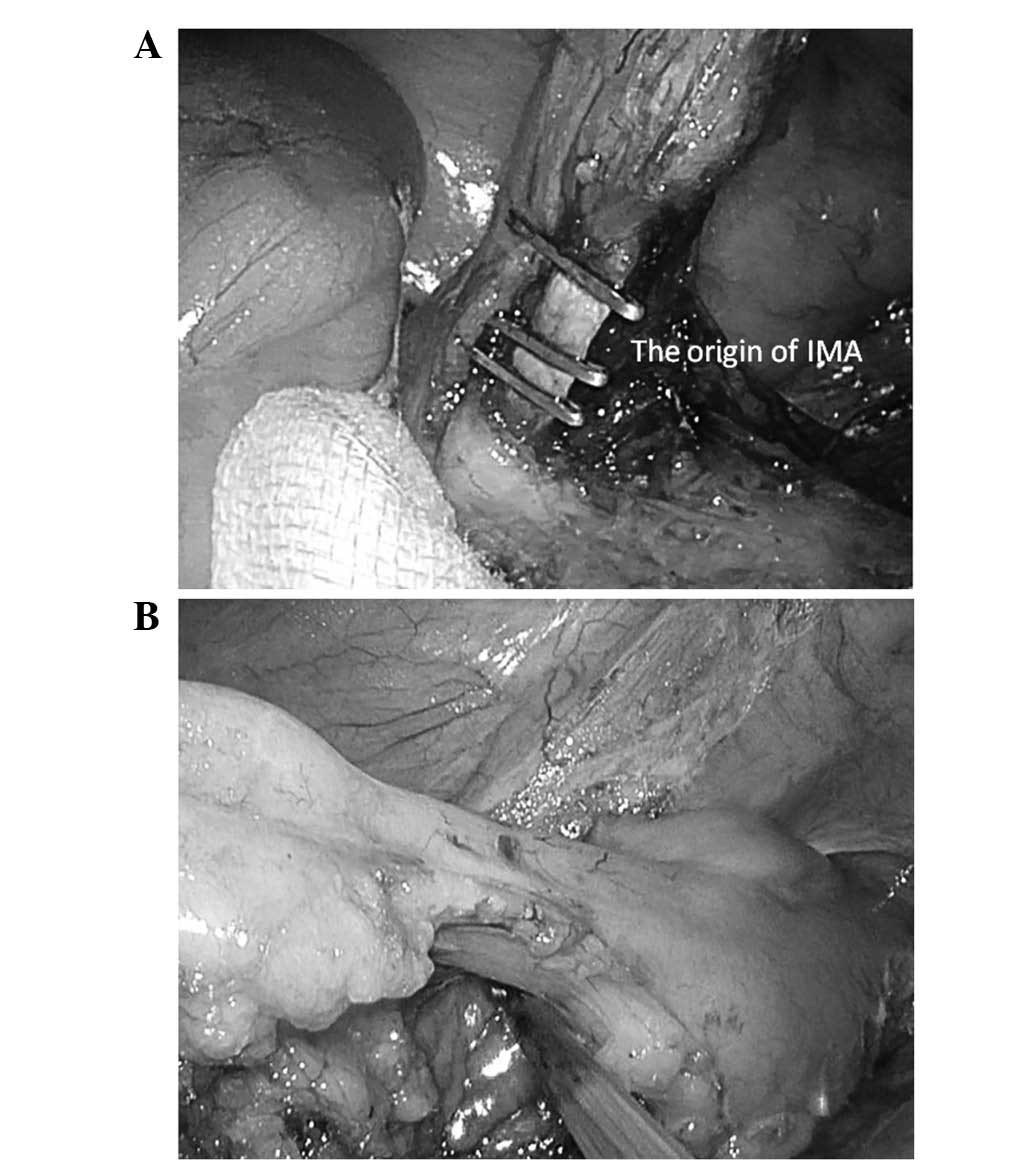
Sigmoidectomy and anterior
resection
The patient was placed in the Trendelenburg
semi-right lateral position. The surgeon and camera operator stood
on the right side of the patient. For MLS, the assistant stood
between the patient's legs or on the left. In both groups, the
procedure was performed via a standard medial-to-lateral approach.
The inferior mesenteric artery and the inferior mesenteric vein
were skeletonized, clipped and divided for CME and CVL (Fig. 2). A downwards dissection from the
mesenteric window to the pelvis was then performed. The next step
was mobilization of the sigmoid colon up to the splenic flexure.
The descending colon and sigmoid colon were pulled anteromedially
to ensure preservation of the left ureter and gonadal vessels. The
fat surrounding the rectum for ≥50 mm distal to the lesion was
dissected and then normally transected using an endoscopic linear
stapler (Endo GIA™; Medtronic, Minneapolis, MN, USA) with a purple
cartridge inserted from the umbilical port with a 12 mm EZ Link
(Hakko Co., Ltd.). The specimen was retrieved through the umbilical
incision, and the double stapling technique was applied for
anastomosis.
Statistical analysis
Data are presented as the number (n) per group or as
the mean ± standard deviation, accordingly. Statistical analysis
was performed using commercially available software (SPSS version
14.0 for Windows; SPSS, Inc., Chicago, IL, USA). All variables were
evaluated using a χ2 test or Student's t-test, as
appropriate. P<0.05 was considered to indicate statistically
significant differences.
Results
Patient characteristics
Patient characteristics did not differ significantly
between the MLS and SLS groups: Age, 76.6±4.8 vs. 79.6±12.5 years,
respectively, P=0.73; BMI, 22.4±3.6 vs. 22.7±3.7 kg/m2,
respectively, P=0.68. No other clinical variables, including ASA
status, tumor location and history of prior surgery, differed
significantly between these two groups. In addition, comparison of
these variables between groups on the basis of the tumor location
(right and left colon cancer), no differences were found (Table I).
 | Table I.Patient characteristics. |
Table I.
Patient characteristics.
|
| Total | Right-sided colon
cancer | Left-sided colon
cancer |
|---|
|
|
|
|
|
|---|
| Variable | MLS (n=79) | SLS (n=50) | P-value | MLS (n=36) | SLS (n=27) | P-value | MLS (n=43) | SLS (n=23) | P-value |
|---|
| Age
(years)a | 76.9±5.3 | 76.6±4.8 | 0.73 | 77.8±5.6 | 77.7±5.4 | 0.96 | 76.1±4.9 | 75.1±3.7 | 0.44 |
| Gender (n) |
|
| 0.68 |
|
| 0.17 |
|
| 0.54 |
| Male | 44 | 26 |
| 15 | 16 |
| 29 | 13 |
|
|
Female | 35 | 24 |
| 21 | 11 |
| 14 | 10 |
|
| BMI
(kg/m2)a | 22.4±3.6 | 22.7±3.7 | 0.57 | 21.9±4.5 | 23.1±3.7 | 0.26 | 22.7±2.7 | 22.3±3.7 | 0.55 |
| ASA status (n) |
|
| 0.33 |
|
| 0.19 |
|
| 0.82 |
| 1 | 2 | 4 |
| 0 | 2 |
| 2 | 2 |
|
| 2 | 63 | 39 |
| 31 | 23 |
| 32 | 16 |
|
| 3 | 14 | 7 |
| 5 | 2 |
| 9 | 5 |
|
| Prior surgery
(n) | 24 | 18 | 0.64 | 7 | 9 | 0.33 | 17 | 9 | 0.82 |
| Tumor location
(n) |
|
| 0.61 |
|
|
|
|
|
|
|
Cecum | 11 | 6 |
| 11 | 6 |
|
|
|
|
|
Ascending colon | 16 | 15 |
| 16 | 15 |
|
|
|
|
|
Transverse colon | 9 | 6 |
| 9 | 6 |
|
|
|
|
|
Descending colon | 3 | 2 |
|
|
|
| 3 | 2 |
|
| Sigmoid
colon | 29 | 12 |
|
|
|
| 29 | 12 |
|
|
Rectosigmoid colon | 11 | 9 |
|
|
|
| 11 | 9 |
|
Surgical outcomes. The surgical statistics are
listed in Table II. All surgical
outcomes, including surgery time, blood loss, hospital stay and
delay until first bowel motion, were similar between the MLS and
SLS groups. For right-sided colon cancer, surgery time was nearly
equivalent in the two groups (221.3±69.3 vs. 217.3±59.7 min,
respectively, P=0.80). By contrast, for left-sided colon cancer,
surgery time tended to be shorter in the MLS group than in the SLS
group (196.3±51.1 vs. 214.3±69.7 min, respectively, P=0.23);
however, this difference was non-significant.
 | Table II.Surgical outcomes. |
Table II.
Surgical outcomes.
|
| Total | Right-sided colon
cancer | Left-sided colon
cancer |
|---|
|
|
|
|
|
|---|
| Variable | MLS (n=79) | SLS (n=50) | P-value | MLS (n=36) | SLS (n=27) | P-value | MLS (n=43) | SLS (n=23) | P-value |
|---|
| Surgical time
(min)a | 207.7±61.0 | 215.9±63.8 | 0.47 | 221.3±69.3 | 217.3±59.7 | 0.80 | 196.3±51.1 | 214.3±69.7 | 0.23 |
| Estimated blood
loss (ml)a | 56.8±141.5 | 78.6±268.9 | 0.64 | 105.6±188.7 | 134.1±218.7 | 0.75 | 16.0±61.4 | 13.5±31.6 | 0.85 |
| Conversion to
laparotomy (n) | 3 | 1 | 0.96 | 3 | 0 | – | 0 | 1 | – |
| Additional trocars
required (n) | 0 | 1 | – | 0 | 0 | – | 0 | 1 | – |
| Length of hospital
stay (days)a | 10.6±8.8 | 10.1±10.2 | 0.77 | 11.2±10.7 | 8.2±7.3 | 0.22 | 10.2±6.9 | 12.4±12.6 | 0.36 |
| Days until first
bowel motiona | 4.1±3.7 | 4.1±1.9 | 0.42 | 4.3±2.1 | 4.0±1.2 | 0.32 | 4.0±1.5 | 4.4±2.8 | 0.88 |
| Complications
(n) | 6 | 6 | 0.60 | 4 | 2 | 0.95 | 2 | 4 | 0.21 |
| Wound
infection | 0 | 1 |
| 0 | 1 |
| 0 | 0 |
|
|
Anastomotic leakage | 3 | 1 |
| 2 | 0 |
| 1 | 1 |
|
|
Ileus | 1 | 1 |
| 1 | 0 |
| 0 | 1 |
|
|
Urinary | 1 | 1 |
| 0 | 0 |
| 1 | 1 |
|
|
Other | 1 (gastric
ulcer) | 1 (pneumonia) 1
(thrombosis) |
| 1 (gastric
ulcer) | 1 (thrombosis) |
| 0 | 1 (pneumonia) |
|
| Re-admission within
30 days after surgery (n) | 0 | 0 | – | 0 | 0 | – | 0 | 0 | – |
| Number of harvested
lymph nodesa | 20.3±3.9 | 21.9±9.4 | 0.46 | 24.2±16.9 | 24.3±9.2 | 0.98 | 17.0±9.9 | 19.2±9.1 | 0.38 |
| Margin of specimen
(mm)a |
|
Proximal margin | 104.9±64.9 | 99.7±65.5 | 0.66 | 125.2±79.6 | 128.1±69.8 | 0.88 | 87.9±43.5 | 76.3±40.6 | 0.10 |
| Distal
margin | 74.6±41.9 | 82.3±57.8 | 0.38 | 84.7±42.9 | 91.9±69.5 | 0.61 | 66.2±39.6 | 71.0±38.6 | 0.63 |
| Tumor size
(mm)a | 44.3±22.5 | 43.3±22.6 | 0.81 | 48.3±25.3 | 46.6±23.9 | 0.79 | 41.0±19.5 | 39.5±20.7 | 0.76 |
The occurrence of surgical complications was nearly
equivalent in the two groups (n=6 in both groups; P=0.60). The
length of hospital stay and the delay until first bowel motion also
did not differ significantly between the two groups (10.6±8.8 vs.
10.1±10.2 days, respectively, P=0.77; 4.1±3.7 vs. 4.1±1.9 days,
respectively, P=0.42). For right-sided colon cancer, hospital stay
and the delay until first bowel motion appeared to be marginally
longer in the MLS group than in SLS group (11.2±10.7 vs. 8.2±7.3
days, respectively, P=0.22; 4.3±2.1 vs. 4.0±1.2 days, respectively,
P=0.32). By contrast, hospital stay tended to be slightly shorter
in the MLS group than in the SLS group for left-sided colon cancer
(10.2±6.9 vs. 12.4±12.6 days, respectively, P=0.36), whilst delay
until first bowel motion was similar (4.0±1.5 vs. 4.0±2.8 days,
respectively, P=0.88).
In 3 patients in the MLS group, the surgery was
converted to laparotomy due to bulky lymph node metastases (in 1
case) or intra-abdominal adhesions (in 2 cases); 1 case in the SLS
group was converted to laparotomy due to the presence of a
congenital bone disorder. In the SLS group, 1 patient required an
additional port due to a rectal injury. There was no mortality in
either group, and there was no readmission within 30 days
subsequent the procedure. Regarding oncological features, the
number of resected lymph nodes, and the resection margin and tumor
sizes did not differ significantly between the MLS and SLS
groups.
Discussion
The proportion of elderly patients requiring major
abdominal surgery is increasing (24,30). It is
clear that, as patients age, there is an associated increase in
comorbid conditions that often complicate the perioperative
management of elderly patients who undergo major surgery (24,30). MLS
is currently considered to be safe and feasible in elderly
patients, and evidence has suggested that it is not inferior to the
open procedure, as it seems to be less physiologically stressful
than conventional open laparotomy (24,30).
SLS offers a potential advantage in the context of
minimally invasive surgery. Reduced-port surgery aims to reduce the
size and number of ports, preserving the view afforded by the
laparoscope while making the surgery less invasive. A number of
reports have demonstrated its advantages in reducing the number of
laparoscopic ports, including better cosmetic results, reduced
postoperative pain and shorter recovery time (31–35). In
the current study, no statistically significant differences in
short-term outcomes were found between elderly colon cancer
patients who underwent MLS and SLS. To the best of our knowledge,
this is the first reported case-control study involving elderly
patients (mean age, 76.7 years).
The short-term outcomes in this study demonstrated
equivalence with the use of SLS and MLS in elderly patients
(Table II); the overall morbidities
and number of cases with postoperative complications were nearly
equivalent in the two groups. The length of hospital stay and the
time until the first bowel motion following surgery did not differ
significantly between the two groups when patients with left- and
right-sided lesions were combined. For right-sided colon cancer,
hospital stay and delay until first bowel motion tend to be shorter
in the SLS group than in MLS group; however, the differences were
non-significant. These findings suggest that SLS may potentially be
less invasive for elderly patients with right-sided colon cancer.
On the other hand, with left-sided colon cancer, although there was
no significant difference, hospital stay was ~2 days longer in the
SLS group than in the MLS group. A possible reason for this may be
that the duration of surgery tended to be slightly longer for SLS
than for MLS, perhaps related to the trimming of margins on the
anal side of the colon, a procedure which tends to take longer
during SLS than during MLS. It is thus likely that, if technical
development is achieved in the trimming procedure, the difference
in the duration of surgery for left-sided colon cancer may
decrease. As a result, it may be possible to reduce the difference
in the length of hospital stay.
With regard to the oncological quality of the
surgery in the present study, the number of resected lymph nodes
and resection margins did not differ significantly between the SLS
and MLS groups; the mean number of removed lymph nodes was between
17.0 and 24.3 in each group, which is consistent with other studies
(16,17,36).
Regarding the rate of conversion to laparotomy, the current data
indicate conversion rates of 2.0–8.3% in patients when cases with
left- and right-sided colon cancers were combined. The total
conversion rate for the 129 patients was 3.1%, which is consistent
with previous reports (16,36,37).
The current study has certain limitations. Firstly,
the number of cases was insufficient. It is likely that more
accurate data could be obtained by increasing the number of cases
and conducting an investigation with a large cohort. Secondly, this
investigation involved a single institution. Since there were just
two surgeons, it is not necessarily the case that similar results
would be observed at any institution, and collecting cases from
other institutions would produce more universal results. Thirdly,
only short-term outcomes are reported, as it was not possible to
obtain long-term outcomes. In order to demonstrate that SLS and MLS
give similar results in elderly patients, it will be necessary to
include a larger number of cases from other institutions, and use a
longer observation period in the future.
Despite these limitations, the current observations
indicate that SLS has equivalent short-term surgical outcomes to
MLS and is oncologically feasible in elderly patients, consistently
with the results of previous reports in the general population
(16–23). Thus, we believe that these results
justify the use of SLS in the routine treatment of elderly patients
with colon cancer.
In conclusion, the current study suggests that SLS
is equivalent to MLS and is acceptable in elderly patients with
cancer.
References
|
1
|
Center MM, Jemal A and Ward E:
International trends in colorectal cancer incidence rates. Cancer
Epidemiol Biomarkers Prev. 18:1688–1694. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Law WL, Chu KW and Tung PH: Laparoscopic
colorectal resection: A safe option for elderly patients. J Am Coll
Surg. 195:768–773. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yasuda K, Sonoda K, Shiroshita H, Inomata
M, Shiraishi N and Kitano S: Laparoscopically assisted distal
gastrectomy for early gastric cancer in the elderly. Br J Surg.
91:1061–1065. 2004. View
Article : Google Scholar : PubMed/NCBI
|
|
4
|
Choi SI, Lee KY, Park SJ and Lee SH:
Single port laparoscopic right hemicolectomy with D3 dissection for
advanced colon cancer. World J Gastroenterol. 16:275–278. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ramos-Valadez DI, Patel CB, Ragupathi M,
Bartley Pickron T and Haas EM: Single-incision laparoscopic right
hemicolectomy: Safety and feasibility in a series of consecutive
cases. Surg Endosc. 24:2613–2616. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hamzaoglu I, Karahasanoglu T, Baca B,
Karatas A, Aytac E and Kahya AS: Single-port laparoscopic
sphincter-saving mesorectal excision for rectal cancer: Report of
the first 4 human cases. Arch Surg. 146:75–81. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Merchant AM and Lin E: Single-incision
laparoscopic right hemicolectomy for a colon mass. Dis Colon
Rectum. 52:1021–1024. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Uematsu D, Akiyama G, Matsuura M and Hotta
K: Single-access laparoscopic colectomy with a novel multiport
device in sigmoid colectomy for colon cancer. Dis Colon Rectum.
53:496–501. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Fiscon V, Portale G, Migliorini G and
Frigo F: Laparoscopic resection of colorectal cancer in elderly
patients. Tumori. 96:704–708. 2010.PubMed/NCBI
|
|
10
|
Hirano Y, Hattori M, Sato Y, Maeda K,
Douden K and Hashizume Y: The outcome of single-incision
laparoscopic right colectomy for colon carcinoma in the elderly.
Surg Laparosc Endosc Percutan Tech. 22:338–340. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Surgery for colorectal cancer in elderly
patients: A systematic review. Lancet. 356:968–974. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Rutten HJ, den Dulk M, Lemmens VE, van de
Velde CJ and Marijnen CA: Controversies of total mesorectal
excision for rectal cancer in elderly patients. Lancet Oncol.
9:494–501. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Turrentine FE, Wang H, Simpson VB and
Jones RS: Surgical risk factors, morbidity and mortality in elderly
patients. J Am Coll Surg. 203:865–877. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Al-Refaie WB, Parsons HM, Habermann EB,
Kwaan M, Spencer MP, Henderson WG and Rothenberger DA: Operative
outcomes beyond 30-day mortality: Colorectal cancer surgery in
oldest old. Ann Surg. 253:947–952. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Panis Y, Maggiori L, Caranhac G, Bretagnol
F and Vicaut E: Mortality after colorectal cancer surgery: A French
survey of more than 84,000 patients. Ann Surg. 254:738–743;
discussion 743–744. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
A comparison of laparoscopically assisted
and open colectomy for colon cancer. N Engl J Med. 350:2050–2059.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Guillou PJ, Quirke P, Thorpe H, Walker J,
Jayne DG, Smith AM, Heath RM and Brown JM: MRC CLASICC trial group:
Short-term endpoints of conventional versus laparoscopic-assisted
surgery in patients with colorectal cancer (MRC CLASICC trial):
Multicentre, randomised controlled trial. Lancet. 365:1718–1726.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Veldkamp R, Kuhry E, Hop WC, Jeekel J,
Kazemier G, Bonjer HJ, Haglind E, Påhlman L, Cuesta MA, Msika S, et
al: Laparoscopic surgery versus open surgery for colon cancer:
Short-term outcomes of a randomised trial. Lancet Oncol. 6:477–484.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Jayne DG, Guillou PJ, Thorpe H, Quirke P,
Copeland J, Smith AM, Heath RM and Brown JM: UK MRC CLASICC Trial
Group: Randomized trial of laparoscopic-assisted resection of
colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial
Group. J Clin Onco. 25:3061–3068. 2007. View Article : Google Scholar
|
|
20
|
Colon Cancer Laparoscopic or Open
Resection Study Group. Buunen M, Veldkamp R, Hop WC, Kuhry E,
Jeekel J, Haglind E, Påhlman L, Cuesta MA, Msika S, et al: Survival
after laparoscopic surgery versus open surgery for colon cancer:
Long-term outcome of a randomised clinical trial. Lancet Oncol.
10:44–52. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hemandas AK, Abdelrahman T, Flashman KG,
Skull AJ, Senapati A, O'Leary DP and Parvaiz A: Laparoscopic
colorectal surgery produces better outcomes for high risk cancer
patients compared to open surgery. Ann Surg. 252:84–99. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Bagshaw PF, Allardyce RA, Frampton CM,
Frizelle FA, Hewett PJ, McMurrick PJ, Rieger NA, Smith JS, Solomon
MJ and Stevenson AR: Australasian Laparoscopic Colon Cancer Study
Group: Long-term outcomes of the australasian randomized clinical
trial comparing laparoscopic and conventional open surgical
treatments for colon cancer: The Australasian laparoscopic colon
cancer study trial. Ann Surg. 256:915–919. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Cummings LC, Delaney CP and Cooper GS:
Laparoscopic versus open colectomy for colon cancer in an older
population: A cohort study. World J Surg Oncol. 10:312012.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Hinoi T, Kawaguchi Y, Hattori M, Okajima
M, Ohdan H, Yamamoto S, Hasegawa H, Horie H, Murata K, Yamaguchi S,
et al: Laparoscopic versus open surgery for colorectal cancer in
elderly patients: A multicenter matched case-control study. Ann
Surg Oncol. 22:2040–250. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Lacy AM, García-Valdecasas JC, Delgado S,
Castells A, Taurá P, Piqué JM and Visa J: Laparoscopy-assisted
colectomy versus open colectomy for treatment of non-metastatic
colon cancer: A randomised trial. Lancet. 359:2224–2229. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Hohenberger W, Weber K, Matzel K,
Papadopoulos T and Merkel S: Standardized surgery for colonic
cancer: Complete mesocolic excision and central ligation-technical
notes and outcome. Colorectal Dis. 11:354–364; discussion 364–365.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
West NP, Hohenberger W, Weber K, Perrakis
A, Finan PJ and Quirke P: Complete mesocolic excision with central
vascular ligation produces an oncologically superior specimen
compared with standard surgery for carcinoma of the colon. J Clin
Oncol. 28:272–278. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
West NP, Kobayashi H, Takahashi K,
Perrakis A, Weber K, Hohenberger W, Sugihara K and Quirke P:
Understanding optimal colonic cancer surgery: Comparison of
Japanese D3 resection and European complete mesocolic excision with
central vascular ligation. J Clin Oncol. 30:1763–1769. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Tokuoka M, Ide Y, Yamato H, Uemura M,
Hashimoto Y, Matsuyama J, Yokoyama S, Morimoto T, Fukushima Y,
Nomura T, et al: Single-incision plus one port laparoscopic total
pelvic exenteration after neoadjuvant chemotherapy for advanced
primary rectal cancer: A case report. Int Sur. 100:1265–1270. 2015.
View Article : Google Scholar
|
|
30
|
Nakamura T, Mitomi H, Onozato W, Sato T,
Ikeda A, Naito M, Ogura N, Kamata H, Ooki A and Watanabe M:
Oncological outcomes of laparoscopic surgery in elderly patients
with colon cancer: A comparison of patients 64 years or younger
with those 75 years or older. Hepatogastroenterology. 58:1200–1204.
2011. View
Article : Google Scholar : PubMed/NCBI
|
|
31
|
Chen WT, Chang SC, Chiang HC, Lo WY, Jeng
LB, Wu C and Ke TW: Single-incision laparoscopic versus
conventional laparoscopic right hemicolectomy: A comparison of
short-term surgical results. Surg Endosc. 25:1887–1892. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Ramos-Valadez DI, Ragupathi M, Nieto J,
Patel CB, Miller S, Pickron TB and Haas EM: Single-incision versus
conventional laparoscopic sigmoid colectomy: A case-matched series.
Surg Endosc. 26:96–102. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Champagne BJ, Lee EC, Leblanc F, Stein SL
and Delaney CP: Single-incision vs straight laparoscopic segmental
colectomy: A case-controlled study. Dis Colon Rectum. 54:183–186.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Champagne BJ, Papaconstantinou HT, Parmar
SS, Nagle DA, Young-Fadok TM, Lee EC and Delaney CP:
Single-incision versus standard multiport laparoscopic colectomy: A
multicenter, case-controlled comparison. Ann Surg. 255:66–69. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Poon JT, Cheung CW, Fan JK, Lo OS and Law
WL: Single-incision versus conventional laparoscopic colectomy for
colonic neoplasm: A randomized, controlled trial. Surg Endosc.
26:2729–2734. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Leung KL, Kwok SP, Lam SC, Lee JF, Yiu RY,
Ng SS, Lai PB and Lau WY: Laparoscopic resection of rectosigmoid
carcinoma: Prospective randomised trial. Lancet. 363:1187–1192.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Veldkamp R, Gholghesaei M, Bonjer HJ,
Meijer DW, Buunen M, Jeekel J, Anderberg B, Cuesta MA, Cuschierl A,
Fingerhut A, et al: Laparoscopic resection of colon cancer:
Consensus of the European association of endoscopic surgery (EAES).
Surg Endosc. 18:1163–1185. 2004. View Article : Google Scholar : PubMed/NCBI
|