Introduction
Extramedullary plasmacytoma (EMP) is an extremely
rare type of plasmacytoma that is most similar to multiple myeloma.
EMP accounts for ~3% of all plasmacytomas and ~1% of all general
malignancies. It mainly occurs in the upper respiratory tract and
upper gastrointestinal tract (80–90%) (1). Cases of EMP generally present as masses
with sections of nonspecific soft tissue density (2). The diagnosis of EMP requires rigorous
investigation to rule out multiple myeloma and osteolytic lesions:
Immunohistochemical analysis and biopsy/bone marrow puncture
(<5% of plasmacytoid atypia) are performed to rule out multiple
myeloma; serum and urinary protein electrophoresis are performed to
detect M and Bence-Jones protein (no expression), respectively, to
rule out osteolytic lesions. In addition, it is essential to ensure
that the patient is not anemic (2–7). Treatment
for EMP includes radiotherapy with high radiosensitivity (80–100%)
and surgery for localized lesions (8,9); however,
treated patients exhibit a recurrence or dissemination rate of
20–40% (8). In the present study, we
report the case of a 77-year-old male patient who was revealed to
have an unsuspected case of gastric adenocarcinoma with
paravertebral EMP following biopsy. Following a search of the
literature in PUBMED and the China National Knowledge
Infrastructure (CNKI), no studies of EMP in the paravertebral area
could be identified, indicating that our case may be unique. The
process of diagnosis and treatment conforms to the ethics policy of
our hospital.
Case report
Patient presentation and
diagnosis
A 77-year-old male was admitted to Yantai
Yuhuangding Hospital (Yantai, China) presenting with continuous
pain in the epigastrium for months. He had a red blood cell count
of 2.80×1012/l and a hemoglobin level of 90 g/l. The
patient had a long-term history of anemia. His serum calcium level
was 1.87 mmol/l. A urine analysis for Bence Jones proteins was
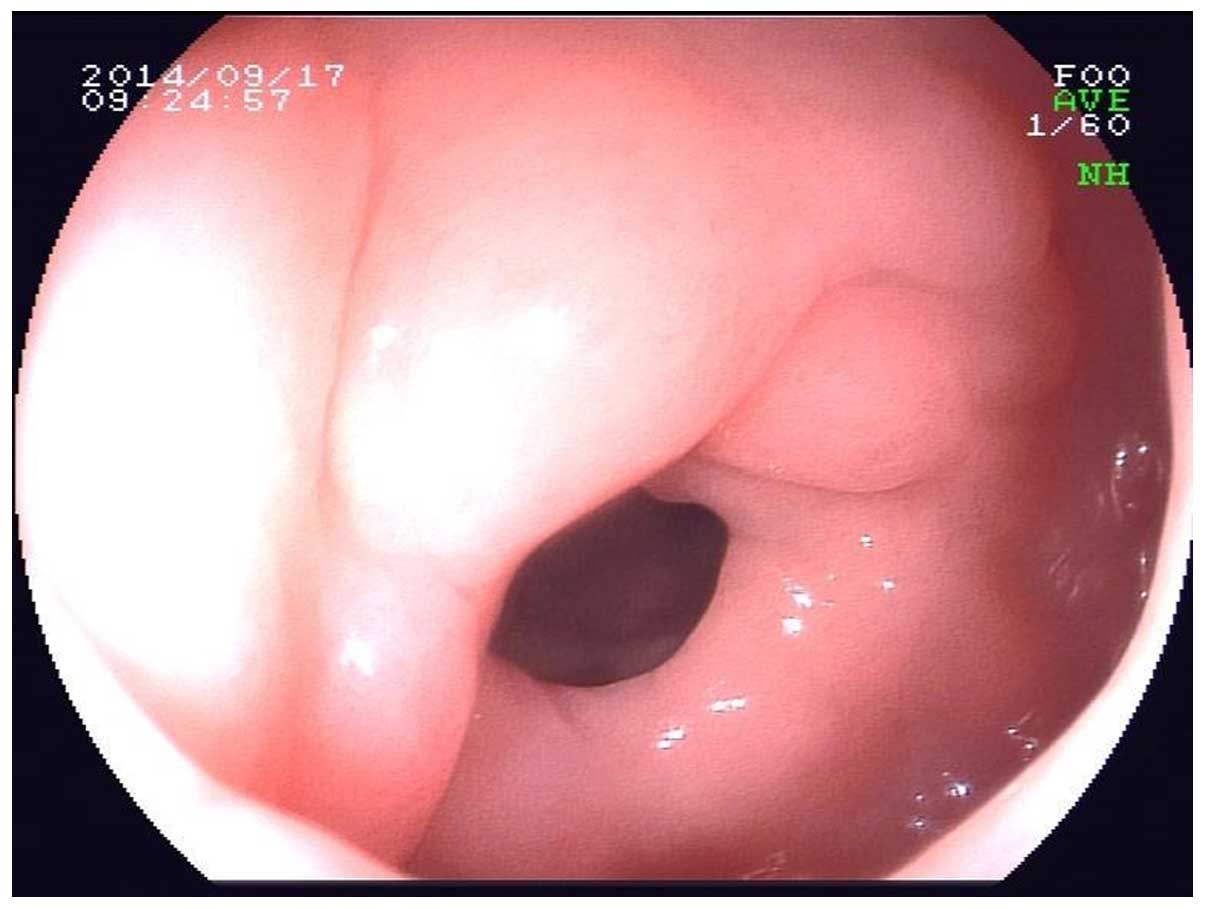
negative. Gastroscopy examination revealed raised masses on the
gastric antrum, an uneven surface, a hard, nodular feeling, and
congestion over an area of ~4×3 cm. Gastric ulcers and atrophic
gastritis were visible (Fig. 1).
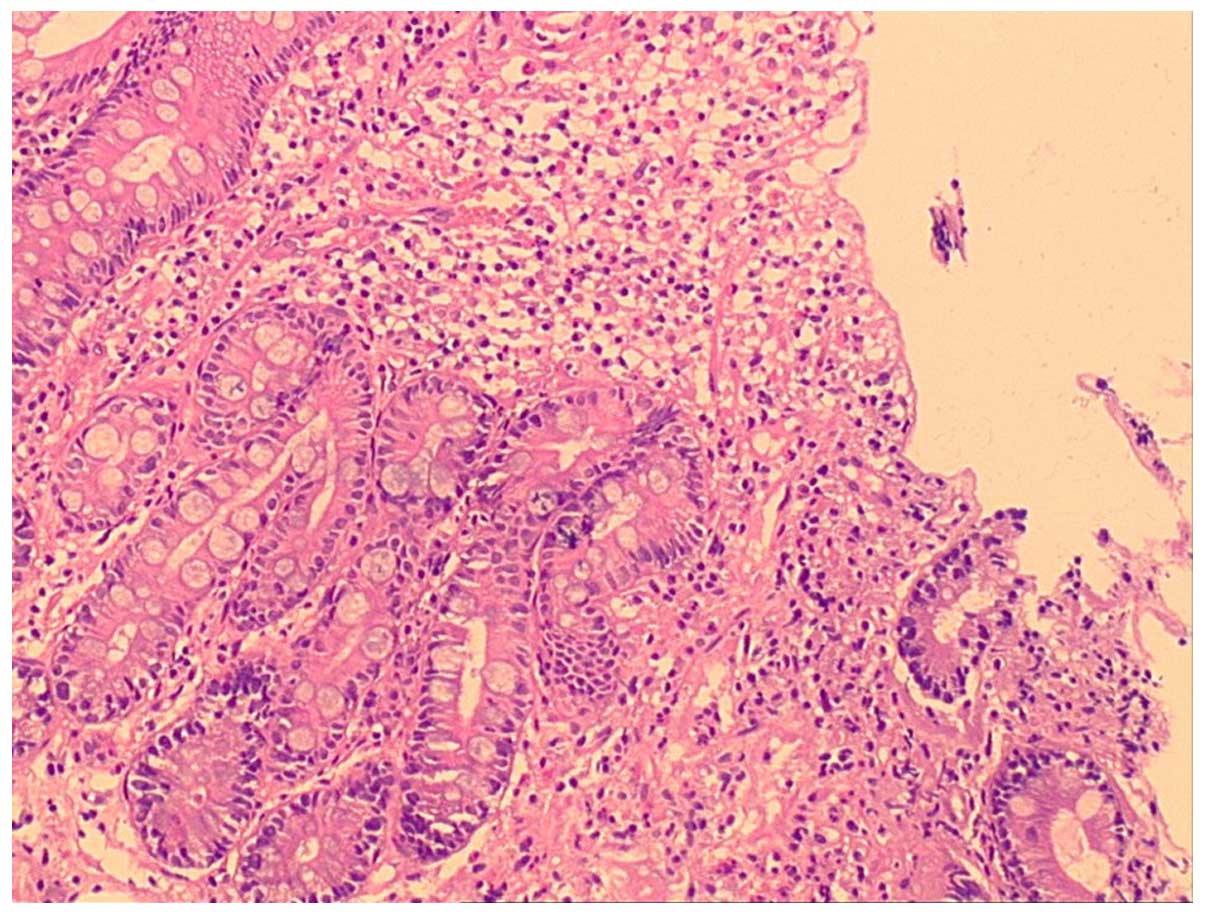
Gastric biopsy revealed an epithelial coating, with visible
effusion on the surface and diffuse infiltration of glands with
atypical hyperplasia. Solid cell nests and single scattered cells
were observed, as well as tumor cells infiltrating through the
muscularis, which conformed with moderately differentiated
adenocarcinoma of the gastric body (with a small number of cells
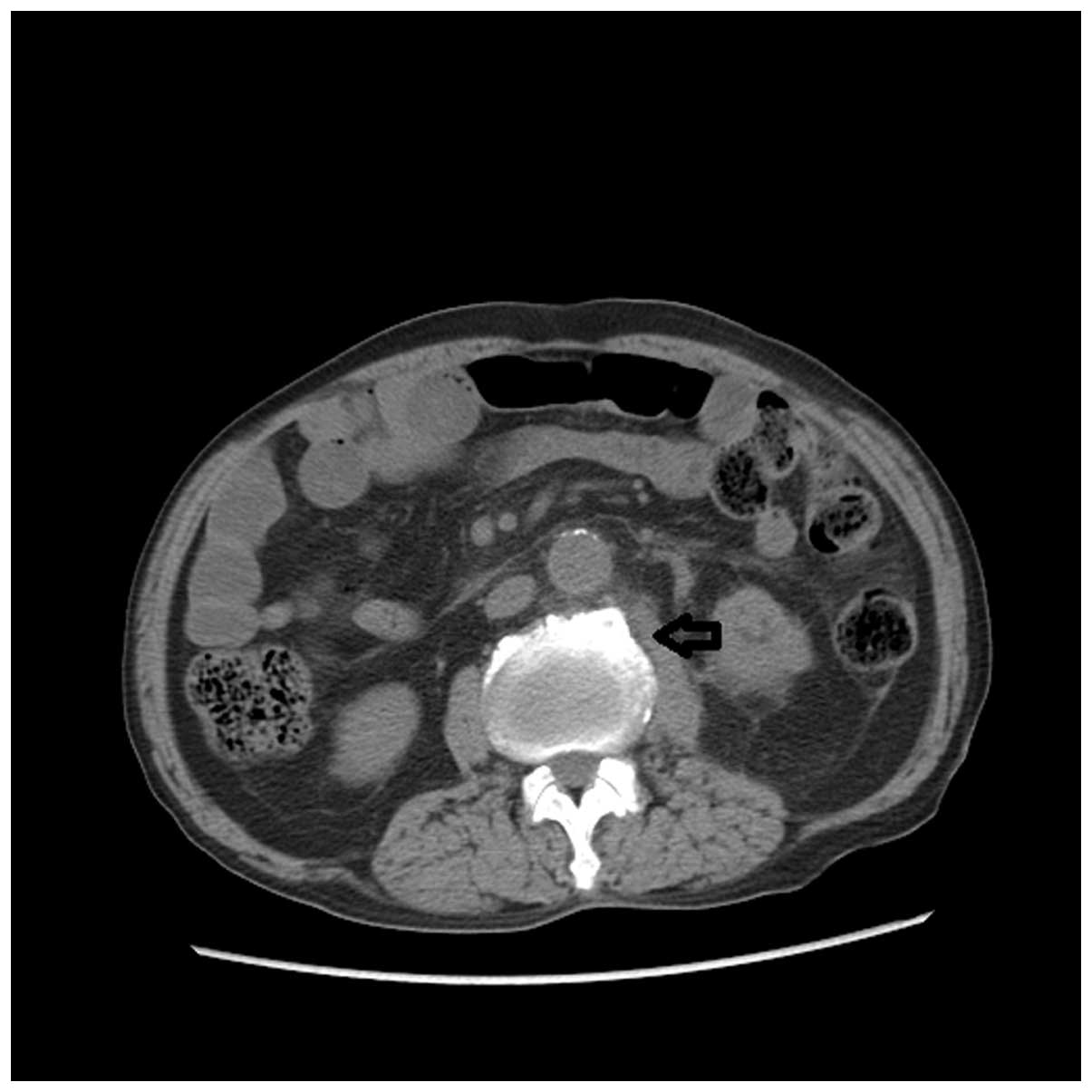
having neuroendocrine differentiation; Fig. 2). A paravertebral mass was visible in
abdominal computed tomography (CT), abdominal ultrasound and
abdominal magnetic resonance imaging. Abdominal CT revealed a
crumby mass with soft tissue density on the left of the 3–4 lumbar
vertebra and abdominal aorta (Fig.
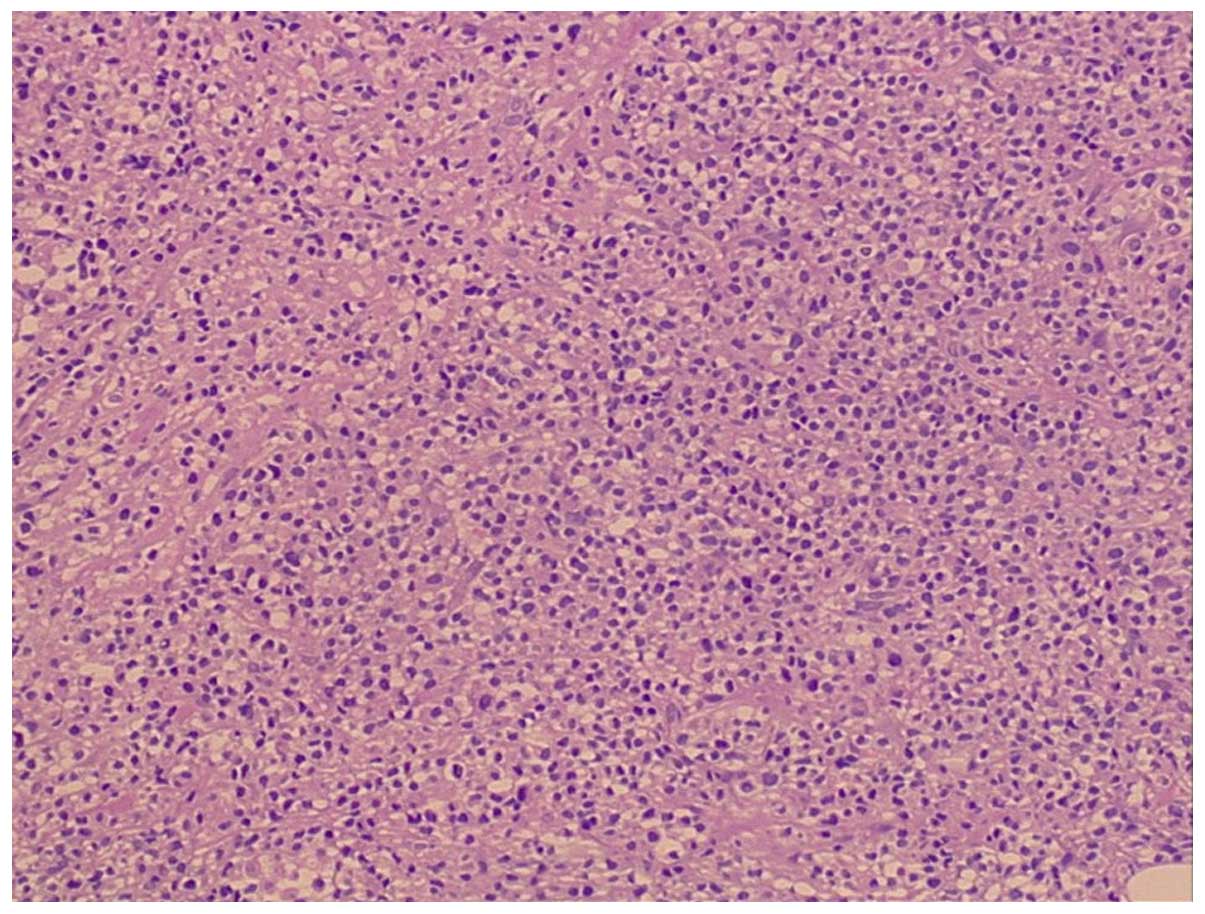
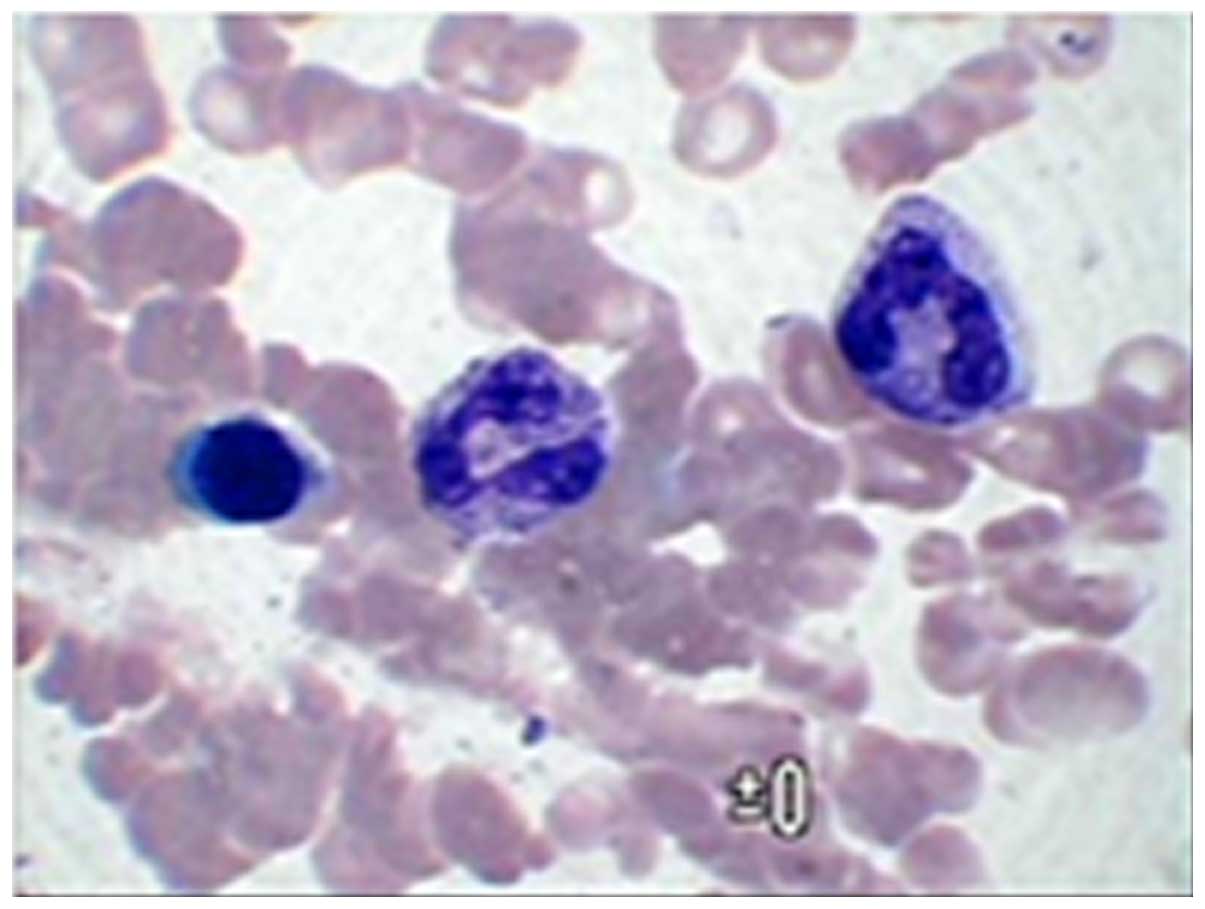
3). Biopsy of the paravertebral mass revealed proliferation and
infiltration of a large number of plasmocytes in adipose fiber
connective tissue (Fig. 4). The
plasma cells had extensive basophilic cytoplasms, and round
eccentric nuclei with pleomorphism. Immunohistochemical staining
revealed that the plasma cells were negative for CD20, CD21, CD3,
CD10, CD30, Bcl-6, Igλ, CK and EMA. The plasma cells were positive
for D138, mum1 and Igκ. The positive rate of Ki-67 was 80%. A bone
marrow biopsy was performed, and no excess plasma cells were
observed (Fig. 5). The histology and
immunohistochemical staining results supported the diagnosis of
EMP.
Treatment
The patient refused surgery. After signing the
informed consent form, radiotherapy was administered to the patient
to treat paravertebral plasmacytoma. Four cycles of oxaliplatin
(200 mg, day 1; Cenexi, Fontenay-sous-Bois, France) plus tegafur,
gimeracil and oteracil potassium capsules (40 mg, days 1–14; Taiho
Pharmaceutical Co., Ltd., Tokyo, Japan) and zoledronate (Novartis
Pharma Schweiz AG, Risch-Rotkreuz, Switzerland) were administered.
The patient responded well to radiation and chemotherapy, and
remains healthy with no evidence of tumor recurrence or secondary
neoplasms one year after the initial diagnosis.
Discussion
The diagnosis and treatment process of this patient
raises two key issues. Firstly, the early clinical symptoms are not
typical; this may lead to misdiagnosis, although comprehensive
diagnosis methods (combining imageology with pathology) are able to
improve the diagnostic accuracy. Secondly, surgery is the most
effective treatment if the conditions allow this. It is useful to
combine local radiotherapy with chemotherapy when surgery cannot be
performed. In addition, local radiotherapy may be of particular
significance.
Plasmacytoma may be classified as multiple myeloma,
solitary plasmacytoma, EMP or plasma cell leukemia. More than 95%
of these tumors are multiple myelomas (10). The incidence of EMP is extremely low,
accounting for just 3% of all plasmacytomas; 80% of these occur in
the upper respiratory or digestive tract (1). Therefore, our case of EMP concurrent
with another type of malignant tumor was rare. Makis et al
(11) reported a case of gastric and
mesenteric plasmacytoma occurring following surgery for colonic
carcinoma. However, the two carcinoma types did not exist at the
same time in this case. Early diagnosis is difficult due to its
unclear and non-specific early clinical symptoms, and misdiagnosis
and missed diagnosis occur frequently. Our patient suffered with
irregular abdominal pain for several months, which could be
diagnosed easily as gastric carcinoma through gastroscopy and
pathology. However, the diagnosis of paravertebral plasmacytoma is
difficult. Domestic diagnostic criteria of EMP is not yet
available. However, the key points of clinical diagnosis may be
summarized as follows: i) An extramedullary lump comprised of
single monoclonal plasma cells; ii) a normal histological bone
marrow test result to eliminate multiple myeloma; iii) a normal
bone check including long bone imageological examination to exclude
isolated plasmacytoma of the bone; iv) no anemia, hypercalcemia or
renal insufficiency caused by plasma cell disease; and v) a
deficient or low level of monoclonal immunoglobulin in the serum or
urine (12). Scott et al
(13) proposed that it was essential
to check the monoclonal immunoglobulin level in serum or urine for
EMP. Following auxiliary examinations, the paravertebral mass of
our patients was observed to be largely in line with the above key
points of diagnosis summarized above.
To date, there is no standardized treatment for EMP.
Alexiou et al (14) observed
that the relapse-free survival time following comprehensive
treatment (radiotherapy plus surgery), radiation therapy alone, and
surgery alone were 300, 144 and 156 months, respectively, by
retrospectively clinical control study. The difference of
statistical analysis (P<0.05) was statistically significant.
Alexiou et al summarized their experience and noted that
surgical resection was the first choice of treatment where
feasible. Radiation and chemotherapy may be administered to
patients with metastasis or surgical contraindication. Dimopoulos
et al (15) observed that
sensitivity to radiotherapy is much higher than that to
chemotherapy, and that fewer side effects are involved in
plasmacytoma of the head and neck. The prognosis of EMP is not bad.
Studies have revealed that the ten-year disease-free survival rate
of EMP is ~70% (16). The incidence
of EMP progressing to multiple myeloma within 10 years was 11–30%
(17). Therefore, preventing the
possibility of EMP leading to multiple myeloma following treatment
is one of the key factors in improving the prognosis. Avilés et
al (17) suggested that the
majority of patients treated with adequate radiation therapy alone
are likely to develop multiple myeloma within the first three years
after diagnosis and treatment. Radiation therapy alone may induce
certain unknown side effects which should be paid attention.
In conclusion, there are few, if any, studies in the
literature describing gastric adenocarcinoma concurrent with
paravertebral plasmacytoma. Publishing our case may aid in the
recognition of this rare disease, thus avoiding misdiagnosis and
inadequate treatment.
Acknowledgements
The present study was supported by the National
Natural Science Foundation of China (grant no. 81071758), Shandong
Science and Technology Development Project (grant no.
2015GSF118142), the Natural Science Foundation of Shandong Province
Joint Programme (grant no. ZR2015HL069) and Yantai Yuhuangding
Hospital Initiative Foundation for Young Scientist (grant no.
201402).
Glossary
Abbreviations
Abbreviations:
|
EMP
|
extramedullary plasmacytoma
|
References
|
1
|
Doki T, Takeuchi O, Kaiho T, Tsuchiya S,
Matsuzaki O and Miyazaki M: Primary isolated extramedullary
plasmacytoma of the colon. Int J Colorectal Dis. 23:719–720. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ooi GC, Chim JC, Au WY and Khong PL:
Radiologic manifestations of primary solitary extramedullary and
multiple solitary plasmacytomas. AJR Am J Roentgenol. 186:821–827.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Luh SP, Lai YS, Tsai CH and Tsao TC:
Extramedullary plasmacytoma (EMP): Report of a case manifested as a
mediastinal mass and multiple pulmonary nodules and review of
literature. World J Surg Oncol. 5:1232007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Nakayama K, Okada D and Koizumi K:
Excision of extramedullary plasmacytoma in a hilar lymph node.
Japan J Lung Cancer. 46:723–726. 2006. View Article : Google Scholar
|
|
5
|
Bertolami A, Henriques AC and Penha FG:
Plasmocitoma extramedular. Arq Med ABC. 30:58–60. 2005.
|
|
6
|
Galieni P, Cavo M, Pulsoni A, Avvisati G,
Bigazzi C, Neri S, Caliceti U, Benni M, Ronconi S and Lauria F:
Clinical outcome of extramedullary plasmacytoma. Haematologica.
85:47–51. 2000.PubMed/NCBI
|
|
7
|
Lee SY, Kim JH, Shin JS, Shin C, In KH,
Kang KH and Yoo SH: A case of extramedullary plasmacytoma arising
from the posterior mediastinum. Korean J Intern Med. 20:173–176.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ching AS, Khoo JB and Chong VF: CT and MR
imaging of solitary extramedullary plasmacytoma of the nasal tract.
AJNR Am J Neuroradiol. 23:1632–1636. 2002.PubMed/NCBI
|
|
9
|
Ferrari S, Tecchio C, Turri G, Richelli S,
Ghimenton C, Monaco S and Todeschini G: Unusual case of solitary
intraparenchymal brain plasmacytoma. J Clin Oncol. 30:e350–e352.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lee HY, Kim JI and Kim KN: Solitary
plasmacytoma of the rib. Korean J Thorac Cardiovasc Surg.
45:269–271. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Makis W, Ciarallo A, Hickeson M and
Lisbona R: Gastric recurrence of a primary colon plasmacytoma:
staging and evaluating response to therapy with 18F-FDG PET/CT. Br
J Radiol. 85:e4–e9. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Soutar R, Lucraft H, Jackson G, Reece A,
Bird J, Low E and Samson D: Guidelines Working Group of the UK
Myeloma Forum; British Committee for Standards in Haematology;
British Society for Haematology: Guidelines on the diagnosis and
management of solitary plasmacytoma of bone and solitary
extramedullary plasmacytoma. Br J Haematol. 124:717–726. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Scott FE, Dupont PA and Webb J:
Plasmacytoma of the stomach: diagnosis with the aid of
immunoperoxidase technique. Cancer. 41:675–681. 1978. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Alexiou C, Kau RJ, Dietzfelbinger H,
Kremer M, Spiess JC, Schratzenstaller B and Arnold W:
Extramedullary plasmacytoma: tumor occurrence and therapeutic
concepts. Cancer. 85:2305–2314. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Dimopoulos MA and Hamilos G: Solitary bone
plasmacytoma and extramedullary plasmacytoma. Curr Treat Options
Oncol. 3:255–259. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Dimopoulos MA, Kiamouris C and Moulopoulos
LA: Solitary plasmacytoma of bone and extramedullary plasmacytoma.
Hematol Oncol Clin North Am. 13:1249–1257. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Avilés A, Huerta-Guzmán J, Delgado S,
Fernández A and Díaz-Maqueo JC: Improved outcome in solitary bone
plasmacytoma with combined therapy. Haematol Oncol. 14:111–117.
1996. View Article : Google Scholar
|