Introduction
Cervical cancer is the leading cause of mortality in
women, with the highest mortality of all gynecologic tumors
(1). World Health Organisation (WHO)
has admitted that as many as 529,409 women worldwide are likely to
be diagnosed with cervical cancer, and 274,883 are likely to
succumb to the disease. No less than 80% of this burden is borne in
less developed countries (1). In
America, it is estimated that there are approximately 92,136 cases
and 37,640 mortalities annually, representing a significant
economic loss, projected at being potentially greater than US $ 3,6
billion (2). It takes approximately
5–10 years for cervical intraepithelial neoplasia (CIN) to develop
into cervical cancer and the progression of disease has
reversibility. If CIN is screened out and treated timely and
completely, a lesion may disappear or develop into cancer (3). Therefore, the key for solving this
problem lies in effective screening, which is also the best way to
prevent and control cervical cancer to a large extent. The
sensitivity of ThinPrep cytology test (TCT) detection is only
55–80% and HPV, although has the highest sensitivity, has very poor
specificity. Thus, a safe, effective and joint detection method for
the early diagnosis of cervical cancer should be identified.
Three-dimensional (3D) color power Doppler may provide an invasive,
real-time, objective and overall assessment on the blood supply
condition of patients, thus, it is an ideal technology for the
evaluation of the blood supply of cervical lesions (4). In this investigation, we have taken
pathology diagnosis as the golden standard to determine the
application value of three-dimensional color power angiography
(3D-CPA), high-risk human papillomavirus (HR-HPV), and TCT joint
detection.
Patients and methods
Patients
A total of 1,900 patients that were examined at the
Gynecological and Cervix Clinic of Maternal and Child Care Service
Center of Xuzhou (Jiangsu, China) from June 2012 to March 2015 were
enrolled in our study. The patients were aged 20–65 years, with an
average of 35.5±4.6 years. The inclusion criteria for the present
study was patients without history of medical application on
vagina, cervical precancerous lesions or conization of cervix in
the previous week. Patients in the menstrual or gestation period
were excluded. TCT, HR-HPV and 3D-CPA examinations were performed
and vascular morphology and typing, vascularization index (VI) were
recorded. Colposcopy biopsy was performed in patients with a
positive outcome of any of the three indices. Pathological
diagnosis was taken as the golden standard for assessment. The
patients enrolled were required to fill a case report form and
provide written informed consent. The study was approved by the
Ethics Committee of Maternal and Child Care Service Center of
Xuzhou.
Sample collection
Cells were collected from the cervical canal via
TCT, and HPV cervix brush, and the brush was placed into preserving
fluid for examination. The collected samples were preserved at 4°C
for ≤3 days. Abnormal secretion of menstruation and vagina was
avoided while drawing samples.
Instruments
GE Voluson E8 color Doppler ultrasonic diagnostic
apparatus (General Electric, Schenectady, NY, USA), intracavitary
probe, 5–9 MHz was applied. Virtual organ computer-aided analysis
(VOCAL) software was utilized to measure relevant vascular
parameter values. Pulse repetition frequency (PRF) of 0.9 was
selected, three-dimensional quantification sampling was set at high
quality, a section was selected every 15°C, and a total of 12
sections was selected from each lesion. Envelope path of the
lesions were drawn manually.
3D power Doppler ultrasonography
examination
First, we performed regular transvaginal 2D
ultrasound examination on cervix under the grayscale mode and
closely examined the properties of tumor in patients with lesions.
For the patients diagnosed with obvious tumor in the cervix by
ultrasonic examination, the tumor was taken as the region of
interest. For the patients diagnosed without tumor in the cervix,
the whole cervix was taken as the region of interest and screening
was performed. Subsequently, the examination was switched to color
power Doppler mode and 3D reconstruction was performed on the
region of interest, 3D distribution and branch of cervical vessels
were exhibited and typing of the vessels was observed. The typing
standard for vessels under ultrasonography (1) included: type I vessels, vessels that
were uniformly distributed, thin, and straight; type II vessels,
vessels that had annular thickening locally; type III vessel,
vessels that were disorderly and unsystematic locally and had a
large number of branches; and type IV vessel, vessels that were
non-uniform, distortedly clustered in the shape of a fire ball.
Manual outlining sampling method and 3D power
Doppler histogram were used for quantitative analysis on the
vessels and blood flow volume. The parameters obtained were: VI
measured the number of color information in the region of interest
and showed the number of vessels detected inside tissues, and
examination on each patient was completed by the same sonographer
using the same diasonograph and the same environment. A VI cut-off
value of ≥3 was defined as positive.
HPV-DNA detection and diagnostic
criteria
HPV typing method - Hybribio medical nucleic acid
molecule hybridization technique and its reagents (introduced from
HybriBio, Hong Kong, China) were applied to typing and detect the
21 common HPV genotypes including 15 types of HR-HPV (16, 18, 31,
33, 35, 39, 45, 51, 52, 53, 56, 58, 59, 66 and 68) and 6 types of
low-risk types (6, 11, 42, 43, 44 and 8304). A positive result of
any of the high-risk types was viewed as positive.
Multiple cervix punch biopsy under
colposcope and endocervical canal curettage (ECC)
Colposcopic biopsy was performed in patients with a
positive outcome of any of the above three indices. For the
patients that had abnormal lesions, samples were collected from the
site of the lesion. For the patients that had no abnormal lesion,
the samples were collected from sites 3, 6, 9 and 12 in the
transformation zone. Furthermore, ECC was performed and the biopsy
tissues sent for pathological examination. According to the degree
of lesion, the lesions in chronic cervicitis were divided into low
level CIN (CINI), high level CIN (CINII-CINIII glandular
involvement), and cervical cancer. Histology of more than low level
CIN was defined as positive.
Statistical analysis
SPSS 17.0 software (SPSS Inc., Chicago, USA) was
applied for statistical analysis. Based on the χ2 test
and the golden standard of pathology, the sensitivity, specificity,
diagnostic rate and Youden index of the three indices under
independent or united screening were computed.
Results
HR-HPV, TCT and 3D-CPA
The VI detection results showed that of the 1,900
patients, 276 cases (14.53%) were confirmed HR-HPV-positive, 214
cases (11.26%) VI-positive, and 164 cases (8.63%) TCT-positive.
Results of biopsy under colposcopic
and pathologic biopsy
A total of 418 cases were confirmed with a positive
outcome of any of the three indices and a cervical biopsy was
obtained. Of these, 162 cases (38.75%) were diagnosed with chronic
cervicitis, 146 cases with low-level CIN (34.93%), 104 cases
(24.88%) with high level CIN, and 6 cases (1.44%) with cervical
cancer. Histology of more than low level CIN was defined as
positive.
Comparison on the positive rate and
pathological coincidence rate of HR-HPV and TCT
Of the 1,900 cases, 276 cases were confirmed with
high-risk HPV infection, the positive rate being 14.52% and
pathological coincidence rate 37.68%. However, the HR-HPV-positive
rate in high level CIN or above was 95.45% (105/110). Cases (164)
were confirmed as TCT-positive, at 8.63% and the pathological
coincidence rate was 82.93% (136/164) (Table I).
 | Table I.Comparison of the positive rate and
pathological coincidence rate between TCT and HPV. |
Table I.
Comparison of the positive rate and
pathological coincidence rate between TCT and HPV.
|
|
| Pathological
results |
|
|---|
|
|
|
|
|
|---|
| TCT cases | N | Inflammation | CINI | High level CIN | Ca | Pathological
coincidence rate with ≥ high level CIN, n/total (%) |
|---|
| ASCUS | 102 | 26 | 33 | 42 | 1 | 42/102 (41.18) |
| LSIL | 26 | 2 | 9 | 14 | 1 | 14/26 (53.85) |
| HSIL | 35 | 0 | 4 | 28 | 3 | 28/35 (80.00) |
| SCC | 1 | 0 | 0 | 0 | 1 |
| High risk HPV | 276 | 44 | 128 | 98 | 6 | 98/276 (35.51) |
Pathological diagnosis was taken as the golden
standard for the sole and joint assessment of the sensitivity,
specificity, diagnostic rate, Youden index of HPV, TCT and VI on
lesions more than CINI (Table
II).
 | Table II.Diagnostic efficiency of sole and
joint screening of the three indexes on lesions more than CINI. |
Table II.
Diagnostic efficiency of sole and
joint screening of the three indexes on lesions more than CINI.
| Index | Sensitivity | Specificity | Diagnostic
coincidence rate | Youden index |
|---|
| VI | 73.44% (188/256) | 83.95% (136/162) | 77.51% (324/418) | 0.574 |
| HPV | 90.63% (232/256) | 72.84% (118/162) | 83.73% (350/418) | 0.635 |
| TCT | 53.13% (136/256) | 79.01% (134/162) | 63.16% (264/418) | 0.321 |
| HPV+TCT | 92.19% (236/256) | 76.54% (124/162) | 86.12% (360/418) | 0.687 |
| HPV+TCT+VI | 94.53% (242/256) | 81.48% (132/162) | 89.47% (374/418) | 0.760 |
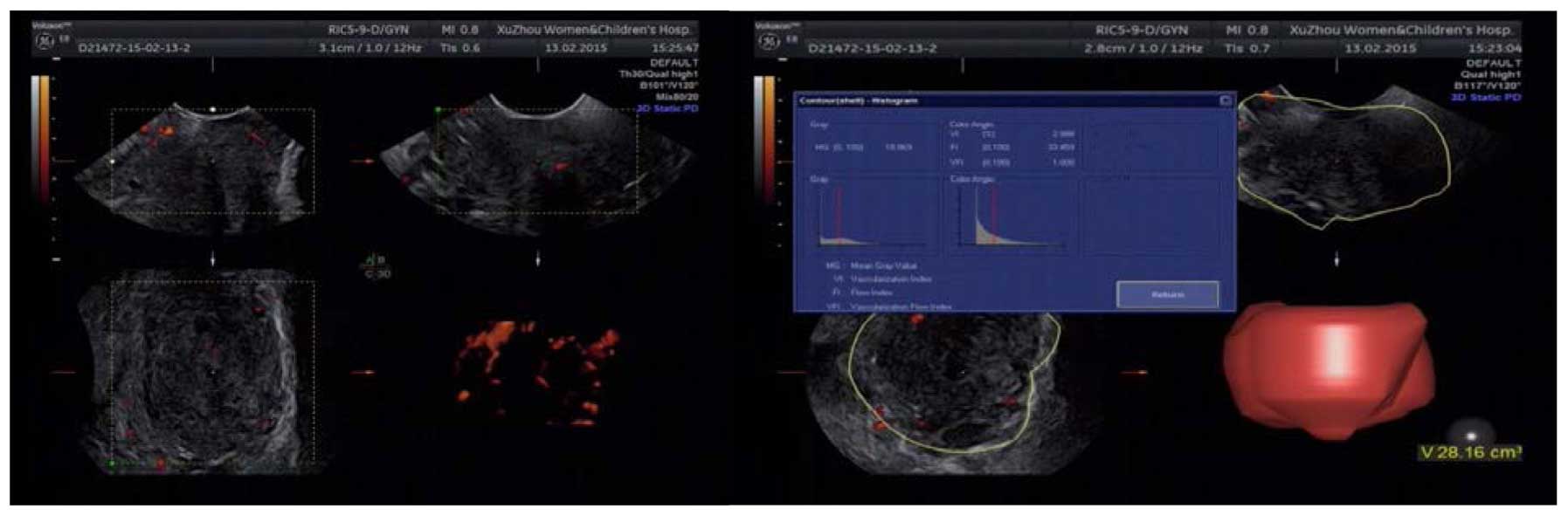
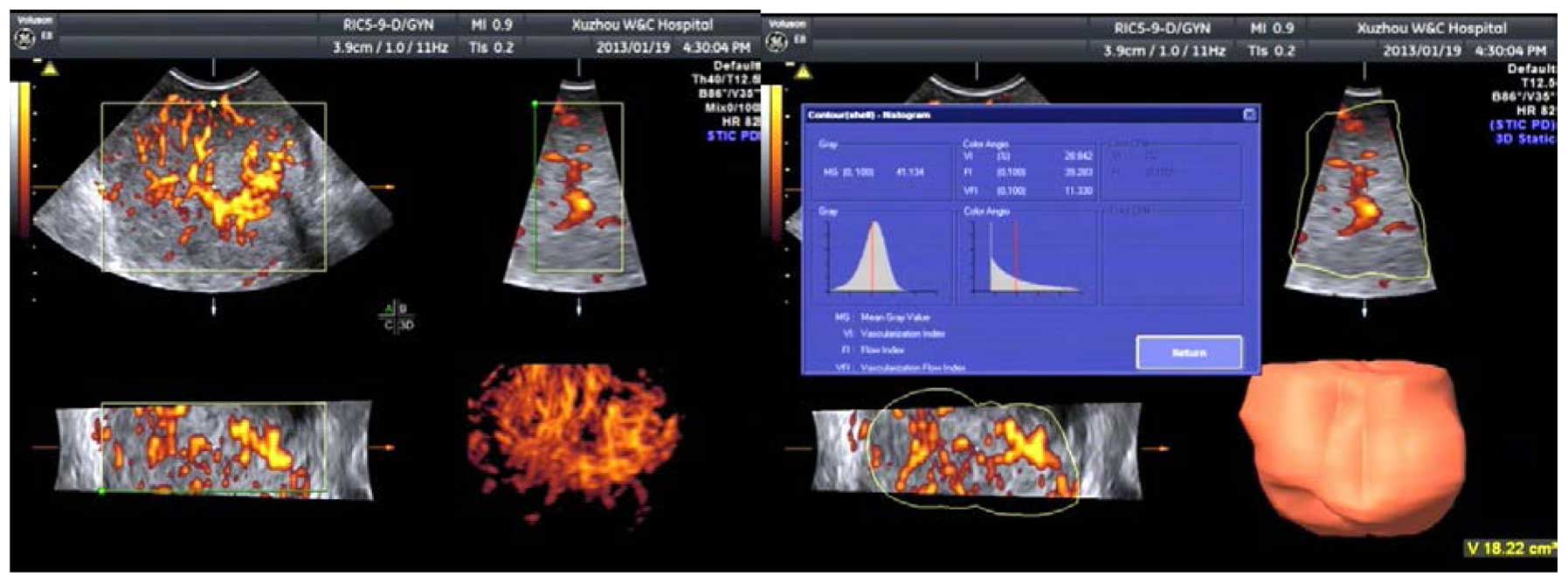
Cervical ultrasonography and vascular
typing
Results from the chronic cervicitis and CINI groups
indicated that the difference on blood flow of cervix between
chronic cervicitis and CINI was not significant. Cervical blood
flow was not rich and blood flow signals were few. Type I
dominated, accounting for 81.48% constituted the high level CIN
group, in which blood flow was relatively rich in some regions of
the cervix, and strip or ‘short rod-like’ vessels were evident.
Type II dominated, accounting for 71.15% constituted the early
stage cervical carcinoma group, in which cervical blood flow was
rich, mussy, and distorted, in the form of fire balls. Type III
dominated and type IV accounted for 66.67% (Figs. 1–3;
Table III).
 | Table III.Vascular typing characteristics of
cervical cancer, high level CIN and control groups. |
Table III.
Vascular typing characteristics of
cervical cancer, high level CIN and control groups.
| Group | Case | Type I | Type II | Type III | Type IV |
|---|
| Cervical cancer | 6 |
0 | 0 | 2 | 4 |
| High level CIN | 104 | 16 | 74 | 14 | 0 |
| Cervicitis | 162 | 132 | 28 | 2 | 0 |
Discussion
Clinical samples have shown that the 5-year survival
rate of patients at the early stage of cervical cancer may reach up
to 80–90% if they diagnosed and treated in a timely manner
(1,2).
Therefore, a timely and effective screening of precancerous lesions
and early stage cervical cancer has become the key for preventing
and treating cervical cancer and reducing mortality (5). Present cervical cancer screening methods
used mainly include exfoliate cytology examination (Pap smear,
Thinprep Cytologic Test, TCT), HPV detection (HCII, HR-HPV typing),
and cytology and HPV detection (6).
These are convenient procedures involving simple operation, high
smear collection and a high detection rate of abnormal cervical
cells, which have made TCT the most important method for the
screening of cervical lesions, which plays a significant role in
the screening of cervical cancer (5,6). However,
TCT detection is greatly affected by subjective factors. For the
same smear, different cytological experts may have different film
reading results. It may be because diagnosis was made on the basis
of cytological morphological characteristics, lacking the
assessment of histological characteristics, thus increasing the
rate of misdiagnosis. Normally, the sensitivity of TCT detection is
55–80%. Once abnormal cells are discovered, its specificity reaches
90%. We showed that TCT has sensitivity of 53.13%, specificity of
79.01%, and a pathological coincidence rate of 82.93%, which again
proved that TCT had better specificity.
At present, it has been acknowledged that persistent
high-risk HPV infection is the fundamental pathogenic factor for
cervical cancer (7). Thus, HPV is
important in the early detection, treatment and follow-up of
cervical lesions. Recent literature has shown that single HPV
detection is the essential condition rather than the sufficient
condition for cervical cancer (7).
HPV inspection has a high sensitivity and poor specificity. Our
study results showed that when HPV screening was performed
independently, its sensitivity was 90.63%, specificity was 72.84%,
and the diagnostic coincidence rate was 83.73%, whereas the
diagnostic coincidence rate with high level CIN was only 37.68%.
Since most HPV-positive patients may become HPV-negative and the
lesions would not develop into cervical lesions, such a result
would undoubtedly aggravate seeking medical assistance and lead to
a series of unnecessary examinations and treatments. HPV detection
is considered significant for condensing the high-risk patients,
distributing the ASCUS and LSIL of undetermined significance, and
monitoring the precancerous lesions as well as the conditions
following treatment (8–10). Sensitivity of HPV detection is
extremely high; however, the false-positive rate is also extremely
high. It may be just a virus infection, and not necessarily the
results of cervical cytological and pathological changes. Thus, a
safe and effective joint detection method for early diagnosis of
cervical cancer should be identified.
Our data showed that HPV infection was 16, 58, 52,
33, 31 and 18 from high to low. HPV16(+) accounted for 83.33% (5/6)
in the cervical cancer group, for 56.12% (55/98) in the high level
CIN group, and for 25% (32/128) in the CINI group. These results
further confirmed that HPV16 had the highest carcinogenicity, thus
requiring the most serious screening and management. HPV18 was
rarely seen in our data.
Previous studies have confirmed from the molecular
level that angiogenesis is important in the occurrence and
development of cervical cancer, and suggested treating angiogenesis
as an independent factor for the diagnosis of cervical cancer
(6,8).
Microvessel density (MVD) may reflect angiogenesis activity
(11). It has been used as the gold
standard to assess the state of angiogenesis. However, the blood
vessel density measured by immunohistochemistry is changeable,
unable to provide an overall blood supply information of tumor, or
guide the decision of therapeutic regimen (12). Thus, a more favorable proxy indicator
that is safe, non-invasive, and well-correlated with MVD and that
could express the vascular condition of tumor should be identified.
3D-CPA technology is newly developed and has combined power of
Doppler mode and the 3D volume sampling mode. It was able to reveal
the vascular structures inside and around the tumor in a dynamic,
3D and all-round manner as well as the vascular trees inside the
tumor in an intuitive and complete manner. Being characterized for
relative independence, high sensitivity and repeatability, 3D-CPA
technology could detect the direction, distribution, and shape of
low blood perfusion of micro-vessels inside the tumor, thus
reflecting the blood supply condition of tumor. By means of VOCAL
software, 3D-CPA supports quantitative analysis on the vessels as
well as blood flow inside the tumor, which is conducive to a
qualitative diagnosis and treatment effect evaluation of the tumors
(9). 3D vascular parameters computed
from VOCAL includes VI, flow index (FI) and vascularization flow
index (VFI). VI was used to measure the number of color information
in the region of interest and show the number of vessels detected
inside tissues. As for the credibility of VI in assisting cervical
lesion detection, some literature has reported that 3D color power
Doppler's vascular tying and VI were correlated with the expression
of MVD and VEGF, which indicated that vascular typing and VI may
reflect the vascular expression of the tumor (10). Besides, the results of our previous
study also showed that, VI and VFI of the cervical cancer group
were significantly higher than those of the CIN and cervicitis
groups, and the difference was statistically significant
(P<0.05). Such a result confirmed that 3D color power Doppler
ultrasonography may reflect the blood supply state of cervix
objectively, providing important reference for the ultrasonic
diagnosis of early cervical cancer and CIN. Thus, it could be
confirmed that 3D color power Doppler ultrasonography was of great
application value (13). In the
present study, we performed a screening independently by VI and
obtained the following parameters: sensitivity, 73.44%;
specificity, 83.95%; and diagnostic coincidence rate, 77.51%.
Although sensitivity was relatively lower than HPV, its specificity
was higher. Notably, it was non-invasive, safe and had very good
repeatability.
A semi-quantitative analysis on the vessels and
blood flow in the area of cervical lesion of the early cervical
cancer, high level CIN, low level CIN and cervicitis groups was
performed. The results showed (Table
II) that the typing of cervical blood flow in the former three
groups were significantly different. The cervical cancer group had
rich blood flow, the volume of the cervix was enlarged and even out
of normal shape, the branches of vessels were complicated,
distorted and irregular, non-uniform, distortedly clustered in the
form of fire balls and was dominated by type III–IV, of which type
IV accounted for 66.67%. The blood flow in the chronic cervicitis
and low level CIN groups had no significant difference, indicating
that blood flow change in the early period of disease was not as
obvious. Thus, it was difficult to identify the mild lesion purely
through ultrasonic vessel typing; the cervical blood flow of the
cervicitis group was not rich and blood flow signals were few, with
type I dominated, accounting for 81.48%; blood flow in some regions
of the high level CIN group was quite rich, and strip or ‘short
rod-like’ vessels were evident, with type II dominated, accounting
for 71.15%, indicating that cervix had new vessels. Based on the
above analysis, we concluded that cervical vessels could reflect
the degree of cervical lesions more objectively, which combined
with VI, could provide more reliable evidence for the diagnosis and
identification of the high level CIN and early cervical cancer.
The American Cancer Society (ACS), American Society
of Colposcopy and Cervical Pathology (ASCCP) and American Society
for Clinical Pathology (ASCP) contended that the optimal strategy
for cervical cancer screening is to maximize the benefits of
screening while minimizing the potential hazards (14). The most commonly used methods for
cervical screening at present are TCT and HPV. The sensitivity of
TCT is low and extremely subjective while the specificity of HPV is
relatively low. To make the early diagnosis of cervical cancer more
accurate, reliable and predictive, there is a need for a reliable
index or method to assist the above detection methods for more
comprehensive judgment. In the present study, we have compared the
sensitivity, specificity, diagnostic rate, and Youden index of
individual 3D-CPA, HR-HPV, and TCT screening, HR-HPV+TCT screening,
3D-CPA+HR-HPV+TCT screening on cervical lesions. The results of the
present study show that the sensitivity of 3D-CPA+HR-HPV+TCT
screening reached 94.53%, and although its specificity was
relatively lower than that of the individual VI screening, it was
still higher than that of HR-HPV+TCT screening. Additionally, its
diagnostic coincidence rate reached 89.47%, which was the highest
rate, while the Youden index was also the highest, reaching up to
0.760. These results indicated that 3D-CPA+HR-HPV+TCT screening had
the best accuracy. Combined with the differences of cervical
high-level lesion and cervical cancer cervical blood flow typing,
the sensitivity of screening was further improved, which indicated
that 3D-CPAHR-HPV+TCT screening had extremely high clinical
application value.
In conclusion, by comparing the correlation between
3D-CPA, HR-HPV, TCT detection and clinical pathological outcomes,
we concluded that th ejoint detection of the three methods may
significantly improve the disease detection rate and screening
authenticity. The 3D-CPA technology can be used as an auxiliary
method for cervical cancer screening. However, since different
groups have different characteristics, the medical environment and
resources should be considered. Thus, the most effective screening
method for patients according to their clinical performances,
high-risk factors of lesion and personal economic conditions should
be identified, for improved contributions to the clinic.
References
|
1
|
Castellsagué X, de Sanjosé S, Aguado T,
Louie L..Bruni KS, Muñoz J, Diaz M, Irwin K, Gacic M, Beauvais O,
et al: HPV and Cervical Cancer in the World 2007 Report.
25:2007.http://www.hpvcentre.net/link_media/HPVReport2007.pdf
|
|
2
|
PAHO publication: Estrategia y Plan de
Acción Regionales sobre la Prevención y el Control del Cáncer
Cervicouterino. Washington DC: 2008.https://www.rho.org/files/PAHO_Regional_Strategy_2010_sp.pdf(In
Spanish).
|
|
3
|
Sherman SM, Moss E and Redman CW: The
invasive cervical cancer review: Psychological issues surrounding
disclosure. Cytopathol. 24:77–80. 2013. View Article : Google Scholar
|
|
4
|
Jiao G, Xu H and Ren L: The diagnostic
value of three-dimensional ultrasound in invasive cervical
tuberculosis. J Tongji Univ. 31:85–87. 2010.(Medical edition).
|
|
5
|
Johnston EI and Logani S: Cytologic
diagnosis of atypical squamous cells of undetermined significance
in perimenopausal and postmenopausal women: lessons learned from
human Papillomavirus DNA testing. Cancer. 111:160–165. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tjalma W, Van Marck E, Weyler J, Dirix L,
Van Daele A, Goovaerts G, Albertyn G and van Dam P: Quantification
and prognostic relevance of angiogenic parameters in invasive
cervical cancer. Br J Cancer. 78:170–174. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Meijer CJ, Snijders PJ and van den Brule
AJ: Screening for cervical cancer: Should we test for infection
with high-risk HPV? CMAJ. 163:535–538. 2000.PubMed/NCBI
|
|
8
|
Landt S, Mordelt K, Schwidde I, Barinoff
J, Korlach S, Stöblen F, Lichtenegger W, Sehouli J and Kümmel S:
Prognostic significance of the angiogenic factors angiogenin,
endoglin and endostatin in cervical cancer. Anticancer Res.
31:2651–2655. 2011.PubMed/NCBI
|
|
9
|
Pairleitner H, Steiner H, Hasenoehrl G and
Staudach A: Three-dimensional power Doppler sonography: imaging and
quantifying blood flow and vascularization. Ultrasound Obstet
Gynecol. 14:139–143. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Li P, Wang X and Zhang Y: Correlation
between the blood flow of cervical cancer and MVD, VEGF under
three-dimensional energy doppler ultrasound detection. J China Med
Univ. 38:8462009.
|
|
11
|
Weidner N, Semple JP, Welch WR and Folkman
J: Tumor angiogenesis and metastases correlation in invasive breast
carcinoma. N Engl J Med. 324:1–8. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hsu KF, Su JM, Huang SC, Cheng YM, Kang
CY, Shen MR, Chang FM and Chou CY: Three-dimensional power Doppler
imaging of early-stage cervical cancer. Ultrasound Obstet Gynecol.
24:664–671. 2004. View
Article : Google Scholar : PubMed/NCBI
|
|
13
|
Liang H, Fu-Min L, Lei S, Peng L and Jian
Z: Transvaginal three-dimensional color power Doppler ultrasound
and cervical MVD measurement in the detection of cervical
intraepithelial neoplasia. Eur Rev Med Pharmacol Sci. 18:1979–1984.
2014.PubMed/NCBI
|
|
14
|
Saslow D, Castle PE, Cox JT, Davey DD,
Einstein MH, Ferris DG, Goldie SJ, Harper DM, Kinney W, Moscicki
AB, et al: American Cancer Society Guideline for human
papillomavirus (HPV) vaccine use to prevent cervical cancer and its
precursors. CA Cancer J Clin. 57:7–28. 2007. View Article : Google Scholar : PubMed/NCBI
|