Introduction
Hepatocellular carcinoma (HCC) is one of the most
common types of primary cancer worldwide, with an estimated
incidence of ~23,000 mortalities from liver or intrahepatic bile
duct cancer (1). The primary
treatment strategy for HCC is resection or liver transplantation;
however, only a minority of patients present with resectable
disease. Although advances in the treatment of HCC have resulted in
prolonged survival of patients, the incidence of recurrence or
extrahepatic metastasis associated with HCC has also risen
(2). This aggressive cancer has a
high recurrence rate, predominantly in the residual liver following
hepatectomy. The recurrence rate following resection is 50% at 2
years and 75% at 5 years (3). The
incidence of extrahepatic recurrence of HCC has been reported to be
14.0–25.8% (4). Patients with
extrahepatic metastasis have a poor prognosis. Current managements
for these patients are oral administration of sorafenib and
possibly transarterial chemoembolization for the hepatic tumors if
the patient has sufficient remaining liver function (5). The most frequent metastatic sites are
the lungs, lymph nodes, bones and adrenal glands (6). Metastases in the mediastinum are rare,
particularly under the arch of the aorta. The present study reports
the case of a patient presenting with hoarseness caused by lymph
node metastasis of HCC under the arch of aorta.
Case report
A 30-year-old male patient who presented with
hoarseness and back pain for 2 months was admitted to the
Department of Hepatopancreatobiliary Surgery, The Affiliated Tumor
Hospital of Xinjiang Medical University (Urumqi, China) in August
2014. The patient had undergone right hepatic lobectomy for HCC 2
years before (in November 2013), and received transarterial
lipiodol (lipiodol plus doxorubicin and cisplatin)
chemoembolization 4 times one month after the resection in The
First Affiliated Hospital of Xinjiang Medical University (Urumqi,
China). A medical history revealed that the patient had been
diagnosed with hepatitis B 14 years prior to admission, and had
been undergoing treatment with entecavir (1 tablet/day) for 2 years
(since November 2011) at his local hospital. Physical examination
revealed enlarged, bilateral supraclavicular masses. The level of
α-fetoprotein in the blood was elevated to 25.75 ng/ml (normal
levels, <13.40 ng/ml), serum hepatitis B surface antigen was
positive and hepatitis B virus DNA levels were 1,640 copies/ml
(normal range, 5×102-5×107 copies/ml)
(7). All other laboratory test
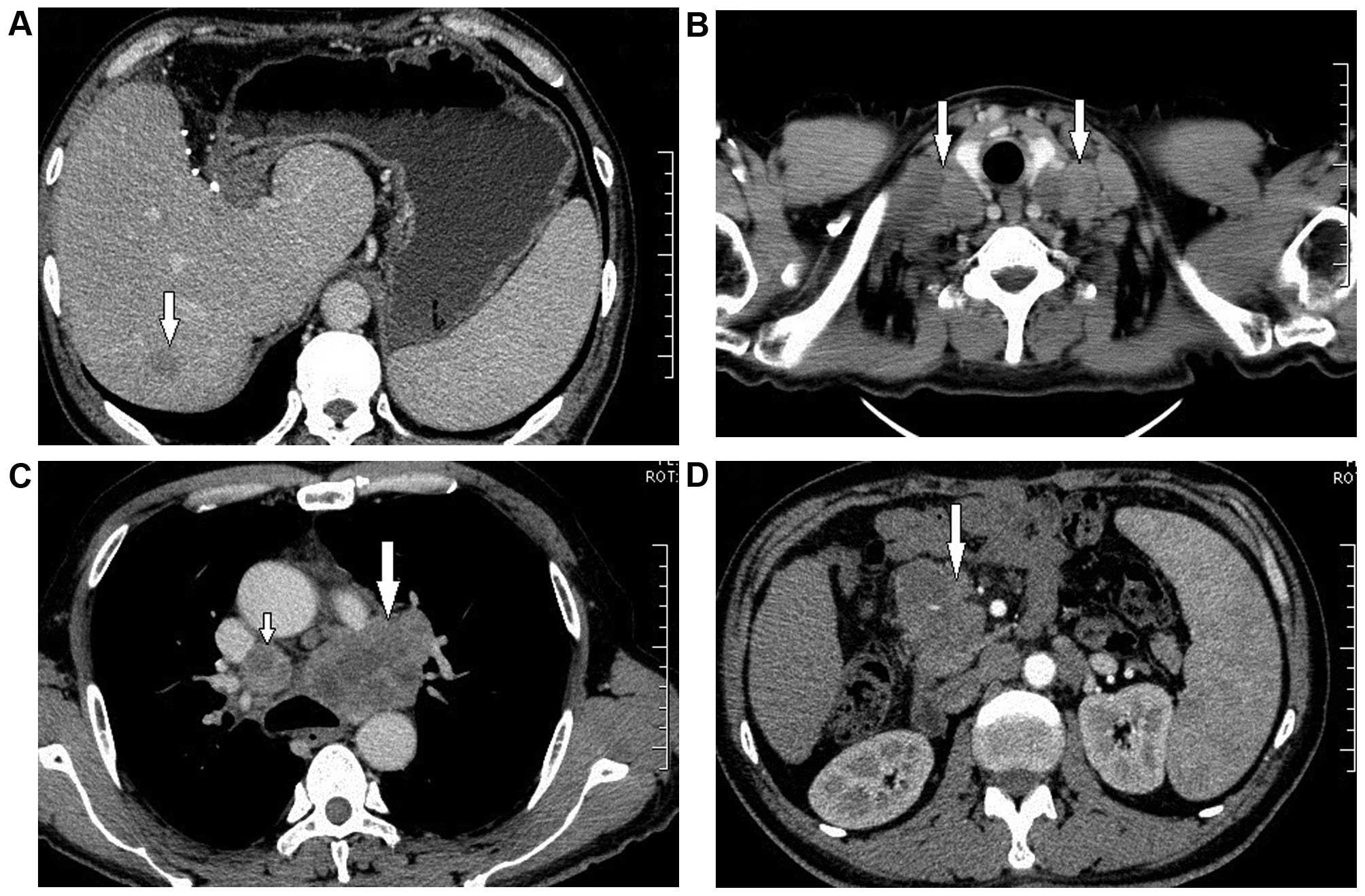
results were normal. A computed tomography scan of the chest and
upper abdomen showed intrahepatic recurrence, and multiple enlarged
lymph nodes in the bilateral clavicular regions, mediastinum and
peritoneum (Fig. 1). The enlarged
lymph node found under the arch of the aorta was considered to have
invaded the left recurrent laryngeal nerve, causing the hoarseness
(Fig. 1C). Percutaneous aspiration
biopsy of the enlarged, right supraclavicular lymph node identified
malignant cells consistent with HCC by hematoxylin and eosin
staining (Fig. 2). The multiple lymph
node metastases complicated with intrahepatic recurrence were
unsuitable for resection or radiofrequency ablation, but the
patient was administered radiotherapy (20 Gy/10 times) in October
2013); back pain was relieved as a result. However, despite the use
of recombinant human interleukin 11, the patient exhibited a
decrease in platelet count from 128×109 cells/l to
70×109 cells/l (normal range,
125×109-350×109 cells/l), which indicated
radiation intolerance. The patient refused sorafenib treatment on
cost grounds and was discharged from the hospital. The patient
succumbed to disease 4 months after radiotherapy. Written informed
consent was obtained from the patients wife for the publication of
the patients information.
Discussion
Lymph node metastasis of HCC is closely associated
with poor survival and a high risk of tumor recurrence. Although
cases with mediastinal lymph node metastasis of HCC have been
reported (8–11), to the best of our knowledge, the
present study describes the first case of hoarseness caused by
lymph node metastasis. In the present case, a pathological
examination of the enlarged, right supraclavicular lymph node
identified malignant cells consistent with HCC.
The treatment options for extrahepatic metastases
developing after hepatic resection of HCC are limited. Regional
lymph node dissection should always be performed to determine the
stage of the tumor. Hepatic resection with regional lymphadenectomy
is a safe procedure for patients with HCC (12), with a systematic review recommending
routine lymph node dissection in patients with HCC at the time of
resection (13). Experience suggests
that a solitary lymph node metastasis from HCC can be treated
surgically if there is no evidence of recurrence in other regions
(14). Radiofrequency ablation is
also effective and may be safely applied to retroperitoneal
metastatic HCC lymph nodes (15).
However, the majority of extrahepatic lymph node metastases of HCC
are multiple and are not suitable for resection or radiofrequency
ablation, as was the case with the present patient.
HCC is known as a radiosensitive tumor, and an
increasing number of reports underline the efficacy of radiotherapy
in the management of HCC (16–18);
however, the application of radiotherapy in patients with HCC is
limited due to the poor radiation tolerance of the normal liver to
local control doses and the varied locations of the tumors. Recent
improvements in radiation therapy delivery techniques have provided
novel tools to treat patients with extrahepatic metastasis.
Patients with intact liver function and without associated symptoms
were found to have the most favorable prognosis out of all patients
undergoing radiotherapy for lymph node metastasis from HCC
(19). In a previous study, a major
response to a radiation dose of ≥45 Gy was observed, with a
dose-response relationship determined for local control
radiotherapy (20). In the present
case, following the administration of 20 Gy radiation, the patient
presented with a decrease in platelet count, which indicated
radiation intolerance, despite relief of the symptom of pain
following treatment. Thus, stereotactic body radiation therapy
should be applied under strict conditions with the expertise of
radiation oncology departments.
Sorafenib has also been shown to be effective in the
treatment of patients with advanced or metastatic HCC (21,22);
however, it is only indicated for patients with well-preserved
liver function (Child-Pugh A class) and advanced stage tumors
(Barcelona Clinic Liver Cancer C) or tumors that progress upon
locoregional treatment (23,24). Despite well-preserved liver function,
the present patient refused to receive sorafenib therapy on cost
grounds.
In conclusion, the treatment options for
extrahepatic metastasis of HCC are limited. The provision of
careful follow-up and the control of extrahepatic recurrence
following treatment are important for improving the quality of life
and prognosis of HCC patients with extrahepatic metastases. Further
studies are required to develop standard treatments that achieve
this, including systemic adjuvant chemotherapy and
radiotherapy.
References
|
1
|
Siegel R, Ma J, Zou Z and Jemal A: Cancer
statistics, 2014. CA Cancer J Clin. 64:9–29. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kanda M, Tateishi R, Yoshida H, Sato T,
Masuzaki R, Ohki T, Imamura J, Goto T, Yoshida H, Hamamura K, et
al: Extrahepatic metastasis of hepatocellular carcinoma: Incidence
and risk factors. Liver Int. 28:1256–1263. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gluer AM, Cocco N, Laurence JM, Johnston
ES, Hollands MJ, Pleass HC, Richardson AJ and Lam VW: Systematic
review of actual 10-year survival following resection for
hepatocellular carcinoma. HPB (Oxford). 14:285–290. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Tanaka K, Shimada H, Matsuo K, Takeda K,
Nagano Y and Togo S: Clinical features of hepatocellular carcinoma
developing extrahepatic recurrences after curative resection. World
J Surg. 32:1738–1747. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
El-Serag HB: Hepatocellular carcinoma. N
Engl J Med. 365:1118–1127. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yang Y, Nagano H, Ota H, Morimoto O,
Nakamura M, Wada H, Noda T, Damdinsuren B, Marubashi S, Miyamoto A,
et al: Patterns and clinicopathologic features of extrahepatic
recurrence of hepatocellular carcinoma after curative resection.
Surgery. 141:196–202. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Yuen MF, Ahn SH, Chen DS, Chen PJ,
Dusheiko GM, Hou JL, Maddrey WC, Mizokami M, Seto WK, Zoulim F and
Lai CL: Chronic hepatitis B virus infection: Disease revisit and
management recommendations. J Clin Gastroenterol. 50:286–294. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Suzumura K, Hirano T, Kuroda N, Iimuro Y,
Okada T, Hashimoto M, Hasegawa S and Fujimoto J: Solitary
mediastinal metastasis of hepatocellular carcinoma treated by
video-assisted thoracic surgery: Report of a case. Gen Thorac
Cardiovasc Surg. 61:651–654. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hung JJ, Lin SC and Hsu WH: Pancoast
syndrome caused by metastasis to the superior mediastinum of
hepatocellular carcinoma. Thorac Cardiovasc Surg. 55:463–465. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chen CC, Yeh HZ, Chang CS, Ko CW, Lien HC,
Wu CY and Hung SW: Transarterial embolization of metastatic
mediastinal hepatocellular carcinoma. World J Gastroenterol.
19:3512–3516. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Oh SY, Seo KW, Jegal Y, Ahn JJ, Min YJ,
Park CR and Hwang JC: Hemothorax caused by spontaneous rupture of a
metastatic mediastinal lymph node in hepatocellular carcinoma: A
case report. Korean J Intern Med. 28:622–625. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Xiaohong S, Huikai L, Feng W, Ti Z,
Yunlong C and Qiang L: Clinical significance of lymph node
metastasis in patients undergoing partial hepatectomy for
hepatocellular carcinoma. World J Surg. 34:1028–1033. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Amini N, Ejaz A, Spolverato G, Maithel SK,
Kim Y and Pawlik TM: Management of lymph nodes during resection of
hepatocellular carcinoma and intrahepatic cholangiocarcinoma: A
systematic review. J Gastrointest Surg. 18:2136–2148. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ueda J, Yoshida H, Mamada Y, Taniai N,
Mineta S, Yoshioka M, Kawano Y, Shimizu T, Hara E, Kawamoto C, et
al: Surgical resection of a solitary para-aortic lymph node
metastasis from hepatocellular carcinoma. World J Gastroenterol.
18:3027–3031. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gao F, Gu Y, Huang J, Zhao M and Wu P:
Radiofrequency ablation of retroperitoneal metastatic lymph nodes
from hepatocellular carcinoma. Acad Radiol. 19:1035–1040. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Jang WI, Kim MS, Bae SH, Cho CK, Yoo HJ,
Seo YS, Kang JK, Kim SY, Lee DH, Han CJ, et al: High-dose
stereotactic body radiotherapy correlates increased local control
and overall survival in patients with inoperable hepatocellular
carcinoma. Radiat Oncol. 8:2502013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kwon JH, Bae SH, Kim JY, Choi BO, Jang HS,
Jang JW, Choi JY, Yoon SK and Chung KW: Long-term effect of
stereotactic body radiation therapy for primary hepatocellular
carcinoma ineligible for local ablation therapy or surgical
resection. Stereotactic radiotherapy for liver cancer. BMC Cancer.
10:4752010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Huang WY, Jen YM, Lee MS, Chang LP, Chen
CM, Ko KH, Lin KT, Lin JC, Chao HL, Lin CS, et al: Stereotactic
body radiation therapy in recurrent hepatocellular carcinoma. Int J
Radiat Oncol Biol Phys. 84:355–361. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kim K, Chie EK, Kim W, Kim YJ, Yoon JH,
Lee HS and Ha SW: Absence of symptom and intact liver function are
positive prognosticators for patients undergoing radiotherapy for
lymph node metastasis from hepatocellular carcinoma. Int J Radiat
Oncol Biol Phys. 78:729–734. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Yoon SM, Kim JH, Choi EK, Ahn SD, Lee SW,
Yi BY, Chung YW, Lee YS and Seo DJ: Radioresponse of hepatocellular
carcinoma-treatment of lymph node metastasis. Cancer Res Treat.
36:79–84. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Llovet JM, Ricci S, Mazzaferro V, Hilgard
P, Gane E, Blanc JF, de Oliveira AC, Santoro A, Raoul JL, Forner A,
et al: Sorafenib in advanced hepatocellular carcinoma. N Engl J
Med. 359:378–390. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Bruix J, Raoul JL, Sherman M, Mazzaferro
V, Bolondi L, Craxi A, Galle PR, Santoro A, Beaugrand M,
Sangiovanni A, et al: Efficacy and safety of sorafenib in patients
with advanced hepatocellular carcinoma: Subanalyses of a phase III
trial. J Hepatol. 57:821–829. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Raoul JL, Bruix J, Greten TF, Sherman M,
Mazzaferro V, Hilgard P, Scherubl H, Scheulen ME, Germanidis G,
Dominguez S, et al: Relationship between baseline hepatic status
and outcome, and effect of sorafenib on liver function: SHARP trial
subanalyses. J Hepatol. 56:1080–1088. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Abou-Alfa GK, Amadori D, Santoro A, Figer
A, De Greve J, Lathia C, Voliotis D, Anderson S, Moscovici M and
Ricci S: Safety and efficacy of sorafenib in patients with
hepatocellular carcinoma (HCC) and Child-Pugh A versus B cirrhosis.
Gastrointest Cancer Res. 4:40–44. 2011.PubMed/NCBI
|