Introduction
Ground glass opacities (GGO) refers to the lesions
manifested as blur and high-density image on pulmonary window,
while these lesions were either invisible or only the solid portion
was visible on mediastinal window. The texture of vessel and
bronchus of lesion were clear. GGO were closely associated with
pulmonary cancer, and were regarded as precancerous lesions
(1). However, the lesions were also
found in inflammation, infection and tuberculosis (2). Thus, early qualitative diagnosis of the
GGO is very important for the treatment of diseases.
The use of pre-set parameter to obtain GGO images
has some limitations with regard to qualitative diagnosis (3). The operational level of technical
personnel, scanning parameter setting, the accuracy of computed
tomography (CT) values, and the quality of the system were
considered to be important factors influencing qualitative
diagnosis (4). The window technique
is a type of amplification technology that takes advantage of the
gray-scale function in computer software to enlarge the visual
gray-scale identification range (5).
It can adjust the window width and window level of lesion on
pulmonary window and mediastinal window continuously and
dynamically, to obtain the best range of gray-scale, and compare
the window characteristics of different GGO to obtain more
sensitive and accurate quantitative data.
The aim of the present study was to examine the
value of window technique in qualitative diagnosis of the GGO in
patients with non-small cell pulmonary cancer. The results showed
that, the window width and window level on pulmonary window and
mediastinal window of malignant lesions were significantly less
than those of benign ones.
Patients and methods
Objects
In total, 124 clinically suspected pulmonary cancer
patients were retrospectively analyzed between January, 2012 and
January, 2016. The lesions were affirmed by puncture biopsy, and
were GGO on pulmonary window but invisible on mediastinal window.
The following conditions were excluded: a clear diagnosis of tumor,
recent history of pneumonia, pulmonary tuberculosis, thoracic
injury, surgery and history of radiation exposure, poor quality
image. The Zaozhuang Municipal Hospital (Shandong, China) Ethics
Committee approved the study. Informed consent was obtained from
the patients or their family members.
Of the 124 cases, 93 patients had tumor, and 31 had
benign lesions (25.0%). Of the 93 tumor lesions, 40 were squamous
carcinoma, 49 were adenocarcinoma, and 4 were others. There were 37
atypical hyperplasia, 35 were in situ, and 21 were invasive
lesions. There were 52 lesions with round or ovoid shape, and 41
were irregular in shape. The average diameter of the lesions was
0.6±0.3 cm (range, 0.3–1.0 cm), with 46 cases having left pulmonary
and 47 cases right pulmonary lesions. The patients with tumors
included 52 males and 41 females, and the average age was 56.9±14.7
years (6–48 years). If the 31 benign lesions, 23 cases were
pneumonia, and 8 cases were tuberculosis, while of the 31 cases 20
were round or ovoid shaped, and 11 irregular in shape. The average
diameter of the lesions was 0.5±0.4 cm (range, 0.2–1.3 cm), 13
lesions were in the left lung, and 18 were in the right lung. The
patients with benign lesions included 17 males and 14 females, and
the average age was 54.6±15.2 years (37–73 years). The difference
of gender, age, pathological changes, morphology and diameter of
comparison between the two groups was not significantly
different.
CT scanning methods
Siemens Sensation 64 multi-detector spiral CT
(Siemens AG, Munich, Germany) was used, with a parameter of pitch
1.2, collimation width 128×0.6 mm, scanning thickness 5 mm, tube
voltage 120 kV, automatic tube current, reconstruction thickness 1
mm, window width 1,500 Hounsfield units (HU) and window level −450
HU on pulmonary window, window width 400 HU and window level 40 HU
on mediastinal window. A plain scan was used without oral contrast
material.
For window technique, two radiology doctors analyzed
the images in a blinded manner. The window width was adjusted
constantly until the lesions were invisible with the fixed
pulmonary window level (−450 HU) on 3-megapixel medical displays,
and then the pulmonary window width was fixed (150 HU), and the
window level was adjusted constantly until the lesions were
invisible. The window width was adjusted constantly until the
lesions were invisible with the fixed mediastinal window level (40
HU), and then the mediastinal window width (400 HU) was fixed, and
the window level adjusted constantly until the lesions were
invisible. Multi-plane reorganization observation was used to
obtain the average. Those above the upper limitation gray-scale
range were enhanced to white, and those below the upper limitation
were compressed to black. M – (W/2) – M + (W/2) was used to
represent (M, window level; W, window width). M = (CTmax
– CTmin)/2, W = CTmax – CTmin.
Statistical analysis
Data were analyzed using SPSS 19.0 statistical
software (Chicago, IL, USA). The quantitative data were expressed
as means ± standard deviation, and the difference of groups was
compared by t-test. Qualitative data were expressed as the number
of cases or percentage (%), and the difference of groups was
compared using the χ2 test. The area under the receiver
operating characteristic (ROC) curve represented the diagnostic
accuracy, and difference with P<0.05 was considered to indicate
a statistically significant difference.
Results
Comparison of window width and window
level
The window width and window level on the pulmonary
and mediastinal windows of malignant lesions was significantly less
than those of benign ones (P<0.05), as shown in Table I.
 | Table I.Comparison of window width and window
level (HU). |
Table I.
Comparison of window width and window
level (HU).
| Groups | Pulmonary window | Mediastinal
window |
|---|
|
|
|
|
|---|
|
| Width | Level | Width | Level |
|---|
| Malignant | 1,356±53 | −210±35 | 353±45 | 26±10 |
| Benign | 2,124±67 | −546±43 | 652±52 | 63±20 |
| t-test | 7.632 | 6.549 | 7.541 | 7.835 |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 |
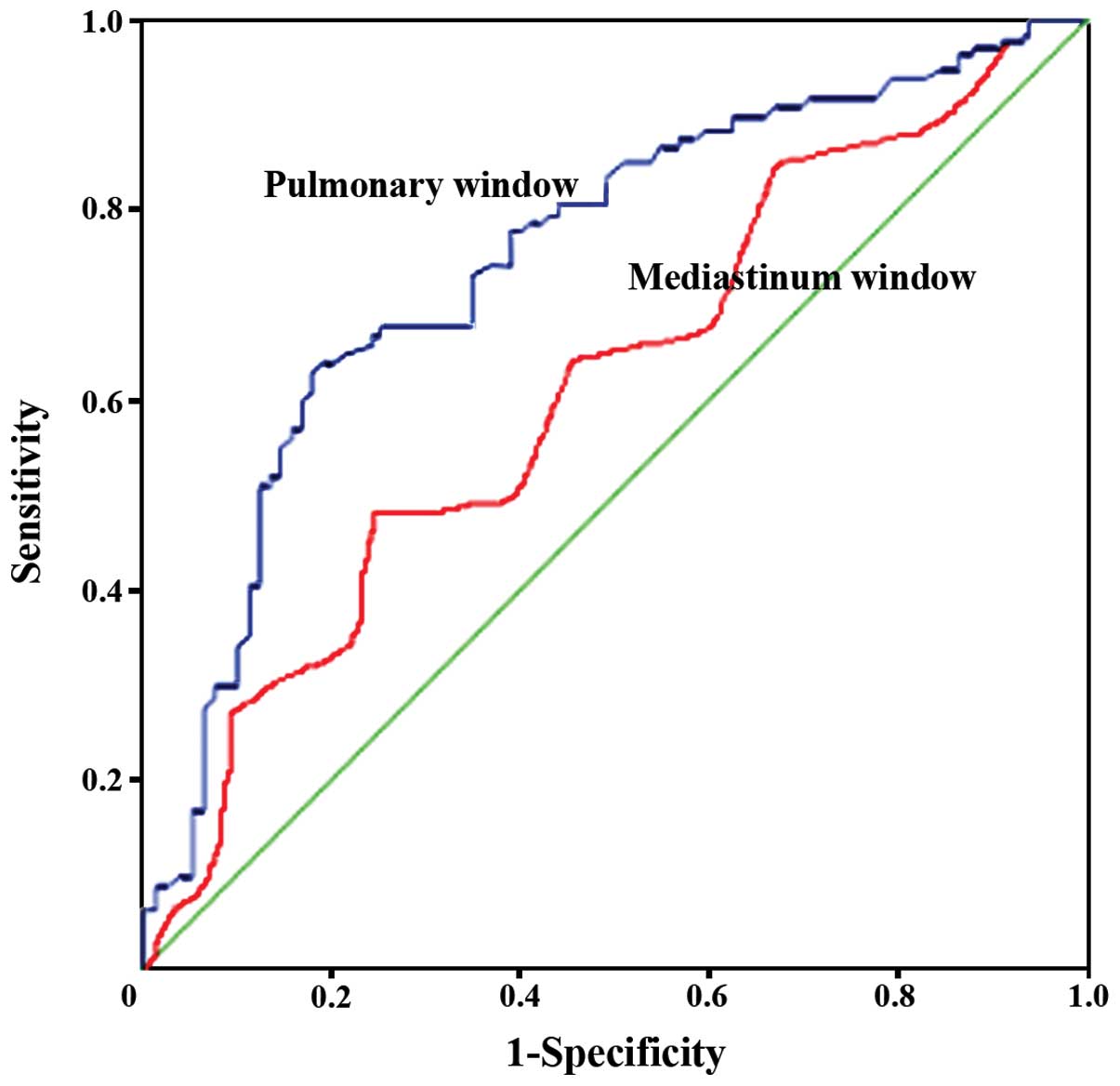
ROC analysis
ROC was applied to analyze the usage of the
pulmonary and mediastinum window technique in the diagnosis of
malignant lesions. The cut-off value on pulmonary window was the
window width and window level of 1,300 and −220 HU, the area under
the ROC was 0.830 [sensitivity was 72.5%, specificity was 84.3%;
95% confidence interval (CI), 0.712–0.945]. The cut-off value on
the mediastinal window was the window width and window level of 360
and 30 HU, and the area under the ROC was 0.623 (sensitivity was
62.0%, specificity was 55.7%; 95% CI, 0.541–0.745), as shown in
Fig. 1.
Discussion
The window width mainly affected the contrast of the
image. The large window width multiplies the levels of the image,
reduces the contrast and deteriorates the detail display, which is
suitable for distinguishing the structure with large density
difference (6). The small window
width decreased the levels of the image, enhanced the contrast, and
optimized the detail display, which was suitable for distinguishing
the structure with small density difference. The window level
mainly affected the image contrast. The high window darkened the
image, and the window was equivalent to the center of the
gray-scale (7). The best window width
and window level is necessary for setting the standard window, and
was manifested as 35 picture/sheet at the center of the image.
Subsequently, the window width and window level was adjusted
slightly and each part of 4–6 images was captured (8). The narrow window technique was suitable
for lesions with small density difference and unclear boundary
(9). Thus, lesions with slight
density differences or a large range and rich layers need to use
the wide window technique (10).
The development of vessels and bronchi pulmonary
window have a greater interference to the qualitative diagnosis of
GGO. Early pulmonary cancer mainly originates in bronchial
epithelium, with the involvement of centrilobular bronchi or
centrilobular arterial nodules, and located around the blood
vessels, around or through the minimum pulmonary arteries that CT
show. The adjustment of the pulmonary window width and window level
can distinguish the imaging range of GGO from blood vessels and
bronchi to improve the accuracy of clinical diagnosis (11,12). The
common parameter is window width of 800–1,000 HU, window level of
−700 HU, and upper bound of −200 HU. Fat, fluid, soft tissue and
bone were located out of the window by analyzing the density, and
in sharp contrast with the pulmonary tissue, which was not suitable
to display the characteristics of lesions and the inflammation.
Additionally, it was difficult to distinguish the lesions in the
center with vascular section. The window width and window level on
pulmonary window and mediastinal window of malignant lesions was
significantly less than those of benign ones. In the malignant
group, the average window width and window level was of 1,356 and
−210 HU on pulmonary window. The diameter of the GGO, the size of
solid or pathological invasive component, and the composition of
ground glass proportion have great limitations to qualitative
diagnosis (13). The tumors can be
divided into gas type and solid type according to mediastinal
window width and window level technology. The gas type has good
prognosis and applicable value (14,15). The
mediastinal window cannot display GGO lesions well, so the
mediastinal window technique remains in limited use.
The adjustment of the pulmonary window width and
window level can highlight the boundaries of the tissues and the
appearing and disappearing range of CT, to improve the accuracy of
clinical diagnosis. The prognosis was assessed based on the size of
tumor alone, but disagreement also exist (16,17).
In conclusion, the cut-off value on pulmonary window
was the window width and window level of 1,300 and −220 HU, the
area under the ROC was 0.830 (sensitivity was 72.5%, specificity
was 84.3%; 95% CI, 0.712–0.945). The cut-off value on the
mediastinal window was the window width and window level of 360 and
30 HU, and the area under the ROC was 0.623 (sensitivity was 62.0%,
specificity was 55.7%; 95% CI, 0.541–0.745). The diagnosis
sensitivity, specificity and accuracy of pulmonary window were
better than those of mediastinal window. However, the frequent
adjustment of window technology will lead to visual fatigue, and
increase workload. Further exploration of a more simple and higher
quantitative inspection method is required.
References
|
1
|
Min JH, Lee HY, Lee KS, Han J, Park K, Ahn
MJ and Lee SJ: Stepwise evolution from a focal pure pulmonary
ground-glass opacity nodule into an invasive lung adenocarcinoma:
an observation for more than 10 years. Lung Cancer. 69:123–126.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Pedersen JH, Saghir Z, Wille MM, Thomsen
LH, Skov BG and Ashraf H: Ground-glass opacity lung nodules in the
era of lung cancer ct screening: radiology, pathology, and clinical
management. Oncology (Williston Park). 30:266–274. 2016.PubMed/NCBI
|
|
3
|
Saji H, Matsubayashi J, Akata S, Shimada
Y, Kato Y, Kudo Y, Nagao T, Park J, Kakihana M, Kajiwara N, et al:
Correlation between whole tumor size and solid component size on
high-resolution computed tomography in the prediction of the degree
of pathologic malignancy and the prognostic outcome in primary lung
adenocarcinoma. Acta Radiol. 56:1187–1195. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lee HY and Lee KS: Ground-glass opacity
nodules: histopathology, imaging evaluation, and clinical
implications. J Thorac Imaging. 26:106–118. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Murakawa T, Konoeda C, Ito T, Inoue Y,
Sano A, Nagayama K and Nakajima J: The ground glass opacity
component can be eliminated from the T-factor assessment of lung
adenocarcinoma. Eur J Cardiothorac Surg. 43:925–932. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Liu B, Mi RH, Wei XD, Chen L, Ai H, Yuan
FF, Yin QS and Song YP: Clinical analysis of grand glass opacity on
CT as the first change of lung infection accompanied by hematologic
malignancies. Zhonghua Yi Xue Za Zhi. 96:163–166. 2016.(In
Chinese). PubMed/NCBI
|
|
7
|
Nam KB, Kim TJ, Park JS, Chung MJ and Lee
KW: Long-term follow-up results from PET/CT surveillance after
surgical resection of lung adenocarcinoma manifesting as
ground-glass opacity. Medicine (Baltimore). 95:e26342016.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lee HN, Kim MY, Koo HJ, Kim SS, Yoon DH,
Lee JC and Song JW: and Thin-Section CT: Thin-section ct
characteristics and longitudinal CT follow-up of chemotherapy
induced interstitial pneumonitis: a retrospective cohort study.
Medicine (Baltimore). 95:e24602016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Cha MJ, Lee KS, Kim HS, Lee SW, Jeong CJ,
Kim EY and Lee HY: Improvement in imaging diagnosis technique and
modalities for solitary pulmonary nodules: from ground-glass
opacity nodules to part-solid and solid nodules. Expert Rev Respir
Med. 10:261–278. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chen CY, Chen CH, Shen TC, Cheng WC, Hsu
CN, Liao CH, Chen CY, Hsia TC, Liao WC, Tu CY, et al: Lung cancer
screening with low-dose computed tomography: experiences from a
tertiary hospital in Taiwan. J Formos Med Assoc. 115:163–170. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Jiang G and Xie D: Early-stage lung cancer
manifested as ground-glass opacity. Zhonghua Wai Ke Za Zhi.
53:790–793. 2015.(In Chinese). PubMed/NCBI
|
|
12
|
Bak SH, Lee HY, Kim JH, Um SW, Kwon OJ,
Han J, Kim HK, Kim J and Lee KS: Quantitative CT scanning analysis
of pure ground-glass opacity nodules predicts further CT scanning
change. Chest. 149:180–191. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ichikawa K, Kobayashi T, Sagawa M,
Katagiri A, Uno Y, Nishioka R and Matsuyama J: A phantom study
investigating the relationship between ground-glass opacity
visibility and physical detectability index in low-dose chest
computed tomography. J Appl Clin Med Phys. 16:50012015.PubMed/NCBI
|
|
14
|
Ikehara M, Saito H, Yamada K, Oshita F,
Noda K, Nakayama H, Masui K, Kameda Y, Komase Y and Miyazawa T:
Prognosis of small adenocarcinoma of the lung based on thin-section
computed tomography and pathological preparations. J Comput Assist
Tomogr. 32:426–431. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Honda T, Kondo T, Murakami S, Saito H,
Oshita F, Ito H, Tsuboi M, Nakayama H, Yokose T, Kameda Y, et al:
Radiographic and pathological analysis of small lung adenocarcinoma
using the new IASLC classification. Clin Radiol. 68:e21–e26. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Yang F, Chen H, Xiang J, Zhang Y, Zhou J,
Hu H, Zhang J and Luo X: Relationship between tumor size and
disease stage in non-small cell lung cancer. BMC Cancer.
10:4742010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Patz EF Jr, Rossi S, Harpole DH Jr,
Herndon JE and Goodman PC: Correlation of tumor size and survival
in patients with stage IA non-small cell lung cancer. Chest.
117:1568–1571. 2000. View Article : Google Scholar : PubMed/NCBI
|