Introduction
Primary renal lymphoma (PRL) is defined as a
non-Hodgkin's lymphoma (NHL) involving the kidney in the absence of
primarily extrarenal lymphatic disease. PRL is rare, as the kidney
is an extranodal organ and does not contain lymphatic tissue
(1). Therefore, the existence of a
PRL has been continuously debated. In recent years, reports of PRL
cases have confirmed the presence of the disease. PRL has been
shown to account for 0.7% of all extranodal lymphomas in North
America and 0.1% of all malignant lymphomas in Japan (2,3). No more
than 70 cases of PRL have been reported in the literature and the
majority are of NHL large B-cell type (4). The precise cause of PRL remains unknown.
It has been suggested that PRL originates from the renal capsule
and infiltrates the renal parenchyma. Another explanation is that
chronic inflammatory conditions of the kidney attract the
infiltration of lymphoid cells and eventually evolve into lymphoma
(5).
PRL is often present on only one side of the kidney
in adult patients, whereas it can be bilateral in pediatric
patients (6,7). PRL lacks clear clinical manifestations
and appears to be similar to renal cell carcinoma (RCC), renal
abscess and other kidney tumor metastases. Patients with PRL may
present with gross hematuria, acute/chronic kidney failure, and
flank pain or weight loss. It has been suggested that flank pain is
one of the most common symptoms of PRL (8).
The diagnosis of PRL includes: i) The presence of a
renal mass; ii) no evidence of extrarenal lymphomatous involvement
in the visceral organs or lymph nodes at first admission; and iii)
the absence of a leukemic blood picture together with no evidence
of myelosuppression (9). However, a
kidney biopsy remains the gold standard for the diagnosis of
primary renal lymphoma (10).
PRL is difficult to diagnose by imaging alone due to
its non-specific manifestations and can be roughly divided into
multiple renal masses, solitary masses, renal invasion from
contiguous retroperitoneal disease, perirenal disease and diffuse
renal infiltration (11,12). PRL is shown as a low echo mass on
ultrasound, and the use of enhanced computed tomography (CT) and
magnetic resonance imaging (MRI) can improve the specificity of
lymphoma. On CT scans, PRL generally presents as an isointense or
low-density mass. On contrast-enhanced CT scans, PRL appears to be
less dense than the adjacent renal parenchyma. On MRI, PRL exhibits
a hypointense signal on T1-weighted images and an isointense to
hypointense signal on T2-weighted images. PRL may also demonstrate
restricted diffusion on diffusion-weighted imaging (13). The mean apparent diffusion coefficient
value has been reported as 2.18–2.30×10−3
mm2/sec for the normal renal parenchyma,
0.88–0.90×10−3 mm2/sec for papillary RCC,
1.23–1.70×10−3 mm2/sec for clear cell RCC,
1.14–1.41×10−3 mm2/sec for chromophobe RCC
(14,15) and 0.64–0.76×10−3
mm2/sec for lymphoma (16,17). It
has also been shown that PRL exhibits an area of intense
fluorodeoxyglucose (18F-FDG) uptake on
18F-FDG positron emission tomography/CT (PET/CT) images.
The standardized uptake value (SUV) of PRL (SUVmean,
6.37±2.28) is significantly higher than renal clear cell carcinoma
(SUVmean, 2.58±0.62), however, it is similar to that of
RCC and renal collecting duct carcinoma (SUVmean,
6.27±1.15) (18). The use of combined
18F-FDG PET/CT greatly contributes to the accurate
diagnosis and timely treatment of PRL, even prior to the biopsy
results being obtained. This can also be used for the evaluation of
the chemotherapy effect and the follow-up for PRL (19).
Chemotherapy is the most common treatment for PRL.
This treatment generally includes 6–8 cycles of a cyclophosphamide,
hydroxydaunorubicin, oncovin and prednisone (CHOP) regimen, or on
the basis of this aforementioned plan, is combined with rituxan for
cluster of differentiation (CD)20-positive NHL, in order to improve
the patient's survival time to 5 years. However, the prognosis of
PRL remains largely unknown. The 1-year mortality rates of PRL can
be as high as 75% (20), the median
survival time is only 8 months to 3 years, and the 5-year survival
rate is only 40–50% (21).
The present study reports the case of a 70-year-old
woman with PRL and provides a literature review of 49 cases of PRL
that have been reported since 1989. Written informed consent was
obtained from the patient.
Case report
In July 2014, a 70-year-old woman, with a medical
history of type 2 diabetes mellitus for 7 years and arterial
hypertension for 10 years, presented to Ningbo Yin Zhou Hospital
(Ningbo, China) due to the sonographic detection of a mass in the
right kidney. The patient did not report any night sweats, fever or
weight loss. The physical examination was unremarkable and there
was no sign of either lymphadenopathy or hepatosplenomegaly. The
laboratory results were as follows: White blood cells (WBC),
7.9×109/l (normal range, 3.5–9.5×109/l);
hemoglobin, 124 g/l (normal range, 115–150 g/l); platelets,
209×109/l (normal range, 125–350×109/l);
blood urea nitrogen, 4.94 mmol/l (normal range, 2.9–8.2 mmol/l);
and creatinine, 40 µmol/l (normal range, 45–84 µmol/l). Urine
routine tests were negative for proteins, red blood cells (RBC) 1
particle/µl (normal range, 0–5 particle/µl), WBC 7 particle/µl
(normal range, 0–9 particle/µl) and bacteria 164 particle/µl
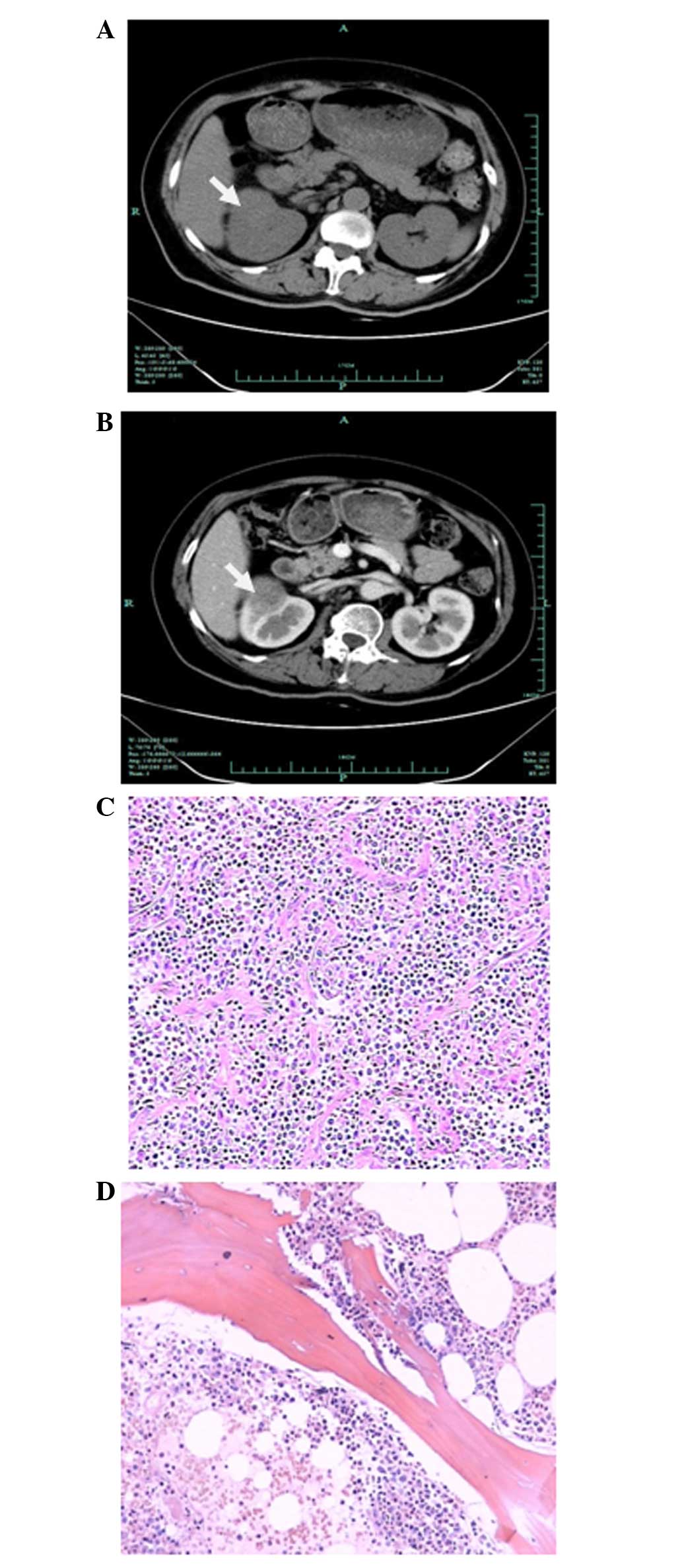
(normal range, 0–75 particle/µl). CT (Fig. 1A) revealed a 3.6-cm mass of right
kidney without associated hydronephrosis or ureteral obstruction.
The patient then underwent contrast-enhanced CT of the abdomen
(Fig. 1B). The results showed that
the mass of the right kidney exhibited continuous progressive
enhancement, with a value of 100 HU in the corticomedullary phase.
The mass was initially suspected to be a malignancy of the right
kidney and subsequently, a right nephrectomy was performed. Tissue
specimens were fixed with 10% formalin, embedded in paraffin and
stained with hematoxylin and eosin. The histological evaluation of
the nephrectomy specimen (Fig. 1C)
revealed diffuse proliferation of large lymphoid cells, which
indicated diffuse large B-cell NHL. Immunohistochemical analysis
revealed that the tumor cells were positive for CD5 (monoclonal
rabbit anti-human antibody; 1:100; #ZA-0510; Zhongshan Jinqiao
Biological Technology Co., Ltd., Beijing, China), CD3 (monoclonal
rabbit anti-human antibody; 1:200; #Kit-0003; Fuzhou Maixin Biotech
Co., Ltd., Fuzhou, China), CD79α (monoclonal rabbit anti-human
antibody; 1:200; #ZM-0293; Zhongshan Jinqiao Biological Technology
Co., Ltd.), CD20 (monoclonal mouse anti-human antibody; 1:100;
#MAB-0669; Fuzhou Maixin Biotech Co., Ltd.), CD43 (monoclonal mouse
anti-human antibody; 1:200; #ZM-0048; Zhongshan Jinqiao Biological
Technology Co., Ltd.), CD10 (monoclonal mouse anti-human antibody;
1:200; #M7308; Dako, Glostrup, Denmark), Ki-67 (monoclonal mouse
anti-human antibody; 1:400; #Kit-0005; Fuzhou Maixin Biotech Co.,
Ltd.) (85%) and mutated melanoma-associated antigen 1 (monoclonal
rabbit anti-human antibody; 1:200; #ZA-0583; Zhongshan Jinqiao
Biological Technology Co., Ltd.), and negative for B-cell lymphoma
(Bcl)-2 (monoclonal mouse anti-human antibody; 1:200; #ZM-0010;
Zhongshan Jinqiao Biological Technology Co., Ltd.), CD23
(monoclonal rabbit anti-human antibody; 1:100; #ZA-0516; Zhongshan
Jinqiao Biological Technology Co., Ltd.), CD21 (monoclonal rabbit
anti-human antibody; 1:100; #ZA-0525; Zhongshan Jinqiao Biological
Technology Co., Ltd.), cyclin D1 (monoclonal rabbit anti-human
antibody; 1:100; #M3642; Dako), p53 (monoclonal mouse anti-human;
1:800; #ZM-0408; Zhongshan Jinqiao Biological Technology Co., Ltd.)
and Bcl-6 (monoclonal mouse anti-human antibody; 1:200; #ZM-0011;
Zhongshan Jinqiao Biological Technology Co., Ltd.). Next, a bone
marrow biopsy was performed, which showed no morphological
involvement of lymphoma (Fig. 1D).
The NHL was finally considered to be PRL, as the imaging and biopsy
results confirmed that there was no sign of peripheral
lymphadenopathy or hepatosplenomegaly. The patient was treated with
6–8 cycles of a CHOP regimen (a combination of 1 g cyclophosphamide
on day 1, 80 mg epirubicin on day 1, 3 mg vindesine on day 1, and
10 mg dexamethasone on days 1–5) (1 cycle, 28 days) and has
completed three courses of treatment to date. On a CT scan
following the third course of treatment, the patient showed a
complete response to the treatment and no major discomfort was
reported. Follow-up examination performed after 2 months of
treatment revealed no local recurrence of the lymphoma. Follow-up
every 3 months is planned for the first 2 years after treatment,
and every 6 months in subsequent years.
Discussion
PRL is extremely rare and a thorough review of PRL
cases has been largely lacking in the literature. The present study
reviewed all 49 cases of PRL reported in the literature since 1989
(Table I). A finding of diffuse large
B-cell lymphoma is the most common pathological sign. Of all 49
cases, 30 were male, 18 were female and 1 had an unrecorded gender.
There were more male patients than female patients, and the ratio
was ~1.6:1. In addition, the site of PRL can be age-related. The
literature review found that PRL generally appears to be bilateral
in patients who are younger than 18 years old and unilateral in
adult patients. Fever is one of the most common symptoms in younger
patients (56%), while abdominal and flank pain are common (62%) in
patients aged from 18–50 years. Weight loss and gross hematuresis
are the most common symptoms (37%) for patients who are older than
50 years. The patients aging from 18–50 years have the highest
survival rate (mean, 62.8 months) compared with patients aged from
0–18 years old (mean, 17.6 months) and >50 years (mean, 48.2
months). In addition, 19 cases of bilateral PRL experienced a mean
survival time of 21 months, and 30 cases of unilateral kidney
experienced a mean survival time of 68 months. It appears that
younger patients and bilateral PRL results in a shorter survival
time and more rapid progression of the disease. Therefore, special
procedure should be considered for those patients, including the
combination of surgery, chemotherapy or radiotherapy.
 | Table I.Literature review of the 49 cases of
primary renal lymphoma reported in the literature since 1989. |
Table I.
Literature review of the 49 cases of
primary renal lymphoma reported in the literature since 1989.
| Case no. | Gender | Age, years | Site | Renal impairment | Presenting
symptoms | Treatment | Chemotherapeutic
agents | Histology | Follow-up
post-treatment | (Ref.) |
|---|
| 1 | Female | 53 | Bilateral | Yes | Poor appetite, meat
repulsion and progressive weight loss | Chemotherapy | CHOP | Non-Hodgkin's
lymphoma | Died at 3 days |
(1) |
| 2 | Female | 58 | Bilateral | Yes | Anorexia, weight
loss, night sweats, malaise | Chemotherapy | CHOP | B-cell
non-Hodgkin's lymphoma | Unknown | (22) |
| 3 | Female | 49 | Bilateral | Yes | Renal impairment
with diuresis, fever, weight loss, lower back pain | Chemotherapy | CHOP | Centroblastic
lymphoma | Died at 10
weeks | (23) |
| 4 | Female | 5 | Bilateral | No | Fever, weight loss,
sweats | Chemotherapy | M-BACOD | Lymphoblastic
B-cell lymphoma | Died at 20
months |
|
| 5 | Male | 4 | Bilateral | No | Fever, nausea,
vomiting | Chemotherapy | LSA2-L2 | Unknown | Died at 16
months |
|
| 6 | Male | 62 | Bilateral | Yes | Macroscopic
hematuria, acute urinary retention, and bilateral
hydronephrosis | Chemotherapy | CHOP | B-cell lymphoma of
the follicular type | Died at 2
months | (5) |
| 7 | Male | 45 | Right | Yes | Unknown | Surgery +
chemotherapy | B-ALL | B-cell lymphoma of
the Burkitt-like type | Alive at 47
months |
|
| 8 | Male | 14 | Bilateral | Yes | Intermittent
headache, flank pain, emetic weight loss and hypertension | Chemotherapy | CCG-5942 | Diffuse large
B-cell lymphoma | Alive at 2
weeks | (24) |
| 9 | Male | 79 | Left | Yes | Generalized body
aches, weakness and decreased urine output | Surgery | None | Marginal-zone
B-cell lymphoma | Alive at 2
months | (25) |
| 10 | Male | 43 | Right | Unknown | Left flank
pain | Surgery | None | B-cell lymphoma of
MALT | Alive at 28
months | (26) |
| 11 | Male | 46 | Bilateral | Yes | Unknown | Surgery +
chemotherapy | Pro-MECE-Cyta BOM +
Flu-Ctx-Idec | Diffuse large
B-cell lymphoma | Alive at 67
months | (27) |
| 12 | Female | 70 | Right | No | Anorexia, malaise,
and daily low-grade fever | Surgery +
chemotherapy | R-CHOP | Diffuse large
B-cell lymphoma | Alive at 8
months | (28) |
| 13 | Female | 65 | Left | Unknown | Unknown | Surgery +
chemotherapy + radiation | R-CHOP | Diffuse large
B-cell lymphoma | Alive at 18
months | (6) |
| 14 | Female | 68 | Bilateral | Yes | Bilaterally severe
flank pain and dysuria | Unknown | Unknown | Large B-cell
lymphoma | Died at 10
days | (29) |
| 15 | Male | 2 | Bilateral | Yes | Progressive
abdominal distention, decreased urine output | Chemotherapy | cpa + L-asp + Vcr +
Prednisolone | T-cell
lymphoma | Unknown | (30) |
| 16 | Female | 71 | Left | No | Weight loss and
fever | Surgery +
chemotherapy | CHOP | B-cell
lymphoma | Died at 4
months | (31) |
| 17 | Male | 50 | Right | No | Abdominal pain | Surgery +
chemotherapy | CHOP | Diffuse large
B-cell lymphoma | Alive at 1
month | (32) |
| 18 | Male | 62 | Left | No | Gross
hematuria | Surgery +
chemotherapy + interferon | R-CHOP | Diffuse B-cell
lymphoma | Alive at 5
years |
|
| 19 | Male | 84 | Left | Yes | Unknown | Surgery +
chemotherapy + interferon | COP | B-cell
lymphoma | Alive at 5
years |
|
| 20 | Male | 58 | Right | Unknown | Headache and
short-term memory loss | Surgery +
chemotherapy | R-CHOP | Diffuse large
B-cell lymphoma | Unknown | (33) |
| 21 | Female | 21 | Bilateral | Yes | Fever, weight loss,
abdominal pain and abdominal masses | Chemotherapy | VACOP-B | Diffuse large
B-cell lymphoma | Unknown | (34) |
| 22 | Male | 5 | Bilateral | Yes | Hypertension | Chemotherapy | CCG-1961 | T-cell
lymphoblastic lymphoma | Died at 2
months | (35) |
| 23 | Male | 57 | Bilateral | Yes | Dyspnea, renal
failure and anemia | Chemotherapy +
autologous stem cell transplantation | R-CHOP | Unknown | Unknown | (36) |
| 24 | Male | 62 | Right | Unknown | Low-grade fever and
dull, non-radiating right flank pain | Surgery +
chemotherapy | R-CHOP | Diffuse large
B-cell lymphoma | Alive at 1
year | (21) |
| 25 | Female | 77 | Left | Yes | Anorexia, astenia
and malaise | Surgery +
chemotherapy | CVP | Diffuse large
B-cell lymphoma | Alive at 15
months | (37) |
| 26 | Male | 46 | Right | Unknown | Weight loss,
evening fever and upper abdominal pain | Chemotherapy | R-CHOP | Diffuse large
B-cell lymphoma | Alive at 7
months |
|
| 27 | Male | 47 | Renal graft | Unknown | Chronic graft
dysfunction | Surgery | None | B-cell
lymphoma | Alive at 6.5
years |
|
| 28 | Male | 74 | Left | Unknown | Unknown | Surgery +
chemotherapy | Unknown | Diffuse small
B-cell lymphoma | Died after
chemotherapy course 2 | (38) |
| 29 | Male | 71 | Right | Unknown | Unknown | Chemotherapy | R-CHOP | Diffuse large
B-cell lymphoma | Alive at 2
years |
|
| 30 | Female | 75 | Left | Unknown | Unknown | Surgery +
chemotherapy | R-CHOP | Diffuse large
B-cell lymphoma | Alive at 1
year |
|
| 31 | Male | 81 | Right | Unknown | Macroscopic
hematuria | Surgery +
chemotherapy | Unknown | Small B-cell
lymphoma | Unknown |
|
| 32 | Female | 52 | Bilateral | Yes | Back pain,
headache, dysuria pollakisuria, hematuria, nonoliguric acute renal
failure, hypertension | Chemotherapy | R-CHOP B-cell
lymphoma | Diffuse large | Alive at 2
years | (39) |
| 33 | Male | 3 | Bilateral | No | Abdominal
distension, abdominal pain and fever | Chemotherapy | BFM-90 | B-cell
lymphoma | Died after
chemotherapy course 5 | (40) |
| 34 | Male | 60 | Right | No | Dyspnea,
intermittent claudication and fatigue | Surgery +
chemotherapy | CHOP | Follicular
non-Hodgkin's lymphoma | Unknown | (12) |
| 35 | Male | 70 | Right | Unknown | Macroscopic
hematuria | Surgery | None | Diffuse large
B-cell lymphoma | Unknown | (41) |
| 36 | Male | 32 | Left | No | Heaviness in
epigastric region, dull ache in left flank and loss of appetite and
weight | Surgery +
chemotherapy | CHOP | B-cell
lymphoma | Died at 2
months | (42) |
| 37 | Male | 72 | Left | Yes | Left flank pain,
weakness and weight loss | Chemotherapy | R-CHOP | Diffuse large
B-cell lymphoma | Alive at 15
months | (4) |
| 38 | Female | 7 | Bilateral | No | Intermittent fever,
joint pain, severe anemia and distended abdomen | Chemotherapy | CHOP | Unknown | Unknown | (43) |
| 39 | Female | 67 | Bilateral | Yes | Epigastric pain,
radiating to the back and associated with vomiting and nausea | Chemotherapy | R-CHOP | Large B-cell
lymphoma | Alive at 4
weeks | (10) |
| 40 | Female | 77 | Left | Yes | Anorexia, weakness,
malaise | Surgery +
chemotherapy | CVP + R | Diffuse large
B-cell lymphoma | Alive at 5.5
years | (44) |
| 41 | Male | 46 | Left | Yes | Weight loss and
left flank pain | Surgery +
chemotherapy + radiation therapy | R-CHOP | Diffuse large
B-cell lymphoma | Alive at 5
years |
|
| 42 | Male | 73 | Right | Yes | Unknown | Surgery | No | Large B-cell
lymphoma | Unknown | (45) |
| 43 | Female | 82 | Right | Yes | Dizziness,
palpitations or loss of consciousness | Chemotherapy | R-CHOP | B-cell
lymphoma | Unknown | (46) |
| 44 | Female | 27 | Bilateral | Yes | Nausea, vomiting
and fever | Chemotherapy | R-CHOP | Diffuse large
B-cell lymphoma | Unknown | (47) |
| 45 | Male | 77 | Left | No | Gross
hematuria | Radiation
therapy | No | Marginal zone
B-cell lymphoma | Alive at 3
years | (48) |
| 46 | Female | 12 | Right | No | Gross
hematuria | Surgery +
chemotherapy |
vcr+dex+cpa+mtx+ara-c+other drugs | Diffuse large
B-cell lymphoma | Alive at 3 years
and 2 months | (49) |
| 47 | N/A | 8 | Bilateral | Yes | Intermittent fever,
joint pain, severeanemia, and distended abdomen | Chemotherapy | R-CHOP | B-cell
lymphoma | Alive at 1
year | (19) |
| 48 | Male | 49 | Right | Unknown | Pain and mass per
abdomen | Surgery | No | B-cell
lymphoma | Alive at 1
year | (50) |
| 49 | Male | 42 | Left | Yes | Abdominal pain and
a mass in the abdomen | Chemotherapy | R-CHOP | Diffuse large
B-cell lymphoma | Alive at 28
months | (51) |
To date, chemotherapy remains the main treatment for
PRL. Among all 49 cases, chemotherapy treatment alone was
implemented in only 21 patients, and the mean survival time was
only 15.8 months. The mean survival time for the 15 patients
treated with the combination of chemotherapy and surgery was 49.4
months. However, the different survival times were not
significantly different (P=0.255) as determined by Kaplan-Meier
analysis using SPSS 17.0 statistical software (SPSS, Inc., Chicago,
IL, USA) whereby P<0.05 was considered to indicate a statistical
significant difference. Despite the lack of statistical
significance, the combination of chemotherapy and surgery produced
longer survival times than single chemotherapy treatment, and the
combined treatments may greatly slow disease progression. However,
early detection and effective treatment is required to improve the
prognosis.
Our review of 49 reported cases of PRL revealed that
a combination of chemotherapy and surgery resulted in longer
survival times than chemotherapy treatment alone. Therefore, the
present patient was treated with 6–8 cycles of CHOP following
nephrectomy. However, the literature review had several
limitations. Firstly, all follow up data was obtained from
different cases and thus, follow-up durations differ. Secondly, the
follow-up durations were reported using different units of time,
therefore, the mean survival time was calculated in months.
Thirdly, a number of studies did not report the patients last
follow-up date. Thus, further studies are required regarding the
prognosis of the disease. The early diagnosis of PRL requires
identification of the high-risk population, vulnerable organs,
symptoms and image results. Pathological diagnosis is important for
an early diagnosis. Chemotherapy is the preferred treatment, but
its combination with radiotherapy, surgery and other means should
be considered for patients with younger ages or bilateral PRL.
In conclusion, the patient in the present study was
diagnosed incidentally with a mass in the right kidney during a
routine physical examination and exhibited no clinical symptoms.
The mass was initially suspected as renal cell cancer and,
subsequently right nephrectomy was performed. However, histological
evaluation of the nephrectomy specimen indicated diffuse large
B-cell NHL. The patient was treated with 6–8 cycles of the CHOP
regimen. Follow-up examination performed after 2 months of
treatment revealed no local recurrence of the lymphoma.
References
|
1
|
Paganelli E, Arisi L, Ferrari ME, Olivetti
G and Tedeschi F: Primary non-Hodgkin's lymphoma of the kidney.
Haematologica. 74:301–304. 1989.PubMed/NCBI
|
|
2
|
Freeman C, Berg JW and Cutler SJ:
Occurrence and prognosis of extranodal lymphomas. Cancer.
29:252–260. 1972. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Aozasa K, Tsujimoto M, Sakurai M, Honda M,
Yamashita K, Hanada M and Sugimoto A: Non-Hodgkin's lymphomas in
Osaka, Japan. Eur J Cancer Clin Oncol. 21:487–492. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Belbaraka R, Elyoubi MB, Boutayeb S and
Errihani H: Primary renal non-Hodgkin lymphoma: An unusual
diagnosis for a renal mass. Indian J Cancer. 48:255–256. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gellrich J, Hakenberg OW, Naumann R,
Manseck A, Lossnitzer A and Wirth MP: Primary renal non-Hodgkin's
lymphoma-a difficult differential diagnosis. Onkologie. 25:273–277.
2002.PubMed/NCBI
|
|
6
|
Ahmad AH, Maclennan GT and Listinsky C:
Primary renal lymphoma: A rare neoplasm that may present as a
primary renal mass. J Urol. 173:2392005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Baran A, Kupeli S and Doğru O: A pediatric
renal lymphoma case presenting with central nervous system
findings. Turk J Haematol. 30:191–193. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Okuno SH, Hoyer JD, Ristow K and Witzig
TE: Primary renal non-Hodgkin's lymphoma. An unusual extranodal
site. Cancer. 75:2258–2261. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yasunaga Y, Hoshida Y, Hashimoto M, Miki
T, Okuyama A and Aozasa K: Malignant lymphoma of the kidney. J Surg
Oncol. 64:207–211. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Al-Salam S, Shaaban A, Alketbi M, Haq NU
and Abouchacra S: Acute kidney injury secondary to renal large
B-cell lymphoma: Role of early renal biopsy. Int Urol Nephrol.
43:237–240. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Cohan RH, Dunnick NR, Leder RA and Baker
ME: Computed tomography of renal lymphoma. J Comput Assist Tomogr.
14:933–938. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Pinggera GM, Peschel R, Buttazzoni A,
Mitterberger M, Friedrich A and Pallwein L: A possible case of
primary renal lymphoma: A case report. Cases J. 2:62332009.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Nguyen DD and Rakita D: Renal lymphoma: MR
appearance with diffusion-weighted imaging. J Comput Assist Tomogr.
37:840–842. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Inci E, Hocaoglu E, Aydin S and Cimilli T:
Diffusion-weighted magnetic resonance imaging in evaluation of
primary solid and cystic renal masses using the Bosniak
classification. Eur J Radiol. 81:815–820. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wang H, Cheng L, Zhang X, Wang D, Guo A,
Gao Y and Ye H: Renal cell carcinoma: Diffusion-weighted MR imaging
for subtype differentiation at 3.0 T. Radiology. 257:135–143. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhang Y, Chen J, Shen J, Zhong J, Ye R and
Liang B: Apparent diffusion coefficient values of necrotic and
solid portion of lymph nodes: Differential diagnostic value in
cervical lymphadenopathy. Clin Radiol. 68:224–231. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wu X, Pertovaara H, Dastidar P, Vornanen
M, Paavolainen L, Marjomäki V, Järvenpää R, Eskola H and
Kellokumpu-Lehtinen PL: ADC measurements in diffuse large B-cell
lymphoma and follicular lymphoma: A DWI and cellularity study. Eur
J Radiol. 82:e158–e164. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ye XH, Chen LH, Wu HB, Feng J, Zhou WL,
Yang RM, Bu ZB, Ding Y, Guan J and Wang QS: 18F-FDG PET/CT
evaluation of lymphoma with renal involvement: Comparison with
renal carcinoma. South Med J. 103:642–649. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Dhull VS, Mukherjee A, Karunanithi S,
Durgapal P, Bal C and Kumar R: Bilateral primary renal lymphoma in
a pediatric patient: Staging and response evaluation with
18F-FDG PET/CT. Rev Esp Med Nucl Imagen Mol. 34:49–52.
2015.PubMed/NCBI
|
|
20
|
Porcaro AB, D'Amico A, Novella G, Curti P,
Ficarra V, Antoniolli SZ, Martignoni G, Matteo B and Malossini G:
Primary lymphoma of the kidney. Report of a case and update of the
literature. Arch Ital Urol Androl. 74:44–47. 2002.PubMed/NCBI
|
|
21
|
Ladha A and Haider G: Primary renal
lymphoma. J Coll Physicians Surg Pak. 18:584–585. 2008.PubMed/NCBI
|
|
22
|
van Gelder T, Michiels JJ, Mulder AH,
Klooswijk AI and Schalekamp MA: Renal insufficiency due to
bilateral primary renal lymphoma. Nephron. 60:108–110. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Arija JA Arranz, Carrion JR, Garcia FR,
Tejedor A, Pérez-Manga G, Tardio J and Menarguez FJ: Primary renal
lymphoma: Report of 3 cases and review of the literature. Am J
Nephrol. 14:148–153. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Levendoglu-Tugal O, Kroop S, Rozenblit GN
and Weiss R: Primary renal lymphoma and hypercalcemia in a child.
Leuk Lymphoma. 43:1141–1146. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Olusanya AA, Huff G, Adeleye O, Faulkner
M, Burnette R, Thompson H, Adeola T and Woods K: Primary renal
non-Hodgkins lymphoma presenting with acute renal failure. J Natl
Med Assoc. 95:220–224. 2003.PubMed/NCBI
|
|
26
|
Tuzel E, Mungan MU, Yorukoglu K, Basakci A
and Kirkali Z: Primary renal lymphoma of mucosa-associated lymphoid
tissue. Urology. 61:4632003. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Cupisti A, Riccioni R, Carulli G, Paoletti
S, Tognetti A, Meola M, Francesca F, Barsotti G and Petrini M:
Bilateral primary renal lymphoma treated by surgery and
chemotherapy. Nephrol Dial Transplant. 19:1629–1633. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zomas A, Leivada A, Gortzolidis G,
Michalis E, Skandalis A and Anagnostopoulos NI: Primary renal
lymphoma presenting with chronic low-grade fever. Int J Hematol.
79:361–363. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Kaya A, Kanbay M, Bayrak O, Eken G, Memis
L, Akcay A and Duranay M: Primary renal lymphoma associated with
hepatitis C virus infection. Leuk Lymphoma. 47:1976–1978. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Sharma SB, Debnath PR and Tripathi R:
Primary renal lymphoma in a child. Indian J Pediatr. 73:9472006.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Tefekli A, Baykal M, Binbay M, Barut M and
Muslumanoglu AY: Lymphoma of the kidney: Primary or initial
manifestation of rapidly progressive systemic disease? Int Urol
Nephrol. 38:775–778. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Fang FS, Zhu HL, Song ZG and Lu XC: Three
cases of primary renal lymphoma. Zhongguo Shi Yan Xue Ye Xue Za
Zhi. 15:1107–1111. 2007.(In Chinese). PubMed/NCBI
|
|
33
|
Rajappa S, Digumarti R, Immaneni SR and
Parage M: Primary renal lymphoma presenting with paraneoplastic
limbic encephalitis. J Clin Oncol. 25:3783–3785. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Omer HA and Hussein MR: Primary renal
lymphoma. Nephrology (Carlton). 12:314–315. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Becker AM, Bowers DC, Margraf LR, Emmons J
and Baum M: Primary renal lymphoma presenting with hypertension.
Pediatr Blood Cancer. 48:711–713. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
James TC, Shaikh H, Escuadro L and Villano
JL: Bilateral primary renal lymphoma. Br J Haematol. 143:12008.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Vázquez Alonso F, Sánchez Ramos C, Prados
FJ Vicente, Geler M Pascual, Carazo E Ruiz, Massare P Becerra,
Padilla C Funes, Rodríguez Herrera F, Cózar Olmo JM and Buñuel M
Tallada: Primary renal lymphoma: Report of three new cases and
literature review. Arch Esp Urol. 62:461–465. 2009.(In Spanish).
PubMed/NCBI
|
|
38
|
Kose F, Sakalli H, Mertsoylu H, Sezer A,
Kocer E, Tokmak N, Kilinc F and Ozyilkan O: Primary renal lymphoma:
Report of four cases. Onkologie. 32:200–202. 2009.PubMed/NCBI
|
|
39
|
Reuter S, Rahbar K, Busch V, Hillebrand U,
Velden J, Pavenstädt H, Schober O and Stegger L: Acute renal
failure due to primary bilateral renal large B-cell lymphoma:
Diagnostics and follow-up by FDG-PET/CT. Clin Nucl Med. 34:722–724.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Jindal B, Agarwala S, Bakhshi S, Jain V,
Gupta AK, Kumar R, Bal CS, Iyer VK and Gupta SD: Bilateral primary
renal lymphoma with orbital metastasis in a child. Pediatr Blood
Cancer. 52:539–541. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Chatzipantelis P, Mastorakis E,
Tzortzakakis D and Salla C: Fine needle aspiration cytology
diagnosis of primary renal lymphoma involving the pleura: A case
report. Acta Cytol. 54:71–74. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Gupta A, Bhatt A, Khaira A, Gupta A and
Ran DS: Primary renal lymphoma: A differential diagnosis of renal
mass in a young male. Saudi J Kidney Dis Transpl. 21:544–545.
2010.PubMed/NCBI
|
|
43
|
Dash SC, Purohit K, Mohanty SK and Dinda
AK: An unusual case of bilateral renal enlargement due to primary
renal lymphoma. Indian J Nephrol. 21:56–58. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Vázquez-Alonso F, Puche-Sanz I,
Sánchez-Ramos C, Flores-Martin J, Vicente-Prados J and Cózar-Olmo
JM: Primary renal lymphoma: Long-term results of two patients
treated with a chemotherapy+rituximab protocol. Case Rep Oncol Med.
2012:7264242012.PubMed/NCBI
|
|
45
|
Brancato T, Alvaro R, Paulis G, Nupieri P,
D'Ascenzo R and Orsolini G: Primary lymphoma of the kidney: Case
report and review of literature. Case Rep Oncol Med. 10:60–62.
2012.
|
|
46
|
Hart S, Ellimoottil C, Shafer D, Mehta V
and Turk TM: A case of primary renal lymphoma. Urology. 80:763–765.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Hu R, Zhang R, Miao M, Zhu K, Yang W and
Liu Z: Central nervous system involvement of primary renal lymphoma
with diffuse large B-cell type lymphoma. Am J Case Rep. 14:292–294.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Dedekam E, Graham J, Strenge K and Mosier
AD: Primary renal lymphoma mimicking a subcapsular hematoma: A case
report. J Radiol Case Rep. 7:18–26. 2013.PubMed/NCBI
|
|
49
|
Hayakawa A, Shimotake N, Kubokawa I,
Mitsuda Y, Mori T, Yanai T, Muramaki M, Miyake H, Fujisawa M and
Iijima K: Primary pediatric stage III renal diffuse large B-cell
lymphoma. Am J Case Rep. 14:34–37. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Kumar BJ Naveen, Barman P, Chowdhury N and
Bora M: Primary renal lymphoma: An unusual presentation of
non-Hodgkin's lymphoma. Indian J Cancer. 51:370–371. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Geetha N, Shahid A, Rajan V and Jacob PM:
Primary renal lymphoma - A case report. Ecancermedicalscience.
8:4662014.PubMed/NCBI
|