Introduction
Hepatocellular carcinoma (HCC) is one of the most
prevalent malignancies worldwide, the seventh most common cancer,
and the third leading cause of cancer-related deaths (1). Although operative mortality and
morbidity of hepatic resection in patients with HCC have been
minimized by advances in surgical techniques, instruments, and
perioperative management, therapeutic outcomes remain
unsatisfactory due to the high incidence of recurrence (2,3).
Therefore, it is important to clarify the predictor of HCC
recurrence and prognosis for decision making in additional adjuvant
treatment after hepatic resection, preoperatively. Several
investigators have reported tumor size, vascular invasion,
intrahepatic metastasis, tumor markers, excessive blood loss, and
allogenic blood transfusion as factors associated with recurrence
of HCC (4–7). Unlike other solid malignancies, the
prognosis of HCC is not solely dependent on tumor burden but also
adversely influenced by impaired liver function secondary due to
the underlying pathogenic condition (8).
The presence of the systemic inflammatory response
is associated with poor therapeutic outcome in patients with
malignant tumors. Several recent investigators reported that the
systemic inflammatory response by the combination of serum
C-reactive protein (CRP) and albumin concentrations, i.e., Glasgow
prognostic score (GPS), predicts cancer-specific survival (9–14). We
previously reported the GPS as a predictor of long-term therapeutic
outcome for hepatobiliary malignancies, including carcinoma of the
ampulla of Vater (15), gallbladder
cancer (16), and unresectable
colorectal cancer liver metastasis (17). However, there have been only few
reports on the relationship between the GPS and long-term outcome
after hepatic resection for HCC (18,19). In
this study, we retrospectively evaluated whether the GPS predicts
disease-free or overall survival after hepatic resection for
HCC.
Patients and methods
Between January 2002 and December 2011, 159 patients
underwent primary hepatic resection for HCC at the Department of
Surgery, The Jikei University Hospital (Tokyo, Japan). Of these, 15
patients were excluded, nine due to additional procedures for other
malignancies, six due to lack of data, leaving the remaining 144
patients for the study. Generally, the extent of hepatic resection
was determined based on retention rate of indocyanine green at 15
min (ICGR15) before surgery and in reference to the
hepatic reserve as described by Miyagawa et al (20).
Hemogram and chemistry profile were routinely
measured for each patient preoperatively. For the assessment of
systemic inflammatory response using the GPS, the patients were
classified into three groups: Patients with normal albumin (≥3.5
g/dl) and normal CRP (≤1.0 mg/dl) as GPS 0, those with low albumin
(<3.5 g/dl) or elevated CRP (>1.0 mg/dl) as GPS 1, and both
low albumin (<3.5 g/dl) and elevated CRP (>1.0 mg/dl) as GPS
2. Patient characteristics were classified into two groups for
log-rank test and the Cox proportional hazard regression model.
Patient age was classified as <65 or ≥65 years. Body mass index
(BMI) was classified as <25 or ≥25. Preoperative
ICGR15 was classified as ≤10% or >10%. Preoperative
serum α-fetoprotein (AFP) was classified as ≤20 or >20 ng/ml.
The type of resection was classified as anatomical resection
(extended lobectomy, lobectomy, segmentectomy or subsegmentectomy)
or non-anatomical limited partial resection. Duration of operation
was classified as <360 or ≥360 min. Blood loss was classified as
<1,000 or ≥1,000 g. Maximal tumor diameter was classified as ≤2,
>2 ≤5, or >5 cm.
We investigated the relation between
clinicopathologic variables and GPS by univariate analysis. The
factors consisted of the following 17 factors: Age, sex, BMI,
hepatitis virus status, Child classification, preoperative
ICGR15, preoperative serum AFP, type of resection,
duration of operation, blood loss, red cell concentrate (RC)
transfusion, fresh frozen plasma (FFP) transfusion, maximal tumor
diameter, tumor number, portal or venous invasion, coexistent
disease, and incidence of postoperative complications.
Next, we investigated the relation between
clinicopathologic variables and disease-free as well as overall
survival after hepatic resection for HCC by univariate and
multivariate analyses. The factors consisted of the following 16
factors: Age, sex, BMI, hepatitis virus status, Child
classification, preoperative ICGR15, preoperative serum
AFP, type of resection, duration of operation, blood loss, RC
transfusion, FFP transfusion, maximal tumor diameter, tumor number,
portal or venous invasion, and the GPS grade.
Recurrence of HCC was defined as newly detected
hypervascular hepatic or extrahepatic tumors by ultrasonography,
computed tomography, magnetic resonance image or angiography, with
or without increase in serum a-fetoprotein, or protein induced by
vitamin K absence or antagonist-II. For recurrent HCC in the liver,
repeated hepatic resection, local ablation therapy or transarterial
chemoembolization was given based on hepatic functional reserve
judged mainly by ICGR15 and the size, number as well as
location of the recurrent tumors. Extrahepatic recurrence was
mainly treated conservatively.
Pulmonary complications were defined as
postoperative pneumonia; postoperative respiratory failure with
pyrexia, dyspenia, and a pulmonary infiltrate on chest X-ray; or
pleural effusion that required thoracentesis. Bile leakage was
defined as a discharge of fluid with an increased bilirubin
concentration (at least 3 times the serum bilirubin concentration
measured at the same time) via the intra-abdominal drains on or
after postoperative day 3 or as the need for radiologic
intervention (i.e., interventional drainage) and relaparotomy for
biliary collections and bile peritonitis, respectively (21). Surgical site infection was defined as
surgical wound infection that affect superficial tissues (skin and
subcutaneous layer) and the deeper tissues (deep incisional or
organ-space) of the incision according to the Centers for Disease
Control and Prevention definitions (22).
This retrospective study was approved by the Ethics
Committee of Jikei University School of Medicine (no. 21–121).
Statistical analysis
Patients' characteristics were analyzed using the
non-paired Student's t-test and Chi-square test. Survival
analyses were performed using Kaplan-Meier method, the Log-rank
test, and the Cox proportional regression model with backward
elimination stepwise approach. All P-values were considered
statistically significant when the associated probability was less
than 0.05. These analyses were conducted using IBM® SPSS
statistics version 20.0 (IBM Japan, Tokyo, Japan).
Results
Patient characteristics, and
univariate analysis of the association between clinicopathologic
variables and Glasgow prognostic score
Patient characteristics, univariate analysis of the
relationship between clinicopathologic variables and the GPS grade
are outlined in Table I. Among the
study population, GPS consisted of GPS 0 in 76, GPS 1 in 58 (low
albumin; n=8, elevated CRP; n=50), and GPS 2 in 10 patients,
respectively. In this study, the five-year disease-free and overall
survival rates after hepatic resection for HCC were 32.9 and 74.5%,
respectively. In univariate analysis of the relationship between
clinicopathologic variables and the GPS grade, maximal tumor
diameter was positively associated with the GPS grade (P=0.002).
Ratio of patients with Child classification B tended to be
positively associated with the GPS grade, which however did not
achieved significance (P=0.053). Coexistent diabetes mellitus was
positively associated with the GPS grade (P=0.008). Post-operative
complications developed in 43 of 144 patients (29.9%), consisting
of pulmonary complications in 11 (7.6%), bile leakage in 12,
(8.3%), massive ascites in 7 (4.9%), and surgical site infection
(SSI) in 11 patients (7.6%), respectively. The GPS grade was
negatively associated with the incidence of SSI (P=0.021). Other
complications were comparable among the three GPS grades.
In-hospital mortality was 3 of 144 patients (2.1%), consisting of
postoperative liver failure in two (1.4%) and sepsis in one patient
(0.7%), respectively.
 | Table I.Patients' characteristics, and
univariate analysis of clinicopathologic variables in relation to
Glasgow prognostic score after elective hepatic resection for
hepatocellular carcinoma. |
Table I.
Patients' characteristics, and
univariate analysis of clinicopathologic variables in relation to
Glasgow prognostic score after elective hepatic resection for
hepatocellular carcinoma.
|
|
| Glasgow prognostic
score |
|
|---|
| P-value
(univariate) |
|---|
| Factor | All patients | 0 (n=76) | 1 (n=58) | 2 (n=10) |
|---|
| Age (years) | 63
(57–71)a | 63 (56–68) | 66 (58–72) | 66 (62–71) | 0.246 |
| Sex
(male:female) | 125:19 | 66:10 | 49:9 | 10:0 | 0.408 |
| Body mass index | 23.3 (21.3–25.4) | 22.9 (21.2–25.4) | 23.3 (21.5–25.0) | 25.3 (23.8–26.9) | 0.159 |
| Hepatitis virus
(HBV:HCV:none) | 38:55:51 | 23:32:21 | 13:21:24 | 2:2:6 | 0.218 |
| Child classification
(A:B) | 134:10 | 74:2 | 52:6 | 8:2 | 0.053 |
| ICGR15
(%) | 12 (8–19) | 12 (8–16) | 13 (9–23) | 13 (8–21) | 0.149 |
| Serum α-fetoprotein
(ng/ml) | 13.7 (5–119.5) | 11 (4.8–26.2) | 38 (6.7–330.0) | 21.5 (10.9–36.7) | 0.183 |
| Type of resection
(anatomical:partial) | 78:66 | 43:33 | 30:28 | 5:5 | 0.824 |
| Duration of operation
(min) | 371 (262–480) | 377 (239–480) | 368 (285–473) | 315 (263–452) | 0.692 |
| Intraoperative blood
loss (g) | 682 (308–1403) | 622 (325–1136) | 1,018
(352–1,845) | 360 (183–760) | 0.125 |
| RC transfusion
(present:absent) | 33:111 | 13:63 | 18:40 | 2:8 | 0.160 |
| FFP transfusion
(present:absent) | 26:118 | 12:64 | 12:46 | 2:8 | 0.755 |
| Tumor diameter
(cm) | 3.2 (2.2–5.5) | 3.0 (2.2–4.2) | 4.0 (2.4–7.4) | 4.0 (2.6–8.2) | 0.002 |
| Tumor number
(single:double:triple or more) | 114:13:17 | 62:9:5 | 43:4:11 | 9:0:1 | 0.161 |
| Portal or venous
invasion (positive:negative) | 33:111 | 15:61 | 16:42 | 2:8 | 0.549 |
| Coexistent
disease |
|
|
|
|
|
|
Hypertension
(present:absent) | 64:80 | 34:42 | 27:31 | 3:7 | 0.621 |
| Diabetes
mellitus (present:absent) | 40:104 | 19:57 | 14:44 | 7:3 | 0.008 |
|
Hyperlipidemia
(present:absent) | 18:126 | 10:66 | 6:52 | 2:8 | 0.673 |
| Postoperative
complications |
|
|
|
|
|
|
Pulmonary complications
(present:absent) | 11:133 | 5:71 | 4:54 | 2:8 | 0.312 |
| Massive
ascites (present:absent) |
7:137 | 3:73 | 4:54 |
0:10 | 0.558 |
| Biliary
leakage (present:absent) | 12:132 | 3:73 | 7:51 | 2:8 | 0.093 |
|
Surgical site infection
(present:absent) | 11:133 | 4:72 | 4:54 | 3:7 | 0.021 |
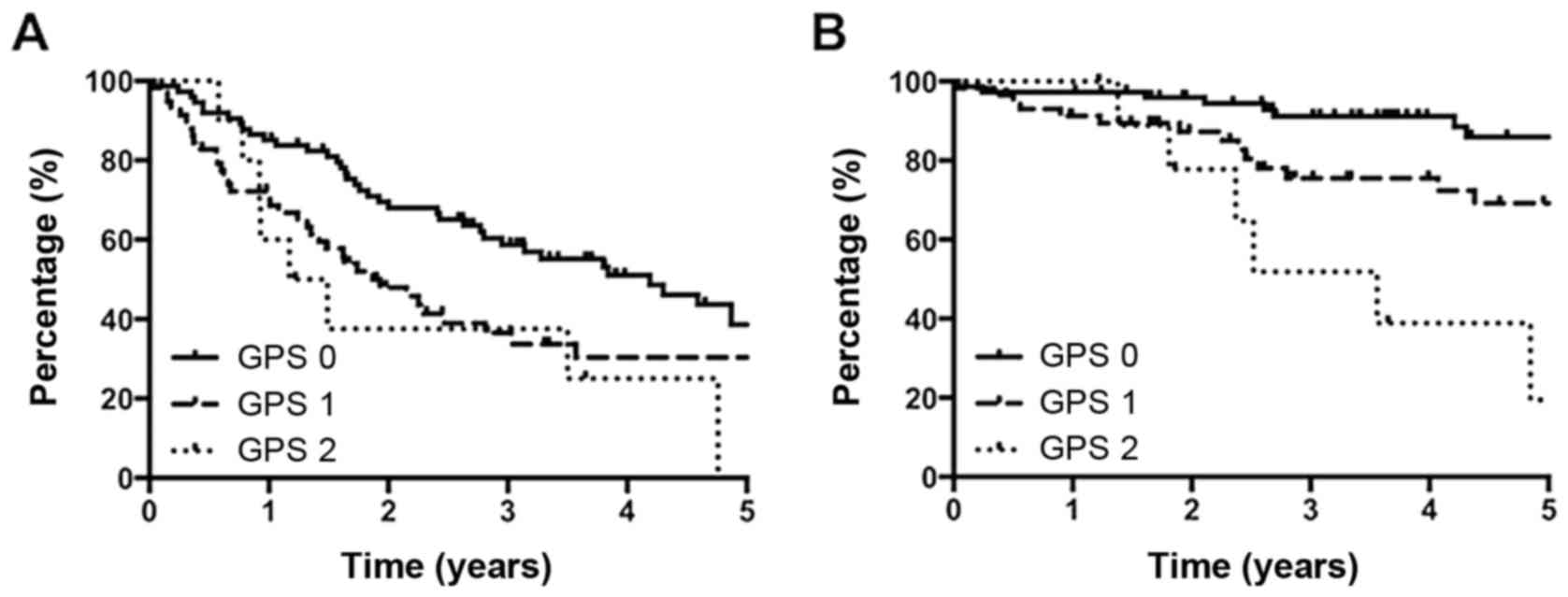
Univariate analysis of
clinicopathologic variables in relation to disease-free as well as
overall survival after hepatic resection for hepatocellular
carcinoma
Table II lists
univariate analysis of the relationship between the
clinicopathologic variables and disease-free as well as overall
survival after hepatic resection for HCC. In univariate analysis of
disease-free survival, ≥65 years of age (P=0.015), >20 ng/ml of
preoperative serum AFP (P=0.015), tumor number of triple or more
(P=0.003), positive portal or venous invasion (P=0.048), and GPS 2
(Fig. 1A; P=0.036) demonstrated
significant correlating with cancer recurrence. In overall
survival, >5 cm of maximal tumor diameter (P=0.011), tumor
number of triple or more (P=0.017), positive portal or venous
invasion (P<0.001), and GPS 1 (Fig.
1B; P=0.022) and GPS 2 (P<0.001) were significantly
associated with poor outcome. More than 200 ng/ml of preoperative
serum AFP tended to be associated with poor overall survival, which
however was not significant (P=0.070).
 | Table II.Univariate analysis of
clinicopathologic variables in relation to disease-free and overall
survival after elective hepatic resection for hepatocellular
carcinoma. |
Table II.
Univariate analysis of
clinicopathologic variables in relation to disease-free and overall
survival after elective hepatic resection for hepatocellular
carcinoma.
|
|
| Disease-free
survival | Overall
survival |
|---|
|
|
|---|
| Factor | N | Hazard ratio (95%
CI) | P-value | Hazard ratio (95%
CI) | P-value |
|---|
| Age (years) |
|
|
|
|
|
|
≥65 | 66 | 1.660
(1.123–2.660) | 0.015 | 1.590
(0.7966–3.249) | 0.186 |
|
<65 | 78 | Ref |
| Ref |
|
| Sex |
|
|
|
|
|
|
Female | 19 | 1.159
(0.5641–2.438) | 0.672 | 1.610
(0.5709–5.571) | 0.322 |
|
Male | 125 | Ref |
| Ref |
|
| Body mass
index |
|
|
|
|
|
|
≥25 | 43 | 0.836
(0.5344–1.319) | 0.451 | 0.6755
(0.3258–1.493) | 0.355 |
|
<25 | 101 | Ref |
| Ref |
|
| Hepatitis
virus |
|
|
|
|
|
|
HBV | 38 | 0.732
(0.413–1.297) | 0.285 | 0.838
(0.318–2.203) | 0.719 |
|
HCV | 55 | 1.170
(0.725–1.888) | 0.521 | 1.294
(0.579–2.893) | 0.530 |
|
None | 51 | Ref |
| Ref |
|
| Child's
classification |
|
|
|
|
|
| B | 10 | 1.350
(0.5885–3.412) | 0.441 | 2.367
(0.8056–16.04) | 0.095 |
| A | 134 | Ref |
| Ref |
|
|
ICGR15 |
|
|
|
|
|
|
>10 | 86 | 1.217
(0.8024–1.860) | 0.358 | 1.402
(0.6954–2.795) | 0.351 |
|
≤10 | 58 | Ref |
| Ref |
|
| Serum α-fetoprotein
(ng/ml) |
|
|
|
|
|
|
>20 | 60 | 1.407
(0.9260–2.210) | 0.015 | 1.878
(0.9483–3.964) | 0.070 |
|
≤20 | 84 | Ref |
| Ref |
|
| Type of
resection |
|
|
|
|
|
|
Anatomical | 78 | 0.9672
(0.6364–1.468) | 0.874 | 1.755
(0.8796–3.519) | 0.114 |
|
Partial | 66 | Ref |
| Ref |
|
| Duration of
operation (min) |
|
|
|
|
|
|
≥360 | 77 | 1.198
(0.7917–1.826) | 0.393 | 0.8851
(0.4420–1.768) | 0.729 |
|
<360 | 67 | Ref |
| Ref |
|
| Intraoperative
blood loss (g) |
|
|
|
|
|
|
≥1,000 | 54 | 1.400
(0.9207–2.223) | 0.114 | 1.712
(0.8590–3.612) | 0.123 |
|
<1,000 | 90 | Ref |
| Ref |
|
| RC transfusion |
|
|
|
|
|
|
Present | 33 | 1.443
(0.8914–2.549) | 0.127 | 1.657
(0.7659–4.135) | 0.181 |
|
Absent | 111 | Ref |
| Ref |
|
| FFP
transfusion |
|
|
|
|
|
|
Present | 26 | 1.357
(0.7836–2.526) | 0.255 | 1.794
(0.8126–4.952) | 0.131 |
|
Absent | 118 | Ref |
| Ref |
|
| Tumor diameter
(cm) |
|
|
|
|
|
|
>5 | 38 | 1.156
(0.831–1.607) | 0.389 | 2.061
(1.179–3.601) | 0.011 |
| >2,
≤5 | 75 | 0.963
(0.727–1.275) | 0.791 | 1.129
(0.666–1.914) | 0.653 |
| ≤2 | 31 | Ref |
| Ref |
|
| Tumor number |
|
|
|
|
|
| Triple
or more | 17 | 2.472
(1.352–4.522) | 0.003 | 2.853
(1.207–6.744) | 0.017 |
|
Double | 13 | 1.180
(0.563–2.473) | 0.660 | 0.791
(0.186–3.367) | 0.751 |
|
Single | 114 | Ref |
| Ref |
|
| Portal or venous
invasion |
|
|
|
|
|
|
Positive | 33 | 1.591
(1.010.2.925) | 0.048 | 4.483
(3.279.18.43) | <0.001 |
|
Negative | 111 | Ref |
| Ref |
|
| Glasgow prognostic
score |
|
|
|
|
|
| 2 | 10 | 2.258
(1.054.4.836) | 0.036 | 7.446
(2.656.20.879) | <0.001 |
| 1 | 58 | 1.503
(0.963.2.346) | 0.073 | 2.530
(1.146.5.585) | 0.022 |
| 0 | 76 | Ref |
| Ref |
|
Multivariate analysis of
clinicopathologic variables in relation to disease-free as well as
overall survival after hepatic resection for hepatocellular
carcinoma
Table III lists
multivariate analysis of the relationship between the
clinicopathologic variables and disease-free as well as overall
survival after hepatic resection for HCC. In multivariate analysis
of disease-free survival, tumor number of triple or more (P=0.004),
positive portal or venous invasion (P=0.034), and GPS 2 (P=0.019)
were independent risk factors of cancer recurrence. In overall
survival, positive portal or venous invasion (P=0.034), and GPS 1
(P=0.042) or GPS 2 (P<0.001) were independent risk factors of
poor outcome.
 | Table III.Multivariate analysis of
clinicopathologic variables in relation to disease-free and overall
survival after elective hepatic resection for hepatocellular
carcinoma. |
Table III.
Multivariate analysis of
clinicopathologic variables in relation to disease-free and overall
survival after elective hepatic resection for hepatocellular
carcinoma.
|
|
| Disease-free
survival | Overall
survival |
|---|
|
|
|---|
| Factor | N | Hazard ratio (95%
CI) | P-value | Hazard ratio (95%
CI) | P-value |
|---|
| Tumor number |
|
|
|
|
|
| Triple
or more | 17 | 2.468
(1.333–4.571) | 0.004 | – | – |
|
Double | 13 | 1.383
(0.653–2.933) | 0.397 | – | – |
|
Single | 114 | Ref |
| – | – |
| Portal or venous
invasion |
|
|
|
|
|
|
Positive | 33 | 1.680
(1.041–2.713) | 0.034 | 4.494
(2.226–9.073) | <0.001 |
|
Negative | 111 | Ref |
| Ref |
|
| Glasgow prognostic
score |
|
|
|
|
|
| 2 | 10 | 2.527
(1.163–5.490) | 0.019 | 8.012
(2.818–22.784) | <0.001 |
| 1 | 58 | 1.392
(0.882–2.198) | 0.156 | 2.277
(1.029–5.039) | 0.042 |
| 0 | 76 | Ref |
| Ref |
|
Discussion
Recent studies have reported the prognostic
significance of the preoperative inflammation-based scores, such as
the GPS, the neutrophil to lymphocyte ratio (23), the platelet to lymphocyte ratio
(24), the Prognostic index (25), and the Prognostic nutritional index
(26). An inflammatory response to
the tumor leads to tumor proliferation and metastasis due to
inhibition of apoptosis and promotion of angiogenesis (27–30). The
GPS is a clinically useful inflammation-based prognostic scoring
system for predicting the postoperative prognosis of the patients
with colorectal cancer (9),
esophageal cancer (10), bladder
cancer (11), pancreatic head cancer
(12), renal clear cell cancer
(13), non-small cell lung cancer
(14), and HCC (18,19). The
GPS is evaluated using only serum CRP and serum albumin, which are
common laboratory parameters for assessment of pre- and
postoperative patients status. Therefore the GPS could stratify the
patients with malignant tumors on prognosis after surgical
resection easily, less-expensive, and less-invasive. Most HCC
patients suffered from chronic hepatitis or cirrhosis, and
synthesis of protein such as CRP and albumin are impaired.
Disease-free survival is probably affected by
remnant liver volume and remnant liver functional reserve. We hope
to show the relationship between remnant liver volume and
therapeutic outcome after hepatic resection for HCC in future
study.
In this study, tumor number of 3 or more, positive
portal or venous invasion, and GPS 2 were independent risk factors
of cancer recurrence in multivariate analysis. Positive portal or
venous invasion, and GPS 1 and 2 were also independent risk factors
of poor overall survival in multivariate analysis. To the best of
our knowledge, this is the first study that patients were clearly
stratified on risk of poor overall survival after hepatic resection
for HCC with respect to grade of the GPS. Moreover, on
postoperative infectious complications, the incidence of surgical
site infection was greater, and that of biliary leakage tended to
correlate with the GPS grade in univariate analysis. Therefore, the
GPS may be able to stratify the patients with HCC on risks of
postoperative complications as well as cancer recurrence and
prognosis after hepatic resection.
The GPS upon diagnosis in patients with HCC was an
independent predictor in disease-free and overall survival after
hepatic resection. Measurement of GPS may help decision making in
the post-operative management of patients with HCC.
References
|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2015. CA Cancer J Clin. 65:5–29. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Poon RT, Fan ST, Lo CM, Ng IO, Liu CL, Lam
CM and Wong J: Improving survival results after resection of
hepatocellular carcinoma: A prospective study of 377 patients over
10 years. Ann Surg. 234:63–70. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Poon RT, Ng IO, Fan ST, Lai EC, Lo CM, Liu
CL and Wong J: Clinicopathologic features of long-term survivors
and disease-free survivors after resection of hepatocellular
carcinoma: A study of a prospective cohort. J Clin Oncol.
19:3037–3044. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Katz SC, Shia J, Liau KH, Gonen M, Ruo L,
Jarnagin WR, Fong Y, D'Angelica MI, Blumgart LH and Dematteo RP:
Operative blood loss independently predicts recurrence and survival
after resection of hepatocellular carcinoma. Ann Surg. 249:617–623.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Arii S, Tanaka J, Yamazoe Y, Minematsu S,
Morino T, Fujita K, Maetani S and Tobe T: Predictive factors for
intrahepatic recurrence of hepatocellular carcinoma after partial
hepatectomy. Cancer. 69:913–919. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yanaga K: Current status of hepatic
resection for hepatocellular carcinoma. J Gastroenterol.
39:919–926. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Shiba H, Ishida Y, Wakiyama S, Iida T,
Matsumoto M, Sakamoto T, Ito R, Gocho T, Furukawa K, Fujiwara Y,
Hirohara S, et al: Negative impact of blood transfusion on
recurrence and prognosis of hepatocellular carcinoma after hepatic
resection. J Gastrointest Surg. 13:1636–1642. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tandon P and Garcia-Tsao G: Prognostic
indicators in hepatocellular carcinoma: A systematic review of 72
studies. Liver Int. 29:502–510. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
McMillian DC, Crozier JE, Canna K,
Angerson WJ and McArdle CS: Evaluation of an inflammation-based
prognostic score (GPS) in patients undergoing resection for colon
and rectal cancer. Int J Colorectal Dis. 22:881–886. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Crumley AB, McMillan DC, McKernan M, Going
JJ, Shearer CJ and Stuart RC: An elevated C-reactive protein
concentration, prior to surgery, predicts poor cancer-specific
survival in patients undergoing resection for gastro-oesophageal
cancer. Br J Cancer. 94:1568–1571. 2006.PubMed/NCBI
|
|
11
|
Hilmy M, Bartlett JM, Underwood MA and
McMillan DC: The relationship between the systemic inflammatory
response and survival in patients with transitional cell carcinoma
of the urinary bladder. Br J Cancer. 92:625–627. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Jamieson NB, Glen P, McMillan DC, McKay
CJ, Foulis AK, Carter R and Imrie CW: Systemic inflammatory
response predicts outcome in patients undergoing resection for
ductal adenocarcinoma head of pancreas. Br J Cancer. 92:21–23.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lamb GW, Aitchison M, Ramsey S, Housley SL
and McMillan DC: Clinical utility of the Glasgow Prognostic Score
in patients undergoing curative nephrectomy for renal clear cell
cancer: Basis of new prognostic scoring systems. Br J Cancer.
106:279–283. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hara M, Matsuzaki Y, Shimuzu T, Tomita M,
Ayabe T, Enomoto Y and Onitsuka T: Preoperative serum C-reactive
protein level in non-small cell lung cancer. Anticancer Res.
27:3001–3004. 2007.PubMed/NCBI
|
|
15
|
Shiba H, Misawa T, Fujiwara Y, Futagawa Y,
Furukawa K, Haruki K, Iwase R, Wakiyama S, Ishida Y and Yanaga K:
Glasgow prognostic score predicts therapeutic outcome after
pancreaticoduodenectomy for carcinoma of the ampulla of vater.
Anticancer Res. 33:2715–2721. 2013.PubMed/NCBI
|
|
16
|
Shiba H, Iwase R, Futagawa Y, Futagawa Y,
Furukawa K, Haruki K, Iwase R, Iida T and Yanaga K: Glasgow
prognostic score predicts therapeutic outcome after surgical
resection for gallbladder cancer. World J Surg. 39:753–758. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Furukawa K, Shiba H, Haruki K, Fujiwara Y,
Iida T, Mitsuyama Y, Ogawa M, Ishida Y, Misawa T and Yanaga K: The
Glasgow prognostic score is valuable for colorectal cancer with
both synchronous and metachronous unresectable liver metastases.
Oncol Lett. 4:324–328. 2012.PubMed/NCBI
|
|
18
|
Ishizuka M, Kubota K, Kita J, Shimoda M,
Kato M and Sawada T: Impact of an inflammation-based prognostic
system on patients undergoing surgery for hepatocellular carcinoma:
A retrospective study of 398 Japanese patients. Am J Surg.
203:101–106. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Horino K, Beppu T, Kuroki H, Mima K, Okabe
H, Nakahara O, Ikuta Y, Chikamoto A, Ishiko T, Takamori H and Baba
H: Glasgow prognostic score as a useful prognostic factor after
hepatectomy for hepatocellular carcinoma. Int J Clin Oncol.
18:829–838. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Miyagawa S, Makuuchi M, Kawasaki S and
Kakazu T: Criteria for safe hepatic resection. Am J Surg.
169:589–594. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Koch M, Garden OJ, Padbury R, Rahbari NN,
Adam R, Capussotti L, Fan ST, Yokoyama Y, Crawford M, Makuuchi M,
et al: Bile leakage after hepatobiliary and pancreatic surgery: A
definition and grading of severity by the International Study Group
of Liver Surgery. Surgery. 149:680–688. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Mangram AJ, Horan TC, Pearson ML, Silver
LC and Jarvis WR: Guideline for prevention of surgical site
infection, 1999. Centers for disease control and prevention (CDC)
hospital infection control practices advisory committee. Am J
Infect Control. 27:97–134; 96. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ding PR, An X, Zhang RX, Fang YJ, Li LR,
Chen G, Wu XJ, Lu ZH, Lin JZ, Kong LH, et al: Elevated preoperative
neutrophil to lymphocyte ratio predicts risk of recurrence
following curative resection for stage IIA colon cancer. Int J
Colorectal Dis. 25:1427–1433. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Shirai Y, Shiba H, Sakamoto T, Horiuchi T,
Haruki K, Fujiwara Y, Futagawa Y, Ohashi T and Yanaga K:
Preoperative platelet to lymphocyte ratio predicts outcome of
patients with pancreatic ductal adenocarcinoma after pancreatic
resection. Surgery. 158:360–365. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kasymjanova G, MacDonald N, Agulnik JS,
Cohen V, Pepe C, Kreisman H, Sharma R and Small D: The predictive
value of pre-treatment inflammatory markers in advanced
non-small-cell lung cancer. Curr Oncol. 17:52–58. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Kanda M, Fujii T, Kodera Y, Nagai S,
Takeda S and Nakao A: Nutritional predictors of postoperative
outcome in pancreatic cancer. Br J Surg. 98:268–274. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Balkwill F and Mantovani A: Inflammation
and cancer: Back to Virchow? Lancet. 357:539–545. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Coussens LM and Werb Z: Inflammation and
cancer. Nature. 420:860–867. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Mantovani A, Allavena P, Sica A and
Balkwill F: Cancer-related inflammation. Nature. 454:436–444. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Grivennikov SI, Greten FR and Karin M:
Immunity, inflammation, and cancer. Cell. 140:883–899. 2010.
View Article : Google Scholar : PubMed/NCBI
|