Introduction
Intrahepatic cholangiocarcinoma (ICC) constitutes
the second most prevalent primary hepatic malignancy following
hepatocellular carcinoma (HCC) (1,2). Whilst
more uncommon in the United States and Europe, the incidence rates
of this malignancy are high in China (2,3). Although
the diagnostic and surgical approaches for the treatment of ICC
have been improved to a certain extent, the survival rates for
patients with ICC remain unfavorable (4). As adjuvant therapy is frequently
ineffective for patients with ICC, complete surgical resection is
currently the only curative treatment (5). However, the majority of patients with
ICC are diagnosed at an advanced stage with intrahepatic and lymph
node metastases, when curative surgery is not a viable option
(6–8).
Despite numerous advances in ICC research, the mechanisms
underlying ICC progression remain poorly understood, and further
studies to identify diagnostic and prognostic factors are
required.
X-linked human ribosomal protein S4 (RPS4X) encodes
a component of the 40S subunit of the ribosomal complex (9) and is not subject to X-inactivation
(10). It has also been reported that
RPS4X haploinsufficiency serves a role in Turner syndrome (11). Previous studies have suggested that
RPS4X may be important in tumor progression, and demonstrated that
RPS4X physically interacts with Y-box binding protein-1 (YB-1) in
breast and ovarian cancer cell lines (12,13). The
RPS4X/YB-1 complex is critical in counteracting cisplatin
resistance in MCF7 and MDA-MB-231 breast cancer cells (12,13).
Furthermore, RPS4X has been identified as an independent prognostic
factor for ovarian and bladder cancer (13,14).
However, the potential diagnostic and prognostic function of RPS4X
in patients with ICC remains to be elucidated. In the present
study, the expression profile of RPS4X, and its diagnostic and
prognostic significance in patients with ICC was evaluated. This
may aid in the future treatment and management of patients with
ICC.
Patients and methods
Patients
A total of 201 patients (146 male, 55 female; age
range, 27–81) with ICC, who underwent surgical resection at the
Eastern Hepatobiliary Surgery Hospital (Shanghai, China) between
July 2000 and December 2006, were included in the current study.
Inflamed bile duct (IBD) samples were collected as normal control
tissues from 8 patients with ICC who underwent a hepatectomy at the
same hospital between March 2008 and September 2008. ICC tissue
samples were pathologically diagnosed at the time of surgery and
independently examined by two pathologists. No patients in the
present study received chemotherapy or radiotherapy prior to
surgery. Tumor stage was defined according to the American Joint
Committee on Cancer Tumor-Node-Metastasis (TNM) staging system
(15).
Follow-up
Patient follow-up examinations were performed
monthly for the first 2–3 months following surgery, and every 2–6
months thereafter. Where tumor recurrence or metastasis was
suspected, magnetic resonance imaging, positron emission
tomography-computed tomography and biopsies were performed. Overall
survival (OS) was defined as the time from the date of hepatectomy
to the final follow-up or mortality. The time to recurrence (TTR)
was defined as the time from the date of hepatectomy to the first
relapse, distant metastasis. The median follow-up time was 22.5
months (range, 0.2–92.3 months). Of the 201 patients with ICC, the
TTR information of 73 patients was not accessible for the follow-up
period or until the date of mortality.
For the use of clinical materials in the current
study, written informed consent was obtained from patients, in
addition to approval from The Ethics Committee of the Eastern
Hepatobiliary Surgery Hospital. All experiments were performed in
accordance with the approved guidelines of the Eastern
Hepatobiliary Surgery Hospital.
Tissue microarray construction (TMA),
immunohistochemistry (IHC), signal evaluation and integrated
optical density (IOD) analysis
TMA construction was performed as described
previously (16,17). Representative formalin-fixed
paraffin-embedded tumor tissues, fixed in 10% neutral formaldehyde
at room temperature for 12–24 h and embedded in paraffin, were
collected and used to construct a long-distance peritumoral TMA
chip. For IHC, 4-µm-thick sections were used and IOD analysis were
performed for evaluating the expression of RPS4X as described
previously (18). An anti-RPS4X
polyclonal antibody was purchased from Abmart (Shanghai, China;
dilution, 1:200; cat. no. P30129S) and an EnVision Detection kit
(cat. no. GK500705: Gene Tech, Shanghai, China), which included a
horseradish peroxidase secondary antibody, was used with ChemMate™
diaminobenzidine Chromogen reagent (Gene Tech Biotechnology Co.,
Ltd. Shanghai, China), to visualize tissue antigens. Slides
omitting the primary antibodies were produced as the negative
control for the IHC assay. Images were captured under high-power
magnification (×200, light microscopy). Mean IOD values were
calculated and analyzed using Image-Pro Plus software (version 6.0;
Media Cybernetics, Inc., Rockville, MD, USA). For the determination
of high or low RPS4X expression levels, optimal cutoff IOD values
were estimated using X-tile software (version 3.6.1; Yale
University, New Haven, CT, USA).
Statistical analysis
All statistical analyses were performed with SPSS
software (version 13.0; SPSS, Inc., Chicago, IL, USA). Differences
between variables were assessed using the χ2
(chi-square) test or Mann-Whitney U test (scatter dot plot). Data
are presented as the mean ± standard error of the mean. The
Kaplan-Meier estimator was used to assess survival and the log-rank
test was applied to compare survival rates between patient
subgroups. Univariate and multivariate analyses were performed
using the Cox's proportional hazards regression model. The
clinicopathological variables that were determined to be
significant in univariate analysis were further evaluated using
Cox's multivariate proportional hazards regression analysis.
Receiver operating characteristic (ROC) curve analysis was used to
determine the predictive significance of parameters. P<0.05 was
considered to indicate a statistically significant difference.
Results
RPS4X is significantly upregulated in
ICC tissue samples
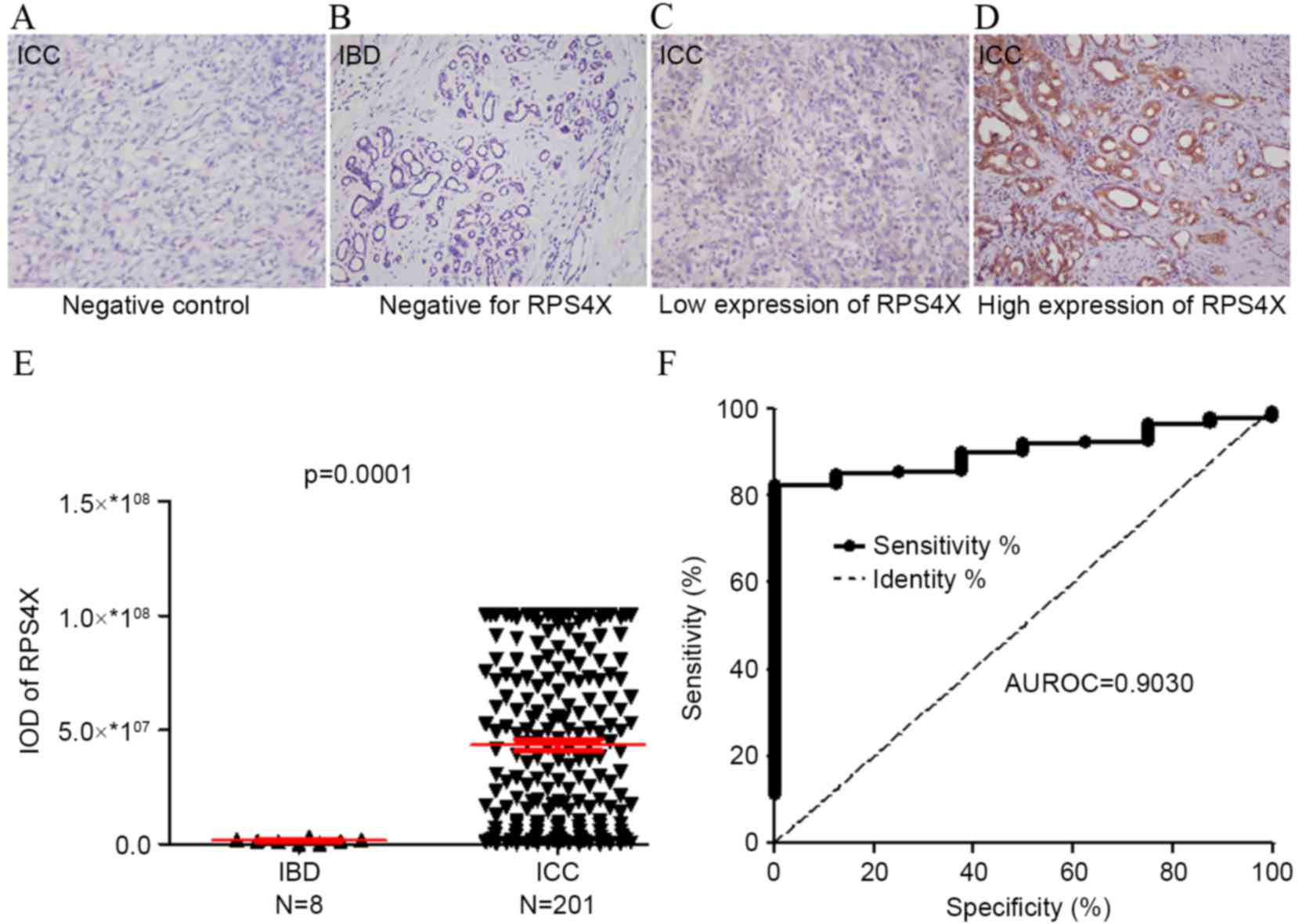
A total of 201 ICC tissue samples and 8 IBD tissue
samples used to construct a TMA, and RPS4X expression levels were
detected using IHC analysis (Fig. 1).
Staining for RPS4X in the ICC tissues (Fig. 1C and D) was observed to be
significantly more intense compared with that observed in the IBD
control tissues (Fig. 1B). The IOD of
each tissue sample was quantitatively analyzed, and the results
demonstrated that the staining intensity of RPS4X in the ICC group
was significantly higher compared with that of the IBD control
group (P=0.0001; Fig. 1E). In
addition, ROC analysis revealed that the area under the curve (AUC)
value of RPS4X was 0.9030, where the optimal cutoff IOD value was
29993910, providing a sensitivity of 82.59% and a specificity of
100% for detecting ICC (Fig. 1F).
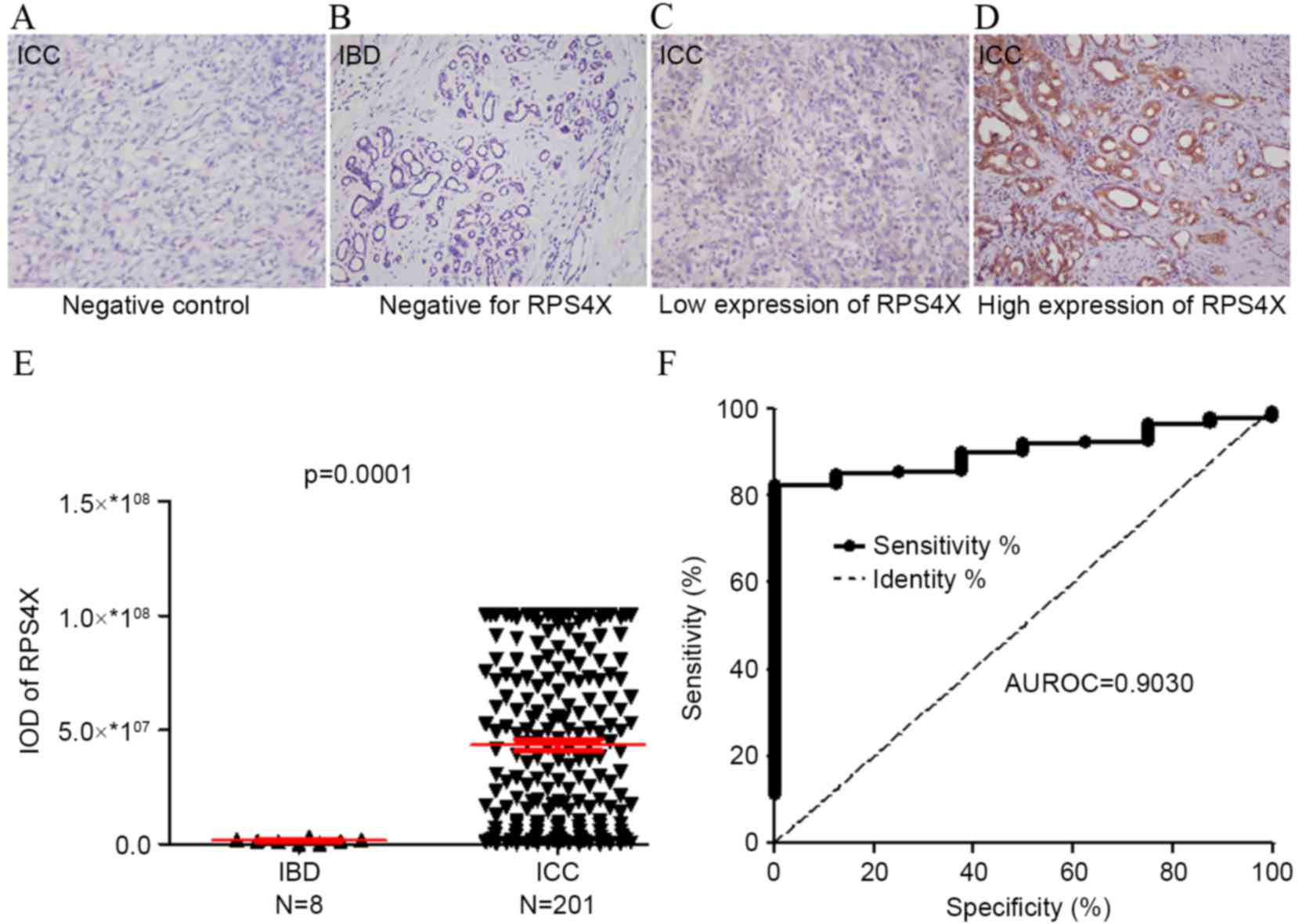 | Figure 1.RPS4X is significantly upregulated in
ICC tissue samples. RPS4X expression in 8 IBD cases and 201 ICC
cases was analyzed using immunohistochemistry. Representative
images (magnification, ×200) taken from the tissue microarray of
the (A) ICC negative control, (B) IBD negative for RPS4X, (C) ICC
with low expression of RPS4X and (D) ICC with high expression of
RPS4X. (E) The IOD for RPS4X was obtained and differences between
the ICC and IBD tissues were analyzed via the Mann-Whitney U test.
(F) ROC curve analysis of RPS4X for discriminating between ICC and
IBD lesions. At a cut-off IOD level of 29993910, RPS4X exhibited
82.59% sensitivity and 100% specificity for detecting ICC. AUROC,
0.9030; 95% confidence interval, 0.8533–0.9527. RPS4X, X-linked
ribosomal protein S4; IBD, inflamed bile duct; ICC intrahepatic
cholangiocarcinoma; IOD, integrated optical density; ROC, receiver
operator characteristic; AUROC, area under the ROC curve. |
High RPS4X expression levels are
associated with the clinicopathological features of patients with
ICC
The association between the clinicopathological
features of ICC and RPS4X expression levels was retrospectively
investigated (Table I). The cohort
included 91 cases of TNM stage I (45.3%), 79 cases of stage II
(39.3%), 5 cases of stage III (2.5%) and 26 cases of stage IV
(12.9%) ICC. RPS4X expression levels in the ICC tissue samples were
determined to be high in 111/201 cases (55.2%) and low in 90/201
cases (44.8%). χ2 test indicated a correlation between
RPS4X expression levels and serum alkaline phosphatase levels
(P=0.031). However, no significant association was observed between
RPS4X expression levels and other clinicopathological parameters,
including age, gender, liver cirrhosis, serum carcinoembryonic
antigen (CEA), serum carbohydrate antigen (CA) 19–9, serum alanine
transaminase, serum γ-glutamyl transpeptidase (GGT), tumor size,
tumor number, microvascular invasion and TNM stage.
 | Table I.Association between RPS4X expression
and the clinicopathological characteristics of patients with
ICC. |
Table I.
Association between RPS4X expression
and the clinicopathological characteristics of patients with
ICC.
|
| RPS4X |
|
|---|
|
|
|
|
|---|
| Clinicopathological
characteristic | Low | High | P-value |
|---|
| Age, years |
|
| 0.138 |
|
<52 | 40 | 61 |
|
>52 | 50 | 50 |
| Gender |
|
| 0.403 |
| Male | 68 | 78 |
|
Female | 22 | 33 |
| Liver cirrhosis
status |
|
| 0.138 |
|
Absent | 56 | 80 |
|
|
Present | 34 | 31 |
|
| Serum CEA, µg/l |
|
| 0.721 |
|
<5 | 72 | 91 |
|
|
>5 | 18 | 20 |
|
| Serum CA19-9,
U/ml |
|
| 0.573 |
| ≤37 | 41 | 55 |
|
|
>37 | 49 | 56 |
|
| Serum ALT, U/l |
|
| 0.172 |
| ≤75 | 80 | 91 |
|
|
>75 | 10 | 20 |
|
| Serum GGT, U/l |
|
| 0.180 |
| ≤50 | 36 | 34 |
|
|
>50 | 54 | 76 |
|
| Serum ALP, U/l |
|
| 0.031a |
|
<119 | 29 | 52 |
|
|
>119 | 61 | 58 |
|
| Tumor size, cm |
|
| 0.944 |
| ≤5 | 32 | 40 |
|
|
>5 | 58 | 71 |
|
| Tumor number |
|
| 0.487 |
|
Single | 72 | 93 |
|
|
Multiple | 18 | 18 |
|
| Microvascular
invasion status |
|
| 0.662 |
|
Absent | 59 | 76 |
|
|
Present | 31 | 35 |
|
| TNM stage |
|
| 0.899 |
| I | 41 | 50 |
|
| II | 34 | 45 |
|
|
III | 3 | 2 |
|
| IV | 12 | 14 |
|
High RPS4X expression levels indicate
poor survival in patients with ICC
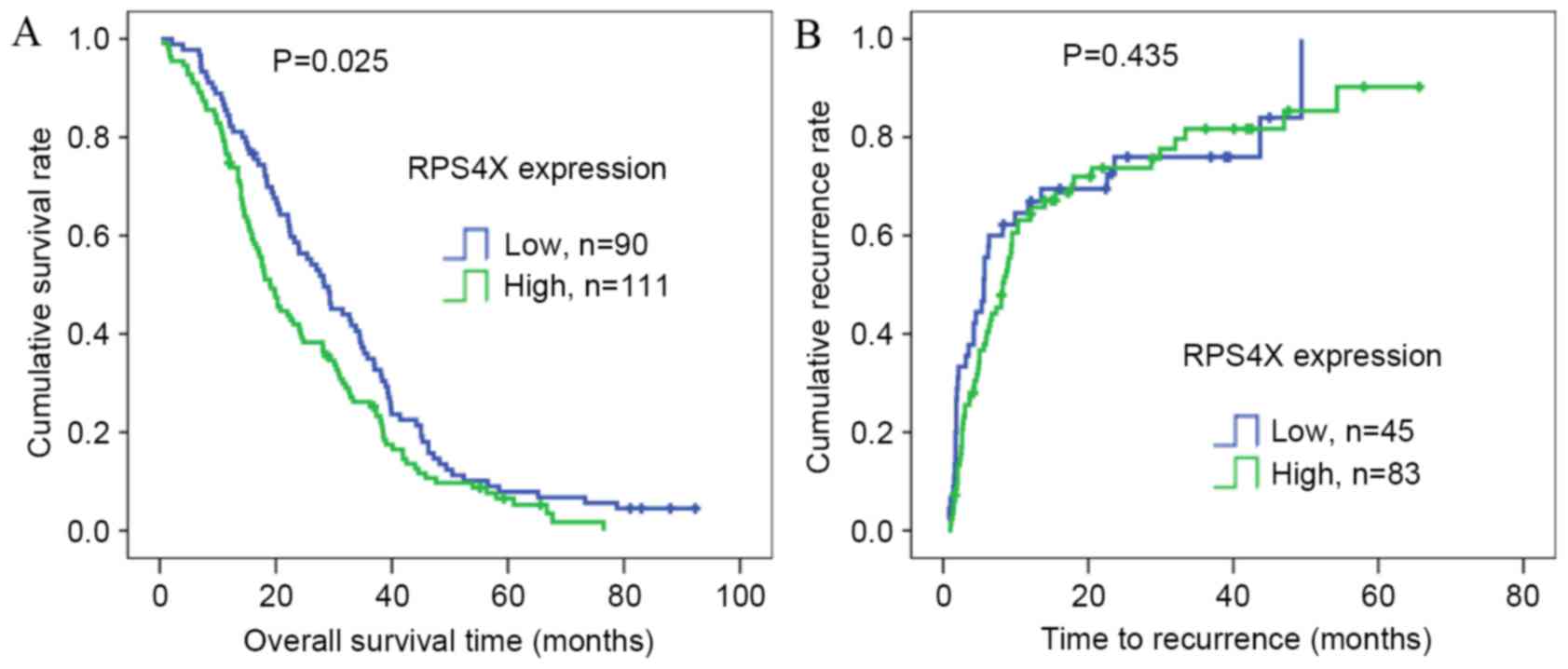
To determine the prognostic value of RPS4X in
postsurgical patients with ICC, Kaplan-Meier OS analysis was
conducted in 201 patients, and TTR analysis was performed in 128
patients according to the collected prognostic information.
Univariate and multivariate analyses of the risk factors
influencing OS and TTR are listed in Table II. Univariate analysis demonstrated
that serum GGT levels (P=0.029), tumor number (P=0.043), TNM stage
(P=0.003) and RPS4X expression (P=0.026) were significantly
associated with OS. Only tumor size (P=0.031) was significantly
associated with TTR, as demonstrated by univariate analysis. OS and
TTR curves according to the IOD values from RPS4X staining are
presented in Fig. 2, respectively. In
addition, Kaplan-Meier analyses revealed that a high RPS4X
expression may indicate poor survival rate of patients with ICC
following surgery (P=0.025; Fig. 2A),
but not TTR.
 | Table II.Univariate and multivariate analysis
of the prognostic value of the clinicopathological characteristics
of patients with ICC. |
Table II.
Univariate and multivariate analysis
of the prognostic value of the clinicopathological characteristics
of patients with ICC.
|
| OS | TTR |
|---|
|
|
|
|
|---|
|
| Univariate | Multivariate | Univariate | Multivariate |
|---|
|
|
|
|
|
|
|---|
| Clinicopathological
characteristic | P-value | HR | 95% Cl | P-value | P-value | HR | 95% Cl | P-value |
|---|
| Age, years: ≤52 vs.
>52 | 0.971 |
|
|
| 0.117 |
|
|
|
| Gender: Male vs.
female | 0.497 |
|
|
| 0.319 |
|
|
|
| Liver cirrhosis:
Absent vs. present | 0.970 |
|
|
| 0.453 |
|
|
|
| Serum CEA, µg/l:
≤10 vs. >10 | 0.065 |
|
|
| 0.957 |
|
|
|
| Serum CA19-9, U/ml:
≤75 vs. >75 | 0.099 |
|
|
| 0.552 |
|
|
|
| Serum ALT, U/l:
≤119 vs. >119 | 0.741 |
|
|
| 0.625 |
|
|
|
| Serum GGT, U/l: ≤50
vs. >50 | 0.029a |
|
| 0.134 | 0.373 |
|
|
|
| Serum ALP, U/l:
≤119 vs. >119 | 0.094 |
|
|
| 0.573 |
|
|
|
| Tumor size, cm: ≤5
vs. >5 | 0.085 |
|
|
| 0.031a | 1.608 | 1.045–2.472 | 0.031a |
| Tumor number:
Single vs. multiple | 0.043a |
|
| 0.144 | 0.188 |
|
|
|
| Microvascular
invasion: Absent vs. present | 0.078 |
|
|
| 0.847 |
|
|
|
| TNM stage: I vs. II
vs. III vs. IV | 0.003a | 1.258 | 1.086–1.457 | 0.002a | 0.135 |
|
|
|
| RPS4X expression:
Low vs. high | 0.026a | 1.424 | 1.065–1.904 | 0.017a | 0.438 |
|
|
|
As presented in Table
II, TNM stage [(hazard ratio (HR) 1.258; 95% confidence
interval (CI), 1.086–1.457; P=0.002)] and RPS4X staining intensity
(HR 1.424; 95% CI, 1.065–1.904; P=0.017) were the independent risk
factors identified for OS. Tumor size (HR 1.608; 95% CI
1.045–2.472; P=0.031) was identified as an independent risk factor
for TTR.
Discussion
ICC is a rare liver malignancy, originating from the
epithelium of the intrahepatic biliary duct (19). Due to its early-stage invasion,
widespread metastasis and ineffective therapeutic options, ICC has
a high mortality rate and a poor prognosis (20). Molecular profiling of the tumor is a
necessary part of treatment selection, and the immunohistochemical
assessment of ICC biomarkers can provide predictive and/or
prognostic information for patients with this disease. According to
numerous previous studies, the number of tumors (single vs.
multiple), completeness of resection (R0) and the presence of
vascular invasion and lymph node metastases are identified as the
most important prognostic factors in patients with ICC (21–24).
However, other potential prognostic biomarkers for ICC remain to be
elucidated.
Previous studies have demonstrated that low
expression levels of RPS4X were associated with an increased risk
of disease recurrence and mortality in patients with bladder and
ovarian cancer (13,14). The present study aimed to determine
the association between RPS4X expression levels and the clinical
outcome of patients with ICC. Tissue samples from a population of
201 patients with ICC and 8 patients with IBD were analyzed using
IHC. The results indicated that RPS4X expression was abnormally
increased in the ICC tissue specimens compared with the normal IBD
tissues. In this cohort of 201 patients with ICC, Kaplan-Meier OS
analysis demonstrated that high levels of RPS4X expression were
associated with a shorter survival time and poor prognosis
following surgical resection of the tumor. Multivariate Cox
regression analysis also revealed that RPS4X expression levels were
an independent prognostic marker in patients with ICC. However,
Kaplan-Meier analyses indicated no significant association between
RPS4X expression levels and TTR in the present study. Concordantly,
multivariate Cox regression analysis also excluded RPS4X expression
levels as an independent prognostic marker for TTR. However, the
missing TTR data (73/201) from the follow-up period potentially
impacted the TTR analysis. To the best of our knowledge, the
present study is the first to demonstrate that the overexpression
of RPS4X is associated with the poor prognosis of patients with
ICC.
The poor prognosis of patients with ICC following
tumor resection has not improved over the last decade, which is
primarily due to late stage diagnosis leading to high rates of
metastasis and recurrence (25,26).
Plasma serum markers for ICC, including CA19-9 and CEA, usually
possess high specificity, but low sensitivity; CA19-9 is increased
in ~50% of ICC cases, whereas CEA is elevated in 15–20% of ICC
cases (27,28). Therefore, these serum markers are
insufficiently sensitive for a definitive diagnosis. In the present
study, ROC analysis of RPS4X expression determined an AUC value of
0.9030 with a sensitivity of 82.59% and a specificity of 100%. This
result indicates that immunohistochemical staining of RPS4X in
tissues enables the differentiation between ICC tissues and IBD.
Tissue biopsy is not routinely recommended for patients with ICC
that are going to undergo curative resection (29). However, a pathological diagnosis is
required prior to systemic chemotherapy or radiotherapy (29), thus tissue markers, such as RPS4X
should be further assessed in biopsy tissues. A previous study
demonstrated that the knockdown of RPS4X expression was able to
decrease DNA synthesis and induce cisplatin resistance in MCF7 and
MDA-MB-231 breast cancer cell lines (11). However, whether RPS4X serves a role in
the response of patients with ICC to systemic adjuvant therapy,
including 5-FU (fluorouracil) -based radiation and
gemcitabine/5-FU, requires further clarification.
In conclusion, the findings of the present study
indicate that increased RPS4X expression levels are a diagnostic
and prognostic biomarker for ICC, which is able to independently
identify patients with a poor clinical prognosis.
Acknowledgements
The present study was supported by the Medical Guide
Fund of the Shanghai Science and Technology Committee (grant no.
134119a0202).
References
|
1
|
Zhang GW, Lin JH, Qian JP and Zhou J:
Identification of risk and prognostic factors for patients with
clonorchiasis-associated intrahepatic cholangiocarcinoma. Ann Surg
Oncol. 21:3628–3637. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Siegel R, Ma J, Zou Z and Jemal A: Cancer
statistics, 2014. CA Cancer J Clin. 64:9–29. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Patel T: Increasing incidence and
mortality of primary intrahepatic cholangiocarcinoma in the United
States. Hepatology. 33:1353–1357. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Brown KM, Parmar AD and Geller DA:
Intrahepatic cholangiocarcinoma. Surg Oncol Clin N Am. 23:231–246.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kawarada Y, Yamagiwa K and Das BC:
Analysis of the relationships between clinicopathologic factors and
survival time in intrahepatic cholangiocarcinoma. Am J Surg.
183:679–685. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Dhanasekaran R, Hemming AW, Zendejas I,
George T, Nelson DR, Soldevila-Pico C, Firpi RJ, Morelli G, Clark V
and Cabrera R: Treatment outcomes and prognostic factors of
intrahepatic cholangiocarcinoma. Oncol Rep. 29:1259–1267.
2013.PubMed/NCBI
|
|
7
|
Roayaie S, Guarrera JV, Ye MQ, Thung SN,
Emre S, Fishbein TM, Guy SR, Sheiner PA, Miller CM and Schwartz ME:
Aggressive surgical treatment of intrahepatic cholangiocarcinoma:
Predictors of outcomes. J Am Coll Surg. 187:365–372. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Zhou XD, Tang ZY, Fan J, Zhou J, Wu ZQ,
Qin LX, Ma ZC, Sun HC, Qiu SJ, Yu Y, et al: Intrahepatic
cholangiocarcinoma: Report of 272 patients compared with 5,829
patients with hepatocellular carcinoma. J Cancer Res Clin Oncol.
135:1073–1080. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Watanabe M, Furuno N, Goebl M, Go M,
Miyauchi K, Sekiguchi T, Basilico C and Nishimito T: Molecular
cloning of the human gene, CCG2, that complements the BHK-derived
temperature-sensitive cell cycle mutant tsBN63: Identity of CCG2
with the human X chromosomal SCAR/RPS4X gene. J Cell Sci.
100:35–43. 1991.PubMed/NCBI
|
|
10
|
Zinn AR, Alagappan RK, Brown LG, Wool I
and Page DC: Structure and function of ribosomal protein S4 genes
on the human and mouse sex chromosomes. Mol Cell Biol.
14:2485–2492. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Watanabe M, Zinn AR, Page DC and Nishimoto
T: Functional equivalence of human X- and Y-encoded isoforms of
ribosomal protein S4 consistent with a role in Turner syndrome. Nat
Genet. 4:268–271. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Garand C, Guay D, Sereduk C, Chow D,
Tsofack SP, Langlois M, Perreault E, Yin HH and Lebel M: An
integrative approach to identify YB-1-interacting proteins required
for cisplatin resistance in MCF7 and MDA-MB-231 breast cancer
cells. Cancer Sci. 102:1410–1417. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Tsofack SP, Meunier L, Sanchez L, Madore
J, Provencher D, Mes-Masson AM and Lebel M: Low expression of the
X-linked ribosomal protein S4 in human serous epithelial ovarian
cancer is associated with a poor prognosis. BMC Cancer. 13:3032013.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Paquet ÉR, Hovington H, Brisson H, Lacombe
C, Larue H, Têtu B, Lacombe L, Fradet Y and Lebel M: Low level of
the X-linked ribosomal protein S4 in human urothelial carcinomas is
associated with a poor prognosis. Biomark Med. 9:187–197. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Edge SB and Compton CC: The American joint
committee on cancer: The 7th edition of the AJCC cancer staging
manual and the future of TNM. Ann Surg Oncol. 17:1471–1474. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Albanghali M, Green A, Rakha E,
Aleskandarany M, Nolan C, Ellis I and Cheung KL: Construction of
tissue microarrays from core needle biopsy-a systematic literature
review. Histopathology. 68:323–332. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Tan D, Li Q, Deeb G, Ramnath N, Slocum HK,
Brooks J, Cheney R, Wiseman S, Anderson T and Loewen G: Thyroid
transcription factor-1 expression prevalence and its clinical
implications in non-small cell lung cancer: A high-throughput
tissue microarray and immunohistochemistry study. Hum Pathol.
34:597–604. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Jin GZ, Li Y, Cong WM, Yu H, Dong H, Shu
H, Liu XH, Yan GQ, Zhang L, Zhang Y, et al: iTRAQ-2DLC-ESI-MS/MS
based identification of a new set of immunohistochemical biomarkers
for classification of dysplastic nodules and small hepatocellular
carcinoma. J Proteome Res. 10:3418–3428. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sang H, Li T, Li H and Liu J: Gab1
regulates proliferation and migration through the PI3K/Akt
signaling pathway in intrahepatic cholangiocarcinoma. Tumour Biol.
36:8367–8377. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hyder O, Hatzaras I, Sotiropoulos GC, Paul
A, Alexandrescu S, Marques H, Pulitano C, Barroso E, Clary BM,
Aldrighetti L, et al: Recurrence after operative management of
intrahepatic cholangiocarcinoma. Surgery. 153:811–818. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ali SM, Clark CJ, Zaydfudim VM, Que FG and
Nagorney DM: Role of major vascular resection in patients with
intrahepatic cholangiocarcinoma. Ann Surg Oncol. 20:2023–2028.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
de Jong MC, Nathan H, Sotiropoulos GC,
Paul A, Alexandrescu S, Marques H, Pulitano C, Barroso E, Clary BM,
Aldrighetti L, et al: Intrahepatic cholangiocarcinoma: An
international multi-institutional analysis of prognostic factors
and lymph node assessment. J Clin Oncol. 29:3140–3145. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Endo I, Gonen M, Yopp AC, Dalal KM, Zhou
Q, Klimstra D, D'Angelica M, DeMatteo RP, Fong Y, Schwartz L, et
al: Intrahepatic cholangiocarcinoma: Rising frequency, improved
survival, and determinants of outcome after resection. Ann Surg.
248:84–96. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ribero D, Pinna AD, Guglielmi A, Ponti A,
Nuzzo G, Giulini SM, Aldrighetti L, Calise F, Gerunda GE, Tomatis
M, et al: Surgical approach for long-term survival of patients with
intrahepatic cholangiocarcinoma: A multi-institutional analysis of
434 patients. Arch Surg. 147:1107–1113. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Razumilava N and Gores GJ:
Cholangiocarcinoma. Lancet. 383:2168–2179. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Rizvi S and Gores GJ: Pathogenesis,
diagnosis, and management of cholangiocarcinoma. Gastroenterology.
145:1215–1229. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Luo X, Yuan L, Wang Y, Ge R, Sun Y and Wei
G: Survival outcomes and prognostic factors of surgical therapy for
all potentially resectable intrahepatic cholangiocarcinoma: A large
single-center cohort study. J Gastrointest Surg. 18:562–572. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Maithel SK, Gamblin TC, Kamel I,
Corona-Villalobos CP, Thomas M and Pawlik TM: Multidisciplinary
approaches to intrahepatic cholangiocarcinoma. Cancer.
119:3929–3942. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Weber SM, Ribero D, O'Reilly EM, Kokudo N,
Miyazaki M and Pawlik TM: Intrahepatic Cholangiocarcinoma: Expert
consensus statement. HPB (Oxford). 17:669–680. 2015. View Article : Google Scholar : PubMed/NCBI
|