Introduction
Female Wolffian adnexal tumor was first reported in
detail in 1973 by Kariminejad and Scully (1) in a study of 9 cases and named ‘female
adnexal tumor of probable Wolffian origin (FATWO)’. The World
Health Organization subsequently renamed FATWO as Wolffian adnexal
tumor (WAT) in 2003. WAT is a rare neoplasm arising from the
remnants of the mesonephric duct and predominantly occurs in the
broad ligament; however, WAT may occur in the ovaries, fallopian
tubes and peritoneum (2). WAT is
typically known to behave in a benign manner; however, under
certain circumstances more aggressive behaviors have been observed
(3). WAT is misdiagnosed due to its
rarity and non-specific clinical features and pathological
histology forms (4). Therefore, owing
to the limited cases and literature, there are no recommended
therapeutic approaches (5). In the
present study, a case of WAT in the ovary was examined, literature
associated with WAT was reviewed and the surgery methods for
patients with WAT were summarized.
Case report
On 28 October 2015, 20 years following a
hysteromyomectomy, a 73-year-old female visited the outpatient
department of the Department of General Surgery, Ninth People's
Hospital (Shanghai, China), presenting with abdominal pain and
bloating for the previous 2 weeks. An abdominal examination
revealed that the patient exhibited abdominal distention, palpation
revealed a large lump with an unclear boundary, but there was no
tenderness or rebound tenderness. An ultrasound scan identified a
large mass and the patient required additional computed tomography
(CT) or magnetic resonance imaging (MRI) examination. The patient
was admitted to the Ninth People's Hospital (Shanghai, China) to
conduct a more detailed examination. Chest X-ray and serum tumor
markers (including a-fetoprotein, carcinoembryonic antigen, cancer
antigen (CA) 199, CA153, CA724 and CA125) were unremarkable and
cardiopulmonary function was acceptable. A routine blood test
identified a moderate inflammatory reaction and slightly decreased
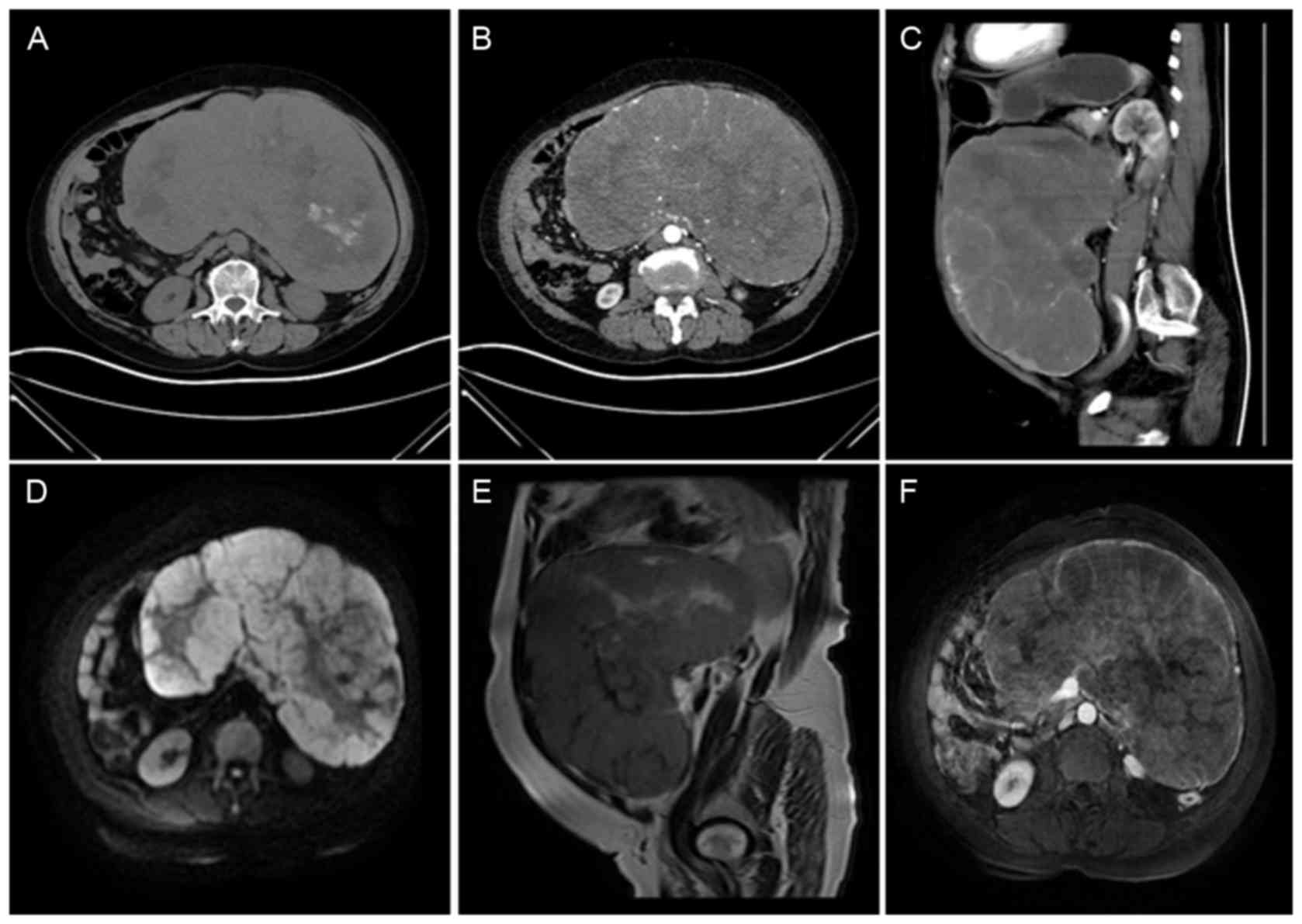
levels of serum albumin. Whole abdomen CT scan and MRI imaging
examinations were conducted (Fig. 1)
which confirmed that there was a large abnormal lobulated soft
tissue mass, the origin of which was uncertain. Since the patient's
abdominal pain and bloating did not improve, and may have worsened
with the increasing tumor size, an exploratory laparotomy was
conducted, following consent being obtained from the patient's
family.
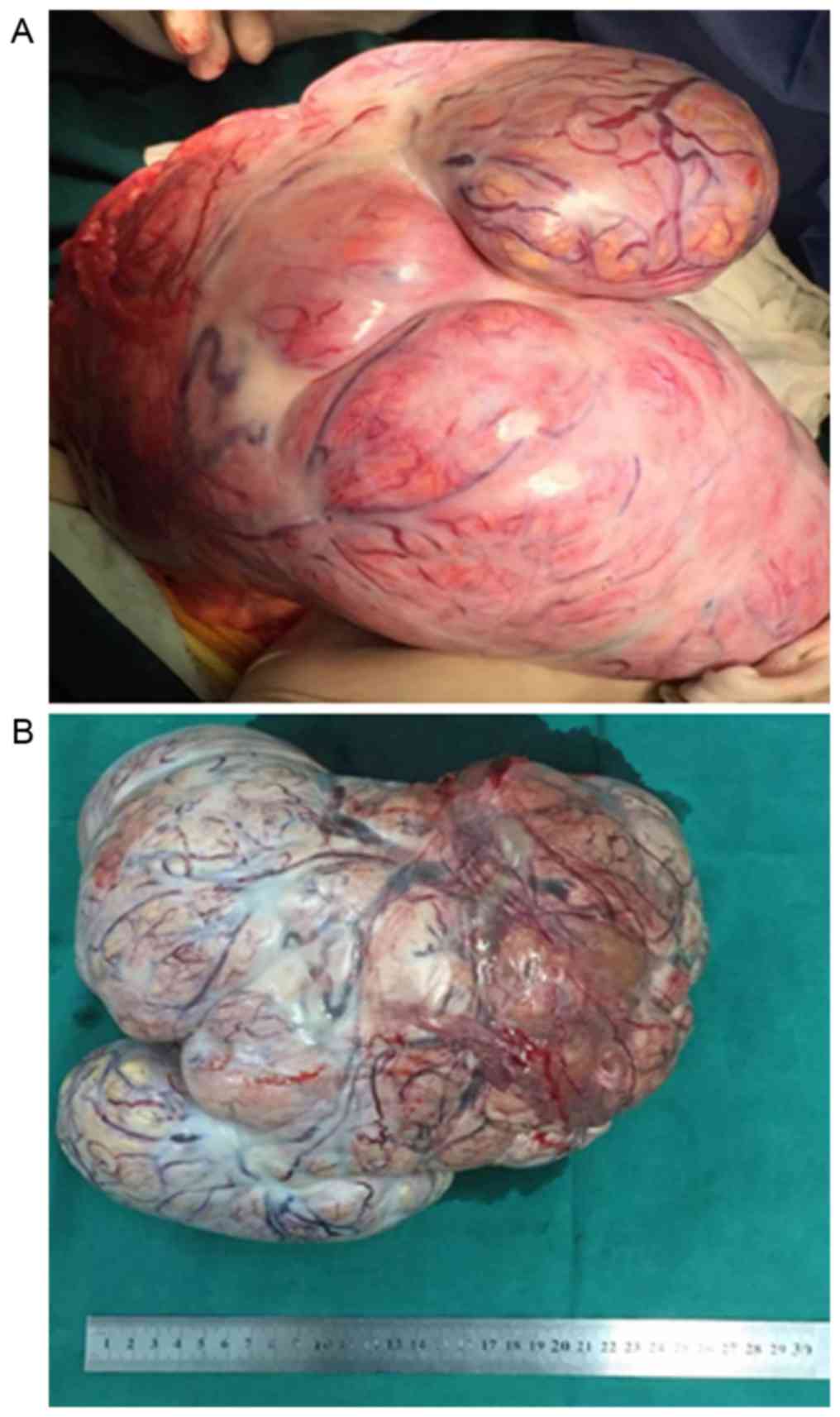
When the abdominal cavity was opened, a large tumor
occupying the patient's entire abdominopelvic cavity was observed.
The tumor was ~26×24×15 cm in size, with a well-encapsulated solid,
ovoid or lobulated appearance (Fig.
2) and exhibited partial adhesion to surrounding tissue. No
traces of ascites were identified. The tumor was gradually
separated which enabled the origin, of the left ovary, to be
identified. The ovarian tumor was removed and examined as frozen
sections (FS) to confirm its pathological features and decide
whether to enlarge the surgery. No enlarged abdominal or pelvic
lymph nodes were identified and the remaining abdomen and pelvis
were identified as normal. When the FS proved negative for
malignancy, simple tumor resection was achieved. The postoperative
period was uneventful and the patient was discharged on day 9
following surgery with no further treatment offered. At the time of
writing (~6 months following this surgery), the patient remained
alive without evidence of tumor metastasis or recurrence and
received regular follow-ups.
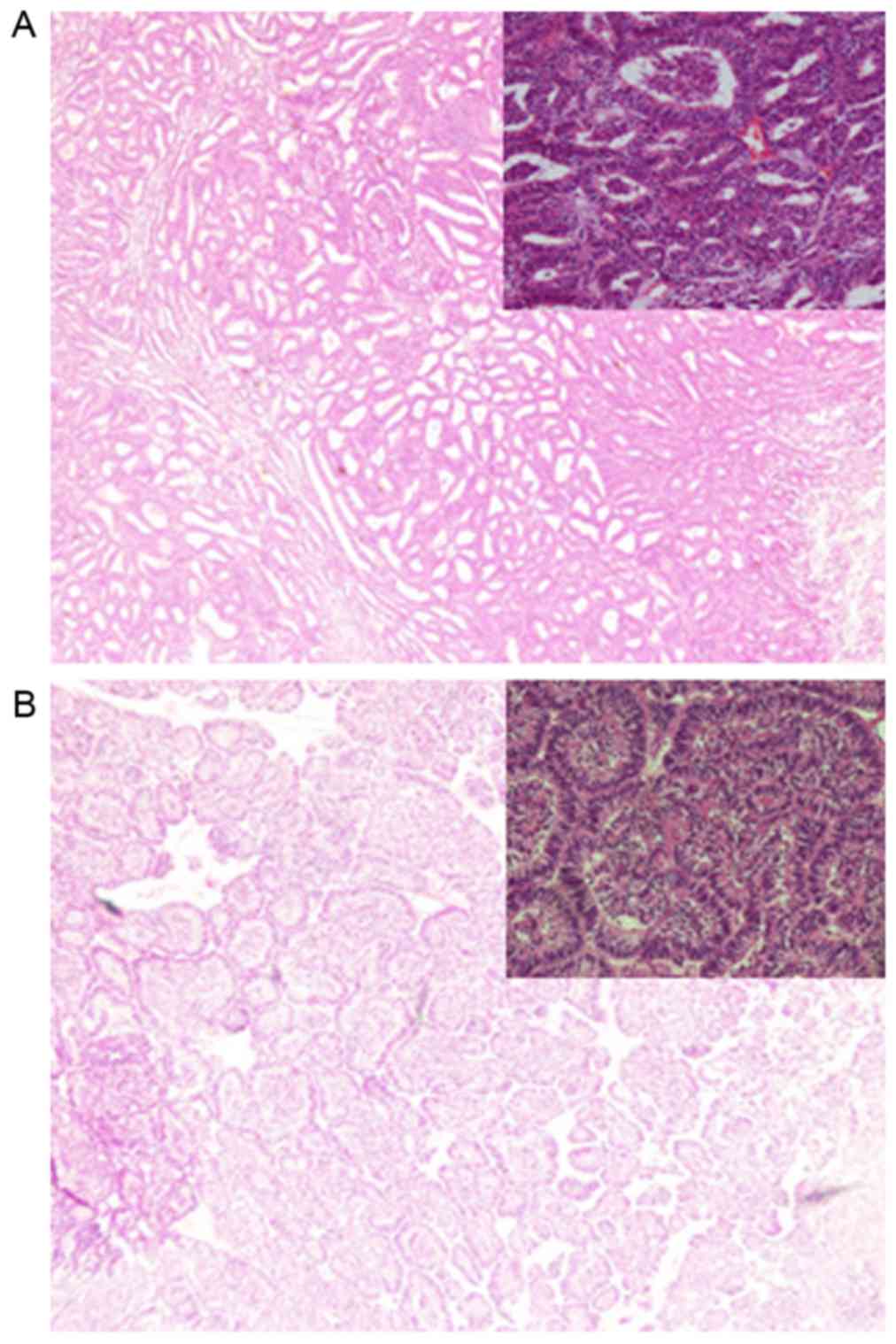
The final pathology report identified the tumor as
an ovary-derived female WAT. The cross-section of mass (4 µm thick)
contained solid and microcystic parts and exhibited a yellow-gray
appearance with focal hemorrhage and necrosis. Characteristic
histopathological patterns identified on microscopic examination
included a solid or diffuse arrangement of the neoplastic
epithelial cells, small or medium-sized cells arranged in a
microcystic, sieve-like, trabecular and closely packed pattern
(Fig. 3). Tissue sections were cut
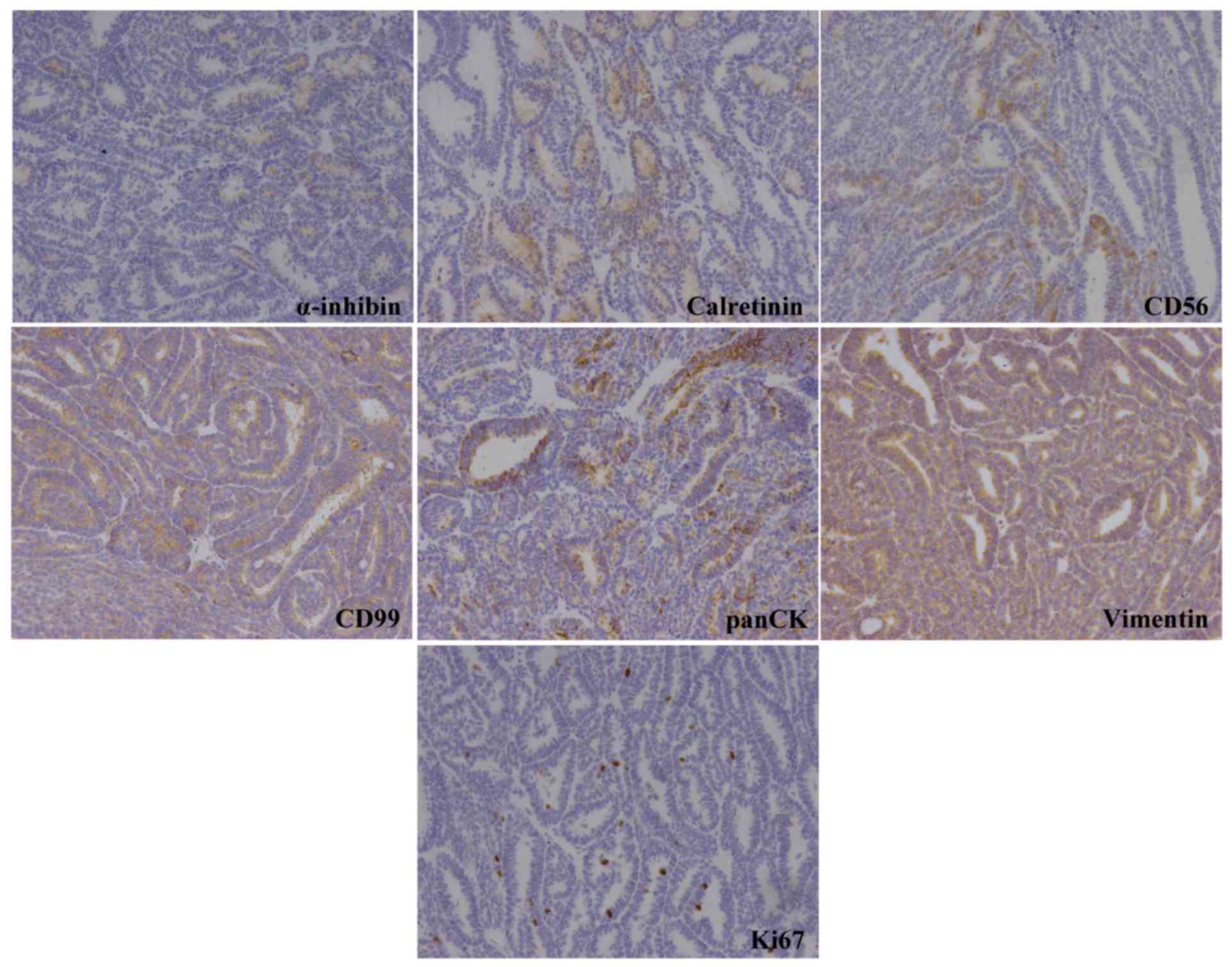
into 4 µm thick pathological section and immunohistochemical
staining was performed using strept avidin-biotin complex dyeing at
room temperature for 40 min. We found that the sections were
positive for vimentin, cluster of differentiation (CD)99 and
pan-cytokeratin (CK) and focally positive for calretinin, α-inhibin
and CD56. The positive proportion of Ki-67 was 3%; however,
staining was negative for chromogranin, epithelial membrane
antigen, CD10, CD34, synaptophysin and S-100 protein (Fig. 4).
The present case report was approved by the Ethics
Committee of the Ninth People's Hospital, School of Medicine,
Shanghai Jiao Tong University. Preoperative informed consent was
obtained from the patient in accordance with institutional
guidance. The pathological samples were obtained from the surgical
resection specimens which did not result in any disadvantages to
the health and prognosis of patient. The present case report
maintains the privacy of the patient.
Discussion
WAT is a rare neoplasm, with <100 cases
worldwide, and arises from the rare persisting remnants of the
mesonephric duct (6). The age at
diagnosis ranged between 18 and 81 years, with a mean age of 50
years (7). The prognosis of the
patient's tumor was not associated with its clinical presentation
and cytology, which made it difficult to diagnose (5). Therefore, there were no clear
recommendations regarding the patient's preoperative diagnosis. The
diagnosis of the present case relied primarily on histopathological
features, which were characterized by a tubular pattern with either
closely packed tubules or solid cords, a sieve-like growth pattern
produced by cysts of various sizes and a diffuse growth composed of
spindle or polygonal cells (8). The
primary differential diagnosis included Sertoli-Leydig cell tumors,
clear cell tumors and granulosa cell tumors since the microscopic
appearance of the aforementioned tumors exhibited similarity to
that of WAT (4–9). A previous study (10) revealed that CD56-positivity may be a
diagnostic biomarker to differentiate between malignant FATWOs and
benign lesions; however, this required further validation. Although
the patient in the present case report had been identified as
ovary-derived WAT, the tumor did not initially induce gynecological
symptoms but induce abdominal pain and bloating. In addition, to
the best of our knowledge, no previous studies had reported a WAT
as large as the tumor in the present patient. Therefore, it was
increasingly difficult to diagnose the present patient and it was
elected to only conduct an exploratory laparotomy.
WAT typically behaves as a benign lesion; however,
in a number of cases, more aggressive behavior has been encountered
(11). Previous studies identified
that ~1/5 of the cases were associated with an adverse outcome and
the principal metastatic sites were the liver and the lung
(6,9).
Owing to the rarity of this type of tumor, there is no standard
surgical therapy for WAT patients. Lesin et al (12) demonstrated that the majority cases of
relapsed WAT had occurred in patients who were initially treated
with tumor resection only, and hypothesized that the optimal
therapy for WAT was complete surgical resection with hysterectomy
and bilateral adnexectomy. In addition, adjuvant chemotherapy or
radiation therapy was controversial and typically not an effective
treatment (7).
The literature review of the present case report
identified 34 studies associated with WAT. To the best of our
knowledge, a total of 18 ovary-derived WAT cases, including the
present case, have now been reported (Table I). In Table
I, the first 11 cases had been reported before (13). It was revealed that the reported
ovary-derived WAT cases age ranged between 28 and 87 years, and 17
cases were patients who exhibited tumors on only one side of the
body. In addition, the tumors identified in the literature report
typically extended to the fallopian tubes, uterus, appendix, lung,
liver and other sites; however, the tumors rarely extended to the
contralateral ovary. Only 1 patient (case no. 12) was diagnosed
with tumors in two ovaries. A total of 16 cases (88.89%) had a
hysterectomy with bilateral salpingo-oophorectomy or bilateral
salpingo-oophorectomy alone, and only 2 cases had a simple tumor
resection. However, there was not enough information to analyze the
statistical difference of disease-free survival in these 18 cases.
Therefore, unless the patient is an unmarried female or too old to
tolerate surgery, it is suggested to select hysterectomy with
bilateral salpingo-oophorectomy. Following the initial surgical
treatment, it is recommended that patients are to be appropriately
followed up for a long-term period. Additionally, the present case
report identified that there was limited optional therapy to treat
recurrent or postoperative metastatic WAT tumors (14). A previous study (6) reported that molecular targeted therapy,
including the tyrosine kinase inhibitor Gleevac® (STI
571), may be considered. However, additional studies are required
to determine the effectiveness of this option.
 | Table I.Summarized literature review of
ovary-derived Wolffian adnexal tumor cases. |
Table I.
Summarized literature review of
ovary-derived Wolffian adnexal tumor cases.
| Case no. | Age, years | Metastasis
status | Size, cm/external
surface | Surgery method | Follow-up |
|---|
| 1 | 56 | Situ | 14, smooth | H, BSO | NED, 7 years |
| 2 | 51 | Situ | Large, smooth | H, BSO | NED, 9 years |
| 3 | 52 | Situ | 15, smooth | H, BSO | NED, 15 years |
| 4 | 28 | Situ | 2, smooth | H, BSO | NED, 2 years |
| 5 | 64 | Metastasis | 8, smooth | BSO, omentectomy | LFU |
| 6 | 51 | Situ | 11, smooth | USO | NED 4 years |
| 7 | Reproductive age | Situ | 11, smooth | USO | NED, 1 years |
| 8 | 56 | Situ | 20, smooth | H, BSO | NED, 1 years |
| 9 | 58 | Situ | 12, smooth | H, BSO | LFU |
| 10 | 41 | Situ | 10, smooth | USO | NED, 1 years |
| 11 | 52 | Situ | 8, smooth | H, BSO | Lung metastasis, 8
years later |
| 12 | 51 | Situ | 10 and 4.5,
smooth | H, BSO | NED, 37 months |
| 13 | 27 | Situ | 10, smooth | STR | NED, 3 years |
| 14 | 75 | Metastasis | 15, smooth | USO | LFU |
| 15 | 87 | Metastasis | 4.5, smooth | H, BSO | NED, 7 months |
| 16 | 62 | Metastasis | / | H, BSO | NED, 19 years |
| 17 | 51 | Situ | 2.5, smooth | H, BSO | LFU |
| 18 | 73 | Situ | 26, smooth | STR | NED, 5 months |
Acknowledgements
The authors thank Dr Hong-Xiu Han for the
pathological and immunohistochemical assistance.
References
|
1
|
Kariminejad MH and Scully RE: Female
adnexal tumor of probable Wolffian origin. A distinctive pathologic
entity. Cancer. 31:671–677. 1973. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Heatley MK: Is female adnexal tumour of
probable Wolffian origin a benign lesion? A systematic review of
the English literature. Pathology. 41:645–648. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Heller DS, Kadire B and Cracchiolo B:
Malignant female adnexal tumor of probable Wolffian origin: A case
report. J Reprod Med. 56:175–177. 2011.PubMed/NCBI
|
|
4
|
Tipps AM, Plaxe SC and Weidner N:
Endometrioid carcinoma with a low-grade spindle cell component: A
tumor resembling an adnexal tumor of probable Wolffian origin. Ann
Diagn Pathol. 15:376–381. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Turkcapar AF, Seçkin B, Güngör T, Sirvan L
and Mollamahmutoğlu L: Diagnosis and management of female adnexal
tumor of probable Wolffian origin (FATWO) arising from ovary: A
case report. J Turk Ger Gynecol Assoc. 14:56–59. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Syriac S, Durie N, Kesterson J, Lele S and
Mhawech-Fauceglia P: Female adnexal tumor of probable Wolffian
origin (FATWO) with recurrence 3 years postsurgery. Int J Gynecol
Pathol. 30:231–235. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Matsuki M, Kaji Y and Matsuo M: Female
adnexal tumour of probable Wolffian origin: MR findings. Br J
Radiol. 72:911–913. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tiltman AJ and Allard U: Female adnexal
tumours of probable Wolffian origin: An immunohistochemical study
comparing tumours, mesonephric remnants and paramesonephric
derivatives. Histopathology. 38:237–242. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ramirez PT, Wolf JK, Malpica A, Deavers
MT, Liu J and Broaddus R: Wolffian duct tumors: Case reports and
review of the literature. Gynecol Oncol. 86:225–230. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nakamura K, Nakayama K, Miura H, Fujiwaki
R, Manabe A, Teshima S, Nagai Y, Miyazaki K and Sawada K: Malignant
female adnexal tumor of Wolffian origin (FATWO) positive for CD56:
A possible diagnostic role for the biomarker. Eur J Gynaecol Oncol.
35:580–583. 2014.
|
|
11
|
Liu Y: Metastatic female adnexal tumor of
possible wolffian origin (FATWO) of the appendix demonstrated by
FDG PET/CT: The first reported case. Clin Nucl Med. 36:136–137.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lesin J, Forko-Ilić J, Plavec A and
Planinić P: Management of Wolffian duct tumor recurrence without
chemotherapy. Arch Gynecol Obstet. 280:855–857. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Young RH and Scully RE: Ovarian tumors of
probable wolffian origin. A report of 11 cases. Am J Surg Pathol.
7:125–135. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tianmin X, Weiqim C, Mianhua C, Xiaocui L,
Hongwen G and Min Y: Tumor of the mesosalpinx: Case report of a
female adnexal tumor of probable Wolffian origin. Eur J Gynaecol
Oncol. 33:233–235. 2012.PubMed/NCBI
|