Introduction
Lung cancer is a severe form malignant disease, with
~80% of patients diagnosed with non-small cell lung cancer
(1). Radio- or chemotherapy prolongs
the overall survival time of the majority of patients with advanced
or relapsed lung cancer and improves their quality of life
(2). However, several phase III
randomized clinical trials have revealed that the most effective
radio- or chemotherapy can only achieve an overall response rate of
20–40% and a 1-year overall survival rate of 35–45% (3–5),
accompanied by severe side effects and toxicity that elderly
patients are intolerant to (6). As
radiosensitization can enhance the efficiency and mitigate the side
effects of radiotherapy, it has been one of the most active fields
of cancer radiotherapy research (7).
An ideal radiosensitizer should be tumor-specific but have low or
absent toxicity to normal cells. However, the most widely used
radiosensitizers, are nitroimidazoles, fluorouracil, cisplatin and
Taxol, which exhibit a sensitizing action on radiotherapy, remain
limited in their clinical use due to high toxicity to normal
tissues (8). Molecular targeted drugs
(MTDs) are extensively studied in cancer therapy (9). By harnessing the distinctions between
cancer cells and normal cells, MTDs target tumor-specific
structures and signal transduction-associated receptors or other
enzymes, proteins and cytokines in order to kill cancer cells and
suppress tumor development (10,11).
Previous studies have suggested that the
overexpression of COX-2 is associated with oncogenesis, and that
COX-2 inhibition or prostaglandin-endoperoxide synthase-2 knockout
can reduce tumor occurrence (12,13). In
addition, there is a negative correlation between COX-2 expression
levels and prognosis (14,15). With its differing expression patterns
in tumor and normal tissues, COX-2 has become a novel target in
cancer therapy for its role in tumor occurrence and development
(12–15). Selective COX-2 inhibitors (SCIs) are
also effective in cancer prophylaxis and tumor therapy, exhibiting
a high efficiency and a good safety profile with few side effects
(16,17).
Representative SCIs, including celecoxib and NS-398,
have exerted notable anticancer effects in several prior in
vitro studies (18,19); however, the results were not as
expected in clinical trials, possibly as SCIs do not kill cancer
cells directly (20,21). Therefore, a combination of SCIs and
radiotherapy or chemotherapy may be necessary to improve the
treatment efficacy. In particular, it has been reported that
radiotherapy stimulates COX-2 expression in a dose-dependent manner
(22), which provides a rational
basis for the combined treatment of SCIs and radiotherapy.
The present study aimed to treat lung cancer A549
cells using celecoxib combined with radiotherapy. Through analysis
of cell cycle progression, cell growth, proliferation and
apoptosis, the efficacy of this combination therapy was evaluated
in cell culture.
Materials and methods
Reagents
Celecoxib was purchased from Selleck Chemicals
(Houston, TX, USA). X-ray radiation was conferred by Radsource 2000
from Radsource, LLC (Brentwood, TN, USA). TRIzol® and
primers were purchased from Invitrogen (Thermo Fisher Scientific,
Inc., Waltham, MA, USA) and the ThermoScript RT reverse
transcription-polymerase chain reaction (RT-PCR) kit was purchased
from Fermentas (Thermo Fisher Scientific, Inc.). The PCR
Amplification kit was obtained from Takara Bio, Inc., (Otsu,
Japan). The Annexin V-Fluorescein Isothiocyanate (FITC) kit (cat.
no. KFG001) was purchased from Nanjing KeyGen Biotech Co., Ltd.
(Nanjing, China). Hoechst 33258 was purchased from Beyotime
Institute of Biotechnology (Haimen, China). The laser confocal
scanning microscope, flow cytometer, PCR thermocycler, gel
electrophoresis imaging system and cell culturing equipment were
all obtained from The Second Affiliated Hospital, Suzhou University
(Suzhou, China).
Cell culture
The human A549 lung adenocarcinoma and H292 lung
mucoepidermoid carcinoma cell lines were purchased from the
Shanghai Institute of Cell Biology, Chinese Academy of Sciences
(Shanghai, China) and cultured using RPMI-1640 medium (Gibco;
Thermo Fisher Scientific, Inc.) containing 10% fetal bovine serum
(Gemini Bio-Products, West Sacramento, CA, USA). Cultures were
maintained in a 5% CO2 incubator at 37°C.
MTT assay
A549 cells were cultured on 96-well plates at 5,000
per well and allowed to grow to ~70% confluence. The medium was
discarded and replaced following cell adherence and the cells were
subjected to dimethyl sulfoxide (DMSO) or celecoxib treatment (100,
200 or 400 µM), with/without prior exposure to 6 Gy X-ray radiation
for 5 min. A total of five replicates were set for each group and
the cells were cultured for 24, 48, 72, 96 and 120 h, respectively.
The medium was renewed for each group every 24 h. MTT solution (5
g/l) was added to each well prior to the chromogenic reaction and
subsequently incubated for an additional 4 h, following which the
incubation was stopped and the medium was carefully aspirated with
a sterile pipette. DMSO (100 µl) was added to each well, followed
by oscillation with a micro-oscillator for 10 min to dissolve the
crystals completely. The optical density (OD) value of each well
was detected under a wavelength of 490 nm, and the survival ratio
was calculated according to following equation: Survival ratio =
(mean OD value of the experimental group-background)/(mean OD value
of the control group-background).
Detection of cell apoptosis by laser
confocal scanning microscopy (LSCM)
A549 cells were cultured on 6-well plates with a
coverslip in each well (50,000/well). Cells were treated with DMSO
(0.1%), Celecoxib (200 µM), X-ray irradiation (6 Gy for 5 min) or
Celecoxib (200 µM) combined with prior X-ray irradiation (6 Gy for
5 min). Serum-free medium and celecoxib-containing medium was
refreshed every 24 h, and the cells were incubated at 37°C for a
total of 48 h. Cells were fixed in 4% formaldehyde in PBS
containing 0.1% TritonX-100 for 15 min at room temperature. Hoechst
33258 staining and mounting were performed according to the
protocol provided by the Beyotime Institute of Biotechnology.
Images were visualized and captured on an Olympus FV3000 microscope
(Olympus Corporation, Tokyo, Japan) using magnification, ×400.
Detection of cell cycle and apoptosis
by flow cytometry
A549 or H292 cells were seeded onto a 6-well plate
(50,000/well) and allowed to grow to ~70% confluence. Cells were
treated as aforementioned for 48 h. Prior to harvesting, cells were
washed twice with PBS. In total, ~1×105 cells were
collected for each group and centrifuged at 500 × g for 5 min at
4°C. For cell cycle analysis, cells were fixed in 70% ethanol at
4°C for 3 h. 100 µl Ribonuclease A (Sigma-Aldrich; Merck KGaA,
Darmstadt, Germany) was added and the system was incubated in a
water bath at 37°C for 15 min. Subsequently, 400 µl propidium
iodide (PI) was added, mixed well and incubate in a dark chamber at
room temperature for 30 min. Samples were detected at an excitation
wavelength of 488 nm (Cytomics FC 500 MCL; Beckman Coulter, Inc.,
Brea, CA, USA). Results were from three replicate experiments. The
percentages of cells in the G0/G1 phase, S
phase and G2/M phase were statistically analyzed using
CXP software (Beckman Coulter, Inc.). The detection of apoptosis
was performed using the Annexin V-FITC kit, according to its
recommended protocol. Early phase apoptosis, which is characterized
by Annexin V-positive staining, was recorded to assess the
pro-apoptotic effect of indicated treatment.
COX-2 expression levesl measured by
RT-PCR
A549 cells (50,000/well) were cultured on a 6-well
plate with 3 technical repeats and grown to ~70% confluence. Cells
were then irradiated with 6 Gy X-ray for 5 min, and subsequently
treated with 100, 200 or 400 µM celecoxib. Total RNA extraction and
target RNA amplification by RT-PCR was performed according to the
protocol provided with the kit under the following conditions: 37°C
for 15 min; 85°C for 5 sec and 4°C for 5 min. cDNA products were
subjected to PCR amplification as follows: 94°C for 5 min followed
by 30 cycles of 94°C for 30 sec, 60°C for 30 sec and 72°C for 30
min followed by a final extension step of 72°C for 5 min. The
following primers were used: COX-2, forward,
5′-CTGGCGCTCAGCCATACAG-3′ and reverse,
5′-CGCACTTATACTGGTCAAAT-CCC-3′; β-actin forward,
5′-GGGACCTGACTGACTACCTC-3′ and reverse, 5′-TCATACTCCTGCTTGCTGAT-3′.
PCR products were separated on a 1% agarose gel at 160 V for 20
min.
Statistical analysis
All data are presented as the mean ± standard
deviation from three independent experiments. Drug doses and
inhibitory rates were subjected to normality tests and accorded
with a normal distribution. Single factor analysis of variance
(ANOVA) was used. A two-way ANOVA test was adopted for analysis of
the cell cycle and apoptosis. P<0.05 was considered to indicate
a statistically significant difference. Statistical analysis was
performed with SPSS v.13.0 (SPSS, Inc., Chicago, IL, USA) and
GraphPad Prism 6.0 (GraphPad Software, Inc., La Jolla, CA,
USA).
Results
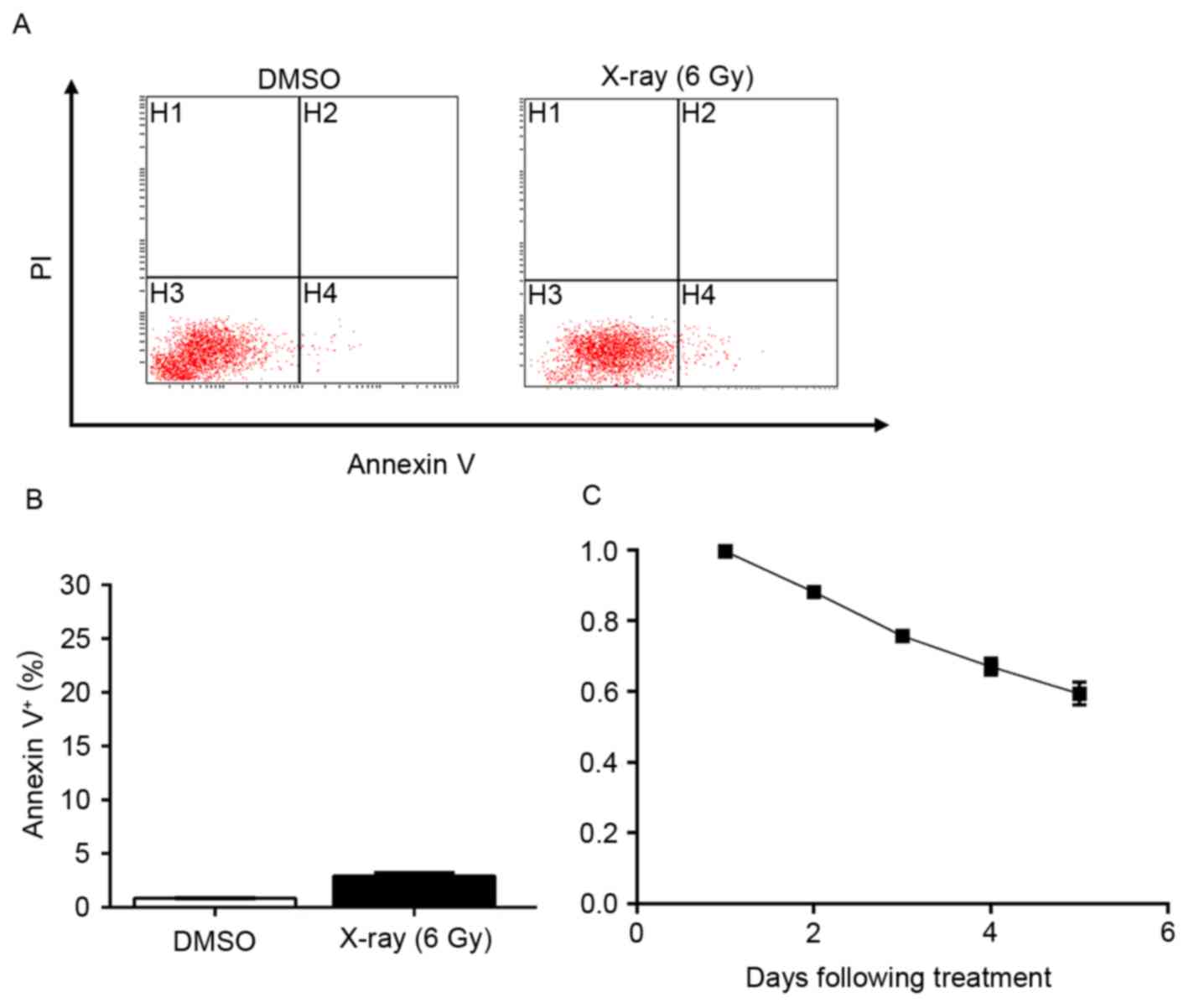
Untreated A549 cells are partially
resistant to X-ray radiation
To evaluate the inhibitory effects of radiation on
lung cancer A549 cells, assessment of apoptosis was performed
subsequent to exposing A549 cells to X-ray radiation (6 Gy). The
results demonstrated that radiation alone mildly induced apoptosis
(Fig. 1A and B). As demonstrated by
an MTT assay, ~50% of A549 cells remained proliferative five days
following exposure (Fig. 1C). These
results indicated that a large portion of A549 cells harbored
resistance to radiation treatment, which necessitates a synergist
to provide improved efficiency.
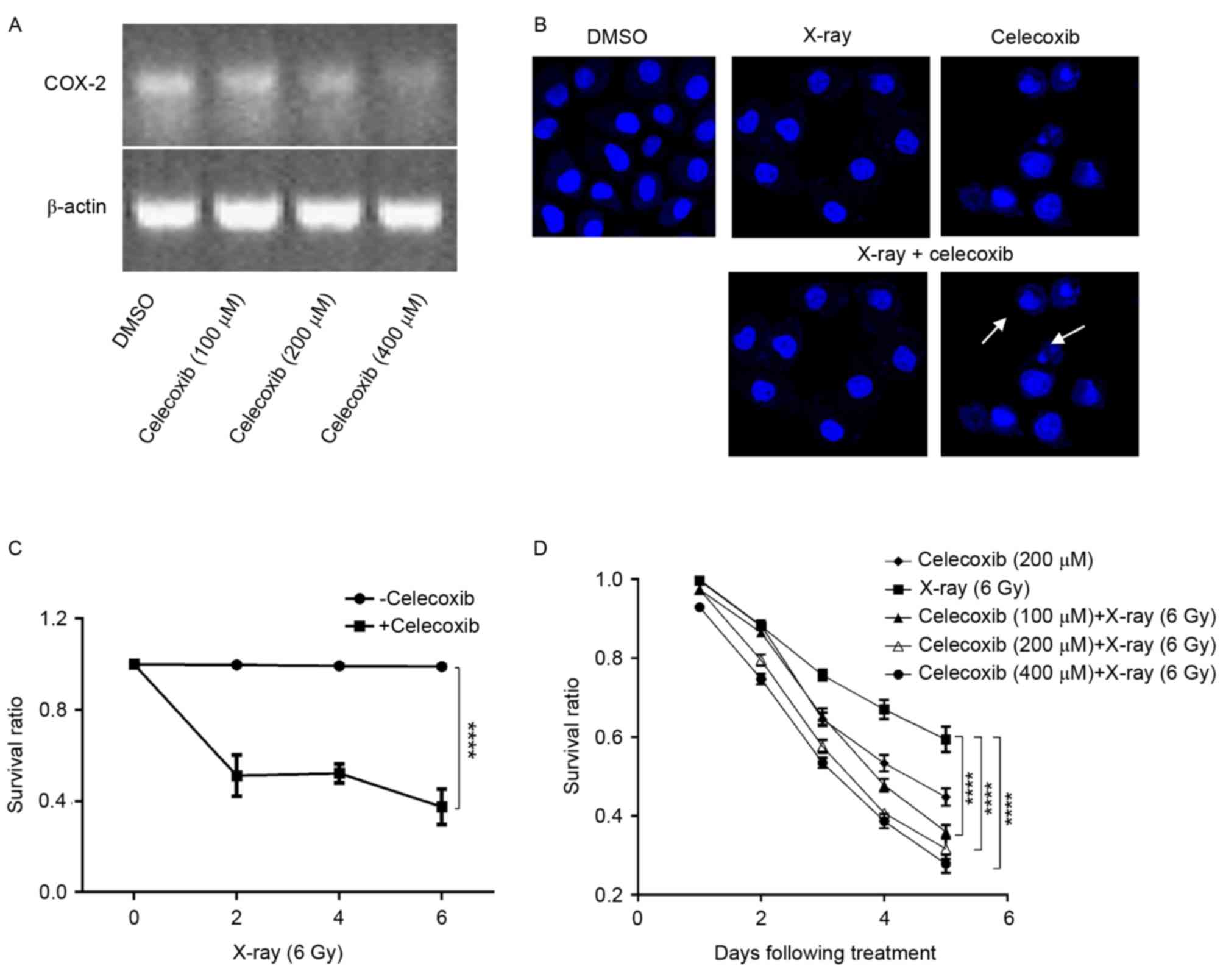
COX-2 inhibitors enhance
radiation-induced growth inhibition
Studies have demonstrated that COX-2 is associated
with tumorigenesis (12,13), and that the expression of COX-2 is
elevated in lung cancer (23).
Furthermore, radiotherapy is a stimulus of COX-2 expression
(22,24), which indicates that COX-2 may be
involved in the resistance of A549 cells to X-ray radiation.
Therefore, COX-2 inhibitors might be able to potentiate the
efficacy of radiotherapy. Based on this radiosensitizing potential,
a cell counting assay was performed using A549 cells treated with
celecoxib, X-ray radiation or celecoxib combined with irradiation.
First, it was revealed that COX-2 expression was sufficiently
inhibited when COX-2 inhibitors were added (Fig. 2A). Nuclear staining was then performed
using Hoechst 33528. Using LSCM, clear apoptosis-associated
morphological changes were observed, including anachromasis,
pyknosis and karyorrhexis, as well as apoptotic bodies,
particularly when celecoxib and X-ray radiation were combined
(Fig. 2B). Furthermore, an MTT assay
was conducted to confirm whether the killing effect of X-rays was
enhanced by COX-2 inhibitors. The results demonstrated that
celecoxib combined with X-ray irradiation had an improved efficacy
compared with X-rays or celecoxib alone, in a time and
dose-dependent manner (Fig. 2C and
D).
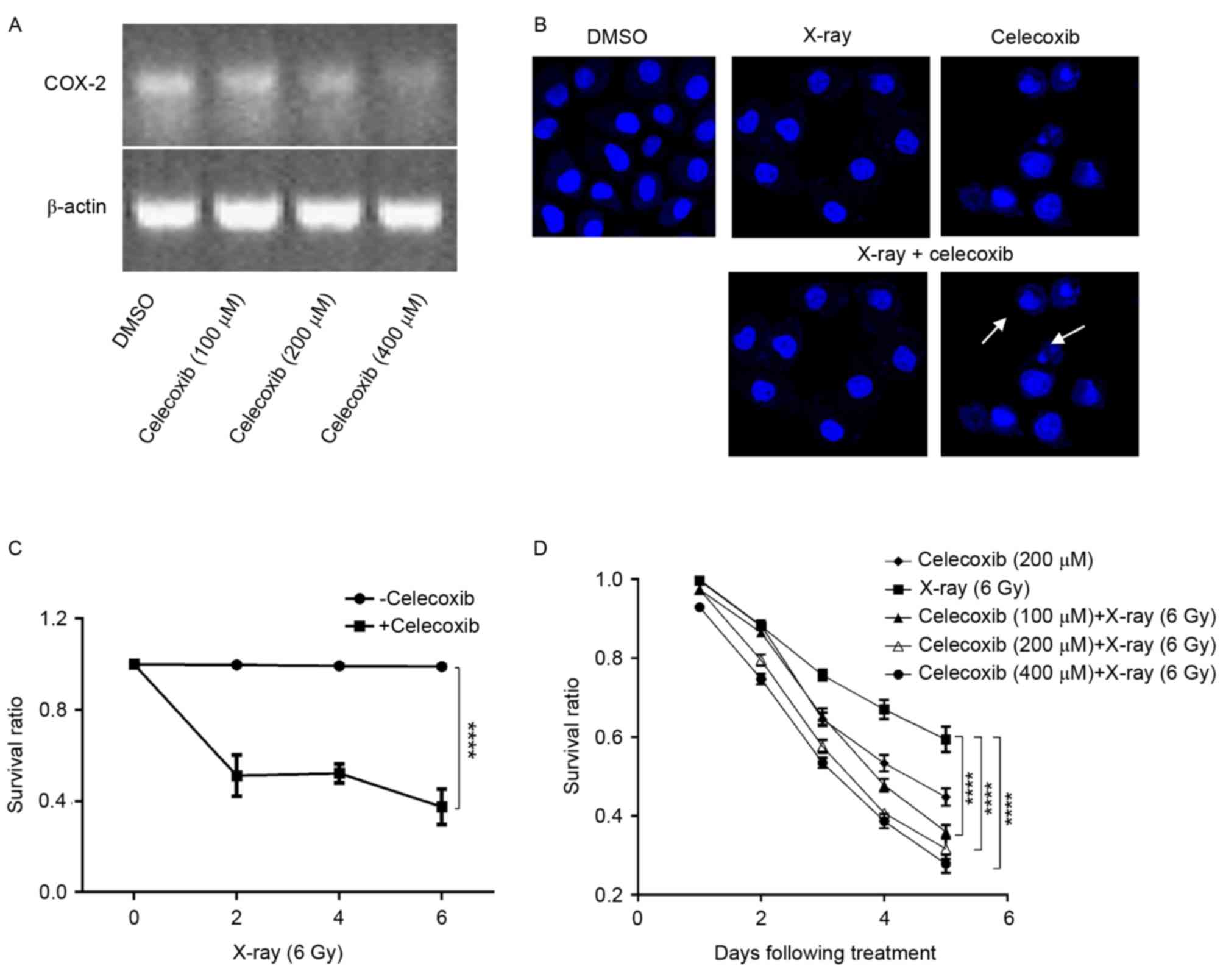 | Figure 2.COX-2 inhibition increases the
sensitivity of lung cancer cells to X-ray radiation. (A) Total RNA
extract was amplified by reverse transcription-polymerase chain
reaction and separated by agarose gel electrophoresis. Upper and
lower lanes are COX-2 and β-actin, respectively. (B) Nuclear
morphology of A549 cells treated with DMSO, X-rays, celecoxib or
celecoxib plus X-ray. Nucleic changes, including anachromasis,
pyknosis and karyorrhexis are indicated by the white arrows. Nuclei
were stained with Hoechst 33258; image magnification, ×400. (C)
A549 cells were irradiated with various doses of X-ray radiation,
then treated with/without 200 µM celecoxib for three days. The
growth inhibition curve is presented. Data are presented as the
mean and standard error of five replicates. ****P<0.0001,
two-way ANOVA. (D) Growth inhibition of A549 cells under indicated
treatment. Data were pooled from three parallels and are presented
as the mean ± standard deviation. Survival ratio at day 5 was
subjected to statistical analysis. ****P<0.0001, two-way ANOVA.
COX-2, cyclooxygenase-2; DMSO, dimethyl sulfoxide; ANOVA, analysis
of variance. |
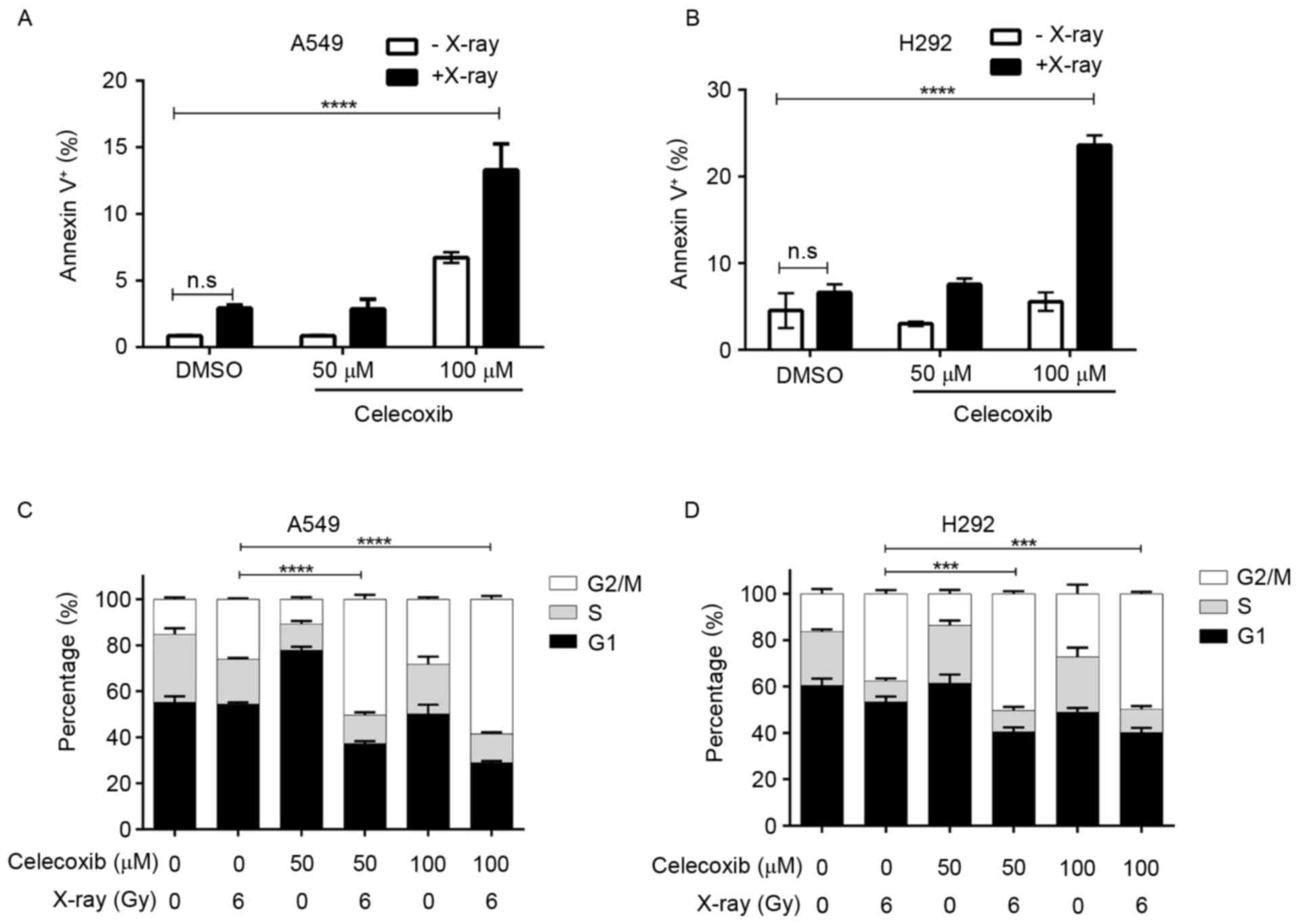
COX-2 inhibitors promote
radiation-induced apoptosis and cell cycle arrest
To quantify the pro-apoptotic function of the
combination treatment, an Annexin-V and PI dual labeling kit was
used to detect cell apoptosis, from which the apoptotic rate was
calculated. The results demonstrated that 100 µM celecoxib or 6 Gy
radiation induced apoptosis in lung cancer A549 cells, but a
combination of the two had an improved pro-apoptotic effect
(Fig. 3A). Comparable results were
also obtained using the H292 lung cancer cell line (Fig. 3B). The number of normally cycling
cells substantially determines the viability of a cell population,
and COX-2 inhibitors have been reported to hamper cell cycle
progression, causing a G0/G1 or
G2/M stage arrest depending on the type of cells
(25). Therefore, it was investigated
whether cell cycle alterations caused by celecoxib contributed to
the improved efficiency of X-ray irradiation. Cell cycle analysis
was conducted under designated conditions. As shown in Fig. 3C, in A549 cells, X-ray treatment
induced G2/M arrest, and this cell cycle blockage was
enhanced significantly by the addition of celecoxib (Fig. 3C, Table
I). The same effect was also observed in H292 cells (Fig. 3D). It was concluded that COX-2
inhibitors sensitize lung cancer cells to X-rays, not only via
suppressing the tumor-promoting effects of COX-2 that are
stimulated by radiotherapy, but also due to enhanced rates of cell
cycle arrest and apoptosis.
 | Table I.Cell cycle analysis for each
experimental group. |
Table I.
Cell cycle analysis for each
experimental group.
| Group | Celexcoxib, µM | X-ray, Gy |
G0/G1,
%a | S, %a | G2/M,
%a |
|---|
| Control |
0 | 0 | 50.01±1.86 | 34.33±1.30 | 15.88±2.05 |
| Celecoxib | 200 | 0 | 56.24±1.53 | 29.17±1.27 | 14.52±1.83 |
| Radiation |
0 | 6 | 63.19±1.87 | 24.17±1.23 | 12.82±1.57 |
| Combination
treatment | 100 | 6 | 67.21±1.93 | 23.27±1.34 | 9.65±1.67 |
|
| 200 | 6 | 73.18±1.89 | 18.36±1.87 | 8.53±1.42 |
|
| 400 | 6 | 78.24±2.05 | 14.25±1.47 | 7.62±1.72 |
Discussion
Surgery, radiotherapy and chemotherapy are the three
main treatments for malignant tumors. Although the response rate of
these therapies has improved over previous years, even higher
efficacy is challenging to achieve due to their concomitant
disadvantages. Radiotherapy is widely adopted for malignant tumors
as a local treatment. However, unfavorable responses are frequently
observed due to tumor resistance to radiation and the intolerance
of patients to severe toxicity and side effects (26–28).
Furthermore, uncontrolled distant metastasis also contributes to
treatment failures. Contemporarily, a combination of radiotherapy
with chemotherapy is the predominant approach of cancer therapy,
but due to toxicity and adverse reactions the effects are
frequently unsatisfactory (26,29).
Therefore, it is essential for oncologists to identify methods of
improving the therapeutic efficacy and local control rate, and to
control the rate of distant metastasis and reduce the impairment of
healthy tissues.
COX is a key enzyme catalyzing the synthesis of
prostaglandins (PG) and thromboxane A2 from arachidonic acid
(30–32). Several types of PG have comprehensive
functions in body, and are involved in a number of physiological
reactions, including cruor, ovulation, parturition, renal function
maintenance and immune response (32,33).
Furthermore, PG performs a pivotal role in inflammation (31). COX includes two subtypes, COX-1 and
COX-2, which are distinct in their biological characteristics.
COX-1 maintains normal physiological functions of the human body,
while COX-2 is associated with inflammation, pain and tumorigenesis
(34,35). Expression of COX-2 is elevated in
numerous tumor tissues, including colon and lung cancer (23,36). A
number of studies have confirmed that COX inhibitors can suppress
tumor occurrence and development (37–40);
however, previous non-specific COX inhibitors have been gradually
aborted due to their gastrointestinal toxicity (41). Thus, selective COX-2 inhibitors have
become an alternative that is being intensively studied. The
antitumor activity of COX-2 inhibitors may contribute to their
functions to promote apoptosis, to suppress angiogenesis, to
inhibit synthesis of PG, to enhance immunity and to prevent tumor
invasion and metastasis (42,43). Radiotherapy is a stimulus of COX-2
overexpression, which functions in a dose-dependent manner
(22,24), indicating a potential mechanism of
tumor reoccurrence and metastasis. This provides a theory basis for
the combination treatment of radiotherapy and COX-2 inhibitors.
To investigate whether COX-2 inhibitors combined
with radiotherapy yield enhanced antitumor effects, lung cancer
A549 cells overexpressing COX-2 were treated with celecoxib,
radiation or a combination of celecoxib and radiation. Through
different methods it was concluded that, under the same conditions,
proliferation of A549 cells is inhibited more evidently by
celecoxib combined with radiotherapy than by the drug or
irradiation alone. Within the combination groups, growth inhibition
became more potent when the concentration of celecoxib was
increased or the exposure time was longer, indicating that this
combination treatment works in a dose- and time-dependent manner.
The results also demonstrated that treatment with 100 µM celecoxib
enhanced the cell cycle arrest and apoptosis caused by radiation.
Consistent outcomes have been reported using other types of cancer
cells. Using mouse fibrosarcoma cells, Raju et al (25) identified that COX-2 inhibitors
triggered an accumulation of cells in the G2/M phase,
and the expression of cyclin A, cyclin B and cyclin dependent
kinase 1/2 (CDK1/2) was also decreased. However, a study by Grösch
et al (44) on colon cancer
cells revealed a G0/G1 arrest caused by COX-2
inhibitors, which lowered the expression levels of cyclin A, cyclin
B and and CDK1/2, and the expression of cell cycle inhibitory
proteins, including p21/waf1 and p27/Kip1, was upregulated.
Therefore, the cell cycle arrest caused by celecoxib may depend on
the type of cancer cells or other unknown factors.
Numerous studies have demonstrated that COX-2
inhibitors induce apoptosis in tumor cells (45–47). A
previous study by Kern et al (45) involving four hepatoma cell lines
expressing COX-2 determined that COX-2 inhibitors induced apoptosis
independent of the phosphorylation state of B-cell lymphoma-2
(Bcl-2), Bcl-2-associated X protein, protein kinase B and
Bcl-2-associated death promoter, but associated with the activation
of caspase-9, caspase-3 and caspase-6. Li et al (46) revealed that, in esophageal carcinoma
cells, COX-2 inhibitors induced the apoptosis of those expressing
COX-2 through a cytochrome c-dependent pathway. It was also
reported that the apoptosis induced by COX-2 inhibitors is not
evident in human hepatoma cells, and COX-2 inhibitor induces
apoptosis in tumor cells is independent of COX-2 expression
(47). In the present study, cell
apoptosis induced by a combination therapy of X-ray irradiation and
COX-2 inhibitors was significantly increased.
The present study corroborates that COX-2 inhibitors
can enhance the killing effect of radiation on lung cancer cells,
which is consistent with the results of prior studies (25,48).
However, the mechanisms underlying the radiosensitizing effect of
COX-2 inhibitors require further investigation. Raju et al
(25) reported that
radiosensitization may be attributed to inhibited sub-lethal DNA
damage repair or an increased percentage of cells in the
radiosensitive G2/M phase. Contradictory results were
recorded in U2251 brain glioma cells, in which COX-2 inhibitors
boosted radiosensitivity without expanding the cell number of the
G2/M phase (49). In the
present study, evident apoptosis was observed in the combination
therapy group, supported by the formation of apoptotic bodies,
which was observed using LSCM, thereby confirming the pro-apoptotic
effects of COX-2 inhibitors combined with radiotherapy on lung
cancer A549 cells. Studies have demonstrated that radiation is
responsible for elevated COX-2 expression (22,24), and
this can be reversed by the addition of a COX-2 inhibitor such as
NS398 (48), which also acts as a
radiosensitizer. Therefore, it was speculated that NS398 may act
upstream COX-2 to exert a radiosensitizing effect and inhibit the
radiation-induced upregulation of COX-2 expression. In the present
study, COX-2 inhibitors were also identified to be a synergist to
radiotherapy, of which the mechanism may be associated with
decreased intracellular expression of COX-2, accompanied by their
effects on improving immunity and inhibiting angiogenesis (50).
To conclude, compared with other intervention groups
and the control, COX-2 inhibitors combined with radiotherapy
exhibit a synergistic effect. This combination significantly
suppressed the growth and proliferation of lung cancer cells and
promoted apoptosis. The present in vitro study provides a
novel insight into the treatment of advanced lung cancer. However,
whether COX-2 inhibitors combined with X-rays are effective in
vivo or in clinical use remains unknown. Therefore, the optimal
dose and toxicity of celecoxib requires further study.
References
|
1
|
Gottfried M, Keizman D, Mishaeli M and
Rabinovich Maimon N: The Current Approach To Advanced Lung Cancer.
Harefuah. 154(521–524): 539–540. 2015.(In Hebrew).
|
|
2
|
Xu P and Le Pechoux C: Chemoradiotherapy
for stage III non-small cell lung cancer: Have we reached the
limit? Chin Clin Oncol. 4:452015.PubMed/NCBI
|
|
3
|
Ahn JS, Ahn YC, Kim JH, Lee CG, Cho EK,
Lee KC, Chen M, Kim DW, Kim HK, Min YJ, et al: Multinational
randomized phase III trial with or without consolidation
chemotherapy using docetaxel and cisplatin after concurrent
chemoradiation in inoperable stage III non-small-cell lung cancer:
KCSG-LU05-04. J Clin Oncol. 33:2660–2666. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Shen WY, Ji J, Zuo YS, Pu J, Xu YM, Zong
CD, Tao GZ, Chen XF, Ji FZ, Zhou XL, et al: Comparison of efficacy
for postoperative chemotherapy and concurrent radiochemotherapy in
patients with IIIA-pN2 non-small cell lung cancer: An early closed
randomized controlled trial. Radiother Oncol. 110:120–125. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sun JM, Ahn YC, Choi EK, Ahn MJ, Ahn JS,
Lee SH, Lee DH, Pyo H, Song SY, Jung SH, et al: Phase III trial of
concurrent thoracic radiotherapy with either first-or third-cycle
chemotherapy for limited-disease small-cell lung cancer. Ann Oncol.
24:2088–2092. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bourgier C, Lacombe J, Solassol J, Mange
A, Pèlegrin A, Ozsahin M and Azria D: Late side-effects after
curative intent radiotherapy: Identification of hypersensitive
patients for personalized strategy. Crit Rev Oncol Hematol.
93:312–319. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Noguchi Y, Nishimura R, Kawara H, Omori K,
Matsumoto K, Tokuyama Y, Uchiyama K and Shimizu Y: Survey of
current status of adverse ocular reactions to paclitaxel and a
retrospective analysis for aiding in early detection of adverse
reactions. Gan To Kagaku Ryoho. 40:819–822. 2013.PubMed/NCBI
|
|
8
|
Linam J and Yang LX: Recent developments
in radiosensitization. Anticancer Res. 35:2479–2485.
2015.PubMed/NCBI
|
|
9
|
Sheppard DW and MacRitchie JA: Building in
molecular diversity for targeted libraries. Drug Discov Today
Technol. 10:e461–e466. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Milano GA: Targeted therapy in non-small
cell lung cancer: A focus on epidermal growth factor receptor
mutations. Chin Clin Oncol. 4:472015.PubMed/NCBI
|
|
11
|
Ricciuti B, Leonardi GC, Metro G, Grignani
F, Paglialunga L, Bellezza G, Baglivo S, Mencaroni C, Baldi A,
Zicari D and Crinò L: Targeting the KRAS variant for treatment of
non-small cell lung cancer: Potential therapeutic applications.
Expert Rev Respir Med. 10:53–68. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Müller-Decker K: Cyclooxygenase-dependent
signaling is causally linked to non-melanoma skin carcinogenesis:
Pharmacological, genetic, and clinical evidence. Cancer Metastasis
Rev. 30:343–361. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Tsujii M: Cyclooxygenase, cancer stem
cells and DNA methylation play important roles in colorectal
carcinogenesis. Digestion. 87:12–16. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lee JY, Myung SK and Song YS: Prognostic
role of cyclooxygenase-2 in epithelial ovarian cancer: A
meta-analysis of observational studies. Gynecol Oncol. 129:613–619.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Magnowska M, Zaborowski M, Surowiak P,
Nowak-Markwitz E, Zabel M and Spaczyński M: COX-2 expression
pattern is related to ovarian cancer differentiation and prognosis,
but is not consistent with new model of pathogenesis. Ginekol
Polska. 85:335–341. 2014. View
Article : Google Scholar
|
|
16
|
Liu R, Xu KP and Tan GS: Cyclooxygenase-2
inhibitors in lung cancer treatment: Bench to bed. Eur J Pharmacol.
769:127–133. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Regulski M, Regulska K, Prukala W,
Piotrowska H, Stanisz B and Murias M: COX-2 inhibitors: A novel
strategy in the management of breast cancer. Drug Discov Today.
21:598–615. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Amir M and Agarwal H: Role of COX-2
selective inhibitors for prevention and treatment of cancer.
Pharmazie. 60:563–570. 2005.PubMed/NCBI
|
|
19
|
Kalgutkar AS and Zhao Z: Discovery and
design of selective cyclooxygenase-2 inhibitors as non-ulcerogenic,
anti-inflammatory drugs with potential utility as anti-cancer
agents. Curr Drug Targets. 2:79–106. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Liu R, Xu KP and Tan GS: Cyclooxygenase-2
inhibitors in lung cancer treatment: Bench to bed. Eur J Pharmacol.
769:127–133. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Mohammadinejad P, Arya P, Esfandbod M,
Kaviani A, Najafi M, Kashani L, Zeinoddini A, Emami SA and
Akhondzadeh S: Celecoxib versus diclofenac in mild to moderate
depression management among breast cancer patients: A double-blind,
placebo-controlled, randomized trial. Ann Pharmacother. 49:953–961.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Steinauer KK, Gibbs I, Ning S, French JN,
Armstrong J and Knox SJ: Radiation induces upregulation of
cyclooxygenase-2 (COX-2) protein in PC-3 cells. Int J Radiat Oncol
Biol Phys. 48:325–328. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Hida T, Yatabe Y, Achiwa H, Muramatsu H,
Kozaki K, Nakamura S, Ogawa M, Mitsudomi T, Sugiura T and Takahashi
T: Increased expression of cyclooxygenase 2 occurs frequently in
human lung cancers, specifically in adenocarcinomas. Cancer Res.
58:3761–3764. 1998.PubMed/NCBI
|
|
24
|
Isoherranen K, Punnonen K, Jansen C and
Uotila P: Ultraviolet irradiation induces cyclooxygenase-2
expression in keratinocytes. Br J Dermatol. 140:1017–1022. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Raju U, Nakata E, Yang P, Newman RA, Ang
KK and Milas L: In vitro enhancement of tumor cell radiosensitivity
by a selective inhibitor of cyclooxygenase-2 enzyme: Mechanistic
considerations. Int J Radiat Oncol Biol Phys. 54:886–894. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Blanco R, Maestu I, de la Torre MG,
Cassinello A and Nuñez I: A review of the management of elderly
patients with non-small-cell lung cancer. Ann Oncol. 26:451–463.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Guy JB, Rancoule C, Méry B, Espenel S,
Wozny AS, Simonet S, Vallard A, Alphonse G, Ardail D,
Rodriguez-Lafrasse C and Magné N: Radiosensitivity and/or
radioresistance of head and neck cancers: Biological angle. Bull
Cancer. 103:41–47. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Chang L, Graham PH, Ni J, Hao J, Bucci J,
Cozzi PJ and Li Y: Targeting PI3K/Akt/mTOR signaling pathway in the
treatment of prostate cancer radioresistance. Crit Rev Oncol
Hematol. 96:507–517. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Chang L, Graham P, Hao J, Bucci J, Malouf
D, Gillatt D and Li Y: Proteomics discovery of radioresistant
cancer biomarkers for radiotherapy. Cancer Lett. 369:289–297. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Spector AA and Kim HY: Discovery of
essential fatty acids. J Lipid Res. 56:11–21. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Frungieri MB, Calandra RS, Mayerhofer A
and Matzkin ME: Cyclooxygenase and prostaglandins in somatic cell
populations of the testis. Reproduction. 149:R169–R180. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Claar D, Hartert TV and Peebles RS Jr: The
role of prostaglandins in allergic lung inflammation and asthma.
Expert Rev Respir Med. 9:55–72. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Sugimoto Y, Inazumi T and Tsuchiya S:
Roles of prostaglandin receptors in female reproduction. J Biochem.
157:73–80. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Tjandrawinata RR, Dahiya R and
Hughes-Fulford M: Induction of cyclo-oxygenase-2 mRNA by
prostaglandin E2 in human prostatic carcinoma cells. Br J Cancer.
75:1111–1118. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Williams CS, Mann M and DuBois RN: The
role of cyclooxygenases in inflammation, cancer, and development.
Oncogene. 18:7908–7916. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Sano H, Kawahito Y, Wilder RL, Hashiramoto
A, Mukai S, Asai K, Kimura S, Kato H, Kondo M and Hla T: Expression
of cyclooxygenase-1 and-2 in human colorectal cancer. Cancer Res.
55:3785–3789. 1995.PubMed/NCBI
|
|
37
|
Azer SA: Overview of molecular pathways in
inflammatory bowel disease associated with colorectal cancer
development. Eur J Gastroenterol Hepatol. 25:271–281. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Harris RE, Beebe J and Alshafie GA:
Reduction in cancer risk by selective and nonselective
cyclooxygenase-2 (COX-2) inhibitors. J Exp Pharmacol. 4:91–96.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Cathcart MC, O'Byrne KJ, Reynolds JV,
O'Sullivan J and Pidgeon GP: COX-derived prostanoid pathways in
gastrointestinal cancer development and progression: Novel targets
for prevention and intervention. Biochim Biophys Acta. 1825:49–63.
2012.PubMed/NCBI
|
|
40
|
Wang X, Baek SJ and Eling T: COX
inhibitors directly alter gene expression: Role in cancer
prevention? Cancer Metastasis Rev. 30:641–657. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Nalamachu S, Pergolizzi JV, Raffa RB,
Lakkireddy DR and Taylor R Jr: Drug-drug interaction between NSAIDS
and low-dose aspirin: A focus on cardiovascular and GI toxicity.
Expert Opin Drug Saf. 13:903–917. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Masferrer JL, Isakson PC and Seibert K:
Cyclooxygenase-2 inhibitors: A new class of anti-inflammatory
agents that spare the gastrointestinal tract. Gastroenterol Clin
North Am. 25:363–372. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Pairet M and Engelhardt G: Distinct
isoforms (COX-1 and COX-2) of cyclooxygenase: Possible
physiological and therapeutic implications. Fundam Clin Pharmacol.
10:1–17. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Grösch S, Tegeder I, Niederberger E,
Bräutigam L and Geisslinger G: COX-2 independent induction of cell
cycle arrest and apoptosis in colon cancer cells by the selective
COX-2 inhibitor celecoxib. FASEB J. 15:2742–2744. 2001.PubMed/NCBI
|
|
45
|
Kern MA, Schubert D, Sahi D, Schöneweiss
MM, Moll I, Haugg AM, Dienes HP, Breuhahn K and Schirmacher P:
Proapoptotic and antiproliferative potential of selective
cyclooxygenase-2 inhibitors in human liver tumor cells. Hepatology.
36:885–894. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Li M, Wu X and Xu XC: Induction of
apoptosis by cyclo-oxygenase-2 inhibitor NS398 through a cytochrome
C-dependent pathway in esophageal cancer cells. Int J Cancer.
93:218–223. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Elder D, Halton DE, Hague A and Paraskeva
C: Induction of apoptotic cell death in human colorectal carcinoma
cell lines by a cyclooxygenase-2 (COX-2)-selective nonsteroidal
anti-inflammatory drug: Independence from COX-2 protein expression.
Clin Cancer Res. 3:1679–1683. 1997.PubMed/NCBI
|
|
48
|
Amirghahari N, Harrison L, Smith M, Rong
X, Naumann I, Ampil F, Shi R, Glass J and Nathan CO: NS 398
radiosensitizes an HNSCC cell line by possibly inhibiting
radiation-induced expression of COX-2. Int J Radiat Oncol Biol
Phys. 57:1405–1412. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Kang KB, Wang TT, Woon CT, Cheah ES, Moore
XL, Zhu C and Wong MC: Enhancement of glioblastoma radioresponse by
a selective COX-2 inhibitor celecoxib: Inhibition of tumor
angiogenesis with extensive tumor necrosis. Int J Radiat Oncol Biol
Phys. 67:888–896. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Lang S, Lauffer L, Clausen C, Löhr I,
Schmitt B, Hölzel D, Wollenberg B, Gires O, Kastenbauer E and
Zeidler R: Impaired monocyte function in cancer patients:
Restoration with a cyclooxygenase-2 inhibitor. FASEB J. 17:286–288.
2003.PubMed/NCBI
|