Introduction
Small cell carcinoma (SCC) usually originates from
the lungs and accounts for ~12.95% of all lung cancer cases in the
USA in 2002 (1). Extra-pulmonary SCC
is commonly identified in the gastrointestinal tract, genitourinary
organs, head or neck (2). While the
prostate and bladder are the most common sites for SCC in the
genitourinary tract, SCC of the kidneys is rare (3). For localized SCC, surgical treatment
with adjuvant chemotherapy is the suggested option (2). Renal cell carcinoma is the most common
type of genitourinary cancer associated with paraneoplastic
syndrome (PNS), but the majority of PNS disappears following
nephrectomy (4). The current case
involved the assessment of a patient who underwent a left radical
nephrectomy due to SCC of the kidney. To the best of our knowledge,
the present study is the first to describe a patient who regained
renal function and did not depend on dialysis following a
nephrectomy due to kidney SCC.
Case report
A 64-year-old female patient was admitted to
Hacettepe University Hospital (Ankara, Turkey) in November 2016
with fatigue and chest pain. The patient presented had a medical
history of asthma and hypertension. Laboratory examination revealed
that the serum creatinine levels, blood urea nitrogen levels and
the estimated glomerular filtration rate (eGFR) were 10.41 mg/dl
(normal range, 0.5–1.3 mg/dl), 175.80 mg/dl (normal range, 8–21
mg/dl) and 3 (normal, >60), respectively. Venous blood gas
analysis revealed acidosis (pH 7.09; normal range, 7.35–7.45). Due
to these test results, the patient underwent a permanent dialysis
catheter placement; the patient required dialysis by a hemodialysis
machine for three consecutive days (2, 3 and 4 h on day 1, 2 and 3,
respectively). The patient provided written informed consent for
the publication of this case report.
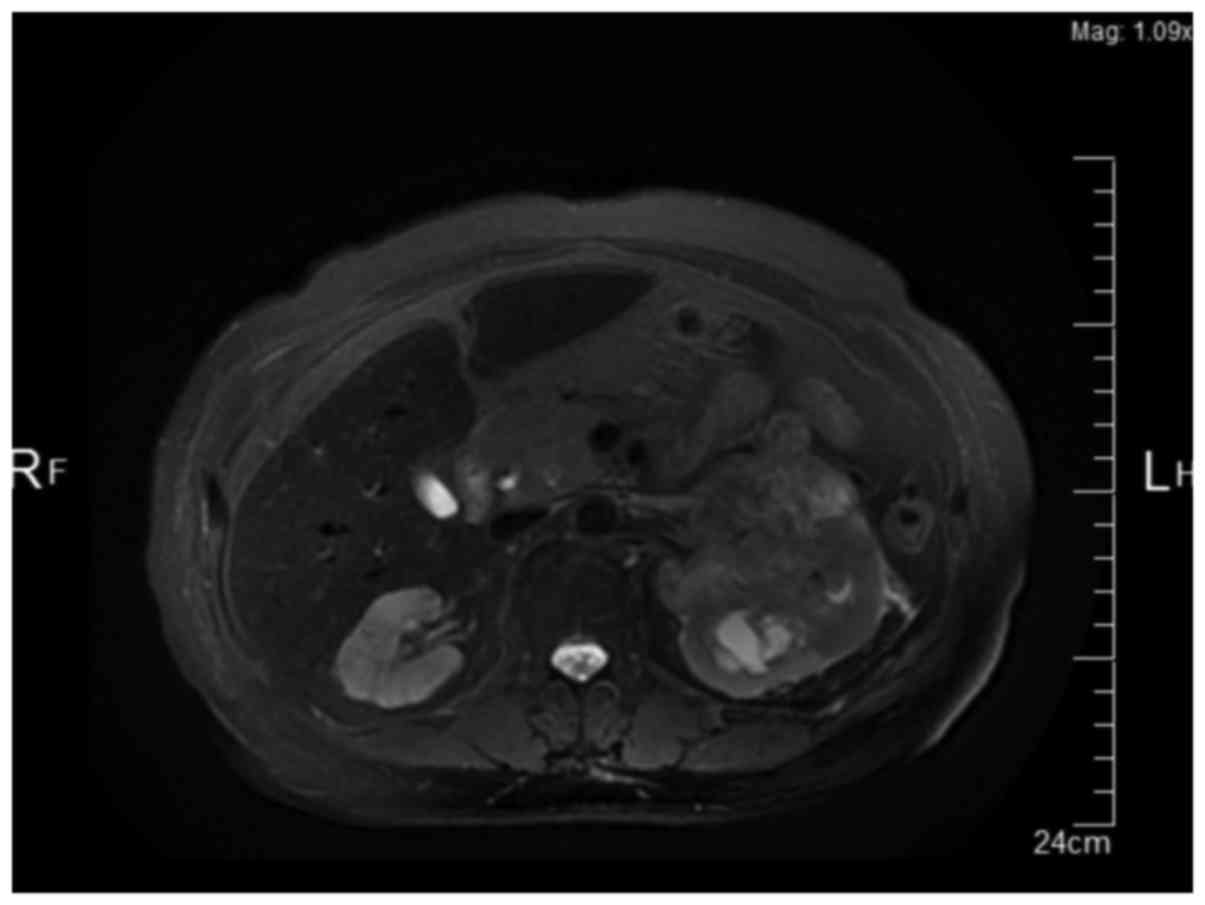
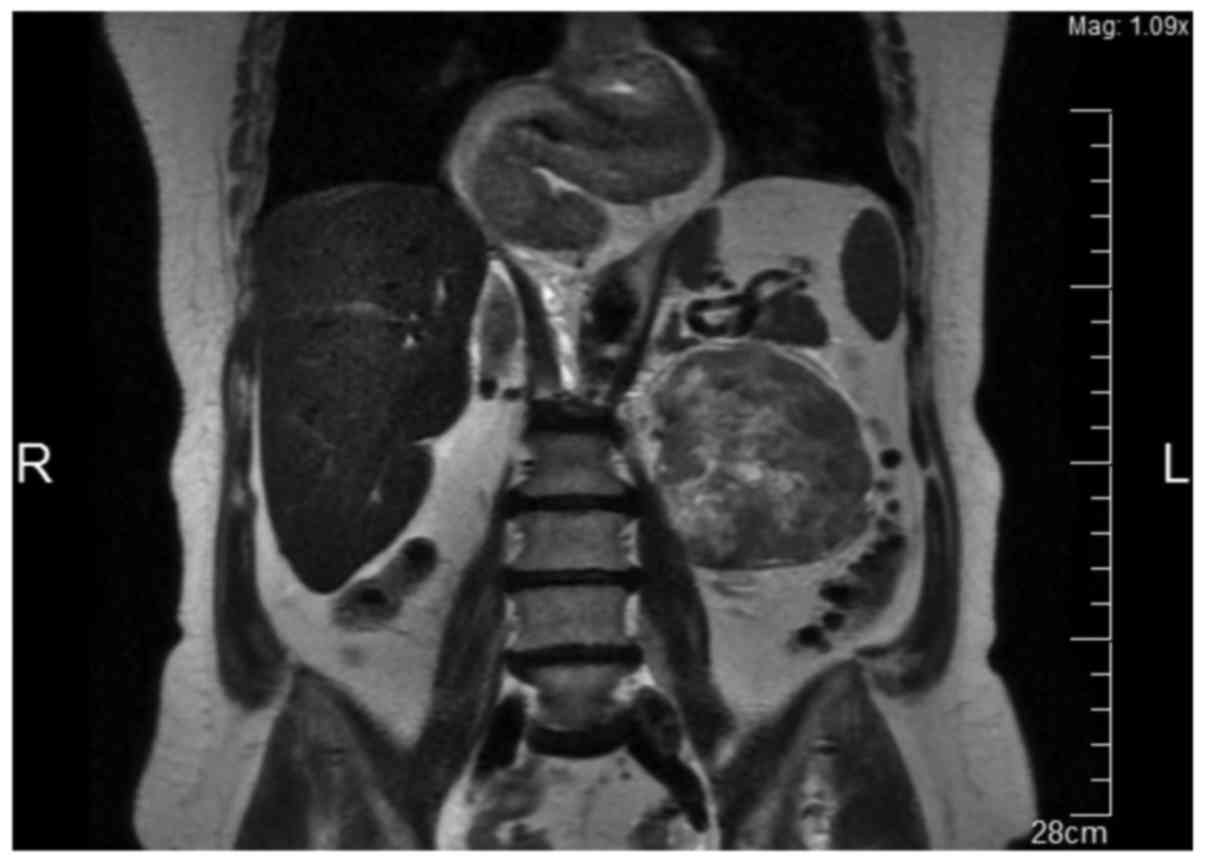
To determine the cause of renal failure, abdominal
ultrasonography (USG) was performed, which revealed a 95×84-mm
solid mass in the left kidney, and hydronephrosis due to the
pressure of the mass. To understand the structure of the mass and
identify potential metastasis, abdominal magnetic resonance imaging
(MRI) and thoracic computed tomography (CT) scans were performed.
Abdominal MRI revealed a 93×88-mm solid lesion originating from the
upper pole of the left kidney, but no evidence of metastasis
(Figs. 1 and 2). The thoracic CT revealed no
metastasis.
The patient underwent laparoscopic radical
nephrectomy via a transperitoneal approach. On macroscopic
examination, the resected kidney was determined to be 11×11×9 cm.
The cut surface of the organ revealed a solid mass (largest
diameter, 10.5 cm) that occupied the renal parenchyma almost
entirely. The tumor filled out the collecting duct system,
obliterated the pelvic cavity and invaded the perinephric and hilar
fat tissue. The tumor reached Gerota's fascia with positive
surgical margins. Following overnight fixation in 4% formaldehyde
at room temperature, samples from the tumor and surrounding kidney
were taken and subjected to routine paraffin embedding procedure.
The paraffin-embedded samples (thickness, 5 µm) were initially
stained with hematoxylin and eosin on Shandon Varistain Gemini
(Shandon, Frankfurt, Germany) automated slide stainer (completed in
50 min at room temperature). Additional histochemical staining with
Jones' methenamine silver method was performed to assess the
non-neoplastic kidney morphology. For this, slides were kept in
0.5% working silver solution for 75 min at 70°C. All light
microscope evaluations were performed using Zeiss Axioscope. A1
optical microscope. Various magnifications (×4, ×10, ×20 or ×40)
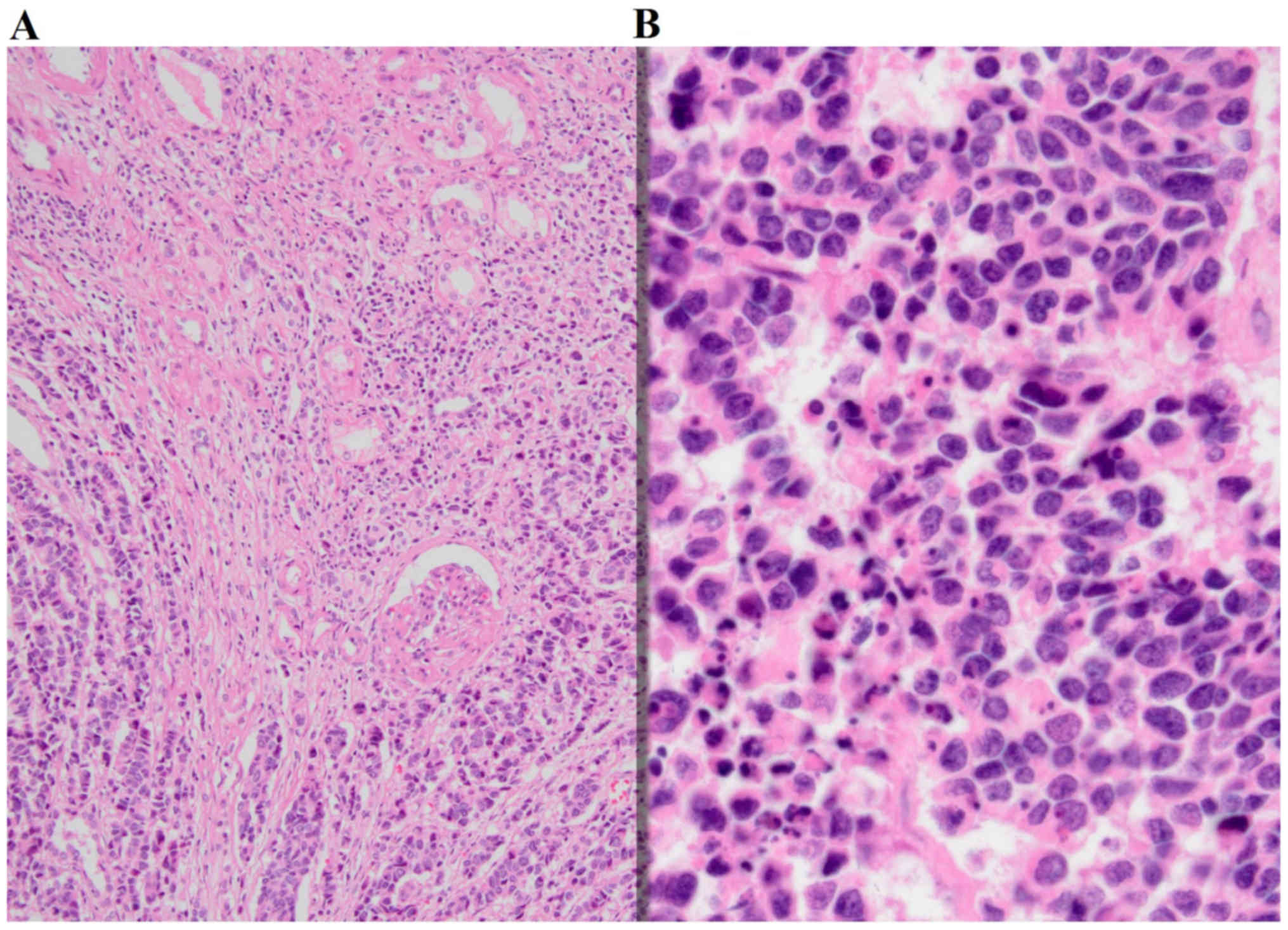
were applied depending on the requirement. Tumor sections revealed
neoplastic cells with narrow cytoplasm and small hyperchromatic
irregular molding nuclei forming hypercellular sheets, nests,
columns and rosette-like structures (Fig.
3). Large areas of necrosis and lymphovascular invasion were
observed. Mitotic rate was high (>50/10 high power field) with
abundant apoptotic figures.
An immunohistochemical panel was performed on the
Leica-BOND-Max automated staining platform (Leica Microsystems,
Wetzlar, Germany). Briefly, the tissue sections from the
representative paraffin blocks that were cut at 4 µm thickness onto
charged slides were deparaffinized with Bond Dewax solution (Leica
Microsystems; cat. no. AR9222) at 75°C. Following the treatment
through a 96% alcohol series and heat induced epitope retrieval
with an EDTA-based buffer (Leica Biosystems, Newcastle Ltd.,
Newcastle Upon Tyne, UK; cat. no. AR9640) at 100°C for 10 min,
tissue sections were incubated for 25 min with the following
primary antibodies at room temperature: Anti-cytokeratin 7 (Leica
Microsystems; dilution, 1:100; cat. no. NCL-L-CK7-560),
anti-synaptophysin (Leica Microsystems; dilution, 1:100; cat. no.
NCL-L-SYNAP-299), anti-chromogranin (Invitrogen; Thermo Fisher
Scientific, Inc.; dilution, 1:100; cat. no. MA5-13096),
anti-thyroid transcription factor-1 (TTF-1) (Leica Microsystems;
dilution, 1:200; cat. no. NCL-L-TTF-1), anti-Pax8 (Thermo Fisher
Scientific, Inc.; dilution, 1:200; cat. no. MA1-117), anti-GATA
binding protein-3 (Biocare Medical; dilution, 1:80; cat. no. CM 405
B) and Wilms Tumor-1 (Biocare Medical; dilution, 1:100; cat. no. CM
258 BK). Washing between the steps was accomplished by TBS (Leica
Microsystems; cat. no. AR9590). Next, the Bond Polymer Refine
Detection kit (Leica Biosystems, Newcastle Ltd.; cat. no. DS9800)
was used for the detection of proteins. The kit included several
reagents which were used sequentially: 3–4% hydrogen peroxide to
block endogenous peroxidase activity (13 min at room temperature),
ready-to-use secondary antibody (9 min at room temperature),
horseradish peroxidase-IgG polymer (9 min at room temperature),
3,3′-diaminobenzidine tetrahydrochloride (DAB) as a chromogen (7
min at room temperature) and hematoxylin for counterstaining (3 min
at room temperature). Immunohistochemically stained slides were
evaluated under the light microscope using various magnifications
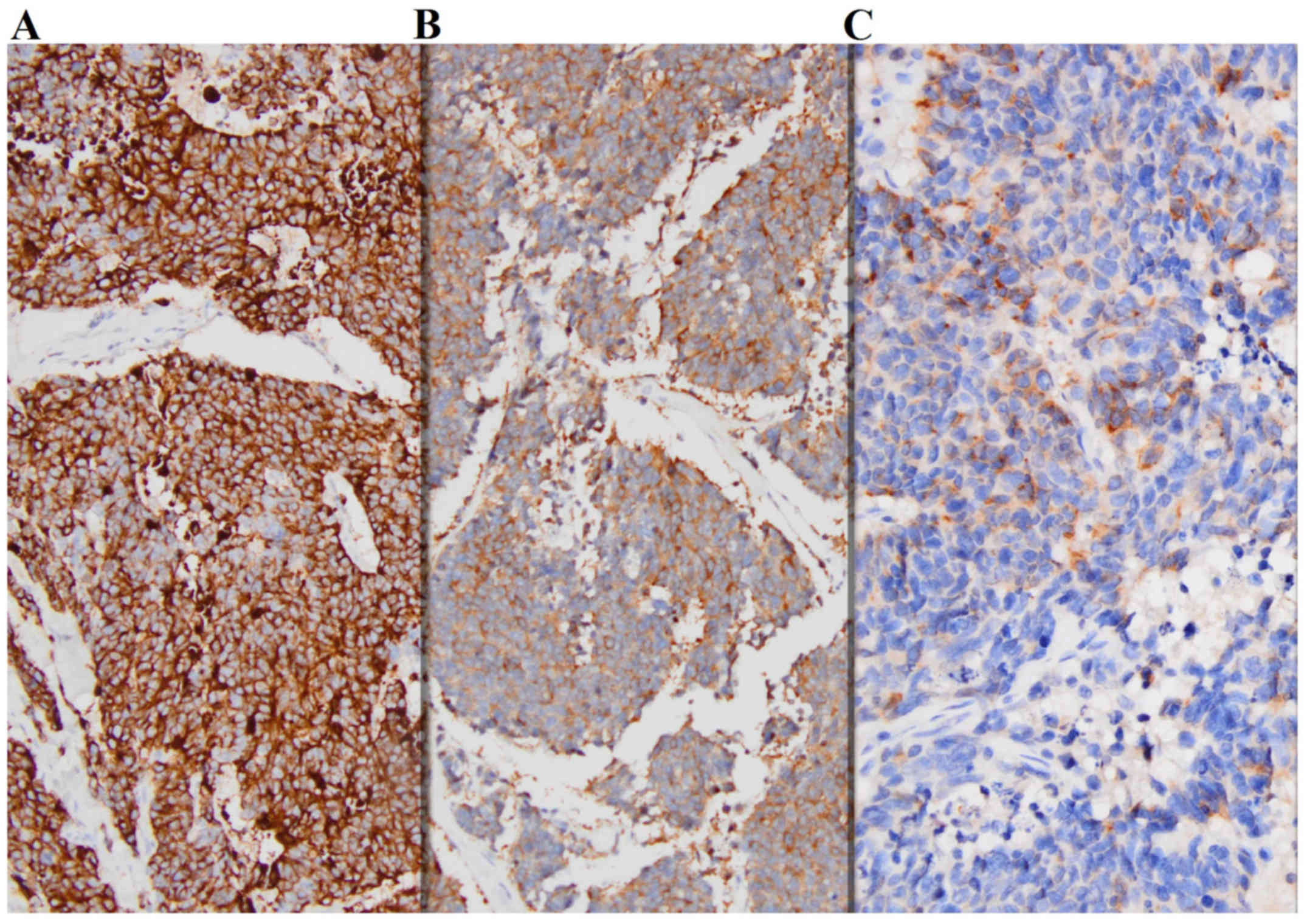
with ×4, ×10, ×20 or ×40 objectives. The tumor cells demonstrated
diffuse and strong reactivity for cytokeratin 7, synaptophysin,
chromogranin and TTF-1 (Fig. 4). No
staining for pax 8, GATA-3 or WT-1 was observed. The diagnosis of
pure small cell carcinoma (poorly differentiated neuroendocrine
carcinoma) of kidney was rendered. No associating component of
renal cell cancer or urothelial carcinoma was identified.
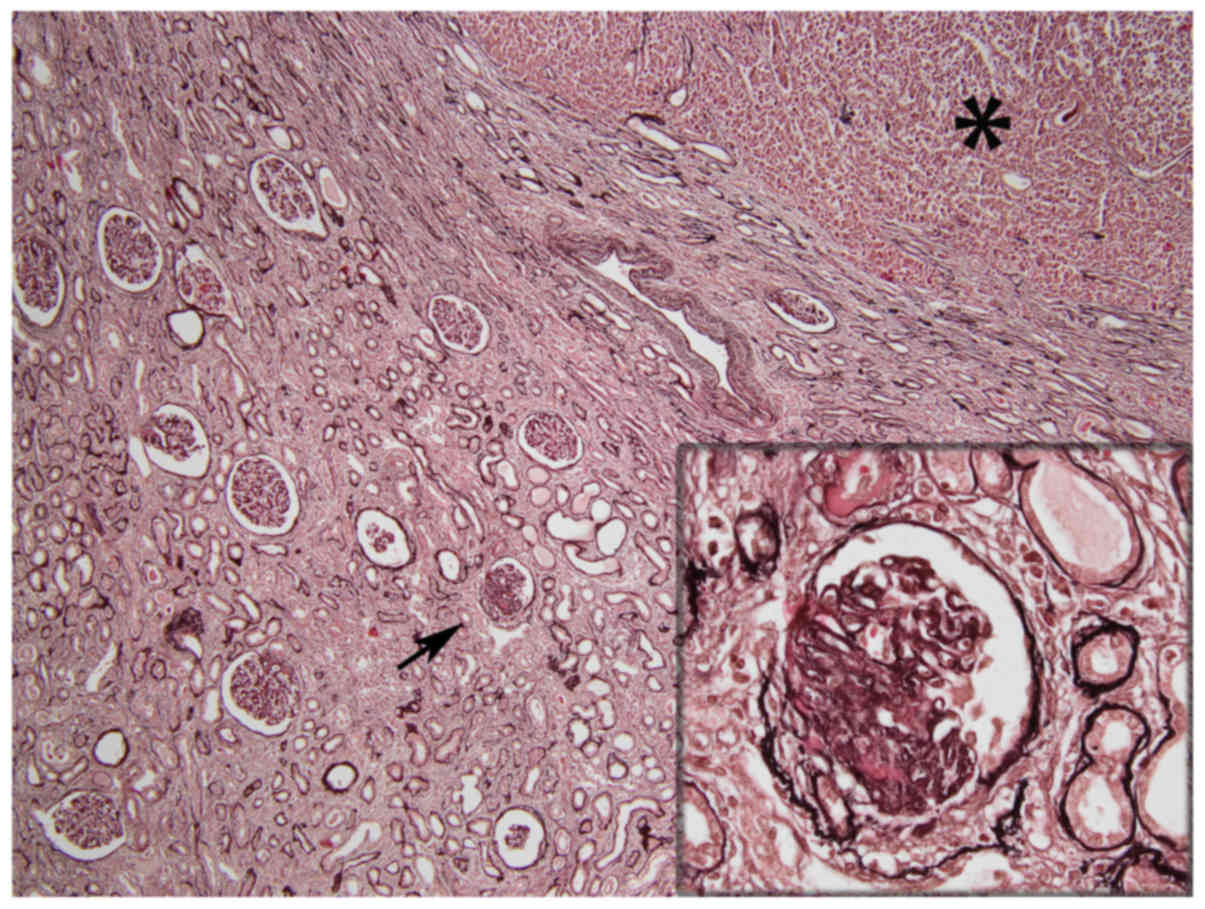
Non-neoplastic renal parenchyma outside the tumor
reflected chronic alterations characterized by widespread tubular
atrophy and interstitial fibrosis with scattered globally and
segmentally sclerotic glomeruli (Fig.
5). There was a mild interstitial inflammatory infiltrate
consisting of limited lymphocytes. No proliferative glomerular
changes were identified. Immunofluorescence staining, performed on
2 µm paraffin sections following antigen retrieval, as previously
described (5), revealed no
immunoglobulin (Ig) G, IgA, IgM, complement component (C3, C4 or
C1q) κ and λ light chains deposition in the glomeruli, tubular
basement membranes or blood vessels, which indicated absent
expression. Considering the absence of proteinuria or hematuria in
the patient, the observed chronic renal parenchymal changes were
consistent with obstructive nephropathy induced by the tumor
obliterating the pelvicalyceal system.
Control positron emission tomography/CT was
performed and revealed no metastasis. The patient required dialysis
10 and 6 times prior to and following surgery, respectively.
Subsequent to surgery, the patient received follow-up every week
(for 8 months) without requiring dialysis or exhibiting evidence of
disease. The patient's preoperative renal failure status was
thought to be paraneoplastic due to the disappearance following
nephrectomy of the primary tumor.
On the date of the final follow-up, serum creatinine
levels, blood urea nitrogen levels and the eGFR were 3.97 mg/dl
(normal range, 0.5–1.3 mg/dl), 91.00 mg/dl (normal range, 8–21
mg/dl) and 11 (normal, >60), respectively. Twelve-hour urine
sample was collected. The collection of urine began in the morning.
Urine protein analysis (12 h) revealed 165.8 mg/12 h (normal, 150
mg/12 h) proteinuria. The patient received adjuvant
carboplatin-etoposide chemotherapy.
Discussion
Due to the rarity of neuroendocrine SCC of the
kidneys, there are limited data associated with the natural course
of and treatments for the disease. The existing data is based only
on a few case reports and patient series.
Recommending treatments for extra-pulmonary SCC is
challenging due to its multiple potential origins. However, a prior
study suggested that patients should be grouped according to
whether they exhibit localized or extended SCC. Chemotherapy is
advised for patients with extended SCC, and surgical treatment with
adjuvant chemotherapy is indicated for patients with localized SCC
(2). The present study received
carboplatin-etoposide adjuvant chemotherapy, as the literature
suggested (2).
SCC of the kidneys was first described by Capella
et al (6) in 1984. In 2003,
Majhail et al (7) demonstrated
that small cell neuroendocrine carcinoma of the kidney is ~3.4
times more common in females, as compared with renal cell
carcinoma. The mean survival time of patients with small cell
neuroendocrine carcinoma of a kidney is <1 year (7). Metastasis is observed in ~60% of
patients with small cell neuroendocrine carcinoma of the kidney,
although there may be no sign of metastasis at the time of
diagnosis (7). Lee et al
(8) determined that the mean duration
for recurrence is 4.8 months. Therefore, occult metastasis were
considered a possible explanation for recurrence in these patients
(8). A close follow-up after initial
treatment is crucial for patients with small cell neuroendocrine
carcinoma of the kidney due to the high risk of early local
recurrence and distant metastasis (8). A cisplatin-based chemotherapy regimen
has been demonstrated to improve survival (7,8).
Following a radical nephrectomy, eGFR initially
decreases but recovers during the long-term follow-up. Extended
follow-up results for eGFR in patients who underwent radical
nephrectomy were reported by Scosyrev et al (9) in 2014. While 85.7% of the patients
underwent radical nephrectomy reached an eGFR of <60 during a
15-year follow up, this rate had decreased to 58.7% at the time of
the final follow-up (9).
All types of genitourinary cancer can cause
paraneoplastic syndrome (PNS), but renal cell carcinoma is the most
common type of tumor causally associated with PNS (4). Sacco et al (4) stated in 2009 that, among patients with
renal cell carcinoma, ~33% exhibit PNS. In patients with renal cell
carcinoma, the majority of PNS cases disappear following
nephrectomy (4). The majority of
endocrinological PNS cases are associated with neuroendocrine
tumors, particularly SCC (4). In the
present study, acute kidney failure was hypothesized to be
associated with PNS. Renal function improved following nephrectomy,
which supported this hypothesis.
While hematological malignancies presenting with
acute renal failure have previously been reported in the
literature, to the best of our knowledge, this is the first study
to assess a patient with a renal tumor who presented with acute
renal failure (10).
To conclude, surgery may be considered as a
treatment option in dialysis-dependent patients with renal tumors,
and surgically eliminating the tumor burden may facilitate the
recovery of patient eGFR.
References
|
1
|
Govindan R, Page N, Morgensztern D, Read
W, Tierney R, Vlahiotis A, Spitznagel EL and Piccirillo J: Changing
epidemiology of small-cell lung cancer in the United States over
the last 30 years: Analysis of the surveillance, epidemiologic, and
end results database. J Clin Oncol. 24:4539–4544. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Dakhil CS, Wick JA, Kumar AK, Satyan MT
and Neupane P: Extrapulmonary small cell carcinoma: The University
of Kansas experience and review of literature. Med Oncol.
31:1872014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Carranza OE, Castañón E, Abella LE,
Zudaire ME, Castillo A, Arévalo E, Fusco JP, Zudaire JJ, Carias R,
Cambeiro M, et al: Clinical management of small-cell carcinoma of
the urinary tract: A 10-year single-center's experience. Clin
Genitourin Cancer. 11:168–174. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sacco E, Pinto F, Sasso F, Racioppi M,
Gulino G, Volpe A and Bassi P: Paraneoplastic syndromes in patients
with urological malignancies. Urol Int. 83:1–11. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Nasr SH, Galgano SJ, Markowitz GS, Stokes
MB and D'Agati VD: Immunofluorescence on pronase-digested paraffin
sections: A valuable salvage technique for renal biopsies. Kidney
Int. 70:2148–2151. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Capella C, Eusebi V and Rosai J: Primary
oat cell carcinoma of the kidney. Am J Surg Pathol. 8:855–861.
1984. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Majhail NS, Elson P and Bukowski RM:
Therapy and outcome of small cell carcinoma of the kidney: Report
of two cases and a systematic review of the literature. Cancer.
97:1436–1441. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lee SY, Hsu HH, Lin HY, Chen YC, Wong YC,
Wang LJ, Ng KF, Chuang CK, Hung CC and Yang CW: Factors associated
with the survival of patients with primary small cell carcinoma of
the kidney. Int J Clin Oncol. 18:139–147. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Scosyrev E, Messing EM, Sylvester R,
Campbell S and Van Poppel H: Renal function after nephron-sparing
surgery versus radical nephrectomy: Results from EORTC randomized
trial 30904. Eur Urol. 65:372–377. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Prakash J, Mandal AK, Vohra R, Wani IA,
Hota JK, Raja R and Singh U: Renal disease is a prodrome of
multiple myeloma: An analysis of 50 patients from eastern India.
Ren Fail. 31:267–271. 2009. View Article : Google Scholar : PubMed/NCBI
|