Introduction
Alveolar soft part sarcoma (ASPS) is a rare form of
soft tissue neoplasm that accounts for between 0.5 and 0.9% of all
soft tissue sarcomas, and between 1 and 15% of malignant tumours in
adults and children, respectively (1). ASPS may occur at any age, with a peak
incidence in the third decade of life. ASPS is usually identified
in the extremities in adults, and the head and neck region in
children, particularly the orbit and tongue. However, it is rare
for primary ASPS lesions to form in the orbit. In the present
study, the clinical manifestations, imaging results, pathological
features, treatment strategies and prognosis of 8 cases of orbital
ASPS over the last 15 years were reviewed. Domestic and foreign
literature regarding ASPS was also reviewed for further
comprehension of this rare type of tumour.
Materials and methods
Ethics statement
The present retrospective study was approved by the
Medical Ethics Committee of the General Hospital of Chinese
People's Armed Police Forces (Beijing, China) and conducted in
compliance with the tenets of The Declaration of Helsinki. All
patients or their parents provided written informed consent.
Patients
Patients with orbital ASPS who were treated over the
last 15 years (from January 2000 to April 2015) at the General
Hospital of Chinese People's Armed Police Forces were considered in
the present study (n=8). A comprehensive retrospective review was
performed to evaluate the characteristics of this type of sarcoma.
Information regarding the clinical course, including clinical
manifestations and treatment, was collected from the patients'
medical records. Computed tomography (CT) and magnetic resonance
imaging (MRI) results were acquired from the database at the
General Hospital of Chinese People's Armed Police Forces. Outcome
information was obtained from follow-up data and phone calls to the
patients or their parents.
Haematoxylin and eosin (H&E)-stained slides,
periodic acid-Schiff (PAS)-stained slides and immunohistochemical
slides were available in all cases. The diagnosis of ASPS was
confirmed by the review of these slides by experienced pathologists
at the General Hospital of Chinese People's Armed Police
Forces.
A review of the English literature based on a PubMed
search spanning 1963 to 2013 and a review of the Chinese literature
based on a China Knowledge National Infrastructure search spanning
from 1981 to 2014 were performed, and all cases of orbital ASPS
with detailed data were included. Cases were excluded if they were
duplicated or their information was too generalized.
Results
Clinical data and ophthalmological
examination
From a total of 8 patients, 3 were male and 5 were
female, with age at presentation ranging between 2 and 51 years
(median, 9.5 years). Patients <20 years of age made up 75.0%
(n=6) of the sample, of which 5 were <10 years of age (62.5%).
The duration of symptoms ranged between 9 days and 1 month. The
tumour was located in the right orbit in 3 cases and the left orbit
in 5 cases. Clinical manifestations were mainly proptosis and
abnormal position of the eye (Fig.
1). Certain individuals also exhibited accompanying eyelid
swelling, blepharoptosis, headache, ophthalmodynia, impaired
vision, diplopia and subconjunctival vasodilatation. Detailed data
are presented in Table I.
 | Table I.Clinical features of patients with
orbital alveolar soft part sarcoma. |
Table I.
Clinical features of patients with
orbital alveolar soft part sarcoma.
| Patient | Age, years/sex | Eye affected | Course of
disease | Clinical
features | Tumour
location | Tumour size,
cm | Management | Follow-up |
|---|
| 1 | 19/M | Right | 1 mh | Proptosis,
diplopia, ophthalmalgia, anorthopia, ocular motility restriction,
conjunctival congestion, papilloedema | Medial part of the
orbit, adhering to medial rectus muscle, extending to apex | 2.5×1.5×1.5 | S+R | 6 mh, no Rec or M,
lost |
| 2 | 51/F | Right | 1 mh | Proptosis,
ophthalmalgia, anorthopia, lid swelling, palpable mass,
papilloedema | Medial optic nerve,
indistinguishable from medial rectus muscle | 3.5×3.5×1.2 | S+E+R | Lost |
| 3 | 2/F | Right | 1 mh | Proptosis,
ophthalmalgia, anorthopia | Inside inferior
rectus muscle throughout its length to apex | 5.0×3.6×0.8 | S | Gave up therapy, 2
mh Rec, 1 yr succumbed |
| 4 | 6/M | Left | 15 days | Proptosis, ptosis,
lid swelling, ocular motility restriction | Inside superior
rectus muscle | 2.0×1.5×1.2 | S+R | 61 mh, no Rec or
M |
| 5 | 2/M | Left | 1 mh | Proptosis, tearing,
anorthopia, ocular motility restriction | Between superior
rectus muscle and levator palpebrae superioris muscle | 2.0×2.0×2.0 | S+R | 49 mh, no Rec or
M |
| 6 | 9/F | Left | 9 days | Proptosis, lid
swelling, ocular motility restriction | Inside medial
rectus muscle | 4.5×3.0×1.0 | E+R+C | 13 mh, no Rec or
M |
| 7 | 10/F | Left | 20 days | Proptosis, lid
swelling, diplopia, pain, vision impaired, anorthopia, ocular
motility restriction, papilloedema | Inferolateral,
indistinguishable from inferior and lateral rectus muscle and optic
nerve | 4.5×3.0×1.5 | B+E | 13 mh, no Rec or
M |
| 8 | 32/F | Left | 1 mh | Vision impaired,
diplopia, proptosis, ophthalmalgia | Indistinguishable
from lateral rectus muscle | 5.0×3.0×2.0 | S+R+C | 3 mh, no Rec or
M |
Table II summarizes
the cases of orbital ASPS reported in the literature listed on
PubMed (1–22), excluding this series. There were 55
cases (33 female and 22 male patients) between 1963 and 2014, with
a median age at diagnosis of 12 years (ranging between 10 months
and 69 years). The lesion was located in the right orbit in 19
cases, the left orbit in 22 cases and the location of the mass was
not provided in 14 cases. The median tumour size was 2.95 cm in the
largest diameter. Table III
summarizes the cases reported in the Chinese literature from 1981
to 2014 (23–36). There were 9 female and 10 male
patients, totalling 19 cases, with a median age at diagnosis of 11
years (range, 2–53 years). The lesion was located in the right
orbit in 7 cases and in the left orbit in 12 cases. The median
tumour size was 2.45 cm. When summing up the data in Tables I–III,
there were 82 patients with orbital ASPS (47 female and 35 male
patients), with a median age of 12 years at diagnosis. The median
tumour size was 2.85 cm. There was a slight female predilection
(female/male ratio, 1.34:1) in orbital ASPS when compared with ASPS
arising in other locations.
 | Table II.Reported cases in PubMed of orbital
alveolar soft part sarcoma. |
Table II.
Reported cases in PubMed of orbital
alveolar soft part sarcoma.
| No. | Author | Country | Number of
cases | Age (median) | Sex | Eye affected | Tumour
location | Tumour size,
cm | Management | Follow-up | (Refs.) |
|---|
| 1 | Mulay et al,
2014 | India | 9 | 1–31 (6) yr | 2 M, 7 F | NM | Intraconal, close
to optic nerve: 1; association with and indistinct from extraocular
muscles: 8 | NM | 7: S+R; 2:
S+R+C | 6–126 mh (median 43
mh)/no Rec or M | (2) |
|
|
|
|
| 12 yr | F | L | Surrounding optic
nerve | 3.9×2.5×2.3 | B+E | 2 mh/no Rec/M |
|
| 2 | Kim et al,
2013 | USA | 2 | 22 yr | M | L | Involving
temporalis muscle | 4.5 | B+S+R+E+C | 7 mh/local Rec, 2
mh/Rec involving anterior cranial fossa, M to lungs and liver | (3) |
| 3 | Majumdar et
al, 2013 | India | 1 | 25 yr | M | R | Abutting superior
rectus muscle | NM | S | 6 mh/no Rec or
M | (4) |
| 4 | Rekhi et al,
2012 | India | 2 | 19 yr | M | NM | NM | 3.0×3.0×2.0 | S | 39 mh/M to lungs,
alive | (5) |
|
|
|
|
| 31 yr | M | NM | NM | NM | S | NM |
|
| 5 | Rose et al,
2011 | Kenya | 1 | 5 yr | M | L | Replace superior
rectus muscle throughout its length | NM | S | 1 mh/no Rec or
M | (1) |
|
|
|
|
| 15 mh | M | L | Antero-inferior
orbit | 2.9×1.8 | NM | NM |
|
| 6 | Alkatan et
al, 2010 | Saudi Arabia | 2 | 6 yr | F | R | Superior orbit,
associated with superior and medial rectus muscles | NM | NM | NM | (6) |
|
|
|
|
| 3 yr | F | R | NM | 1×1×1.5 | S | 3 mh/Rec |
|
| 7 | Pang et al,
2008 | China | 3 | 10 yr | F | R | NM | 1.5×1×0.8 | S | 6 mh/Rec | (7) |
|
|
|
|
| 11 yr | F | R | NM | 7×6×4 | S | Lost |
|
| 8 | Morris et
al, 2005 | USA | 1 | 45 yr | F | L | Retrobulbar,
medially | 2.2×2.0×0.8 | S | 3 mh/no Rec or
M | (8) |
|
|
|
|
| 15 yr | M | NM | Lower eyelid | 2.0 | S+R+C | 16 yr/no Rec or
M |
|
| 9 | Kanhere et
al, 2005 | India | 2 | 14 yr | F | NM | Orbit, no
details | 3.0 | E+R | 1 yr/no Rec or
M | (9) |
|
|
|
|
| 19 yr | M | L | Anterosuperior | 5.0×4.0×3.0 | S; R+C | 1 yr/Rec |
|
| 10 | Kashyap et
al, 2004 | India | 3 | 8 yr | F | L | Superomedial | NM | B+E+R+C | 2 yr/no Rec or
M | (10) |
|
|
|
|
| 12 yr | F | L | Inferolateral | NM | S | 2 yr/no Rec or
M |
|
| 11 | Khan and Burke,
2004 | USA | 1 | 10 yr | F | L | Contiguous with and
indistinguishable from medial rectus muscle | 2.0×2.7 | S Rec or M | 5 yr/no | (11) |
| 12 | Chan et al,
2004 | China | 1 | 4 yr | M | R | Inferotemporal | 3.0 | B+S | 2 yr/no Rec or
M | (12) |
| 13 | Lasudry and
Heimann, 2000 | Belgium | 1 | 2 yr | M | L | Displace or involve
the superior rectus/levator muscle complex | NM | B+C+E | 1 yr/no Rec or
M | (13) |
| 14 | Coupland et
al, 1991 | Germany | 1 | 32 yr | M | L | Among optic nerve,
medial and superior rectus muscle | 1.6×1.5×1.5 | S | 4 yr/no Rec or
M | (14) |
| 15 | Chodankar et
al, 1986 | India | 1 | 15 yr | M | L | Inferior | 2.0×1.0×1.0 | S | 9 mh/no Rec or
M | (15) |
| 16 | Font et al,
1982 | USA | 17 | 11 mh-69 yr (18
yr) | 13 F; 4 M | 8 R, 8 L; 1 NM | Not mentioned, 1
case with a figure revealed overlying lateral rectus muscle | NM | B1, B+S+EN1, S5,
S+R5, E2, E+R2 | 3.5–20.6 yr (median
11.4 yr) 10 alive (2 Rec), 2 succumbed to M, 2 lost, 3 succumbed
for other reasons | (16) |
| 17 | Ishikura et
al, 1979 | Japan | 1 | 15 mh | F | R | NM | NM | B+E+R | 4 yr/no Rec or
M | (17) |
| 18 | Mukherjee and
Agrawal, 1979 | India | 1 | 30 yr | M | R | Extending from
superior temporal to apex, orbicularis infiltrated | NM | E | Lost | (18) |
| 19 | Varghese et
al, 1968 | India | 1 | 13 yr | F | L | Lateral side,
infiltrating lateral rectus muscle | NM | E | A number of
mh/Rec | (19) |
| 20 | Abrahams et
al, 1968 | USA | 1 | 55 yr | M | R | Inferior rectus
muscle replaced by tumor | 2.5×1.8×0.8 | E | 1 yr/no Rec or
M | (20) |
| 21 | Altamirano-Dimas
and Albores-Saavedra, 1966 | Mexico | 2 | 10 mh | M | R | Attached to
inferior oblique muscle | 3.5×3×2 | S | 1 yr/Rec
succumbed | (21) |
|
|
|
|
| 3 yr | F | L | External portion
surgery | 3.5 | S | Succumbed
during |
|
| 22 | Nirankari et
al, 1963 | India | 1 | 38 yr | M | R | NM | 3×1.5 | S+E+R | 1 yr/R, lost | (22) |
 | Table III.Reported cases in Chinese
publications of orbital alveolar soft part sarcoma. |
Table III.
Reported cases in Chinese
publications of orbital alveolar soft part sarcoma.
| No. | Author, year | Number of
cases | Age, years
(median) | Sex | Eye affected | Tumour
location | Tumour size,
cm | Follow-up | Management | (Refs.) |
|---|
| 1 | Cheng et al,
2013 | 5 | 3–19 (8) | 4 M, 1 F | 3 L, 2 R | Indistinguishable
from medial rectus muscle (1);
superior rectus muscle (1); lateral
rectus muscle (1); inferior rectus
muscle (2) | Largest diameter:
2–2.7 | 9–108 mh (median 52
mh), 4 cases no Rec/M, 1 case Rec | S+EN | (23) |
| 2 | Du and Wu,
2012 | 1 | 10 | F | L | Lateral,
indistinguishable from lacrimal gland | 1.5 | NM | S | (24) |
| 3 | Feng et al,
2010 | 1 | 2 | F | R | Adhering to
inferior oblique muscle | 2×2 | NM | S | (25) |
| 4 | Hu et al,
2009 | 1 | 8 | M | L | Retrobulbar,
lateral | NM | NM | NM | (26) |
| 5 | He et al,
2004 | 2 | 9 | F | L | Superotemporal,
lateral rectus muscle thickened | 2.5×2.3×2 | 7 yr R; S 0.5 yr no
Rec | S+R | (27) |
|
|
|
| 13 | F | L | Retrobulbar,
intraconal | 2.4×2×1.5 | 2 mh R; S 0.5 yr no
Rec | S+R |
|
| 6 | Dong et al,
2004 | 1 | 18 | M | R | Retrobulbar,
inferomedial, intraconal | 2.5×2.8 | NM | S | (28) |
| 7 | Wang et al,
2003 | 1 | 53 | M | L | Medially,
indistinguishable from medial rectus muscle | 4×3 | NM | S | (29) |
| 8 | Dong et al,
1996 | 1 | 25 | M | R | Retrobulbar,
medially, nodules in lungs and liver | 3xx3×1.2 | 1.3 yr Rec; S+C
alive | S | (30) |
| 9 | Xu, 1995 | 1 | 14 | M | L | Apex | NM | NM | B+E | (31) |
| 10 | Li et al,
1993 | 1 | 20 | F | L | Indistinguishable
from lateral rectus muscle | 2×0.5×0.8 | 3 yr/no Rec or
M | S | (32) |
| 11 | Liu, 1989 | 1 | 8 | F | R | Full of orbit | NM | 6.8 yr no
Rec/M | S | (33) |
| 12 | Wei, 1985 | 1 | 23 | M | R | NM | NM | 4 yr Rec; S 3 yr no
R/M | S | (34) |
| 13 | Huo et al,
1982 | 1 | 10 | F | L | Supraorbital | NM | 2 mh Rec; S 6 mh no
Rec/M | S+E | (35) |
| 14 | Ni, 1981 | 1 | 20 | F | L | NM | NM | 6 yr/no Rec/M | E | (36) |
Imaging features
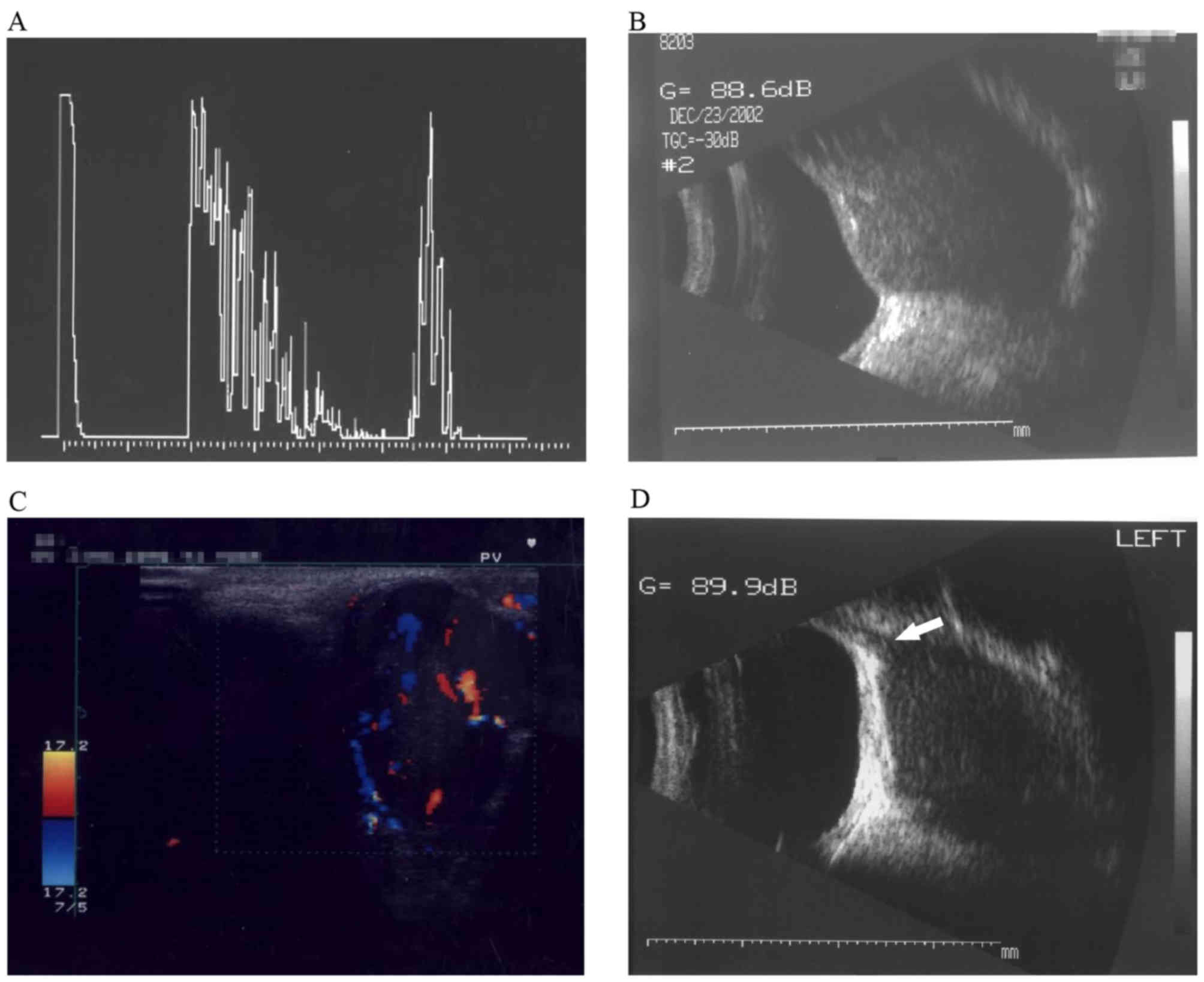
Ultrasonography was performed in 4 of the selected
cases, which demonstrated hypoechoic inhomogeneous soft tissue
masses with increased flow (Fig. 2).
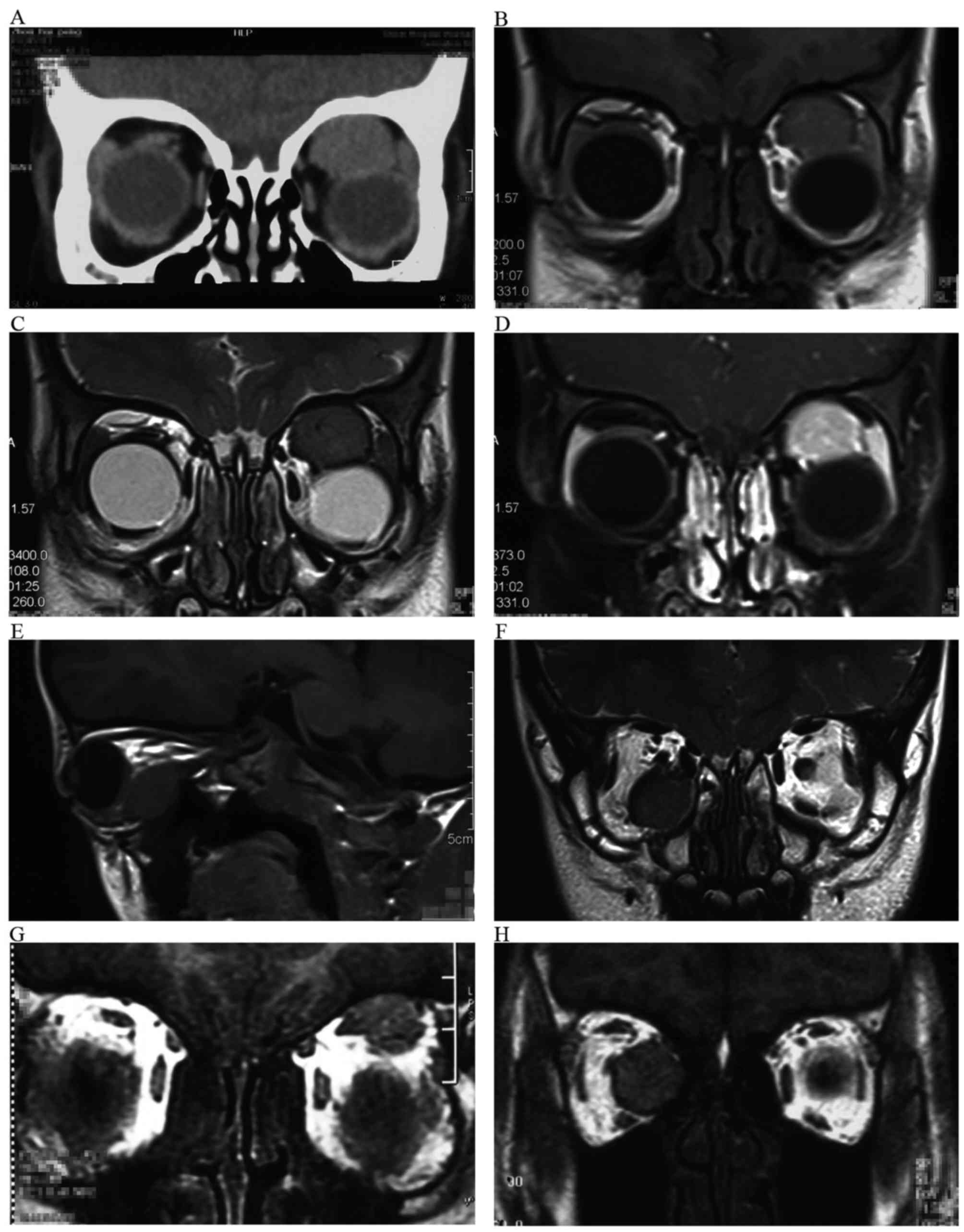
A computed tomography (CT) examination revealed well-circumscribed
ovoid and enhanced masses in all cases (Fig. 3A). MRI demonstrated that all the
tumours exhibited intermediate signal intensity in T1- and
T2-weighted images (Fig. 3B and C),
in addition to marked enhancement in contrast-enhanced images
(Fig. 3D). Imaging features
demonstrated that the lesions were located in the medial part of
the orbit in 3 cases, in the supraorbital foramen in 2 cases and in
the infraorbital foramen in 2 cases, and, in 1 case, the lesion
filled the orbital cavity. The tumours were associated with the
extraocular muscles (Figs. 2D and
3E-H). Tumours were located
intramuscularly in 3 cases, indistinguishable from the muscles in 3
cases and abutting the muscles in 2 cases. The average largest
diameter of the masses was 3.6 cm (range, 2.0–5.0 cm).
Histopathological features
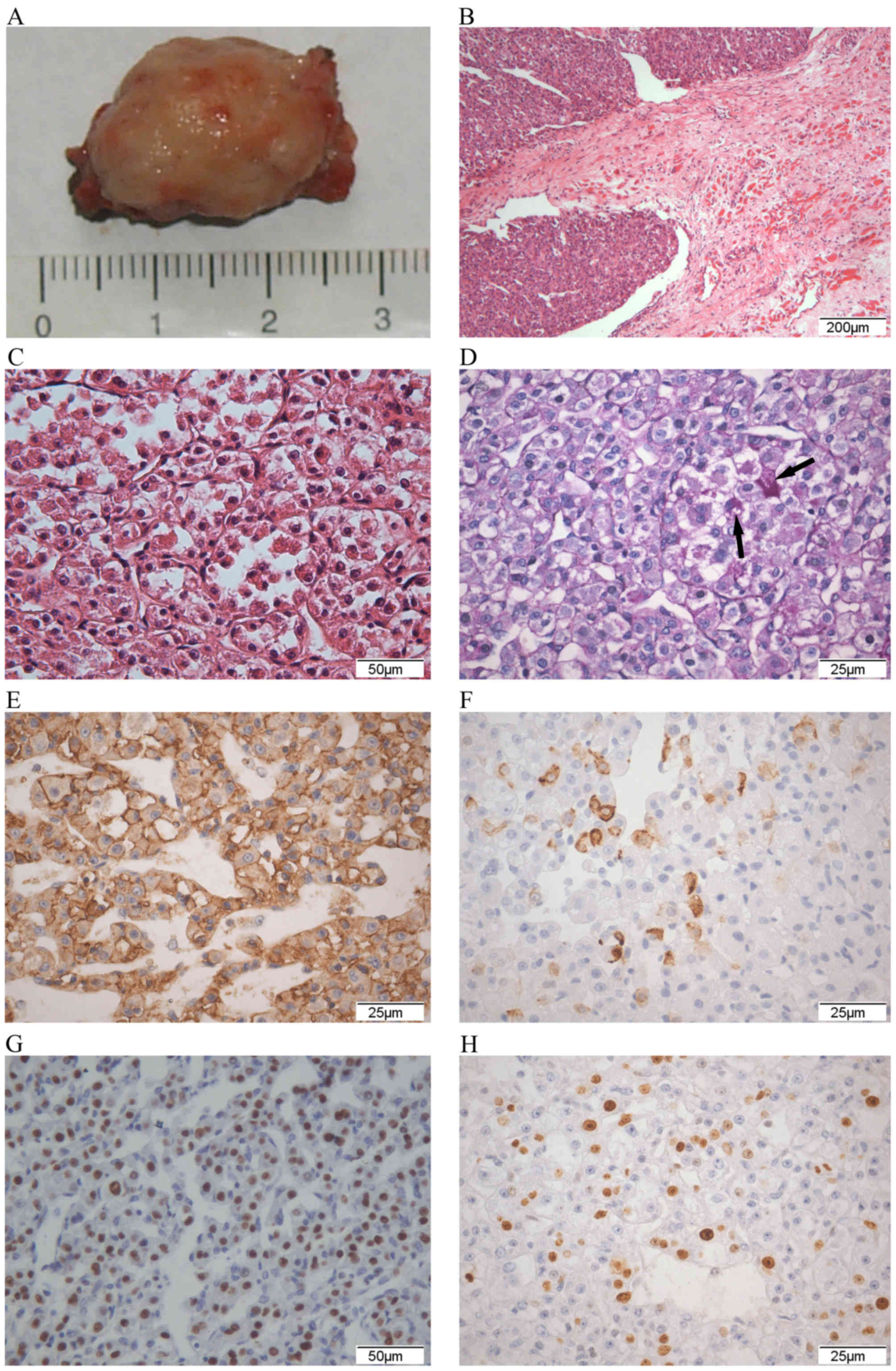
As presented in Fig.
4, overall, these poorly circumscribed pale grey or grey-yellow
masses were soft and friable, tending to haemorrhage (Fig. 4A). Microscopic examination identified
that the characteristic arrangement of the tumour cells was
organoid, in a nesting or alveolar pattern, which was more obvious
at low magnification. The size and appearance of the nests tended
to be uniform. The tumour cell nests were separated by delicate
septa of connective tissue containing sinusoidal vascular channels
lined by flattened endotheliocytes. The large oval or polygonal
tumour cells had a distinctly epithelioid appearance with somewhat
similar size and shape. The cell borders were sharply defined.
There were 1 or 2 large vesicular nuclei with prominent nucleoli
per cell. Nuclear atypia was not common. Eosinophilic cytoplasm was
abundant, with a finely granular, transparent or vacuolar pattern
(Fig. 4C). Mitotic figures were
uncommon. All cases were positive for diastase following PAS
staining (Fig. 4D), although this may
not have been apparent from H&E staining. Tumour emboli could
be observed in the small vessels in the tumour tissue of cases 4
and 5. Cases 2, 3 and 4 were positive for vimentin by
immunohistochemistry. Cases 1, 6 and 7 had desmin-positive foci
(Fig. 4F). Smooth muscle actin was
positive in a number of tumour cells in case 6. Transcription
factor binding to immunoglobulin heavy-chain enhancer 3 (TFE3) was
positive in all cases with the exception of case 3 (Fig. 4G). Cluster of differentiation (CD) 147
was positive in all cases. Other markers, including cytokeratin,
epithelial membrane antigen (EMA), carcinoembryonic antigen, actin,
neuron-specific enolase (NSE), synaptophysin, chromogranin A, S-100
protein, melanoma, melan A, CD99, CD34 and α-fetoprotein, were
negative in all cases. The antigen Ki-67 proliferation index was
<10% in the majority of cases, but was 15% in cases 2 and 3
(Fig. 4H; Table IV).
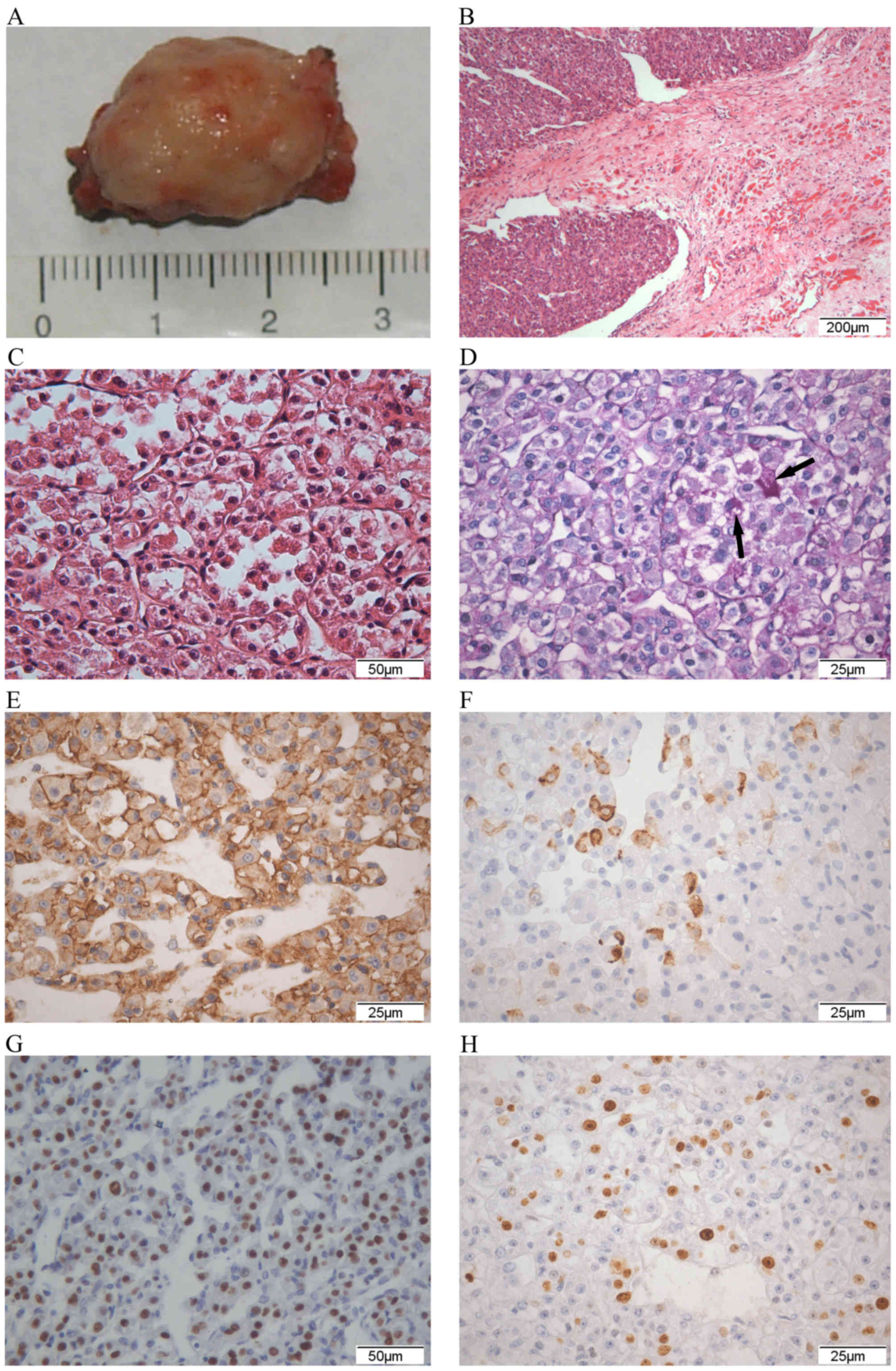 | Figure 4.Histopathological examination of
alveolar soft part sarcoma. (A) Gross examination of the
histopathological specimen revealed an encapsulated mass measuring
2.5×1.5×1.5 cm. It had adhered to the medial rectus muscle of the
right eye and extended to the apex. (B) Image of tissue from case 7
showing the association between the tumour and the extraocular
muscle. The left top of the fig. is the tumour and the remaining
muscle is located at the low right (H&E; magnification, ×50).
(C) Image of tissue from case 5 demonstrating nesting or organoid
arrangement separated by delicate partitions of fibrous connective
tissue, which formed a characteristic pseudoalveolar pattern. Blood
sinusoid was easily observed between the nests. The individual
tumour cells were round or polygonal with abundant eosinophilic and
finely granular cytoplasm and those at the nest centre were sparse.
Nuclear atypia was not obvious (H&E; magnification, ×200). (D)
PAS stain with diastase digestion of tissue from case 7 exhibited
the characteristic PAS-positive pruinose crystalline inclusions in
the cytoplasm of certain tumour cells (indicated by arrow). (PAS;
magnification, ×400). (E) Image of tissue from case 6 showing
strong membrane immunoreactivity of CD147 in certain tumour cells
(DAB; magnification, ×400). (F) Desmin immunostaining identified
focal cytoplasmic immunoreactivity in tissue from case 7 (DAB;
magnification, ×400). (G) The transcription factor for
immunoglobulin heavy-chain enhancer 3 immunostaining of tissue from
case 6 demonstrated specific marked nuclear immunoreactivity in
certain tumour cells (DAB; magnification, ×200). (H) Immunostaining
of tissue from case 3 revealed nuclear immunoreactivity for Ki-67
in certain tumour cells (DAB; magnification, ×400). PAS, periodic
acid-Schiff; CD, cluster of differentiation; DAB,
3,3′-diaminobenzidine; H&E, haematoxylin and eosin. |
 | Table IV.Immunohistochemical results of the
patients with orbital alveolar soft part sarcoma. |
Table IV.
Immunohistochemical results of the
patients with orbital alveolar soft part sarcoma.
| Case | Immunohistochemical
result |
|---|
| 1 |
Vimentin− desmin
focus+ actin− CK− NSE−
Syn− CgA− S-100− TFE3++
CD147+ Ki-67+5% |
| 2 | Vimentin
focus+ desmin− CK− NSE−
Syn− CgA− S-100− CEA−
TFE3++ CD147+ Ki-67+15% |
| 3 |
Vimentin+ desmin−
SMA− actin− CK− EMA−
NSE− Syn− CgA− S-100−
HMB45− CEA− AFP− CD34−
CD31− TFE3− CD147+ Ki-67+15% |
| 4 |
Vimentin+ desmin−
actin− CK− NSE− Syn−
CgA− S-100− HMB45− AFP−
CD34− CD99− TFE3++
CD147+ Ki-67+5% |
| 5 |
Vimentin− desmin−
CK− Syn− CgA− S-100−
Mela A− SMA− CD34−
CD99− TFE3++ CD147+ Ki-67+5% |
| 6 |
Vimentin− desmin
partly+ CK− NSE− Syn−
CgA− S-100− AFP− SMA
partly+ CD34++ TFE3++
CD147+ Ki-67+10% |
| 7 |
Vimentin− desmin
partly+ CK− NSE− Syn−
CgA− S-100− AFP− SMA−
CD34++ TFE3+++ CD147+
Ki-67+8% |
| 8 |
Vimentin− desmin−
Myogenin− CK− NSE− Syn−
CgA− S-100− CD56− CD34−
TFE3++ CD147+ Ki-67+5% |
Treatment and follow-up
Cases 1, 3, 4, 5 and 8 underwent surgical excision
of the tumour, cases 2 and 6 underwent orbital exenteration, and
case 7 underwent partial orbital exenteration. Cases 1, 2, 4, 5, 6
and 8 received postoperative local radiotherapy on the orbital
region. Cases 6 and 8 received chemotherapy. Case 1 was doing well
at 6 months and was then lost to follow-up. Cases 4, 5, 6, 7 and 8
were doing well with no evidence of local recurrence or metastasis
during the follow-up period (between 3 and 61 months). Local
recurrence of the tumour developed at 3 months post-tumorectomy in
case 3, with the patient succumbing 1 year after being withdrawn
from treatment by the patient's parents. Case 2 visited the
hospital presenting with recurrence of the tumour 3 months after
undergoing tumorectomy at another hospital. A doctor advised
orbital exenteration, which the patient declined, instead opting to
undergo excision of the tumour only. Local recurrence developed
again after 3 months. CT and MRI demonstrated that the orbital
cavity was occupied by the tumour. The patient underwent orbital
exenteration. The tumour was recurrent 3 months after surgery and
the patient received radiotherapy. The patient complained of
gradually aggravated headaches after 1 month. MRI demonstrated
invasion to the sphenoid bone. The patient eventually
succumbed.
The median period of follow-up following surgical
treatment was 12 months (range, 3–61 months) in the series of the
present study, whereas the period was 12 months (range, 2–247
months) in the PubMed literature (Table
II) and 48 months (range, 2–108 months) in the Chinese
literature (Table III). In the 65
patients with follow-up data, 43 (66.2%) were alive with no
evidence of disease during the follow-up period, 12 patients
(18.5%) were alive with local recurrence, and 2 (3.1%) exhibited
metastases to the lungs and liver. Certain patients (n=4; 6.2%)
succumbed to metastatic disease and 4 (6.2%) succumbed to
non-related causes.
Discussion
Alveolar soft part sarcoma (ASPS) is a rare tumour
primarily affecting children and adolescents. There is a slight
female preponderance in adults (60% of patients are female)
(37), which is not observed in
children (38). ASPS predominantly
affects the deep soft tissues of the extremities in adults,
particularly the thighs and buttocks; the arms, thorax and
retroperitoneum are seldom involved (39). The most common location in children is
the head and neck region, particularly the orbit and tongue
(16,40). Following the review of hundreds of
reports, it was identified that, in 172 cases, orbital involvement
had the second-highest incidence (15.1%), following the buttock and
thigh, and that orbital involvement had the highest incidence in
ASPS arising in the head and neck region (55%) (41).
Characteristics of orbital ASPS
From these data, it was concluded that orbital ASPS
has characteristics distinct from those of ASPS arising in other
locations: i) Orbital ASPS involves a younger population; the
median age of the patients when ASPS is diagnosed in locations
other than the orbit was >30 years (42,43),
whereas that of patients with orbital ASPS is <15 years; ii) the
course of disease is usually shorter in orbital ASPS since the
symptoms are easily noticed by the patient or parents, therefore:
i) Tumour size in orbital ASPS is frequently smaller than ASPS
arising in other locations. The median size of orbital ASPS is
usually <5 cm, whereas that in other locations is >5 cm
(5,42).
Clinical features
Orbital ASPS has no defining clinical features. As
with other space-occupying lesions in the orbit, patients with ASPS
primarily present with proptosis, abnormal position of the eyes,
eyelid swelling, and conjunctival congestion with dilated and
tortuous vessels (16). In certain
cases, metastasis to the lungs or brain may be the presenting
feature of ASPS (44).
Imaging features
Ultrasonography of ASPS is non-specific, but often
reveals a slightly hypoechoic or hyperechoic and heterogeneous soft
tissue mass with markedly increased blood flow. CT usually
demonstrates a soft tissue mass that is homogeneous and isodense to
muscle with vigorous enhancement. Reports in the literature on MRI
of this tumour have identified intermediate or hyperintense signal
intensity in T1-weighted images and hyperintense signal intensity
in T2-weighted images. The majority of lesions exhibit marked
intense enhancement in contrast-enhanced MRI (45,46). A
number of studies have focused on the characteristic imaging
features of orbital ASPS. In the present series of cases analysed,
all the lesions demonstrated intermediate signal intensity in T1-
and T2-weighted images, the majority with marked enhancement in
contrast-enhanced images.
Diagnosis and differential diagnosis
There are no distinct characteristics in the
clinical and imaging features of this kind of tumour. Owing to the
high vascularization, the tumour may be misinterpreted as a type of
vasogenic tumour, including hemangioma, lymphangioma or
hemangiopericytoma, by clinicians prior to surgery (47). The final diagnosis should be dependent
on the pathological examination following surgery. The
pathomorphological features of ASPS should allow for differential
diagnosis from other tumours, including paraganglioncytoma,
granular cell tumour, amelanotic melanoma, alveolar
rhabdomyosarcoma and metastatic renal cell carcinoma (48). PAS is an important stain for the
diagnosis of ASPS, as ASPS possesses PAS-positive
diastase-resistant granules in >80% of cases (49). All the present cases were
PAS-positive. Immunohistochemical examination is also important for
differential diagnosis. The majority of ASPS tumour cells exhibit
moderate to strong nuclear staining of TFE3, which is a sensitive
and specific marker for ASPS. Monocarboxylate transporter protein 1
and its cellular chaperone protein CD147 also demonstrate positive
reactions in PAS-positive diastase-resistant cells. There are no
other specific markers for ASPS, which does not express the common
antigens of the epithelium (e.g. cytokeratin and EMA),
neuroendocrine cells (e.g. NSE, synaptophysin, chromogranin and
S-100 protein) or melanocytes (e.g. human melanoma black-45 and
melan A). However, certain markers are positive in the
aforementioned tumours, allowing for differential diagnosis. The
representative pathological features combined with supplementary
examinations, including immunohistochemical staining, PAS staining
and molecular biology technologies, are useful for the pathological
and differential diagnosis of ASPS.
Histogenesis of the tumour
The histogenesis of ASPS has been controversial for
a number of years. Genetic studies on ASPS have confirmed a
specific fusion gene involving the ASPS critical region-1 gene and
TFE3 and the resultant fusion protein generated by the unbalanced
chromosomal translocation [der(17)t(X:17)(p11;25)] (50). Therefore, it is generally accepted
that ASPS is a sarcoma associated with chromosomal translocation,
therefore it is sorted into a class containing uncertain
differentiated tumours.
It was hypothesized for a number of years that ASPS
represented an unusual form of myogenic tumour (51–53).
Subsequently, conflicting results on the expression of
muscle-associated markers have disproved this hypothesis (54,55).
Previously, genetic expression profiles of ASPS identified that
certain muscle-specific transcripts were increased, which suggests
an association with muscle cell progenitors (56). ASPS has a marked predilection to arise
on the thighs, buttocks and abdominal or chest walls, which
suggests that ASPS is associated with skeletal muscles or
musculofascial planes (37). The
present series and the cases reviewed revealed that orbital ASPS is
generally associated with the extraocular muscles. There were 19
and 9 patients in Tables II and
III respectively, whose tumours had
been mentioned definitely to be abutting, adhering to or
indistinguishable from the extraocular muscles. In the present
series, the tumours were clearly observed during the surgical
procedures. The tumours were revealed following longitudinally
splitting the thickened extraocular muscles in 3 cases, whereas the
tumours grew along with and were indistinguishable from the
extraocular muscles in 3 cases. There were 6 cases expressing
vimentin or desmin in the present series, which were identified
using immunohistochemistry. Although immunohistochemical
examination of muscle-associated markers in previous years did not
demonstrate myogenic histogenesis, the growth pattern of this
tumour suggests that orbital ASPS is associated with the
extraocular muscles.
Treatment
Generally, complete surgical excision of the
localized tumour with a microscopically negative margin is the
established treatment for ASPS. The possibility of recurrence is
rare if the lesion has been completely resected (57). The pathological status of surgical
margin, which indicates whether active tumour tissue remains, is
important for prognosis. Surgery is also the primary treatment in
orbital ASPS; however, due to the narrow space and complex
organization of the orbit, it is occasionally impossible to perform
a complete resection if the patient declines to undergo an
exenteration. Previous studies have demonstrated that chemotherapy
and radiotherapy do not improve the survival rate; however,
radiotherapy as an adjuvant therapy has been demonstrated to
decrease the risk of local recurrence (50,58).
Metastasectomy may markedly prolong the survival rate of patients
with pulmonary metastases of ASPS (16,37).
Prognosis
It has been reported that the biological behaviour
of ASPS is relatively indolent, with the 2-, 5-, 10- and 20-year
overall survival rates being 77, 60, 38 and 15%, respectively
(37). Metastases occur most commonly
in the lungs, brain and bones (37).
Since ~1/3 patients develop metastases to the lungs or brain
decades after initial diagnosis, long-term follow-up is strongly
advised for all cases of ASPS.
According to previous studies, the patient's age,
tumour size and presence of metastases at diagnosis are significant
prognostic factors in ASPS. It is hypothesized that younger age
with a tumour size of <5 cm and absence of metastases is
associated with a more favourable outcome (48,59). If
the tumour is resected completely, younger patients may achieve a
good prognosis with prolonged survival rates (40,60).
Certain studies have reported 100% survival rates beyond 5 years in
paediatric patients (38). However,
there was an exception in the present series: A 2-year-old patient
succumbed 1 year after diagnosis, possibly due to the large tumour
and withdrawal from therapy.
The prognosis is improved in patients with ASPS
located in the orbit and tongue, which is possibly associated with
smaller lesions, younger age at diagnosis and shorter course of
disease (16,40), which was also demonstrated in the
present review.
It is known that there are no histopathological
features predictive of prognosis in ASPS (48). However, in the present series, 2 cases
(cases 2 and 3) recurred shortly following surgery (<3 months).
Of these, 1 patient succumbed 1 year later and the other had an
invasion to the brain that was possibly fatal. It is notable that
the Ki-67 proliferation index was 15% in these 2 cases, whereas it
was ≤10% in 5 cases, suggesting that the Ki-67 proliferation index
may be associated with ASPS prognosis. Further study is required in
order to investigate this association.
In conclusion, orbital ASPS exhibits characteristics
that are distinct from those of ASPS arising in other locations.
Orbital ASPS usually affects a younger population, the course of
disease is shorter and the tumour size is smaller. Therefore, the
prognosis is improved in orbital ASPS. Orbital ASPS may have an
association with the extraocular muscles and the Ki-67
proliferation index may be associated with prognosis of ASPS.
Glossary
Abbreviations
Abbreviations:
|
ASPS
|
alveolar soft part sarcoma
|
|
CT
|
computed tomography
|
|
MRI
|
magnetic resonance imaging
|
|
PAS
|
periodic acid-Schiff
|
|
SMA
|
smooth muscle actin
|
|
TFE3
|
transcription factor for
immunoglobulin heavy-chain enhancer 3
|
|
EMA
|
epithelial membrane antigen
|
|
CEA
|
carcinoembryonic antigen
|
|
NSE
|
neuron-specific enolase
|
|
AFP
|
α-fetoprotein
|
References
|
1
|
Rose AM, Kabiru J and Rose GE: Alveolar
soft-part sarcoma of the orbit. Afr J Paediatr Surg. 8:82–84. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mulay K, Ali MJ, Honavar SG and Reddy VA:
Orbital alveolar soft-part sarcoma: Clinico-pathological profiles,
management and outcomes. J Cancer Res Ther. 10:294–298. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kim HJ, Wojno T, Grossniklaus HE and
Shehata BM: Alveolar soft-part sarcoma of the orbit: Report of 2
cases with review of the literature. Ophthal Plast Reconstr Surg.
29:e138–e142. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Majumdar K, Saran R, Tyagi I, Jain A,
Jagetia A, Sinha S and Singh A: Cytodiagnosis of alveolar soft part
sarcoma: Report of two cases with special emphasis on the first
orbital lesion diagnosed by aspiration cytology. J Cytol. 30:58–61.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Rekhi B, Ingle A, Agarwal M, Puri A,
Laskar S and Jambhekar NA: Alveolar soft part sarcoma ‘revisited’:
Clinicopathological review of 47 cases from a tertiary cancer
referral centre, including immunohistochemical expression of TFE3
in 22 cases and 21 other tumors. Pathology. 44:11–17. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Alkatan H, Al-Shedoukhy AA, Chaudhry IA
and Al-Ayoubi A: Orbital alveolar soft part sarcoma:
Histopathologic report of two cases. Saudi J Ophthalmol. 24:57–61.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Pang LJ, Chang B, Zou H, Qi Y, Jiang JF,
Li HA, Hu WH, Chen YZ, Liu CX, Zhang WJ and Li F: Alveolar soft
part sarcoma: A biomarker diagnostic strategy using TFE3
immunoassay and ASPL-TFE3 fusion transcripts in paraffin-embedded
tumor tissues. Diagn Mol Pathol. 17:245–252. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Morris WR, Padgett DM, Osborn FD and
Fleming JC: Pathologic quiz case: An orbital mass in a 45-year-old
woman. Alveolar soft part sarcoma. Arch Pathol Lab Med.
129:534–536. 2005.PubMed/NCBI
|
|
9
|
Kanhere HA, Pai PS, Neeli SI, Kantharia R,
Saoji RR and D'cruz AK: Alveolar soft part sarcoma of the head and
neck. Int J Oral Maxillofac Surg. 34:268–272. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kashyap S, Sen S, Sharma MC, Betharia SM
and Bajaj MS: Alveolar soft-part sarcoma of the orbit: Report of
three cases. Can J Ophthalmol. 39:552–556. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Khan AO and Burke MJ: Alveolar soft-part
sarcoma of the orbit. J Pediatr Ophthalmol Strabismus. 41:245–246.
2004.PubMed/NCBI
|
|
12
|
Chan WM, Liu DT, Lai CK, Tse MW, Ng JS and
Lam DS: Soft tissue sarcomas. Case 2. Orbital alveolar soft part
sarcoma in a child. J Clin Oncol. 22:2027–2029. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lasudry J and Heimann P: Cytogenetic
analysis of rare orbital tumors: Further evidence for diagnostic
implication. Orbit. 19:87–95. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Coupland SE, Heimann H, Hoffmeister B, Lee
WR, Foerster MH and Gross U: Immunohistochemical examination of an
orbital alveolar soft part sarcoma. Graefes Arch Clin Exp
Ophthalmol. 237:266–272. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Chodankar CM, Pandit SP, Joshi MG and
Deodhar KP: Alveolar soft-part sarcoma of the orbit (a case
report). Indian J Ophthalmol. 34:67–68. 1986.PubMed/NCBI
|
|
16
|
Font RL, Jurco S III and Zimmerman LE:
Alveolar soft-part sarcoma of the orbit: A clinicopathologic
analysis of seventeen cases and a review of the literature. Hum
Pathol. 13:569–579. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ishikura A, Kimura A and Yamamoto S: A
case of alveolar soft part sarcoma. Jpn J Cancer Clin.
25:6931979.
|
|
18
|
Mukherjee PK and Agrawal S: Alveolar soft
part sarcoma of the orbit. Indian J Ophthalmol. 27:15–17.
1979.PubMed/NCBI
|
|
19
|
Varghese S, Nair B and Joseph TA: Orbital
malignant non-chromaffin paraganglioma. Alveolar soft tissue
sarcoma. Br J Ophthalmol. 52:713–715. 1968. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Abrahams IW, Fenton RH and Vidone R:
Alveolar soft-part sarcoma of the orbit. Arch Ophthalmol.
79:185–188. 1968. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Altamirano-Dimas M and Albores-Saavedra J:
Alveolar soft part sarcoma of the orbit. Arch Ophthalmol.
75:496–499. 1966. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Nirankari MS, Greer CH and Chaddah MR:
Malignant non-chromaffin paraganglioma in the orbit. Br J
Ophthalmol. 47:357–363. 1963. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Cheng Y, Sha Y, Huang W, Hong R and Cai R:
CT and MRI features of orbital alveolar soft part sarcoma. Chin J
Radiol. 47:1147–1148. 2013.(In Chinese).
|
|
24
|
Du C and Wu F: A case report of orbital
alveolar soft part sarcoma and review of literatures. J ClinRadiol.
31:1814–1815. 2012.(In Chinese).
|
|
25
|
Feng N, Ma Z and Li C: Ultrasound features
of a case of right orbital alveolar soft part sarcoma. Chin J
Ultrasonogr. 19:6872010.(In Chinese).
|
|
26
|
Hu P, Zhou Z, Wang J, Peng W, Cheng Y, Zhu
L and Tang F: Radiological features and clinicopathological
findings of alveolar soft part sarcoma. Chin Oncol. 19:12–16.
2009.(In Chinese).
|
|
27
|
He W, Luo Q, Xia R and Yang G: Two cases
of orbital relapsing alveolar soft part sarcoma. Chin J Ophthalmol.
40:848–850. 2004.(In Chinese).
|
|
28
|
Dong G, Wang J and Xie D: A case of
intraorbital alveolar soft part sarcoma. Chin J Pract Ophthalmol.
22:3202004.(In Chinese).
|
|
29
|
Wang R and Wang W: A case of alveolar soft
part sarcoma in orbit, sphenoidal, frontal, ethmoid and maxillary
sinus. Chin Arch Otolaryngol Head Neck Surg. 10:2792003.(In
Chinese).
|
|
30
|
Dong X, Wang L and Yan Q: Intraorbital
alveolar soft part sarcoma. Chin J Diagnpathol. 3:1841996.(In
Chinese).
|
|
31
|
Xu D: A case report of orbital alveolar
soft part sarcoma. Guangdong Med J. 16:428–429. 1995.(In
Chinese).
|
|
32
|
Li M, Zhang D and Yan H: Primary orbital
alveolar soft part sarcoma. J Clin Ophthalmol. 1:123–124. 1993.(In
Chinese).
|
|
33
|
Liu F: A case of orbital alveolar soft
part sarcoma. Chin J Cancer. 4:3311989.(In Chinese).
|
|
34
|
Wei Y: A case of orbital alveolar soft
part sarcoma. Chin J Ophthalmol. 21:2521985.(In Chinese).
|
|
35
|
Huo J, Xiong Q, Ni K and Wang R:
Investigation of a case of orbital tumor. J Xinjiang Med
University. 1:3221982.(In Chinese).
|
|
36
|
Ni C: Observation of ultrastructure of
primary orbital alveolar soft part sarcoma. Chin J Ophthalmol.
17:5–7. 1981.(In Chinese).
|
|
37
|
Lieberman PH, Brennan MF, Kimmel M,
Erlandson RA, Garin-Chesa P and Flehinger BY: Alveolar soft-part
sarcoma. A clinico-pathologic study of half a century. Cancer.
63:1–13. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Casanova M, Ferrari A, Bisogno G,
Cecchetto G, Basso E, De Bernardi B, Indolfi P, Bellani F Fossati
and Carli M: Alveolar soft part sarcoma in children and
adolescents: A report from the soft-tissue sarcoma italian
cooperative group. Ann Oncol. 11:1445–1449. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Evans HL: Alveolar soft-part sarcoma. A
study of 13 typical examples and one with a histologically atypical
component. Cancer. 55:912–917. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Fanburg-Smith JC, Miettinen M, Folpe AL,
Weiss SW and Childers EL: Lingual alveolar soft part sarcoma; 14
cases: Novel clinical and morphological observations.
Histopathology. 45:526–537. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Ordóñez NG: Alveolar soft part sarcoma: A
review and update. Adv Anat Pathol. 6:125–139. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Pennacchioli E, Fiore M, Collini P,
Radaelli S, Dileo P, Stacchiotti S, Casali PG and Gronchi A:
Alveolar soft part sarcoma: Clinical presentation, treatment, and
outcome in a series of 33 patients at a single institution. Ann
Surg Oncol. 17:3229–3233. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Reis H, Hager T, Wohlschlaeger J, Bauer S,
Katenkamp K, Katenkamp D and Baba HA: Mammalian target of rapamycin
pathway activity in alveolar soft part sarcoma. Hum Pathol.
44:2266–2274. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Khanna P, Paidas CN and Gilbert-Barness E:
Alveolar soft part sarcoma: Clinical, histopathological, molecular,
and ultrastructural aspects. Fetal Pediatr Pathol. 27:31–40. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Viry F, Orbach D, Klijanienko J, Fréneaux
P, Pierron G, Michon J, Neuenschwander S and Brisse HJ: Alveolar
soft part sarcoma-radiologic patterns in children and adolescents.
Pediatr Radiol. 43:1174–1181. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Chen YD, Hsieh MS, Yao MS, Lin YH and Chan
WP: MRI of alveolar soft part sarcoma. Comput Med Imaging Graph.
30:479–482. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Chu WC, Howard RG, Roebuck DJ, Chik KW and
Li CK: Periorbital alveolar soft part sarcoma with radiologic
features mimicking haemangioma. Med Pediatr Oncol. 41:145–146.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Folpe AL and Deyrup AT: Alveolar soft-part
sarcoma: A review and update. J Clin Pathol. 59:1127–1132. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Enzinger FM and Weiss SW: Soft tissue
tumors. 3rd. St Louis: C. V. Mosby; pp. 1067–1074. 1995
|
|
50
|
Portera CA Jr, Ho V, Patel SR, Hunt KK,
Feig BW, Respondek PM, Yasko AW, Benjamin RS, Pollock RE and
Pisters PW: Alveolar soft part sarcoma: Clinical course and
patterns of metastasis in 70 patients treated at a single
institution. Cancer. 91:585–591. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Miettinen M and Ekfors T: Alveolar soft
part sarcoma. Immunohistochemical evidence for muscle cell
differentiation. Am J Clin Pathol. 93:32–38. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Rosai J, Dias P, Parham DM, Shapiro DN and
Houghton P: MyoD1 protein expression in alveolar soft part sarcoma
as confirmatory evidence of its skeletal muscle nature. Am J Surg
Pathol. 15:974–981. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Foschini MP and Eusebi V: Alveolar
soft-part sarcoma: A new type of rhabdomyosarcoma? Semin Diagn
Pathol. 11:58–68. 1994.PubMed/NCBI
|
|
54
|
Wang NP, Bacchi CE, Jiang JJ, McNutt MA
and Gown AM: Does alveolar soft-part sarcoma exhibit skeletal
muscle differentiation? An immunocytochemical and biochemical study
of myogenic regulatory protein expression. Mod Pathol. 9:496–506.
1996.PubMed/NCBI
|
|
55
|
Gómez JA, Amin MB, Ro JY, Linden MD, Lee
MW and Zarbo RJ: Immunohistochemical profile of myogenin and MyoD1
does not support skeletal muscle lineage in alveolar soft part
sarcoma. Arch Pathol Lab Med. 123:503–507. 1999.PubMed/NCBI
|
|
56
|
Stockwin LH, Vistica DT, Kenney S, Schrump
DS, Butcher DO, Raffeld M and Shoemaker RH: Gene expression
profiling of alveolar soft-part sarcoma (ASPS). BMC Cancer.
9:222009. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Kayton ML, Meyers P, Wexler LH, Gerald WL
and LaQuaglia MP: Clinical presentation, treatment, and outcome of
alveolar soft part sarcoma in children, adolescents, and young
adults. J Pediatr Surg. 41:187–193. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Sherman N, Vavilala M, Pollock R, Romsdahl
M and Jaffe N: Radiation therapy for alveolar soft-part sarcoma.
Med Pediatr Oncol. 22:380–383. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Jia Y, Wu D, Shang C, Yu J and Zhang KR:
Alveolar soft part sarcoma occurring on the abdominal wall of a
2-year-old child. J Pediatr Hematol Oncol. 33:e80–e82. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Pappo AS, Parham DM, Cain A, Luo X, Bowman
LC, Furman WL, Rao BN and Pratt CB: Alveolar soft part sarcoma in
children and adolescents: Clinical features and outcome of 11
patients. Med Pediatr Oncol. 26:81–84. 1996. View Article : Google Scholar : PubMed/NCBI
|