Introduction
Oral malignant tumors (OMTs) are typically squamous
cell carcinomas (SCC) or malignant melanomas; OMTs are treated by
the surgical resection of the tumor. The reconstruction of oral
cavity defects following OMT resection, including total glossectomy
(TG), poses a formidable challenge for the restoration of
postoperative oral function (1–12). The
decannulation of a tracheostomy tube or extubation of a
endotracheal tube, or restoration of oral intake function unaided
by a nasogastric or gastric tube, are representative indicators of
the restoration of postoperative oral function in patients that
underwent OMT resection with reconstruction (1–12).
Previously, we reported a significant correlation between the
likelihood of restoring oral intake function and reduced extents of
tongue base resection in an analysis based on 53 patients between
1993 and 2005 (1), and in 25 patients
that underwent segmental mandibulectomy (SM) with reconstruction to
treat mandibular bone defects between 2004 and 2011 (2). The postoperative functional outcomes for
patients in conditions including TG has been well studied (3–5).
The development of lung metastasis subsequent to the
treatment of OMT is associated with reduced overall survival time
(13). The association between
overall survival time with oral cavity defects, including TG, has
also been reported (6). However, to
the best of our knowledge, the association between lung metastasis
and oral cavity defects has not been investigated.
The present study investigated whether oral defects
following resection, including of the tongue base or mandibular
bone, are associated with decannulation, oral intake recovery and
survival, including lung metastasis-free survival, in patients that
underwent OMT resection with reconstruction.
Materials and methods
Patients
Between January 2013 and January 2016, 109 patients,
including 67 males and 33 females, with a histopathological
diagnosis of primary OMT underwent tumor resection with
reconstruction at the Department of Head and Neck Surgery, Aichi
Cancer Center Hospital (Nagoya, Japan). Of these patients, 4
underwent tumor resection with total laryngectomy; these patients
were excluded from the present study. Thus, a total of 105 patients
that underwent OMT resection with laryngeal preservation and
reconstruction were enrolled in the study. The study was approved
by the institutional review board and all patients provided
informed consent for the treatments and examinations.
Staging
The clinical staging of tumors was based on data
from routine physical examination, nasopharyngoscopy, enhanced
cervical computed tomography (CT) or magnetic resonance imaging,
and 18F-2-fluorodeoxyglucose positron emission tomography with CT.
The TNM classification was determined as per the International
Union Against Cancer criteria (seventh edition) (14).
Treatments
All patients underwent reconstruction with or
without laryngeal suspension following the en bloc resection of the
primary tumor, with or without neck dissection. Neck dissection was
not performed in cases of recurrent disease with a history of neck
dissection. For reconstruction, a total of 96 free flaps and 11
pedicled flaps were raised. In addition, two patients had
reconstructions featuring 2 flaps; the first patient underwent
reconstruction with a rectus abdominus myocutaneous free flap and a
pectoralis major musculocutaneous pedicled flap, and the second
underwent reconstruction with a recutus abdominus myochutaneous
free flap and a deltopectoral pedicled flap. Laryngeal suspension
was performed in accordance with two criteria: i) The excision of
the bilateral suprahyoid muscles, and ii) the presence of ≥50 % of
the tongue base, as described previously (1). With respect to airway management during
surgery, 100 patients underwent tracheostomy due to postoperative
bleeding, whereas 5 patients did not require tracheostomy. A
nasogastric tube was inserted into all patients to allow tube
feeding. Postoperative rehabilitation for the purpose of
decannulation and the restoration of oral intake was assisted by a
speech-language pathologist and nurses, as previously described
(1). A total of 26 patients underwent
postoperative radiotherapy, with or without platinum-based
chemotherapy, due to the presence of a positive surgical margin,
multiple lymph node metastases or extranodal tumor spread. The
remaining methods for postoperative treatment and follow-up
protocols have been previously described (14).
Defects due to tumor resection
The extent of three anatomical defects, including
the tongue base, mobile tongue and mandible bone, due to tumor
resection was classified with Urken's classification, as previously
described (2,7). Bone defects resulting from SM were
described with combinations of the letter C (condyle), R (ramus), B
(bony) and S (symphysis) (2,7), and the number of defects was numbered
0–5 based on the number of sections removed.
Clinical parameters
The following clinical parameters were extracted
from the medical records of the patients: Age, sex, clinical T and
N classification, clinical stage, tumor site (tongue or other),
pathological diagnosis (SCC or other), recurrence status, history
of radiotherapy and surgery, induction chemotherapy, extent of
mobile tongue resection, extent of tongue base resection, section
of SM (section 0/1-5), skin resection, lateral pharynx resection
and laryngeal suspension status, type of neck dissection
(unilateral or bilateral), reconstruction flap (free or pedicle),
tracheostomy indication, smoking and alcohol consumption status,
Charlson comorbidity index (CCI; a weighted index based on 19
comorbid conditions) (15), body mass
index, American Society of Anesthesiologists (ASA) score (16), % vital capacity, forced expiratory
rate per 1 sec (FEV1%), forced expiratory volume per 1 sec (FEV1.0)
and postoperative radiotherapy status.
Statistical analysis
Statistical analysis was performed using the JMP
software package (version 9; SAS Institute, Cary, NC, USA). The
associations between tracheostomy indication (presence/absence) and
clinical parameters were assessed using a Mann-Whiney U or
χ2 test. Applying the method described previously
(1), the proportion of patients that
achieved decannulation and the restoration of unaided oral intake
following surgery was calculated by the Kaplan Meier method; the
duration was defined as the period from surgery to the target
event, or until the date of last contact. The target events were:
Free of tracheostomy tube, or extubation of endotracheal tube, for
decannulation; free of tube feeding, including nasogastric or
gastric tube, for oral intake recovery. Oral intake was defined as
the ability to intake a limited diet, e.g., soft diet, without tube
feeding. Applying a modified version of a previous method (14,15),
various cutoff values for decannulation following resection by SM
and tongue base resection were tested by univariate survival
analysis, performed using Cox's proportional model. A multivariate
analysis was performed to assess the clinical parameters associated
with decannulation and oral intake recovery. The associations of
the high (SM of 4–5 sections and/or TG) and low risk (SM of 0–3
sections and no TG) groups with clinical parameters was assessed
using a Mann Whitney U or χ2 test. A multivariate
analysis adjusted for clinical stage (IV/I–III), past history of or
postoperative radiotherapy (yes/no) and age (per 1 year) was
performed to investigate the factors associated with both
decannulation and oral intake recovery. Differences between groups
in overall, local recurrence-free, regional recurrence-free,
distant metastasis-free, and lung metastasis-free survival time
were assessed by a Wilcoxon test (14). The associations between decannulation,
oral intake recovery and lung metastasis were assessed using a
χ2 test. P<0.05 was considered to indicate a
statistically significant difference.
Results
Patient characteristics
The clinical characteristics of the patients are
listed in Table I.
 | Table I.Clinical parameters. |
Table I.
Clinical parameters.
| A, Associations
between patient characteristics with tracheostomy indications and
resection risk, as determined with the Mann-Whitney U test |
|---|
|
|---|
|
|
| Tracheostomy
indication |
| Resection group |
|
|---|
|
|
|
|
|
|
|
|---|
| Parameter | Total, n | Presence | Absence | P-value | High risk | Low risk | P-value |
|---|
| Sex |
|
|
| 0.34 |
|
| 0.77 |
| Male | 69 | 67 | 2 |
| 10 | 59 |
|
|
Female | 36 | 33 | 3 |
| 6 | 30 |
|
| T stage |
|
|
| 0.18 |
|
| 0.03 |
| T1 | 2 | 2 | 0 |
| 2 | 36 |
|
| T2 | 27 | 24 | 3 |
|
|
|
|
| T3 | 9 | 8 | 1 |
|
|
|
|
| T4 | 67 | 66 | 1 |
| 14 | 53 |
|
| N stage |
|
|
| 0.64 |
|
| 0.34 |
| N0 | 51 | 47 | 4 |
| 6 | 45 |
|
| N1 | 12 | 12 | 0 |
| 10 | 44 |
|
|
N2a/b | 25 | 24 | 1 |
|
|
|
|
| N2c | 16 | 16 | 0 |
|
|
|
|
| N3 | 1 | 1 | 0 |
|
|
|
|
| Clinical stage |
|
|
| 0.044 |
|
| 0.10 |
| I | 1 | 1 | 0 |
| 2 | 26 |
|
| II | 20 | 17 | 3 |
|
|
|
|
| III | 7 | 6 | 1 |
|
|
|
|
| IV | 77 | 76 | 1 |
| 14 | 63 |
|
| Tumor site |
|
|
| 1.00 |
|
| 0.86 |
|
Tongue | 48 | 46 | 2 |
| 7 | 41 |
|
|
Other | 57 | 54 | 3 |
| 9 | 48 |
|
| Pathological
diagnosis |
|
|
| 1.00 |
|
| 1.00 |
|
Squamous cell carcinoma | 95 | 90 | 5 |
| 15 | 80 |
|
|
Other | 10 | 10 | 0 |
| 1 | 9 |
|
| Recurrence
status |
|
|
| 0.18 |
|
| 0.77 |
|
New | 72 | 70 | 2 |
| 12 | 29 |
|
|
Recurrence | 33 | 30 | 3 |
| 4 | 60 |
|
| Radiotherapy |
|
|
| 0.28 |
|
| 0.81 |
|
Yes | 22 | 20 | 2 |
| 3 | 19 |
|
| No | 83 | 80 | 3 |
| 13 | 70 |
|
| Surgery |
|
|
| 0.12 |
|
| 0.55 |
|
Yes | 28 | 25 | 3 |
| 3 | 25 |
|
| No | 77 | 75 | 2 |
| 13 | 64 |
|
| Induction
chemotherapy |
|
|
| 0.16 |
|
| 0.06 |
|
Yes | 37 | 37 | 0 |
| 9 | 28 |
|
| No | 68 | 63 | 5 |
| 7 | 61 |
|
| Mobile tongue
resection |
|
|
| 0.22 |
|
| <0.01 |
|
None | 43 | 39 | 4 |
| 1 | 42 |
|
|
1/4 | 8 | 7 | 1 |
| 15 | 47 |
|
|
1/2 | 15 | 15 | 0 |
|
|
|
|
|
3/4 | 17 | 17 | 0 |
|
|
|
|
|
Total | 22 | 22 | 0 |
|
|
|
|
| Tongue base
resection |
|
|
| 0.54 |
| N/A |
|
|
None | 66 | 61 | 5 |
|
|
|
|
|
1/4 | 11 | 11 | 0 |
|
|
|
|
|
1/2 | 12 | 12 | 0 |
|
|
|
|
|
3/4 | 10 | 10 | 0 |
|
|
|
|
| Total
glossectomy | 6 | 6 | 0 |
|
|
|
|
| Sections of
segmental mandibulectomy |
|
|
| 0.05 |
| N/A |
|
| 0 | 63 | 61 | 3 |
|
|
|
|
| 1 | 2 | 1 | 1 |
|
|
|
|
| 2 | 19 | 19 | 0 |
|
|
|
|
| 3 | 11 | 10 | 1 |
|
|
|
|
| 4 | 6 | 6 | 0 |
|
|
|
|
| 5 | 4 | 4 | 0 |
|
|
|
|
| Skin resection |
|
|
| 1.00 |
|
| <0.01 |
|
Yes | 19 | 18 | 1 |
| 7 | 12 |
|
| No | 86 | 82 | 4 |
| 9 | 77 |
|
| Lateral pharynx
resection |
|
|
| 0.32 |
|
| 0.77 |
|
Yes | 32 | 32 | 0 |
| 4 | 28 |
|
| No | 73 | 68 | 5 |
| 12 | 61 |
|
| Laryngeal
suspension |
|
|
| 0.08 |
|
| <0.01 |
|
Yes | 43 | 43 | 0 |
| 16 | 17 |
|
| No | 62 | 57 | 5 |
| 0 | 62 |
|
| Type of neck
dissection |
|
|
| 0.19 |
|
| 0.14 |
|
None | 11 | 10 | 1 |
| 0 | 11 |
|
|
Unilateral | 54 | 50 | 4 |
|
|
|
|
|
Bilateral | 40 | 40 | 0 |
| 16 | 78 |
|
| Reconstruction
flap |
|
|
| <0.01 |
|
| 0.60 |
|
Free | 97 | 95 | 2 |
| 16 | 81 |
|
|
Pedicle | 8 | 5 | 3 |
| 0 | 8 |
|
| Tracheostomy
indication |
| N/A |
|
|
|
| 1.00 |
|
Yes | 100 |
|
|
| 16 | 84 |
|
| No | 5 |
|
|
| 0 | 5 |
|
| Smoking |
|
|
| 0.07 |
|
| 0.28 |
|
Smoker | 65 | 64 | 1 |
| 12 | 53 |
|
|
Non-smoker | 40 | 36 | 4 |
| 4 | 36 |
|
| Alcohol |
|
|
| 0.17 |
|
| 0.24 |
|
Drinker | 58 | 57 | 1 |
| 11 | 47 |
|
|
Non-drinker | 47 | 43 | 4 |
| 5 | 42 |
|
| History of or
postoperative radiotherapy |
|
|
| 1.00 |
|
| 0.10 |
|
Yes | 46 | 44 | 2 |
| 10 | 36 |
|
| No | 59 | 56 | 3 |
| 6 | 53 |
|
|
| B, Associations
between patient characteristics (as mean ± standard deviation) with
tracheostomy indications and resection risk, as determined with the
χ2 test |
|
|
|
| Tracheostomy
indication |
| Resection
group |
|
|
|
|
|
|
|
|
|
Parameter | All
patients |
Presence | Absence | P-value | High
risk | Low
risk | P-value |
|
| Age | 57.3±16.6 | 57.2±16.8 | 59.0±12.4 | 0.98 | 57.1±21.4 | 57.3±15.7 | 0.57 |
| Charlson
comorbidity index | 1.37±1.61 | 1.38±1.64 | 1.20±0.84 | 0.80 | 1.38±1.36 | 1.37±1.65 | 0.78 |
| Body mass index
(kg/m2) | 20.8±3.36 | 20.9±3.31 | 18.3±3.42 | 0.12 | 19.8±3.30 | 21.0±3.35 | 0.10 |
| ASA-PS | 1.63±0.52 | 1.64±0.52 | 1.40±0.55 | 0.32 | 1.88±0.34 | 1.58±0.54 | 0.03 |
| Vital capacity
(%) | 102.9±80.3 | 103.2±82.2 | 97.6±18.3 | 0.79 | 95.3±11.9 | 104.2±86.6 | 0.82 |
| FEV1% (%) | 81.7±8.69 | 81.1±8.84 | 79.2±4.67 | 0.32 | 79.6±9.39 | 82.0±8.57 | 0.26 |
| FEV1.0 (l) | 2.61±0.82 | 2.63±0.82 | 2.30±0.81 | 0.39 | 2.50±0.78 | 2.63±0.83 | 0.60 |
Sites of the primary tumor were as follows: Tongue,
48; lower gum, 35; cheek mucosa, 9; floor of mouth, 7; upper gum,
3; mandible bone, 2; lip, 1. Histological classifications of the
primary tumors were as follows: SCC, 95; malignant melanoma, 3;
osteosarcoma, 2; undifferentiated sarcoma, 2; adenoid cystic
carcinoma, 1; adenocarcinoma (not otherwise specified), 1;
rhabdomyosarcoma, 1.
Tongue base defects were as follows: None, 66;
one-quarter of tongue base, 11; one-half of tongue base, 12;
three-quarters of tongue base, 10; TG, 6. Mobile tongue defects
were as follows: None, 43; one-quarter of mobile tongue, 8;
one-half of tongue base, 15; three-quarters of mobile tongue, 17;
total mobile tongue resection, 4.
A total of 42 patients had bone defects from SM, as
follows: B, 2; RB, 18; BS, 1; CRB, 2; RBS, 9; RBSB, 6; RBSBR, 4.
Patients were grouped by the extent of the bone defect as follows:
0 sections (i.e., no SM, n=63), 1 section (n=2; B, 2), 2 sections
(n=19; RB, 18; BS, 1), 3 sections (n=11; CRB, 2; RBS, 9), 4
sections (n=6; RBSB, 6), 5 sections (n=4; RBSBR, 4).
Tracheostomy and follow-up
Indications for tracheostomy were present in 95.2%
(100/105) of the study population. The association between clinical
parameters and tracheostomy indication is described in Table I. Positive indication for tracheostomy
was significantly associated with a higher clinical stage
(P<0.05) and free flap reconstruction (P<0.01). In the entire
study population, 93 (88.6%) and 84 (80%) were able to achieve
decannulation and oral intake, respectively. The mean ± standard
deviation (SD) durations of follow-up for the entire study
population, for the 78 (74.3%) surviving patients and for the 27
(25.7%) deceased patients were 486±300, 526±313 and 369±225 days,
respectively.
Decannulation and oral intake recovery
by Cox's proportional hazards model
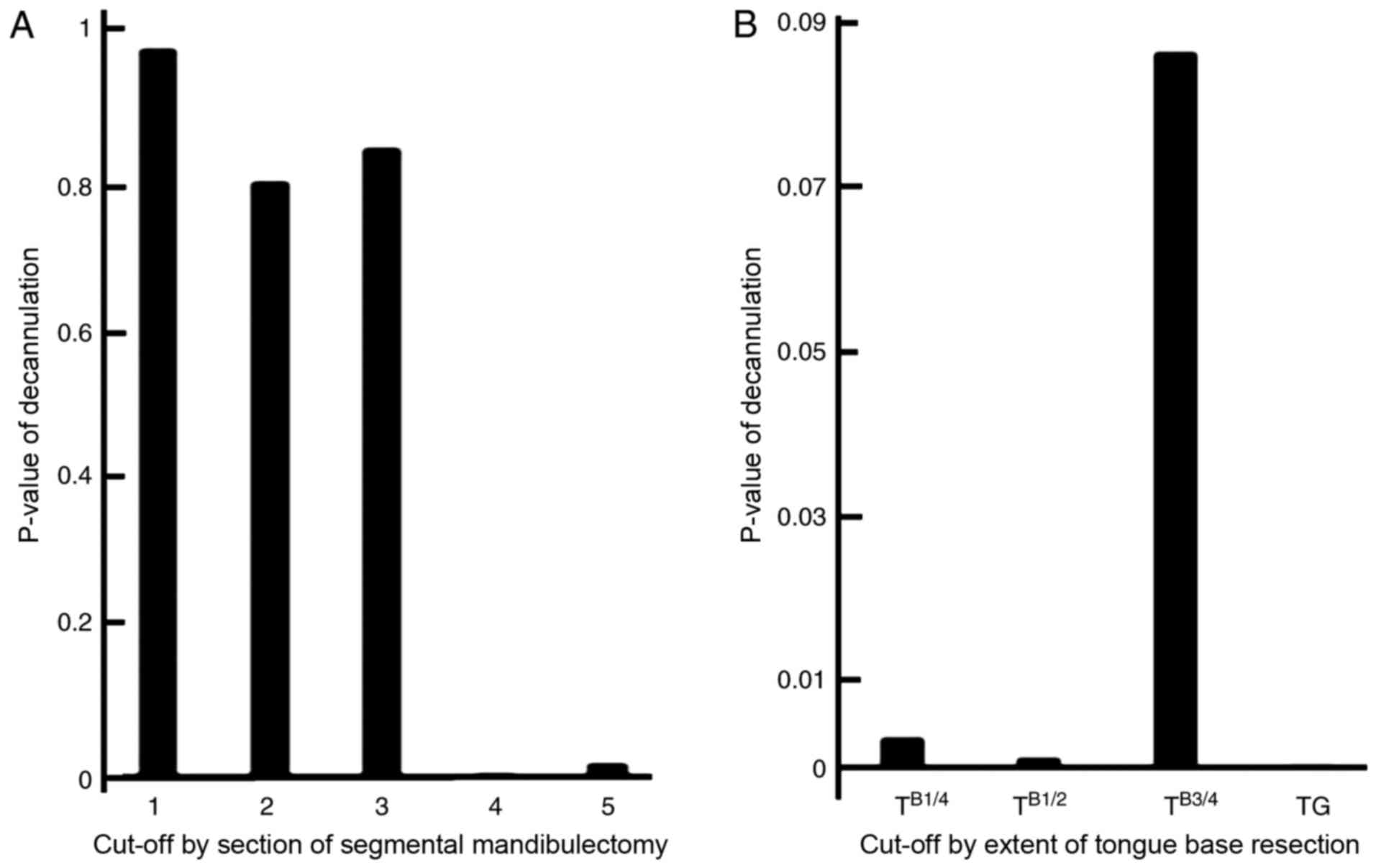
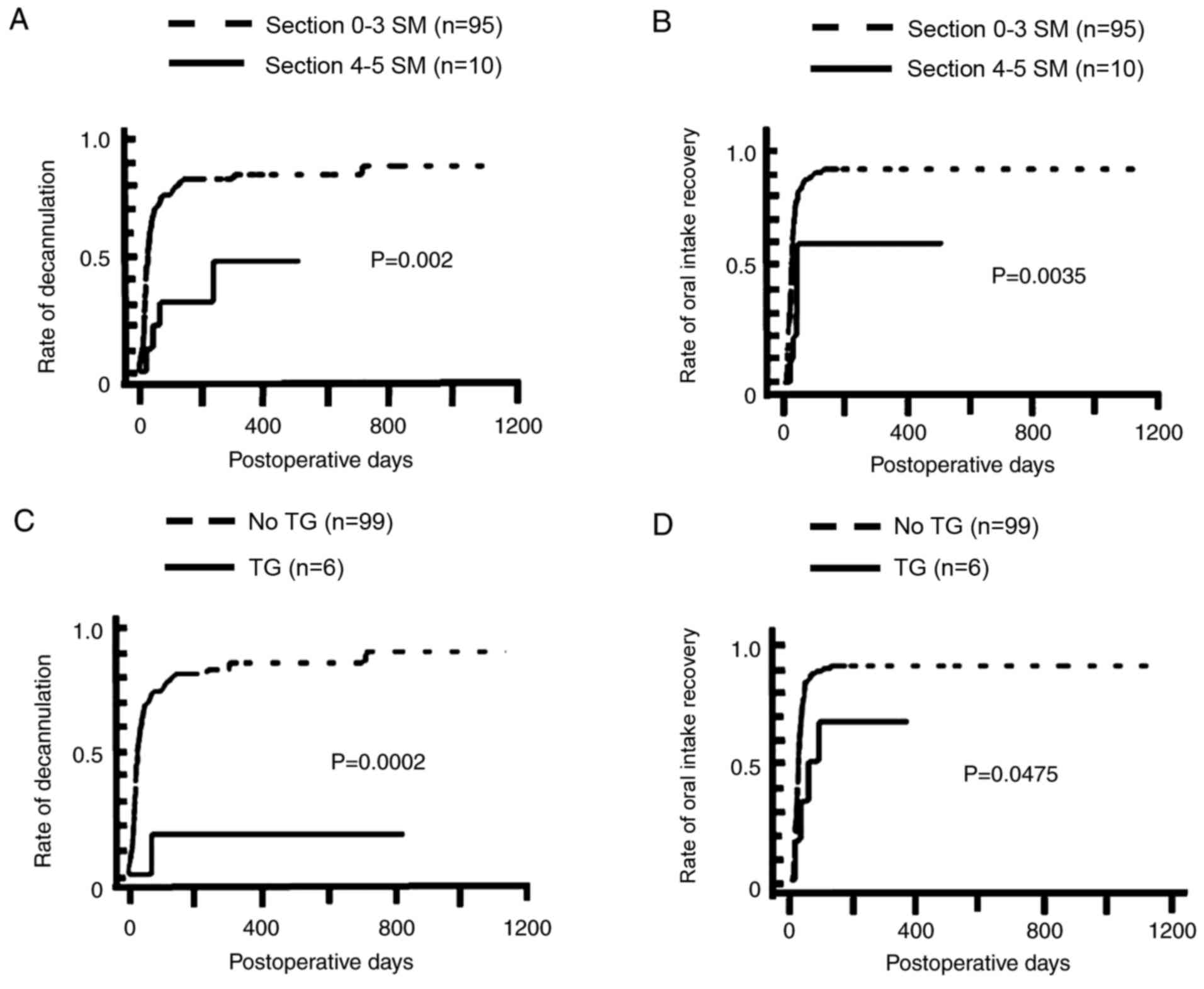
P-value and various cutoff values of decannulation
for the extent of SM and tongue base resection, tested in a
univariate analysis using Cox's proportional hazards model, are
included in Fig. 1. Based on a
univariate analysis, 4–5 section SM (n=10) was significantly
associated with a lower rate of decannulation (P<0.01) and the
recovery of oral intake (P<0.01). Furthermore TG (n=6) was
significantly associated with a lower rate of decannulation
(P<0.001) and oral intake recovery (P<0.05; Fig. 2). Of the 6 patients that underwent TG,
1 (16.7%) and 4 (66.7%) patients were able to achieve decannulation
and oral intake, respectively. Of the 10 patients that underwent SM
(4–5 sections), 4 (40.0%) and 6 (60.0%) patients were able to
achieve decannulation and oral intake, respectively. The results of
multivariate analysis, subsequent to adjusting for the extent of SM
(0–3 vs. 4–5 sections of SM) and tongue base resection (non-TG vs.
TG), are included in Table II. The
SM of 4–5 sections was significantly associated with a lower rate
of decannulation (P<0.02) and oral intake recovery (P<0.01);
TG was significantly associated with a lower rate of decannulation
(P<0.01) and oral intake recovery (P<0.01).
 | Table II.Multivariate analysis adjusted for
tongue base resection and segmental mandibulectomy. |
Table II.
Multivariate analysis adjusted for
tongue base resection and segmental mandibulectomy.
|
| Oral intake
recovery | Decannulation |
|---|
|
|
|
|
|---|
| Parameter | HR | 95% CI | P-value | HR | 95% CI | P-value |
|---|
| Tongue base
resection, TG vs. non-TG | 0.35 | 0.11–0.85 | 0.018 | 0.08 | 0.004–0.34 | <0.01 |
| Sections of
segmental mandibulectomy, 4–5 vs. 0–3 | 0.32 | 0.12–0.67 | <0.01 | 0.23 | 0.07–0.56 | <0.01 |
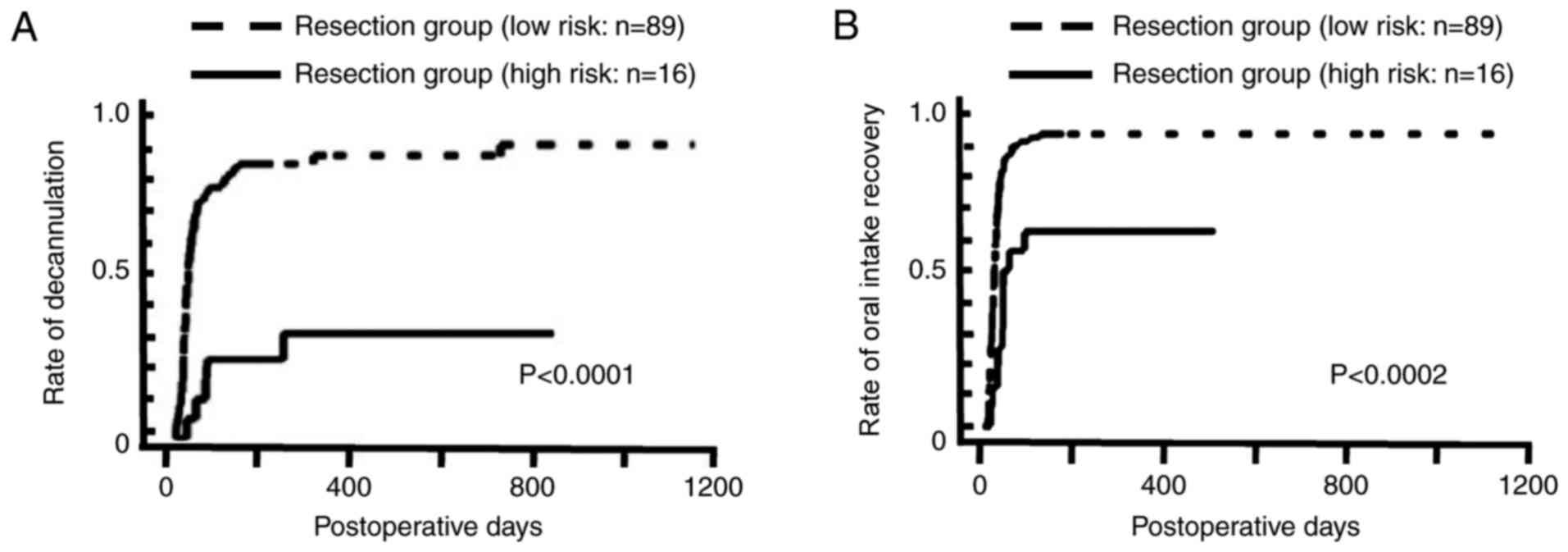
High and low risk groups
The patients were divided into high (4–5 sections SM
and/or TG, n=16) and low risk (0–3 sections SM and no TG, n=89)
groups. From the high risk group, 5 (31.3%) and 10 (62.5%) patients
were able to achieve decannulation and unaided oral intake,
respectively. In the low risk group, 79 (88.8%) and 83 (93.3%)
achieved decannulation and oral intake, respectively. For the 5
patients in the high risk group that achieved decannulation, the
mean ± SD period from the initial surgery to decannulation was
87.2±84.71 days. For the 79 patients in the low risk group that
achieved decannulation, the mean ± SD period from the initial
operation to decannulation was 43.73±86.51 days. Patients in the
high risk group had a significantly lower rate of decannulation
(P<0.0001) and oral intake recovery (P<0.0002) in the
univariate analysis (Fig. 3). The
association between the clinical parameters with the two groups
(high and low risk) are included in Table
I. Patients in the low risk group were less likely to have
undergone mobile tongue resection (P<0.01), skin resection
(P<0.01) or laryngeal suspension (P<0.01) than those in the
high risk group.
Multivariate analysis for
decannulation and oral intake recovery
The results of the multivariate analysis for
decannulation and oral intake recovery, performed subsequent to
adjusting for clinical stage (IV/I–III), past history of or
postoperative radiotherapy (yes/no) and age (per 1 year), is
included in Table III. The high
risk group exhibited a significantly lower rate of decannulation
(P<0.01) and oral intake recovery (P<0.01). Patients with a
history of radiotherapy or postoperative radiotherapy were less
likely to recover oral intake (P<0.03).
 | Table III.Multivariate analysis adjusted for
resection group, clinical stage, radiotherapy status and age. |
Table III.
Multivariate analysis adjusted for
resection group, clinical stage, radiotherapy status and age.
|
| Decannulation | Oral intake
recovery |
|---|
|
|
|
|
|---|
| Parameter | HR | 95% CI | P-value | HR | 95% CI | P-value |
|---|
| Resection group,
high vs. low risk | 0.17 | 0.06–0.38 | <0.01 | 0.37 | 0.18–0.68 | <0.01 |
| Clinical stage, IV
vs. I–III | 0.61 | 0.38–1.01 | 0.05 | 0.81 | 0.52–1.33 | 0.40 |
| Past history or
postoperative radiotherapy, yes/no | 0.67 | 0.42–1.05 | 0.08 | 0.60 | 0.39–0.93 | 0.022 |
| Age per 1 year | 0.99 | 0.98–1.00 | 0.14 | 0.99 | 0.98–1.00 | 0.05 |
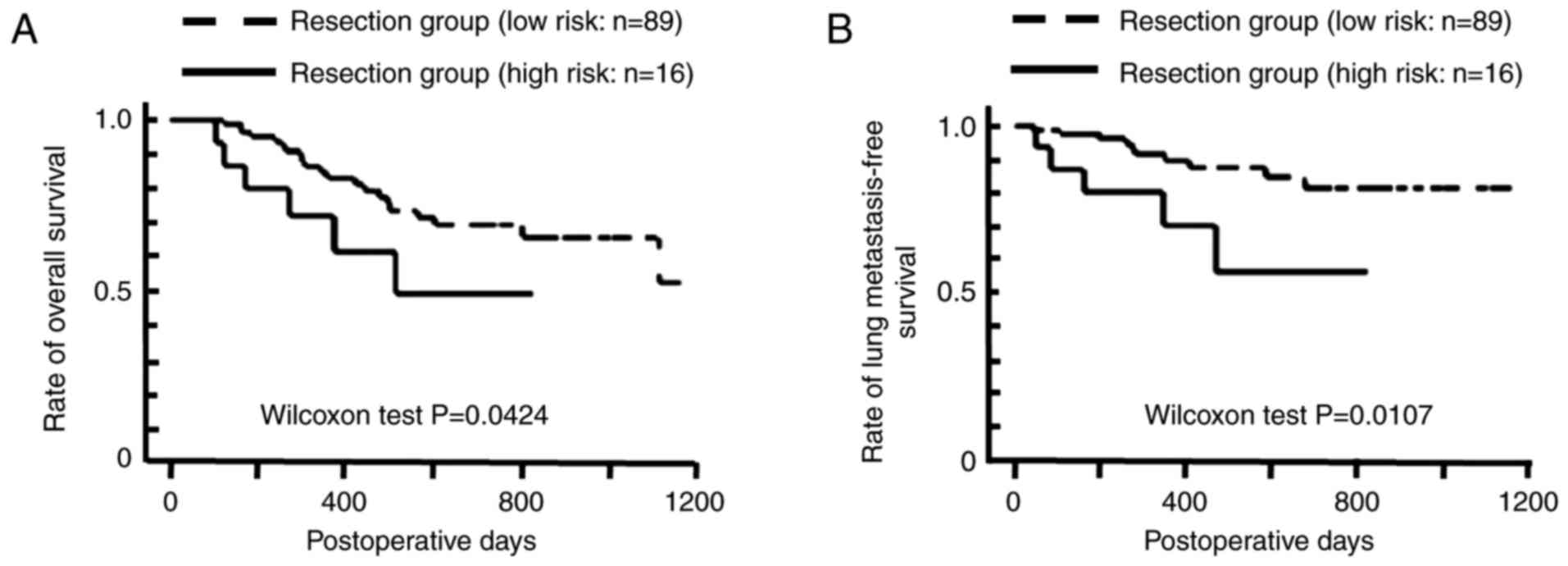
Survival
A total of 10 patients were diagnosed with lung
metastasis by imaging, and 5 by pathological analysis. Patients in
the high risk groups exhibited significantly shorter overall
(P<0.05) and lung metastasis-free (P<0.02) survival time than
the low risk groups. However, patients in the high risk group did
not exhibit a significant difference in local recurrence free
(P=0.78), regional recurrence free (P=0.94) or distant metastasis
free (P=0.0515) survival time. The Kaplan Meier curves for the
overall and lung-metastasis free survival times are included in
Fig. 4. A significant association was
observed between decannulation and oral intake recovery
(P<0.01); however, lung metastasis was not significantly
associated with decannulation (P=0.17) or oral intake recovery
(P=0.37).
Discussion
In the present study, it was demonstrated for the
first time that patients that underwent OMT resection (SM of 4–5
sections or TG) had a significantly lower rate of decannulation
(P<0.0001) and oral intake recovery (P<0.0002), as well as
shorter overall (P<0.05) and lung metastasis-free (P<0.02)
survival time.
Results of a national survey in the United Kingdom
revealed that 69% of clinical units performed tracheostomy
‘usually’ or ‘almost always’ following free flap surgery (8). Lee et al (9) reported in 2015 that tracheostomy is
commonly performed to secure the airway after oral cancer resection
with reconstruction. The data from the present study, that 95.2% of
the patients had an indication for tracheostomy, is consistent with
those reports (8,9).
Additionally, consistent with the previous reports
of associations between functional outcomes and TG (3,4), TG was
significantly associated with a lower rate of decannulation in the
105 patients that underwent head and neck cancer resection with
larynx preservation and reconstruction (3), and the functional outcomes, including
oral intake recovery following subtotal glossectomy, were superior
compared with TG in a review of TG without laryngectomy (4). All these findings indicate that there is
an association of TG with a lower rate of decannulation and oral
intake recovery (3,4).
A total of 6 of the 7 patients that underwent
reconstruction following large composite resection with
hemimandibulectomy remained dependent on tube-feeding, which is
also consistent with a previous report of functional outcomes
subsequent to SM (10). Additionally,
the observation from the present study of a significant association
between the SM of 4–5 sections and a lower rate of oral intake
recovery is consistent with the previous study (10).
The lack of uniformity in measurements of oral
function subsequent to head and neck surgery with reconstruction
has been discussed in several reviews (11,12).
Therefore, the present study functionally measured oral intake and
decannulation using the Kaplan-Meier method, and assessed the
association using Cox's proportional hazards model, in subjects
that underwent OMT resection, as described in a previous study in
which oral intake was functionally measured in subjects that
underwent tongue base resection (1).
Patients that undergo TG or the SM of 4–5 sections
exhibit poor overall survival time (6,10). The
present study, in addition to previous studies, reports a direct
association between lung metastasis and shorter overall survival
time in patients with OMT (13,14). We
hypothesized that the association of TG or 4–5 sections of SM with
reduced survival time may be associated with lung metastases, as
the lung is the most common site for distant metastasis in OMT
(14). Accordingly, in the present
study, patients with TG or 4–5 sections of SM exhibited a
significantly shorter overall and lung metastasis free survival
time. Thus, TG or 4–5 sections of SM may be a novel prognostic
marker for lung metastasis in OMT. In addition, the results of the
present study suggested that offering OMT resection with
laryngectomy to patients undergoing 4–5 section SM or TG with
reconstruction may be advisable; patients from the high risk group
exhibited a significantly decreased rate of decannulation and oral
intake recovery compared with that exhibited by those from the low
risk group (0–3 sections SM and no TG).
The small number of subjects and the retrospective
design are key limitations of the present study. Future studies
with increased sample sizes may provide more robust results.
In conclusion, the present study demonstrated for
the first time that high risk patients (SM of 4–5 sections or TG)
undergoing OMT resection with reconstruction exhibit a
significantly lower rate of decannulation (P<0.0001) and oral
intake recovery (P<0.0002), in addition to shorter reduced
overall (P<0.05) and lung metastasis-free (P<0.02) survival
time, when compared with low risk patients (SM of 0–3 sections and
no TG). These results suggest that TG or 4–5 section SM are
prognostic parameters for both functional and survival outcomes,
including lung metastasis, for individuals with OMT.
Acknowledgements
The present study was supported by JSPS KAKENHI
(grant no. 16K11253).
References
|
1
|
Fujimoto Y, Hasegawa Y, Yamana H, Ando A
and Nakashima T: Swallowing function following extensive resection
of oral or oropharyngeal cancer with laryngeal suspension and
cricopharyngeal myotomy. Laryngoscope. 117:1343–1348. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mizukami T, Hyodo I, Fukamizu H and Mineta
H: Reconstruction of lateral mandibular defect: A comparison of
functional and aesthetic outcomes of bony reconstruction vs soft
tissue reconstruction long-term follow-up. Acta Otolaryngol.
133:1304–1310. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Isaac A, Zhang H, Varshney S, Hamilton S,
Harris JR, O'Connell DA, Biron VL and Sekaly H: Predictors of
Failed and Delayed Decannulation after Head and Neck Surgery.
Otolaryngol Head Neck Surg. 155:437–442. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Rigby MH and Hayden RE: Total glossectomy
without laryngectomy-a review of functional outcomes and
reconstructive principles. Curr Opin Otolaryngol Head Neck Surg.
22:414–448. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Dziegielewski PT, Ho ML, Rieger J, Singh
P, Landgille M, Harris JR and Seikaly H: Total glossectomy with
laryngeal preservation and free flap reconstruction: Objective
functional outcomes and systemic review of the literature.
Laryngoscope. 123:140–145. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chang EI, Yu P, Skoracki RJ, Liu J and
Hanasono MM: Comprehensive analysis of functional outcomes and
survival after microvascular reconstruction of glossectomy defects.
Ann Surg Oncol. 22:3061–3069. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Urken ML, Weinberg H, Vickery C,
Bunchbinder D, Lawson W and Biller HF: Oromandibular reconstruction
using microvascular composite free flaps. Report of 71 cases and a
new classification scheme for bony, soft-tissue, and neurologic
defects. Arch Otolaryngol Head Neck Surg. 117:733–744. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Marsh M, Elliott S, Anand R and Brennan
PA: Early postoperative care for free flap head & neck
reconstructive surgery a national survey of practice. Br J Oral
maxillofac Surg. 47:182–185. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lee HJ, Kim JW, Choi SY, Kim CS, Kwon TG
and Paeng JY: The evaluation of a scoring system in airway
management after oral cancer surgery. Maxillofac Plast Reconstr
Surg. 37:192015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Butler CE and Lewin JS: Reconstruction of
large composite oromandibulomaxillary defects with free vertical
recuts abdominis myocutaneous flaps. Plast Reconstr Surg.
113:499–507. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kreeft AM, van der Molen L, Hilgers FJ and
Baim AJ: Speech and swallowing after surgical treatment of advanced
oral and oropharyngeal carcinoma: A systematic review of the
literature. Eur Arch Otorhinolaryngol. 266:1687–1698. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Rathod S, Livergant J, Klein J, Witterick
I and Ringash J: A systemic review of quality life in head neck
cancer treated with surgery with without adjuvant treatement. Oral
Oncol. 51:888–900. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Shiiba M, Unozawa M, Higo M, Kouzu Y,
Kasamatsu A, Sakamoto Y, Ogawara K, Uzawa K, Takiguchi Y and
Tanzawa H: Controlling distant metastasis and surgical treatment
are crucial for improving clinical outcome in uncommon head and
neck malignancies, such as non-squamous carcinoma. Mol Clin Oncol.
2:609–617. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Suzuki H, Beppu S, Hanai N, Hirakawa H and
Hasegawa Y: Lymph node density predicts lung metastasis in oral
squamous cell carcinoma. Br J Oral Maxillofac Surg. 54:213–218.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Suzuki H, Hanai N, Nishikawa D, Fukuda Y,
Koide Y, Kodaira T, Tachibana H, Tomita N, Makita C and Hasegawa Y:
The Charlson comorbidity index is a prognostic factor in sinonasal
tract squamous cell carcinoma. Jpn J Clin Oncol. 46:646–651. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Coskunfirat OK, Chen HC, Spanio S and Tang
YB: The safety of microvascular free tissue transfer in the elderly
population. Plast Reconstr Surg. 115:771–775. 2005. View Article : Google Scholar : PubMed/NCBI
|