Introduction
Third molar extractions are one of the most common
and basic outpatient interventions in oral and maxillofacial
surgery (1). With the continuous
development of medical technologies and research on new devices,
minimally-invasive tooth extraction has been widely applied.
Simplified procedures and shorter surgery relieve pain and reduce
complications. However, patients still suffer some pain, swelling,
limitation in mouth mobility, and other symptoms after surgery
(2,3).
Hematological tumors are common malignant tumors, including various
leukemias, malignant lymphomas, and multiple myeloma. The main
treatment for these tumors is chemotherapy, which causes
immunosuppression and reduced immunity. Dental treatment for
patients with hematological tumors should be conducted during
chemotherapy to reduce the probability of infections. This can
effectively prevent the incidence of various complications that can
negatively impact the quality of life (4,5). Reducing
dental malaise and postoperative complications is a critical issue
for oral and maxillofacial surgery doctors. Bromelain is the
generic term for a series of proteases found in the fruit and stem
of pineapples. Bromelain has anti-inflammatory properties and can
promote wound healing (6). Oral
administration of bromelain during the perioperative period for
third molar extractions can effectively improve quality of life
(7). Herein, we present research
conducted on the administration of bromelain during third molar
extraction in chemotherapy patients with hematological tumors. We
report good efficacy for bromelain in reducing pain and preventing
postoperative complications.
Materials and methods
Patient data
We recruited 72 patients with hematological tumors
accompanied by mandibular-impacted third molar who met the standard
hemogram from January 2015 to December 2015. Inclusion criteria:
diagnosis of hematological tumor; white blood cell count
3–12×109/l, platelet count ≥60×109/l,
absolute neutrophil count ≥109/l; average score of the
difficulty of mandibular impacted third molar extraction ≥14,
patients had difficulties with tooth extraction; and informed
consent form signed by patients. Exclusion criteria:
contraindications of surgery; long-term administration of
medication, recent administration of glucocorticoids, antibiotics,
or anodyne; recurrent pericoronitis of the impacted tooth; moderate
caries of the wisdom tooth and adjacent teeth; periapical
periodontitis, pulpitis, or periodontitis. The study was approved
by the Ethics Committee of Hubei Maternal and Child Health Care
Hospital of China. We randomly divided patients into equal
experimental and control groups, each with 36 patients. The
double-blind method was used to conduct perioperative treatment for
patients in the two groups. General clinical data for the patients
in the two groups were statistically comparable (Table I).
 | Table I.General clinical data. |
Table I.
General clinical data.
| Item | Control group
n=36 | Observation group
n=36 | t/χ2 | P-value |
|---|
| Sex
(male/female) | 20/16 | 22/14 | 0.057 | 0.811 |
| Age (year) | 15–45 | 16–45 |
|
|
| Average age
(year) | 23.76±5.48 | 24.35±5.57 | 0.453 | 0.651 |
| BMI
(kg/m2) | 22.13±3.45 | 22.76±3.38 | 0.783 | 0.436 |
| Hematological tumor
classification (n, %) |
|
|
|
|
| Acute
lymphoblastic leukemia | 13 (36.11) | 12 (33.33) | 0.585 | 0.964 |
| Acute
non-lymphocytic leukemia | 11 (30.56) | 9
(25.00) |
|
|
| Aplastic
anemia | 5
(13.89) | 6
(16.67) |
|
|
|
Non-Hodgkin's lymphoma | 4
(11.11) | 5
(13.89) |
|
|
|
Langerhans cell
histocytosis | 3 (8.33) | 4
(11.11) |
|
|
| Impacted type (n,
%) |
|
| 0.224 | 0.894 |
| Vertical
impaction | 18 (50.00) | 16 (44.44) |
|
|
| Central
loxosis impaction | 10 (27.78) | 11 (30.56) |
|
|
| Level of
impaction | 8
(22.22) | 9
(25.00) |
|
|
Preoperative preparation
All patients received routine examination and dental
X-ray film before surgery. The degree of swelling, index of
limitation of mouth opening, and related data were measured before
surgery. Three medical staff independently measured the data to
obtain the average. Patients in the experimental group started to
take bromelain enteric-coated capsules orally (Guangxi Province
Nanning City Baihui Pharmaceutical Group, approval number:
MPN-H45021171) one day before surgery. Dosage: 30,000 units every
time, three times/day. Chloroprocaine hydrochloride (4 ml of 2%)
and epinephrine (1:100,000) were used for inferior alveolar nerve
block anesthesia.
Surgical methods
We first conducted routine disinfection and drape,
and then proceeded with traditional chisel, standing out method and
bone removing method. After extraction, fragments in the alveolar
fossa were cleared. We used normal saline to wash and then closed
the wound. Patients who had their gingival open received sutures in
an open manner. Sterilized cotton roll was used to compress the
wound. Patients were told to tightly bite the roll for 30 min and
then gently spit it out.
Postoperative treatment
The control group received cold-hot compress for two
days. The experimental group continued to receive oral bromelain
enteric-coated capsules on the day of the surgery. Dosage: 30,000
units every time, three times/day, continuous administration for
three days. When patients suffered adverse reactions, like nausea,
allergy, or vomiting, they immediately stopped the treatment and
quit the study.
Detection of indexes and
evaluation
The visual analog score (VAS) was adopted to
evaluate the pain degree of patients. The score range was 0–10 (0
for no pain and 10 for intolerable severe pain). Standard: no pain:
0–1 points for no pain or little pain or pain hard to feel; mild:
2–3 points for tolerable pain that did not affect sleep; moderate:
3–6 points for pain that altered normal daily activities and sleep;
severe: ≥7 points for intolerable pain, patients took ibuprofen
sustained release capsule or return for a visit.
Swelling degree
The line connecting method was used to measure
distances. CT distance: the distance of the skin surface from the
tragion (T point) on the affected side of the cheek to the cheilion
(C point) on the same side. ME distance: the distance on the skin
surface from the external canthus point on the same side (E point)
to the mandibular angle point (M point). Value difference of CT+ME
before and after surgery indicated the swelling degree.
Limitation of mouth opening
We measured the distance from the upper central
incisor margin to the lower at the biggest positive mouth opening
state before and after surgery. Distance differences before and
after surgery indicated the limitation of mouth opening degree.
Blood and saliva samples were collected on
postoperative days 1, 3, and 7. ELISA was used to determine the
expression of IL-25 in gingival crevicular fluid and levels of
TNF-α, EGFR, and β-FGF in serum. Kits for detection of IL-25,
TNF-α, EGFR, and β-FGF were provided by Rapid Bio Company.
Operations were conducted strictly according to instructions of the
kits. OD value was measured at 450 nm wavelength.
One week after surgery, the quality of life after
tooth extraction was evaluated by the modified postoperative
symptom severity scale (PoSSe) method. Patients were scored in 7
dimensions: food, language, feeling, swelling, pain, nausea, and
daily living. PoSSe value was negatively correlated with the living
quality of patients.
Statistical analysis
Data were processed by SPSS 19.0 statistics
software. Measurement data were expressed as mean ± standard
deviation and t-test was used to compare groups. Enumeration data
were processed by χ2 test. P<0.05 was considered to
indicate a statistically significant difference.
Results
Pain after molar surgery
We compared several scores for the experimental and
control groups after molar surgery. According to the VAS results of
pain after surgery, the pain decreased in both groups from day 1 to
day 7 after surgery (Table II).
However, the experimental group exhibited significantly lower
scores at each time point compared to the control group (Table II), indicating more efficient pain
reduction.
 | Table II.Pain by VAS scale. |
Table II.
Pain by VAS scale.
| Group | Cases | Postoperative day
1 | Postoperative day
3 | Postoperative day
7 |
|---|
| Experimental | 36 | 5.35±1.14 | 4.06±1.13 | 2.23±1.02 |
| Control | 36 | 6.06±1.23 | 4.73±1.25 | 2.76±1.17 |
| t-value |
| 2.540 | 2.368 | 2.049 |
| P-value |
| 0.013 | 0.019 | 0.044 |
Swelling after molar surgery
In terms of swelling degree after surgery, swelling
decreased in both groups from day 1 to day 7 after surgery
(Table III). However, the
experimental group exhibited significantly lower swelling than the
control group at each time point (Table
III), indicating more efficient swelling management.
 | Table III.Swelling. |
Table III.
Swelling.
| Group | Cases | Postoperative day
1 | Postoperative day
3 | Postoperative day
7 |
|---|
| Experimental | 36 | 2.23±0.34 | 1.23±0.13 | 0.23±0.11 |
| Control | 36 | 2.85±0.43 | 1.98±0.27 | 1.01±0.37 |
| t-value |
| 6.786 | 15.017 | 12.124 |
| P-value |
| <0.0001 | <0.0001 | <0.0001 |
Limitation of mouth opening
The limitation of mouth opening degree decreased in
both groups from day 1 to day 7 after surgery (Table IV). However, the experimental group
exhibited significantly lower scores than the control group at each
time point (Table IV), indicating
more efficient functional recovery after surgery.
 | Table IV.Limitation of mouth opening
degree. |
Table IV.
Limitation of mouth opening
degree.
| Group | Cases | Postoperative day
1 | Postoperative day
3 | Postoperative day
7 |
|---|
| Experimental | 36 | 2.15±0.34 | 1.16±0.33 | 0.43±0.12 |
| Control | 36 | 2.76±0.53 | 1.83±0.45 | 1.16±0.27 |
| t-value |
| 5.812 | 7.204 | 14.824 |
| P-value |
| <0.0001 | <0.0001 | <0.0001 |
Values of molecular markers
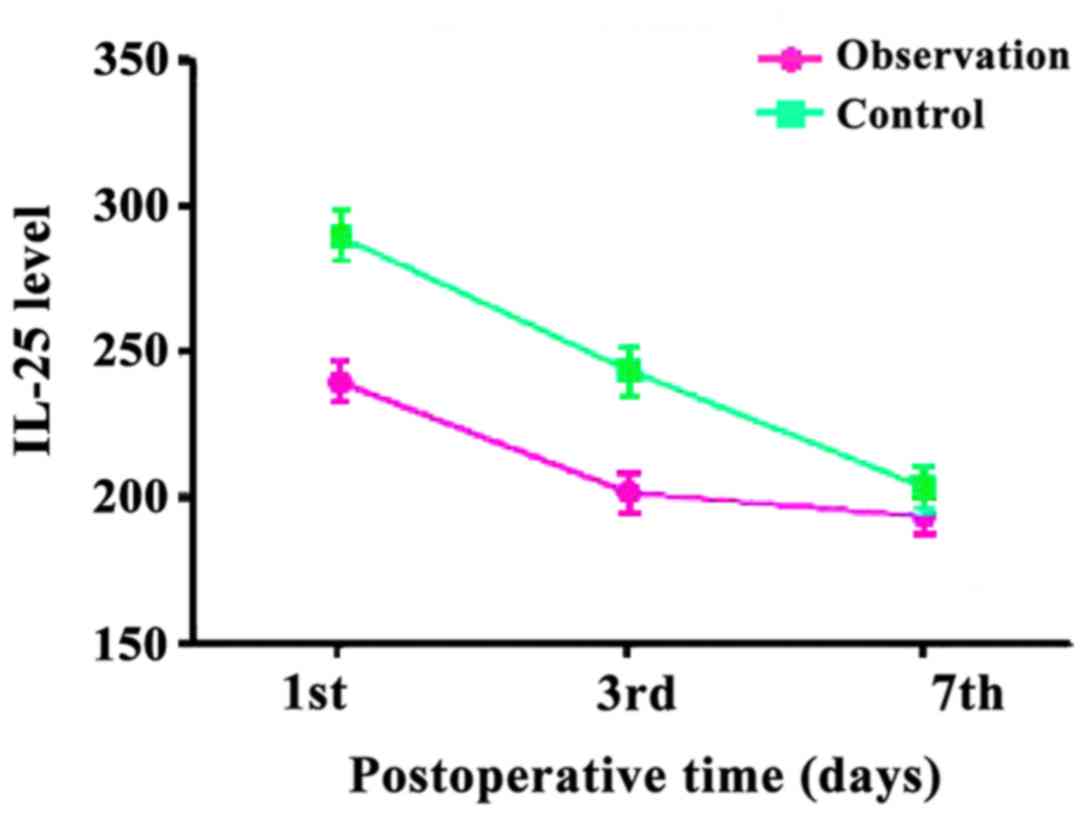
We next compared the concentration of IL-25 in
gingival crevicular fluid and levels of TNF-α, EGFR, and β-FGF in
serum. In the experimental group, the levels of IL-25 on
postoperative days 1, 3 and 7 were 239.43±7.24, 201.67±7.23, and
193.45±6.25 pg/ml. In the control group, the levels of IL-25 were
289.63±9.27, 243.54±8.46, and 203.47±7.36 pg/ml. The values in the
experimental group were significantly lower than in the control
group, although the difference was smaller at day 7 (Fig. 1).
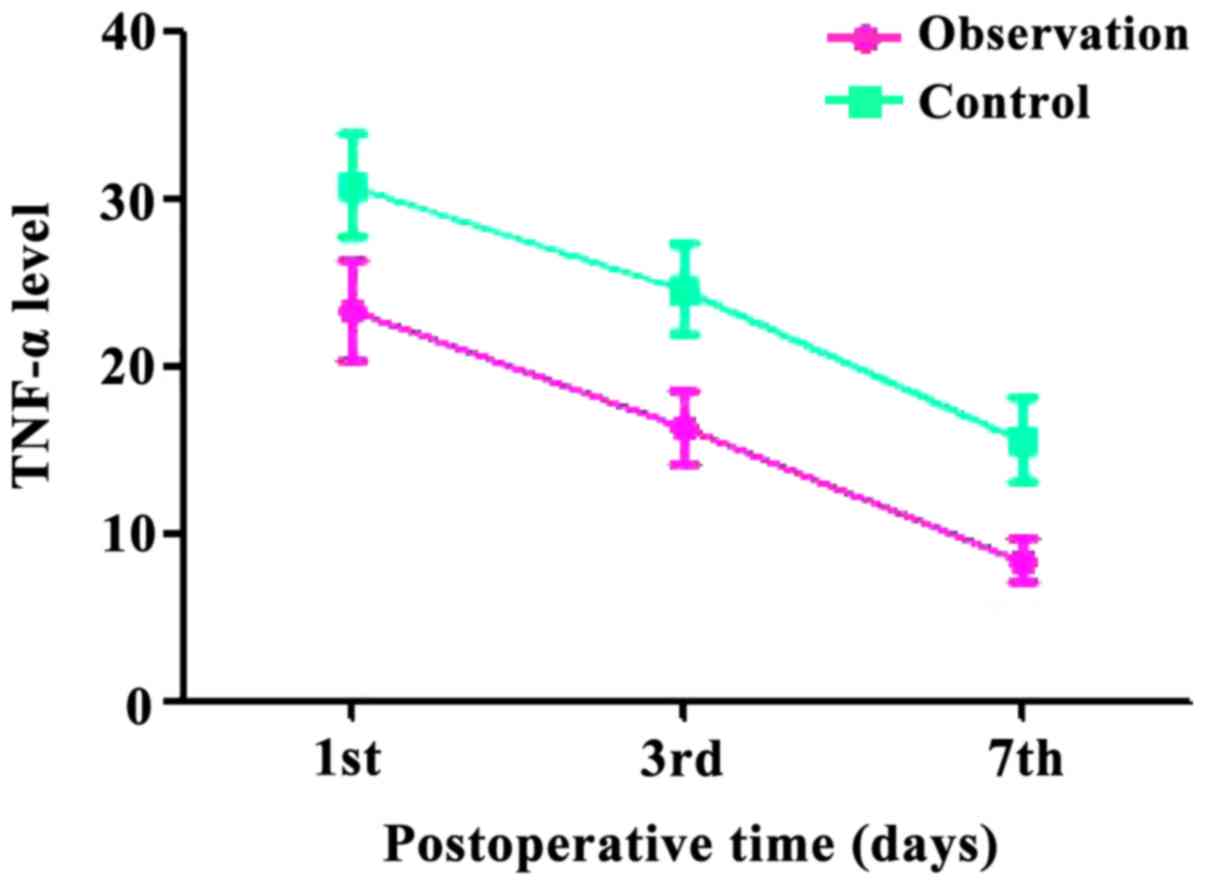
In the experimental group, the levels of TNF-α level
were 23.36±3.42, 16.36±2.27, and 8.43±1.34 pg/ml. In the control
group, the levels of TNF-α were 30.78±3.42, 24.56±2.68, and
18.62±2.46 pg/ml. The values in the experimental group were
significantly lower than in the control group at each time point
and the differences were the same over time (Fig. 2).
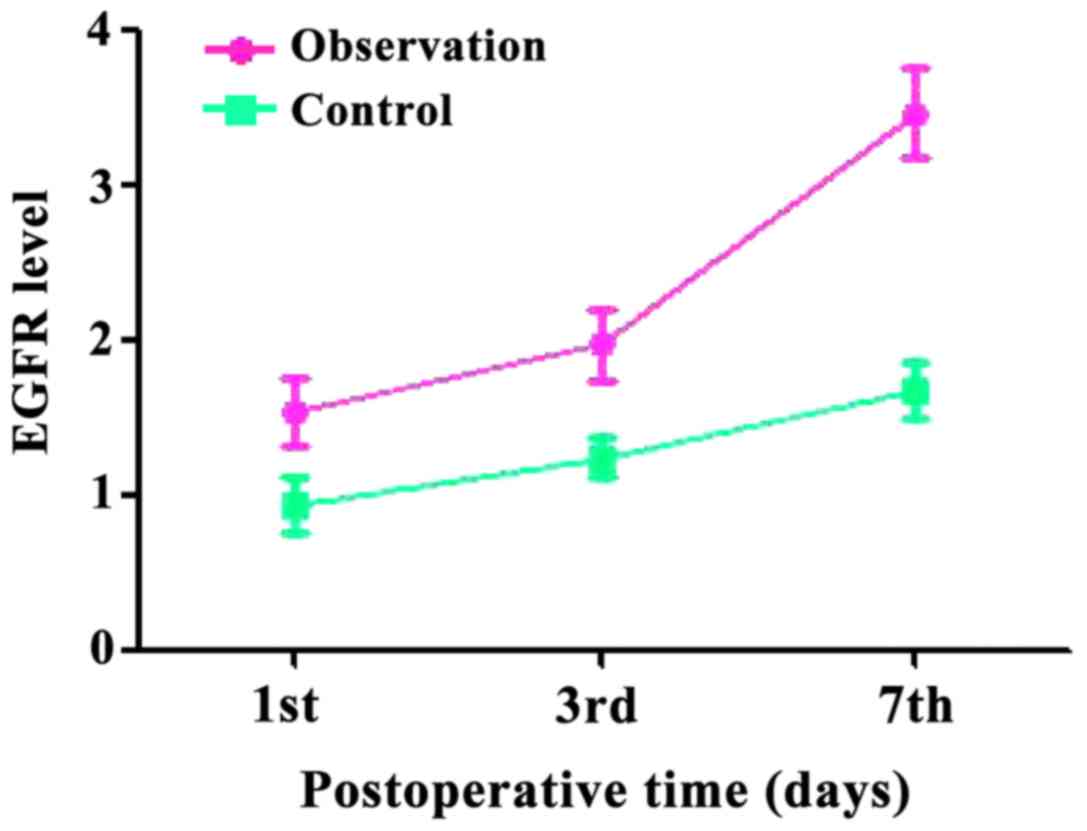
The levels of EGFR in the experimental group were
1.53±0.22, 1.97±0.23, and 3.46±0.29 ng/ml. The levels of EGFR in
the control group were 0.94±0.18, 1.24±0.13, and 1.67±0.18 ng/ml.
The values in the experimental group were significantly higher than
in the control group at each time point and the differences grew
over time (Fig. 3).
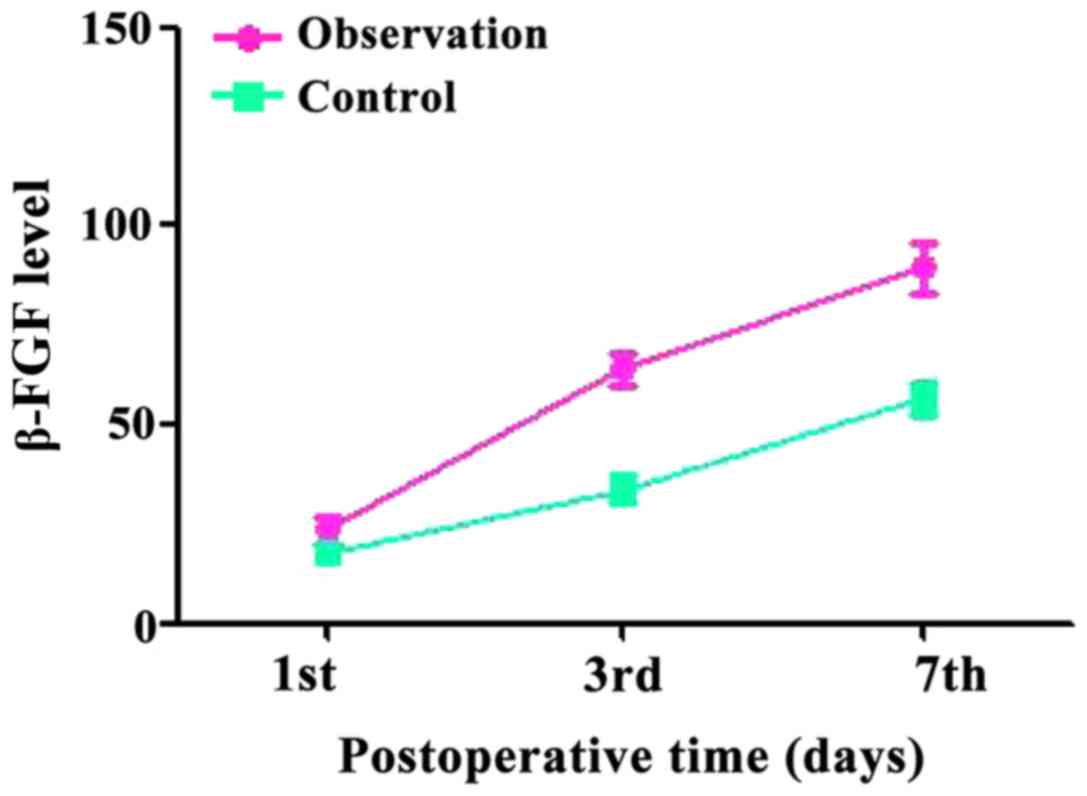
The levels of β-FGF in the experimental group were
23.43±3.42, 63.97±4.23, and 89.46±6.29 pg/ml. In the control group,
the levels were 17.53±2.74, 33.56±3.43, and 56.47±4.35 pg/ml. The
values were similar in the two groups at day 1, but the values in
the experimental group were significantly higher at days 3 and 7
(Fig. 4).
Quality of life
One week after surgery, the comparison of quality of
life for the two groups showed that the experimental group scored
better than the control group in all items (food, language,
feeling, swelling, pain, nausea, and daily living). The differences
were statistically significant (Table
V).
 | Table V.PoSSe scores. |
Table V.
PoSSe scores.
| Item | Observation group
(n=36) | Control group
(n=36) | t-value | P-value |
|---|
| Food |
5.76±2.78 |
7.96±2.18 |
3.763 |
0.0004 |
| Language |
1.17±0.63 |
2.57±0.93 |
7.478 | <0.0001 |
| Felling |
0.83±0.36 |
1.44±0.76 |
4.325 | <0.0001 |
| Swelling |
3.28±1.57 |
4.76±2.06 |
3.428 |
0.0010 |
| Pain |
4.16±2.01 |
6.23±1.01 |
5.521 | <0.0001 |
| Nausea |
0.21±0.12 |
0.91±0.21 | 17.365 | <0.0001 |
| Daily living |
1.38±0.34 |
3.38±0.54 | 18.805 | <0.0001 |
Discussion
The occurrence rate of complications after
extraction of third molars can reach up to 20%. Therefore,
effective prevention of complications in these procedures has
become a key priority for dentists (8). Postoperative complications include pain,
dry socket, face swelling, limited mouth opening, and other. These
symptoms typically last for seven days, causing serious impact on
the daily life of patients (9). Pain
results from damaged tissues, which irritates the nerves.
Destruction of tissue during surgery leads to edema and swelling of
the face as part of the normal reactive edema. Moderate swelling is
a protective reaction to trauma; however, excessive swelling has
damaging consequences and even leads to infection (10,11). The
mechanism explaining the limited mouth opening is that cutting soft
tissue during surgery irritates the temporal tendon and the muscle
in nasal alar, causing a reflex spasm (12). Clinical treatment of complications
after tooth extraction include cold-hot compress, drainage tube,
and oral administration of non-steroidal anti-inflammatory drugs.
These treatments need to extend for a period after surgery to
shorten the durations of pain, swelling, and limited mouth opening.
These complications affect the normal administration of
chemotherapy in patients with hematological tumors and may even
lead to chemotherapy failure. Therefore, it is especially important
to identify convenient and effective treatments for these
complications (13). Bromelain is a
good anti-inflammatory drug that can promote wound repair. Our
results suggest that patients on bromelain showed obvious
improvement in postoperative pain, swelling, and mouth opening. The
quality of life in the bromelain group was higher than in the
control group.
The inflammatory response is the most basic reaction
to injuries and is a necessary stage for injury repair after third
molar extraction (14). The stress
response of tissue after surgery will result in the activation of
IL-25 and TNF-α, which can be detected in serum. IL-25 is a
Th2-type inflammatory factor that can strengthen the Th2 immune
response. Meanwhile, various types of chemotactic factors will
gather at the inflammation site and worsen the inflammatory
response. TNF-α activates genes related to the inflammatory
reaction, promotes hyperplasia of macrophages, and worsens the
stress response (15,16). Our results show that IL-25 and TNF-c
were lower in the bromelain group than in the control group. This
is because bromelain can not only clear the wound during the
inflammatory response but also downregulate IL-25 and TNF-α,
relieving the inflammatory reaction at the wound surface.
Patients with hematological tumors receive
extraction of the third molar during chemotherapy. Rapid repair of
the wound after surgery is critical for the success of later
chemotherapy rounds. EGFR can promote cell division, increase cell
migration, promote wound healing, and improve the quality of tissue
repair. EGFR selectively gathers with epidermal cells, inflammatory
cells, and fibroblasts and forces their migration towards the wound
site. EGFR also promotes cell division and proliferation (17,18). β-FGF
can stimulate the differentiation and proliferation of fibroblasts,
improve the level of collagen, increase the growth and
epithelization speed of granulation tissue, and induce the
generation of microvessels. β-FGF belongs to one of the most active
angiogenesis factors and is used as a marker for the quality and
speed of wound healing (19). Our
research indicates that EGFR and β-FGF were elevated in the
bromelain group due to its ability to regulate the expression of
EGFR and β-FGF, promote the proliferations of fibroblasts,
endothelial cells, and epithelial cells, increase the growth and
epithelization speed of granulation tissue, develop new
capillaries, degrade excess fibers, and increase the quality and
speed of wound healing (20).
In conclusion, bromelain can reduce complications
after third molar extraction, including pain, swelling, and limited
mouth opening. This is an important advantage for patients
undergoing chemotherapy for hematological tumors. Besides,
bromelain can promote the recovery effect, improve the quality of
life after surgery, and its administration is convenient, easy,
economic, and has non-invasive characteristics that deserve wider
clinical attention and application.
References
|
1
|
Zor ZF, Isik B and Cetiner S: Efficacy of
preemptive lornoxicam on postoperative analgesia after surgical
removal of mandibular third molars. Oral Surg Oral Med Oral Pathol
Oral Radiol. 117:27–31. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Carvalho RW, Araújo-Filho RC and
Vasconcelos BC: Adverse events during the removal of impacted
maxillary third molars. Int J Oral Maxillofac Surg. 43:1142–1147.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Alcântara CE, Falci SG, Oliveira-Ferreira
F, Santos CR and Pinheiro ML: Pre-emptive effect of dexamethasone
and methylprednisolone on pain, swelling, and trismus after third
molar surgery: A split-mouth randomized triple-blind clinical
trial. Int J Oral Maxillofac Surg. 43:93–98. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Díaz Gómez L, Seguro Fernandez A, Jaen
Olasolo J, Villanego Beltran I, Diaz Diaz V, Gonzalez Calvo E,
Ingunza Baron L, Gutierrez Bayard L, Salas Buzon MC and Garduño S:
EP-1143: Splenic irradiation as treatment modality in neoplastic
hematological disorders. Radiother Oncol. 119(Suppl 1):
5462016.http://www.thegreenjournal.com/article/S0167-8140(16)32393-3/fulltext
View Article : Google Scholar
|
|
5
|
Hegde AM, Joshi S, Rai K and Shetty S:
Evaluation of oral hygiene status, salivary characteristics and
dental caries experience in acute lymphoblastic leukemic (ALL)
children. J Clin Pediatr Dent. 35:319–323. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bhatnagar P, Pant AB, Shukla Y, Panda A
and Gupta KC: Hyaluronic acid grafted PLGA copolymer nanoparticles
enhance the targeted delivery of bromelain in Ehrlich's ascites
carcinoma. Eur J Pharm Biopharm. 105:176–192. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
de la Barrera-Núñez MC, Yáñez-Vico RM,
Batista-Cruzado A, Heurtebise-Saavedra JM, Castillo-de Oyagüe R and
Torres-Lagares D: Prospective double-blind clinical trial
evaluating the effectiveness of Bromelain in the third molar
extraction postoperative period. Med Oral Patol Oral Cir Bucal.
19:e157–e162. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Aravena PC, Astudillo P and Manterola C:
Design of a scale for measuring post-surgical complications in
third molar surgery. Int J Oral Maxillofac Surg. 43:1008–1014.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ghaeminia H, Hoppenreijs TJM, Xi T, Fennis
JP, Maal TJ, Bergé SJ and Meijer GJ: Postoperative socket
irrigation with drinking tap water reduces the risk of inflammatory
complications following surgical removal of third molars: A
multicenter randomized trial. Clin Oral Investig. 21:71–83. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Quiding H, Jonzon B, Svensson O, Webster
L, Reimfelt A, Karin A, Karlsten R and Segerdahl M: TRPV1
antagonistic analgesic effect: A randomized study of AZD1386 in
pain after third molar extraction. Pain. 154:808–812. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Sortino F and Cicciù M: Strategies used to
inhibit postoperative swelling following removal of impacted lower
third molar. Dent Res J Isfahan. 8:162–171. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Trindade PAK, Giglio FPM,
Colombini-Ishikiriama BL, Calvo AM, Modena KC, Ribeiro DA, Dionísio
TJ, Brozoski DT, Lauris JR, Faria FA, et al: Comparison of oral
versus sublingual piroxicam during postoperative pain management
after lower third molar extraction. Int J Oral Maxillofac Surg.
40:292–297. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Isiordia-Espinoza MA, de Jesús
Pozos-Guillén A and Aragon-Martinez OH: Analgesic efficacy and
safety of single-dose tramadol and non-steroidal anti-inflammatory
drugs in operations on the third molars: A systematic review and
meta-analysis. Br J Oral Maxillofac Surg. 52:775–783. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Bello SA, Adeyemo WL, Bamgbose BO, Obi EV
and Adeyinka AA: Effect of age, impaction types and operative time
on inflammatory tissue reactions following lower third molar
surgery. Head Face Med. 7:82011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Swaidani S, Bulek K, Kang Z, Gulen MF, Liu
C, Yin W, Abbadi A, Aronica M and Li X: T cell-derived Act1 is
necessary for IL-25-mediated Th2 responses and allergic airway
inflammation. J Immunol. 187:3155–3164. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Billeter AT, Hellmann JL, Bhatnagar A and
Polk HC Jr: Transient receptor potential ion channels: Powerful
regulators of cell function. Ann Surg. 259:229–235. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Morgillo F, Martinelli E, Troiani T,
Orditura M, De Vita F and Ciardiello F: Antitumor activity of
sorafenib in human cancer cell lines with acquired resistance to
EGFR and VEGFR tyrosine kinase inhibitors. PLoS One. 6:e28841.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Maretzky T, Evers A, Zhou W, Swendeman SL,
Wong PM, Rafii S, Reiss K and Blobel CP: Migration of growth
factor-stimulated epithelial and endothelial cells depends on EGFR
transactivation by ADAM17. Nat Commun. 2:2292011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Komura M, Komura H, Konishi K, Ishimaru T,
Hoshi K, Takato T, Tabata Y and Iwanaka T: Promotion of tracheal
cartilage growth by intra-tracheal injection of basic fibroblast
growth factor (b-FGF). J Pediatr Surg. 49:296–300. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
de Oliveira Caetano GA, Villela SDJ, de
Oliveira MMNF, de Paula Leonel F and Tamy WP: Particle passage
kinetics and neutral detergent fiber degradability of silage of
pineapple waste (aerial parts) under different packing densities.
Rev Bras Zootec. 43:49–53. 2014.http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1516-35982014000100008l
View Article : Google Scholar
|