Introduction
Intravascular large B-cell lymphoma (IVLBCL) is a
rare subtype of diffuse large B-cell lymphoma (LBCL) with a
distinct intravascular proliferation of clonal lymphocytes. The
incidence in males is slightly higher than that for females.
Patients with IVLBCL usually have no lymphadenopathy, but tumor
cells invade the blood vessels of multiple organs, such as the bone
marrow, central nervous system, skin, lungs, liver, kidneys, and
intestinal tract (1). Therefore, the
clinical presentation is highly variable. Diagnosis of IVLBCL
depends on histopathology, and can be challenging to diagnose due
to the variable clinical manifestations, low incidence and
diagnostic awareness deficiency.
IVLBCL is typically treated with chemotherapy
including a chimeric anti-CD20 monoclonal antibody (most commonly
rituximab), which has been reported to achieve a relatively good
response (2), and autologous stem
cell transplantation can also lead to good outcomes (3). Here, we report three cases of primary
pulmonary IVLBCL diagnosed in our unit from 2010 to 2015. Also, we
review the intravascular large B-cell lymphoma (IVLBCL) based on
these cases and previous reports. The Ethics Committees of Drum
Tower Hospital approved the current study based on the three
cases.
Case report
Case 1
A 68-year-old male patient was admitted to the
respiratory unit of our hospital with a 3-month history of
progressive dyspnea on exertion, dry cough, intermittent high
fevers to 39°C, and weight loss. He had been treated with various
courses of antibiotics without improvement. He had a 20-year
history of diabetes mellitus, but no history of lung disease or
smoking. The vital signs and physical examination were normal,
except for a temperature (38.3°C).
Blood tests revealed pancytopenia, with an elevated
lactate dehydrogenase, β2-MG, and erythrocyte
sedimentation rate; also, EBV-DNA copies level exceeded the normal
level, which was 5.69×103 (IU/ml).
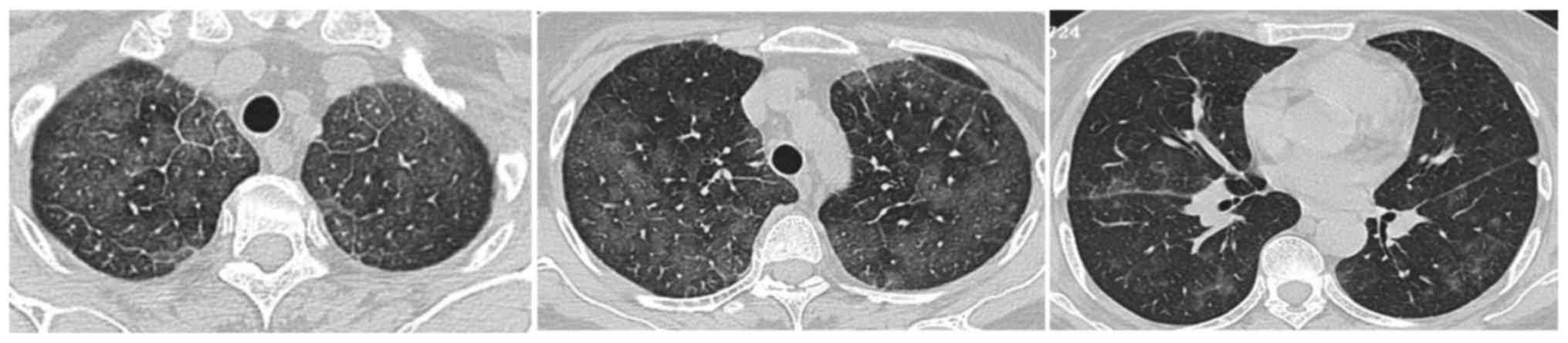
High resolution computed tomography (HRCT) revealed
thickened interlobular septa, multiple nodules and patchy ground
glass opacities bilaterally (Fig. 1).
A bone marrow biopsy showed diminution of hematopoietic cells, and
megakaryocytes were not identified. Transbronchial lung biopsy
(TBLB) revealed a small amount of atypical cells in the alveolar
interstitium, but there was not sufficient pathologic change to
establish a diagnosis. An open lung biopsy was performed, revealing
a primary pulmonary lymphoma, diffuse large B-cell, non-germinal
center origin. Immunohistochemical stains demonstrated that the
cells were immunoreactive for for CD20 and Mum-1, and negative for
CD3, CD10, CK, BCL-6 and MPO. The expression of CD4, CD3, CD5, CD8,
CD38, CD7 and CD2 on the large cells was detected by flow
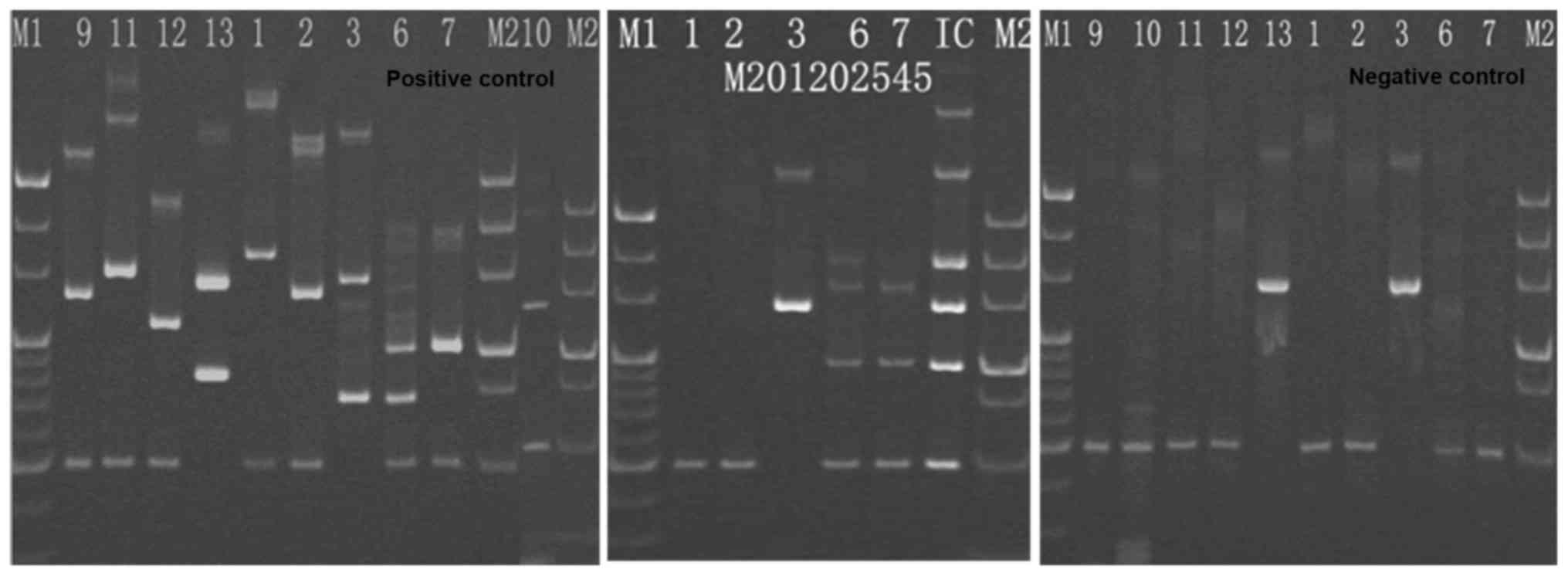
cytometry. Clonal rearrangements of Igκ-VJ and Igκ-V/in were
detected by PCR (Fig. 2), without
IGH/BCL2, BCL6, c-MYC fragmantation and P53 deletion. The patient
treated with rituximab, cyclophosphamide, pirarubicin, vincristine,
and prednisone [R-CHOP]. However, during the initial infusion of
rituximab, anaphylacitc shock occurred. Treatment was changed from
[R-CHOP] to [CHOP]. Complete remission (CR) was observed following
4 cycles of treatment, as visualized by CT scan (Fig. 3). Then the patient subsequently
received two cycles of [CHOP] consolidation chemotherapy. One year
later, the patient was readmitted with a relapse. Four cycles of
[CHOP] regimen were administered followed by ifosfamide,
carboplatin, and etoposide [ICE]. But only partial remission was
achieved. He died from infection secondary to myelosuppression 1
year later.
Case 2
A 60-year-old female patient was admitted to the
respiratory unit with a 1-month history of progressive dyspnea, and
20 days of intermittent high fever. The temperature fluctuated
between 38 and 39°C. She had been treated wide-spectrum antibiotics
and indomethacin, but dyspnea and fever did not resolve. Her past
medical history included a renal cyst and hysterectomy, but no lung
disease. She was a non-smoker. On examination, anemia, fever and
tachypnea were found.
Laboratory investigation Following diagnosis, the
patient returned home for treatment, and she received
cyclophosphamide, pirarubicin, vincristine, and prednisone [CHOP].
revealed a mild anemia, elevated LDH and ESR (Table I).
 | Table I.Pertinent laboratory data at the time
of the patient's initial evaluation. |
Table I.
Pertinent laboratory data at the time
of the patient's initial evaluation.
|
| Admission value |
|
|---|
|
|
|
|
|---|
| Variable | CASE 1 | CASE 2 | CASE 3 | Reference range |
|---|
| WBC
(×109/l) | 3.0 | 6.1 | 4.5 | 4–10 |
| Hb (g/l) | 79 | 90 | 87 | 130–175 |
| PLT
(×109/l) | 90 | 102 | 107 | 100–300 |
| ESR (mm/hr) | 106 | 80 | 97 | 2–15 |
| B2-MG (mg/l) | 8.15 | Not checked | Not checked | 1.09–2.53 |
| LDH (IU/l) | 2,340 | 1,434 | 1,095 | 85–250 |
| ALB (g/l) | 28.7 | 29.2 | 31 | 32–55 |
| AST (IU/l) | 37.3 | 29.5 | 40 | 10–42 |
| ALT (IU/l) | 28 | 17.1 | 36 | 10–40 |
| BUN (mmol/l) | 6.7 | 5.3 | 3.7 | 2.85–7.14 |
| CREA (umol/l) | 81 | 75 | 46.6 | 53–115 |
| EBV-DNA (IU/ml) |
5.69×103 | Negative | Not checked |
<5.0×102 |
| CRP (mg/l) | 13.4 | 79.9 | 88.5 | 0–8 |
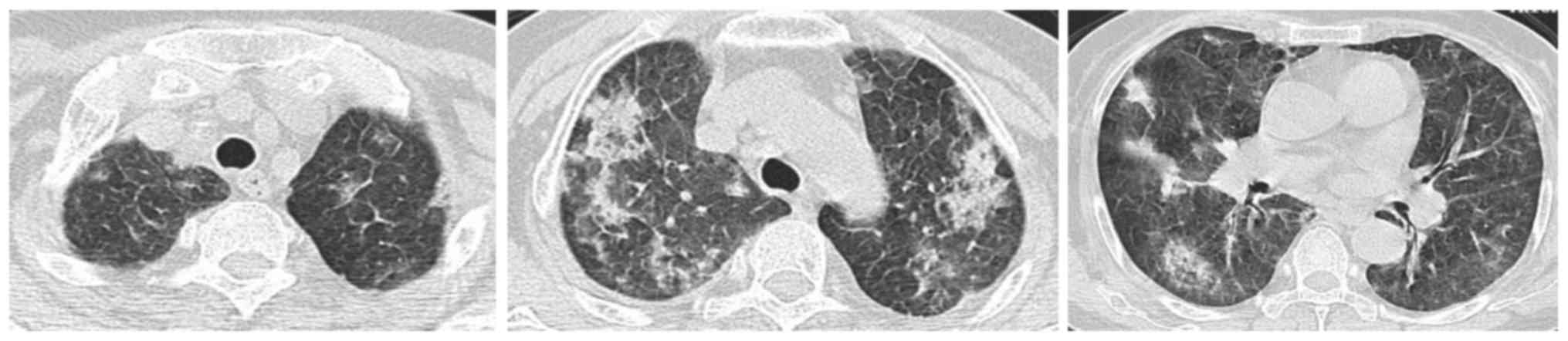
HRCT revealed diffuse centrilobular nodules and GGO
bilaterally, and predominantly in the middle and upper lung. In the
upper lung, thickened interlobular septa can also be seen (Fig. 4).
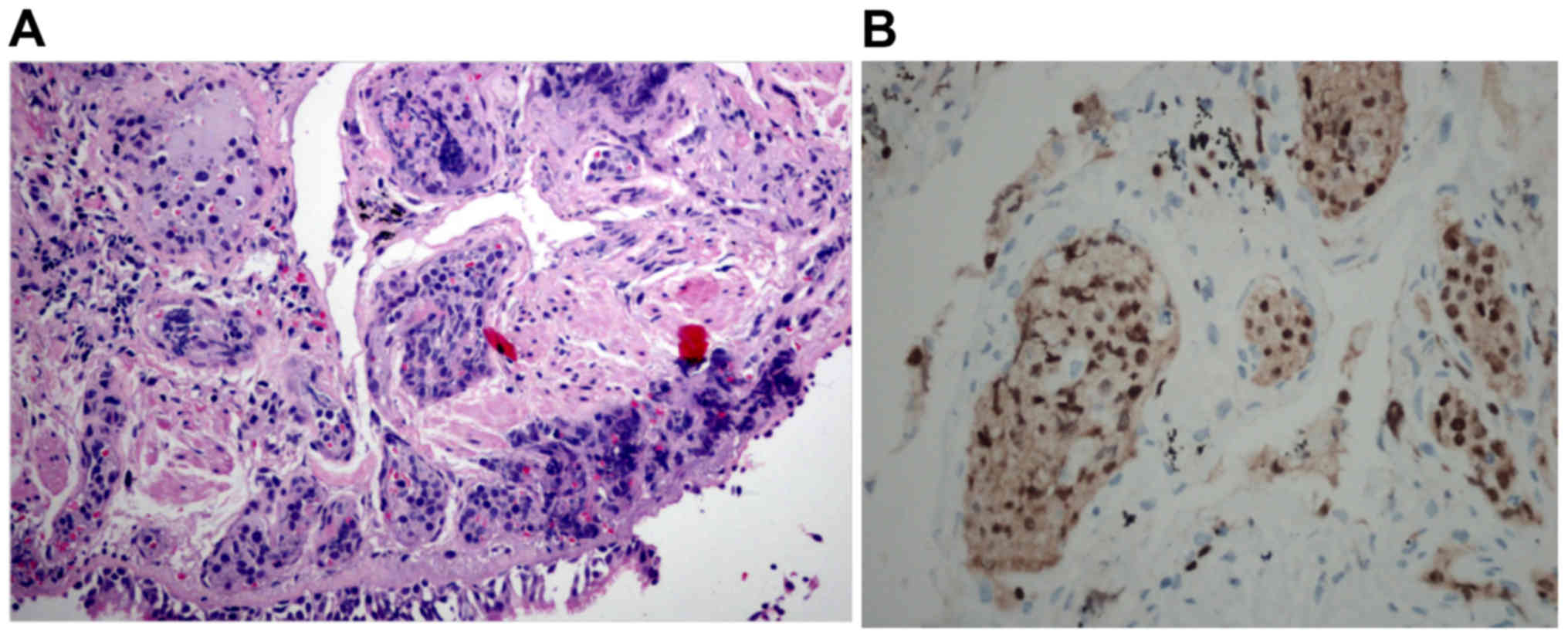
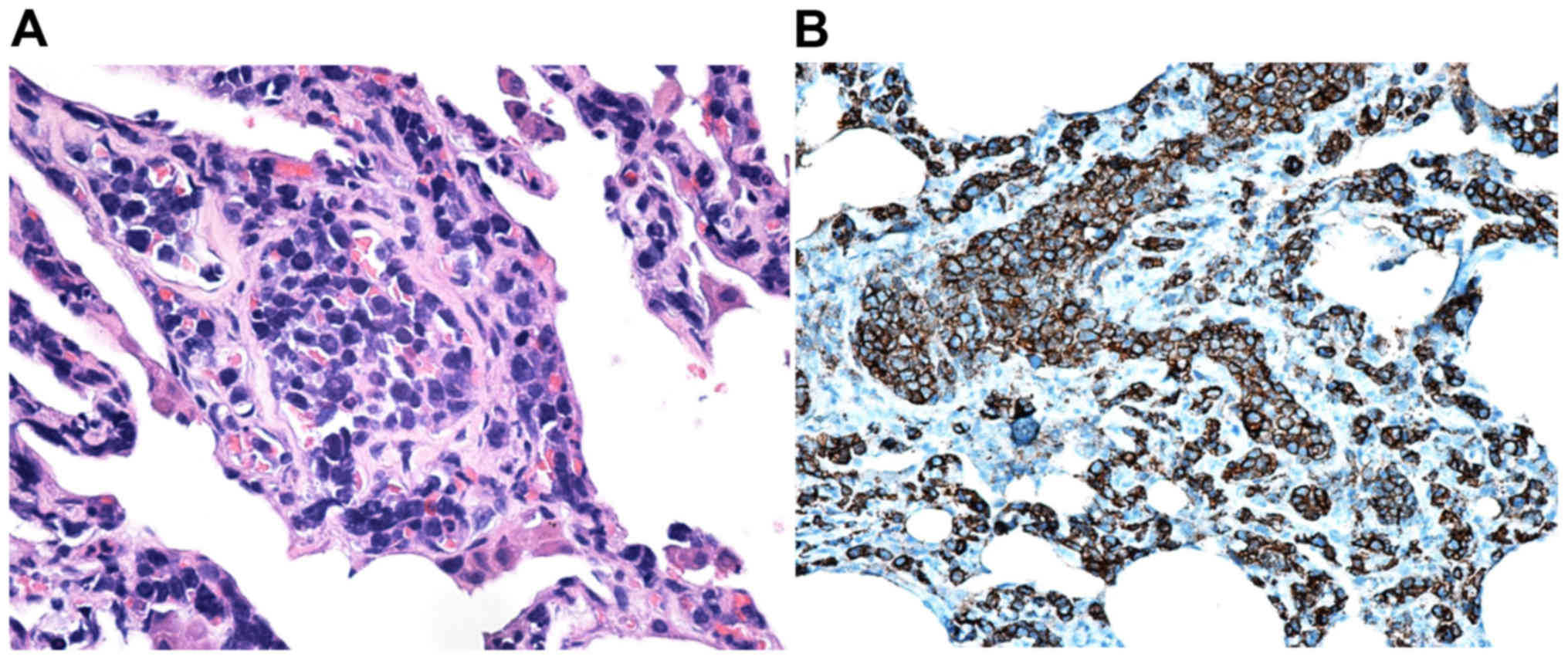
TBLB showed that CD20 positive atypical lymphocytes
in the capillaries of the lung. Immunohistochemical stains
demonstrated that these cells were immunoreactive to CD20, 20%
positive for Ki-67 and negative for CD3 and CK (Fig. 5). The features were consistent with
IVLBCL.
At first it seemed that treatment was effective and
dyspnea improved. But she died quickly due to severe, concomitant
infection.
Case 3
A 69-year-old female was admitted with a 2-month
history of productive cough, exertional dyspnea, and one week of
fever. The temperature fluctuated between 37.3 and 37.8°C. She was
managed with antitussives, expectorants, and bronchodilators, and
antibiotics without improvement. In the past history, she had a
cholecystectomy. She was a non-smoker. On examination she was found
to have lip cyanosis, swollen feet, and an elevated temperature
(39.2°C).
Her laboratory investigation findings are shown in
Table I. In brief, LDH and ESR were
both elevated significantly besides moderate anemia. A HRCT of the
chest revealed patchy GGO in both lungs, with isolated thickening
of interlobular septa (Fig. 6). A
TBLB showed atypical lymphocytes in the vascular system of the
lung. Immunohistochemical stains demonstrated that these cells were
positive for CD20, CD79a, Mum-1, and LCA, but negative for CD3,
CD5, CD7, CD56, CD10, CK, TTF1, CD3ε, EBER and MPO (Fig. 7).
Following diagnosis, she returned home and received
chemotherapy with [CHOP] regimen. Then she was lost to
follow-up.
Discussion
In 1958, Pfleger and Tappeiner first described
IVLBCL. After that, cases of IVLBCL were reported in succession. In
2008, the WHO classified it as a rare, specific type of
non-Hodgkins lymphoma (NHL). IVLBCL typically occurs in elderly
patients with male to female ratio of 1.3 to 1. The main feature of
this type of lymphoma is that it is a diffuse, occlusive
proliferation in vessels, especially in the capillaries, small
arteries and veins (4). Previously,
about 50% cases were diagnosed by post-mortem. Now, with the
development of immunohistochemical and monoclonal antibodies, and a
greater clinical awareness, establishing the diagnosis of this
disease during lifetime, similar to our cases, is believed to be
increasing (5).
The clinical manifestations of IVLBCL include both
constitutional symptoms, such as fever, weight loss, night sweats,
and general fatigue, and organ-specific symptoms due to tumor cells
infiltrating the vessels of any organ. The heterogeneous and
nonspecific symptoms make identification of this disease in
patients challenging. Laboratory findings suggestive of IVLBCL or
other lymphoproliferative diseases include elevation of the
C-reactive protein (CRP), LDH, β2-MG, interleukin-2R
(IL-2R) or serum albumin. Close correlation between increased LDH
level and the differentiation of tumor cells has been reported
(6–8).
When lungs are involved by IVLBCL, the clinical
manifestations include cough, sputum production, and dyspnea. Some
patients also present with hypoxemia, hypercalcemia, pulmonary
embolism, pulmonary hypertension or hemophagocytic syndrome
(9–11). Lung function frequently shows impaired
lung volumes or diffusion capacity (12). The appearance of lungs on HRCT is
varied, with findings including centrilobular nodules, interlobular
septal thickening, and GGO. Interstitial shadows and thickening of
bronchovascular bundles usually suggest haematological and/or
lymphatic spread (12).
Recently, 18F-FDG PET/CT has emerged as a
powerful imaging modality in the assessment, diagnosis, staging and
treatment response in lymphoma (13).
When respiratory symptoms suggest pulmonary involvement without
abnormal performance in lung HRCT scan, FDG-PET/CT can be a useful
tool for the early diagnosis of IVLBCL (13,14).
All of our cases had fever, dyspnea, hypoxaemia,
anemia, increased LDH and an elevated ESR levels. Two of the three
patients had increased level of CRP. These clues suggested to us
that these patients may have had some kind of lymphoproliferative
diseases. Besides, HRCT showed GGO, nodules, and thickened
interlobular septa bilaterally in the lungs, which denoted us that
the disease may spread along lymphatic structures. Two of the three
had ventilation impairment and diffusion abnormalities (Table II). The radiological characteristics
and pulmonary function characteristics are similar to those seen in
interstitial lung diseases (ILD). Therefore, histopathologic
analysis is required to make diagnosis.
 | Table II.Lung function and blood gas
analysis. |
Table II.
Lung function and blood gas
analysis.
| Variable | CASE 1 | CASE 2 | CASE 3 | Reference range |
|---|
| FVC/pred (%) | 91.4 | 65 | 62.7 | >80 |
| DLCO/pred (%) | 80 | 38.3 | 43.2 | >80 |
| PaO2
(mmHg) | 61 | 62 | 48 | 80–100 |
| PaCO2
(mmHg) | 32.2 | 32 | 29.5 | 35–45 |
The histopathology of IVLBCL shows large malignant
lymphocytes filling small vascular lumina. In addition, the bone
marrow seems to be the most relevant diagnostic site for Asian
patients (5).
Regarding pulmonary investigations, an open lung
biopsy or a trans-thoracoscopy lung biopsy is the most powerful
method for diagnosis. Sometimes TBLB may also be useful, especially
in patients with abnormal HRCT features (15). For our patients, two of them (CASE 2
and 3) were diagnosed by TBLB. In addition, when the pathology of
CASE 1 was re-reviewed following diagnosis by open lung biopsy, we
found that we could set up the same diagnosis by TBLB. The
diagnosis was missed at first, because this disease was not
considered at that time. However, the bone marrow biopsy was
unremarkable in our case (CASE 1).
A timely and accurate diagnosis and the appropriate
treatment can significantly improve the clinical outcomes.
Currently there is no established treatment for IVLBCL because of
the small number of cases. The treatment of cases with lung
involvement is similar to that for diffuse LBCL, consisting of CHOP
or CHOP-like regimens plus rituximab (CHOP-R or CHOP-like-R) and
CNS prophylaxis (16–18).
As for the survival time, it was reported that the
mean 3-year overall survival was 33 months according to the report
from Ferreri and coworkers (19).
Although IVLBCL and primary pulmonary IVLBCL are
rare diseases, we have made a diagnosis and treated three patients
during 5 years. After review of these cases, we conclude: 1. Rare
diseases may be encountered in clinical work. 2. Since HRCT
characteristics of primary pulmonary IVLBCL is similar to ILD, both
diagnosis and differential diagnosis are very important. 3. TBLB
can be useful for diagnosis, as shown in our cases.
Acknowledgements
The present study was supported by the National
Natural Science Fund of China (grant no. 81570055). We thank Prof.
Dr. Med. Ulrich Costabel (from Department of
Pneumology/Allergology, Ruhrlandklinik, University Hospital,
University Duisburg-Essen, Essen, Germany) and Associate Professor
Paul John Wolters (from Department of Medicine, University of
California, San Francisco, CA, USA) for article layout, logic
sequential adjustment and text revision work. This abstract was
presented at the American Thoracic Society 2017 International
Conference, May 19–24, 2017 in Washington, DC, IL, USA and was
published as abstract no. 6579 in American Journal of Respiratory
and Critical Care Medicine 2017.
References
|
1
|
Ferreri AJ, Campo E, Seymour JF, Willemze
R, Ilariucci F, Ambrosetti A, Zucca E, Rossi G, López-Guillermo A,
Pavlovsky MA, et al: Intravascular lymphoma: Clinical presentation,
natural history, management and prognostic factors in a series of
38 cases, with special emphasis on the ‘cutaneous variant’. Br J
Haematol. 127:173–183. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ferreri AJ, Dognini GP, Govi S, Crocchiolo
R, Bouzani M, Bollinger CR, D'Incan M, Delaporte E, Hamadani M,
Jardin F, et al: Can rituximab change the usually dismal prognosis
of patients with intravascular large B-cell lymphoma? J Clin Oncol.
26:1–5136. 2008. View Article : Google Scholar
|
|
3
|
Sawamoto A, Narimatsu H, Suzuki T,
Kurahashi S, Sugimoto T and Sugiura I: Long-term remission after
autologous peripheral blood stem cell transplantation for relapsed
intravascular lymphoma. Bone Marrow Transplant. 37:233–234. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Swerdlow SH, Campo E, Harris NL, Jaffe ES,
Pileri SA, Stein H, Thiele J and Vardiman JW: WHO classification of
tumours of haematopoietic and lymphoid tissue. Fourth. Geneva:
World Health Organization; 2008
|
|
5
|
Mahasneh T, Harrington Z, Williamson J,
Alkhawaja D, Duflou J and Shin JS: Intravascular large B-cell
lymphoma complicated by invasive pulmonary aspergillosis: A rare
presentation. Respirol Case Rep. 2:67–69. 2014.PubMed/NCBI
|
|
6
|
Anila KR, Nair RA, Koshy SM and Jacob PM:
Primary intravascular large B-cell lymphoma of pituitary. Indian J
Pathol Microbiol. 55:549–551. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ponzoni M and Ferreri AJ: Intravascular
large B cell lymphoma: Widespread but not everywhere. Acta
Haematol. 131:16–17. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Khalifa KA, Alkilani AA, Ismail H and
Soliman MA: Evaluation of some biochemical markers as prognostic
factors in malignant lymphoma. J Egypt Natl Canc Inst. 20:47–54.
2008.PubMed/NCBI
|
|
9
|
Sinha N, Lantigua L, Niazi M and
Diaz-Fuentes G: An elderly lady with fever of unknown etiology and
severe pulmonary hypertension: Intravascular lymphoma-an elusive
diagnosis. Case Rep Med. 2013:1537982013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chinen Y, Nakao M, Sugitani-Yamamoto M,
Kiyota M, Horiike S, Kuroda J and Taniwaki M: Intravascular B-cell
lymphoma with hypercalcemia as the initial presentation. Int J
Hematol. 94:567–570. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Fung KM, Chakrabarty JH, Kern WF,
Magharyous H, Gehrs BC and Li S: Intravascular large B-cell
lymphoma with hemophagocytic syndrome (Asian variant) in a
Caucasian patient. Int J Clin Exp Pathol. 5:448–454.
2012.PubMed/NCBI
|
|
12
|
Yu H, Chen G, Zhang R and Jin X: Primary
intravascular large B-cell lymphoma of lung: A report of one case
and review. Diagn Pathol. 7:702012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Seam P, Juweid ME and Cheson BD: The role
of FDG-PET scans in patients with lymphoma. Blood. 110:3507–3516.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wagner T, Brechemier D, Dugert E, Le
Guellec S, Julian A, Hitzel A and Beyne-Rauzy O: Diffuse pulmonary
uptake on FDG-PET with normal CT diagnosed as intravascular large
B-cell lymphoma: A case report and a discussion of the causes of
diffuse FDG uptake in the lungs. Cancer Imaging. 23:7–12. 2012.
View Article : Google Scholar
|
|
15
|
Nishizawa T, Saraya T, Ishii H and Goto H:
Antemortem diagnosis with multiple random skin biopsies and
transbronchial lung biopsy in a patient with intravascular large
B-cell lymphoma, the so-called Asian variant lymphoma. BMJ Case
Rep. 2014:pii: bcr20132026612014. View Article : Google Scholar
|
|
16
|
Chen Y, Ding C, Lin Q, Yang K, Li Y and
Chen S: Primary intravascular large B-cell lymphoma of the lung: A
review and case report. J Thorac Dis. 6:E242–E245. 2014.PubMed/NCBI
|
|
17
|
Takahashi H, Tomita N, Yokoyama M, Tsunoda
S, Yano T, Murayama K, Hashimoto C, Tamura K, Sato K and
Ishigatsubo Y: Prognostic impact of extranodal involvement in
diffuse large B-cell lymphoma in the rituximab era. Cancer.
118:4166–4172. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Shimada K, Matsue K, Yamamoto K, Murase T,
Ichikawa N, Okamoto M, Niitsu N, Kosugi H, Tsukamoto N, Miwa H, et
al: Retrospective analysis of intravascular large B-cell lymphoma
treated with rituximab-containing chemotherapy as reported by the
IVL study group in Japan. J Clin Oncol. 26:3189–3195. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ferreri AJ, Campo E, Ambrosetti A,
Ilariucci F, Seymour JF, Willemze R, Arrigoni G, Rossi G,
López-Guillermo A, Berti E, et al: Anthracycline-based chemotherapy
as primary treatment for intravascular lymphoma. Ann Oncol.
15:1215–1221. 2004. View Article : Google Scholar : PubMed/NCBI
|