Introduction
Brain metastases (BM), particularly those from
non-small cell lung cancer (NSCLC), constitute an increasing
proportion of the global cancer burden. It is estimated that 50% of
all patients with BM will experience a primary lung malignancy
(1). In patients with central nervous
system (CNS) metastases, the administration of standard
chemotherapies or targeted agents is limited due to low CNS
penetration of antineoplastic agents across the blood-brain barrier
(2).
However, in the last decade, several biological
agents targeting specific molecular alterations, including
gefitinib or erlotinib targeting epidermal growth factor receptor
(EGFR) mutations and crizotinib targeting anaplastic lymphoma
kinase (ALK) translocations, have been approved for clinical use
and used in personalized treatment regimes (3–7). Selected
molecular-targeted therapy for BM of lung cancer has been notably
effective, demonstrated by response rates, progression-free
survival and quality of life in small studies and case reports
(8–11); however, there are limited data
available regarding the differential genetic aberrations between
lung adenocarcinoma BM (LCBM) and primary lung cancer (LC)
(12).
Next-generation sequencing (NGS) technologies
provide an unprecedented opportunity to identify the clinically
actionable mutations relevant to personalized cancer care, and are
increasingly used for the mutational analysis of tumors for
clinical and research applications (13–15).
Targeted NGS permits the concurrent deep sequencing of hundreds of
cancer genes, and has emerged as a sensitive and efficient tool to
detect complex and heterogeneous gene mutations (16–18).
In the present study, targeted NGS was conducted to
detect potentially actionable genetic aberrations in LCBM as well
as primary LC, to provide target gene mutation profiles and an
improved understanding of the genetic mechanism underlying lung
cancer metastasis. The aim of the present study was to identify
novel and potentially beneficial therapeutic targets for patients
with BM.
Materials and methods
Patients
A total of 28 formalin-fixed, paraffin-embedded
(FFPE) tumor samples, including 13 cases of LC and 15 cases of
LCBM, were retrospectively collected from the archives of the
Pathology Laboratory in Huashan Hospital North in Fudan University
(Shanghai, China) between January 2013 and December 2015. There
were 10 unstained FFPE tissue sections (10 µm) that were cut for
DNA and RNA extraction. The pathologist identified the lesional
area and the percentage tumor cell content (minimum of 50%) for
each case, which were the areas microdissected for extraction.
Assessment of BM was concluded using all of the radiology reports,
which contained brain imaging or pathology.
DNA and RNA extraction from FFPE
samples
Genomic DNA was extracted from FFPE slices of solid
tumor using the QiagenQIAamp DNA FFPE kit (Qiagen, Inc., Valencia,
CA, USA), according to the manufacturer's protocol. DNA was eluted
with 40 µl elution buffer (10 mM Tris-Cl, pH 8.3; 0.1 mM EDTA;
0.04% NaN3). The concentration was measured using the
Qubit HS kit (Thermo Fisher Scientific, Inc., Waltham, MA, USA).
Total cellular RNA was extracted using the QiagenRNeasy FFPE kit,
according to the manufacturer's protocol with minor modifications
as specified below (Qiagen, Inc.). A total of 1 ml xylene was added
to the 1.5 ml tube containing the FFPE tissue. The tube was
vortexed vigorously for 10 sec and centrifuged at 21,130 × g for 2
min at 25°C. The supernatant was carefully removed using a pipette.
Then 1 ml ethanol (96–100%) was added into the tube, followed by
vigorous vortexing followed by centrifugation at 21,130 × g for 2
min at 25°C. The above step was repeated once. Then, the ethanol
was carefully removed. The tube was kept open at room temperature
(15–25°C) for 10 min until all residual ethanol evaporated. Then,
the manufacturer's protocol (Qiagen, Inc.) was followed, adding 150
µl Buffer PKD and following the remaining steps in order to obtain
RNA. The RNA concentration was measured with the Qubit®
RNA kit (Thermo Fisher Scientific, Inc.), and RNA integrity was
evaluated using RNA gel electrophoresis (1% agarose gel in 0.5% TBE
buffer, running for 35 min at a 120 v voltage; with a ratio of 28S
rRNA to 18S rRNA of ~2:1). Reverse transcription of RNA to cDNA was
conducted using the SuperScript™ VILO™ cDNA synthesis kit (Thermo
Fisher Scientific, Inc.), and was followed by library
construction.
Sequencing library construction
The OncoAim™ cancer panel (Singlera Genomics, Inc.,
Shanghai, China) was used with the recommended DNA input (20 ng for
FFPE samples) to generate sequencing libraries compatible with
MiSeq system Dx (DX-410-1001; llumina, Inc., San Diego, CA, USA).
The panel included 400 amplicons targeting cancer hotspots, the
specific genetic loci of which were depicted on the website of the
Singlera Genomics, Inc. (Shanghai, China; http://www.singlera.com.cn/product/index.aspx?pid=1).
The targeted regions were amplified using the customized OncoAim™
cancer panel followed by the addition of P5/P7 dual barcode
adapters (Illumina, Inc.).
In addition, 20 ng reverse transcribed cDNA was
amplified with the OncoAim™ RNA fusion panel (Singlera Genomics,
Inc.) to generate sequencing libraries compatible with MiSeq. The
panel included 170 amplicons targeting fusion events for ALK, Ret
proto-oncogene, proto-oncogene c-Ros1 and neurotrophic receptor
tyrosine kinase, along with five genes (hydroxymethulbilane
synthase, integrin subunit β 7, lamin A/C, MYC proto-oncogene, bHLH
transcription factor and TATA-box binding protein) as internal
expression controls. Fusion variants, if present, were enriched by
the customized OncoAim™ RNA fusion panel followed by a P5/P7
addition (Illumina, Inc.).
LabChip® GX Touch (PerkinElmer, Inc.,
Waltham, MA, USA) was used to confirm successful library
amplifications to a desired length (~220 bp), and library
concentration was assessed using the Qubit™ HS kit (Thermo Fisher
Scientific, Inc.). No detectable DNA in the library prepared from
non-template control (negative control) was used to indicate that
no DNA contamination was introduced during library preparation.
There were 12–16 barcoded libraries that were pooled. The ratios
were confirmed and quantified by qPCR using KAPA Library
Quantification kit (Kapa Biosystems, Inc., Wilmington, MA, USA)
following the manufacturer's protocol, using the Bio-Rad CFX96 qPCR
system (Bio-Rad Laboratories, Inc., Hercules, CA, USA). The KAPA
Library Quantification kit uses the novel KAPA SYBR FAST DNA
Polymerase, engineered through a process of directed evolution for
high-performance SYBR Green I-based qPCR (Kapa Biosystems, Inc.,
Wilmington, MA, USA). The qPCR primers are
5′-AATGATACGGCGACCACCGA-3′ and 5′-CAAGCAGAAGACGGCATACGA-3′. The PCR
cycling conditions were: initial denaturation: 95°C for 5 min;
cycling: 35 cycles of 95°C for 30 sec and 60°C for 45 sec. The
library concentration was calculated against the standard curve
generated from 6 standards using qPCR software on the Bio-Rad CFX96
qPCR system (CFX Maestro software 12004110; Bio-Rad Laboratiories,
Inc.).
Data processing
A bioinformatic analysis pipeline was created using
a corresponding OncoAim™ cancer panel pipeline (OncoAim™ version
7.2) and OncoAim™ RNA fusion panel pipeline (OncoAim™ RNA version
3.1). Briefly, raw reads (fastq files) were quality-filtered with
FastQC version 0.9.5 (Babraham Bioinformatics, Cambridge, UK) and
base quality score recalibration was performed. Clean reads were
assembled and aligned against the reference genome hg19, or the
targeted fusion reference to detect sequence/structure variations.
The Burrow-Wheeler Aligner algorithm (https://github.com/lh3/bwa; version 0.7.12-r1039; Dec
2015) was implemented into the procedure for alignment, using
default parameters. Insertions and deletions in sequence alignment
files were left-aligned, and local realignment was conducted with
the Genome Analysis Toolkit (https://github.com/broadgsa/gatk; Broad Institute,
Cambridge, MA, USA) and Freebayes (https://github.com/ekg/freebayes; version
0.9.21–26-gbfd9832). Unique reads derived from the GATK were used
for variant calling. All samples were processed in parallel, and
each sample had split individual variant files. The median
coverage/locus was 500–1,000 to ensure confident variant calling.
The minimum confidence threshold for variant and insertion/deletion
(indel) calling was set to 0.05 (5%). Single nucleotide changes
(SNC) and indels were separately evaluated. Fusion transcripts were
normalized to total mapped reads to calculate the CP100 K
(counts/100,000 mapped reads), for a fair comparison across
different libraries. Variation annotation, effect prediction and
clinical practice guidance, including The National Comprehensive
Cancer Network (www.nccn.org), were integrated into
the OncoAim™ cancer panel pipeline through vcf files. Additionally,
descriptive statistics and data visualization were performed using
Microsoft Excel 2010 (Microsoft Corporation, Redmond, WA, USA) and
R packages (version 3.4.1; http://cran.r-project.org/src/base/R-3/R-3.4.1.tar.gz).
The Integrative Genomics Viewer (version 2.3.94, Broad Institute)
was used for visualization and confirmation of specific SNC/indel
loci.
Confirmation of mutations using Sanger
sequencing
A total of 2 samples with novel tumor protein (TP)53
mutations were selected from targeted NGS for validation testing
using primer-specific PCR and Sanger sequencing. Sanger sequencing
was performed using a DNA direct sequencing company (Sangon Biotech
Co., Ltd., Shanghai, China). TP53-p.V166_H169del primer: forward,
5′-GTTTCTTTGCTGCCGTCTTC-3′ and reverse, 5′-CTTAACCCCTCCTCCCAGAG-3′.
TP53-7577157-63del TACTCAG primer: Forward,
5′-CTTGGGCCTGTGTTATCTCC-3′ and reverse,
5′-TAACTGCACCCTTGGTCTCC-3′.
Statistical analysis
Descriptive statistics were calculated with
Microsoft Excel 2010 (Microsoft Corp, Redmond, Wash). The data were
described as the number of mutations. All statistical tests were
performed using IBM SPSS Statistics version 19 (IBM Corp., Armonk,
NY, USA). The χ2 test or Fisher's exact test was used to
calculate the P-values for the detected number of mutations or the
frequency of mutated genes between LC and LCBM samples. P<0.05
was considered to indicate a statistically significant
difference.
Results
Patient characteristics
Characteristics of the 13 patients with LC and 15
patients with LCBM are presented in Table
I. The median age of patients diagnosed with LC and LCBM was 61
years (range, 50–74 years) and 55 years (range, 35–65 years),
respectively. Overall, 57% of patients (16 cases) were male, and
the majority of patients (24 cases) did not have a history of
smoking. The majority of patients (89.3%, 25/28) were diagnosed in
advanced (tumor-node-metastasis III and IV) stages (19).
 | Table I.Baseline characteristics of all
patients (n=28). |
Table I.
Baseline characteristics of all
patients (n=28).
| Characteristics | LC (n=13) | LCBM (n=15) |
|---|
| Age, years |
|
|
|
Median | 61 | 55 |
|
Range | 50–74 | 35–65 |
| Sex |
|
|
|
Male | 9 | 7 |
|
Female | 4 | 8 |
| Smoking
history |
|
|
| Never
smoked | 9 | 15 |
| Have
smoked | 4 | 0 |
|
Pathological diagnosis | LC | LCBM |
| TNM stage |
|
|
|
Ia-IIb | 3 | 0 |
|
IIIa-IIIb | 10 | 0 |
| IV |
| 15 |
| BM | No | Yes |
NGS
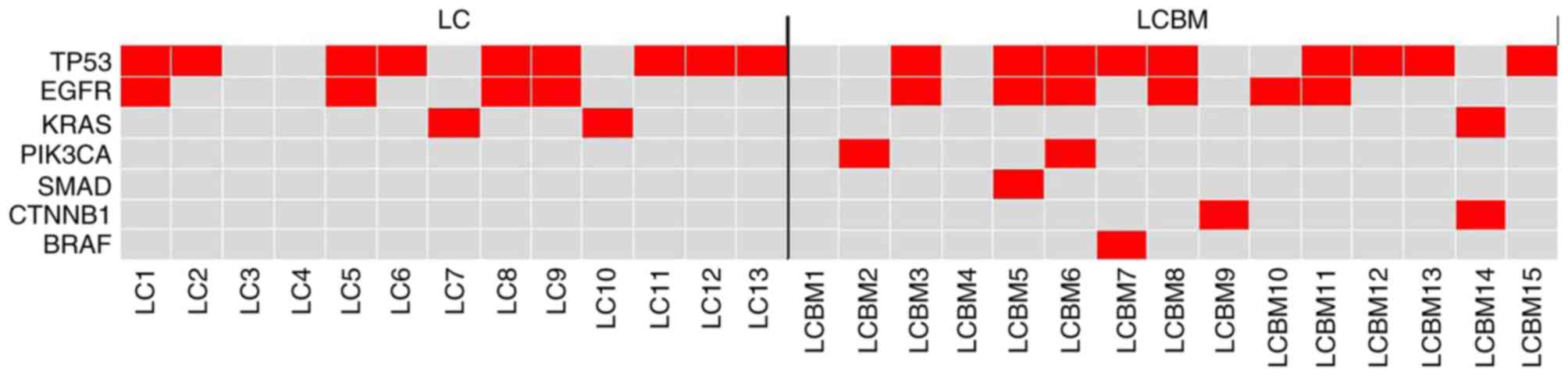
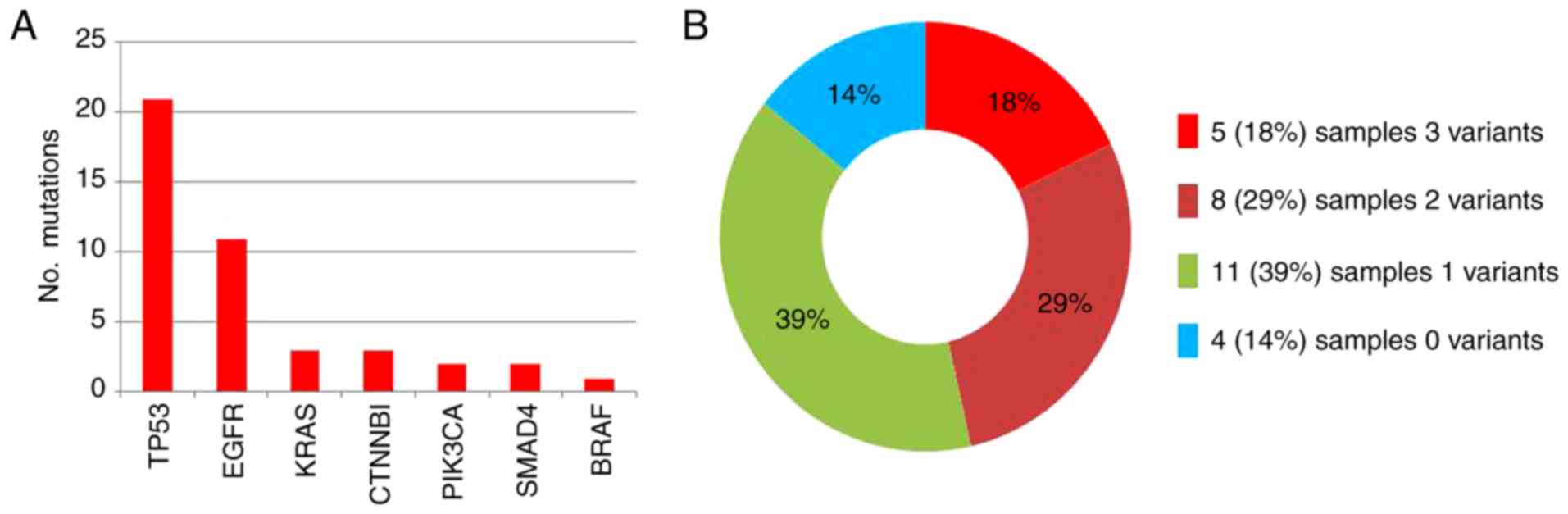
A total of 28 samples were successfully sequenced.
Table II presents the results of NGS
of 28 samples with the OncoAim™ cancer panel and the presence of
each sample gene mutation can be observed in Fig. 1. The mutated genes in these 28 samples
were TP53, EGFR, Kirsten rat sarcoma viral oncogene homolog (KRAS),
catenin β1 (CTNNB1), phosphatidylinositol-4,5-bisphosphate 3-kinase
catalytic subunit α (PIK3CA), mothers against decapentaplegic
homolog 4 (SMAD4) and proto-oncogene B-Raf (BRAF). The number of
mutant genes are summarized in Fig.
2A, and were identified in 21/28 (75.0%), 11/28 (39.3%), 3/28
(10.7%), 3/28 (10.7%), 2/28 (7.1%), 2/28 (7.1%) and 1/28 (3.6%) of
samples, respectively. Overall, 43 variants in the 7 genes were
observed. These 43 genomic variant aberrations included 36 base
substitutions and 7 short deletions. A total of 5 samples (5/28,
18%) exhibited 3 potentially biologically significant variants, 8
samples (8/28, 29%) exhibited 2 variants, 11 samples (11/28, 39%)
exhibited only a single variant, and 4 samples (4/28, 14%)
exhibited no alterations (Fig. 2B).
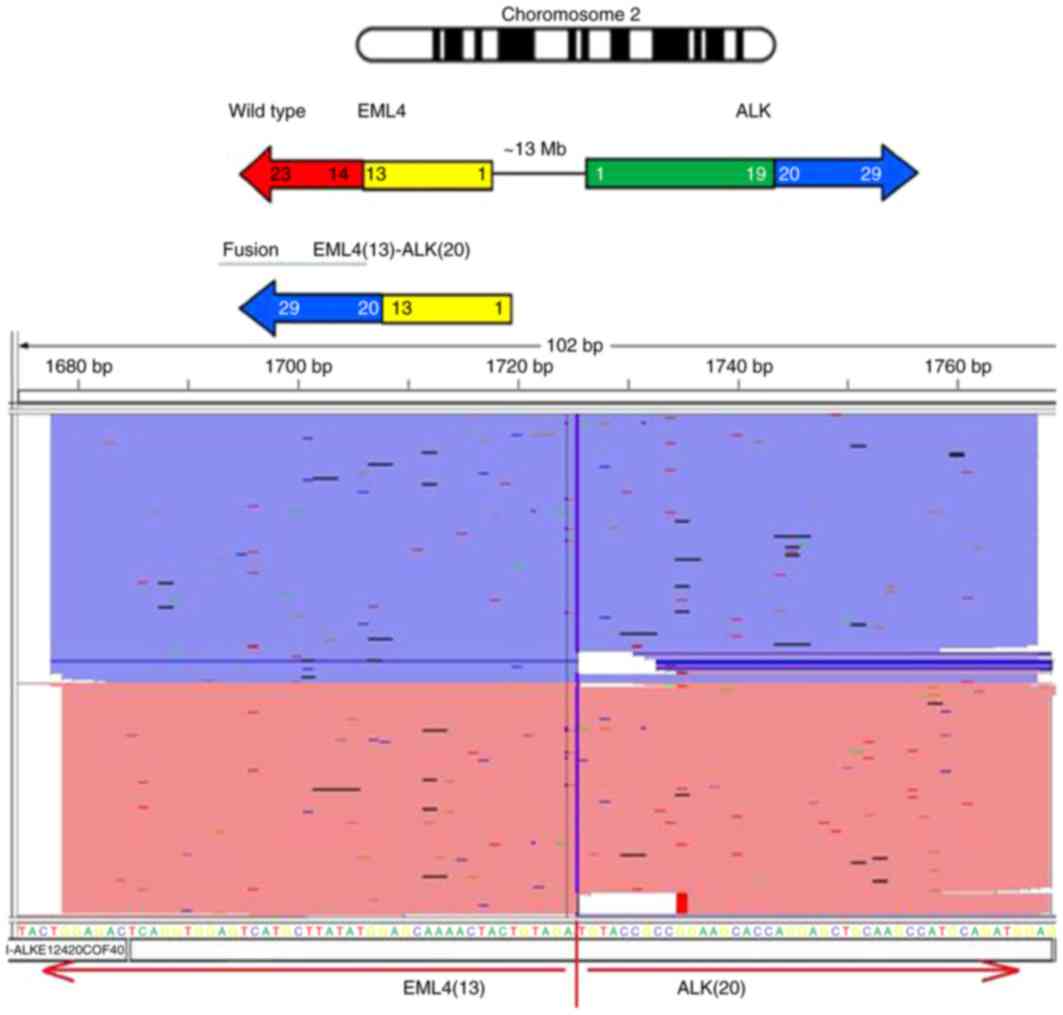
The average number of variants was 1.5/tumor. The RNA fusion panel
tests revealed only echinoderm microtubule associated protein like
4 [EML4 (13)]-ALK (20) in 1sample of LCBM (Fig. 3).
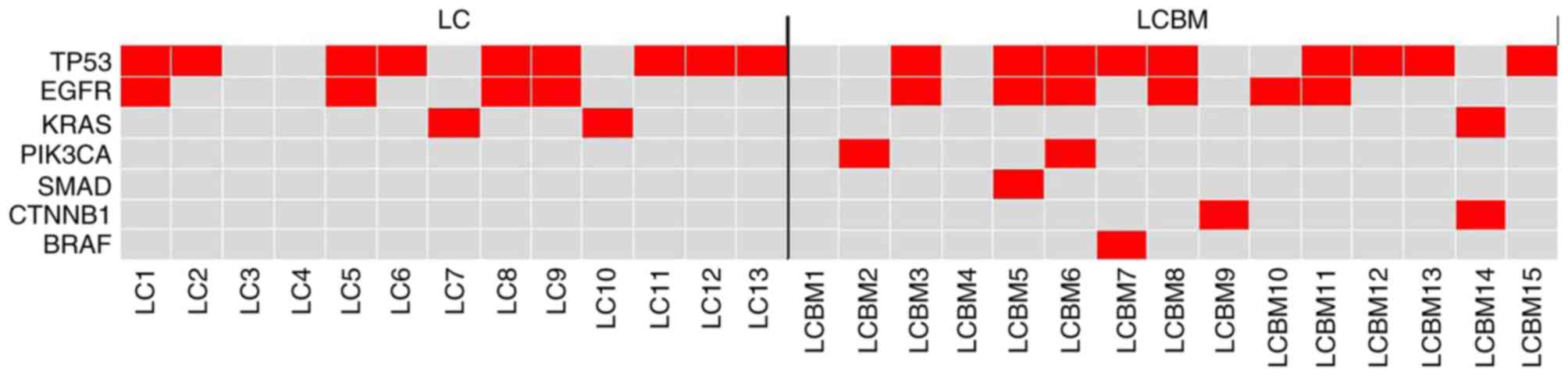 | Figure 1.Heat map depicting the somatic
mutations identified in each sample. Red indicates variants,
whereas gray indicates no variants detected. The y-axis indicates
the gene name and the x-axis indicates the identification of the
matched pairings, including 13 samples of LC and 15 samples of
LCBM. LCBM, lung adenocarcinoma brain metastasis; TP53, tumor
protein 53; EGFR, epithelial growth factor receptor; CTNNB1,
catenin-β1; KRAS, Kirsten rat sarcoma viral oncogene; PIK3CA,
phosphatidylinositol-4,5-bisphosphate 3-kinase; BRAF,
proto-oncogene B-Raf; SMAD4, mothers against decapentaplegic
homolog 4. |
 | Table II.Mutation profiles in 28 clinical
samples. |
Table II.
Mutation profiles in 28 clinical
samples.
| Mutant gene | LC (n=13) | LCBM (n=15) | Mutation
frequency |
|---|
| TP53 |
|
| 21/28 |
|
p.T125T | 1 |
|
|
|
p.P151A |
| 1 |
|
|
p.V173L | 1 |
|
|
|
p.R175H |
| 2 |
|
|
p.C176F | 1 |
|
|
|
p.E180G | 4 | 1 |
|
|
p.D207G |
| 1 |
|
|
p.Y234C | 1 |
|
|
|
p.Y236Y |
| 1 |
|
|
p.M237V | 1 |
|
|
|
p.G245C |
| 1 |
|
|
p.T253I | 1 |
|
|
|
p.R267P |
| 1 |
|
|
p.R273L | 1 |
|
|
|
p.V166_H169del |
| 1 |
|
| 7577157-63del
TACTCAG |
| 1 |
|
| EGFR |
|
| 11/28 |
| Exon21 |
|
|
|
|
p.L858R | 1 | 4 |
|
| Exon19 |
|
|
|
|
p.L747_T751del LREAT | 1 |
|
|
|
p.E746_A750del ELREA | 2 | 2 |
|
| Exon18 |
|
|
|
|
p.G719A | 1 |
|
|
| KRAS |
|
| 3/28 |
|
p.Q61L | 1 |
|
|
|
p.G12D | 1 |
|
|
|
p.G12C |
| 1 |
|
| CTNNB1 |
|
| 3/28 |
|
p.D32V |
| 1 |
|
|
p.S37C |
| 1 |
|
|
p.S45F |
| 1 |
|
| PIK3CA |
|
| 2/28 |
|
p.W1051a |
| 1 |
|
|
p.E545K |
| 1 |
|
| SMAD4 |
|
| 2/28 |
|
p.L533R |
| 2 |
|
| BRAF |
|
| 1/28 |
|
p.V600E |
| 1 |
|
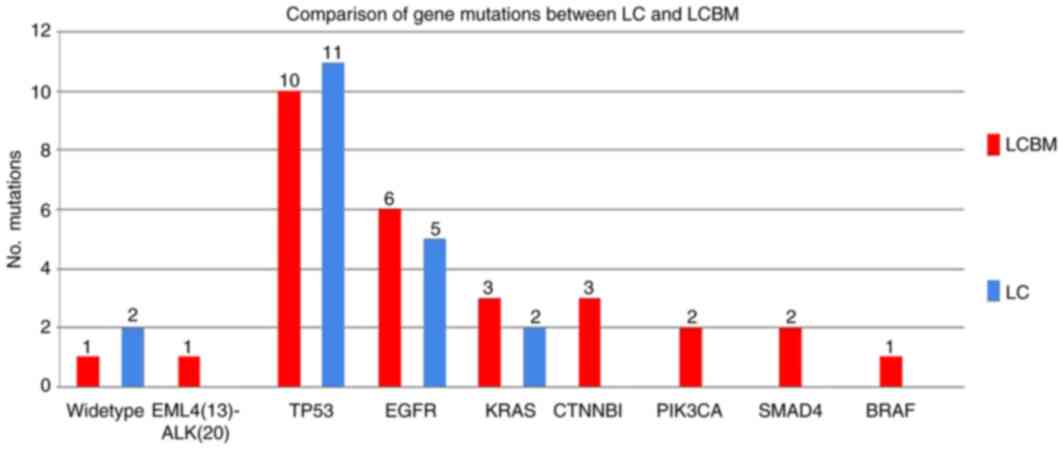
Comparison of gene mutations between
LC and LCBM
The mutated genes in LCBM tissues were TP53, EGFR,
CTNNB1, PIK3CA, SMAD4, KRAS and BRAF, which were identified in
10/15 (66.7%), 6/15 (40.0%), 3/15 (20.0%), 2/15 (13.3%), 2/15
(13.3%), 1/15 (6.7%) and 1/15 (6.7%) of samples, respectively. The
mutated genes of LC were TP53, EGFR and KRAS, which were exhibited
in 11/13 (84.6%), 5/13 (38.5%) and 2/13 (18.2%) of samples,
respectively. EML4-ALK rearrangement existed in 1 LCBM sample. A
total of 2 LC samples and 1 LCBM sample exhibited no genetic
alterations (Fig. 4). No significant
differences were identified in the number of mutations or the
frequency of TP53, EGFR or KRAS between patients with LC (n=13) and
patients with LCBM (n=15; P>0.05).
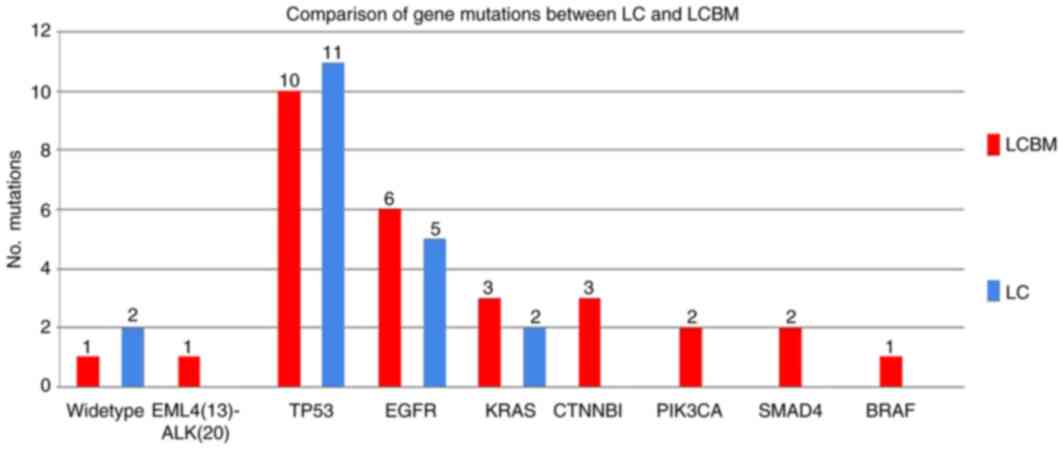 | Figure 4.Variant frequency detected by next
generation sequencing in 28 formalin-fixed, paraffin-embedded
samples sub-grouped by LC and LCBM. CTNNB1, PI3KCA, SMAD4, BRAF and
EML4-ALK mutations were present in the metastatic lesions in 3/15,
2/15, 2/15, 1/15 and 1/15 LCBM cases, but not in primary LC. LCBM,
lung adenocarcinoma brain metastasis; LC, lung adenocarcinoma;
TP53, tumor protein 53; EGFR, epithelial growth factor receptor;
CTNNB1, catenin-β1; KRAS, Kirsten rat sarcoma viral oncogene;
PIK3CA, phosphatidylinositol-4,5-bisphosphate 3-kinase gene; BRAF,
proto-oncogene B-Raf; EML4, echinoderm microtubule associated
protein Like 4; ALK, anaplastic lymphoma kinase; SMAD4, mothers
against decapentaplegic homolog 4. |
Novel TP53 gene mutations in LCBM and
mutation verification by Sanger sequencing
The LCBM-7 and LCBM-11 samples exhibited a novel
TP53 mutation form p.V166_H169del and a new splice site mutation
for 7577157-63del TACTCAG, respectively, located in the non-coding
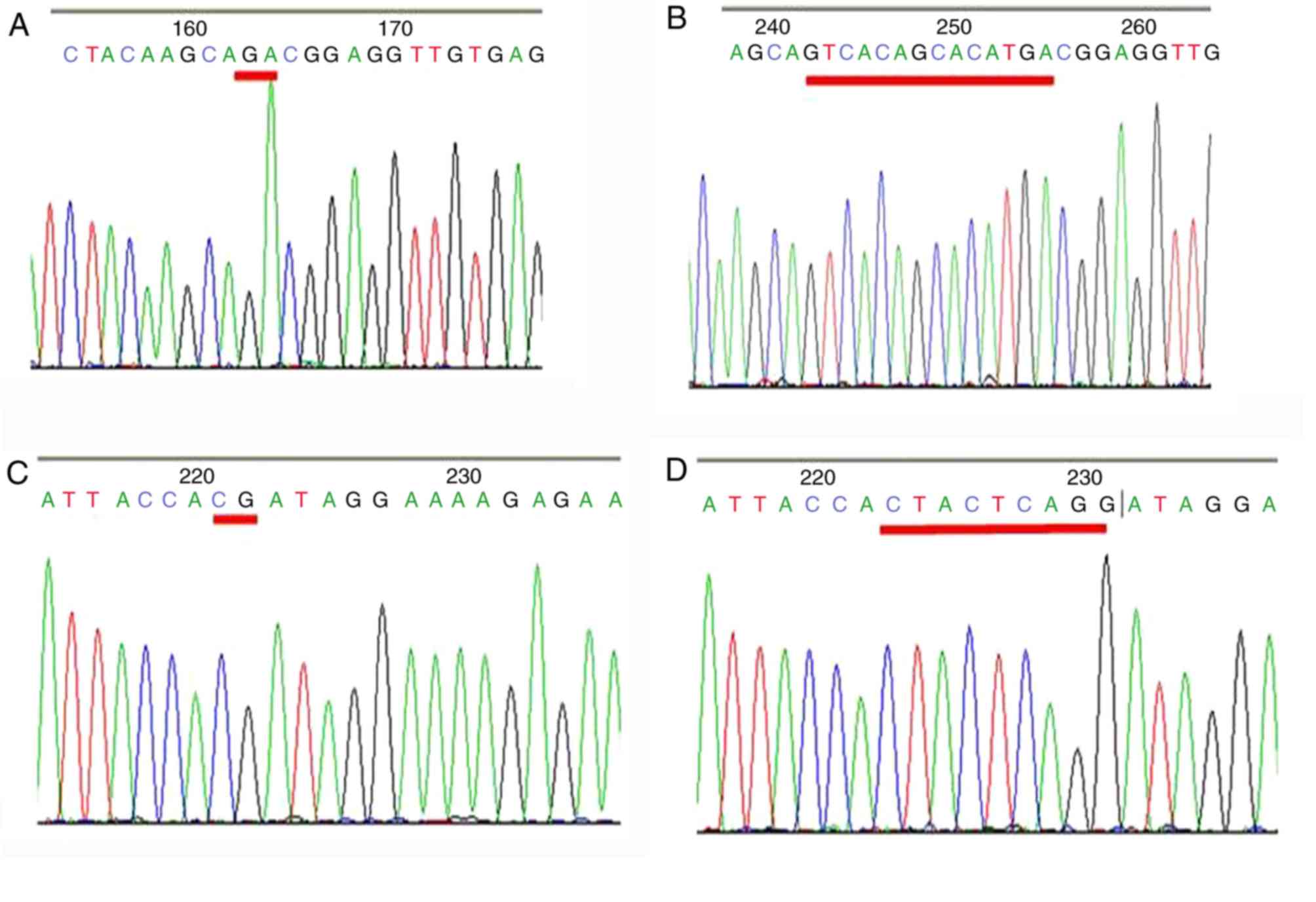
regions. Fig. 5A depicts the Sanger
sequencing chromatograms of p.V166_H169del compared with the
wild-type (Fig. 5B). Fig. 5C depicts the Sanger sequencing
chromatograms of 7577157-63del TACTCAG compared with the wild-type
(Fig. 5D).
Discussion
Lung cancer is the most common cause of
cancer-associated mortality globally, and 80–85% of these cases are
NSCLC (20). In total, 10–50% of
patients with NSCLC develop BM (21).
Treatment options are palliative, and usually include a combination
of steroids, radiation and surgery (22). Despite advances in cancer therapy, the
median survival time for patients with lung cancer BM is only 6–11
months (23). The poor prognosis
associated with disseminated disease that has metastasized to the
brain is not addressed by existing therapies. Efforts to develop
improved personalized therapies and prognostic biomarkers must be
driven by the understanding of the mechanisms underlying this
disease. In the present study, a genetic alteration profile of the
BM was produced, as well as for primary LC, with the intention of
identifying potential biomarkers associated with brain metastasis
from lung cancer. Currently, limited numbers of biomarkers possess
the potential to be used clinically for BM, however a large number
of promising candidate biomarkers are being evaluated in current
studies, and may soon become relevant for clinical practice
(12).
The targeted NGS analysis of 15 tumor samples from
patients with LCBM as well as 13 patients with primary LC revealed
that 14/15 (93.3%) patients exhibited ≥1 somatic molecular
activating mutation and 11/13 (84.6%) had ≥1 molecular aberration.
The most frequent genomic alterations in these types of cancer were
TP53 (11 for LC, 10 For LCBM), KRAS (1 for LC, 2 for LCBM) and EGFR
(5 for LC, 6 for LCBM). Notably, mutations in CTNNB1, BRAF, SMAD4
and PIK3CA were identified only in LCBM, although their frequencies
were low.
In the present study, 60.7% (17/28) of the lung
cancer samples analyzed exhibited a TP53 mutation, which is higher
than that reported in a number of studies from Western countries
(24,25). This discrepancy may be explained by
relatively few early-stage samples being analyzed in the present
cohort. Lung cancer tissues exhibiting EGFR mutations have
demonstrated success in responding to EGFR tyrosine kinase
inhibitors (26,27). An equal distribution of EGFR mutations
in exon 19 (5/28) and the L858R point mutation in exon 21 (5/28)
were identified in the present study, followed by the p.G719A point
mutation in exon 8 (1/28).
KRAS mutations were observed in patients with LC in
a previous study; KRAS and other driver mutations, including EGFR,
human epidermal growth factor receptor 2 and BRAF, being mutually
exclusive, as KRAS mutations may represent negative predictive
biomarkers for tumor responses in patients with NSCLC treated with
EGFR-TKIs (28). Whereas EGFR
mutations were identified more frequently in never-smokers, KRAS
mutations were first identified among patients who reported greater
tobacco use (29). KRAS mutations
were identified in 20–30% of patients with lung cancer in North
American populations (30). The
prevalence of KRAS mutations in the present study was less than
that observed in the Caucasian group. Similarly, a recent study
also identified KRAS mutations in 8.3% (113/1,368) of a patient
cohort with LC (31). In the present
study, BRAF and PIK3CA mutations were identified in a small
proportion of patients with LCBM, however were not exhibited in
patients with LC. However, these results do not imply that these
mutations are associated with BM in patients with lung cancer as
mutations of BRAF (11) and PIK3CA
(32) have been identified in a
variety of brain tumors and BM; however, to the best of our
knowledge, SMAD4 and CTNNB1 mutations have not previously been
identified in brain tumors. Mutations of SMAD4 have been identified
primarily in pancreatic and colorectal cancer, and among other
types of cancer only occasionally (≤7% in lung cancer) (33). SMAD4 L533R is a pathogenic mutation,
which was first identified in juvenile polyposis (34). Inactivation of SMAD4 was considered to
serve an important function in impairing transforming growth factor
(TGF)-β signaling. Yu et al (35) reported that activation of the
TGF-β/SMAD signaling pathway promotes LC metastasis by enhancing
the ability of LC cells to extravasate into distant organs. It is
reasonable to consider that SMAD4 is also involved in LCBM.
Mutational analysis of exon 3 of CTNNB1 in the
present study identified p.S45F, p.S37C and p.D32V mutations. These
mutations caused amino acid substitutions in 3/15 LCBM samples
(Ser33Phe, Ser33Cys and Ser37Cys). The mutations in exon 3 of
CTNNB1 affected glycogen synthase kinase-3β phosphorylation sites
of the degradation-targeting box of CTNNB1 and resulted in nuclear
CTNNB1 protein accumulation (36).
Notably, CTNNB1 mutations were detected in BM from primary LC, in
the present study. This finding is consistent with a recent study
by Mäki-Nevala et al (37),
which demonstrated that CTNNB1 mutations located at codon 37 were
detected in two specimens of LCBM. If codons 33 and 37 are a
possible location for a number of CTNNB1 mutations in LCBM, this
would indicate that CTNNB1 mutations may be important for a
secondary event during cancer progression in a carcinogen-specific
manner.
There were two novel types of TP53 deletion
mutations in LCBM identified in the present study, the TP53
c.495_506del 12 (p.V166_H169del VTAH) and TP53 intron region
(7577157-63del TACTCAG), which were validated by Sanger sequencing.
Han et al (38) revealed a
deletion of two bases, which altered glutamine 167 to alanine, and
the resulting frame-shift produced an in-frame stop codon located
at amino acid 179 in a human colon cancer cell line (HCC 278). This
mutation may be associated with “slippage” or misalignment during
DNA replication, due to the occurrence of the CA dinucleotide four
times within a stretch of 12 bases (codons 166–169). A novel TP53
gene splice variant was observed in the present study, a 7-base
deletion at position 7577157-63 at the splice site of intron 7,
which may affect the splice site of exon 8. Although splice sites
in TP53 are not typical mutation sites, there is evidence that TP53
splicing mutations lead to exon dropping, indicating a biological
relevance (39). Whether these two
novel mutations serve a function in BM of lung cancer should be
subject to further investigation.
There are several limitations to the present study.
The sample size was small, and the retrospective design hindered
the ability to study more clinically relevant outcomes, including
personalized treatment success, due to the rarity of BM specimens.
The NGS approach is designed to detect actionable mutations,
including single nucleotide variants, insertions and deletions;
however, copy number variants, including gene amplifications and
structural variants/rearrangements, are detected less frequently.
Therefore, the data acquired may underestimate the mutation burden
for the cases. There was no opportunity to investigate matched
primary tumors or to analyze in detail intra-patient differences in
the mutation status of these genes between tumor sites.
In conclusion, NGS demonstrated a high-throughput in
mutational analysis for the patients with LCBM, calculated by
detecting the molecular alterations that have a potential clinical
relevance. Such findings may assist in clinical decision-making
regarding therapeutic intervention for individual patients and
provide improved diagnosis or prognosis.
Acknowledgements
The present study was supported by the Research Fund
for Shanghai Leading Talents (2015–2017).
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Mulvenna PM: The management of brain
metastases in patients with non-small cell lung cancer is it time
to go back to the drawing board? Clin Oncol (R Coll Radiol).
22:365–373. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ting CY, Fan CH, Liu HL, Huang CY, Hsieh
HY, Yen TC, Wei KC and Yeh CK: Concurrent blood-brain barrier
opening and local drug delivery using drug-carrying microbubbles
and focused ultrasound for brain glioma treatment. Biomaterials.
33:704–712. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Cardarella S and Johnson BE: The impact of
genomic changes on treatment of lung cancer. Am J Respir Crit Care
Med. 188:770–775. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lindman NI, Cagle PT, Beasley MB, Chitale
DA, Dacic S, Giaccone G, Jenkins RB, Kwiatkowski DJ, Saldivar JS,
Squire J, et al: Molecular testing guidelines for selection of lung
cancer patients for EGFR and ALK tyrosine kinase inhibitors:
Guideline from the College of American Pathologists, International
Association for the Study of Lung Cancer, and Association for
Molecular Pathology. J Thorac. 8:823–859. 2013. View Article : Google Scholar
|
|
5
|
Tartarone A, Lazzari C, Lerose R,
Conteduca V, Improta G, Zupa A, Bulotta A, Aieta M and Gregorc V:
Mechanisms of resistance to EGFR tyrosine kinase inhibitors
gefitinib/erlotinib and to ALK inhibitor crizotinib. Lung Cancer.
81:328–336. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lindeman NI, Cagle PT, Beasley MB, Chitale
DA, Dacic S, Giaccone G, Jenkins RB, Kwiatkowski DJ, Saldivar JS,
Squire J, et al: Molecular testing guideline for selection of lung
cancer patients for EGFR and ALK tyrosine kinase inhibitors:
guideline from the College of American Pathologists, International
Association for the Study of Lung Cancer, and Association for
Molecular Pathology. Arch Pathol Lab Med. 137:828–860. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Shaw AT, Ou SH, Bang YJ, Camidge DR,
Solomon BJ, Salgia R, Riely GJ, Varella-Garcia M, Shapiro GI, Costa
DB, et al: Crizotinib in ROS1-rearranged non-small-cell lung
cancer. N Engl J Med. 371:1963–1971. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Zer A and Leighl N: Promising targets and
current clinical trials in metastatic non-squamous NSCLC. Front
Oncol. 4:3292014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Welsh JW, Komaki R, Amini A, Munsell MF,
Unger W, Allen PK, Chang JY, Wefel JS, McGovern SL, Garland LL, et
al: Phase II trial of erlotinib plus concurrent whole-brain
radiation therapy for patients with brain metastases from
non-small-cell lung cancer. J Clin Oncol. 31:895–902. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Gadgeel SM, Gandhi L, Riely GJ, Chiappori
AA, West HL, Azada MC, Morcos PN, Lee RM, Garcia L, Yu L, et al:
Safety and activity of alectinib against systemic disease and brain
metastases in patients with crizotinib-resistant ALK-rearranged
non-small-cell lungcancer (AF-002JG): Results from the dose-finding
portion of aphase 1/2 study. Lancet Oncol. 15:1119–1128. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Robinson SD, O'Shaughnessy JA, Cowey CL
and Konduri K: BRAF V600E-mutated lung adenocarcinoma with
metastases to the brain responding to treatment with vemurafenib.
Lung Cancer. 85:326–330. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Preusser M, Berghoff AS, Koller R,
Zielinski CC, Hainfellner JA, Liebmann-Reindl S, Popitsch N, Geier
CB, Streubel B and Birner P: Spectrum of gene mutations detected by
next generation exome sequencing in brain metastases of lung
adenocarcinoma. Eur J Cancer. 51:1803–1811. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ellis MJ, Ding L, Shen D, Luo J, Suman VJ,
Wallis JW, Van Tine BA, Hoog J, Goiffon RJ, Goldstein TC, et al:
Whole-genome analysis informs breast cancer response to aromatase
inhibition. Nature. 486:353–360. 2012.PubMed/NCBI
|
|
14
|
Boland GM, Piha-Paul SA, Subbiah V,
Routbort M, Herbrich SM, Baggerly K, Patel KP, Brusco L, Horombe C,
Naing A, et al: Clinical next generation sequencing to identify
actionable aberrations in a phase I program. Oncotarget.
6:20099–20110. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Movva S, Wen W, Chen W, Millis SZ,
Gatalica Z, Reddy S, von Mehren M and Van Tine BA: Multi-platform
profiling of over 2000 sarcomas: Identification of biomarkers and
novel therapeutic targets. Oncotarget. 6:12234–12247. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Sie D, Snijders PJ, Meijer GA, Doeleman
MW, van Moorsel MI, van Essen HF, Eijk PP, Grünberg K, van Grieken
NC, Thunnissen E, et al: Performance of amplicon-based next
generation DNA sequencing for diagnostic gene mutation profiling in
oncopathology. Cell Oncol (Dordr). 37:353–361. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hagemann IS, Devarakonda S, Lockwood CM,
Spencer DH, Guebert K, Bredemeyer AJ, Al-Kateb H, Nguyen TT,
Duncavage EJ, Cottrell CE, et al: Clinical next-generation
sequencing in patients with non-small cell lung cancer. Cancer.
121:631–639. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Frampton GM, Fichtenholtz A, Otto GA, Wang
K, Downing SR, He J, Schnall-Levin M, White J, Sanford EM, An P, et
al: Development and validation of a clinical cancer genomic
profiling test based on massively parallel DNA sequencing. Nat
Biotechnol. 31:1023–1031. 2013. View
Article : Google Scholar : PubMed/NCBI
|
|
19
|
Detterbeck FC, Boffa DJ, Kim AW and Tanoue
LT: The 8th edition lung cancer stage classification. CHEST.
151:193–203. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Torre LA, Bray F, Siegel RL, Ferlay J,
Lortet-Tieulent J and Jemal A: Global cancer statistics, 2012. CA
Cancer J Clin. 65:87–108. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Bailon O, Kallel A, Chouahnia K, Billot S,
Ferrari D and Carpentier AF: Management of brain metastases from
non-small cell lung carcinoma. Rev Neurol (Paris). 167:579–591.
2011.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Lemjabbar-Alaoui H, Hassan OU, Yang YW and
Buchanan P: Lung cancer: Biology and treatment options. Biochim
Biophys Acta. 1856:189–210. 2015.PubMed/NCBI
|
|
23
|
Andrews DW, Scott CB, Sperduto PW,
Flanders AE, Gaspar LE, Schell MC, Werner-Wasik M, Demas W, Ryu J,
Bahary JP, et al: Whole brain radiation therapy with or without
stereotactic radio surgery boost for patients with one to three
brain metastases: Phase III results of the RTOG 9508 randomised
trial. Lancet. 363:1665–1672. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Cancer Genome Atlas Research Network, .
Comprehensive molecular profiling of lung adenocarcinoma. Nature.
511:543–550. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Imielinski M, Berger AH, Hammerman PS,
Hernandez B, Pugh TJ, Hodis E, Cho J, Suh J, Capelletti M,
Sivachenko A, et al: Mapping the hallmarks of lung adenocarcinoma
with massively parallel sequencing. Cell. 150:1107–1120. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Dienstmann R, Rodon J, Barretina J and
Tabernero J: Genomic medicine frontier in human solid tumors:
Prospects and challenges. J Clin Oncol. 31:1874–1884. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Russo A, Franchina T, Ricciardi GR, Picone
A, Ferraro G, Zanghì M, Toscano G, Giordano A and Adamo V: A decade
of EGFR inhibition in EGFR-mutated non small cell lung cancer
(NSCLC): Old successes and future perspectives. Oncotarget.
6:26814–26825. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Mao C, Qiu LX, Liao RY, Du FB, Ding H,
Yang WC, Li J and Chen Q: KRAS mutations and resistance to
EGFR-TKIs treatment in patients with non-small cell lung cancer: A
meta-analysis of 22 studies. Lung Cancer. 69:272–278. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Riely GJ, Kris MG, Rosenbaum D, Marks J,
Li A, Chitale DA, Nafa K, Riedel ER, Hsu M, Pao W, et al: Frequency
and distinctive spectrum of KRAS mutations in never smokers with
lung adenocarcinoma. Clin Cancer Res. 14:5731–5734. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Arrieta O, Cardona AF, Martín C, Más-López
L, Corrales-Rodríguez L, Bramuglia G, Castillo-Fernandez O,
Meyerson M, Amieva-Rivera E, Campos-Parra AD, et al: Updated
frequency of EGFR and KRAS mutations in non-small-cell lung cancer
in Latin America: The Latin-American Consortium for the
Investigation of Lung Cancer (CLICaP). J Thorac Oncol. 10:838–843.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Zheng D, Wang R, Zhang Y, Pan Y, Cheng X,
Cheng C, Zheng S, Li H, Gong R, Li Y, et al: The prevalence and
prognostic significance of KRAS mutation subtypes in lung
adenocarcinomas from Chinese populations. Onco Targets Ther.
9:833–843. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Paik PK, Shen R, Won H, Rekhtman N, Wang
L, Sima CS, Arora A, Seshan V, Ladanyi M, Berger MF and Kris MG:
Next generation sequencing of stage IV squamous cell lung cancers
reveals an association of PI3K aberrations and evidence of clonal
heterogeneity in patients with brain metastases. Cancer Discov.
5:610–621. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Yanagisawa K, Uchida K, Nagatake M, Masuda
A, Sugiyama M, Saito T, Yamaki K, Takahashi T and Osada H:
Heterogeneities in the biological and biochemical function of Smad2
and Smad4 mutants naturally occurring in human lung cancers.
Oncogene. 19:2305–2311. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Gallione CJ, Repetto CJ, Legius E, Rustgi
AK, Schelley SL, Tejpar S, Mitchell G, Drouin E, Westermann CJ and
Marchuk DA: A combined syndrome of juvenile polyposis and
hereditary haemorrhagic telangiectasia associated with mutations in
MADH4 (SMAD4). Lancet. 363:852–859. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Yu JR, Tai Y, Jin Y, Hammell MC, Wilkinson
JE, Roe JS, Vakoc CR and Van Aelst L: TGF-β/Smad signaling through
DOCK4 facilitates lung adenocarcinoma metastasis. Genes Dev.
29:250–261. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Kitaewa MN, Grogan L, Williams JP, Dimond
E, Nakahara K, Hausner P, DeNobile JW, Soballe PW and Kirsch IR:
Mutations in beta-catenin are uncommon in colorectal cancer
occurring in occasional replication error-positive tumors. Cancer
Res. 57:4478–4481. 1997.PubMed/NCBI
|
|
37
|
Mäki-Nevala S, Sarhadi VK, Rönty M,
Kettunen E, Husgafvel-Pursiainen K, Wolff H, Knuuttila A and
Knuutila S: Hot spot mutations in Finnish non-small cell lung
cancers. Lung Cancer. 99:102–110. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Han ES, Moyer MP, Naylor S and Sakaguchi
AY: Mutation in the TP53 gene in colorectal carcinoma detected by
polymerase chain reaction. Genes Chromosomes Cancer. 3:313–317.
1991. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Lai MY, Chang HC, Li HP, Ku CK, Chen PJ,
Sheu JC, Huang GT, Lee PH and Chen DS: Splicing mutations of the
p53 gene in human hepatocellular carcinoma. Cancer Res.
53:1653–1656. 1993.PubMed/NCBI
|