Introduction
In 2012, breast cancer was the most common cancer in
females worldwide (1). It is
estimated that 1.6 million new diagnoses of breast cancer and 1.2
million breast cancer-associated mortalities occur in China every
year (2). Surgery is the primary
treatment for localized breast cancer, while adjunctive therapies,
including radiotherapy, chemotherapy, hormonal therapy and targeted
therapy may also improve the survival rate of patients (3–5). However,
delayed diagnosis, recurrence and acquiring resistance remain
obstacles to the successful treatment of breast cancer. Therefore,
the identification of associated detection biomarkers and
therapeutic targets is essential for the accurate and sensitive
diagnosis and prognosis of breast cancer.
Erythropoietin-producing hepatocellular (Eph)
receptors belong to the tyrosine kinase receptor family, which was
first identified as being involved in the tumorigenic process 3
decades ago (6). In the human genome,
there are 9 EphA receptors and 5 EphB receptors, which serve key
roles in normal physiology, including cell migration, cell
adhesion, cell proliferation and cell-fate determination. These
activities depend on the binding of their Eph receptor-interacting
(ephrin) proteins, of which there are 8 members. Compelling
evidence has demonstrated that Eph receptors and ephrins affect
tumor growth, invasiveness, angiogenesis and metastasis (7–9). EphA6, an
EphA receptor, was previously identified to serve a critical role
in carcinogenesis, but its role in cancer progression has only been
studied in prostate cancer (10).
Therefore, the expression level and clinical significance of EphA6
in breast cancer remains unclear.
In the present study, the mRNA expression of EphA6
in paired breast cancer and adjacent non-cancerous tissues was
investigated using reverse transcription-quantitative polymerase
chain reaction (RT-qPCR). Additionally, the protein expression of
EphA6 in 116 patients with breast cancer was analyzed by
immunohistochemistry (IHC) and the association between EphA6
expression and clinicopathological parameters was examined. The
outcome of patients was used to determine whether EphA6 may be used
as a diagnostic and prognostic marker for breast cancer.
Materials and methods
Patients and tissue samples
All tissue samples were collected from Huashan
Hospital Affiliated to Fudan University (Shanghai, China). Paired
breast cancer samples and adjacent non-cancerous tissues (≥5 cm
from the tumor edge) were collected from 26 patients who had
undergone mastectomy at Huashan Hospital between January 2011 and
July 2012. The samples were immediately stored at −80°C prior to
total RNA extraction. For immunohistochemical assays, 116
formalin-fixed, paraffin-embedded (FFPE) breast cancer tissues,
fixed in 4% formaldehyde, for 24–48 h at room temperature, were
obtained from the Department of Pathology (Huashan Hospital
Affiliated to Fudan University, Shanghai, China) between January
2008 and September 2008. None of the patients were pretreated with
chemotherapy or radiotherapy prior to mastectomy. The patients
whose specimens were used for immunohistochemical assays, were
followed up for ~8 years (88–96 months) and their
clinicopathological variables are summarized in Table I. Histological grading of primary
breast cancer was evaluated according to the Nottingham grading
system (11). Breast cancer subtypes
were defined according to the St. Gallen Consensus 2013 (12). Written informed consent was obtained
from all patients prior to surgery and the present study was
approved by the Institutional Review Board of Shanghai Medical
College at Fudan University (Shanghai, China).
 | Table I.Association between EphA6 and
clinicopathological characteristics. |
Table I.
Association between EphA6 and
clinicopathological characteristics.
|
|
| EphA6 expression, n
(%) |
|
|---|
|
|
|
|
|
|---|
| Variable | Total, n | Low | High | P-value |
|---|
| All cases
(n=116) | 116 | 55 (47.4) | 61 (52.6) |
|
| Age |
|
|
| 0.4511 |
| <50
years | 59 | 30 (50.8) | 29 (49.2) |
|
| ≥50
years | 57 | 25 (43.9) | 32 (56.1) |
|
| Tumor size |
|
|
| 0.5793 |
| <2.5
cm | 88 | 43 (48.9) | 45 (51.1) |
|
| ≥2.5
cm | 28 | 12 (42.9) | 16 (57.1) |
|
| Lymph node
metastasis |
|
|
| 0.8525 |
| Negative
(−) | 58 | 28 (48.3) | 30 (51.7) |
|
| Positive
(+) | 58 | 27 (46.6) | 31 (53.4) |
|
| TNM
classification |
|
|
| 0.7455 |
| I | 46 | 21 (45.7) | 25 (54.3) |
|
| II | 53 | 27 (50.9) | 26 (49.1) |
|
| III | 17 | 7 (41.2) | 10 (58.8) |
|
| Histological
grade |
|
|
| <0.001 |
| I
(well) | 33 | 25 (75.8) | 8 (24.2) |
|
| II
(moderate) | 52 | 21 (40.4) | 31 (59.6) |
|
| III
(poor) | 31 | 9 (29.0) | 22 (71.0) |
|
| Estrogen receptor
status |
|
|
| 0.0247 |
|
Negative | 44 | 15 (34.1) | 29 (65.9) |
|
|
Positive | 72 | 40 (55.6) | 32 (44.4) |
|
| Progesterone
receptor status |
|
|
| 0.0015 |
|
Negative | 56 | 18 (32.1) | 38 (67.9) |
|
|
Positive | 60 | 37 (61.7) | 23 (38.3) |
|
| HER-2 status |
|
|
| 0.0106 |
|
Negative | 77 | 43 (55.8) | 34 (44.2) |
|
|
Positive | 39 | 12 (30.8) | 27 (69.2) |
|
| Ki-67 status |
|
|
| 0.1145 |
|
Negative | 40 | 23 (57.5) | 17 (42.5) |
|
|
Positive | 76 | 32 (42.1) | 44 (57.9) |
|
| p53 status |
|
|
| 0.8974 |
|
Negative | 52 | 25 (48.1) | 27 (51.9) |
|
|
Positive | 64 | 30 (46.9) | 34 (53.1) |
|
| Subtype |
|
|
| 0.0164 |
| Luminal
A | 42 | 27 (64.3) | 15 (35.7) |
|
| Luminal
B (HER-2-negative) | 12 | 6 (50.0) | 6 (50.0) |
|
| Luminal
B (HER-2-positive) | 18 | 7 (38.9) | 11 (61.1) |
|
| HER-2
enriched | 21 | 4 (19.0) | 17 (81.0) |
|
|
Basal-like (Triple
negative) | 23 | 11 (47.8) | 12 (52.2) |
|
| Survival
status |
|
|
| 0.0141 |
|
Alive | 103 | 53 (51.5) | 50 (48.5) |
|
|
Deceased | 13 | 2 (15.4) | 11 (84.6) |
|
RT-qPCR
Total RNA from 26 fresh breast cancer samples and
corresponding adjacent non-cancerous breast tissues was extracted
using TRIzol reagent (Invitrogen; Thermo Fisher Scientific, Inc.,
Waltham, MA, USA), according to the manufacturer's protocol. All
RNA samples were then treated with 1 U/µl RNase-free DNase (Promega
Corporation, Madison, WI, USA) to eliminate genomic DNA. The
concentration and quality of RNA was evaluated using the NanoDrop
2000 spectrophotometer (Thermo Fisher Scientific, Inc.). cDNA was
then synthesized from 500 ng total RNA using the PrimeScript RT
Master Mix kit (Takara, Dalian, China). RT-qPCR was performed on
the 7900HT Fast Real-Time PCR System (Applied Biosystems; Thermo
Fisher Scientific, Inc.) using Power SYBR Green PCR Master mix
(Applied Biosystems; Thermo Fisher Scientific, Inc.) to detect the
expression level of EphA6, with GAPDH as a normalizing control. The
primers for EphA6 and GAPDH, designed by Sangon Biotech Co., Ltd.
(Shanghai, China), were as follows: EphA6 forward,
5′-TTGGAGAAGTCTGTAGTGGG-3′ and reverse, 5′-CTTCTTTGCCGATCCATGTG-3′;
and GAPDH forward, 5′-CTGACTTCAACAGCGACACC-3′ and reverse,
5′-TGCTGTAGCCAAATTCGTTGT-3′. The thermocycling conditions were as
follows: One cycle at 95°C for 10 min, followed by 40 cycles of
amplification at 95°C for 15 sec and 60°C for 1 min. The relative
EphA6 mRNA expression of tumor and normal tissues was calculated
using the following equations: ΔCq=Cq (EphA6)-Cq (GAPDH); ΔΔCq=ΔCq
(tumor)-ΔCq (normal); fold change=2−ΔΔCq (13).
IHC
Sections (4 µm) were cut from FFPE specimens.
Subsequent to baking for 2 h at 60°C, the sections were dewaxed
with xylene and rehydrated in a descending alcohol series (100, 95
and 70%, successively). Endogenous peroxidase activity was blocked
with 0.3% hydrogen peroxide for 30 min at 37°C. For antigen
retrieval, the sections were submerged in sodium citrate buffer (pH
6.0) at high pressure for 10 min, and were then incubated with
normal goat serum (dilution, 1:20) for 30 min at 37°C to reduce
nonspecific binding. The sections were incubated with the rabbit
anti-EphA6 polyclonal antibody (dilution, 1:50; catalog no.
AP51189; Abgent Inc., San Diego, CA, USA) was used at a dilution of
1:50 overnight at 4°C, followed by incubation with a
poly-horseradish peroxidase (HRP) anti-mouse rabbit secondary
antibody (Ready-To-Use; catalog no. D-3004-30; Shanghai Long Island
Antibody Diagnostica Inc., Shanghai, China) for 45 min at 37°C.
Subsequent to rinsing, sections were stained with
3,3′-diaminobenzidine for 30 sec at room temperature. Finally, in
order to observe the nucleus, the sections were counterstained with
hematoxylin for 1 min at room temperature, dehydrated with 70%
alcohol and cleared with xylene.
Immunoreactivity was assessed with a confocal BX-51
microscope (Olympus America Inc., Melville, NY, USA; magnification,
×400); results were evaluated separately by two independent
pathologists (Professor Tang, Huashan Hospital, Shanghai, China and
Professor Liu, The Fifth People's Hospital of Shanghai, China) who
were blinded to the patient clinical information. The average
scores provided by the two pathologists were used to evaluate EphA6
expression. The immunoreactivity score (IRS) was calculated using
the following formula: IRS=staining intensity score (0, no
staining; 1, weak staining; 2, moderate staining; and 3, strong
staining) × percentage of positively stained tumor cells score (0,
0–5; 1, 5–25; 2, 25–50; and 3, 50–100%). Based on these scores, the
expression levels of EphA6 were defined as high (IRS >4) or low
(IRS ≤4) (14). Estrogen receptor
(ER) and progesterone receptor (PR) expression was considered
absent (nuclear staining in <1% of tumor cells) or positive
(nuclear staining in ≥1% of tumor cells) (15). For the common clinicopathological
marker Ki-67, samples with <14% positive nuclear-stained tumor
cells were categorized as Ki-67 negative (16). HER-2 expression was scored as: 0, no
reactivity or membrane staining in <10% of tumor cells; 1+,
faint/barely perceptible staining in >10% of tumor cells; 2+,
weak to moderate membrane staining in >10% of tumor cells; or
3+, uniform intense membrane staining in >10% of invasive tumor
cells. Samples scored 2+ were retested using fluorescence in
situ hybridization (FISH). If the IHC score was 3+ or the FISH
amplified ratio of HER-2 to CEP17 was >2.2, samples were
considered positive for HER-2 (17).
Statistical analysis
Statistical analysis was performed using SPSS
version 19.0 (SPSS, Inc., Chicago, IL, USA). Student's t-test was
used to compare the differences in EphA6 expression between the
cancerous and healthy breast tissues. The χ2 test was
applied to investigate the association between EphA6 expression and
clinicopathological characteristics. Overall survival (OS) was
defined as the time period between the date of surgery and the date
of mortality or final clinical follow-up. Survival curves were
generated using the Kaplan-Meier method and comparisons were
analyzed by the log-rank test. The Cox proportional hazards model
was used for the univariate and multivariate analyses, and the
adjusted hazard ratios and their 95% confidence intervals were
calculated. P<0.05 was considered to indicate a statistically
significant difference.
Results
Upregulation of EphA6 mRNA and protein
expression in breast cancer tissues
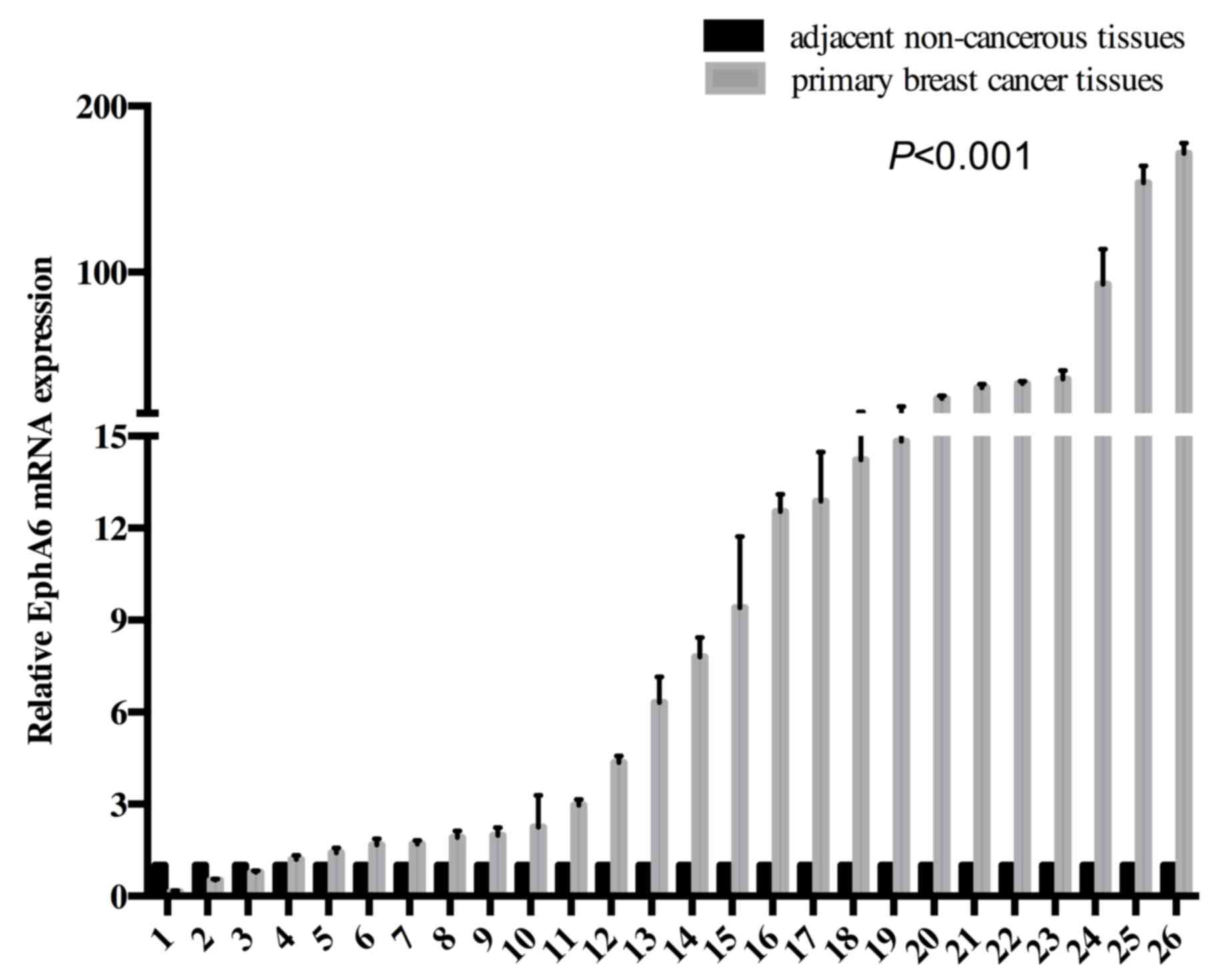
EphA6 mRNA expression levels in the breast cancer
tissues of 26 patients were significantly higher than that in the
matched adjacent non-cancerous tissues, as determined by RT-qPCR
analysis (P<0.001; Fig. 1).
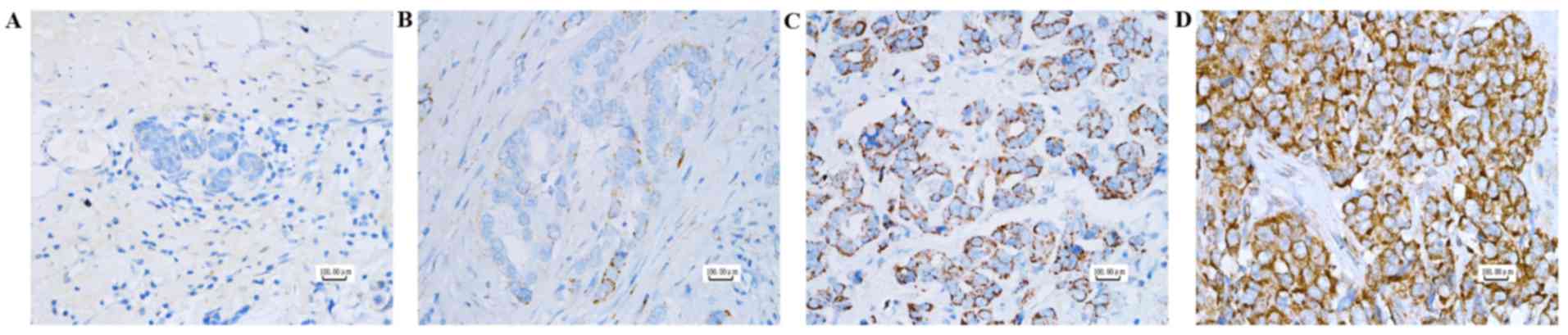
Additionally, IHC revealed that protein expression of EphA6 was
absent in normal breast tissues and positive (weak-strong staining)
in cancer tissues (Fig. 2). EphA6
staining was primarily observed in the cell cytoplasm and was
present as coarse granules. In addition, EphA6 expression was
positively associated with histological grade. As also demonstrated
in Table I, more advanced
histological grades were associated with a higher EphA6
expression.
Association between EphA6 expression
and clinicopathological characteristics
To determine the significance of EphA6 in breast
cancer, the association between the EphA6 expression in 116
patients with breast cancer and their clinicopathological
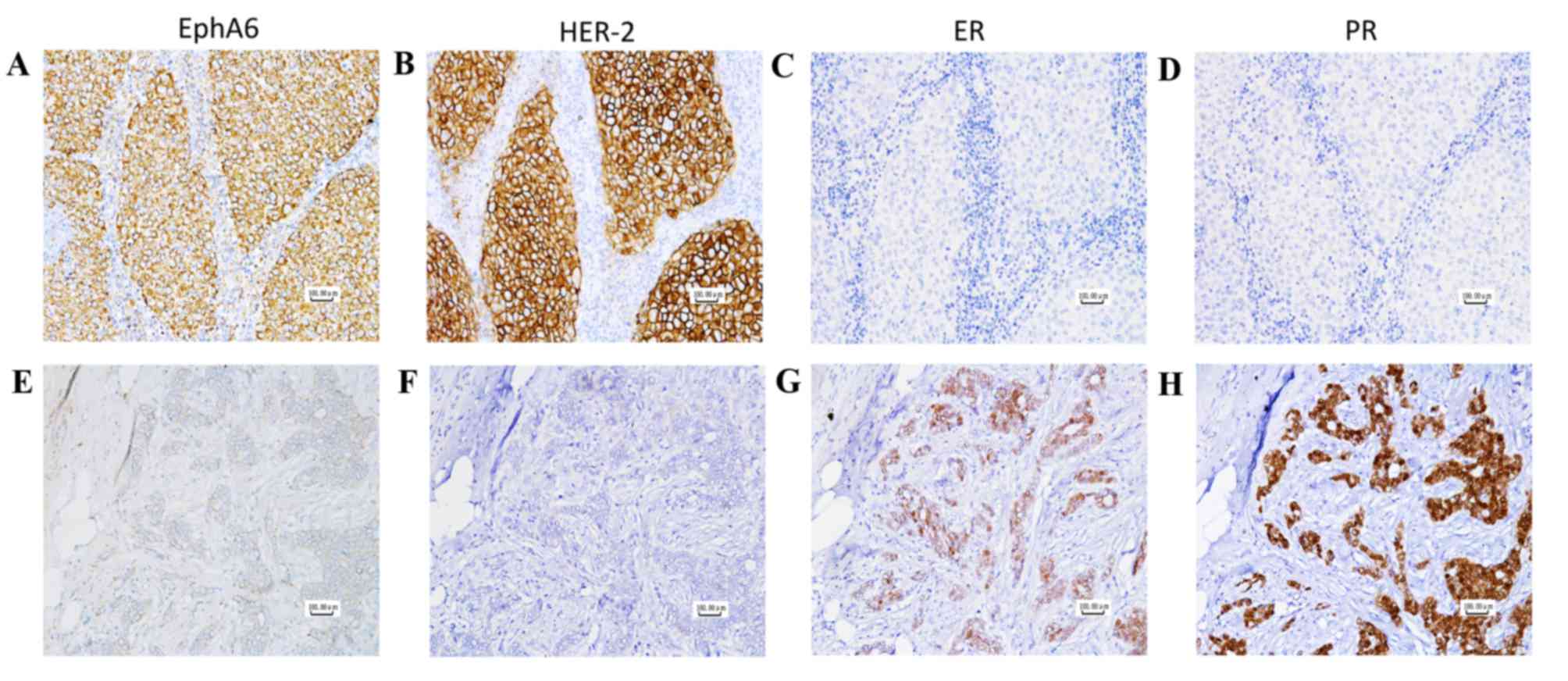
characteristics was studied. As demonstrated in Table I, EphA6 expression was significantly
positively associated with histological grade (P<0.001) and
HER-2 overexpression (P=0.0106), but was significantly negatively
associated with ER positivity (P=0.0247) and PR positivity
(P=0.0015). The association between EphA6 and ER, PR and HER-2
expression is demonstrated in Fig. 3.
The increased expression of EphA6 was also associated with breast
cancer subtypes (P=0.0164). In the HER-2 enriched subtype, 17 out
of 21 patients (81%) exhibited the overexpression of EphA6
(Table I). However, no significant
association was observed between EphA6 expression and other
clinicopathological characteristics, including age, tumor size,
lymph node metastasis, Tumor-Node-Metastasis (TNM) stage (18), or the status of the common
clinicopathological markers, Ki-67 and tumor protein p53
(P>0.05).
Prognostic significance of EPHA6
expression in breast cancer
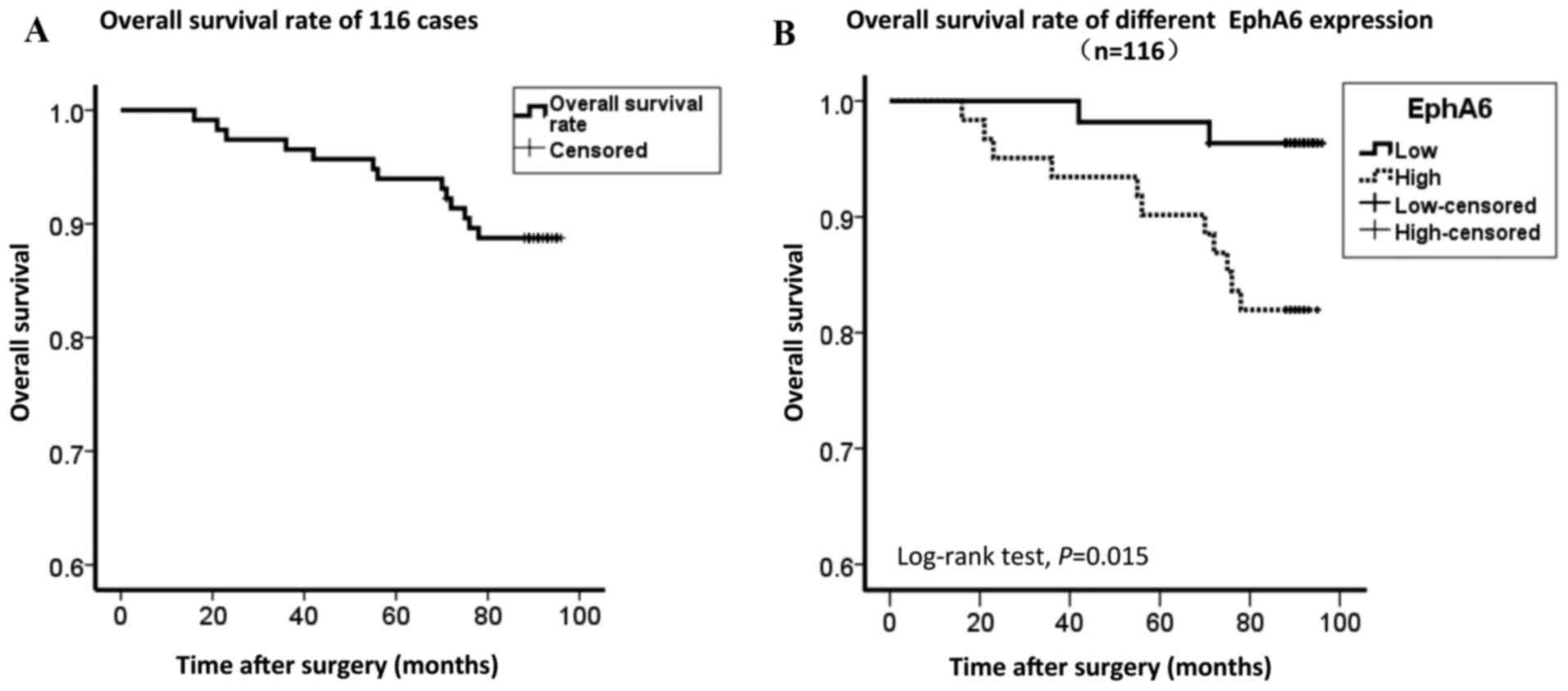
The prognostic value of EphA6 expression was
determined in 116 patients with breast cancer using Kaplan-Meier
analysis and the log-rank test. The start time was between April
2008 to November 2008, and the end time was April 2016. At the end
of the follow-up period 50/61 (82.0%) patients with high EphA6
expression had survived, while 53/55 (96.4%) patients with low
EphA6 expression had survived. The OS rate of the 116 patients with
breast cancer was 88.8% (Fig. 4A),
and the OS rate of patients with high EphA6 expression was
significantly lower than that of patients with low EphA6 expression
(P=0.015; Fig. 4B). As demonstrated
in Table II, univariate analysis
identified that OS was associated with EphA6 expression (P=0.015),
age (P=0.048), TNM stage (P=0.024), histological grade (P=0.035)
and breast cancer subtypes (P=0.020). Furthermore, Cox multivariate
regression analysis demonstrated that EphA6 expression (P=0.046),
TNM stage (P=0.007) and breast cancer subtypes (P=0.040) were
independent prognostic factors for OS. These results indicated that
the EphA6 expression level was significantly associated with the
clinical prognosis of patients with breast cancer.
 | Table II.Univariate and multivariate analysis
of prognostic indicators in breast cancer. |
Table II.
Univariate and multivariate analysis
of prognostic indicators in breast cancer.
|
| Univariate analysis
(n=116) | Multivariate
analysis (n=116) |
|---|
|
|
|
|
|---|
| Variable | HR | 95% CI | P-value | HR | 95% CI | P-value |
|---|
| EphA6
expression | 5.296 | 1.174–23.897 | 0.015 | 5.248 | 1.031–26.728 | 0.046 |
| Age | 0.294 | 0.081–1.069 | 0.048 | 0.265 | 0.070–1.010 | 0.052 |
| Tumor size | 2.207 | 0.722–6.750 | 0.154 |
|
|
|
| Lymph node
metastasis | 1.158 | 0.389–3.447 | 0.792 |
|
|
|
| TNM
classification | 2.393 | 1.097–5.222 | 0.024 | 2.974 | 1.350–6.553 | 0.007 |
| Histological
grade | 2.295 | 1.030–5.118 | 0.035 | 1.215 | 0.468–3.154 | 0.690 |
| ER | 0.356 | 0.116–1.088 | 0.058 |
|
|
|
| PR | 0.390 | 0.120–1.267 | 0.104 |
|
|
|
| HER-2 | 1.228 | 0.402–3.755 | 0.718 |
|
|
|
| Ki-67 | 1.841 | 0.507–6.690 | 0.346 |
|
|
|
| p53 | 1.299 | 0.425–3.972 | 0.645 |
|
|
|
| Subtype | 1.540 | 1.049–2.262 | 0.020 | 1.555 | 1.021–2.369 | 0.040 |
Discussion
EphA6, a member of the Eph receptor family, is
widely expressed in human healthy tissues with organ-specific
patterns. A previous study demonstrated that EphA6 was
downregulated in colorectal carcinoma and renal cell carcinoma
(19), whereas the role of EphA6 in
tumorigenesis and its potential molecular mechanisms have not yet
been investigated. In a previous study, Li et al (10) demonstrated that overexpression of
EphA6 contributed to human prostate cancer progression. However, to
the best of our knowledge, the function and prognostic significance
of EphA6 in human breast cancer has not been previously
investigated.
Breast cancer is a heterogeneous disease with a wide
range of potential clinical outcomes, pathological entities and
molecular features. Based on the status of ER, PR and HER-2, the
St. Gallen Consensus formulated 4 subtypes of breast cancer:
Luminal A; luminal B; HER-2-overexpressing; and triple negative
breast cancer. These subclasses have prognostic value across
multiple targeted therapy settings (20).
In the present study, EphA6 mRNA and protein
expression were significantly upregulated in breast cancer tissues
compared with matched adjacent non-cancerous tissues (P<0.001).
In addition, IHC analysis of 116 FFPE breast cancer specimens
revealed that EphA6 expression was significantly associated with
histological grade (P<0.001), ER (P=0.0247), PR (P=0.0015) and
HER-2 (P=0.0106) status and breast cancer subtypes (P=0.0164). High
EphA6 expression was more likely to occur in ER (−), PR (−), HER-2
(+) or HER-2-overexpressing subtypes of breast cancer, or those
with a high histological grade. Therefore, the HER-2 overexpression
subtypes were defined as ER-negative, PR-negative and
HER2-positive. In addition, overexpression of EphA6 in patients
with breast cancer was markedly associated with a poor survival
rate. Univariate and multivariate analysis indicated that high
EphA6 expression level was an independent prognostic indicator for
patients with breast cancer (P=0.015 and P=0.046,
respectively).
ER and HER-2 are predictive markers for associated
targeted therapies (21). Patients
with ER-positive breast cancer are generally advised to undergo
adjuvant endocrine therapy, which may decrease the recurrence and
mortality rates (22). The
amplification of HER-2 has been observed in ≤20% of breast cancers
(23), and overexpression of HER-2
has been reported to be associated with a poor prognosis, a high
frequency of recurrence and a reduced OS rate (24). Herceptin is a humanized monoclonal
antibody that targets HER-2 and enhances its response to
chemotherapeutic agents (25). As
with HER-2, EphA6 also belongs to the receptor tyrosine kinase
family, suggesting that EphA6 may also be a possible alternative
target site for monoclonal antibody therapy. In addition, there is
crosstalk between the ER and HER family signaling pathways, which
contributes to the resistance to endocrine therapies against the ER
pathway (26). Therefore, a
reciprocal inhibition may exist in steroid receptor and growth
factor receptor signaling, in accordance with the observations that
EphA6 expression is positively associated with HER-2 expression and
negatively associated with ER and PR expression.
Eph family members may generate a bidirectional
signal by binding to cell surface-associated ephrin ligands. As one
of the most studied members of the Eph family, EphA2 overexpression
was revealed to be inversely associated with hormone receptor (ER
and PR) expression in endometrial carcinomas (27) and significantly associated with the
poor prognosis of HER-2 overexpressing patients with breast cancer
(28), which was similar to the
results for EphA6 in the present study. In addition, an increasing
volume of evidence has suggested that the EPHA2-ephrin-A1 system
serves a crucial role in tumorigenesis and vascularization during
carcinogenesis (8). Therefore, these
results indicated EphA6 may also function by interacting with
ephrin-A1 or other ephrins.
In conclusion, to the best of our knowledge, the
present study is the first to report the expression and clinical
relevance of EphA6 in breast cancer. EphA6 overexpression was
revealed to be associated with indicators of a poor prognosis,
including high histological grades, low expression of steroid
hormone receptors and amplification of HER-2. The results of the
present study also demonstrated that high expression of EphA6 was
more prevalent in HER-2-enriched breast cancer than in other
phenotypes. Furthermore, EphA6 overexpression was identified to be
an important independent prognostic indicator in breast cancer. In
an era of high precision medicine, EphA6 may be a useful
therapeutic target, particularly in patients with breast cancer
that exhibit HER-2 overexpression and lack the steroid receptor.
However, the underlying mechanisms of the activity of EphA6 in
breast cancer remain unknown and additional studies are required to
improve the understanding of its molecular mechanisms.
References
|
1
|
Ferlay J, Soerjomataram I, Dikshit R, Eser
S, Mathers C, Rebelo M, Parkin DM, Forman D and Bray F: Cancer
incidence and mortality worldwide: Sources, methods and major
patterns in GLOBOCAN 2012. Int J Cancer. 136:E359–E386. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Fan L, Strasser-Weippl K, Li JJ, St Louis
J, Finkelstein DM, Yu KD, Chen WQ, Shao ZM and Goss PE: Breast
cancer in China. Lancet Oncol. 15:e279–e289. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bernier J, Rossier C and Horiot JC: Recent
advances in regional treatment of breast carcinoma. Crit Rev Oncol
Hemato. 99:107–114. 2016. View Article : Google Scholar
|
|
4
|
Partridge AH: Chemotherapy in
premenopausal breast cancer patients. Breast Care (Basel).
10:307–310. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Rakha EA: Pitfalls in outcome prediction
of breast cancer. J Clin Pathol. 66:458–464. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hirai H, Maru Y, Hagiwara K, Nishida J and
Takaku F: A novel putative tyrosine kinase receptor encoded by the
eph gene. Science. 238:1717–1720. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Pasquale EB: Eph-ephrin bidirectional
signaling in physiology and disease. Cell. 133:38–52. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Pasquale EB: Eph receptors and ephrins in
cancer: Bidirectional signalling and beyond. Nat Rev Cancer.
10:165–180. 2010. View
Article : Google Scholar : PubMed/NCBI
|
|
9
|
Pasquale EB: Eph receptor signalling casts
a wide net on cell behaviour. Nat Rev Mol Cell Biol. 6:462–475.
2005. View
Article : Google Scholar : PubMed/NCBI
|
|
10
|
Li S, Ma Y, Xie C, Wu Z, Kang Z, Fang Z,
Su B and Guan M: EphA6 promotes angiogenesis and prostate cancer
metastasis and is associated with human prostate cancer
progression. Oncotarget. 6:22587–22597. 2015.PubMed/NCBI
|
|
11
|
Elston CW and Ellis IO: Pathological
prognostic factors in breast cancer. I. The value of histological
grade in breast cancer: Experience from a large study with
long-term follow-up. Histopathology. 19:403–410. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Untch M, Gerber B, Harbeck N, Jackisch C,
Marschner N, Möbus V, von Minckwitz G, Loibl S, Beckmann MW,
Blohmer JU, et al: 13th stGallen international breast cancer
conference 2013 primary therapy of early breast cancer evidence,
controversies, consensus opinion of a german team of experts
(zurich 2013). Breast Care (Basel). 8:221–229. 2013.PubMed/NCBI
|
|
13
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
You Y, Li H, Qin X, Ran Y and Wang F:
Down-regulated ECRG4 expression in breast cancer and its
correlation with tumor progression and poor prognosis-A short
report. Cell Oncol (Dordr). 39:89–95. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Parl FF, Schmidt BP, Dupont WD and Wagner
RK: Prognostic significance of estrogen receptor status in breast
cancer in relation to tumor stage, axillary node metastasis, and
histopathologic grading. Cancer. 54:2237–2242. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Howell SJ, Wardley AM and Armstrong AC:
Re: Ki67 index, HER2 status, and prognosis of patients with luminal
B breast cancer. J Natl Cancer Inst. 101:1730–1731. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wolff AC, Hammond ME, Schwartz JN, Hagerty
KL, Allred DC, Cote RJ, Dowsett M, Fitzgibbons PL, Hanna WM, Langer
A, et al: American society of clinical oncology/college of American
pathologists guideline recommendations for human epidermal growth
factor receptor 2 testing in breast cancer. J Clin Oncol.
25:118–145. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Edge SB and Compton CC: The American joint
committee on cancer: The 7th edition of the AJCC cancer staging
manual and the future of TNM. Ann Surg Oncol. 17:1471–1474. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hafner C, Schmitz G, Meyer S, Bataille F,
Hau P, Langmann T, Dietmaier W, Landthaler M and Vogt T:
Differential gene expression of Eph receptors and ephrins in benign
human tissues and cancers. Clin Chem. 50:490–499. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Rouzier R, Perou CM, Symmans WF, Ibrahim
N, Cristofanilli M, Anderson K, Hess KR, Stec J, Ayers M, Wagner P,
et al: Breast cancer molecular subtypes respond differently to
preoperative chemotherapy. Clin Cancer Res. 11:5678–5685. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kourea HP, Zolota V and Scopa CD: Targeted
pathways in breast cancer: Molecular and protein markers guiding
therapeutic decisions. Curr Mol Pharmacol. 7:4–21. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Payne SJ, Bowen RL, Jones JL and Wells CA:
Predictive markers in breast cancer-the present. Histopathology.
52:82–90. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Gajria D and Chandarlapaty S:
HER2-amplified breast cancer: Mechanisms of trastuzumab resistance
and novel targeted therapies. Expert Rev Anticancer Ther.
11:263–275. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
English DP, Roque DM and Santin AD: HER2
expression beyond breast cancer: Therapeutic implications for
gynecologic malignancies. Mol Diagn Ther. 17:85–99. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Pietras RJ, Pegram MD, Finn RS, Maneval DA
and Slamon DJ: Remission of human breast cancer xenografts on
therapy with humanized monoclonal antibody to HER-2 receptor and
DNA-reactive drugs. Oncogene. 17:2235–2249. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Arpino G, Wiechmann L, Osborne CK and
Schiff R: Crosstalk between the estrogen receptor and the HER
tyrosine kinase receptor family: Molecular mechanism and clinical
implications for endocrine therapy resistance. Endocr Rev.
29:217–233. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kamat AA, Coffey D, Merritt WM, Nugent E,
Urbauer D, Lin YG, Edwards C, Broaddus R, Coleman RL and Sood AK:
EphA2 overexpression is associated with lack of hormone receptor
expression and poor outcome in endometrial cancer. Cancer.
115:2684–2692. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zhuang G, Brantley-Sieders DM, Vaught D,
Yu J, Xie L, Wells S, Jackson D, Muraoka-Cook R, Arteaga C and Chen
J: Elevation of receptor tyrosine kinase EphA2 mediates resistance
to trastuzumab therapy. Cancer Res. 70:299–308. 2010. View Article : Google Scholar : PubMed/NCBI
|