Introduction
Breast cancer is the most frequently diagnosed
cancer and is the leading cause of female mortality worldwide,
accounting for 25% of the total number of cancer cases and 15% of
all cancer-associated female mortality (1). The incidence of breast cancer is still
progressively increasing (2).
Therefore, females with breast cancer represent a major public
health priority and has received hundreds of billions of US dollars
over the last 20 years to fund studies and drug development
(3). In order to bridge the gap
between preclinical and clinical studies, murine models are broadly
used to mimic the development of breast cancer and assess the
efficacy of therapeutic strategies. It is evident that no single
murine model is able to replicate the process of cancer progression
(4,5),
therefore it is important to choose a relevant and appropriate
model.
Murine models of breast cancer currently used are:
Xenograft models, syngeneic murine models (directly implanted,
chemically or virally induced) and genetically engineered mice
(GEM) (including transgenic and knockout methods) (6). GEM is generated to mimic human breast
cancer by targeted expression of growth factors, receptors,
proteases, oncogenes or tumor suppressor genes; this has the
advantage of elucidating the roles that transgenes serve in breast
tumorigenesis and the efficacy of targeted therapeutics (7–10).
However, GEM typically takes several months to generate and has a
high cost. Furthermore, transgenic models exhibit a low incidence
of metastasis, thus it is not possible to investigate the
underlying molecular mechanisms of cancer metastasis or
metastasis-related therapies (4,11).
Xenograft models serve a dominant role in screening
drugs for safety and efficacy. This type of model is easy to
operate and is widely utilized to study inhibitors of steroid
receptor signaling and drug resistance (12,13).
However, the formation of solid tumors is influenced by the extent
of mice immunodeficiency. Nude mice exhibit insufficiency of tumor
growth and a low metastasis rate due to natural killer cell or B
cell immune response (14,15). Additionally, the tumor xenograft in
immune-deficient mice obviates the tumor-host interaction, impairs
the metastatic microenvironment and tends to generate false
positive results (16,17).
A syngeneic murine model, the most common type of
model used for studying mechanisms of tumor growth and metastasis,
is characterized by implanted cells or tissue of the same species
or genotype as the host animal (18).
Therefore, these models provide the context of an intact immune
system and host stroma and extracellular matrix for evaluating the
tumor-environment interaction, antitumor immune response and
primary metastatic tumor relevance. In mammary tumor models, 4T1 or
4T1-luc models are useful tools for investigating antitumor and
anti-metastatic effects of various drugs due to their high invasive
nature (5,19–22),
making it a well-accepted model for diverse studies.
The selection of modeling methods varies in
different studies, including tissue and cell inoculation,
orthotopic implantation (OS), subcutaneous implantation (SQ) and
tail vein injection (TV). As for the syngeneic model, the
characteristic of tumor progression is related to the inocula, the
implantation site and the number of inoculated cells (4,5,16,20,23,24).
Therefore, a good understanding of the characteristics of models
induced by distinct methods will aid investigators to make
appropriate choices, according to the research requirements. The
aim of the present study was to compare distinct methods involving
inocula and implantation site in mouse models, to provide reference
information for preclinical studies; in particular, to elucidate
the distinctions of growth, metastasis, survival and histopathology
of tumors produced using OS and SQ.
Materials and methods
Chemicals and reagents
D-luciferin was purchased from Gold Biotechnology
Inc. (St. Louis, MO, USA). The primary antibody against cluster of
differentiation (CD) 31 (catalog no. ab28364) was purchased from
Abcam (Cambridge, UK). Two-step histostaining reagent kit
(PV-9000), and hematoxylin and eosin staining kit (ZLI-9615) were
purchased from Beijing Zhong Shan Jinqiao Biotechnology Co., Ltd.
(Beijing, China).
Preparation of cell and tissue
suspension
The 4T1-luc2 murine breast cancer cell line
(PerkinElmer, Inc., Waltham, MA, USA) was cultured in RPMI-1640
medium (Gibco®; Thermo Fisher Scientific, Inc., Waltham,
MA, USA), supplemented with 10% fetal bovine serum
(Gibco®; Thermo Fisher Scientific Inc.) and 1%
penicillin-streptomycin (HyClone; GE Healthcare Life Sciences,
Logan, UT, USA). Cells were suspended at a density of
1×104 cells/25 µl. Tissue suspension was prepared as
aforementioned, with modification (25,26); the
4T1-luc2 breast tumor was ground into a single cell suspension and
filtered through a 70 µm disposable cell strainer (Thermo Fisher
Scientific, Inc.) in PBS and finally suspended at a concentration
of 1×104 cells/25 µl.
Animal model
Female BALB/c mice (n=20; 8 weeks old; 18–20 g) were
purchased from Vital River Laboratory Animal Technology Co. Ltd.,
(Beijing, China) and randomly assigned to each group (n=10).
Animals were housed at 22±5°C in a 12 h light/dark cycle and fed
rodent chow and water freely. Orthotopic mammary fat pad
implantation was performed as follows: Female BALB/c mice were
inoculated with 25 µl cell or tissue suspension (1×104)
in the mammary fat pads under anesthesia via Matrx VMS anesthesia
machine (Midmark Corporation, Dayton, OH, USA) by continuous
inhalation of 2% isoflurane gas for 5–10 min. Sterile tweezers were
used to lift the fourth nipple and a syringe needle (BD
Biosciences, San Jose, CA, USA) was used to implant cell or tissue
suspensions directly into the mammary fat pad. For subcutaneous
implantation, female BALB/c mice were subcutaneously inoculated
with 25 µl cell suspension (1×104) under anesthesia by
continuous inhalation of 2% isoflurane gas for 5–10 min. The skin
was tented up and the 4T1-luc2 cells were implanted under the skin
in the dorsal flank regions. Tumor length (L) and width (W) were
measured twice weekly using calipers, and tumor volume (V) was
calculated as [V = (L × W2)/2]. Bioluminescence images
of primary tumor were captured using IVIS Spectrum (PerkinElmer,
Inc.) 10 min after intraperitoneal injection of D-luciferin (150
mg/kg, 200 µl). After ~30 days, the primary tumors were removed and
incisions were sutured under isoflurane anesthesia. Subsequently,
the lung metastasis was detected with bioluminescent imaging. Light
outputs were quantified using Living Image (version 4.3;
PerkinElmer, Inc.). At day 56, the mice were sacrificed following
anesthetization by pentobarbital (60 mg/kg intraperitoneal
injection) and lung tissues were obtained for histology analysis.
Humane endpoints for the present study were as follows: Body
weight, which was monitored twice weekly. When the weight after
tumor cell inoculation decreased by >10% when compared with the
initial weight of the mouse. Secondly, behavioral observations
taken during the experiment. When the food/water consumption and
the daily activity reduced by 50%, or if the fur became dull.
Thirdly, tumor length and width were measured twice weekly using
digital calipers. When the volume of primary tumor reached ~800
mm3, the mice were sacrificed. Also painkillers were
administered following tumor resection. If mice appeared in pain
even with following painkiller administration, the mice were
sacrificed. If continuous bleeding and wound infection were
observed, the mice were sacrificed. Finally, if the wounds fail to
heal following tumor resection past 5 days, the mice were
sacrificed. All animal experiments were approved by the Institution
of Animal Care and Use Committee of Capital Medical University
(ref. no. AEEI-2014-052).
Histology and
immunohistochemistry
The breast tumors and lungs were selected for
histological examination. Tissues were dissected, paraffin-embedded
and sectioned (6 µm thick). Sections were stained with hematoxylin
and eosin (H&E). Anti-CD31 rabbit polyclonal antibody was used
for immunohistochemical (IHC) staining of breast tumor and lung
sections for microvessel density (MVD) analysis. IHC staining of
CD31 was performed according to the manufacturer's protocol.
Briefly, paraffin-embedded sections were deparaffinized with xylene
and rehydrated in a graded ethanol series at room temperature, and
endogenous peroxidase activity was quenched (30 min) by 3%
H2O2 in methanol. Sections were subsequently
pretreated in boiling citrate buffer for 20 min. Sections were
blocked in 10% normal goat serum in PBS for 60 min and then
incubated with primary antibodies (anti-CD31 rabbit polyclonal
antibody, dilution 1:100) overnight at 4°C. Following two washes in
PBS, sections were incubated with 100 µl goat anti-rabbit secondary
antibody from the two-step histostaining reagent kit (Beijing Zhong
Shan Jinqiao Biotechnology Co., Ltd.) according to the
manufacturer's protocol for 30 min at room temperature. The
immunoreaction was visualized when brown precipitates formed
following incubation in diaminobenzidine. Sections were
subsequently washed with water and counterstained with 0.5%
hematoxylin for 3 min at room temperature. Finally, sections were
viewed using an upright light microscope (magnification, ×200 or
×100) (Olympus BX53; Olympus Corporation, Tokyo, Japan). MVD was
determined in five fields with a higher density of CD31+
cells and cell clusters. The presence of visible blood vessel lumen
was not required to be defined as positive (27).
Statistical analysis
Results are presented as the mean ± standard
deviation for individual experiments. Statistical significance was
determined by Student's t-test or repeated measures analysis of
variance followeed by Dunnett's test for multiple comparisons.
Kaplan-Meier estimator survival statistical analysis was utilized
for survival data. All calculations were performed using GraphPad
Prism (version 5.0; GraphPad Software Inc., La Jolla, CA, USA).
P<0.05 was considered to indicate a statistically significant
difference.
Results
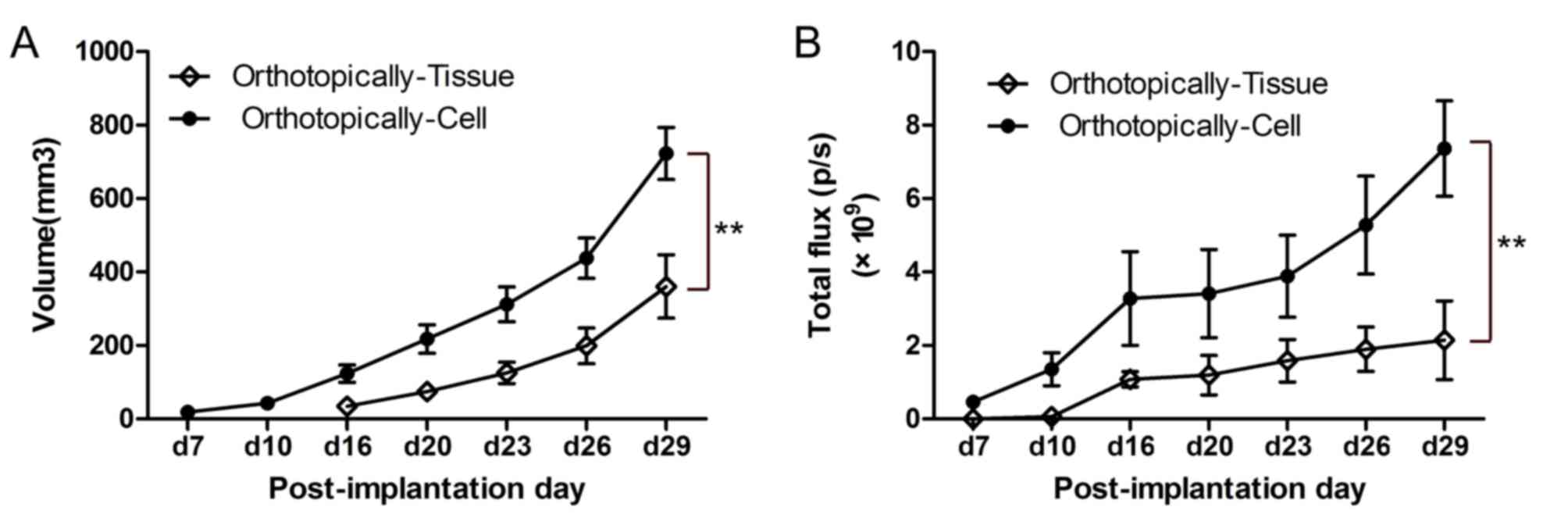
Cell suspension generates larger
breast tumor compared with tissue suspension
After 7 days of implantation, the tumor growth was
determined using calipers and a bioluminescence imaging system. The
cell suspension, visualized and determined at an earlier time point
(7 days vs. 16 days; Fig1A),
generated larger primary tumors compared with that of the tissue
suspension (722.81±70.77 vs. 360.67±86.12 mm3).
Bioluminescence imaging also revealed increased total flux of tumor
in animals inoculated with the cell suspension [(7.36±1.29)
×109 vs. (2.14±1.07) ×109 photons/sec;
Fig. 1B].
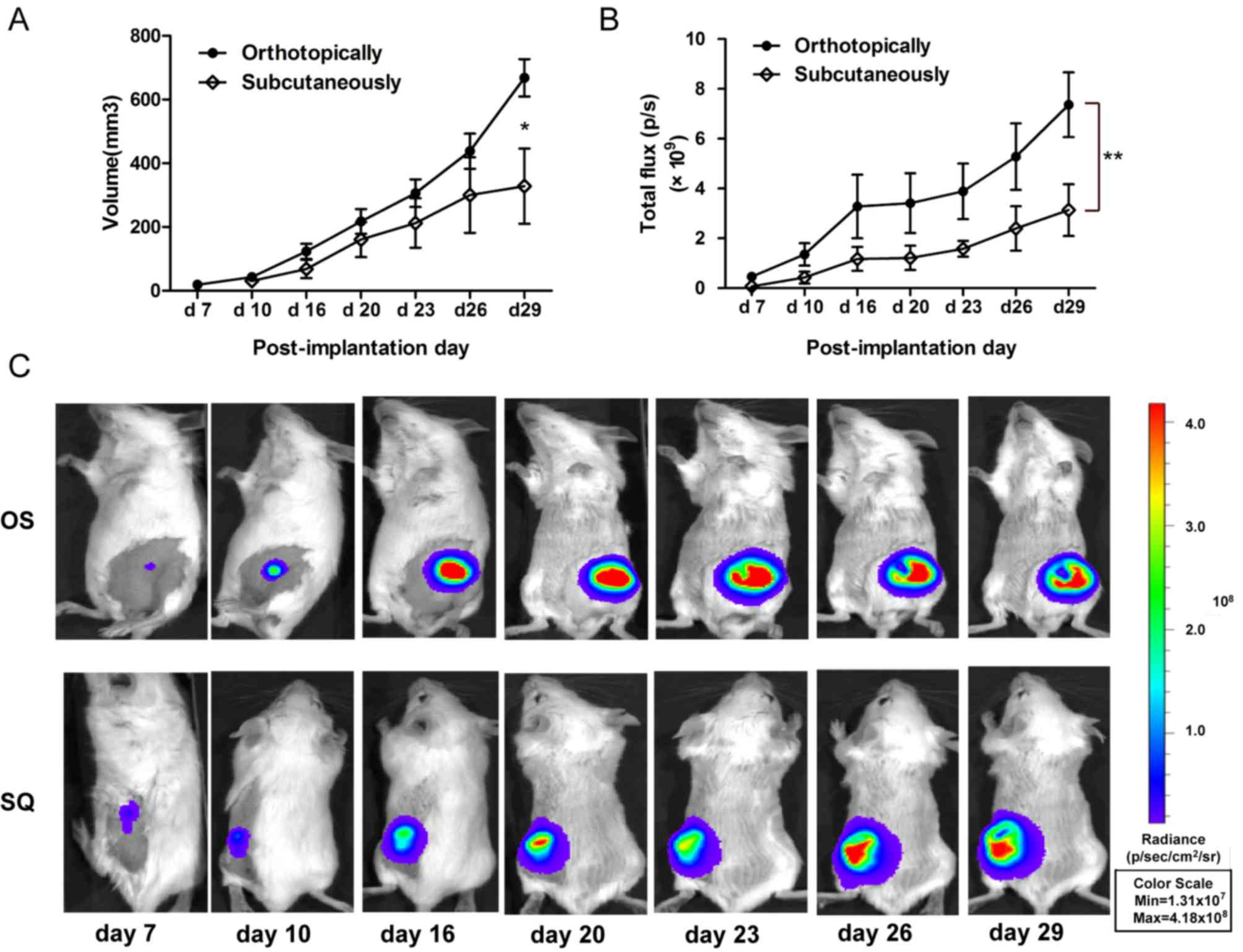
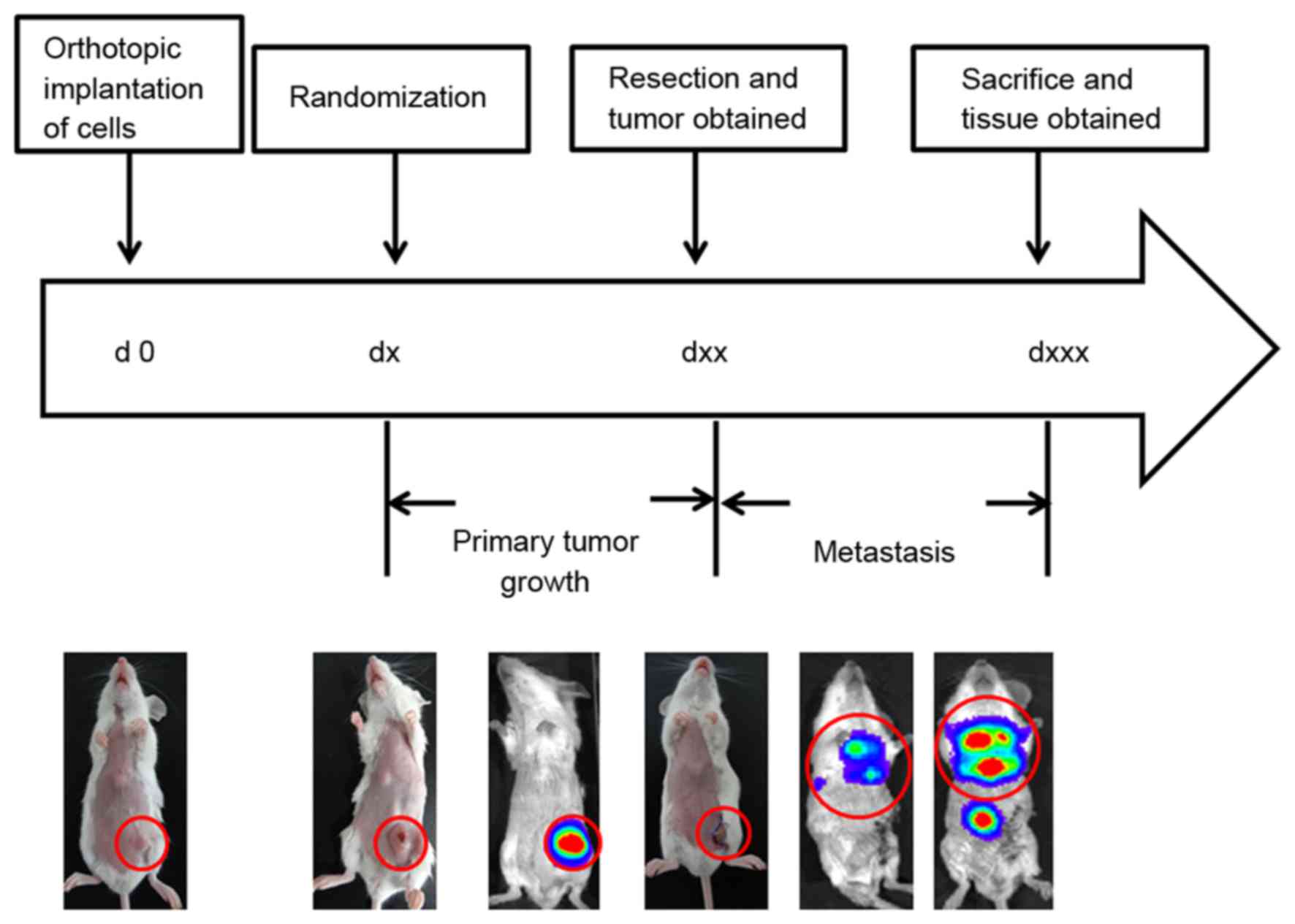
OS produces larger and less variable
tumors with increased lung metastasis compared with SQ
The 4T1-luc2 cell suspension was implanted via OS or
SQ in BALB/c mice. The tumor growth and metastasis were detected
in vivo using an imaging system or calipers. The volume of
tumor produced using OS implantation increased to 722.81
mm3 at day 29, which was increased compared with that of
SQ implantation (447.18±145.20 mm3). The variation in OS
tumor volume was decreased compared with SQ (Fig. 2A). Furthermore, the tumor progression
of OS and SQ was additionally analyzed by quantification of
bioluminescent signals. The results of the present study
demonstrate that the increased trend of total flux of OS tumor was
significantly increased, compared with that of SQ tumor
[(7.36±1.29) ×109 vs. (3.14±1.04) ×109
photons/sec; Fig. 2B)]. Following
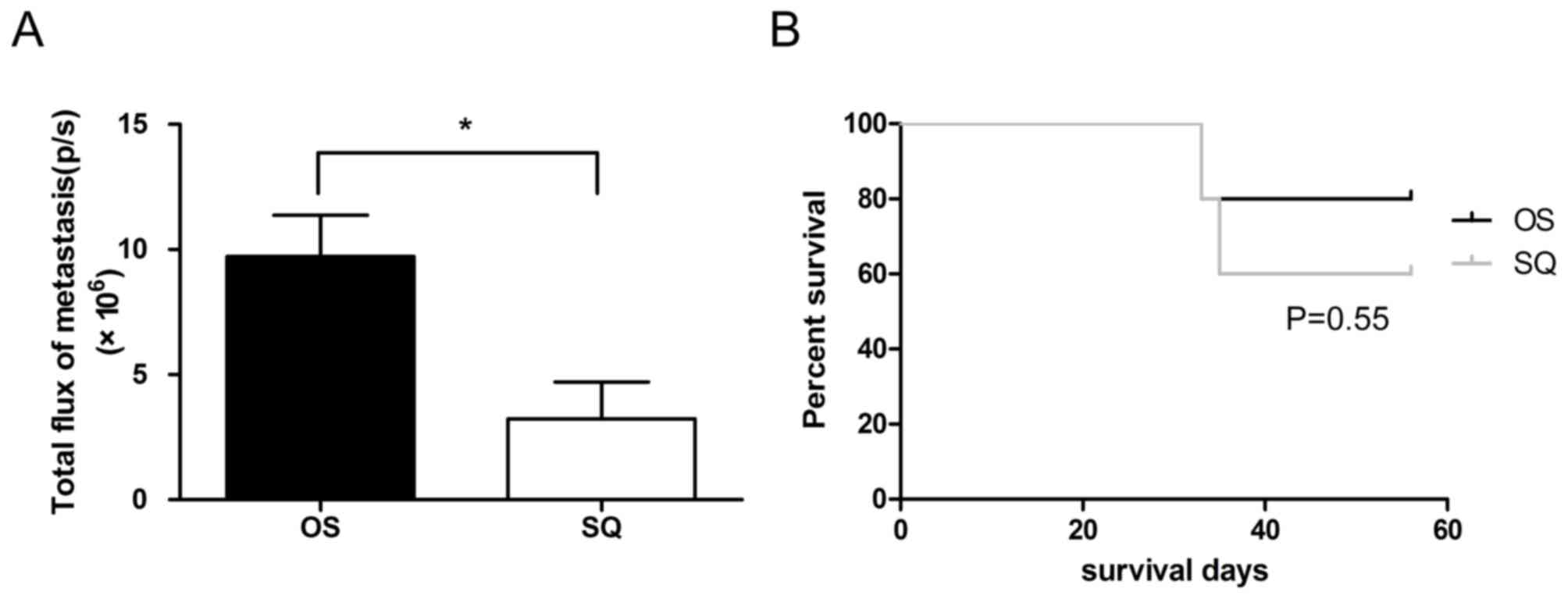
resection of the primary tumor, bioluminescent signals of lung
metastasis were determined. The results of the present study
revealed that OS implantation induced increased lung metastasis,
compared with that in SQ implantation (Fig. 3A), and the total flux of OS lung
metastasis (9.17×106 photons/sec) increased by 1.8 times
compared with SQ (3.23×106 photons/sec). Although OS
produced tumors of increased size and increased lung metastasis
compared with SQ, there was no difference in mass mortality between
the OS and SQ groups (Fig. 3B).
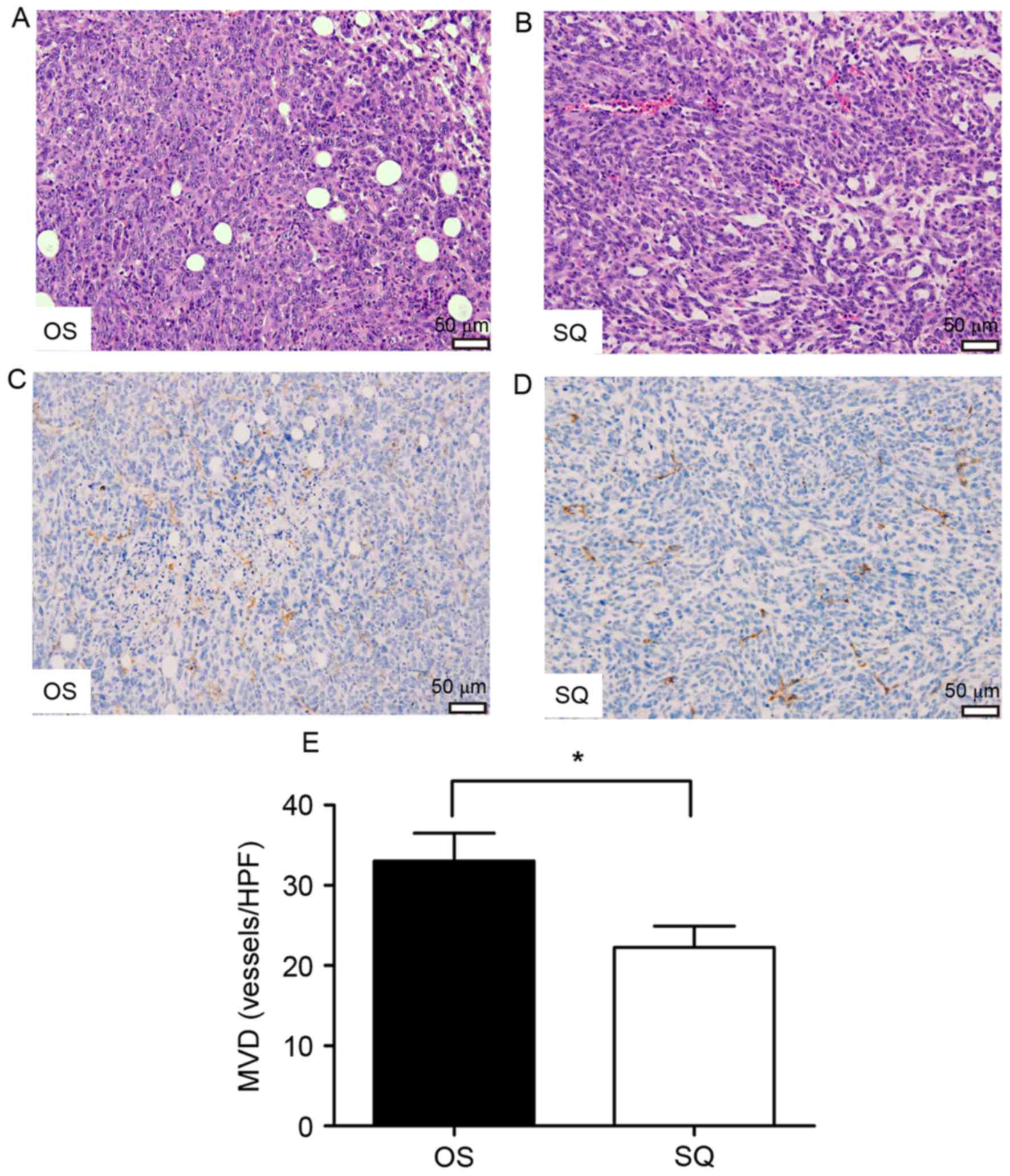
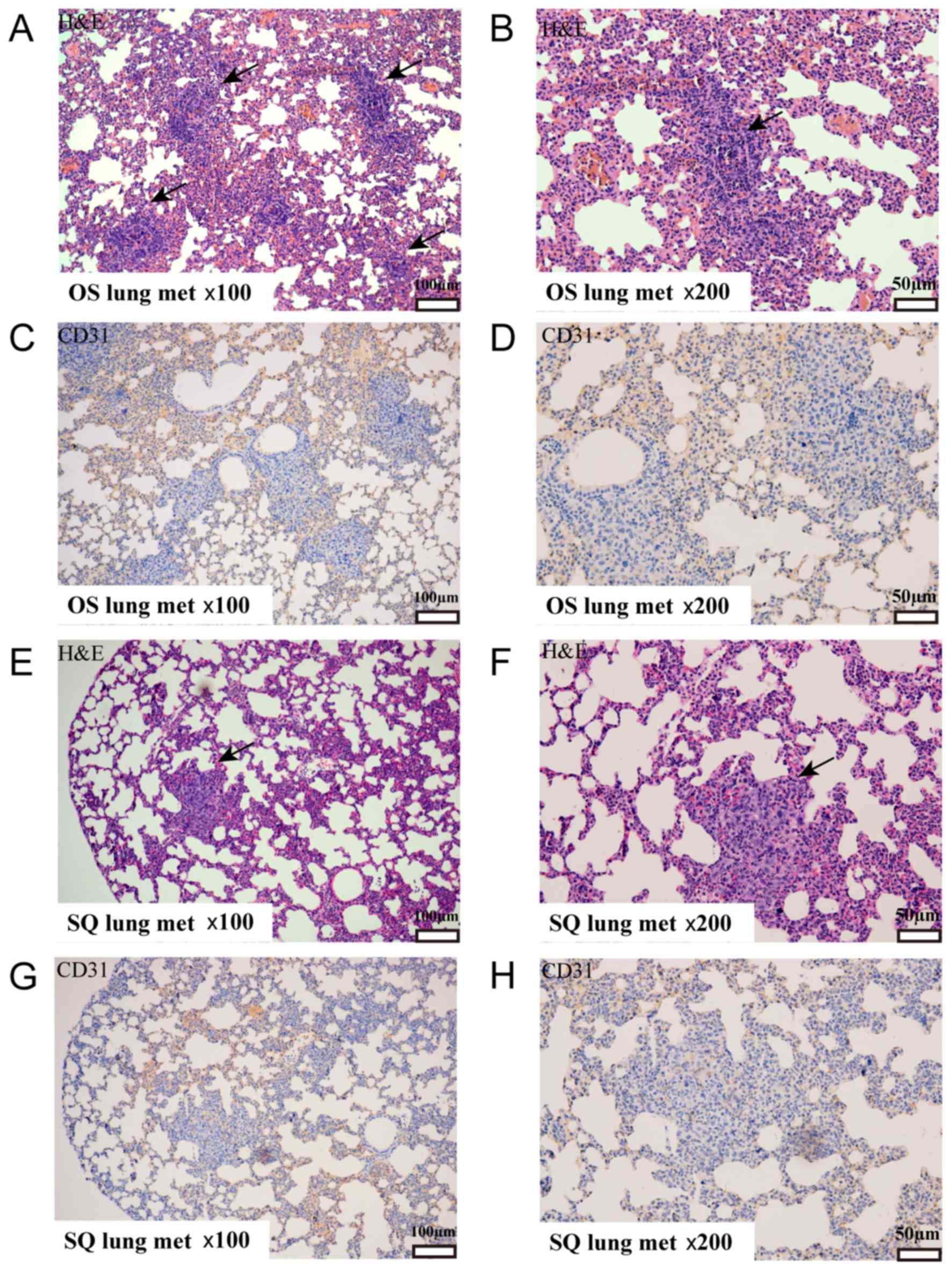
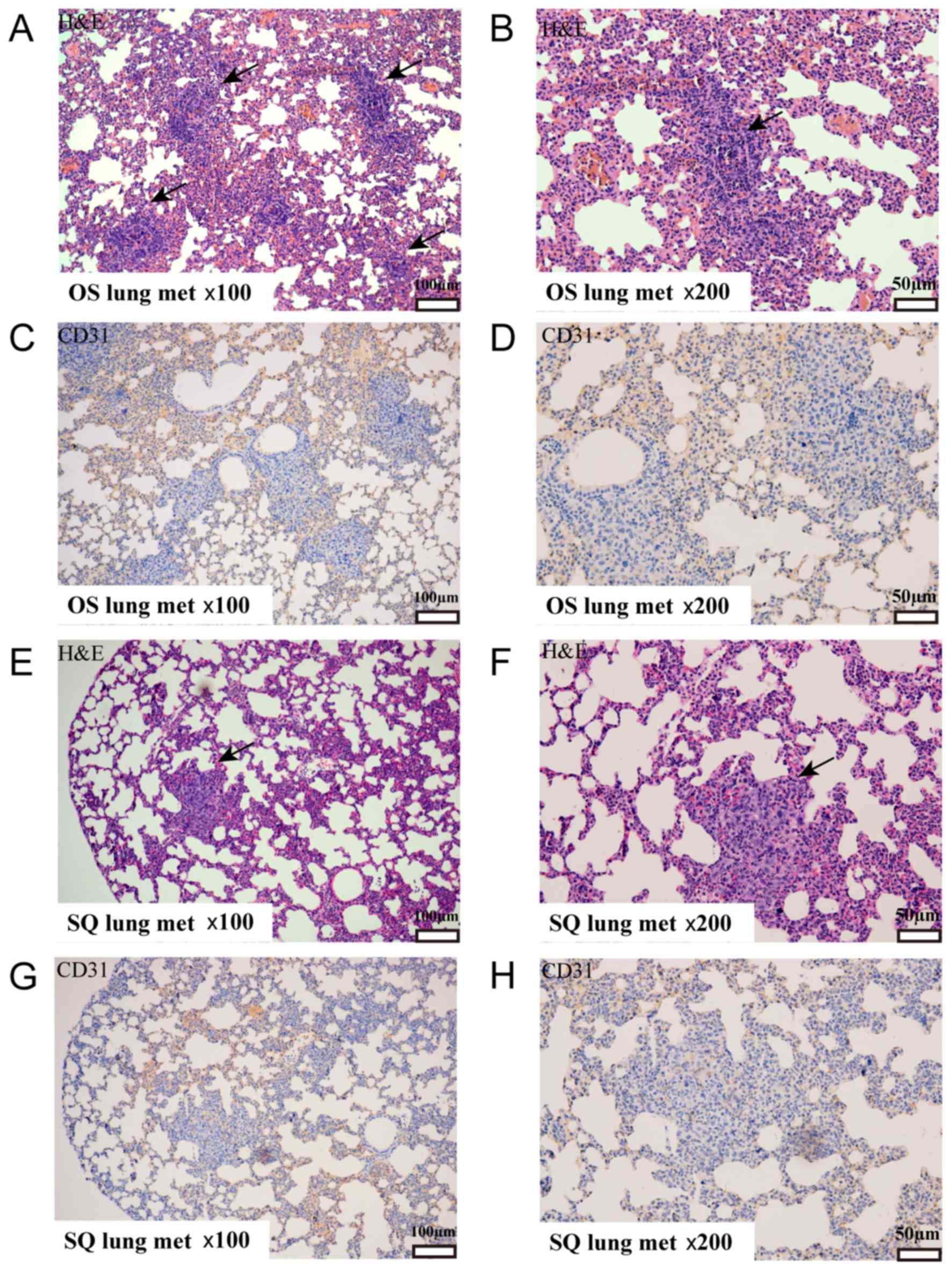
Histology
Primary tumors and metastatic lungs were fixed in
buffered formalin and embedded in paraffin. Subsequently, tissue
sections were stained by H&E and probed with an anti-CD31
antibody. OS and SQ tumors presented as a solid mass comprising
poorly differentiated cancer cells (Fig.
4A and B). Notably, OS primary tumors revealed increased tissue
heterogeneity with the involvement of adipocytes. Quantification of
MVD demonstrated a marked variation between the tumors collected
from OS and SQ (Fig. 4C-E) as an
increased number of blood vessels were observed in OS.
Additionally, H&E staining identified that OS and SQ produced
isolated lung metastatic tumors (Fig.
5A-H). An increased number of metastatic tumor foci were
visualized using microscopy in OS sections.
 | Figure 5.The metastatic lungs were fixed in
buffered formalin, embedded in paraffin and stained. (A) OS section
stained with H&E; magnification, ×100. (B) OS section stained
with H&E; magnification, ×200. (C) OS section stained with
anti-CD31 antibody; magnification, ×100. (D) OS section stained
with anti-CD31 antibody; magnification, ×200. (E) SQ section
stained with H&E; magnification, ×100. (F) SQ section stained
with H&E; magnification, ×200. (G) SQ section stained with
anti-CD31 antibody; magnification, ×100. (H) SQ section stained
with anti-CD31 antibody; magnification, ×200. H&E, Hematoxylin
and eosin; OS, orthotopic implantation; SQ, subcutaneous
implantation; CD, cluster of differentiation; met, metastasis. |
Discussion
It is critical to select a proper model to mimic the
initiation and progression of breast cancer when evaluating the
efficacy of antitumor drugs and it is considered the key to success
in studies (4,28). A number of murine models have become
available during the last two decades and syngeneic breast cancer
murine models, including the 4T1 series of murine mammary cancer
models (5,19–22,29),
remain widely used, owing to its syngeneic property of cancer cells
and experimental mice. Animal models comprising distinct methods
exhibit varied characteristic and application scope. Thus,
understanding the advantages and limitations of these modeling
methods is required.
Cultured tumor cells or tumor tissue implantation
were considered in the present study as there is currently no
consensus for mouse modeling. It was hypothesized that tissue
inoculation led to improved growth as they possessed stroma and
extracellular matrix. Previous studies demonstrated that tissue
inoculation resulted in decreased latency period and increased
metastatic rate (6,30,31).
Despite this, results of the present study identified that 4T1-luc2
tissue inoculation caused a decreased tumor growth and a delay in
tumor development. This is hypothesized to be a result of the
increased potency of tissues in provoking an immune reaction,
consequently causing increased necrosis or apoptosis (5,32). An
additional reason for the effects observed in the present study may
be that the tissue disposal process damaged the stroma and
extracellular matrix, which facilitated tumor growth. Thus, on the
basis of the results of the present study, cultured 4T1-luc2 cells
injected directly were considered to be a beneficial option.
The implantation site was subsequently compared
using cultured 4T1-luc2 cells. Following inoculation of an equal
number of cells using OS and SQ, tumor growth and metastasis were
continuously determined by an in vivo imaging system and
caliper measurement. The tumor activity and size of OS were
increased compared with that of SQ during tumor development. OS
primary tumors were of increased size and decreased variability.
The results of the present study are consistent with previous
studies of cancer cell growth and limitation of cell viability in
SQ (4,5,16,18,21,31,33).
The decreased variation of OS tumor volume is favored for narrowing
the gap within the group and for strengthening comparability
between groups. As previous studies revealed, implantation into the
mammary pad formed cancer cells with increased aggressive potential
(33,34). SQ primary tumors were observed to
possess increased localization and were easy to remove in surgery.
In comparison, OS primary tumors exhibited an increased invasive
growth pattern. Subsequently, with ~2-fold primary tumor burden, OS
models exhibited increased lung metastases. It is known that tumor
growth and metastasis are dependent on the malignant biological
behavior of cancer cell and on the tumor microenvironment where
tumor cells were located (35,36). The
results of the present study identified an increased number of
CD31+ vessels in OS tumors. Evidently, increased
angiogenesis activity provided adequate blood and nutrients for
tumor growth and metastasis in the OS model. In addition,
adipocytes were observed in OS tumors which validates that adipose
tissues and adipocytes support tumorigenesis and metastasis,
particularly in hormone-dependent cancers (37). The results of the present study
indicate that OS models may be more suitable for studies involving
tumor-microenvironment interaction. The common experimental
protocol for the orthotopic breast cancer model is presented in
Fig. 6. Although there are numerous
advantages of OS, SQ implantation remains widely used (24) and is often combined with tail
injection to observe metastasis.
In these murine models, the majority of studies have
applied between 5×104 and 2×106 4T1 or
4T1-luc2 cells for inoculation into each mouse. The tumor volume
reached ≥1,000 mm3 in 2 weeks, with an overall survival
time of between 30 and 40 days (22,33,38,39).
In the present study, 1×104 cells were inoculated into
each animal which resulted in a decreased volume of primary tumor
(<1,000 mm3) and there was no mass mortality
following primary tumor resection in SQ and OS models. The
experiment was ended at day 56 due to ethical considerations. The
results of the present study are considered to be of importance for
designing experiments to improve mimicking the real clinical
situation of cancer development, with less tumor burden.
The results of the present study identified that the
various inocula (tissue or cell) and implantation site (OS or SQ)
led to various rates of tumor growth and metastasis. OS generated
increased malignant behavior compared with that of SQ. By
understanding the characteristics of murine breast cancer models
established by diverse methods, it is possible to select an
appropriate model to use in further studies.
Acknowledgements
The authors would like to thank Yun-feng Zhao
(Institute of Microbiology, Chinese Academy of Sciences, Beijing,
China) for technical support with the animal experiments and
Jin-Ping Li (Department of Medical Biochemistry and Microbiology,
Uppsala University, Uppsala, Sweden) for manuscript revision.
Funding
The present study was funded by the National Natural
Science Foundation of China (grant nos. 81673924 and 81373815), the
Beijing Natural Science Foundation (grant no. 7162084), the
Specialized Research Fund for the Doctoral Program of Higher
Education of China (grant no. 20131107110014) and the Swedish
Cancer Foundation (grant no. 150815).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YZ, GLZ, XS, KXC, GWY and MWY conducted the
experiments. XMW and GLZ conceived and designed the experiments. CM
and NN analyzed the data. YZ and GLZ wrote the manuscript.
Ethics approval and consent to
participate
Animal experiments were conducted in accordance with
the Provision and General Recommendation of Chinese Experimental
Animals Administration Legislation and were approved by the
Institution of Animal Care and Use Committee of Capital Medical
University (ref. no. AEEI-2014-052).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Torre LA, Bray F, Siegel RL, Ferlay J,
Lortet-Tieulent J and Jemal A: Global cancer statistics, 2012. CA
Cancer J Clin. 65:87–108. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Shi XJ, Au WW, Wu KS, Chen LX and Lin K:
Mortality characteristics and prediction of female breast cancer in
China from 1991 to 2011. Asian Pac J Cancer Prev. 15:2785–2791.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Light DW: Global drug discovery: Europe is
ahead. Health Aff (Millwood). 28:w969–w977. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ottewell PD, Coleman RE and Holen I: From
genetic abnormality to metastases: Murine models of breast cancer
and their use in the development of anticancer therapies. Breast
Cancer Res Treat. 96:101–113. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Rashid OM and Takabe K: Animal models for
exploring the pharmacokinetics of breast cancer therapies. Expert
Opin Drug Metab Toxicol. 11:221–230. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wagner KU: Models of breast cancer: Quo
vadis, animal modeling? Breast Cancer Res. 6:31–38. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Donehower LA, Harvey M, Slagle BL,
McArthur MJ, Montgomery CA Jr, Butel JS and Bradley A: Mice
deficient for p53 are developmentally normal but susceptible to
spontaneous tumours. Nature. 356:215–221. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Escobar Galvis ML, Jia J, Zhang X,
Jastrebova N, Spillmann D, Gottfridsson E, van Kuppevelt TH,
Zcharia E, Vlodavsky I, Lindahl U and Li JP: Transgenic or
tumor-induced expression of heparanase upregulates sulfation of
heparan sulfate. Nat Chem Biol. 3:773–778. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Matsui Y, Halter SA, Holt JT, Hogan BL and
Coffey RJ: Development of mammary hyperplasia and neoplasia in
MMTV-TGF alpha transgenic mice. Cell. 61:1147–1155. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ursini-Siegel J, Schade B, Cardiff RD and
Muller WJ: Insights from transgenic mouse models of ERBB2-induced
breast cancer. Nat Rev Cancer. 7:389–397. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Menezes ME, Das SK, Emdad L, Windle JJ,
Wang XY, Sarkar D and Fisher PB: Genetically engineered mice as
experimental tools to dissect the critical events in breast cancer.
Adv Cancer Res. 121:331–382. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chakravarty G, Mathur A, Mallade P,
Gerlach S, Willis J, Datta A, Srivastav S, Abdel-Mageed AB and
Mondal D: Nelfinavir targets multiple drug resistance mechanisms to
increase the efficacy of doxorubicin in MCF-7/Dox breast cancer
cells. Biochimie. 124:53–64. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Li H, Pan GF, Jiang ZZ, Yang J, Sun LX and
Zhang LY: Triptolide inhibits human breast cancer MCF-7 cell growth
via downregulation of the ERα-mediated signaling pathway. Acta
Pharmacol Sin. 36:606–613. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Habu S, Fukui H, Shimamura K, Kasai M,
Nagai Y, Okumura K and Tamaoki N: In vivo effects of anti-asialo
GM1. I. Reduction of NK activity and enhancement of transplanted
tumor growth in nude mice. J Immunol. 127:34–38. 1981.PubMed/NCBI
|
|
15
|
Marangoni E, Vincent-Salomon A, Auger N,
Degeorges A, Assayag F, de Cremoux P, de Plater L, Guyader C, De
Pinieux G, Judde JG, et al: A new model of patient tumor-derived
breast cancer xenografts for preclinical assays. Clin Cancer Res.
13:3989–3998. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Schuh JC: Trials, tribulations, and trends
in tumor modeling in mice. Toxicol Pathol. 32 Suppl 1:S53–S66.
2004. View Article : Google Scholar
|
|
17
|
Talmadge JE, Singh RK, Fidler IJ and Raz
A: Murine models to evaluate novel and conventional therapeutic
strategies for cancer. Am J Pathol. 170:793–804. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Gravekamp C, Sypniewska R, Gauntt S,
Tarango M, Price P and Reddick R: Behavior of metastatic and
nonmetastatic breast tumors in old mice. Exp Biol Med (Maywood).
229:665–675. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Singh M, Ramos I, Asafu-Adjei D,
Quispe-Tintaya W, Chandra D, Jahangir A, Zang X, Aggarwal BB and
Gravekamp C: Curcumin improves the therapeutic efficacy of
Listeria(at)-Mage-b vaccine in correlation with improved T-cell
responses in blood of a triple-negative breast cancer model 4T1.
Cancer Med. 2:571–582. 2013. View
Article : Google Scholar : PubMed/NCBI
|
|
20
|
Takahashi K, Nagai N, Ogura K, Tsuneyama
K, Saiki I, Irimura T and Hayakawa Y: Mammary tissue
microenvironment determines T cell-dependent breast
cancer-associated inflammation. Cancer Sci. 106:867–874. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Tao K, Fang M, Alroy J and Sahagian GG:
Imagable 4T1 model for the study of late stage breast cancer. BMC
Cancer. 8:2282008. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zhou H, Roy S, Cochran E, Zouaoui R, Chu
CL, Duffner J, Zhao G, Smith S, Galcheva-Gargova Z, Karlgren J, et
al: M402, a novel heparan sulfate mimetic, targets multiple
pathways implicated in tumor progression and metastasis. PLoS One.
6:e211062011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Lee HS, Ha AW and Kim WK: Effect of
resveratrol on the metastasis of 4T1 mouse breast cancer cells in
vitro and in vivo. Nutr Res Pract. 6:294–300. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Mehta RR, Katta H, Kalra A, Patel R, Gupta
A, Alimirah F, Murillo G, Peng X, Unni A, Muzzio M and Mehta RG:
Efficacy and mechanism of action of Deguelin in suppressing
metastasis of 4T1 cells. Clin Exp Metastasis. 30:855–866. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Gibson-D'Ambrosio RE, Samuel M and
D'Ambrosio SM: A method for isolating large numbers of viable
disaggregated cells from various human tissues for cell culture
establishment. In Vitro Cell Dev Biol. 22:529–534. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Weigand A, Boos AM, Tasbihi K, Beier JP,
Dalton PD, Schrauder M, Horch RE, Beckmann MW, Strissel PL and
Strick R: Selective isolation and characterization of primary cells
from normal breast and tumors reveal plasticity of adipose derived
stem cells. Breast Cancer Res. 18:322016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Weidner N, Semple JP, Welch WR and Folkman
J: Tumor angiogenesis and metastasis-correlation in invasive breast
carcinoma. N Engl J Med. 324:1–8. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Jordan VC: Proven value of translational
research with appropriate animal models to advance breast cancer
treatment and save lives: The tamoxifen tale. Br J Clin Pharmacol.
79:254–267. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Clarke R: Animal models of breast cancer:
Their diversity and role in biomedical research. Breast Cancer Res
Treat. 39:1–6. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Morioka CY, Saito S, Ohzawa K, Asano S,
Hibino Y, Nakada Y, Kita KI and Watanabe A: Subcutaneously
inoculated cells and implanted pancreatic cancer tissue show
different patterns of metastases in Syrian golden hamsters. JOP.
1:183–190. 2000.PubMed/NCBI
|
|
31
|
Rao Q, You A, Guo Z, Zuo B, Gao X, Zhang
T, Du Z, Wu C and Yin H: Intrahepatic tissue implantation
represents a favorable approach for establishing orthotopic
transplantation hepatocellular carcinoma mouse models. PLoS One.
11:e1482632016. View Article : Google Scholar
|
|
32
|
de la Cruz-Merino L, Barco-Sánchez A,
Henao Carrasco F, Nogales Fernández E, Vallejo Benítez A, Brugal
Molina J, Martínez Peinado A, Grueso López A, Ruiz Borrego M, Codes
Manuel de Villena M, et al: New insights into the role of the
immune microenvironment in breast carcinoma. Clin Dev Immunol.
2013:7853172013. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Rashid OM, Nagahashi M, Ramachandran S,
Dumur C, Schaum J, Yamada A, Terracina KP, Milstien S, Spiegel S
and Takabe K: An improved syngeneic orthotopic murine model of
human breast cancer progression. Breast Cancer Res Treat.
147:501–512. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Rashid OM, Nagahashi M, Ramachandran S,
Dumur CI, Schaum JC, Yamada A, Aoyagi T, Milstien S, Spiegel S and
Takabe K: Is tail vein injection a relevant breast cancer lung
metastasis model? J Thorac Dis. 5:385–392. 2013.PubMed/NCBI
|
|
35
|
Bibby MC: Orthotopic models of cancer for
preclinical drug evaluation: Advantages and disadvantages. Eur J
Cancer. 40:852–857. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Fidler IJ: The pathogenesis of cancer
metastasis: The ‘seed and soil’ hypothesis revisited. Nat Rev
Cancer. 3:453–458. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Nieman KM, Romero IL, Van Houten B and
Lengyel E: Adipose tissue and adipocytes support tumorigenesis and
metastasis. Biochim Biophys Acta. 1831:1533–1541. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Hammond E, Brandt R and Dredge K: PG545, a
heparan sulfate mimetic, reduces heparanase expression in vivo,
blocks spontaneous metastases and enhances overall survival in the
4T1 breast carcinoma model. PLoS One. 7:e521752012. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Kim JB, Urban K, Cochran E, Lee S, Ang A,
Rice B, Bata A, Campbell K, Coffee R, Gorodinsky A, et al:
Non-invasive detection of a small number of bioluminescent cancer
cells in vivo. PLoS One. 5:e93642010. View Article : Google Scholar : PubMed/NCBI
|