Introduction
Renal cell carcinoma (RCC) accounts for
approximately 3% of adult malignancies (1). The incidence of RCC has increased over
the last two decades worldwide and affects all ethnic groups.
Although RCC develops slowly, over 200,000 new cases of kidney
cancer are diagnosed each year (2).
Improved RCC detection has resulted in increased diagnoses and is
attributed to medical evaluation for unrelated conditions, routine
health checkups and improved methods of detection, such as computed
tomography or MRI. Despite increased detection, the prognosis
varies widely; about 30% of patients have metastatic disease when
diagnosed, and 20–30% of patients have local or distant recurrence
five years after radical or partial nephrectomy (3,4). Apart
from RCC being highly resistant to chemotherapy, radiation, and
immunotherapy, few predictive or prognostic markers have been
identified. Identification of an RCC prognostic marker would hasten
the development of new therapeutic strategies, and improve patient
survival.
Increased rates of glycolysis and lipogenesis occur
in most cancers as described by the Warburg effect (5). Some enzymes involved in this increased
metabolic rate have changes in both molecular and protein
expression levels. Among these enzymes, ATP citrate lyase (ACLY)
serves as a physiological shunt between glucose metabolism and
fatty acid synthesis (6). ACLY can
produce acetyl-CoA, which is a building block for cholesterol,
fatty acid synthesis, because ACLY is closely related to energy
metabolism, so it is imperative to support cells growth. However,
ACLY expression patterns and its association with
clinicopathological features of RCC remain unclear. In this study,
we investigated the expression levels of ACLY at both RNA and
protein level in RCC tissues, and tested the circulating ACLY
level, and then determined whether the expression level of ACLY was
correlated to clinicopathological parameters of patients with
RCC.
Materials and methods
Tissue and serum samples
This study was approved by the ethics board of the
Harbin Medical University Cancer Hospital. Informed consent was
obtained from all patients before inclusion in this study. Fresh
RCC tissue was collected after radical nephrectomy. Adjacent normal
kidney tissues 0.5–2 cm from the tumor margin were also collected.
All of these tissue samples were stored in liquid nitrogen or were
fixed with 1% (v/v) paraformaldehyde. Patient serum samples
were collected during admission to the hospital and were stored at
−20°C. All patients were classified according to the current WHO
classification for RCC and tumors were staged according to the
Union for Internationale Cancer Control (UICC) classification.
Demographic and clinicopathological data were also obtained.
Cell lines
Human RCC, 786-0 and GRC-1 (7), and normal human kidney cells, HK-2 were
purchased from the Cell Bank of the Chinese Academy of Sciences
(Shanghai, China). All of the cells were maintained in DMEM (Gibco;
Thermo Fisher Scientific, Inc., Waltham, MA, USA) supplemented with
10% FBS (Gibco; Thermo Fisher Scientific, Inc.) and incubated at
37°C in humidified air with 5% CO2.
Immunohistochemistry and tissue
section scoring
Fixed specimens were embedded in paraffin and cut
making 4 µm thick serial sections for hematoxylin & eosin
(H&E) and IHC staining according to standard methods. As for
IHC staining, briefly, each section was deparaffinized and
rehydrated, and then the sections were autoclaved in 10 mM citrate
buffer at 120°C for 2 min for antigen retrieval. Next, the sections
were washed three times with phosphate-buffered saline (PBS, pH
7.3), and then soaked in 3% H2O2 for 15 min
and subsequently washed three times. After non-specific sites were
blocked with 10% normal calf serum, sections were incubated with
primary antibody (anti-ACLY antibody at 1:300 dilution, D221957;
Sangon Biotech Co. Ltd., Shanghai, China) overnight at 4°C
overnight. After antibody incubation, sections were then washed
with PBS three times. Two-step incubations with a secondary
antibody were performed using biotin-labeled goat anti-rabbit IgG
and horseradish peroxidase-labeled avidin (A0277 and A0303;
Beyotime Institute of Biotechnology, Haimen, China). DAB counter
staining then followed, and the sections were re-stained with
hematin (H8070; Beijing Solarbio Science & Technology Co.,
Ltd., Beijing, China). Finally, the sections were independently
evaluated by pathologists. Sections were scored according to the
percentage of cytoplasm-positive cells and intensity as follows: 0,
no immunostaining; 1, weak; 2, moderate; and 3, strong; 0,
negative; 1, <25% positive cells; 2, 26–50% positive cells; 3,
>50% positive cells, respectively (8). The score was the sum of the extension
and the staining intensity. The samples with scores 0–2 were
considered negative, and those with scores 3–6 were considered
positive.
Reverse transcription-quantitaive
polymerase chain reaction (RT-qPCR)
Total RNA was extracted from tissue samples using
the TRIzol reagent (Invitrogen, Beijing, China). RT-qPCR was
performed using an SYBR Premix Ex Taq™ Reverse Transcription-PCR
kit (Takara Bio, Inc., Otsu, Japan). The primers for human ACLY
were, while the primers for β-actin were. The method of Livak and
Schmittgen (9) and reference ΔCq
values were used for calculations of ΔΔCq and all relative quantity
values for assessing expression of ACLY mRNA in RCC and adjacent
tissue. β-actin was used as internal controls.
Western blot analysis
Total protein was obtained from frozen tissues as
previously described (10). Briefly,
40 µg of total protein was separated on an SDS-PAGE gel, the
proteins then were transferred to a nitrocellulose membrane and
probed with primary antibodies (anti-human ACLY antibody at 1:1,000
dilution, D221957; Sangon Biotech Co. Ltd.) overnight at 4°C. The
following day, the membranes were washed with Tris-buffered saline
and Tween-20 and incubated with a secondary anti-rabbit IgG
antibody conjugated with horseradish peroxidase (WLA023; Wanleibio
Co., Ltd., Shenyang, China). Next, membranes were incubated with
enhanced chemiluminescence, and protein expression was visualized
after exposure to X-ray film. Densitometry analysis was performed.
β-actin (1:1,000, WL01845; Wanleibio Co., Ltd.) was used as an
internal control.
Determination of serum ACLY
concentrations
According to a previous study (11), ACLY serum concentrations were measured
using a commercial ELISA kit (Glory Science Co., Ltd., Shanghai
China).
Transfection with siRNA
siRNA targeting ACLY and negative controls were
synthesized by GenePharma. According to the manufacturer's
recommendations, all cell transfections were carried out with the
Lipofectamine® 2000 Transfection Reagent (Invitrogen;
Thermo Fisher Scientific, Inc., Waltham, MA, USA).
Cell proliferation assay
Cell proliferation was determined using a Cell
Counting Kit (CCK-8; Dojindo Molecular Technologies, Inc.,
Kumamoto, Japan). The 786-0, GRC-1, HK-2, 786-0 transfected with
siRNA and 786-0 transfected with negative controls were plated in
96-well plates at a density of 5×103 cells/well in 100
µl of media. Cells were then cultured for 72 h. The absorbance of
cells was measured at 450 nm. The OD values measured represented
cellular proliferation. All experiments were performed in
triplicate.
Transwell migration assay
The assay was performed using 24 well Corning
chamber plates with an 8 µm pore polycarbonate membrane filters
(Corning Incorporated, Corning, NY, USA). 1×105
cells/well were placed in the upper chamber containing DMEM with
10% FBS; the lower chamber also contained DMEM with 10% FBS. The
plates with cells were incubated at 37°C in a 5% CO2
incubator for 48 h. After incubation, cells on the membrane filter
were fixed with 4% (v/v) formaldehyde for 10 min at room
temperature. The cells were then stained with 0.5% crystal violet
for 30 min. The migratory cells on the lower membrane surface were
counted using bright field microscopy at 200 × magnification. Five
random fields were counted for each filter, and each sample was
assayed in triplicate.
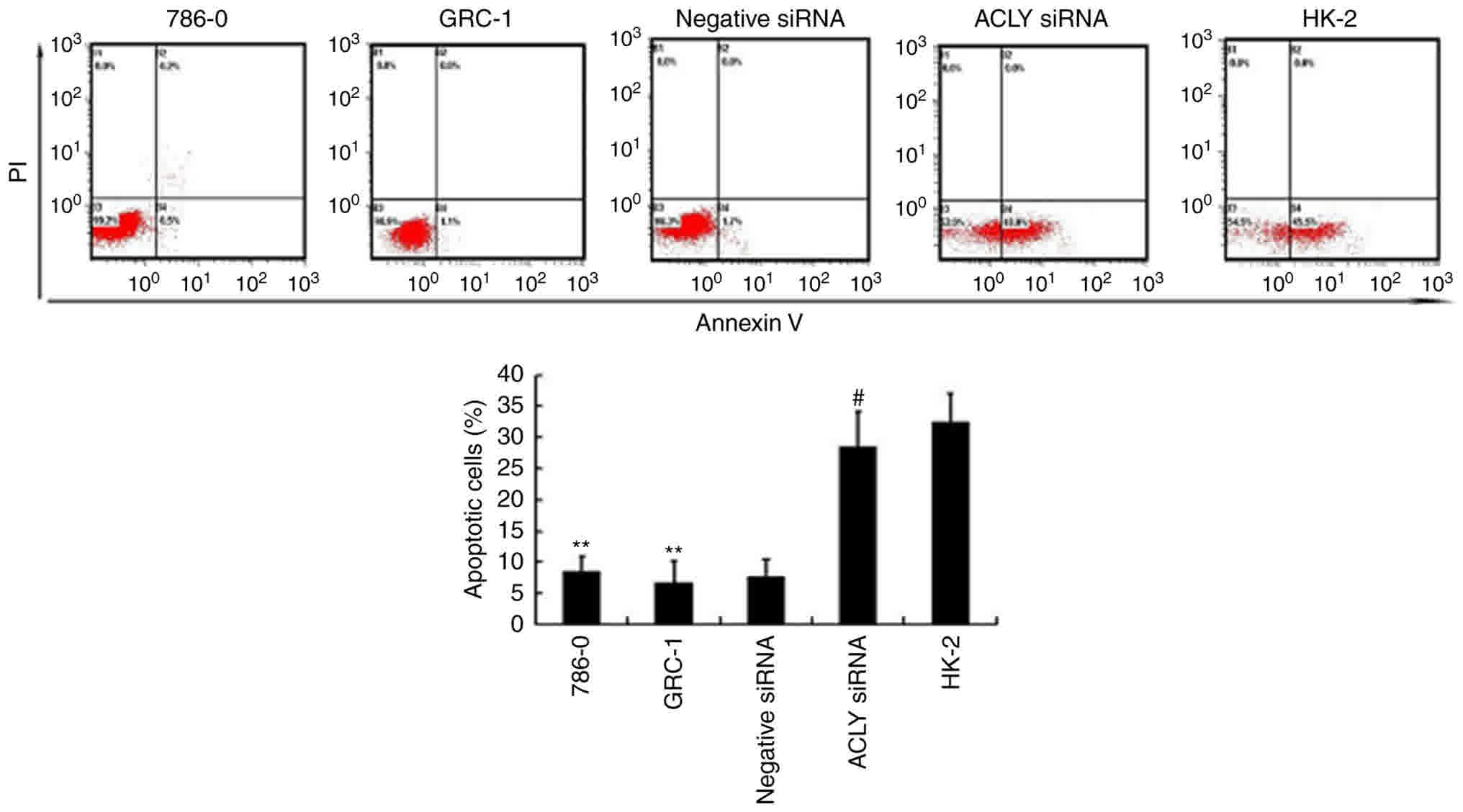
Cell apoptosis assessment
Cellular apoptosis was measured using flow cytometry
(BD Accuri Cytometers, Ann Arbor, MI USA), Annexin V, and propidium
iodide (PI) (Apoptosis Detection kit, Annexin V-FITC; BD,
Biosciences Pharmingen, San Diego, CA, USA), according to the
manufacturer's guidelines.
Statistical analysis
All statistical analyses were performed using the
SSPS (vesrion 19.0; SPSS, Inc., Chicago, IL, USA) software suite.
Differences in RCC ACLY expression compared with adjacent kidney
tissue ACLY expression were evaluated by one-way ANOVA followed
with Newman-Keuls post hoc test. P<0.05 was considered to
indicate a statistically significant difference.
Results
Clinicopathological findings in RCC
patients
The clinicopathologic characteristics of study
patients with RCC are shown in Table
I. Patients ranged in age from 31 to 77 years and included 21
males and 12 females. All patients in the study were diagnosed with
clear cell RCC (ccRCC) by pathologists. The tumor Fuhrman grades
ranged from I to IV (12), and the
TNM stages ranged from T1N0M0 to T3bN0M0.
 | Table I.Association of ACLY expression with
TNM stage and Fuhrman grade in ccRCC. |
Table I.
Association of ACLY expression with
TNM stage and Fuhrman grade in ccRCC.
|
|
| ACLY expression
(score for percentage of positive cells) |
|
|---|
|
|
|
|
|
|---|
|
Characteristics | No. | 0 | 1 | 2 | 3 | P-value |
|---|
| TNM stage |
|
|
|
|
| <0.05 |
|
T1N0M0 | 23 | 3 (13.0) | 2 (8.8) | 3
(13.0) | 15 (65.2) |
|
|
T2N0M0 | 6 | 0 | 1 (16.7) | 0 | 5 (83.3) |
|
| T2N1M0
or T2N0M1 | 2 | 0 | 0 | 1
(50.0) | 1 (50.0) |
|
|
T3N0M0 | 2 | 0 | 0 | 0 | 2 (100) |
|
| Nuclear grade |
|
|
|
|
| <0.01 |
| I | 11 | 2 (18.2) | 0 | 1 (9.1) | 8 (72.7) |
|
| II | 14 | 1 (7.1) | 1 (7.1) | 2
(14.3) | 10 (71.5) |
|
|
III–IV | 8 | 0 | 0 | 1
(12.5) | 7 (87.5) |
|
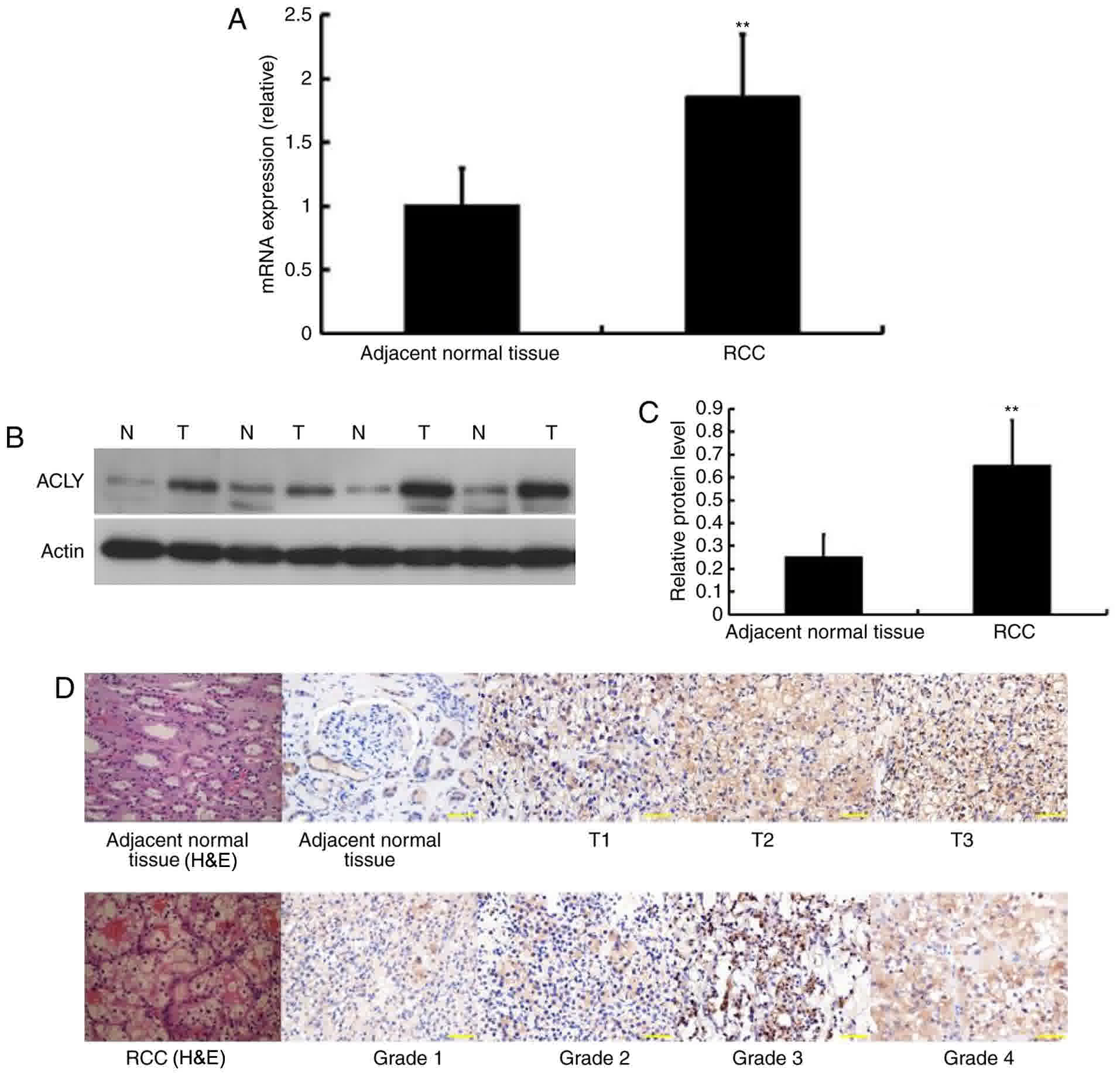
ACLY is highly expressed in primary
RCC tissues
We evaluated the ACLY expression levels at the
molecular level using RT-PCR. Mean ACLY mRNA expression in ccRCC
was significantly higher when compared with surrounding normal
kidney tissue in paired analyses (Fig.
1A).
To further investigate the ACLY protein expression
levels in ccRCC and adjacent normal tissues, we performed
immunoblotting assays. Of the 33 tumor and adjacent tissues, 30
cases showed significantly higher expression of ACLY levels in
ccRCC tissues than in adjacent tissues, the other 3 presented weak
expression. The remaining two ccRCC cases only showed weak ACLY
expression. These results were in line with previous IHC findings
for ACLY expression (Fig. 1B and
C).
According to the IHC, we found that ACLY was
detected in both cytoplasm and nucleus. Moreover, compared to the
adjacent normal tissues, primary ccRCC tissues showed significantly
higher expression of ACLY. More importantly, with an increasing
Fuhrman grade and clinical stage, ACLY expression increased
progressively. A representative illustration was shown in Fig. 1D.
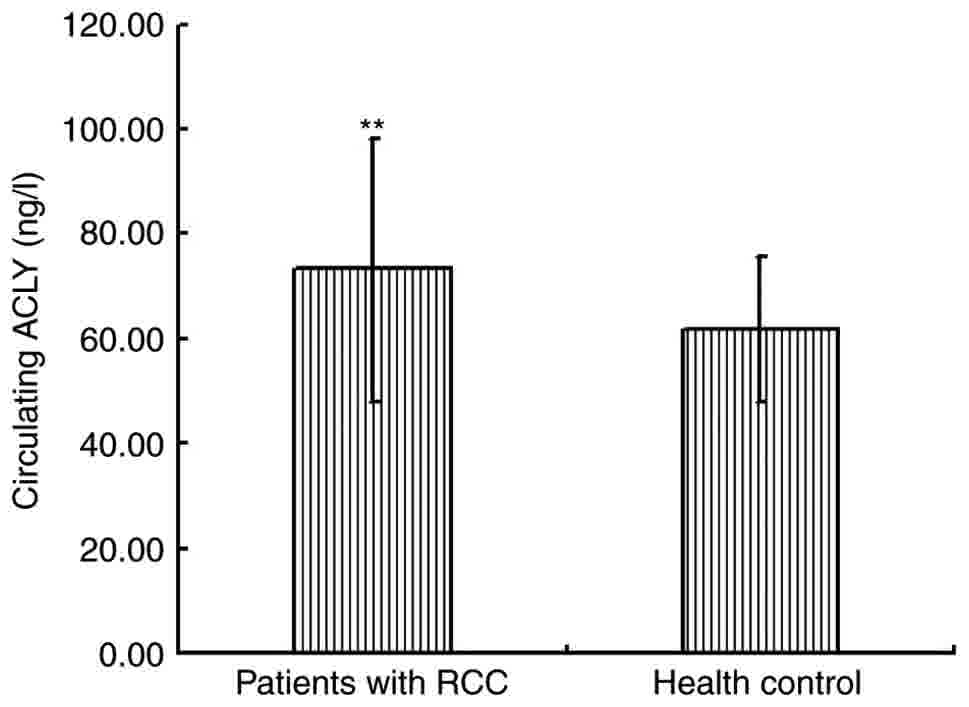
Determination of serum ACLY
concentrations
We assessed serum ACLY by ELISA in 10 healthy men
and 37 patients with ccRCC. We found that ACLY serum concentrations
were significantly higher in patients with ccRCC, compared with
healthy controls (Fig. 2). Moreover,
serum ACLY concentrations correlated with the TNM stage and Fuhrman
grade of ccRCC and could be related to the higher metabolic rate in
cancer cells.
The relationship ACLY expression in ccRCC with
clinicopathologic parameters. Next, we analyzed the relationship
between the intensity of ACLY expression ccRCC and
clinicopathologic parameters, such as age and sex of the patients,
TNM stage and Fuhrman nuclear grade. The ACLY expression intensity
was classified as negative, weak, moderate, and strong expression.
We found no significant relationship between the intensity of ACLY
expression and the age or sex of the patients. Of the patients with
ccRCC, the high percentage of ACLY positive cells was significantly
associated with both higher Fuhrman nuclear grade and higher TNM
stage (Table II).
 | Table II.Expression of ACLY protein in RCC
tissues by immunohistochemistry. |
Table II.
Expression of ACLY protein in RCC
tissues by immunohistochemistry.
|
|
| ACLY
expression |
|
|---|
|
|
|
|
|
|---|
|
Characteristics | No. | 0 | 1 | 2 | 3 | P-value |
|---|
| Tumor diameter,
cm |
|
|
|
|
| <0.05 |
|
<7 | 23 | 3 | 2 | 3 | 15 |
|
|
7–10 | 6 | 0 | 1 | 0 | 5 |
|
|
>10 | 4 | 0 | 0 | 1 | 3 |
|
| Nuclear grade |
|
|
|
|
| <0.01 |
| I | 11 | 2 | 0 | 1 | 8 |
|
| II | 14 | 1 | 1 | 2 | 10 |
|
|
III–IV | 8 | 0 | 0 | 1 | 7 |
|
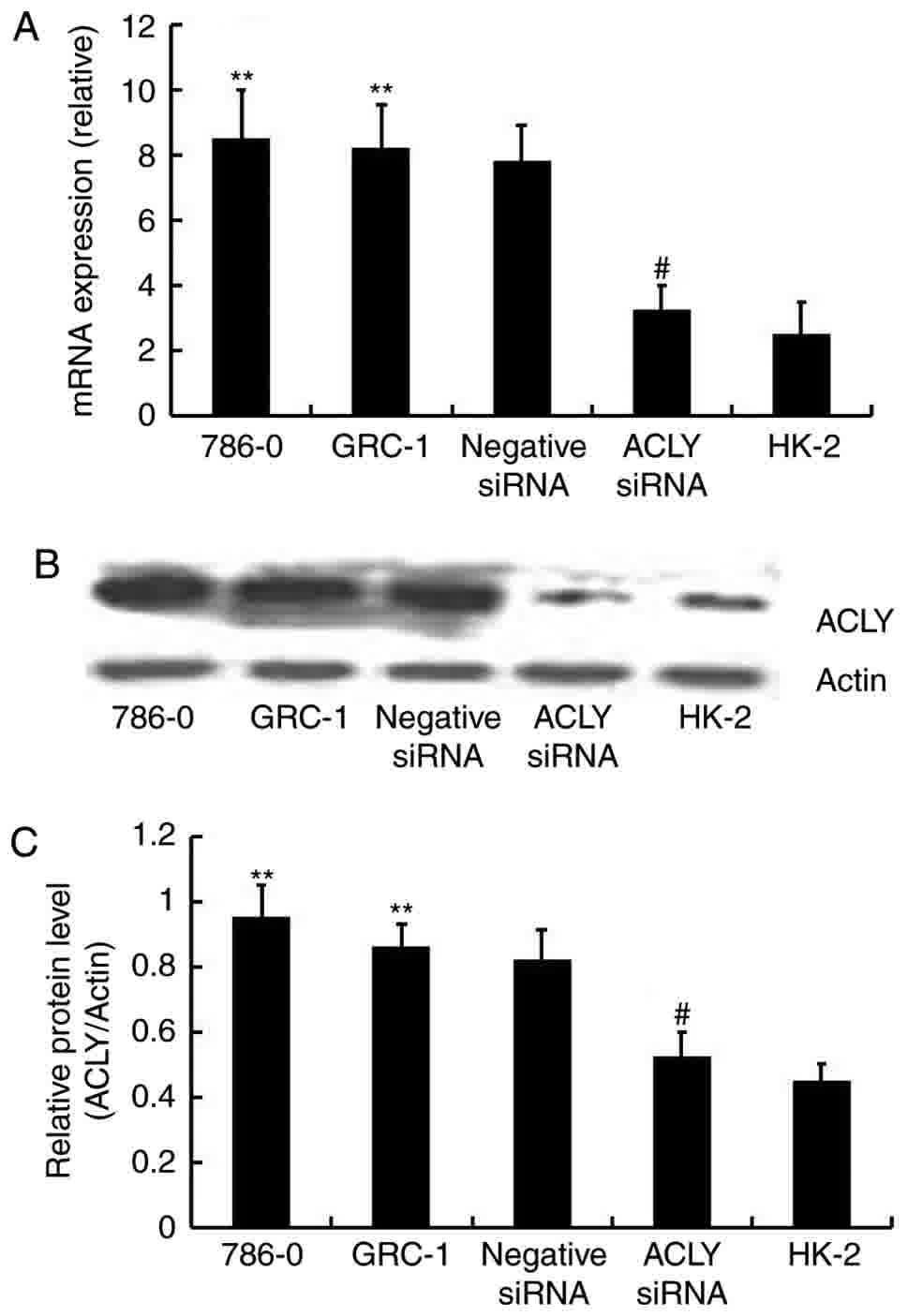
siRNA downregulated ACLY expression at
both the molecular and protein levels
We knocked down ACLY expression using ACLY-specific
siRNA to evaluate the effects of ACLY downregulation on RCC cells.
We confirmed the knockdown effect using RT-qPCR and western
blotting methods and found that the level of ACLY mRNA (Fig. 3A) and protein expression (Fig. 3B and C) were significantly decreased
in HK-2 cells, and 786-0 cells transfected siRNA. The results
indicated that ACLY expression was successfully downregulated in
RCC cells.
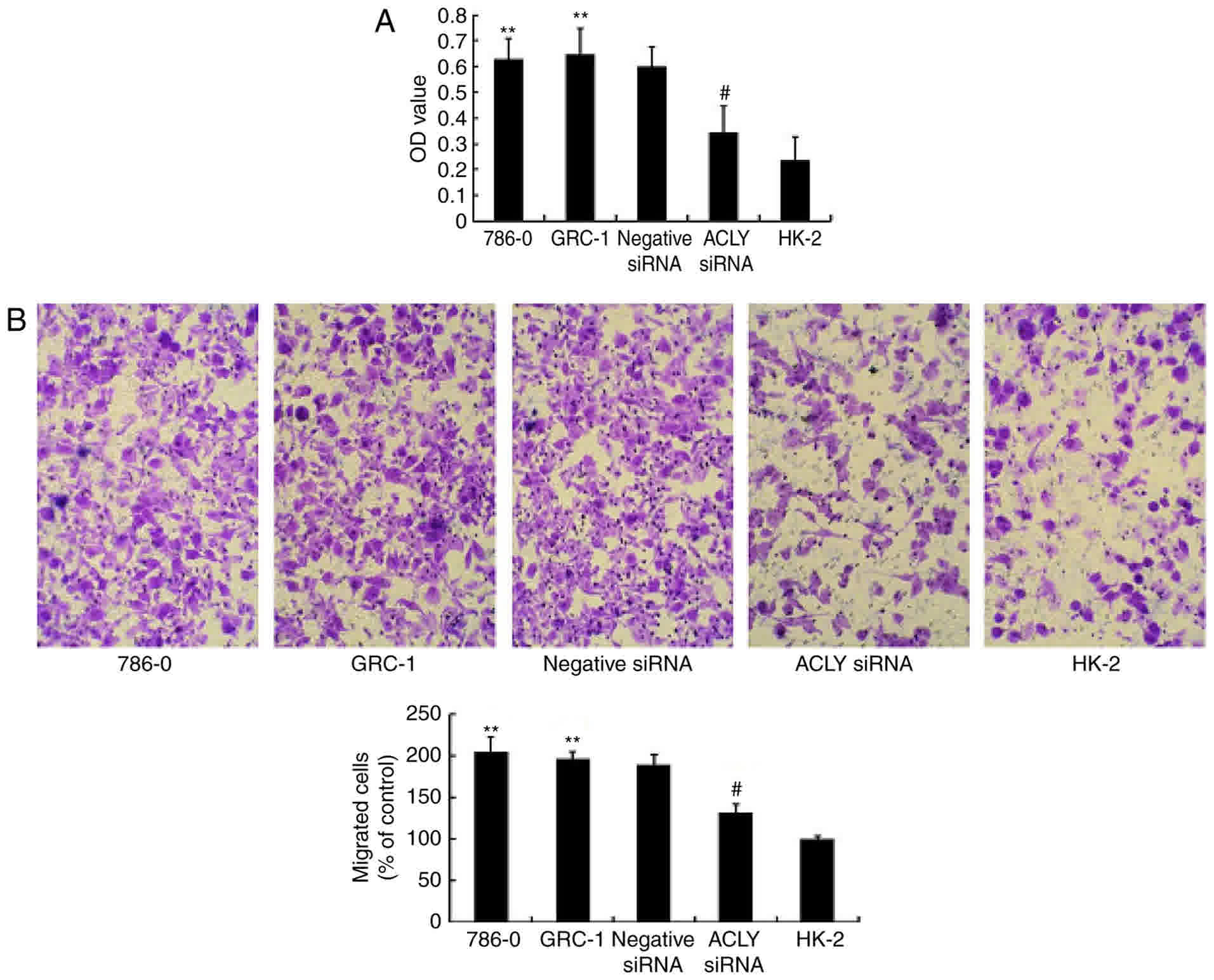
siRNA downregulated ACLY inhibited
proliferation and migration of RCC cells, but promoted apoptosis of
the cells
Compared with 786-0, GRC-1, and HK-2 cells,
transfected 786-0 cells demonstrated significantly suppressed
proliferation (P<0.01; Fig. 4A),
and fewer transfected 786-0 cells migrated through the transwell
compared with negative controls, (P<0.05 Fig. 4B). And, flow cytometry showed in
Fig. 5, that RCC knocked down with
ACLY promotes apoptosis as compared with transfected HK-2 or
non-transfected RCC.
Discussion
Several studies demonstrated that cancer cell
metabolism could be changed if sufficient ATP and the building
blocks needed to sustain molecular synthesis are provided (13–15).
Reprogramming cancer metabolism is also one of the hallmarks of
cancer (16). In RCC, glucose uptake
and glycolytic activity were significantly increased (17). ACLY is a key enzyme that participates
in de novo glycolysis and lipogenesis. Our study found that
ACLY expression was significantly increased in RCC compared with
adjacent normal tissue. Moreover, IHC showed that high ACLY
expression was primarily located in the cytoplasm of renal cancer
cells. Also, our results suggested that ACLY expression was closely
related to the stages and grades of RCC. Compared to healthy
control subjects, serum ACLY concentrations were higher in RCC
thant in negative controls. These findings suggest that ACLY could
contribute to glycolysis and lipogenesis in RCC and that ACLY might
be a useful marker for predicting, prognosing, and providing early
diagnosis of RCC.
High ACLY expression in RCC might be involved in the
metabolic shift of this cancer, suggesting that RCC progress relies
on aerobic glycolysis, which is also observed in fumarate hydratase
(FH)-deficient RCC and succinate dehydrogenase-deficient RCC
(18,19). Although aerobic glycolysis has not
been shown to produce sufficient ATP for RCC, but it has does
facilitate cancer cell metabolism of nutrients within the biomass
(nucleotides, amino acids, and lipids) that is required for cancer
cell proliferation (20). Glycolytic
intermediates, such as acetyl-CoA, are also the most important
precursors of fatty acid. Acetyl-CoA originates from glucose and is
used to synthesize citrate in the tricarboxylic acid cycle, which
is needed to maintain high ATP/ADP and NADH/NAD+ in
proliferating cells (21). Aerobic
glycolysis may at least, partly account for the higher ACLY
expression at the higher stages and grades of RCC in our study.
RCC, especially ccRCC, is histologically
characterized by high tumor cell lipid content and a richly
vascularized tumor stroma (22).
Moreover, enhanced fatty acid synthesis is also required for
proliferation and differentiation of malignant cells. Because ACLY
is a key enzyme in the de novo lipogenesis, by catalyzing
the conversion of cytosolic citrate into acetyl CoA and
oxaloacetate, high molecular and protein ACLY expression in RCC
might be closely linked with high tumor cell lipid content. A
recent study also demonstrated that de novo
glucose-dependent ACLY mediated lipogenesis inhibited ACLY
activity, which could result in inhibition of proliferation and
defective endomembrane expansion (23). Upregulated ACLY activity can increase
lipid droplet formation forming building blocks to support growth
in breast cancer cells (24).
Additionally, the possible mechanism for anti-apoptosis effect of
ACLY in RCC may be related with promotion of lipogenesis in
mitochondria, because inhibition of ACLY would impair lipogenesis,
involving activation of AMPK and blocking of its downstream protein
ACC1 (25), further mitochondrial
function would be impaired (26).
Moreover, intrinsic apoptotic pathway is the mitochondria-dependent
in some extent (27). Therefore, a
deep understanding of the role of high ACLY expression may provide
opportunities to find novel and more effective therapeutic
approaches.
Based on ACLY expression levels in this study, ACLY
might become a novel marker for prognostic evaluation in RCC. Our
data showed that high ACLY expression was observed in high RCC
grades and stages. We also showed that ACLY overexpression
correlated with poor RCC differentiation. A previous report on
non-small cell lung cancer demonstrated that ACLY is a useful
marker for non-small cell lung cancer identification and higher
levels correlated with a poor prognosis (28). This finding was consistent with our
present observations. Generally speaking, ACLY localized in the
cytoplasm, however, we also observed that the ACLY protein
localized in both the cytoplasm and nucleus in clinical ccRCC
samples, which showed that ACLY overexpression may not only be
involved in energy metabolism, but may take part in the regulation
of gene expression, such as DNA regulation, and methyltransferase-1
and histone acetylation, in RCC (20,29,30). Taken
together, we show that these factors contribute to cancer
development. Further studies are required to to gain a deeper
understanding of the molecular basis of different ACLY subcellular
localizations in RCC.
Finally, since ACLY downregulation by siRNA in RCC
cells negatively affect biological behavior, in vitro, we
think that ACLY could play an important role in maintaining the
overall metabolism, progression, and invasion of tumor cells.
However, precise cancer metabolism is complex, but at least we can
say that the adverse effects of lower ACLY levels on the tumor
cells could be at least partially responsible for decreased
lipogenesis and impaired biological energy. Recently, the study of
Xin et al (31) stated that
decreased ACLY could reduce tumor growth and invasion and promote
apoptosis in Saos-2, PC-3, Hela, and A549 cells, in vitro,
which could have been due to decreased expression of common
intermediates in the mevalonate pathway. Although the precise
mechanisms for the anti-apoptosis effect of ACLY remain unclear,
ACLY inhibition impairs lipogenesis, which involves AMPK activation
and blockage of its downstream protein ACC1 (32), and impairs mitochondrial function
(26). Moreover, the intrinsic
apoptotic pathway is mitochondria-dependent to some extent
(27). We, therefore, suggest that
the anti-apoptosis effect of ACLY in RCC may be related to the
advancement of lipogenesis in mitochondria. However, another recent
study indicated that the interaction between cytoplasmic low
molecular weight cyclin-E and ACLY upregulates ACLY enzymatic
activity, promoting migration and invasion of breast cancer cells
growth (33).
The small number of cases and lack of long-term
follow-up are major limitation of our study. To investigate the
precise effect of ACLY expression on overall survival or progress
free survival in ccRCC, further studies with a large number of
participants and long-term follow-up are warranted.
In conclusion, our results show much higher ACLY
expression in RCC compared with adjacent normal kidney tissue. And,
ACLY protein expression was located in the cytoplasm and nucleus
and was associated with RCC stage and nuclear grade. Therefore,
ACLY is should be considered to be a new marker to evaluate the
biological aggressiveness of RCC, and be a potential target for RCC
treatment.
Acknowledgements
The authors would like to thank Dr Hongshuang Dai
and Ms Haibo Li for their assistance in collecting samples and
technical assistance.
Funding
The study was supported by Heilongjiang postdoctoral
scientific research developmental fund (grant no. LBH-Q15104).
Availability of data and materials
The datasets used or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
LT and CL conceived and designed the experiments. LT
and YS performed the experiments and drafted the manuscript. CL
collected the samples. YCa and YCe performed the cell biological
studies and the statistical analysis. WW performed the ELISA assay.
YW and JL performed the statistical analysis. YX collected and
analyzed the data, and revised the manuscript. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Board of
Harbin Medical University Cancer Hospital. Written consent was
obtained by all patients who participated in the study.
Consent for publication
All patients participated in the present study
provided written informed consent for the publication.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Patel C, Ahmed A and Ellsworth P: Renal
cell carcinoma: A reappraisal. Urol Nurs. 32:182–190.
2012.PubMed/NCBI
|
|
2
|
Saito K and Kihara K: Role of C-reactive
protein as a biomarker for renal cell carcinoma. Exp Rev Anticancer
Ther. 10:1979–1989. 2010. View Article : Google Scholar
|
|
3
|
Crispen PL, Boorjian SA, Lohse CM,
Leibovich BC and Kwon ED: Predicting disease progression after
nephrectomy for localized renal cell carcinoma: The utility of
prognostic models and molecular biomarkers. Cancer. 113:450–460.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zisman A, Pantuck AJ, Wieder J, Chao DH,
Dorey F, Said JW, deKernion JB, Figlin RA and Belldegrun AS: Risk
group assessment and clinical outcome algorithm to predict the
natural history of patients with surgically resected renal cell
carcinoma. J Clin Oncol. 20:4559–4566. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tran Q, Lee H and Park J, Kim SH and Park
J: Targeting cancer metabolism-revisiting the Warburg effects.
Toxicol Res. 32:177–193. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Deberardinis RJ, Sayed N, Ditsworth D and
Thompson CB: Brick by brick: Metabolism and tumor cell growth. Curr
Opin Genet Dev. 18:54–61. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Jiang Z, Liu X, Chang K, Liu X and Xiong
J: Allyl isothiocyanate inhibits the proliferation of renal
carcinoma cell line GRC-1 by inducing an imbalance between Bcl2 and
bax. Med Sci Monit. 22:4283–4288. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Pinto F, Campanella NC, Abrahão-Machado
LF, Scapulatempo-Neto C, de Oliveira AT, Brito MJ, Andrade RP,
Guimarães DP and Reis RM: The embryonic Brachyury transcription
factor is a novel biomarker of GIST aggressiveness and poor
survival. Gastric Cancer. 19:651–659. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wang H, Liu C, Han J, Zhen L, Zhang T, He
X, Xu E and Li M: HER2 expression in renal cell carcinoma is rare
and negatively correlated with that in normal renal tissue. Oncol
Lett. 4:194–198. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yi X, Pashaj A, Xia M and Moreau R:
Reversal of obesity-induced hypertriglyceridemia by (R)-α-lipoic
acid in ZDF (fa/fa) rats. Biochem Biophys Res Commun. 439:390–395.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fuhrman SA, Lasky LC and Limas C:
Prognostic significance of morphologic parameters in renal cell
carcinoma. Am J Surg Pathol. 6:655–663. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Cantor JR and Sabatini DM: Cancer cell
metabolism: One hallmark, many faces. Cancer Discov. 2:881–898.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ward PS and Thompson CB: Metabolic
reprogramming: A cancer hallmark even Warburg did not anticipate.
Cancer Cell. 21:297–308. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wittig R and Coy JF: The role of glucose
metabolism and glucose-associated signalling in cancer. Perspect
Medicin Chem. 1:64–82. 2008.PubMed/NCBI
|
|
16
|
Hanahan D and Weinberg RA: Hallmarks of
cancer: The next generation. Cell. 144:646–674. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lucarelli G, Galleggiante V, Rutigliano M,
Sanguedolce F, Cagiano S, Bufo P, Lastilla G, Maiorano E, Ribatti
D, Giglio A, et al: Metabolomic profile of glycolysis and the
pentose phosphate pathway identifies the central role of
glucose-6-phosphate dehydrogenase in clear cell-renal cell
carcinoma. Oncotarget. 6:13371–13386. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Tomlinson IP, Alam NA, Rowan AJ, Barclay
E, Jaeger EE, Kelsell D, Leigh I, Gorman P, Lamlum H, Rahman S, et
al: Germline mutations in FH predispose to dominantly inherited
uterine fibroids, skin leiomyomata and papillary renal cell cancer.
Nat Genet. 30:406–410. 2002. View
Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ricketts CJ, Shuch B, Vocke CD, Metwalli
AR, Bratslavsky G, Middelton L, Yang Y, Wei MH, Pautler SE,
Peterson J, et al: Succinate dehydrogenase kidney cancer: An
aggressive example of the Warburg effect in cancer. J Urol.
188:2063–2071. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Vander Heiden MG, Cantley LC and Thompson
CB: Understanding the Warburg effect: The metabolic requirements of
cell proliferation. Science. 324:1029–1033. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hatzivassiliou G, Zhao F, Bauer DE,
Andreadis C, Shaw AN, Dhanak D, Hingorani SR, Tuveson DA and
Thompson CB: ATP citrate lyase inhibition can suppress tumor cell
growth. Cancer Cell. 8:311–321. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Massari F, Ciccarese C, Santoni M,
Brunelli M, Piva F, Modena A, Bimbatti D, Fantinel E, Santini D,
Cheng L, et al: Metabolic alterations in renal cell carcinoma.
Cancer Treat Rev. 41:767–776. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Dufort FJ, Gumina MR, Ta NL, Tao Y, Heyse
SA, Scott DA, Richardson AD, Seyfried TN and Chiles TC:
Glucose-dependent de novo lipogenesis in B lymphocytes: A
requirement for atp-citrate lyase in lipopolysaccharide-induced
differentiation. J Biol Chem. 289:7011–7024. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Lucenay KS, Doostan I, Karakas C, Bui T,
Ding Z, Mills GB, Hunt KK and Keyomarsi K: Cyclin E associates with
the lipogenic enzyme ATP-citrate lyase to enable malignant growth
of breast cancer cells. Cancer Res. 76:2406–2418. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Tyszka-Czochara M, Konieczny P and Majka
M: Caffeic acid expands anti-tumor effect of metformin in human
metastaticcervical carcinoma HTB-34 cells: Implications of AMPK
activation andimpairment of fatty acids de novo biosynthesis. Int J
Mol Sci. 18:E4622017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Jones JE, Esler WP, Patel R, Lanba A, Vera
NB, Pfefferkorn JA and Vernochet C: Inhibition of acetyl-coa
carboxylase 1 (ACC1) and 2 (ACC2) reduces proliferation and de novo
lipogenesis of EGFRvIII human glioblastoma cells. PLoS One.
12:e01695662017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Neely AM, Zhao G, Schwarzer C, Stivers NS,
Whitt AG, Meng S, Burlison JA, Machen TE and Li C:
N-(3-oxo-acyl)-homoserine lactone induces apoptosis primarily
through amitochondrial pathway in fibroblasts. Cell Microbiol.
20:2018. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Migita T, Narita T, Nomura K, Miyagi E,
Inazuka F, Matsuura M, Ushijima M, Mashima T, Seimiya H, Satoh Y,
et al: ATP citrate lyase: Activation and therapeutic implications
in non-small cell lung cancer. Cancer Res. 68:8547–8554. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Gentile Londono T, Lu C, Lodato PM, Tse S,
Olejniczak SH, Witze ES, Thompson CB and Wellen KE: DNMT1 is
regulated by ATP-citrate lyase and maintains methylation patterns
during adipocyte differentiation. Mol Cell Bio. 33:3864–3878. 2013.
View Article : Google Scholar
|
|
30
|
Migita T, Okabe S, Ikeda K, Igarashi S,
Sugawara S, Tomida A, Soga T, Taguchi R and Seimiya H: Inhibition
of ATP citrate lyase induces triglyceride accumulation with altered
fatty acid composition in cancer cells. Int J Cancer. 135:37–47.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Xin M, Qiao Z, Li J, Liu J, Song S, Zhao
X, Miao P, Tang T, Wang L, Liu W, et al: miR-22 inhibits tumor
growth and metastasis by targeting ATP citrate lyase: Evidence in
osteosarcoma, prostate cancer, cervical cancer and lung cancer.
Oncotarget. 7:44252–44265. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Tyszka-Czochara M, Konieczny P and Majka
M: Caffeic acid expands anti-tumor effect of metformin in human
metastaticcervical carcinoma HTB-34 cells: Implications of AMPK
activation andimpairment of fatty acids de novo biosynthesis. Int J
Mol Sci. 18:pii: E462. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Lucenay KS, Doostan I, Karakas C, Bui T,
Ding Z, Mills GB, Hunt KK and Keyomarsi K: Cyclin E associates with
the lipogenic enzyme ATP-citrate lyase to enable malignant growth
of breast cancer cells. Cancer Res. 76:2406–2418. 2015. View Article : Google Scholar
|